Abstract
Objective:
Suicide is a serious public health concern, but little is known about the relationship between access to mental health care and suicide deaths, and whether suicide rates differ by mental health provider Health Professional Shortage Areas (HPSAs). This study investigated the associations between mental health HPSAs and suicide rates.
Method:
We used generalized linear mixed models to test the associations between HPSAs and suicide rates from 2010 to 2018. For each county during a 3-year period, the total number of suicides was obtained from Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (WONDER).
Results:
Mental health HPSAs had higher suicide rates (adjusted incidence rate ratio (IRR), 1.06 [95% CI, 1.03–1.09]). The interaction terms of mental health HPSAs and time (adjusted IRR, 1.01 [95% CI, 1.00–1.01]) showed that the association between mental health shortage areas and suicide rates has increased over time.
Conclusions:
Suicide rates are more common in mental health provider shortage areas, and this association has been growing over time. The study’s findings suggest that many communities in the US are likely facing simultaneous challenges of limited access to mental health care, social and economic disadvantage, and high burden of suicide.
Keywords: Access to care, mental health shortage areas, suicide rates
Introduction
The increasing rate of suicide in the United States (US) is a major public health concern. Data from the Centers for Disease Control and Prevention (CDC) reveal that in the US, the overall age-adjusted rate of suicide increased 35%, from 10.5 per 100,000 to 14.2 from 1999 to 2018.1 Suicide rates have been increasing more rapidly in more rural areas in recent years and it has been suggested that these geographic disparities in suicide rates reflect suicide risk factors known to be prevalent in less urban areas, such as limited access to mental health care.2
Although the availability of behavioral health services has been increasing,3access to mental health treatment continues to be a major issue.4–7 Data from the CDC’s National Violent Death Reporting System showed that from 2005 to 2010, more than seventy percent of all suicide decedents did not receive mental health treatment two months before death.8In fact, studies have shown that states receiving less federal mental health aid, having greater proportion of people without health insurance, and having less psychiatrist supply have with higher suicide rates.9 In the US, the number of active psychologists declined from 1 per 3,652 people in 2008 to 1 per 3,802 people in 2013 and number of active psychiatrists declined from 1 per 7,825 people to 1 per 8,476 people during the same time period.10 However, these seemingly minor changes in provider supply in the aggregate do not account for their uneven distribution across the US, with a more drastic lack of providers in certain areas, particularly rural areas, and other areas having an overabundance of providers (e.g., California and New York). In addition, the number of psychiatrists may be a limited proxy for access to care since other mental health care workforce, including psychologists, social workers, psychiatric nurses, and other therapists provide the bulk of care in mental health settings and also provide suicide interventions in various settings.11
Mental health provider Health Professional Shortage Areas (HPSAs) represent an indicator of mental health care workforce shortage in the US based upon the ratio of residents to mental health providers.12 This ratio threshold depends on the need for mental health care in the area, which is determined based on percentage living under poverty level, age distribution, and prevalence of substance misuse including alcohol misuse.12 Prior literature has shown that individuals with serious mental illnesses living in shortage areas are more likely to have general hospital admissions.13 Mental health HPSAs have also been associated with poorer health outcomes, such as higher county-level rates of neonatal abstinence syndrome14 and higher state-level suicide rates,15 likely due to undertreated substance use disorders and lack of access to care. It has also been shown that an increase in behavioral health providers was associated with a slight decrease in firearm-related suicides.16 To our knowledge no studies have investigated the association between mental health provider shortage areas at the county level and suicide rates. Furthermore, no studies have investigated the relationship between these shortage areas and suicide rates differ based upon whether suicides were firearm or non-firearm related. A better understanding of this association would inform interventions at community levels aimed at decreasing suicide rates.
To address this gap in the literature, this study aimed to (1) describe the trend of mental health HPSAs, (2) test the longitudinal association between mental health HPSA status and suicide rates (overall, firearm-related, and non-firearm-related) in the US from 2010 to 2018, and (3) test whether this association between HPSAs and suicide rates has changed over time and differs by rurality.
We hypothesized that suicide rates will be significantly greater in counties with mental health provider shortages, and that the association between mental health HPSAs and suicide rates will be greater over time and in more rural counties.
Methods
This study was a secondary analysis with variables drawn from various datasets and included suicide rates among adults age 25 and older from January 1, 2010, to December 31, 2018 in counties designated as "none" or "whole" mental health HPSAs.
1. Mental health provider HPSAs
Mental health HPSAs, designated by the Health Resources and Services Administration (HRSA), was obtained from the Area Health Resource Files.17 Mental health HPSAs are designated based on the ratio of mental health providers, which include psychiatrists, clinical psychologists, clinical social workers, psychiatric nurse specialists, and marriage and family therapists, to residents in specific geographic counties.18 HPSAs for years 2010, 2013, and 2016 were used to analyze suicide rates for years 2010–2012, 2013–2015, and 2016–2018, respectively.
Counties designed as "partial" were excluded from this study, as done in prior literature19,20 because this status was difficult to interpret. A partial county could have one small part of town without or with a shortage, which would be more reflective of either none or whole mental health HPSA, respectively. Because of the ambiguity of the partial status and to minimize the error of associating counties with or without predominant shortages of providers and suicide rates, we did not include them in this study. Nevertheless, a sensitivity analysis (described below) that included "partial" mental health HPSAs was conducted.
2. Suicides
Suicides were coded as X60-X84, Y87.0, and U03 in the International Classification of Diseases, Tenth Revision, which was obtained from the CDC Wide-ranging Online Data for Epidemiologic Research (WONDER) records.21 Due to the classification of age range in this database, 25 was the youngest age for an adult and this age range had been used in previous mortality studies.22,23
To account for access to firearms as a potential confounder, we analyzed firearm- and non-firearm-related suicide rates separately. Firearm-related suicides were coded as ICD-10 codes: X72–X74 and non-firearm-related suicides was calculated as the difference between suicides and firearm-related suicides. Total suicides, firearm-related suicides, non-firearm-related suicides, and population were each aggregated in 3-year periods per county for years 2010 to 2012, 2013 to 2015, and 2016 to 2018 as done in prior studies3 and to limit missing data.
3. County-level population characteristics
County-level socioeconomic variables were derived from the American Community Survey (ACS) 5-Year Estimates for years 2010 (2006–2010), 2013 (2009–2013), and 2016 (2012–2016)24 except for proportion of the county population without health insurance, which was measured from the ACS 5- Year Estimates for 2012 (2008–2012) because data from prior years were not available. The socioeconomic variables were chosen a priori due to their association with increased suicide rates in prior literature.3 These variables include percentage with less than high school or equivalent educational attainment among the population ages 25 and older, percentage of families and people whose income in the past 12 months is below the poverty level among those 18 years and older, percentage of adults without health insurance, percentage of males, median age, and percentage of white non-Hispanic or Latino race/ethnicity.
Social capital index was derived from the Social Capital Project.25 Prior research showed that social capital index was associated with lower suicide rates in the US so this variable was included.3 Social capital index was created using principal component analyses from the following population characteristics: (1) Family Unity Subindex: share of births in past year to women who were unmarried, share of women ages 35–44 who are currently married (and not separated), share of children living in a single-parent family; (2) Community Health Subindex: registered non-religious non-profits per 1,000; religious congregations per 1,000; informal Civil Society Sub-Index: combination of share who volunteered, attended a public meeting, reported having worked with neighbors to fix/improve something, served on a committee or as an officer, attended a meeting where politics was discussed, and took part in a demonstration in the past year; (3) Institutional Health Subindex: averaged (over 2012 and 2016) of votes in the presidential election per citizen ages 18 and older; mail-back response rates for the 2010 census; (4) Violent crimes per 100,000.25 The social capital index scores range from −4.3 to 2.9.
The rural-urban continuum codes (RUCC) was derived from the US Department of Agriculture’s Economic Research Service.26 The RUCC is a 9-category classification system based on the county population and adjacency to large metropolitan areas, which we used to examine how effects of independent variables may be modified by rurality. We collapsed the nine categories into three: 1, 2, or 3 were designated as living in a metropolitan county; 4, 6, or 8 as rural county adjacent to metropolitan county; and 5, 7, or 9 as rural remote county as categorized in prior literature.14 For this collapsed variable, called Rurality, higher values indicate greater rurality.
4. Data included, excluded, and missing
For 2010 to 2012, 2,583 counties were designated as "none" or "whole" mental health HPSAs; 554 were "partial" mental health HPSAs and were excluded. There were 144 missing data elements from county-level characteristics including suicide rates. Thus, a total of 2,439 counties were included for this period. For 2013 to 2015, 2,478 counties were designated as "none" or "whole" mental health HPSAs; 659 were "partial" mental health HPSAs and were excluded. There were 145 missing data elements from county-level characteristics. A total of 2,333 counties were included for this period. For 2016 to 2018, 2,402 counties were designated as "none" or "whole" mental health HPSAs; 735 were "partial" mental health HPSAs and were excluded. There were 142 missing data elements from county-level characteristics. A total of 2,260 counties were included for this period.
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline for cross-sectional studies.27
5. Statistical Analysis
Descriptive statistics were calculated and the collinearity among the variables of interest was evaluated. A generalized linear mixed model with maximum likelihood estimation approach was used to test the longitudinal relationship between mental health HPSA status and 3-year suicide rates from 2010 to 2018.
Chi-squared test compared unadjusted suicide rates between counties that were and were not mental health shortage areas. Incidence rate ratios (IRRs) and corresponding 95% confidence intervals were estimated using univariate and multivariate negative binomial regressions for Models A, B, and C. Model A used county-level number of suicides per 3-year time periods as the dependent variable, corresponding population during this time as the exposure variable, counties as a random effect, and the following fixed effects variables: mental health HPSAs, rurality, time, low educational attainment, poverty, social capital index, without health insurance, male gender, population ages 65 and over, and non-Hispanic/Latino white race. For sensitivity analysis, suicide rates among "partial" and "whole" mental health HPSAs were grouped together and compared with rates among counties without any mental health shortage areas.
We analyzed firearm-related and non-firearm-related suicide deaths per 3-year time periods as two dependent variables in separate analyses in Model B and Model C, respectively. The exposure, random effects, and fixed effects variables for Model B and Model C were the same as Model A.
Investigations of interaction terms between mental health HPSAs and (1) time and (2) rurality were completed in a separate analysis. Each interaction term was evaluated independently, and stratified analysis was conducted on any significant interaction term(s).
All testing was 2-sided and statistical significance was set at p<.05. Analyses were conducted using Stata/MP statistical software version 13.0 (StataCorp Inc) and SPSS version 24.0.
Results
This study included 7,032 counties across three time periods. During the study period, the percentages of counties with mental health HPSAs increased from 83.5% in 2010 to 87.6% in 2016. The suicide rate (per 100,000 people) increased from 17.1 to 21.7 from 2010–2012 to 2016–2018 (Table 1).
Table 1.
Demographics.
| All years* | 2010–2012 | 2013–2015 | 2016–2018 | |
|---|---|---|---|---|
| Total counties | 7032 | 2439 | 2333 | 2260 |
| Population | 866,862,580 | 331,041,622 | 324,469,966 | 211,350,992 |
| Suicides | 161,674 | 56,525 | 59,366 | 45,783 |
| Suicide rates per 100,000 | 18.7 | 17.1 | 18.3 | 21.7 |
| Population characteristics, mean (SD) | ||||
| Low education | 64.2 (6.6) | 63.7 (6.6) | 64.5 (6.6) | 64.5 (6.6) |
| Poverty | 14.3 (5.7) | 13.7 (5.5) | 14.7 (5.6) | 14.7 (5.8) |
| Social capital index | 0.1 (1.0) | 0.1 (1.0) | 0.1 (1.0) | 0.1 (1.0) |
| No health insurance | 14.4 (5.8) | 15.3 (5.8) | 15.3 (5.7) | 12.4 (5.3) |
| Male gender | 50.1 (2.4) | 50 (2.3) | 50.1 (2.4) | 50.2 (2.5) |
| White non-Hispanic race/ethnicity | 78.9 (19.6) | 79.7 (19.5) | 78.6 (19.8) | 78.3 (19.7) |
| Age | 41.1 (4.8) | 41.1 (4.8) | 41.1 (4.8) | 41 (4.9) |
| Counties that were mental health HPSAs (%) | 6030 (85.8%) | 2036 (83.5%) | 2015 (86.4%) | 1979 (87.6%) |
| Population | 665,593,056 | 248,697,558 | 260,122,316 | 156,773,182 |
| Suicides | 126,662 | 42,733 | 48,074 | 35,855 |
| Suicide rates per 100,000 | 19.0 | 17.2 | 18.5 | 22.9 |
| Population characteristics, mean (SD) | ||||
| Low education | 63.8 (6.3) | 63.3 (6.2) | 64.1 (6.4) | 64.1 (6.3) |
| Poverty | 14.8 (5.6) | 14.2 (5.5) | 15.2 (5.6) | 15.1 (5.7) |
| Social capital index | 0.1 (1.1) | 0 (1.1) | 0.1 (1.1) | 0.1 (1.1) |
| No health insurance | 14.7 (5.9) | 15.7 (5.9) | 15.7 (5.8) | 12.7 (5.3) |
| Male gender | 50.2 (2.5) | 50.1 (2.4) | 50.2 (2.4) | 50.3 (2.5) |
| White non-Hispanic race/ethnicity | 78.7 (20.1) | 79.4 (20.2) | 78.5 (20.2) | 78.1 (20.0) |
| Age | 41.1 (4.9) | 41.1 (4.9) | 41.1 (4.9) | 41 (5.0) |
| Counties that were not mental health HPSAs (%) | 1002 (14.2%) | 403 (16.5%) | 318 (13.6%) | 281 (12.4%) |
| Population | 199,371,112 | 80,949,274 | 64,104,927 | 54,316,911 |
| Suicides | 34,703 | 13,584 | 11,239 | 9880 |
| Suicide rates per 100,000 | 17.4 | 16.8 | 17.5 | 18.2 |
| Population characteristics, mean (SD) | ||||
| Low education | 66.6 (7.6) | 65.8 (7.7) | 66.9 (7.4) | 67.4 (7.5) |
| Poverty | 11.5 (5.0) | 11.2 (5.0) | 11.7 (5.1) | 11.5 (5.0) |
| Social capital index | 0.2 (0.8) | 0.2 (0.8) | 0.2 (0.8) | 0.3 (0.8) |
| No health insurance | 12.4 (4.9) | 13.2 (4.6) | 13.1 (4.9) | 10.3 (4.6) |
| Male gender | 49.4 (1.7) | 49.3 (1.6) | 49.4 (1.8) | 49.4 (1.8) |
| White non-Hispanic race/ethnicity | 80.3 (16.4) | 81.3 (15.5) | 79.6 (16.8) | 79.4 (17) |
| Age | 41 (4.2) | 41.1 (4.0) | 40.9 (3.9) | 41 (4.7) |
Abbreviations: mental health HPSAs, mental health provider Health Professional Shortage Areas; low education, percentage with less than high school or equivalent educational attainment among the population ages 25 and older, poverty, percentage of families and people whose income in the past 12 months is below the poverty level among those 18 years and older; no health insurance, percentage of adults without health insurance; male gender, percentage of males; white non-Hispanic race/ethnicity, percentage of white non-Hispanic or Latino race/ethnicity.
Note: Demographic characteristics only reflected US counties that were included in this study.
For “All years,” the populations across each of the three-year periods were aggregated.
Among metropolitan counties, mental health HPSAs increased from 64.6% in 2010 to 87.3% in 2013 to 96.1% in 2016. Among rural counties adjacent to metropolitan counties, mental health HPSAs increased from 83.7% in 2010 to 84.6% in 2013 to 93.1% in 2016. Among rural counties not adjacent to metropolitan counties, mental health HPSAs increased from 84.5% in 2010 to 86.8% in 2013 to 93.7% in 2016.
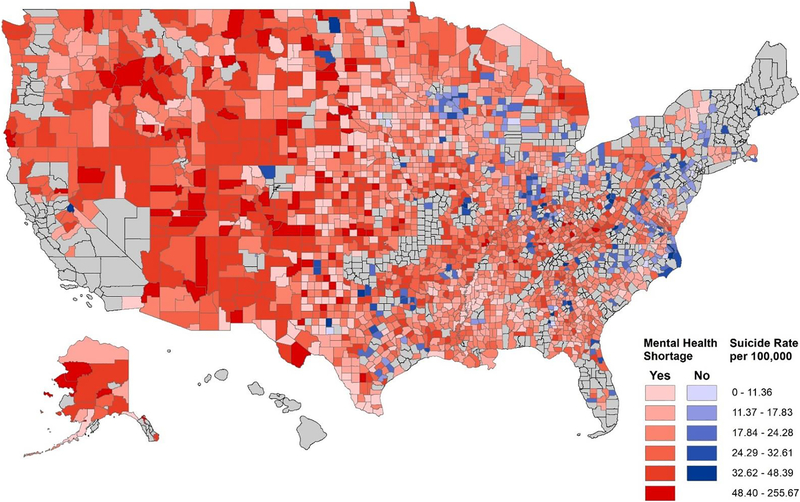
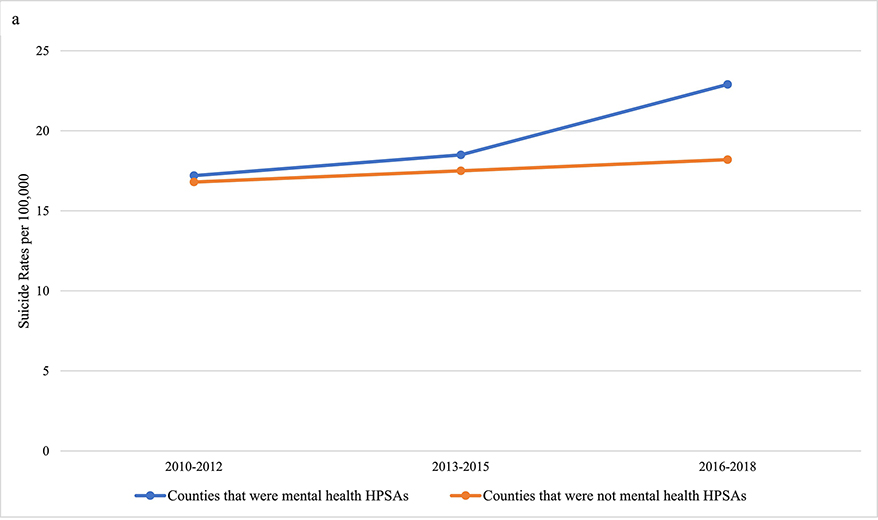
There was substantial variation of suicide rates across counties that were and were not mental health HPSAs (Figure 1). Suicide rates were higher in mental health HPSAs compared with non-HPSAs (overall average: 19.0 vs 17.4 per 100,000 people, respectively) (p<0.001). Suicide rates in counties that were mental health HPSAs increased from 17.2 in 2010–2012 to 18.5 in 2013– 2015 to 22.9 in 2016–2018 per 100,000 people. Suicide rates in counties that were not mental health HPSAs increased from 16.8 in 2010–2012 to 17.5 in 2013–2015 18.2 in 2016–2018 per 100,000 people (Figure 2a).
Figure 1. Heat map of mental health HPSAs and county-level suicide rates, 2016–2018.
Abbreviations: mental health HPSAs, mental health provider Health Professional Shortage Areas Note: Counties are outlined in black. Red highlighted counties represent counties that were mental health HPSAs. Blue highlighted counties represent counties that were not mental health pHPSAs. Gray highlighted counties were excluded from this analysis due to partial mental health HPSA status or missing data. Darker red and blue colors in gradations represent higher suicide rates.
Figure 2a. Unadjusted suicide rates by county-level mental health HPSAs status from 2010 to 2018.
In the multivariate analysis (Table 2; Model A), mental health HPSAs (adjusted IRR, 1.06 [95% CI, 1.03–1.09], p < 0.001), time (adjusted IRR, 1.03 [95% CI, 1.03–1.03], p < 0.001), proportion of the population without health insurance (adjusted IRR, 1.02 [95% CI, 1.01–1.02], p < 0.001), proportion of the population that were male (adjusted IRR, 1.01 [95% CI, 1.01–1.02], p < 0.001), and proportion of the population that were white non-Hispanic race/ethnicity (adjusted IRR, 1.01 [95% CI, 1.01–1.01], p < 0.001) were associated with increased suicide rates. Social capital index (adjusted IRR, 0.93 [95% CI, 0.91–0.94], p < 0.001) was associated with decreased suicide rates. Sensitivity analysis showed that mental health HPSAs, that included "partial" mental health HPSA counties, was significantly associated with suicide rates (adjusted IRR, 1.07 [95% CI, 1.04–1.09], p < 0.001) even after controlling for the same covariates as in Model A (adjusted IRR, 1.03 [95% CI, 1.01–1.05], p < 0.011).
Table 2.
Generalized Linear Mixed Models with Negative Binomial Distributions.
| Univariate | General Suicide Rates (Model A) | Firearm-related Suicide Rates (Model B) | Non-firearm-related Suicide Rates (Model C) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Population characteristic | IRR | 95% CI | p | aIRR | 95% CI | p | aIRR | 95% CI | p | aIRR | 95% CI | p |
| Mental health HPSAs | 1.10 | 1.07, 1.14 | <0.001 | 1.06 | 1.03, 1.09 | <0.001 | 1.07 | 1.03, 1.11 | <0.001 | 1.05 | 1.01, 1.09 | 0.010 |
| Rurality | 1.02 | 1.01, 1.03 | <0.001 | 1.00 | 0.99, 1.01 | 0.948 | 1.00 | 0.99, 1.02 | 0.711 | 1.00 | 0.98, 1.01 | 0.649 |
| Time | 1.02 | 1.02, 1.02 | <0.001 | 1.03 | 1.03, 1.03 | <0.001 | 1.03 | 1.03, 1.04 | <0.001 | 1.03 | 1.03, 1.03 | <0.001 |
| Low Education | 1.00 | 0.99, 1.00 | <0.001 | 1.00 | 1.00, 1.00 | 0.005 | 1.00 | 0.99, 1.00 | 0.003 | 1.01 | 1.01, 1.01 | <0.001 |
| Poverty | 1.01 | 1.00, 1.01 | <0.001 | 1.00 | 1.00, 1.00 | 0.428 | 1.01 | 1.00, 1.01 | <0.001 | 0.99 | 0.98, 0.99 | <0.001 |
| Social Capital Index | 0.99 | 0.98, 1.01 | 0.390 | 0.93 | 0.91, 0.94 | <0.001 | 0.93 | 0.91, 0.95 | <0.001 | 0.92 | 0.90, 0.94 | <0.001 |
| No health insurance | 1.00 | 1.00, 1.00 | 0.888 | 1.02 | 1.01, 1.02 | <0.001 | 1.03 | 1.02, 1.03 | <0.001 | 1.00 | 1.00, 1.01 | 0.093 |
| Male gender | 1.01 | 1.01, 1.02 | <0.001 | 1.01 | 1.01, 1.02 | <0.001 | 1.01 | 1.00, 1.01 | 0.104 | 1.03 | 1.02, 1.03 | <0.001 |
| White non-Hispanic race/ethnicity | 1.00 | 1.00, 1.00 | <0.001 | 1.01 | 1.01, 1.01 | <0.001 | 1.01 | 1.01, 1.01 | <0.001 | 1.01 | 1.00, 1.01 | <0.001 |
| Median age | 1.01 | 1.00, 1.01 | <0.001 | 1.00 | 1.00, 1.01 | <0.001 | 1.01 | 1.00, 1.01 | <0.001 | 1.00 | 1.00, 1.01 | 0.007 |
| Variance explained | 4.62% | 8.80% | 7.10% | |||||||||
Abbreviations: IRR, incidence rate ratio; aIRR, adjusted incidence rate ratio; mental health HPSAs, mental health provider Health Professional Shortage Areas; low education, percentage with less than high school or equivalent educational attainment among the population ages 25 and older; poverty, percentage of families and people whose income in the past 12 months is below the poverty level among those 18 years and older; no health insurance, percentage of adults without health insurance; male gender, percentage of males; white non-Hispanic race/ethnicity, percentage of white non-Hispanic or Latino race/ethnicity.
Mental health HPSAs were significantly associated with suicide rates for both firearm (adjusted IRR, 1.07 [95% CI, 1.03–1.11], p < 0.001) and non-firearm-related (adjusted IRR, 1.05 [95% CI, 1.01–1.09], p = 0.010) suicide rates, respectively (Table 2; Models B and C).
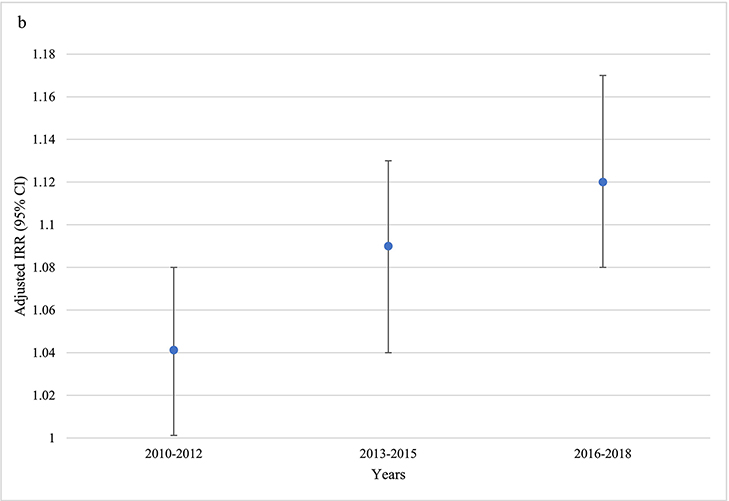
Interactions of mental health HPSAs x time (adjusted IRR, 1.01 [95% CI, 1.00–1.01], p = 0.002) was significant. Interaction of mental health HPSAs x rurality was also significant (adjusted IRR, 1.03 [95% CI, 1.00–1.05], p = 0.042). To better interpret each significant interaction term, results were stratified by the three time periods and rurality.
Adjusted IRRs between mental health HPSAs and suicide rates increased during this period (adjusted IRR, 1.04 [95% CI, 1.00–1.08], p = 0.047 for 2010–2012; adjusted IRR, 1.09 [95% CI, 1.04–1.13], p < 0.001 for 2013–2015; adjusted IRR, 1.12 [95% CI, 1.08–1.17], p < 0.001 for 2016–2018) (Figure 2b).
Figure 2b. Adjusted incidence rate ratio of suicide rates by mental health pHPSAs from 2010 to 2018.
Abbreviations: aIRR, adjusted incidence rate ratio
Note: Models for each time period adjusted for rurality, percentage with less than high school or equivalent educational attainment among the population ages 25 and older, percentage of families and people whose income in the past 12 months is below the poverty level among those 18 years and older, social capital index, percentage of adults without health insurance, percentage of males, percentage of white non-Hispanic or Latino race/ethnicity, and median age.
Adjusted IRRs between mental health HPSAs and suicide rates were higher in more rural counties (adjusted IRR, 1.06 [95% CI, 1.02–1.10], p = 0.003 for metropolitan counties; adjusted IRR, 1.06 [95% CI, 1.01–1.10], p = 0.017 for rural counties adjacent to metropolitan counties; adjusted IRR, 1.15 [95% CI, 1.07–1.24], p < 0.001 for rural counties not adjacent to metropolitan counties).
Discussion
This study examined county-level suicide rate trajectories for adults aged 25 and older in the US from 2010 to 2018. Among the US counties that were included in this study, the percentage of mental health shortage areas increased from 83.5% to 87.6%. This increase in shortage areas was more than three times higher among metropolitan as compared to the most rural counties. During this period, suicide rates increased from 17.1 to 21.7. Although counties with and without mental health shortage areas both experienced increases in suicide rates, those with shortage areas had greater increases in suicide rates.
Overall, suicide rates increased by six percent among counties designated as mental health HPSAs as compared with those without HPSAs after adjusting for other socioeconomic characteristics from 2010 to 2018. The relationship between mental health HPSAs and suicide rates was also significant for non-firearm-related suicide rates, suggesting that this association is not likely to be solely explained by greater access to firearms in provider shortage areas. The modest effect size of these findings reminds us that multiple factors likely contribute to suicide and that reducing suicide rates will require a multifaceted approach. Our study also suggests that mental health provider shortage areas might be increasingly more relevant as the increased risk of suicide in mental health shortage areas has tripled during the eight-year study period. And this increased suicide risk among shortage areas was greater in more rural counties.
While this study did not assess causal pathways, it is possible that reduced access to mental health services in these shortage areas could lead to a higher burden of under-treated or untreated mental illnesses. It could be that low supply of mental health providers, high demand of mental health care, or the combination of both factors could drive the increase in suicide rates. Mental health providers are trained to provide suicide prevention interventions shown to be associated with decreased suicidal behavior.28,29 For areas where there might be higher mental health demands such as a higher prevalence of substance use disorders, having adequate access to mental health treatment could reduce substance misuse and development of a substance use disorder, leading to a lower risk of suicidal behavior.30,31
Our study also found that other county-level population characteristics including rurality and poverty were significantly associated with increased suicide rates in the univariate model, which is consistent with previous studies.3,32 However, the association between these characteristics and suicide rates became non-significant after adjusting for other population characteristics, suggesting that these other characteristics including mental health provider shortage areas might partially explain why suicide rates are higher in more rural areas of the country. Moreover, the significant interaction of mental health shortage areas and rurality suggests that suicide rates are higher in more rural areas especially in areas with more limited health resources such as mental health provider shortages. Interestingly, a higher percentage of people without health insurance was associated with greater firearm-related suicides, but not significantly associated with non-firearm-related suicides. Since there are specific clinical interventions targeted at firearm access in suicide risk assessments, having health insurance could have a significant impact on firearm-related suicide via access to firearm-related suicide intervention.
There are several limitations to this study. First, the observed associations could be due to confounders not accounted for in this study. For example, prevalence of substance use disorders, which has been associated with higher rates of suicide, may be associated with mental health HPSAs and may also be a more direct contributor to suicide.3 Second, this study used counties as units for suicide rates and variation within large or densely populated counties may exist for many of the metrics measured. Third, national mortality data may misclassify suicide deaths, leading to underestimation.
Our findings suggest that mental health provider shortage areas face higher burden of suicide rates even after adjusting for socioeconomic and other county-level factors. While this study did not assess for causal pathways for this association, it is possible that reduced access to mental health providers in shortage areas could lead to greater under-treated and untreated mental illnesses, leading to higher suicide rates due to delays in diagnosis and resource shortages. Further investigation of the relationship between shortages of mental health professionals and suicide deaths is needed. Nevertheless, this study’s findings suggest that communities in the US are likely facing simultaneous challenges of limited access to mental health care, social and economic disadvantage, and high burden of suicide. Regardless of the causal relationship between mental health HPSAs and suicide rates, these findings may help identify communities at risk for elevated suicide rates, which could be a priority for allocating mental health resources to areas with greater risk for suicide.
Acknowledgement
This work was supported in part by the National Institutes of Mental Health (NIMH) grant R25-MH101079 to Dr. Ku.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hedegaard H, Curtin SC, Warner M. Increase in Suicide Mortality in the United States, 1999–2018; 2020. [PubMed]
- 2.Kegler SR, Stone DM, Holland KM. Trends in Suicide by Level of Urbanization — United States, 1999–2015. MMWRMorb Mortal Wkly Rep. 2017;66(10):270–273. 10.15585/mmwr.mm6610a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steelesmith DL, Fontanella CA, Campo J V, Bridge JA, Warren KL, Root ED. Contextual Factors Associated With County-Level Suicide Rates in the United States, 1999 to 2016. JAMA Netw open. 2019;2(9):e1910936. 10.1001/jamanetworkopen.2019.10936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, Dernier O, Frank RG, et al. Prevalence and Treatment of Mental Disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–2523. 10.1056/NEJMsa043266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McAlpine DD, Mechanic D. Utilization of specialty mental health care among persons with severe mental illness: the roles of demographics, need, insurance, and risk. Health Serv Res. 2000;35(1 Pt 2):277–292. [PMC free article] [PubMed] [Google Scholar]
- 6.Shim RS, Baltrus P, Ye J, Rust G. Prevalence, treatment, and control of depressive symptoms in the United States: Results from the National Health and Nutrition Examination Survey (NHANES), 2005–2008. J Am Board FamMed. 2011;24(1):33–38. 10.3122/jabfm.2011.01.100121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang PS, Angermeyer M, Borges G, et al. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):177–185. [PMC free article] [PubMed] [Google Scholar]
- 8.Niederkrotenthaler T, Logan JE, Karch DL, Crosby A. Characteristics of U.S. Suicide Decedents in 2005–2010 Who Had Received Mental Health Treatment. Psychiatr Serv. 2014;65(3):387–390. 10.1176/appi.ps.201300124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tondo L, Albert MJ, Baldessarini RJ. Suicide rates in relation to health care access in the United States: An ecological study. J Clin Psychiatry. 2006;67(4):517–523. 10.4088/JCP.v67n0402 [DOI] [PubMed] [Google Scholar]
- 10.Lin L, Nigrinis A, Christidis P, Stamm K. Demographics of the U.S. Psychology Workforce Findings from the American Community Survey American Psychological Association Center for Workforce Studies.; 2015.
- 11.Institute of Medicine. The Mental Health and Substance Use Workforce for Older Adults: In Whose Hands? National Academies Press; 2012. 10.17226/13400 [DOI] [PubMed] [Google Scholar]
- 12.42 CFR Appendix C to Part 5 - Criteria for Designation of Areas Having Shortages of Mental Health Professionals - Content Details - CFR-2007-title42-vol1-part5-appC. https://www.govinfo.gov/app/details/CFR-2007-title42-vol1/CFR-2007-title42-vol1-part5-appC. Accessed July 2, 2020.
- 13.Moseley C, Shen J, Cochran C. Mental Health Services Availability and Admission of the Seriously Mentally Ill From the Emergency Department - PubMed. J Heal Hum Serv Adm. 2008;31(3):292–308. [PubMed] [Google Scholar]
- 14.Patrick SW, Faherty LJ, Dick AW, Scott TA, Dudley J, Stein BD. Association among County-Level Economic Factors, Clinician Supply, Metropolitan or Rural Location, and Neonatal Abstinence Syndrome. JAMA - J Am Med Assoc. 2019;321(4):385–393. 10.1001/jama.2018.20851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson KF, Brookover DL. Counselors’ Role in Decreasing Suicide in Mental Health Professional Shortage Areas in the United States. J Ment Heal Couns. 2020;42(2):170–186.. 10.17744/mehc.42.2.06 [DOI] [Google Scholar]
- 16.Goldstein E V, Prater LC, Wickizer TM. Behavioral health care and firearm suicide: Do states with greater treatment capacity have lower suicide rates? Health Aff. 2019;38(10):1711–1718. 10.1377/hlthaff.2019.00753 [DOI] [PubMed] [Google Scholar]
- 17.Health Resources and Services. Area Health Resources Files. https://data.hrsa.gov/topics/health-workforce/ahrf. Accessed March 30, 2020.
- 18.Public Health Service. Criteria for designation of mental health professional shortage areas--PHS. Final rule. Fed Regist. 1992;57(14):2473–2480. [PubMed] [Google Scholar]
- 19.Brown TM, Parmar G, Durant RW, et al. Health professional shortage areas, insurance status, and cardiovascular disease prevention in the reasons for geographic and racial differences in stroke (REGARDS) study. J Health Care Poor Underserved. 2011;22(4):1179–1189. 10.1353/hpu.2011.0127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Durant RW, Parmar G, Shuaib F, et al. Awareness and management of chronic disease, insurance status, and health professional shortage areas in the REasons for Geographic and Racial Differences in Stroke (REGARDS): A cross-sectional study. BMC Health Serv Res. 2012;12(1):208. 10.1186/1472-6963-12-208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. CDC WONDER. https://wonder.cdc.gov/. Accessed March 28, 2020.
- 22.Curtin SC, Arias E. Mortality Trends by Race and Ethnicity Among Adults Aged 25 and over: United States, 2000–2017 Key Findings Data from the National Vital Statistics System.; 2000.
- 23.Curtin SC, Tejada-Vera B. Mortality Among Adults Aged 25 and Over by Marital Status: United States, 2010–2017. NCHS Heal E-Stat. 2019. [Google Scholar]
- 24.US Census Bureau. American FactFinder - Search. https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t. Accessed March 22, 2020.
- 25.Vice Chairman’s staff, 115th Cong. 2nd Sess. U.S. Congress, Joint Economic Committee, Social Capital Project. “The Geography of Social Capital in America.”; 2018.
- 26.Economic Research Service. USDA ERS - Rural-Urban Continuum Codes. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/. Accessed March 22, 2020.
- 27.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. UroToday Int J. 2009;2(2). 10.4038/jccpsl.v13i2.2965 [DOI] [Google Scholar]
- 28.D’Anci KE, Uhl S, Giradi G, Martin C. Treatments for the prevention and management of suicide. Ann Intern Med. 2019;171(5):334–342. 10.7326/M19-0869 [DOI] [PubMed] [Google Scholar]
- 29.Doupnik SK, Rudd B, Schmutte T, et al. Association of Suicide Prevention Interventions With Subsequent Suicide Attempts, Linkage to Follow-up Care, and Depression Symptoms for Acute Care Settings. JAMA Psychiatry. 2020. 10.1001/jamapsychiatry.2020.1586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holmstrand C, Bogren M, Mattisson C, Brådvik L. Long-term suicide risk in no, one or more mental disorders: The Lundby Study 1947–1997. Acta Psychiatr Scand. 2015;132(6):459–469. 10.1111/acps.12506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bohnert KM, Ilgen MA, Louzon S, McCarthy JF, Katz IR. Substance use disorders and the risk of suicide mortality among men and women in the US Veterans Health Administration. Addiction. 2017;112(7):1193–1201. 10.1111/add.13774 [DOI] [PubMed] [Google Scholar]
- 32.Kegler SR, Stone DM, Holland KM. Trends in Suicide by Level of Urbanization — United States, 1999–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):270–273. 10.15585/mmwr.mm6610a2 [DOI] [PMC free article] [PubMed] [Google Scholar]