Abstract
Background:
Quadriceps strength asymmetry at the time of return-to-sport (RTS) after anterior cruciate ligament reconstruction (ACLR) contributes to altered landing mechanics. However, the impact of RTS quadriceps strength on longitudinal alterations in landing mechanics, a risk factor for poor knee joint health over time, is not understood. The purpose of this study was to test the hypothesis that young athletes with quadriceps strength asymmetry at the time of RTS clearance after ACLR would demonstrate asymmetric landing mechanics 2 years later compared to those without quadriceps strength asymmetry.
Methods:
We followed 57 young athletes (age at RTS=17.6±3.0 years; 77% females) with primary, unilateral ACLR for 2 years following RTS clearance. At RTS, we measured isometric quadriceps strength bilaterally and calculated limb-symmetry indices [LSI=(involved/uninvolved)x100%]. Using RTS quadriceps LSI, we divided participants into High-Quadriceps (HQ; LSI≥90%) and Low-Quadriceps (LQ; LSI<85%) groups. Two years later, we assessed landing mechanics during a drop-vertical jump (DVJ) task using three-dimensional motion analysis. We compared involved/uninvolved limb values and LSI between the HQ and LQ groups using Mann-Whitney U tests.
Results:
The LQ group (n=26) demonstrated greater asymmetry (lower LSI) during landing at 2 years post-RTS for knee flexion excursion (p=0.016) and peak vertical ground reaction force (p=0.006) compared to the HQ group (n=28). There were no group differences in uninvolved or involved limb values for all variables (all p>0.093).
Conclusion:
Young athletes after ACLR with quadriceps strength asymmetry at the time of RTS favored the uninvolved limb during DVJ landing 2 years later. These landing asymmetries may relate to long-term knee joint health after ACLR.
Keywords: ACL reconstruction, Strength, Biomechanics, Knee
1. INTRODUCTION
Anterior cruciate ligament (ACL) injuries most often occur in athletes participating in sports that involve cutting, pivoting, jumping, or landing.[2, 3] After ACL injury, ACL reconstruction (ACLR) is often performed, with goals of restoring joint stability and normalizing knee kinematics.[2, 3, 36] Despite surgery and post-operative rehabilitation, multiple previous studies demonstrate that individuals after ACLR demonstrate persistent alterations in movement patterns and knee loading when compared to individuals without a history of ACLR, in both daily tasks (such as walking and squatting)[9, 47, 53] and in dynamic, sport-related tasks (such as jumping, landing, and cutting).[7, 8, 13, 41, 42, 50]
During double-limb jumping and landing tasks, it has been observed that individuals after ACLR demonstrate knee-avoidant loading patterns.[7, 8, 28, 41, 42, 50] Specifically, individuals post-ACLR preferentially load the uninjured knee by shifting away from the injured knee, resulting in lower ground reaction forces[7, 28, 41, 42, 50] and sagittal-plane knee moments[7, 28, 50] in the ACL-reconstructed limb. Because abnormal and asymmetric knee loading and movement patterns during jump-landing tasks after ACLR are linked with 2nd ACL injury[43] and poor longitudinal knee function and joint health over time,[6, 19] it is critical that we identify modifiable clinical impairments associated with altered knee loading that can be treated during rehabilitation.
A key clinical impairment associated with altered knee loading in those after ACLR is quadriceps strength deficits/strength asymmetry. Despite the restoration of quadriceps strength being a primary goal during rehabilitation,[26, 34] strength deficits are persistent and pervasive in individuals following ACLR.[27, 51, 61] Recent cross-sectional studies at the time of (return-to-sport) RTS clearance have also shown that individuals with quadriceps strength asymmetry demonstrate significantly greater knee-avoidant joint loading during both single-leg landing[20, 39] and double-legged landing tasks,[50] compared to individuals without quadriceps strength asymmetry after ACLR and healthy individuals. Specific to double-legged landing, a recent cross-sectional study found that young athletes after ACLR with quadriceps strength asymmetry (>15% side-to-side deficit) at the time of RTS clearance demonstrated more preferential loading of the uninjured knee (ie., shifting away from the ACL-reconstructed knee) when compared with healthy young athletes and young athletes after ACLR with symmetric quadriceps strength (<10% side-to-side deficit).[50] These findings, alongside other previous work, contribute to a body of evidence demonstrating better knee-related function,[17, 39, 51] performance,[51] and knee loading[20, 39, 50] in individuals after ACLR with quadriceps symmetry within 10% of the uninjured limb, and support this strength symmetry value as a criterion threshold to be used in RTS readiness decision-making.[14, 26, 33]
However, the impact of quadriceps strength symmetry at the important decision-making time point of RTS clearance on knee loading over time after RTS is not currently well understood. It is important that we understand the association between quadriceps strength at RTS and longitudinal knee loading, because allowing athletes to RTS without sufficient quadriceps strength restoration/symmetry may increase the risk of 2nd ACL injury and long-term poor knee joint health via longitudinal altered knee joint loading. In the current study, we investigated if young athletes with and without quadriceps strength asymmetry at the time of RTS clearance demonstrated differences in double-legged drop-landing mechanics 2 years later. In addition, as secondary analyses, we examined the change in quadriceps strength symmetry between RTS clearance and 2 years post-RTS clearance, as well as if quadriceps strength symmetry measured at 2 years post-RTS clearance was associated with double-legged drop-landing mechanics also measured at 2 years post-RTS clearance. Our primary hypothesis was that young athletes after ACLR with quadriceps strength asymmetry at RTS clearance would demonstrate greater asymmetry during a double-legged drop-landing task 2 years later when compared to young athletes with symmetric quadriceps strength at RTS clearance. Additionally, we hypothesized that quadriceps strength symmetry would improve over the 2 years following RTS clearance, but that double-legged drop-landing symmetry at 2 years would not differ between those with and without quadriceps strength asymmetry when strength was measured at the 2 year time point.
2. METHODS
2.1. Participants
Participants in the current analysis took part in the larger ACL REconstruction Long-term outcomes in Adolescents and Young adults (ACL-RELAY) Study, described in our previous work.[18, 20, 22, 57] The ACL-RELAY Study is an ongoing, prospective study that evaluates longitudinal outcomes in young athletes after ACLR and takes place at Cincinnati Children’s Hospital Medical Center. We recruited a convenience sample of participants from orthopedic practices and physical therapy clinics in the greater Cincinnati/Northern Kentucky (USA) areas to participate in the study. To be enrolled, we required potential participants to have been previously cleared to RTS by their orthopaedic surgeon and rehabilitation specialist (within the previous 4 weeks), and we required that they were planning to return to regular participation in cutting and pivoting sports (greater than 50 hours per year). We did not control ACLR rehabilitation nor the decision of RTS clearance, including whether any RTS discharge criteria were used in this decision. We excluded potential participants for the following reasons: 1) low back pain or lower extremity injury or surgery in either limb (other than their primary ACL injury) that required the care of a physician in the previous year, or 2) sustaining a concomitant knee ligament injury alongside their primary ACL injury (with the exception grade 1 medial collateral ligament sprain). We did not exclude potential participants based on ACLR graft type, included potential participants with and without meniscus repair or partial menisectomy at the time of ACLR. All participants provided informed consent or parental permission/assent (when younger than 18 years old) prior to participating in the study, and all study procedures were approved by the Cincinnati Children’s Hospital Medical Center Institutional Review Board.
The participants in these analyses (n=57) were a subset of individuals from the overall ACL-RELAY Study that were recruited between 2007 and 2015 and completed both baseline (time of RTS clearance) and 2 year post-RTS clearance testing. Additionally, in the current analyses, we excluded participants from the ACL-RELAY Study with a modified ACLR procedure due to open epiphyseal plates in the tibia and/or femur or those with a history of bilateral or multiple ACL injuries. We have reported portions of the strength and motion capture data included in the current analyses in our previous work.[17, 19–21, 50] At the baseline study visit at the time of RTS clearance, we collected demographic data including age and sex via participant report. Operative reports, injury magnetic resonance imaging scans, and participant report were used at the RTS visit to determine the presence of meniscus injury at the time of ACLR and graft type used during ACLR. We evaluated pre-injury activity level using the Tegner activity scale[55] and body weight and height at RTS using a digital scale and stadiometer (Tanita; Arlington Heights, IL).
2.2. Measurement of Quadriceps Strength at RTS and 2 Years Post-RTS
At the time of RTS clearance, we measured isometric quadriceps muscle strength using an electromechanical dynamometer (Biodex Medical Systems; Shirley, NY). To perform quadriceps strength testing, we positioned the participants in the dynamometer with the trunk supported, the hips flexed to 90 degrees, and the knee joint flexed to 60 degrees and aligned with the dynamometer axis, as described previously.[17, 20, 50, 51] Additionally, we secured the distal shank to the resistance pad and stabilized the participants’ pelvis and testing limb thigh with straps. The participants performed one practice trial, followed by 3 recorded maximum-effort isometric contraction trials (5 seconds duration for each trial, 15 seconds of rest between each trial). We tested the uninvolved limb first, and provided real-time verbal feedback during testing to encourage maximal effort from the participants. These methods to measure quadriceps strength in individuals after ACL injuries and ACLR are able to differentiate asymmetries in strength between the involved and uninvolved limbs.[29, 51] Upon completing testing, we calculated the global peak torque value from among all 3 trials for both limbs and used these values to calculate a limb-symmetry index (LSI) using Equation 1 (Equation 1: LSI = [involved value/uninvolved value]*100%). We then used the RTS quadriceps strength LSI value to divide the participants into quadriceps strength symmetry groups: high-quadriceps (HQ; RTS quadriceps LSI≥90%) and low-quadriceps (LQ; RTS quadriceps LSI <85%) groups. These strength symmetry groups were based on: 1) previous studies that have divided individuals after ACLR based on quadriceps strength symmetry,[20, 39, 51] 2) recommended RTS criteria cutoffs for quadriceps strength symmetry after ACLR (ie., ≥90%),[26, 33] and 3) previous work indicating that limb differences greater than 10% reflect differences in muscle performance beyond measurement error.[49] In addition to measuring quadriceps strength at the RTS clearance testing visit, we also re-evaluated bilateral quadriceps strength at the 2-year post-RTS clearance testing visit, using the same methods described. The 2-year post-RTS testing visit took place within 6 weeks of 24 months following the baseline testing visit at the time of RTS clearance.
2.3. Three-Dimensional Motion Analysis during Landing at 2 Years Post-RTS
2.3.1. Drop-Vertical Jump Landing Task.
At the 2-year post-RTS testing visit, we evaluated double-legged drop-landing mechanics. To do so, the participants performed a drop-vertical jump (DVJ) task while we collected three-dimensional motion capture data. To complete the DVJ task, the participants stood on top a 31cm box, positioned directly behind two force plates. We instructed the participants to drop off the box, land on both feet, and immediately perform a maximum vertical jump with the arms directed toward an overhead target, as previously described.[15, 43, 50] Participants and the box were positioned to maximize the likelihood that each foot landed on a separate force plate. We collected 3 acceptable trials for each participant, and we excluded trials if the participants jumped vertically or forward off the box, did not land with each foot on a separate force plate, or paused during the transition from landing to the vertical jump portion. The DVJ task performed using these methods has been used extensively in previous work to identify young athletes at risk for initial ACL injury,[15] identify landing asymmetries after ACLR,[1, 41, 50] and to identify young athletes after ACLR at risk for second ACL injury.[43] Participants in the current study also previously performed the DVJ task during their study visit at the time of RTS clearance, and were familiar with the task.
2.3.2. Data Collection and Processing.
We collected kinematic and kinetic data during the DVJ task using a three-dimensional motion capture system that included 12 cameras (Eagle cameras; Motion Analysis Corporation, Santa Rosa, CA, USA; 240 Hz) and 2 embedded force plates (AMTI, Watertown, MA, USA; 1200 Hz) that were synchronized with the motion capture system. The motion capture system tracked 37 retroreflective markers that were adhered to the bilateral upper extremities (bilateral acromion processes, lateral epicondyles, wrists), trunk (sternal notch), pelvis (bilateral anterior superior iliac spines, 1 superior/lateral sacral offset marker), hips (bilateral greater trochanters), thighs (bilateral anterior lower thighs), knees (bilateral medial and lateral knee joint lines), shanks (bilateral tibial tubercles, lateral shanks, distal tibias), ankles (bilateral medial and lateral malleoli), and feet (bilateral base of the 5th metatarsals, between 1st/2nd metatarsal-phalangeal joint, heels, dorsum of feet) of each participant. The markers were used to determine joint centers and to track segment motion during the performance of each DVJ landing trial. Upon collecting the motion capture data, we used Visual 3D (Version 4.0; C-Motion, Inc., Germantown, MD, USA) and custom-written MATLAB (Mathworks, Natick, MA, USA) scripts to calculate joint angles and moments.[12, 16] Before calculating joint moments, we first match-filtered marker trajectories and force plate data using a low-pass 4th order Butterworth digital filter with a 12 Hz cutoff frequency.[24, 48] These experimental methods for processing biomechanical data have demonstrated high reliability in obtaining kinematic and kinetic variables of interest (VOIs) in previous studies.[11, 50] We calculated VOIs during the landing phase of the DVJ, which was defined as the period of time from initial contact on the force plate (when vGRF exceeded 10 newtons) until the participant’s center of mass reached its lowest vertical position.[20, 42, 43, 50] VOIs calculated included involved limb and uninvolved limb knee flexion excursion (degrees), peak internal knee extension moment (IKEM; newton-meters), and peak vertical ground reaction force (VGRF; newtons), based on previous DVJ studies in individuals after ACLR.[41, 42, 50] Peak values (IKEM, VGRF) were calculated as the mean of the peak of the 3 trials. We normalized peak IKEM and peak vGRF to body mass in kilograms and body weight in newtons, respectively. In addition to involved and uninvolved limb values, we also calculated LSI using Equation 1 for each VOI to determine DVJ landing symmetry (ie., preferential loading of one side or the other).
2.4. Statistical Analyses
We performed all statistical analyses using IBM SPSS Version 24.0 (SPSS Inc.; Chicago, IL).
2.4.1. RTS Quadriceps Group Comparisons.
We compared demographic, injury, and surgical data between the RTS HQ and LQ groups using independent t-tests and chi-square tests (α = 0.05). Prior to performing group comparisons of 2-year post-RTS biomechanical data, we examined normality for the biomechanical VOIs using histograms and quantile-quantile plots and examined group variance equality for the biomechanical VOIs using Levene’s tests. We found that the 2-year post-RTS biomechanical data did not meet the normality or equal variance assumptions of parametric statistical testing, and we were unable to successfully transform these data to meet these assumptions. Due to these findings, we compared 2-year post-RTS biomechanical landing data (involved limb values, uninvolved limb values, and LSI values) between the RTS HQ and LQ groups using Mann Whitney U tests (α = 0.05).
2.4.2. Secondary Analyses.
In addition to the primary analyses, we also compared between-limb values (involved limb vs uninvolved limb) for all 2-year post-RTS biomechanical VOIs (knee flexion excursion, peak IKEM, and peak VGRF) using Wilcoxon Signed Ranks Tests. Between-limb comparisons of 2-year post-RTS biomechanical VOIs were performed across the entire cohort (n=57), within the RTS HQ group (n=28), and within the RTS LQ group (n=26). We also performed secondary analyses to examine the change in quadriceps strength symmetry between RTS clearance and 2 years post-RTS. First, using 2-year post-RTS quadriceps strength data, we determined the proportions of participants categorized as HQ or LQ at 2 years post-RTS. In addition, we determined the proportions of participants that changed quadriceps strength groups over the 2 years following RTS clearance, as well as compared involved limb quadriceps strength values (Nm/kg), uninvolved limb quadriceps strength values (Nm/kg), and quadriceps strength LSI values between time points (RTS; 2 years post-RTS) with Wilcoxon signed-rank tests. Lastly, to determine whether quadriceps strength symmetry measured at 2 years post-RTS (as opposed to the time of RTS clearance) was associated with landing mechanics at 2 years post-RTS, we compared 2-year post-RTS biomechanical landing data for each VOI between 2-year post-RTS HQ and LQ groups using Mann Whitney U tests (α = 0.05). For all analyses (demographic, primary, and secondary), we did not adjust the alpha level relative to the number of comparisons due to the preliminary nature of this investigation and to balance risk of Type 1 and Type 2 error.
2.4.3. Post-Hoc Power Calculation.
We also performed a post-hoc power calculation for the Mann Whitney U test group comparisons between the RTS HQ and LQ groups, based on an alpha level of 0.05, and an effect size of 0.87. The effect size was determined based on previous work comparing landing symmetry in peak IKEM during a DVJ task between similarly-divided HQ and LQ groups after ACLR at the time of RTS clearance (HQ LSI: 90.0 ± 23.6%; LQ LSI: 60.9 ± 40.9%).[50]
3. RESULTS
3.1. RTS Quadriceps Strength Group Allocation and Power Calculation
Of the 57 participants included in the current analyses, 28 (49%) were allocated to the HQ group at the time of RTS clearance, 26 (46%) were allocated to the LQ group at the time of RTS clearance, and 3 (5%) participants had a RTS quadriceps LSI between 85.0% and 89.9%.These 3 participants were excluded from HQ/LQ group comparisons. We found that 87% power was achieved for the Mann Whitney U HQ and LQ group comparisons based on the parameters of the post-hoc power calculation.
3.2. Demographic Data Comparisons
The RTS HQ and LQ groups did not differ significantly in sex distribution, meniscus injury proportions, age at the time of RTS clearance, or age at 2 years post-RTS clearance (Table 1; all p>0.364). The RTS HQ group had a higher proportion of hamstring autografts and the RTS LQ group had a higher proportion of bone-patellar tendon-bone autografts (Table 1). Additionally, the RTS LQ group had a shorter time from surgery to RTS clearance, lower preinjury Tegner activity scale scores, and higher body mass index values at 2 years post-RTS clearance (Table 1).
TABLE 1.
DEMOGRAPHIC DATA FOR RTS HQ AND LQ GROUPS
| RTS HQ group (n=28) | RTS LQ group (n=26) | p# | |
|---|---|---|---|
| Sex Distribution, n | |||
| Female | 21 (75%) | 20 (77%) | 0.869 |
| Male | 7 (25%) | 6 (23%) | |
| Graft Type | |||
| Hamstring autograft | 21 (75%) | 9 (35%) | 0.008 |
| BPTB autograft | 5 (18%) | 15 (58%) | |
| Allograft | 2 (7%) | 2 (7%) | |
| Meniscus Injury | |||
| Yes | 14 (50%) | 15 (58%) | 0.571 |
| No | 14 (50%) | 11 (42%) | |
| Age at RTS and 2 Years Post-RTS* | 17.9 ± 2.6 | 17.3 ± 2.9 | 0.406 |
| (years) | 19.9 ± 2.7 | 19.3 ± 2.9 | 0.364 |
| Time from Surgery to RTS Clearance* (months) | 8.4 ± 2.3 | 7.1 ± 1.6 | 0.020 |
| Preinjury Tegner Score* | 9.1 ± 0.6 | 8.7 ± 0.8 | 0.024 |
| Body Mass Index at 2 Years Post-RTS* | 23.9 ± 2.6 | 25.7 ± 3.7 | 0.043 |
Data are reported as mean ± standard deviation.
P-value is from independent t-test for continuous data or Chi-square test for categorical data. BPTB, bone-patellar tendon-bone;
RTS, return-to-sport
3.3. Comparisons of 2-Year Post-RTS Landing Mechanics and Landing Symmetry Data between RTS Quadriceps Strength Groups
The RTS HQ and LQ groups did not statistically differ in involved values for knee flexion excursion, peak IKEM, or peak VGRF (Table 2) during the DVJ at 2 years post-RTS clearance. Similarly, the RTS HQ and LQ groups did not statistically differ in uninvolved values for knee flexion excursion, peak IKEM, or peak VGRF (Table 2) during the DVJ at 2 years post-RTS clearance. The RTS LQ group demonstrated greater asymmetry (i.e., lower LSI) during the DVJ at 2 years post-RTS clearance compared to the RTS HQ group for KFE (data are shown as median (interquartile range); LQ: 92.3% (9.5%); HQ: 100.0% (15.7%); p=0.016) and peak VGRF (LQ: 89.8% (18.2%); HQ: 102.6% (27.0%); p=0.006)(Figure 1). The RTS HQ and LQ groups did not statistically differ in peak IKEM symmetry (LQ: 89.0% (20.8%); HQ: 93.4% (28.2%); p=0.691) at 2 years post-RTS (Figure 1).
TABLE 2.
INVOLVED AND UNINVOLVED LIMB TWO-YEAR POST-RTS LANDING MECHANICS DATA COMPARISONS BETWEEN RTS QUADRICEPS GROUPS
| RTS HQ Group | RTS LQ Group | p# | |
|---|---|---|---|
| 2-Year Knee Flexion Excursion* | |||
| Involved limb, degrees | 60.2 (15.4) | 59.4 (17.1) | .283 |
| Uninvolved limb, degrees | 60.9 (15.5) | 61.4 (14.8) | .782 |
| 2-Year Peak IKEM* | |||
| Involved limb, Nm/kg | 0.99 (0.29) | 1.06 (0.25) | .489 |
| Uninvolved limb, Nm/kg | 1.07 (0.35) | 1.14 (0.37) | .556 |
| 2-Year Peak VGRF* | |||
| Involved limb, N/N | 1.54 (0.42) | 1.47 (0.32) | .341 |
| Uninvolved limb, N/N | 1.48 (0.41) | 1.69 (0.43) | .093 |
Data are presented as median (interquartile range).
P-value is from Mann Whitney U test. RTS, return-to-sport. IKEM, internal knee extension moment. Nm, newton-meters. kg, kilograms. VGRF, vertical ground reaction force. N, newton.
FIGURE 1. TWO-YEAR POST-RTS LANDING SYMMETRY COMPARISONS BETWEEN RTS QUADRICEPS GROUPS (color not necessarily needed in print).
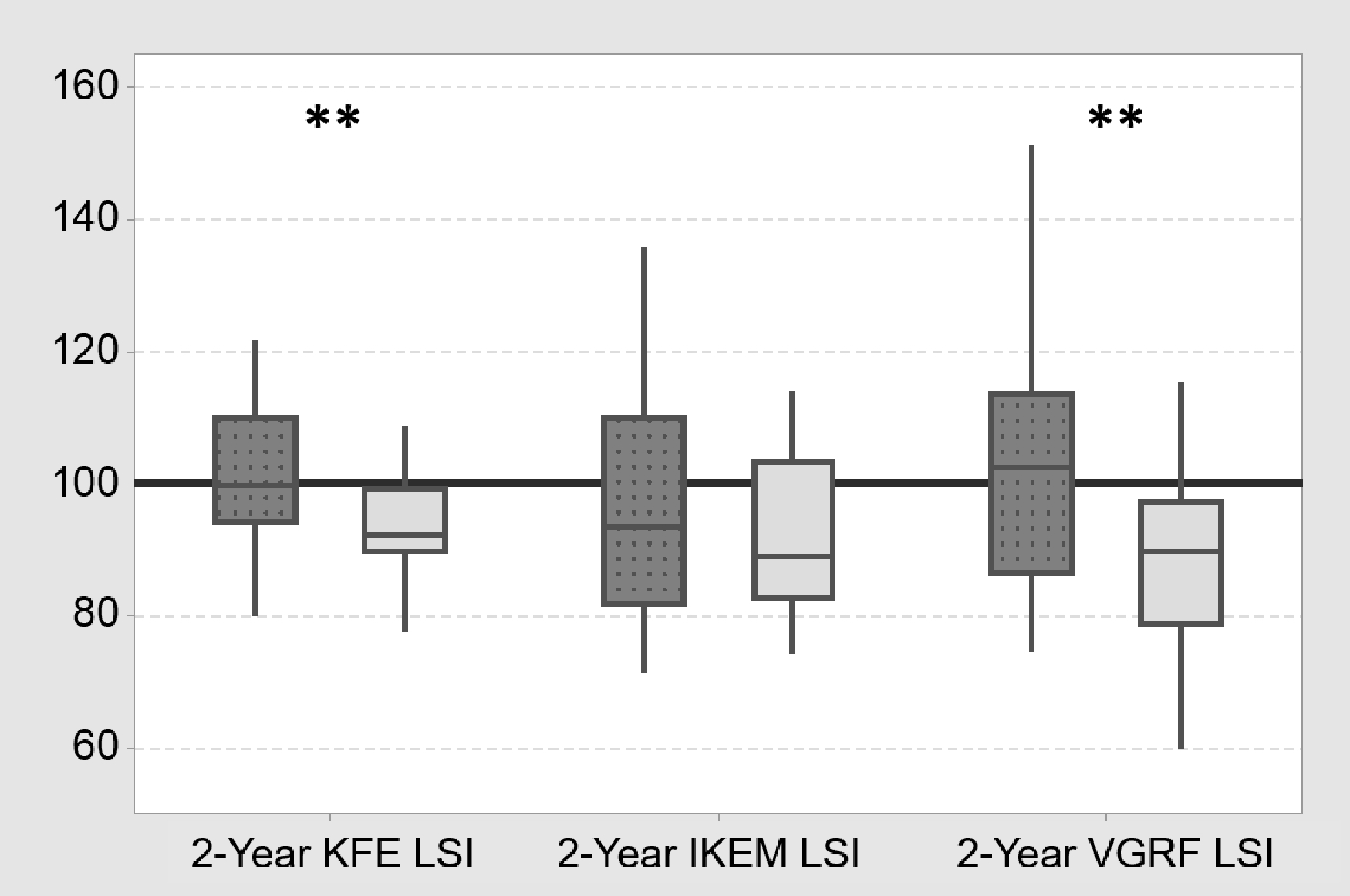
Dark gray dotted box plots are data from the RTS HQ group. Light gray box plots are data from the RTS LQ group. The red line indicates perfect symmetry (LSI=100%). ** indicates p<0.05 for Mann Whitney U group comparisons. The values demonstrated within the box plots are median (middle line), interquartile range (top and bottom of the box), and the highest and lowest observations (whiskers). RTS, return-to-sport; KFE, knee flexion excursion; LSI, limb symmetry index; IKEM, internal knee extension moment; VGRF, vertical ground reaction force
3.4. Secondary Analyses
3.4.1. Between-Limb Comparisons of 2-Year Post-RTS Biomechanical VOIs.
Across the entire cohort (n=57), uninvolved limb 2-year post-RTS peak IKEM and peak VGRF values were higher than involved limb values (p=0.001, p=0.021, respectively), while 2-year post-RTS knee flexion excursion values did not differ between limbs (p=0.083). Within the RTS HQ group (n=28), neither 2-year post-RTS knee flexion excursion, peak IKEM, nor peak VGRF values differed between limbs (p=0.649, p=0.092, p=0.785, respectively). Within the RTS LQ group (n=26), uninvolved limb 2-year post-RTS knee flexion excursion, peak IKEM, and peak VGRF values were higher than involved limb values (p=0.003, p=0.003, p<0.001, respectively).
3.4.2. Quadriceps Strength Changes and Secondary Group Allocation using 2-Year Post-RTS Quadriceps Strength.
Using 2 years post-RTS clearance quadriceps strength data, 38 participants (67%) had 2-year quadriceps LSI ≥ 90%, 9 (16%) had 2-year quadriceps LSI < 85%, and 10 participants (17%) had a 2-year quadriceps LSI between 85.0% and 89.9%. Examining strength group categorization over time, 20 participants (35%) were classified in the HQ group at both the RTS and 2 year post-RTS time points, 15 participants (26%) improved from the LQ to the HQ group over the 2 years, 7 participants (12%) were classified in the LQ group at both time points, and 2 (4%) participants moved from the HQ to the LQ group. Thirteen of the participants (23%) had quadriceps LSI between 85.0% and 89.9% at RTS, 2 years post-RTS, or both. Including all participants (n=57), involved limb quadriceps strength values and quadriceps strength LSI values improved from the time of RTS clearance to 2 years post-RTS clearance (Table 3), whereas uninvolved limb quadriceps strength values did not change over time (Table 3).
TABLE 3.
INVOLVED LIMB STRENGTH, UNINVOLVED LIMB STRENGTH, STRENGTH SYMMETRY BETWEEN RTS AND 2 YEARS POST-RTS TESTING SESSIONS
| RTS Value | 2-Year Post-RTS Value | p^ | |
|---|---|---|---|
| Involved limb quadriceps strength*, Nm/kg | 2.34 (0.56) | 2.52 (0.53) | .002 |
| Uninvolved limb quadriceps strength*, Nm/kg | 2.62 (0.71) | 2.60 (0.52) | .734 |
| Quadriceps strength symmetry*, % | 91.3 (19.8) | 96.8 (18.3) | .002 |
Data are presented as median (interquartile range) and include all participants (n=57).
P-value is from Wilcoxen signed-rank test. RTS, return-to-sport. Nm, newton-meters. kg, kilograms. %, percentage.
3.4.3. Comparisons of 2-Year Post-RTS Landing Mechanics Data between 2-Year Quadriceps Strength Groups.
When 2-year post-RTS clearance quadriceps strength was used for group allocation, the 2-year HQ and LQ groups did not differ in involved limb values for knee flexion excursion (p=0.432), peak IKEM (p=0.968), or peak VGRF (p=0.464) during DVJ landing at 2 years post-RTS. Additionally, the 2-year HQ and LQ groups did not differ in uninvolved limb values for knee flexion excursion (p=0.128), peak IKEM (p=0.947), or peak VGRF (p=0.661) during DVJ landing at 2 years post-RTS. Lastly, the 2-year HQ and LQ groups did not differ in symmetry values (i.e., LSI) for knee flexion excursion (p=0.214), peak IKEM (p=0.685), or peak VGRF (p=0.893) during DVJ landing at 2 years post-RTS.
4. DISCUSSION
The most important finding from our study was that young athletes categorized in the RTS LQ group (quadriceps LSI<85%) demonstrated greater asymmetry in drop-landing during a DVJ task 2 years later, when compared to young athletes categorized in the RTS HQ group (quadriceps LSI≥90%). Specifically, the RTS LQ group demonstrated greater asymmetry in 2-year post-RTS knee flexion excursion and peak VGRF compared to the RTS HQ group. These findings were in support of our primary hypothesis for these analyses. Surprisingly, the RTS quadriceps symmetry groups did not statistically differ in individual limb values (involved or uninvolved limb) for all VOIs evaluated, suggesting that the lower symmetry values (i.e., LSI) observed in the RTS LQ group were likely driven by a subtle shift toward the uninjured knee and away from the ACL-reconstructed knee. In addition to the primary analyses, we performed secondary analyses to examine changes in quadriceps strength symmetry over the 2 years following RTS clearance. We found that the majority of participants (67%) had quadriceps strength LSI≥90% at 2 years post-RTS clearance, while only 16% had quadriceps strength LSI<85% at 2 years. In addition, involved limb quadriceps strength and quadriceps LSI improved over the 2 years. When comparing 2-year post-RTS landing mechanics between the 2-year quadriceps strength symmetry groups, we found no statistical differences in involved limb values, uninvolved limb values, or LSI for all 4 VOIs. These secondary analysis findings suggest that altered movement patterns that develop early after ACLR in the setting of quadriceps strength deficits persist over time, despite subsequent improvements in quadriceps strength. Overall, the findings of our study appear to indicate that quadriceps strength asymmetry at the time of RTS clearance may negatively affect longitudinal knee loading during landing, supporting a quadriceps symmetry threshold of 90% for use in RTS decision-making.
Multiple previous studies have established that quadriceps strength deficits or strength asymmetry after ACLR are associated with altered knee loading across both daily and sport-related tasks.[20, 25, 29, 39, 50] Lewek and colleagues[29] found that individuals with symmetric quadriceps strength after ACLR demonstrated knee loading during the early stance phase of walking and jogging similar to a healthy control group, whereas individuals with asymmetric quadriceps strength demonstrated knee-avoidant loading (decreased sagittal-plane knee angles and moments) during both tasks. Similarly, at the time of RTS clearance after ACLR, quadriceps strength asymmetry has also been linked with knee-avoidant loading patterns during jump-landing tasks.[20, 39, 50] Specific to double-legged landing, Schmitt and colleagues[50] found that young athletes recently cleared for RTS in a LQ group (LSI<85%) demonstrated worse asymmetry for all kinetic VOIs (peak IKEM and peak VGRF) during DVJ landing when compared with both healthy control participants and young athletes post-ACLR in a HQ group (LSI≥90%). Our current work adds to the findings from these cross-sectional studies by demonstrating that young athletes with quadriceps strength asymmetry at the time of RTS clearance continue to demonstrate knee-avoidant loading during landing 2 years later when compared with those with symmetric quadriceps strength at RTS. From our secondary analyses, we also found that, overall, quadriceps strength symmetry improved over the 2 years after RTS clearance, with only 16% of participants categorized in the LQ group at both time points, and these improvements in quadriceps strength symmetry were driven by improvements in involved limb quadriceps strength over this time. Our findings are similar to results from previous studies, which showed that it may take up to 2 years for quadriceps strength to normalize in active individuals following ACLR.[46, 47] In addition, in our secondary analyses, we found no group differences in 2-year landing mechanics between strength symmetry groups using 2-year quadriceps strength data. Taken together, these findings may indicate that altered knee loading patterns that develop early after ACLR in those with quadriceps strength asymmetry persist over the 2 years following RTS, despite subsequent improvements in quadriceps strength/symmetry over this same period, and may represent learned nonuse movement patterning. This is also consistent with recent findings from Chan and Sigward,[4] who demonstrated that individuals early after ACLR (approximately 3 months post-surgery) unload the involved knee across various double-leg tasks, despite being able to adequately load the involved knee when provided targeted feedback.
Normalizing knee joint loading should be a primary focus of rehabilitation, given its potential role in early osteoarthritis pathogenesis and long-term joint health following ACLR. Multiple studies have demonstrated that degeneration of the knee cartilage matrix begins as early as 1 to 2 years following ACLR,[30, 31, 54, 56] and in the long-term, knee osteoarthritis is commonly identified 10 to 15 years after ACLR.[23, 32, 37, 38] Previous theoretical models have suggested that an altered loading environment within the knee joint due to alterations in knee kinematics and kinetics may contribute to the development of osteoarthritis in individuals post-ACLR.[5, 40] Palmieri-Smith and colleagues[40] proposed that alterations in sagittal-plane knee mechanics in response to quadriceps weakness may shift cartilage loading to areas unaccustomed to this load (or, perhaps more importantly, removing cartilage loading from areas accustomed to it), and lead to the development of osteoarthritis. Whereas increased knee joint loading has been associated with progression of osteoarthritis in individuals without a history of ACLR,[35, 52] recent studies suggests that involved knee joint underloading during gait[44, 45, 59] and during a landing task[6] in individuals after ACLR may be associated with the development of early cartilage degeneration. Our data in the current study and well as previous work[20, 25, 29, 39, 50] demonstrate that restoring quadriceps strength may be one key step in helping to normalize knee loading in individuals after ACLR. However, it is likely that other unique rehabilitation intervention strategies are needed, as quadriceps strength and strength symmetry have only explained modest amounts of the variation in movement patterns during dynamic, sport-related tasks in young athletes following ACLR.[20, 50] In addition, from the findings in this study, the RTS HQ and LQ groups did not differ in 2-year peak IKEM symmetry, and the median values for both groups were near 90%. These findings suggest that even with early restoration of quadriceps strength symmetry at the time of RTS, knee-joint specific loading may remain asymmetric over time after ACLR. To address persistent asymmetric movement patterns, recent evidence suggests that targeted movement retraining through the use of feedback mechanisms[4] or by gradually progressing load tolerance via body weight support[10] may be helpful alongside strength training interventions for individuals following ACLR.
We should recognize several important limitations when interpreting the results from this study. First, the cohort of individuals post-ACLR in our study included young athletes with a history of high-level sports participation, and only those planning to return to cutting and pivoting sports. In addition, we required that ACLR participants have previous RTS clearance from their surgeon and rehabilitation specialist. Thus, the included sample of ACLR participants may not be generalizable to all individuals following ACLR; in particular, older or less active patients, or patients who may not have fully completed rehabilitation until the discharge to activity stage. Secondly, our study included participants after ACLR with a variety of graft types (bone-patellar tendon-bone autografts, hamstring autografts, and allografts), and the graft type distribution differed between the quadriceps groups, with the RTS HQ group having a higher proportion of hamstring autografts and the RTS LQ group having a higher proportion of bone-patellar tendon-bone autografts. Due to not being a primary aim of our current study, we did not consider the effect of graft type on longitudinal knee loading during landing in the current analyses. However, the strength differences between the RTS HQ and LQ groups might have been affected by graft type (greater strength asymmetry in individuals with bone-patellar tendon-bone autografts), and rehab strategies specific to graft type may be needed for those susceptible to quadriceps weakness (i.e., bone-patellar tendon-bone autografts[60]). Thirdly, we did not control for or evaluate potential activities that may have affected landing symmetry over the 2 years following RTS after ACLR, including strength and conditioning or neuromuscular injury prevention programs. Fourthly, when grouping into HQ and LQ groups using 2-year post-RTS quadriceps strength LSI for the secondary analyses, 17% of participants (n=10) had quadriceps strength LSI between 85% and 89.9%, and were excluded. This may have underpowered or introduced bias into these secondary analyses. Fifthly, without preinjury data or without following healthy participants for a 2-year period, we are unable to determine if the observed landing asymmetries at 2 years post-RTS exceed those that might be observed in healthy populations or if they are clinically relevant. Lastly, our study did not evaluate all potentially important clinical factors that might influence altered knee loading over time, such as meniscus injury or psychological readiness at the time of RTS. Specifically, previous work has shown that psychological factors like fear of reinjury and lack of confidence may contribute to altered knee loading in individuals following ACLR,[58, 62] and future work should seek to further understand the contributions of both muscle strength and psychological factors on longitudinal knee loading during dynamic tasks.
5. CONCLUSION
Compared with the HQ group, the LQ group from the time of RTS clearance demonstrated greater double-legged landing asymmetry 2 years later. Additionally, quadriceps strength symmetry appears to improve significantly over the 2 years following RTS clearance, potentially indicating that altered movement strategies that develop early after ACLR in those with quadriceps strength deficits may persist over time, despite improvements in strength.
6. ACKNOWLEDGMENTS
The authors thank the staff of the Division of Sports Medicine and the Sports and Orthopaedic Team in the Division of Occupational Therapy and Physical Therapy for their contribution to this work.
FUNDING
This work was funded by support from the National Institutes of Health grant F32-AR055844, the National Football League Charities Medical Research Grants 2007, 2008, 2009, 2011, the Sports Physical Therapy Section Legacy Fund grant 2015, and the Foundation for Physical Therapy Promotion of Doctoral Studies (PODS) II Scholarship. The funding agencies had no role in the study design, collection, analysis, nor interpretation of the data presented. Additionally, the funding agencies were not involved in the writing of the manuscript, nor the decision to submit the manuscript for publication.
Footnotes
DECLARATION OF INTERESTS
We have no competing interests or conflicts of interest to declare for this study.
ETHICAL APPROVAL OF RESEARCH ON HUMANS
The Institutional Review Board at Cincinnati Children’s Hospital Medical Center (Cincinnati, Ohio, USA) approved the protocol for this study (Project 2008–0514).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Bell DR, Blackburn JT, Hackney AC, Marshall SW, Beutler AI, Padua DA (2014) Jump-landing biomechanics and knee-laxity change across the menstrual cycle in women with anterior cruciate ligament reconstruction. J Athl Train 49:154–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE (2005) Treatment of anterior cruciate ligament injuries, part 2. Am J Sports Med 33:1751–1767 [DOI] [PubMed] [Google Scholar]
- 3.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE (2005) Treatment of anterior cruciate ligament injuries, part I. Am J Sports Med 33:1579–1602 [DOI] [PubMed] [Google Scholar]
- 4.Chan MS, Sigward SM (2019) Loading Behaviors Do Not Match Loading Abilities Postanterior Cruciate Ligament Reconstruction. Med Sci Sports Exerc 51:1626–1634 [DOI] [PubMed] [Google Scholar]
- 5.Chaudhari AM, Briant PL, Bevill SL, Koo S, Andriacchi TP (2008) Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc 40:215–222 [DOI] [PubMed] [Google Scholar]
- 6.Culvenor AG, Perraton L, Guermazi A, Bryant AL, Whitehead TS, Morris HG, et al. (2016) Knee kinematics and kinetics are associated with early patellofemoral osteoarthritis following anterior cruciate ligament reconstruction. Osteoarthritis Cartilage 24:1548–1553 [DOI] [PubMed] [Google Scholar]
- 7.Decker MJ, Torry MR, Noonan TJ, Riviere A, Sterett WI (2002) Landing adaptations after ACL reconstruction. Med Sci Sports Exerc 34:1408–1413 [DOI] [PubMed] [Google Scholar]
- 8.Delahunt E, Sweeney L, Chawke M, Kelleher J, Murphy K, Patterson M, et al. (2012) Lower limb kinematic alterations during drop vertical jumps in female athletes who have undergone anterior cruciate ligament reconstruction. J Orthop Res 30:72–78 [DOI] [PubMed] [Google Scholar]
- 9.DeVita P, Hortobagyi T, Barrier J (1998) Gait biomechanics are not normal after anterior cruciate ligament reconstruction and accelerated rehabilitation. Med Sci Sports Exerc 30:1481–1488 [DOI] [PubMed] [Google Scholar]
- 10.Elias ARC, Harris KJ, LaStayo PC, Mizner RL (2018) Clinical Efficacy of Jump Training Augmented With Body Weight Support After ACL Reconstruction: A Randomized Controlled Trial. Am J Sports Med 46:1650–1660 [DOI] [PubMed] [Google Scholar]
- 11.Ford KR, Myer GD, Hewett TE (2007) Reliability of landing 3D motion analysis: implications for longitudinal analyses. Med Sci Sports Exerc 39:2021–2028 [DOI] [PubMed] [Google Scholar]
- 12.Ford KR, Shapiro R, Myer GD, Van Den Bogert AJ, Hewett TE (2010) Longitudinal sex differences during landing in knee abduction in young athletes. Med Sci Sports Exerc 42:1923–1931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gokeler A, Hof AL, Arnold MP, Dijkstra PU, Postema K, Otten E (2010) Abnormal landing strategies after ACL reconstruction. Scand J Med Sci Sports 20:e12–19 [DOI] [PubMed] [Google Scholar]
- 14.Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D (2017) Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 25:192–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hewett TE, Myer GD, Ford KR, Heidt RS Jr., Colosimo AJ, McLean SG, et al. (2005) Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med 33:492–501 [DOI] [PubMed] [Google Scholar]
- 16.Hoffman JT, McNally MP, Wordeman SC, Hewett TE (2015) Validation of a method to accurately correct anterior superior iliac spine marker occlusion. J Biomech 48:1224–1228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ithurburn MP, Altenburger AR, Thomas S, Hewett TE, Paterno MV, Schmitt LC (2018) Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Knee Surg Sports Traumatol Arthrosc 26:426–433 [DOI] [PubMed] [Google Scholar]
- 18.Ithurburn MP, Longfellow MA, Thomas S, Paterno MV, Schmitt LC (2019) Knee Function, Strength, and Resumption of Preinjury Sports Participation in Young Athletes Following Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther 49:145–153 [DOI] [PubMed] [Google Scholar]
- 19.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC (2017) Young Athletes After Anterior Cruciate Ligament Reconstruction With Single-Leg Landing Asymmetries at the Time of Return to Sport Demonstrate Decreased Knee Function 2 Years Later. Am J Sports Med 45:2604–2613 [DOI] [PubMed] [Google Scholar]
- 20.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC (2015) Young Athletes With Quadriceps Femoris Strength Asymmetry at Return to Sport After Anterior Cruciate Ligament Reconstruction Demonstrate Asymmetric Single-Leg Drop-Landing Mechanics. Am J Sports Med 43:2727–2737 [DOI] [PubMed] [Google Scholar]
- 21.Ithurburn MP, Paterno MV, Thomas S, Pennell ML, Evans KD, Magnussen RA, et al. (2019) Change in Drop-Landing Mechanics Over 2 Years in Young Athletes After Anterior Cruciate Ligament Reconstruction. Am J Sports Med 47:2608–2616 [DOI] [PubMed] [Google Scholar]
- 22.Ithurburn MP, Paterno MV, Thomas S, Pennell ML, Evans KD, Magnussen RA, et al. (2019) Clinical measures associated with knee function over two years in young athletes after ACL reconstruction. Knee 26:355–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Janssen RP, du Mee AW, van Valkenburg J, Sala HA, Tseng CM (2013) Anterior cruciate ligament reconstruction with 4-strand hamstring autograft and accelerated rehabilitation: a 10-year prospective study on clinical results, knee osteoarthritis and its predictors. Knee Surg Sports Traumatol Arthrosc 21:1977–1988 [DOI] [PubMed] [Google Scholar]
- 24.Kristianslund E, Krosshaug T, van den Bogert AJ (2012) Effect of low pass filtering on joint moments from inverse dynamics: implications for injury prevention. J Biomech 45:666–671 [DOI] [PubMed] [Google Scholar]
- 25.Kuenze CM, Foot N, Saliba SA, Hart JM (2015) Drop-Landing Performance and Knee-Extension Strength After Anterior Cruciate Ligament Reconstruction. J Athl Train 50:596–602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kvist J (2004) Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med 34:269–280 [DOI] [PubMed] [Google Scholar]
- 27.Lepley AS, Grooms DR, Burland JP, Davi SM, Kinsella-Shaw JM, Lepley LK (2019) Quadriceps muscle function following anterior cruciate ligament reconstruction: systemic differences in neural and morphological characteristics. Exp Brain Res 237:1267–1278 [DOI] [PubMed] [Google Scholar]
- 28.Lepley AS, Kuenze CM (2018) Hip and Knee Kinematics and Kinetics During Landing Tasks After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. J Athl Train 53:144–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lewek M, Rudolph K, Axe M, Snyder-Mackler L (2002) The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon) 17:56–63 [DOI] [PubMed] [Google Scholar]
- 30.Li H, Tao H, Hua Y, Chen J, Li Y, Chen S (2013) Quantitative magnetic resonance imaging assessment of cartilage status: a comparison between young men with and without anterior cruciate ligament reconstruction. Arthroscopy 29:2012–2019 [DOI] [PubMed] [Google Scholar]
- 31.Li X, Kuo D, Theologis A, Carballido-Gamio J, Stehling C, Link TM, et al. (2011) Cartilage in anterior cruciate ligament-reconstructed knees: MR imaging T1 ρand T2 - Initial experience with 1-year follow-up. Radiology 258:505–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50:3145–3152 [DOI] [PubMed] [Google Scholar]
- 33.Lynch AD, Logerstedt DS, Grindem H, Eitzen I, Hicks GE, Axe MJ, et al. (2015) Consensus criteria for defining ‘successful outcome’ after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med 49:335–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mikkelsen C, Werner S, Eriksson E (2000) Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc 8:337–342 [DOI] [PubMed] [Google Scholar]
- 35.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S (2002) Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis 61:617–622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murawski CD, van Eck CF, Irrgang JJ, Tashman S, Fu FH (2014) Operative treatment of primary anterior cruciate ligament rupture in adults. J Bone Joint Surg Am 96:685–694 [DOI] [PubMed] [Google Scholar]
- 37.Murray JR, Lindh AM, Hogan NA, Trezies AJ, Hutchinson JW, Parish E, et al. (2012) Does anterior cruciate ligament reconstruction lead to degenerative disease?: Thirteen-year results after bone-patellar tendon-bone autograft. Am J Sports Med 40:404–413 [DOI] [PubMed] [Google Scholar]
- 38.Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, et al. (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 38:2201–2210 [DOI] [PubMed] [Google Scholar]
- 39.Palmieri-Smith RM, Lepley LK (2015) Quadriceps Strength Asymmetry After Anterior Cruciate Ligament Reconstruction Alters Knee Joint Biomechanics and Functional Performance at Time of Return to Activity. Am J Sports Med 43:1662–1669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Palmieri-Smith RM, Thomas AC (2009) A neuromuscular mechanism of posttraumatic osteoarthritis associated with ACL injury. Exerc Sport Sci Rev 37:147–153 [DOI] [PubMed] [Google Scholar]
- 41.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE (2007) Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med 17:258–262 [DOI] [PubMed] [Google Scholar]
- 42.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Hewett TE (2011) Effects of sex on compensatory landing strategies upon return to sport after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 41:553–559 [DOI] [PubMed] [Google Scholar]
- 43.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, et al. (2010) Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 38:1968–1978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pietrosimone B, Blackburn JT, Harkey MS, Luc BA, Hackney AC, Padua DA, et al. (2016) Greater Mechanical Loading During Walking Is Associated With Less Collagen Turnover in Individuals With Anterior Cruciate Ligament Reconstruction. Am J Sports Med 44:425–432 [DOI] [PubMed] [Google Scholar]
- 45.Pietrosimone B, Loeser RF, Blackburn JT, Padua DA, Harkey MS, Stanley LE, et al. (2017) Biochemical markers of cartilage metabolism are associated with walking biomechanics 6-months following anterior cruciate ligament reconstruction. J Orthop Res 35:2288–2297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A (1999) Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 29:400–412 [DOI] [PubMed] [Google Scholar]
- 47.Roewer BD, Di Stasi SL, Snyder-Mackler L (2011) Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech 44:1948–1953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roewer BD, Ford KR, Myer GD, Hewett TE (2014) The ‘impact’ of force filtering cut-off frequency on the peak knee abduction moment during landing: artefact or ‘artifiction’? Br J Sports Med 48:464–468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sapega AA (1990) Muscle performance evaluation in orthopaedic practice. J Bone Joint Surg Am 72:1562–1574 [PubMed] [Google Scholar]
- 50.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE (2015) Strength Asymmetry and Landing Mechanics at Return to Sport after Anterior Cruciate Ligament Reconstruction. Med Sci Sports Exerc 47:1426–1434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schmitt LC, Paterno MV, Hewett TE (2012) The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 42:750–759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sharma L, Hurwitz DE, Thonar EJ, Sum JA, Lenz ME, Dunlop DD, et al. (1998) Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum 41:1233–1240 [DOI] [PubMed] [Google Scholar]
- 53.Sigward SM, Chan MM, Lin PE, Almansouri SY, Pratt KA (2018) Compensatory Strategies That Reduce Knee Extensor Demand During a Bilateral Squat Change From 3 to 5 Months Following Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther 48:713–718 [DOI] [PubMed] [Google Scholar]
- 54.Su F, Hilton JF, Nardo L, Wu S, Liang F, Link TM, et al. (2013) Cartilage morphology and T1rho and T2 quantification in ACL-reconstructed knees: a 2-year follow-up. Osteoarthritis Cartilage 21:1058–1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 43–49 [PubMed] [Google Scholar]
- 56.Theologis AA, Haughom B, Liang F, Zhang Y, Majumdar S, Link TM, et al. (2014) Comparison of T1rho relaxation times between ACL-reconstructed knees and contralateral uninjured knees. Knee Surg Sports Traumatol Arthrosc 22:298–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Toole AR, Ithurburn MP, Rauh MJ, Hewett TE, Paterno MV, Schmitt LC (2017) Young Athletes Cleared for Sports Participation After Anterior Cruciate Ligament Reconstruction: How Many Actually Meet Recommended Return-to-Sport Criterion Cutoffs? J Orthop Sports Phys Ther 47:825–833 [DOI] [PubMed] [Google Scholar]
- 58.Trigsted SM, Cook DB, Pickett KA, Cadmus-Bertram L, Dunn WR, Bell DR (2018) Greater fear of reinjury is related to stiffened jump-landing biomechanics and muscle activation in women after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 26:3682–3689 [DOI] [PubMed] [Google Scholar]
- 59.Wellsandt E, Gardinier ES, Manal K, Axe MJ, Buchanan TS, Snyder-Mackler L (2016) Decreased Knee Joint Loading Associated With Early Knee Osteoarthritis After Anterior Cruciate Ligament Injury. Am J Sports Med 44:143–151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xergia SA, McClelland JA, Kvist J, Vasiliadis HS, Georgoulis AD (2011) The influence of graft choice on isokinetic muscle strength 4–24 months after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19:768–780 [DOI] [PubMed] [Google Scholar]
- 61.Xergia SA, Pappas E, Zampeli F, Georgiou S, Georgoulis AD (2013) Asymmetries in functional hop tests, lower extremity kinematics, and isokinetic strength persist 6 to 9 months following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 43:154–162 [DOI] [PubMed] [Google Scholar]
- 62.Zarzycki R, Failla M, Capin JJ, Snyder-Mackler L (2018) Psychological Readiness to Return to Sport Is Associated With Knee Kinematic Asymmetry During Gait Following Anterior Cruciate Ligament Reconstruction. J Orthop Sports Phys Ther 48:968–973 [DOI] [PMC free article] [PubMed] [Google Scholar]


