Abstract
The new recommendation of the International Commission on Radiological Protection for occupational eye dose is an equivalent dose limit to the eye of 20 mSv year –1 , averaged over a 5-year period. This recommendation is a drastic reduction from the previous limit of 150 mSv year –1 . Hence, it is important to protect physicians’ eyes from X-ray radiation. Particularly in interventional radiology (IVR) procedures, many physicians use protective lead (Pb) glasses to reduce their occupational exposure. This study assessed the shielding effects of novel 0.07 mm Pb glasses.
The novel glasses (XR-700) have Pb–acrylic lens molded in three dimensions. We studied the novel type of 0.07 mm Pb glasses over a period of seven consecutive months. The eye dose occupational radiation exposure of seven IVR physicians was evaluated during various procedures. All IVR physicians wore eye dosimeters (DOSIRIS™) close to the left side of the left eye. To calculate the shielding effects of the glasses, this same type of eye dosimeter was worn both inside and outside of the Pb lenses.
The average shielding effect of the novel glasses across the seven physicians was 61.4%. Our results suggest an improved shielding effect for IVR physicians that use these glasses. No physician complained that the new glasses were uncomfortable; therefore comfort is not a problem.
The lightweight glasses were acceptable to IVR physicians, who often must perform long procedures. Thus, the novel glasses are comfortable and reasonably protective. Based on the results of this study, we recommend that IVR physicians use these novel 0.07 mm Pb glasses to reduce their exposure.
INTRODUCTION
Interventional radiology (IVR) procedures, which can substantially benefit patients, can also injure both patients and physicians due to exposure to X-ray radiation [ 1–9 ]. Thus, radiation protection of patients and physicians in IVR is very important [ 10–18 ].
The new recommendation of the International Commission on Radiological Protection (ICRP) for occupational eye dose is an equivalent dose limit to the eye of 20 mSv year –1 , averaged over a 5-year period, with no single year exceeding 50 mSv [ 19 , 20 ]. This recommendation is a drastic reduction from the previous limit of 150 mSv year –1 . Hence, it has become more important than ever to evaluate the occupational exposure of IVR physicians and protect their eyes from X-rays using glasses with lead (Pb)-infused lenses [ 21–28 ].
Because IVR involves procedures of long duration, lightweight Pb glasses (i.e. 0.07 mm Pb-equivalent) are preferable for physicians. Thus, 0.07 mm Pb glasses have gradually become widely used in IVR procedures. While such glasses are lightweight and comfortable, the version currently on the market reduces X-rays in IVR procedures by only ~50–60% [ 29–31 ]. We believe that this shielding effect is not sufficient and that more effective eye protection is needed.
Although the radiation shielding effect of 0.75 mm Pb-equivalent glasses is excellent, such glasses are heavy and uncomfortable, especially during long procedures [ 32 ].
Recently, an improved version of X-ray-protective 0.07 mm Pb eyewear has been developed. In this study, we evaluated the X-ray shielding effects of these novel glasses in an IVR clinical setting.
MATERIALS AND METHODS
Novel 0.07 mm Pb-equivalent eyewear
The novel glasses (XR-700) have Pb–acrylic lens molded in three dimensions; thus, we can expect that scattered radiation from the sides and underneath will be cut drastically. The novel glasses are lightweight, with a mass of 42 g. For improved fit, and thus improved protection by minimizing the gaps between the Pb–acrylic lenses and the face, the glasses offer two ways in which they can be adjusted to the facial shape of the physician: (i) the gap between the nose pads has an adjustable width, allowing the bridge to be adjusted by up to ~5 mm; and (ii) the angle of the sides (temples) of the glasses can be adjusted in four steps, with a change of 9° for each step.
Dosimetry
We used digital angiography X-ray systems with a flat-panel detector (Infinix Celeve-i, CANON, Japan) for all procedures. We studied the novel type of 0.07 mm Pb glasses ( Fig. 1 ) over a period of seven consecutive months, during which time doses were monitored over 1-month intervals. In our institution, the eye dose occupational radiation exposure of seven IVR physicians was evaluated during various procedures: coronary angiography, percutaneous coronary intervention, percutaneous peripheral intervention, pacemaker implantation and catheter ablation. During these procedures, the IVR physicians wore the novel glasses.
Fig. 1.

Novel protective eyewear that shields the eyes from X-ray radiation. (a) Details of the new 0.07 mm Pb protective glasses.
• The lenses of the novel glasses are molded three-dimensionally, so that they can block scattered radiation not only from the front but also from the sides and below.
• The nose pad and side (temple) of the spectacles can be adjusted.
These light and comfortable 0.07 mm Pb protective glasses have been adapted to reduce the burden on the operator during a long procedure.
(b) Overview of how the angle of the temple can be adjusted.
Four adjustments can be made in steps, with a change of 9° for each step.
During all procedures, the physicians were typically positioned close to the right side of the patient and used a ceiling protection plate (0.5 mm Pb) if one was available. The methods used to evaluate the eye radiation dose have been described previously [ 29 ]. Briefly, all IVR physicians wore eye dosimeters (DOSIRIS™) close to the left side of the left eye; these measure the 3 mm dose equivalent, Hp(3). To calculate the shielding effects of the glasses, this same type of eye dosimeter was worn both inside and outside of the Pb lenses, as in our previous study [ 29 ]. Using the resulting outside (D out ) and inside (D in ) doses, we calculated the shielding effect of the glasses as follows:
Shielding effect = ( D out – D in )/ D out × 100%
We also determined the estimated annual eye dose (EAED) as follows:
 |
RESULTS
Table 1 lists details about the procedures conducted by the seven physicians. No physician complained that the new glasses were uncomfortable, thus comfort is not a problem.
Table 1.
Details of the procedures conducted by each physician
| Physician no. | Number of procedures | Fluoroscopy time (min) | Used size of the Pb glasses |
|---|---|---|---|
| 1 | 20.9 ± 5.2 | 508.8 ± 169.1 | Small |
| 2 | 21.9 ± 3.4 | 247.3 ± 83.8 | Large |
| 3 | 10.4 ± 3.6 | 120.5 ± 44.6 | Large |
| 4 | 19.4 ± 4.3 | 218.6 ± 55.0 | Large |
| 5 | 12.7 ± 3.0 | 183.7 ± 35.1 | Regular |
| 6 | 22.0 ± 6.1 | 254.6 ± 89.4 | Regular |
| 7 | 10.9 ± 3.5 | 136.3 ± 73.2 | Regular |
| Average ± SD | 15.1 ± 6.2 | 238.5 ± 120.2 |
Results are presented as the mean ± standard deviation (SD) of the monthly averages
Table 2 summarizes the results of our study. The average shielding effect of the novel glasses across the seven physicians was 61.4%. The glasses come in three sizes (small, regular and large), and it seems that the shielding effect did not significantly differ with the size.
Table 2.
Summary of the results of our 7-month study
| Physician no. | Inside dose [Hp(3)] (mSv) | Outside dose [Hp(3)] (mSv) | Shielding effect (%) |
|---|---|---|---|
| 1 | 1.04 ± 0.17 | 2.64 ± 0.3 | 60.9 ± 2.43 |
| 2 | 0.80 ± 0.38 | 1.97 ± 0.85 | 59.61 ± 2.93 |
| 3 | 0.17 ± 0.09 | 0.44 ± 0.28 | 60.13 ± 5.12 |
| 4 | 0.59 ± 0.18 | 1.61 ± 0.41 | 63.36 ± 3.23 |
| 5 | 0.50 ± 0.22 | 1.31 ± 0.60 | 58.85 ± 4.12 |
| 6 | 1.04 ± 0.33 | 2.76 ± 0.93 | 60.81 ± 1.06 |
| 7 | 0.45 ± 0.2 | 1.14 ± 0.51 | 61.83 ± 0.77 |
| Average ± SD | 0.66 ± 0.30 | 1.70 ± 0.77 | 61.4 ± 1.91 |
Results are presented as the mean ± standard deviation (SD) of the monthly averages.
Table 3 lists the estimated annual equivalent dose to the lens of the eye across all physicians while using the novel glasses. The radiation doses (mean ± standard deviation) inside and outside of the novel glasses were 7.9 ± 3.6 and 20.4 ± 9.2 mSv year –1 , respectively.
Table 3.
Estimated annual dose to the lens of the eye
| Physician no. | Inside dose [Hp(3)] (mSv) | Outside dose [Hp(3)] (mSv) |
|---|---|---|
| 1 | 12.5 ± 2.0 | 31.7 ± 3.6 |
| 2 | 9.6 ± 4.6 | 23.6 ± 10.2 |
| 3 | 2.0 ± 1.1 | 5.3 ± 3.4 |
| 4 | 7.1 ± 2.2 | 19.3 ± 4.9 |
| 5 | 6.0 ± 2.6 | 15.7 ± 7.2 |
| 6 | 12.5 ± 4.0 | 33.1 ± 11.2 |
| 7 | 5.4 ± 2.4 | 13.7 ± 6.1 |
| Average ± SD | 7.9 ± 3.9 | 20.3 ± 10.0 |
Figure 2 shows a bar graph of the average shielding effect of the novel glasses, and Figure 3 shows the numbers and types of procedure for each physician; most of them were for coronary angiography. Figure 4 shows the correlations between the doses (mSv month −1 ) inside and outside the novel glasses, which were significant ( R 2 = 0.98).
Fig. 2.

Seven-month average of the shielding effect for each physician.
Fig. 3.
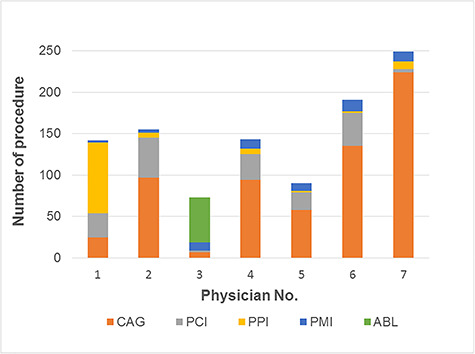
Numbers and types of procedures performed by each physician.
CAG, coronary angiography; PCI, percutaneous coronary intervention; PPI, percutaneous peripheral intervention; PMI, pacemaker implantation; ABL, catheter ablation.
Fig. 4.

Differences between the doses measured near the eye inside and outside the glasses.
DISCUSSION
Although reports have been published on the basic effects of radiation protection products [ 33–43 ], few studies have evaluated the shielding effects of Pb glasses in a clinical setting, such as IVR [ 29–31 ]. Prevention of occupational eye radiation dose is important, particularly for IVR physicians; thus, Pb glasses that provide better shielding are required. Although heavy Pb glasses (i.e. 0.75 mm Pb) have such an effect, they are uncomfortable and thus physicians might not tolerate wearing them for long procedures. Thus the development of new, light (0.07 mm Pb) eyewear is desirable.
Now, such eyewear has been developed, and we performed a clinical study of their use during IVR procedures. For the first time, we present occupational eye dose data of seven physicians over 7 months and can report the shielding effects of these glasses. Previous versions of these glasses could block ~50–60% of the X-ray dose in clinical settings [ 29–31 ]. We found that the new versions block ~61.4% ( Table 2 ), a slight improvement, although it is not clear whether there is a statistically significant difference.
One likely reason for this improvement is that the scattered rays coming from below may be shielded by the new glasses as the gap between the lenses and the face is reduced through adjustments at the nose and at the temples. Moreover, there are three different sizes of glasses, possibly further improving fit. These results indicate that the novel glasses are useful for reducing eye exposure.
Because of the strong correlation ( R 2 = 0.979) between the measurements made inside and outside of the novel glasses, it may be possible to estimate the inner dose from one dosimeter placed outside of them. However, in our dosimeter test setting, the shielding effect may contribute to a reduction in radiation exposures, mainly in the AP direction, because, the dosimeters are attached on the front and back of the glass. In actual exposure scenarios (i.e. in a clinical setting), scattered radiation can enter the eyes from above, from below and from the side, as well as from the front. Therefore, more research may be required in actual exposure scenarios in order to estimate the eye doses more accurately.
The shielding effect of the glasses, the type and number of procedures for each physician and the fluoroscopic time are shown in Figs 2 and 3 and Table 1 , respectively. The results show that the shielding effect did not differ greatly with the type and number of procedures or the fluoroscopic time.
In our study, the occupational EAED of the IVR physicians was lower than the new maximum allowable radiation limit (20 mSv year –1 ).
Finally, like the previous versions, the new glasses are also light and comfortable. However, a previous study (Monte Carlo simulation method, i.e. computer-based calculation) reported a shielding effect of 74% for ‘wrap-around’ 0.07 mm Pb glasses [ 36 ]. The novel 0.07 mm Pb glasses tested in this clinical study are of a ‘wrap-around’ design, but the shielding effect was lower than projected by the Monte Carlo simulation. This was probably because the glasses are not fully ‘wrap-around’ when in use in the clinical IVR setting because there is a small gap between the face and the glasses. In addition, the value of the shielding effect might be affected by variations in the direction, position and angle of the physician’s head during the procedure. Thus, the version we tested requires further improvement to achieve a fully ‘wrap-around’ design in clinical settings.
In summary, it is important to protect physicians’ eyes from X-ray radiation. Particularly in IVR procedures, many physicians use protective Pb glasses to reduce their occupational exposure. However, the shielding effects of Pb glasses depend on their specific features, and the impact of these is unclear in clinical settings. This study assessed the shielding effects of novel 0.07 mm Pb glasses worn by seven physicians in IVR laboratories for seven consecutive months. The average shielding effect was 61.4%. The new, improved 0.07 mm Pb glasses are as comfortable as the previous version. Because IVR procedures are typically of long duration, we recommend that physicians wear lightweight glasses. We particularly recommend that IVR physicians use the novel 0.07 mm Pb glasses to reduce their X-ray exposure.
This was an initial study of the novel 0.07 mm Pb glasses. Further investigation and statistical analysis are required based on a controlled comparison study, such as a multiinstitute evaluation over a long duration (a full year).
CONCLUSIONS
We performed a clinical study of the physician eye dose and shielding effect of novel 0.07 mm Pb glasses during cardiac IVR procedures. The average shielding effect of the glasses was >60%. Our results imply some improvement in shielding of the eyes of IVR physicians that use these glasses. The lightweight glasses were found acceptable by IVR physicians, who often must perform long procedures. Thus, the novel glasses are comfortable and reasonably protective. Based on the results of this study, we recommend that IVR physicians use these novel 0.07 mm Pb glasses to reduce their exposure.
ACKNOWLEDGEMENTS
We thank Dr Mamoru Kato, Research Institute for Brain and Blood Vessels-Akita, Japan, for his invaluable assistance. We also thank Mr Hiroki Ishii, Tohoku University, Japan, for helpful advice regarding the technical analysis.
CONFLICT OF INTEREST
None declared
FUNDING
This study was supported in part by the Industrial Disease Clinical Research grant (200601), Japan.
References
- 1. Valentin J . Avoidance of radiation injuries from medical interventional procedures . Ann ICRP 2001. ; 30:7–67. [DOI] [PubMed] [Google Scholar]
- 2. Kato M , Chida K , Nakamura Met al. New real-time patient radiation dosimeter for use in radiofrequency catheter ablation . J Radiat Res 2019. ; 60 : 215 – 20 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chida K , Kato M , Saito Het al. Radiation dose of interventional radiology system using a flat-panel detector . Am J Roentgenol 2009. ; 193 : 1680 – 5 . [DOI] [PubMed] [Google Scholar]
- 4. Clairand I , Ginjaume M , Vanhavere Fet al. First EURADOS intercomparison exercise of eye lens dosemeters for medical applications . Radiat Prot Dosimetry 2016. ; 170 : 21 – 6 . [DOI] [PubMed] [Google Scholar]
- 5. Chida K , Saito H , Otani Het al. Relationship between fluoroscopic time, dose–area product, body weight, and maximum radiation skin dose in cardiac interventional procedures . Am J Roentgenol 2006. ; 186 : 774 – 8 . [DOI] [PubMed] [Google Scholar]
- 6. Inaba Y , Chida K , Murabayashi Yet al. An initial investigation of a wireless patient radiation dosimeter for use in interventional radiology . Radiol Phys Technol 2020;13:321–6. . [DOI] [PubMed] [Google Scholar]
- 7. Martin CJ , Magee JS . Assessment of eye and body dose for interventional radiologists, cardiologists, and other interventional staff . J Radiol Prot 2013. ; 33 : 445 – 60 . [DOI] [PubMed] [Google Scholar]
- 8. Chida K , Kato M , Inaba Yet al. Real-time patient radiation dosimeter for use in interventional radiology . Phys Med 2016. ; 32 : 1475 – 8 . [DOI] [PubMed] [Google Scholar]
- 9. Nakamura M , Chida K , Zuguchi M . Novel dosimeter using a nontoxic phosphor for real-time monitoring of patient radiation dose in interventional radiology . AJR Am J Roentgenol 2015. ; 205 : W202 – 6 . [DOI] [PubMed] [Google Scholar]
- 10. Cousins C , Miller DL , Bernardi Get al. ICRP PUBLICATION 120: Radiological protection in cardiology . Ann ICRP 2013. ; 42 : 1–125 . [DOI] [PubMed] [Google Scholar]
- 11. Chida K , Ohno T , Kakizaki Set al. Radiation dose to the pediatric cardiac catheterization and intervention patient . Am J Roentgenol 2010. ; 195 : 1175 – 9 . [DOI] [PubMed] [Google Scholar]
- 12. Kato M , Chida K , Sato Tet al. The necessity of follow-up for radiation skin injuries in patients after percutaneous coronary interventions: radiation skin injuries will often be overlooked clinically . Acta Radiol 2012. ; 53 : 1040 – 4 . [DOI] [PubMed] [Google Scholar]
- 13. Vano E , Fernandez JM , Resel LEet al. Staff lens doses in interventional urology. A comparison with interventional radiology, cardiology and vascular surgery values . J Radiol Prot 2016. ; 36 : 37 – 48 . [DOI] [PubMed] [Google Scholar]
- 14. Chida K , Inaba Y , Masuyama Het al. Evaluating the performance of a MOSFET dosimeter at diagnostic X-ray energies for interventional radiology . Radiol Phys Technol 2009. ; 2 : 58 – 61 . [DOI] [PubMed] [Google Scholar]
- 15. Inaba Y , Chida K , Kobayashi Ret al. A cross-sectional study of the radiation dose and image quality of X-ray equipment used in IVR . J Appl Clin Med Phys 2016. ; 17 : 391 – 401 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chida K , Kagaya Y , Saito Het al. Total entrance skin dose: an effective indicator of maximum radiation dose to the skin during percutaneous coronary intervention . AJR Am J Roentgenol 2007. ; 189 : W224 – 7 . [DOI] [PubMed] [Google Scholar]
- 17. Matin CJ . Protecting interventional radiology and cardiology staff: are current designs of lead glasses and eye dosemeters fit for purpose? J Radiol Prot 2018. ; 38 : E22 – 5 . [DOI] [PubMed] [Google Scholar]
- 18. Kawauchi S , Chida K , Moritake Tet al. Estimation of patient lens dose associated with c-arm cone-beam computed tomography usage during interventional neuroradiology . Radiat Prot Dosimetry 2019. ; 184 : 138 – 47 . [DOI] [PubMed] [Google Scholar]
- 19. ICRP Statement on Tissue Reactions , April 2011. , http://www.icrp.org/page.asp?id=123
- 20. ICRP . ICRP Publication 118: ICRP statement on tissue reactions/early and late effects of radiation in normal tissues and organs, threshold doses for tissue reactions in a radiation protection context . Ann ICRP 2012. ; 41 : 1 – 132 . [DOI] [PubMed] [Google Scholar]
- 21. Chida K , Kaga Y , Haga Yet al. Occupational dose in interventional radiology procedures . Am J Roentgenol 2013. ; 200 : 138 – 41 . [DOI] [PubMed] [Google Scholar]
- 22. Inaba Y , Chida K , Kobayashi Ret al. Fundamental study of a real-time occupational dosimetry system for interventional radiology staff . J Radiol Prot 2014. ; 34 : N65 – 71 . [DOI] [PubMed] [Google Scholar]
- 23. Vano E , Sanchez RM , Fernandez JM . Strategies to optimise occupational radiation protection in interventional cardiology using simultaneous registration of patient and staff doses . J Radiol Prot 2018. ; 38 : 1077 – 88 . [DOI] [PubMed] [Google Scholar]
- 24. Chida K , Takahashi T , Ito Det al. Clarifying and visualizing sources of staff-received scattered radiation in interventional procedures . Am J Roentgenol 2011. ; 197 : W900 – 3 . [DOI] [PubMed] [Google Scholar]
- 25. Haga Y , Chida K , Kimura Yet al. Radiation eye dose to medical staff during respiratory endoscopy under X-ray fluoroscopy . J Radiat Res 2020;691–6. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Morishima Y , Chida K , Watanabe H . Estimation of the dose of radiation received by patient and physician during a Videofluoroscopic swallowing study . Dysphagia 2016. ; 31 : 574 – 8 . [DOI] [PubMed] [Google Scholar]
- 27. Chida K , Morishima Y , Inaba Yet al. Physician-received scatter radiation with angiography systems used for interventional radiology: comparison among many X-ray systems . Radiat Prot Dosimetry 2012. ; 149 : 410 – 6 . [DOI] [PubMed] [Google Scholar]
- 28. Efstathopoulos EP , Pantos I , Andreou Met al. Occupational radiation doses to the extremities and the eyes in interventional radiology and cardiology procedures . Br J Radiol 2011. ; 84 : 70 – 7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Haga Y , Chida K , Kaga Yet al. Occupational eye dose in interventional cardiology procedures . Sci Rep 2017. ; 7 : 569 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kato M , Chida K , Ishida Tet al. Occupational radiation exposure of the eye in neurovascular interventional physician . Radiat Prot Dosimetry 2019. ; 185 : 151 – 6 . [DOI] [PubMed] [Google Scholar]
- 31. Kato M , Chida K , Ishida Tet al. Occupational radiation exposure dose of the eye in department of cardiac arrhythmia physician . Radiat Prot Dosimetry 2019. ; 187 : 361 – 8 . [DOI] [PubMed] [Google Scholar]
- 32. Endo M , Haga Y , Abe Met al. Clinical study on the shielding effect of the 0.75mmPb glasses in cardiac IVR procedures . Rinsho Hoshasen 2020. ; 65 : 71 – 5 (in Japanese) . [Google Scholar]
- 33. Morishima Y , Chida K , Meguro T . Effectiveness of additional lead shielding to protect staff from scattering radiation during endoscopic retrograde cholangiopancreatography procedures . J Radiat Res 2018. ; 59 : 225 – 32 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zuguchi M , Chida K , Taura Met al. Usefulness of non-lead aprons in radiation protection for physicians performing interventional procedures . Radiat Prot Dosimetry 2008. ; 131 : 531 – 4 . [DOI] [PubMed] [Google Scholar]
- 35. Ishii H , Haga Y , Sota Met al. Performance of the DOSIRIS™ eye lens dosimeter . J Radiol Prot 2019. ; 39 : N19 – 26 . [DOI] [PubMed] [Google Scholar]
- 36. Koukorava C , Farah J , Struelens Let al. Efficiency of radiation protection equipment in interventional radiology: a systematic Monte Carlo study of eye lens and whole body doses . J Radiol Prot 2014. ; 34 : 509 – 28 . [DOI] [PubMed] [Google Scholar]
- 37. Ishii H , Chida K , Satsurai Ket al. A phantom study to determine the optimal placement of eye dosemeters on interventional cardiology staff . Radiat Prot Dosimetry 2019. ; 185 : 409 – 13 . [DOI] [PubMed] [Google Scholar]
- 38. Chida K , Kato M , Kagaya Yet al. Radiation dose and radiation protection for patients and physicians during interventional procedure . J Radiat Res 2010. ; 51 : 97 – 105 . [DOI] [PubMed] [Google Scholar]
- 39. Chida K , Nishimura Y , Sato Yet al. Examination of the long-term stability of radiation survey meters and electronic pocket dosemeters . Radiat Prot Dosimetry 2008. ; 129 : 431 – 4 . [DOI] [PubMed] [Google Scholar]
- 40. Koenig AM , Maas J , Viniol Set al. Scatter radiation reduction with a radiation-absorbing pad in interventional radiology examinations . Eur J Radiol 2020. ; 132 : 109245 . [DOI] [PubMed] [Google Scholar]
- 41. Chida K , Morishima Y , Masuyama Het al. Effect of radiation monitoring method and formula differences on estimated physician dose during percutaneous coronary intervention . Acta Radiol 2009. ; 50 : 170 – 3 . [DOI] [PubMed] [Google Scholar]
- 42. ORAMED: Optimization of Radiation Protection of Medical Staff . EURADOS Report 2012–02 , Braunschweig; , 2012, April. , http://www.eurados.org/~/media/Files/Eurados/documents/EURADOS_Report_201202.pdf [Google Scholar]
- 43. Morishima Y , Chida K , Katahira Y . The effectiveness of additional lead-shielding drape and low pulse rate fluoroscopy in protecting staff from scatter radiation during cardiac resynchronization therapy (CRT) . Jpn J Radiol 2019. ; 37 : 95 – 101 . [DOI] [PubMed] [Google Scholar]


