Abstract
Background:
Among Medicare value-based payment programs for acute myocardial infarction (AMI), the Hospital Readmissions Reduction Program (HRRP) uses ICD-10 codes to identify the program denominator, while the Bundled Payments for Care Improvement Advanced (BPCIA) program uses DRGs. The extent to which these programs target similar patients, whether they target the intended population (Type 1 myocardial infarction), and whether outcomes are comparable between cohorts is not known.
Methods:
In a retrospective study of 2,176 patients hospitalized in an integrated health system, a cohort of patients assigned a principal ICD-10 diagnosis of AMI and a cohort of patients assigned an AMI DRG were compared according to patient-level agreement and outcomes such as mortality and readmission.
Results:
1,935 patients were included in the ICD-10 cohort compared to 662 patients in the DRG cohort. Only 421 patients were included in both AMI cohorts (19.3% agreement). DRG cohort patients were older (70 vs. 65 years, p<0.001), more often female (48% vs 30%, p<0.001), and had higher rates of heart failure (52% vs. 33%, p<0.001) and kidney disease (42% vs. 25%, p<0.001). Comparing outcomes, the DRG cohort had significantly higher unadjusted rates of 30-day mortality (6.6% vs. 2.5%, p<0.001), 1-year mortality (21% vs. 8%, p<0.001), and 90-day readmission (26% vs. 19%, p=0.006) than the ICD-10 cohort. Two observations help explain these differences: 61% of ICD-10 cohort patients were assigned procedural DRGs for revascularization instead of an AMI DRG, and Type 1 MI patients made up a smaller proportion of the DRG cohort (34%) than the ICD-10 cohort (78%).
Conclusions:
The method used to identify denominators for value-based payment programs has important implications for the patient characteristics and outcomes of the populations. As national and local quality initiatives mature, an emphasis on ICD-10 codes to define AMI cohorts would better represent Type 1 MI patients.
Keywords: quality, outcome and process assessment, acute myocardial infarction, pay for performance, Medicare
Introduction
National efforts to improve inpatient cardiovascular care now include several value-based payment reforms initiated by the Center for Medicare and Medicaid Services (CMS): these include the Hospital Readmissions Reduction Program (HRRP), the Value-Based Purchasing program (VBP) and the voluntary Bundled Payments for Care Improvement Advanced (BPCIA). Because of its relatively high incidence and cost in the Medicare population and the availability of numerous evidence-based therapies that improve outcomes for Type 1 myocardial infarction (T1MI), acute myocardial infarction (AMI) is a condition targeted by all three programs.1,2 These programs do not define AMI uniformly, however. While the BPCIA uses Medicare-severity diagnosis related groups (DRG) to define eligible AMI hospitalizations,3 the HRRP and VBP programs use AMI codes from the international classification of diseases, 10th revision (ICD-10).4,5
Broadly, how AMI populations are defined is important to the work of hospitals, payers, researchers, and ratings agencies. Hospitals are continuously analyzing performance data to focus improvement efforts, but may not consider whether these data come from DRG or ICD-10 cohorts. Payers may dispense payments for inpatient care according to DRG diagnoses while at the same time measuring quality based on ICD-10 diagnoses. Researchers and ratings agencies, meanwhile, usually analyze AMI care based on a single population, either ICD-10 or DRG. In each of these cases, whether observations in one AMI population (e.g. DRG) are generalizable to another AMI population (e.g. ICD-10) is unknown. An assumption of equivalence between these populations, if untrue, has the potential to undermine efforts to improve AMI care.
With this in mind, we sought to characterize the extent to which DRG and ICD-10 diagnoses of AMI identify similar populations. We used data from a large integrated health system to determine patient-level agreement between AMI cohorts defined by ICD-10 codes versus AMI DRGs. We also compared cohorts according to outcome measures, such as 30-day mortality and readmission that are linked to value-based programs, as well as process measures of excellence in AMI care, such as cardiac rehabilitation referral rates.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request. In a retrospective cohort analysis, we collected data for all patients who were admitted to a UCHealth hospital between January 1, 2017 and June 30, 2018 and were discharged alive with a diagnosis of AMI according to either the discharge DRG or principal ICD-10 code. UCHealth is a not-for-profit integrated health care system that included 8 Colorado hospitals, including the University of Colorado Hospital, during the timeframe of the study. Eligible AMI diagnoses were chosen to align with value-based payment programs (see “Exposure” section below). Patients with AMI who did not receive an eligible administrative AMI diagnosis were not included.
Exposure
Patients were divided into two cohorts – an ICD-10 cohort and a DRG cohort – though cohorts were not mutually exclusive. The DRG cohort was comprised of patients with a hospitalization during the study period that was assigned one of three DRGs for AMI described in the inclusion criteria for the BPCIA program.3 Patients in the ICD-10 cohort were hospitalized during the study period with a primary discharge ICD-10 code included on a list of nine codes used by the HRRP and VBP programs.4,5 A full list of DRGs and ICD-10 codes defining cohort inclusion can be found in Supplemental Table I. For patients with multiple AMI admissions, only their first AMI encounter during the study period was included in the analysis.
Outcomes
Outcome measures were selected for relevance to performance in value-based policy programs: these included rates of 30-day mortality, 1-year mortality, 30-day readmission and 90-day readmission. In order to understand rates of resource utilization in the two cohorts, we also compared cohorts according to process measures such as length of stay, inpatient medication use and utilization of cardiac testing and services. Among the medications analyzed were aspirin, beta blockers, oral P2Y12 inhibitors and high dose HMG-CoA reductase inhibitors (atorvastatin dose ≥ 40 mg, rosuvastatin dose ≥ 20 mg). Among the cardiac tests and services examined were cardiac rehabilitation referrals, cardiac catheterizations and cardiac imaging tests including echocardiography, computed tomography (Cardiac CT) and magnetic resonance imaging (Cardiac MRI). Finally, the ten most common principal ICD-10 diagnoses in the DRG cohort were enumerated, as were the ten most common DRG assignments in the ICD-10 cohort.
Statistical analysis
Patient-level agreement between the ICD-10 and DRG cohorts was assessed by percent agreement. Univariate logistic regression was used to determine the difference between groups for each categorized characteristic and outcome (e.g. medication rates and mortality rates), where the p-value associated with the Chi-Square test statistics was reported. Univariate linear regression was used to compare non-categorized characteristics and outcomes (e.g. age, mean length of stay), where the p-value corresponded to a two-sample t-test assuming equal variances. Some patients were captured by both the ICD-10 and DRG cohorts. While summary statistics for each cohort include all patients in the cohort, including these overlap patients, statistical comparisons between groups reflect differences between patients included in only one of the cohorts. All statistical analysis and data manipulation was carried out in R, version 3.6.0 (R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria, 2014).
Subgroup Chart Review of UCH patients
All patients in the study who were admitted to the University of Colorado Hospital (UCH) were part of a subgroup analysis in which chart reviews were performed to establish a gold-standard diagnosis based on the Fourth Universal Definition of Myocardial Infarction (4-UDMI).6 Five reviewers completed reviews (AEL, KSR, EWR, JDR, NMB) and uncertain or questionable cases were adjudicated by agreement between two reviewers (AEL, KSR). UCH was chosen for review because all five reviewers had access to medical records from this site. More details regarding the methods used for chart reviews are described in the Supplemental Methods.
Subgroup analysis
Baseline characteristics of UCH patients are compared to those of UCHealth patients in Supplemental Table II. Agreement between patients with chart-confirmed T1MI versus patients in the ICD-10 and DRG cohorts was assessed by percent agreement and dual-comparison Cohen’s kappa coefficients. T1MI patients were then used as the reference group for process and outcome measure comparisons to UCH patients in the ICD-10 and DRG cohorts. Statistical methods were identical to those described above in the “statistical analysis” section.
Sensitivity Analysis
Unadjusted analyses, as described above, were used for our main outcome measures because, while covariates are used by CMS and others for risk-adjusted comparisons between hospitals, our analysis was designed to compare cohorts within a single hospital system in order to highlight differences between cohorts that are directly relevant to local quality measurement and improvement. As a sensitivity analysis of the extent to which differences between cohorts are attributable to measured differences between cohorts, multivariate regression was performed using age, sex, and baseline rates of heart failure (HF), chronic kidney disease (CKD), and diabetes mellitus as covariates (Supplemental Table III).
Data acquisition and handling
With the exception of chart review data, all clinical data for the study were obtained from the Health Data Compass, an electronic data warehouse that integrates input from the UCHealth electronic health record (EHR) with outside sources such as the Colorado State Death Registry and Colorado All Payer Claims Database.7 This study was reviewed and approved by the Colorado Multiple Institutions Review Board (COMIRB 19–1877).
Results
Between January 1, 2017 and June 30, 2018, a total of 2,176 patients at UCHealth hospitals had an eligible DRG or primary ICD-10 diagnosis of AMI. Patient demographics and characteristics are described in Table 1. Baseline characteristics between DRG and ICD-10 cohort patients were different, most notably in terms of mean age (70 vs. 65 years, p<0.001) and gender (48% female vs 30%, p<0.001). Patients in the DRG cohort also had higher rates of comorbidities such as HF (52% vs. 33%, p<0.001), CKD (42% vs. 25%, p>0.001) and diabetes mellitus (41% vs. 37%, p=0.041) than the ICD-10 cohort. Further, patients in the DRG cohort were less often cared for by a Cardiologist (58% vs. 74%, p<0.001).
Table 1.
Baseline patient characteristics of AMI cohorts
| ICD-10 | DRG | p† value | *T1MI-UCH | *ICD10-UCH | p† value | *DRG-UCH | p† value | |
|---|---|---|---|---|---|---|---|---|
| Total n | 1935 | 662 | 425 | 525 | 258 | |||
| Demographics | ||||||||
| Age (median) | 65.2 (sd=13.4) |
70.3 (sd=14.9) |
<0.001 | 63.7 (sd=13.8) |
63.3 (sd = 14.0) |
0.192 | 68.3 (sd=15.1) |
<0.001 |
| Female | 577 (29.8%) | 321 (48.5%) | <0.001 | 128 (30.1%) | 172 (32.8%) | 0.758 | 126 (48.8%) | <0.001 |
| White or Caucasian | 1497 (77.4%) | 492 (74.3%) | 0.095 | 226 (53.2%) | 278 (53.0%) | 0.571 | 136 (52.7%) | 0.649 |
| Cardiology Team | 1430 (73.9%) | 385 (58.2%) | <0.001 | 218 (51.3%) | 269 (51.2%) | 0.607 | 107 (41.5%) | 0.006 |
| Medical History | ||||||||
| Diabetes Mellitus | 713 (36.8%) | 273 (41.2%) | 0.041 | 185 (43.5%) | 220 (41.9%) | 0.405 | 103 (39.9%) | 0.104 |
| Hypertension | 1510 (78.0%) | 560 (84.6%) | 0.002 | 324 (76.2%) | 400 (76.2%) | 0.963 | 213 (82.6%) | 0.084 |
| Hyperlipidemia | 1333 (68.9%) | 373 (56.3%) | <0.001 | 216 (50.8%) | 259 (49.3%) | 0.459 | 102 (39.5%) | 0.004 |
| Heart Failure | 646 (33.4%) | 347 (52.4%) | <0.001 | 169 (39.8%) | 211 (40.2%) | 0.242 | 136 (52.7%) | <0.001 |
| Peripheral Artery Disease | 78 (4.0%) | 24 (3.6%) | 0.305 | 15 (3.5%) | 15 (2.9%) | 0.311 | 1 (0.4%) | 0.012 |
| Prior Stroke | 330 (17.05%) | 167 (25.2%) | <0.001 | 81 (19.1%) | 103 (19.6%) | 0.325 | 58 (22.5%) | 0.332 |
| COPD | 288 (14.9%) | 138 (20.9%) | <0.001 | 68 (16.0%) | 87 (16.6%) | 0.818 | 61 (23.6%) | 0.010 |
| Chronic Kidney Disease | 487 (25.2%) | 279 (42.2%) | <0.001 | 118 (27.8%) | 166 (31.6%) | 0.189 | 122 (47.3%) | <0.001 |
| Dementia | 67 (3.5%) | 65 (9.8%) | <0.001 | 11 (2.6%) | 16 (3.1%) | 0.603 | 26 (10.1%) | <0.001 |
| Cancer | 356 (18.4%) | 137 (20.7%) | 0.235 | 61 (14.4%) | 81 (15.4%) | 0.470 | 52 (20.2%) | 0.009 |
| Home Medications | ||||||||
| Aspirin | 149 (7.7%) | 100 (15.1%) | <0.001 | 42 (9.9%) | 55 (10.5%) | 0.999 | 48 (18.6%) | <0.001 |
| P2Y12 Inhibitor | 91 (4.7%) | 52 (7.9%) | <0.001 | 30 (7.1%) | 36 (6.9%) | 0.279 | 23 (8.91%) | 0.548 |
| Beta Blocker | 172 (8.9%) | 112 (16.9%) | <0.001 | 58 (13.7%) | 68 (13.0%) | 0.116 | 54 (20.9%) | 0.049 |
| Any Statin | 172 (8.9%) | 99 (15.0%) | <0.001 | 53 (12.5%) | 64 (12.2%) | 0.715 | 47 (18.2%) | 0.085 |
| ACEi, ARB, ARNI | 152 (7.9%) | 81 (12.2%) | <0.001 | 51 (12.0%) | 58 (11.1%) | 0.159 | 43 (16.7%) | 0.265 |
| Oral Anticoagulation | 34 (1.8%) | 32 (4.8%) | <0.001 | 10 (2.4%) | 14 (2.7%) | 0.999 | 16 (6.2%) | 0.003 |
Subgroup analysis of all patients cared for at the University of Colorado Hospital (UCH).
Reference group for the main study cohort was ICD-10; reference group for the UCH subgroup was T1MI (T1MI-UCH).
Abbreviations: ACEi=angiotensin-converting enzyme inhibitor; ARB=angiotensin-receptor blocker; ARNI = angiotensin-receptor neprilysin inhibitor; COPD = chronic obstructice pulmonary disease; DOAC = direct oral anticoagulant; DRG = Diagnosis Related Group; ICD-10 = international classification of diseases, 10th revision; T1MI = Type 1 myocardial infarction
Out of the total cohort, 662 patients (30%) had an eligible DRG diagnosis of AMI and 1,935 patients (89%) had a primary ICD-10 diagnosis of AMI. 421 encounters had both an ICD-10 and a DRG diagnosis of AMI, corresponding to 19.3% concordance between the two cohorts (Figure 1). Among patients in the ICD-10 cohort who were not assigned a DRG for AMI, 61% were instead assigned a DRG for percutaneous coronary intervention (PCI) or coronary artery bypass graft surgery (CABG) (Figure 2). A complete listing of the ten most frequent ICD-10 assignments for the DRG cohort are provided in Supplemental Table IV and the ten most frequent DRG assignments for the ICD-10 cohort are provided in Supplemental Table V.
Figure 1.
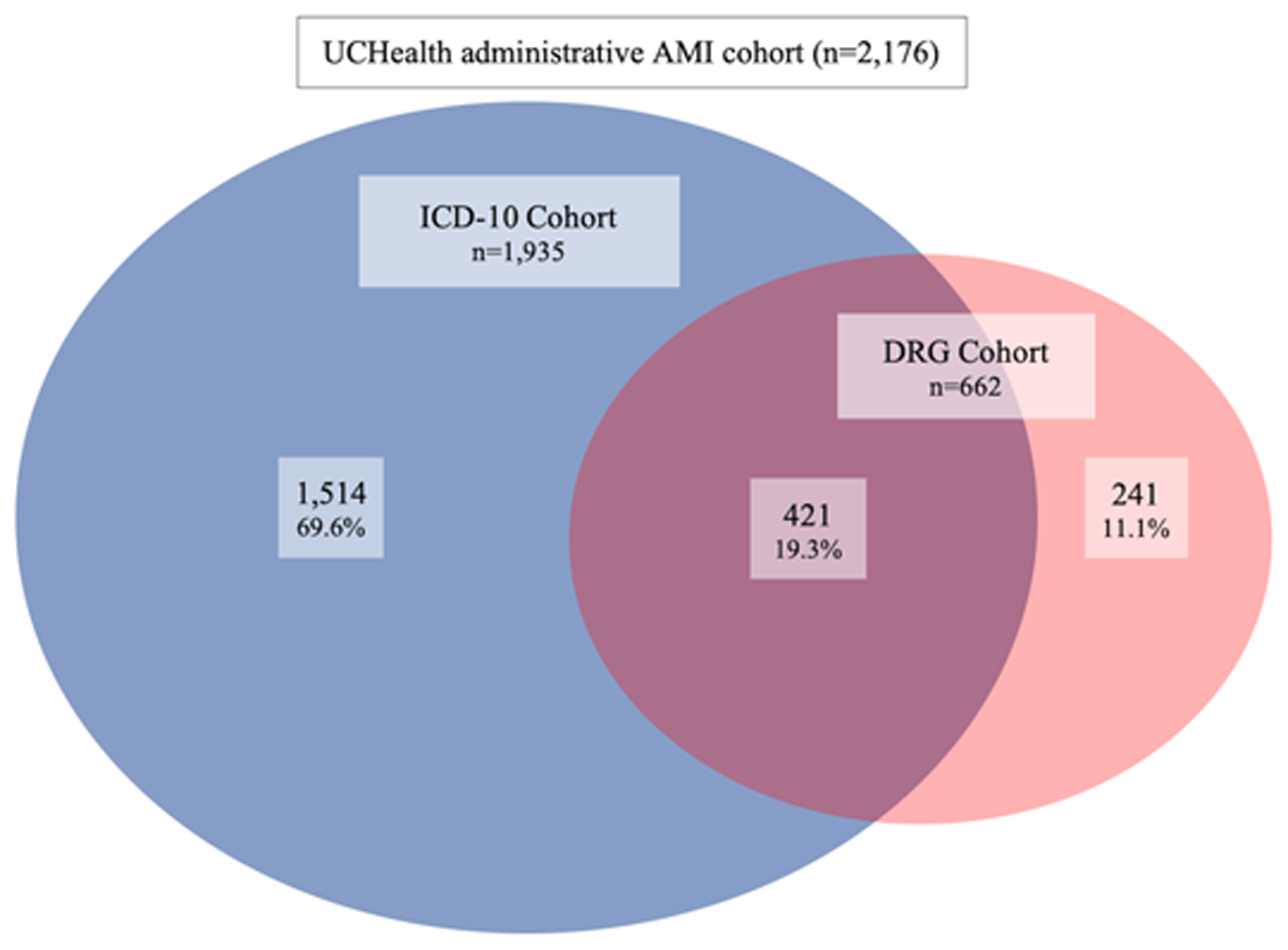
AMI cohort agreement in an integrated health system
Abbreviations: AMI = acute myocardial infarction; DRG = diagnosis related group; ICD-10 = international classification of diseases, 10th revision.
Figure 2.
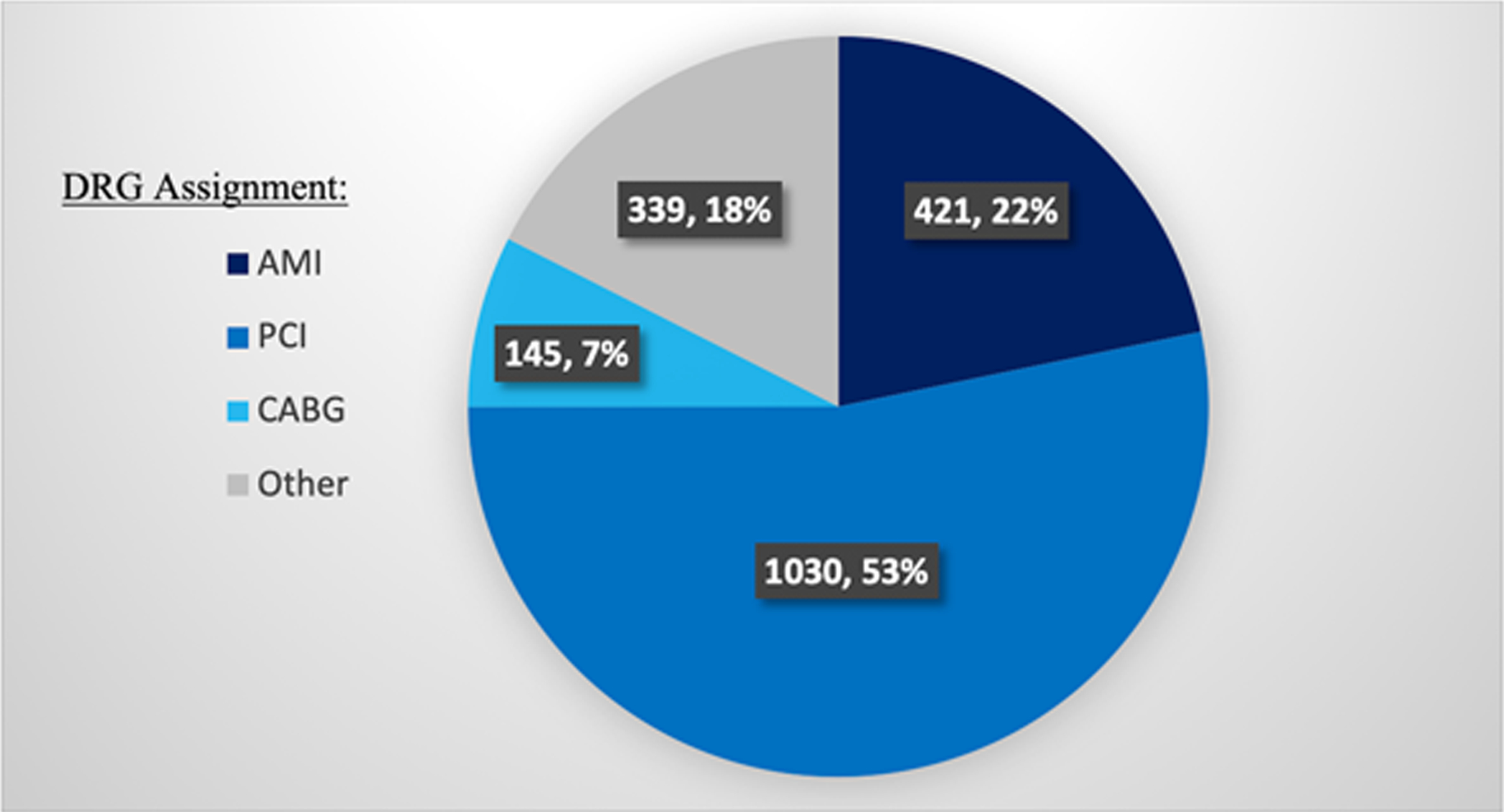
DRG assignments in the ICD-10 cohort for AMI
Abbreviations: AMI = acute myocardial infarction; PCI = percutaneous coronary intervention, CABG = coronary artery bypass grafting.
Significant differences in outcome and process measures were observed between the DRG and ICD-10 cohorts (Table 2). In terms of inpatient medication use, significantly fewer patients in the DRG group were prescribed P2Y12 inhibitors (44.6% vs. 81.6%, p<0.001) and high dose statins (80.2% vs. 92.5%, p<0.001) during their inpatient stay. Smaller, but still significant, differences were observed for inpatient aspirin and beta blocker use. Rates of cardiac catheterization (32.8% vs. 65.2%, p<0.001) and cardiac rehabilitation referral (22.4% vs. 57.8%, p<0.001) were also significantly lower in the DRG cohort. The only process measures that were not significantly different between the DRG and ICD-10 cohorts were hospital length of stay and rates of inpatient echocardiography. In terms of outcomes, rates of 30-day mortality (6.6 vs. 2.5%, p<0.001), 1-year mortality (20.8% vs. 8.0%, p<0.001), and 90-day readmission (26.4% vs. 18.9%, p=0.006) were all higher in the DRG cohort than the ICD-10 cohort. Differences in rates of 30-day readmission were not statistically significant (18.5% vs. 13.9%, p=0.065). These results were robust to sensitivity analysis using multivariate comparisons (Supplemental Table III) with the exception of differences in 90-day readmissions, which were no longer statistically significant, and length of stay, for which differences were shown to be significantly different after adjustment (3.9 days in DRG vs. 4.0 days in ICD-10, p=0.006).
Table 2.
Univariate comparison of quality measures and rates of resource utilization among different AMI cohorts
| ICD-10 | DRG | *T1MI-UCH | *ICD10-UCH | *DRG-UCH | |
|---|---|---|---|---|---|
| Total n | 1935 | 662 | 425 | 525 | 258 |
| Outcome measures | |||||
| 1 year mortality | 168 (8.7%) ref |
147 (22.2%) p<0.001 |
44 (10.4%) ref |
53 (10.1%) p=0.134 |
61 (23.6%) p<0.001 |
| 30 day mortality | 51 (2.64%) ref |
47 (7.1%) p<0.001 |
7 (1.7%) ref |
8 (1.5%) p=0.078 |
13 (5.0%) p=0.013 |
| 90 day readmission | 365 (18.9%) ref |
171 (25.8%) p=0.016 |
93 (21.9%) ref |
114 (21.7%) p=0.236 |
68 (26.4%) p=0.445 |
| 30 day readmission | 269 (13.9%) ref |
123 (18.6%) p=0.065 |
62 (14.6%) ref |
76 (14.5%) p=0.454 |
45 (17.4%) p=0.719 |
| Medications administered | |||||
| Aspirin | 1916 (99.0%) ref |
622 (94.0%) p<0.001 |
424 (99.8%) ref |
519 (98.9%) p=0.992 |
235 (91.1%) p<0.001 |
| P2Y12 inhibitors | 1579 (81.6%) Ref |
295 (44.6%) p<0.001 |
340 (80.0%) ref |
393 (74.9%) p=0.846 |
98 (38.0%) p<0.001 |
| High-dose Statin | 1790 (92.5%) ref |
531 (80.2%) p<0.001 |
407 (95.8%) ref |
500 (95.2%) p=0.923 |
219 (84.9%) p<0.001 |
| Beta Blocker | 1804 (93.2%) ref |
553 (82.5%) p<0.001 |
401 (94.4%) ref |
477 (90.9%) p=0.940 |
197 (76.4%) p<0.001 |
| Process measures | |||||
| Length of Stay | 4.03 days ref |
3.88 days p=0.059 |
5.81 days ref |
5.79 days p=0.448 |
4.88 days p=0.054 |
| Echocardiography | 1294 (66.9%) ref |
421 (63.6%) p=0.052 |
218 (51.3%) ref |
271 (51.6%) p=0.551 |
122 (47.3%) p=0.209 |
| Stress Test | 24 (1.2%) ref |
33 (5.0%) p<0.001 |
9 (2.1%) ref |
20 (3.8%) p=0.879 |
30 (11.6%) p<0.001 |
| Cardiac CT | 7 (0.4%) ref |
11 (1.7%) p<0.001 |
3 (0.7%) ref |
4 (0.8%) p=0.288 |
8 (3.1%) p=0.991 |
| Cardiac MRI | 11 (0.6%) ref |
8 (1.2%) p=0.016 |
8 (1.9%) ref |
11 (2.1%) p=0.588 |
7 (2.7%) p=0.332 |
| Cardiac Catheterization | 1262 (65.2%) ref |
217 (32.8%) p<0.001 |
282 (66.4%) ref |
323 (61.5%) p=0.818 |
81 (31.4%) p<0.001 |
| Cardiac rehabilitation referral | 1118 (57.8%) ref |
148 (22.4%) p<0.001 |
68 (16.0%) ref |
79 (15.0%) p=0.981 |
17 (6.6%) P<0.001 |
Part of a subgroup analysis of all patients cared for at the University of Colorado Hospital (UCH).
Abbreviations: CT = computed tomography; MRI = magnetic resonance imaging; DRG = diagnosis related group; ICD-10 = international classification of diseases, 10th revision; T1MI = Type 1 myocardial infarction
A chart review subgroup analysis of all 645 AMI patients treated at UCH included 525 patients from the ICD-10 cohort and 258 from the DRG cohort. Baseline patient characteristics for the UCH subgroup compared to the UCHealth cohort are described in Supplemental Table II. Characteristics such as mean age and rates of diabetes, CKD, HF, and home medication use were different between the UCH cohort and the larger UCHealth cohort. Yet, agreement between ICD-10 and DRG subgroups from UCH was similar to the overall UCHealth cohort, with 138 patients being included in both subgroups (21.4% agreement).
Out of the 645 subgroup patients, gold-standard diagnosis based on chart review revealed that 425 (66%) were diagnosed with Type 1 MI (T1MI), 101 (16%) had Type 2 MI (T2MI) and 119 (18%) were diagnosed with non-ischemic myocardial injury (NIMI). Focusing on patients with T1MI, 78% (409/525) of patients in the ICD10-UCH subgroup were diagnosed with T1MI, compared to 34% (89/258) in the DRG-UCH subgroup (Figure 3). Patients that were only captured by the ICD10-UCH subgroup had the highest proportion of T1MI diagnoses 87% (336/387), compared with 53% (73/138) among patients in both subgroups and 13% (16/120) among patients only included in DRG-UCH subgroup (Supplemental Figure I). Most T1MI patients not assigned an AMI DRG were assigned a DRG for PCI (189/425, 44%) or CABG (47/425, 11%) (Supplemental Table VI). Overall patient-level agreement between T1MI and ICD-10 was fair (80% agreement, kappa 0.49 with 95% CI 0.42 to 0.56) while T1MI agreement with the DRG cohort was poor (22% agreement, kappa −0.47 with 95% CI −0.54 to −0.40) (Supplemental Table VII).
Figure 3.
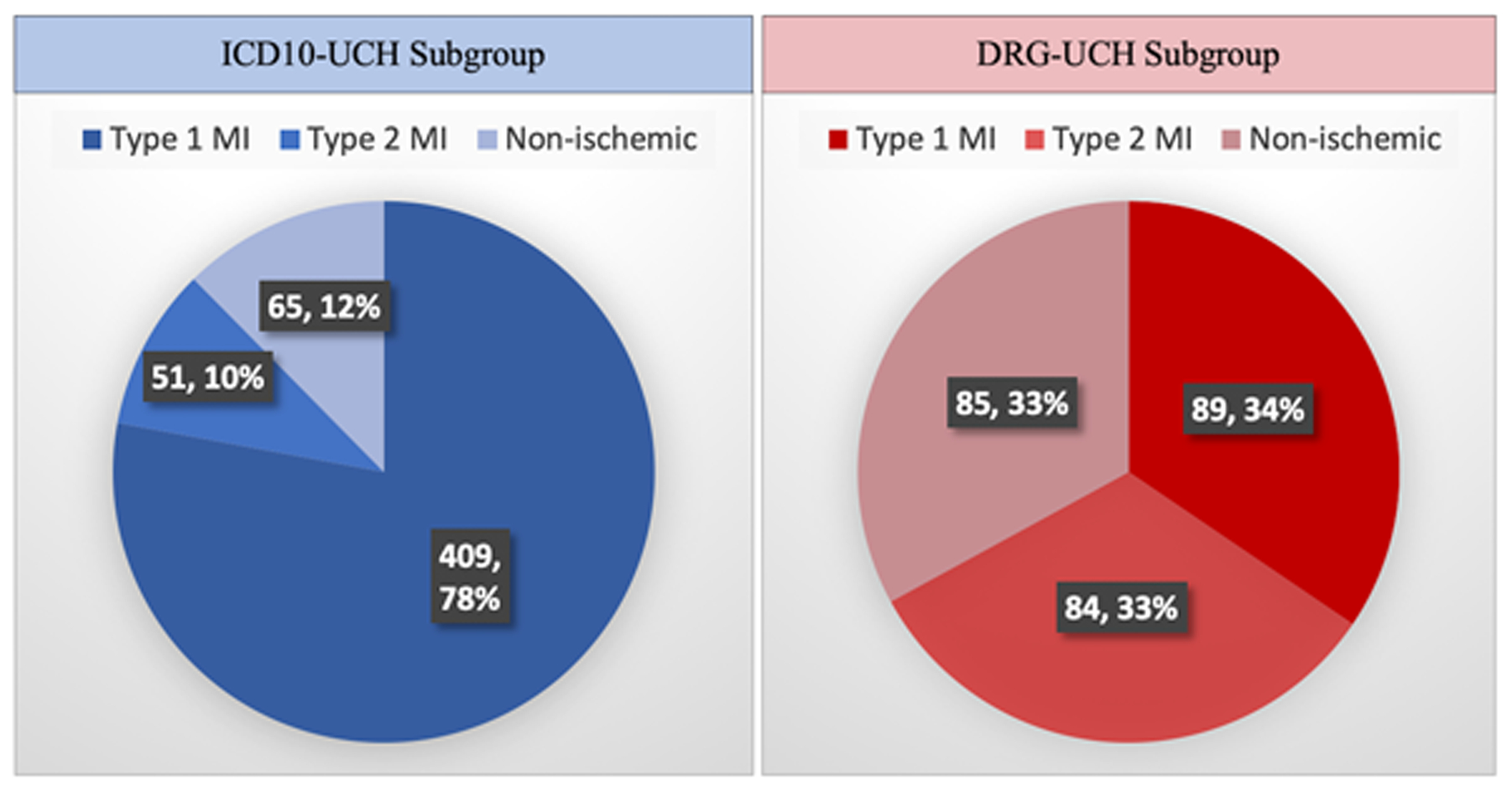
ICD10-UCH and DRG-UCH subgroups stratified by chart review diagnosis*
*Part of a subgroup analysis of all patients cared for at the University of Colorado Hospital (UCH).
Abbreviations: UCH = University of Colorado Hospital, DRG = diagnosis related group; ICD-10 = international classification of diseases, 10th revision; Type 1 MI = Type 1 myocardial infarction; Type 2 MI = Type 2 myocardial infarction; non-ischemic = non-ischemic myocardial injury
The baseline characteristics for T1MI patients were more similar to the ICD10-UCH subgroup than the DRG-UCH subgroup: while the ICD-10 cohort was not significantly different from the T1MI cohort in any of twenty baseline characteristics examined in this study, the DRG-UCH cohort was significantly different according to thirteen of twenty baseline characteristics including age, sex and rates heart failure and chronic kidney disease, among others (Table 1). T1MI patients were also more similar to ICD-10 patients in terms of process and outcomes measures in that there were no significant differences between T1MI patients and the ICD10-UCH subgroup. Patients in the DRG-UCH group, in contrast, were significantly different from T1MI patients in terms of 30-day mortality (5.0% vs. 1.7%, p=0.013), 1-year mortality (23.6% vs. 10.4%, p<0.001), rates of stress testing (11.6% vs. 2.1%, p<0.001), cardiac catheterization (31.4% vs. 66.4%, p<0.001), referral to cardiac rehabilitation (6.6% vs. 16.0%, p<0.001) and rates of inpatient use of aspirin (99% vs. 91%, p<0.001), P2Y12 inhibitors (38% vs. 80%, p<0.001), high-dose statins (85% vs. 96%, p<0.001) and beta blockers (76% vs. 94%, p<0.001) (Table 2). These findings were also robust to sensitivity analysis using multivariate comparisons (Supplemental Table II) with the exception of differences in 30-day mortality and inpatient aspirin use, which were no longer statistically significant, and length of stay, for which differences were shown to be significantly different after adjustment (4.9 days in DRG-UCH vs. 5.8 days in T1MI, p<0.001).
Discussion
In a retrospective cohort study of patients admitted to a large integrated health system in Colorado, only 19% of AMI patients were included in both the ICD-10 and DRG cohorts. The poor agreement between cohorts is partly explained by the observation that the majority of ICD-10 cohort patients (61%) were assigned a DRG for PCI or CABG. Perhaps more notably, patients in the DRG cohort were significantly less likely to receive medical therapy for AMI or undergo cardiac catheterization and had significantly higher rates of mortality and readmission. A subgroup analysis of patients admitted to the University of Colorado Hospital (UCH) suggests that these differences may, in part, be attributable to lower rates of true Type 1 MI in the DRG cohort (34%) compared to the ICD-10 cohort (78%). Similar to the ICD-10 cohort, the majority of Type 1 MI patients in the UCH subgroup were assigned a procedural DRG for PCI or CABG.
The simplest and most actionable conclusion to draw from these data is that hospitals must take considerable care when examining institutional outcomes and process measures for AMI patients. In particular, attention must be paid to how these patient populations are defined, as AMI populations defined by a DRG may be fundamentally different and receive different care than populations defined by ICD-10 codes. There are numerous practicing clinicians involved in the care of patients with AMI who likely have little, if any, understanding of the differences in these methodologies. Moreover, Chief Medical and Quality Officers, who contend with quality issues related to all the documented diagnoses in a hospital, typically think of AMI as one group of patients, not two. Extrapolating assumptions regarding performance (outcomes) and methods for improvement from one population (e.g. ICD-10) to a second dissimilar population (e.g. DRG) carries the risk of sub-optimizing patient care. That risk rises significantly when well-intentioned clinicians and leaders are not aware they are making this mental leap.
As it relates to national health policy, in addition to recent concerns raised about the equity8–11, safety12,13 and efficacy14,15 of value-based payment programs, these findings raise concern regarding a lack of standardization in AMI inclusion criteria. Our findings are particularly relevant to hospitals participating in the BPCIA program for AMI, which uses an AMI DRG to define program inclusion and an ICD-10 based cohort for measuring the quality of AMI care. Our findings suggest that quality is measured in a group of patients (ICD-10 cohort) that is substantially different from the patients actually included in the program (DRG cohort). The program’s use of two differing definitions for AMI – as opposed to holding the population definition constant – is akin to asking hospitals to do two things at once.
A central assumption of value-based payment programs – exemplified by the HRRP, VBP and BPCIA programs – is that there are modifiable behaviors that can be incentivized by restructuring hospital payments.16 In the case of AMI, the evidentiary basis for “good” behaviors that improve readmission rates, such as cardiac rehabilitation, are primarily based on trials in Type 1 MI patients.17 Performance measures endorsed by the American Heart Association and American College of Cardiology cater specifically to the care of patients with Type 1 MI.2 This is in part because there are very few evidence-based therapies for patients with T2MI and NIMI.18,19 Improving outcomes in the “non-Type 1 MI” population is an active area of research,20 but in the meantime, care of these patients should not be lumped together with care of individuals with Type 1 MI.
If value-based programs are to more effectively target Type 1 MI, the subgroup analysis from our study strongly supports using an ICD-10 based definition for AMI over a DRG-based definition. The ICD-10 group was comprised by a higher percentage of Type 1 MI patients than the DRG group (78% vs. 34%) and, not surprisingly, the ICD-10 cohort was more representative of outcomes and patterns of care among Type 1 MI patients. Our data suggest that this is likely because the majority of Type 1 MI patients (55%) end up with a procedural DRG, either for PCI or CABG (Supplemental Table IV), a finding that is consistent with nationwide trends in revascularization.21 The AMI DRG, therefore, includes only those “leftover” patients who were likely either too ill to undergo revascularization or for whom revascularization was not indicated. This is perhaps not surprising given that this group was composed primarily (66%) of T2MI and NIMI patients. With this in mind, patients included in DRGs for AMI may be suboptimal “targets” for payment reforms designed to improve AMI—specifically Type 1 MI—care.
It is important to note that ICD-10 based AMI cohorts are not perfect – over 20% of ICD-10 patients in our subgroup analysis had either T2MI or NIMI, which is similar to prior studies of ICD-9 codes.22–24 While our results suggest that T1MI patients and ICD-10 patients have similar outcomes, our single center analysis is likely under-powered to detect small differences observed in other studies.24 Further, while the ICD-10 system certainly has more diagnostic specificity than the DRG system, ICD-10 only recently implemented a code for Type 2 MI25 and still does not have a code for NIMI. While this new T2MI code is omitted from the cohort definitions for HRRP and VBP programs,4,5 T2MI and NIMI patients will continue to be misclassified in clinician documentation and, in some cases, included in these programs.26,27 They may simply be included less than a similar program, like the BPCIA, using DRG-based cohorts.
A critical question is whether there is a better way to define and administer AMI cohorts for value-based programs. Given the existing infrastructure of clinical cardiovascular registries, it is appropriate to determine whether these registries more reliably track performance measures among AMI patients. Transcatheter aortic valve replacement (TAVR) could provide a blueprint for this path as registry participation is mandated under the national coverage decision and as TAVR is increasingly paid for under the BPCIA.28,29 This provides an opportunity to use registry data to assess the quality of TAVR care within this value-based program.
This study has multiple limitations. First, it was conducted in a single integrated system of hospitals and, by design, only included patients with a coded diagnosis of AMI according to the discharge DRG or principal ICD-10 code. With this in mind, these findings must be applied with caution since they may be biased by institution-specific documentation and coding practices. Given the algorithmic nature of coding and secular trends in AMI care, we suspect that most hospitals would find that a majority of ICD-10 AMI patients are assigned a revascularization DRG (instead of an AMI DRG). Nevertheless, future studies should examine the extent to which there is hospital-level and system-level variation in this observation. Variation in MI types comprising ICD-10 versus DRG cohorts also merits further study since our findings are based on a single hospital and may not be representative of the whole UCHealth system. Rather than using our estimates of the proportion of MI types within each cohort, we would instead encourage institutions to sample their own AMI patients to better understand the breakdown of MI types within their ICD-10 and DRG cohorts. That we had 100% interrater agreement in terms of assessing T1MI based on chart review (see Supplemental Methods) suggests that such analyses are feasible, though we can never fully account for omitted or overlooked clinical information that may have changed a patient’s AMI diagnosis. A final limitation of our study is that the electronic health record is less reliable than more traditional sources of outcomes data.30 We wonder, for example, if rates of cardiac rehab referral would have been higher if we had been able to query a registry to answer our research question. We did our best to overcome this limitation by using a novel electronic data warehouse that integrates our EHR data with several local and regional healthcare databases.7
In conclusion, we found that a cohort defined by AMI DRGs differed significantly from a cohort derived using principal ICD-10 codes for AMI: there was little overlap between cohorts and DRG cohort patients had more comorbidities and higher rates of mortality and readmission. Likely contributing to these findings, we observed that many AMI patients in the ICD-10 cohort were assigned a procedural DRG for revascularization and that the DRG cohort contained a significantly higher proportion of T2MI and NIMI patients than the ICD-10 cohort. As national policy programs mature in defining patient populations and optimal measures of care, these findings suggest a need to revisit disparate and imperfect administrative definitions of AMI.
Supplementary Material
What is known
Medicare administers multiple value-based payment programs for AMI, some of which use ICD-10 codes to define AMI cohorts while others use AMI DRGs. The extent to which the AMI populations identified by these different mechanisms overlap is not known.
What the study adds
In a large health system in Colorado, there was only 19% agreement between ICD-10 and DRG-based inclusion criteria for value-based programs targeting AMI.
Compared to patients in the ICD-10 cohort, AMI patients in the DRG cohort had significantly higher rates of death both at 30 days and 1 year and readmission at 90 days.
These differences may be attributable to the fact that only 34% of patients with an AMI DRG had a Type 1 MI, compared to 78% of patients identified by ICD-10 codes.
Together, these findings suggest that divergent AMI cohorts in value-based programs have the potential to confuse efforts to improve AMI care.
Funding:
Dr. Levy received funding from National Institutes of Health (NIH) T32 Training Grant 5T32-HL007822. This publication was supported in part by NIH/NCATS Colorado CTSA Grant Number UL1 TR001082. Utilization of the REDCap database was supported by NIH/NCRR Colorado CTSI Grant Number UL1 TR002535. Data support was provided by the Health Data Compass Data Warehouse project (healthdatacompass.org).
Non-standard Abbreviations and Acronyms:
- AMI
Acute myocardial infarction
- BPCIA
Bundled Payments for Care Improvement Advanced
- CMS
Center for Medicare and Medicaid Services
- CKD
Chronic kidney disease
- CABG
Coronary artery bypass graft surgery
- DRG
Diagnosis related groups
- EHR
Electronic health record
- 4-UDMI
Fourth Universal Definition of Myocardial Infarction
- HF
Heart failure
- statin
HMG-CoA reductase inhibitors
- HRRP
Hospital Readmissions Reduction Program
- ICD-10
International classification of diseases, 10th revision
- NIMI
Non-ischemic myocardial injury
- PCI
Percutaneous coronary intervention
- TAVR
Transcatheter aortic valve replacement
- T1MI
Type 1 myocardial infarction
- T2MI
Type 2 myocardial infarction
- UCH
University of Colorado Hospital
Footnotes
Disclosures: The authors report no conflicts of interest. This program evaluation was determined to not be human subjects research by the Colorado Multiple Institutional Review Board.
References
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139:e56–e66. [DOI] [PubMed] [Google Scholar]
- 2.Jneid H, Addison D, Bhatt DL, Fonarow GC, Gokak S, Grady KL, Green LA, Heidenreich PA, Ho PM, Jurgens CY, et al. 2017 AHA/ACC Clinical Performance and Quality Measures for Adults With ST-Elevation and Non–ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2017;10:e000032. [DOI] [PubMed] [Google Scholar]
- 3.Center for Medicare and Medicaid Innovation (CMMI). BPCI Advanced. innovation.cms.gov. https://innovation.cms.gov/initiatives/bpci-advanced. Published May 31, 2019. Accessed June 5, 2019.
- 4.Centers for Medicare & Medicaid Services (CMS). Measure Methodology Reports: Mortality Measures. qualitynet.org. https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1163010421830. Published March 2019. Accessed March 30, 2019.
- 5.Centers for Medicare & Medicaid Services (CMS). Measure Methodology Reports: Readmission Measures. qualitynet.org. https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1219069855841. Published March 2019. Accessed March 30, 2019.
- 6.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20):97. [Google Scholar]
- 7.Health Data Compass. ucdenver.edu. http://www.ucdenver.edu/about/departments/healthdatacompass/Pages/default.aspx. Accessed June 5, 2019.
- 8.Blustein J, Borden WB, Valentine M. Hospital Performance, the Local Economy, and the Local Workforce: Findings from a US National Longitudinal Study. Sheikh A, ed. PLOS Med. 2010;7(6):e1000297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krinsky S, Ryan AM, Mijanovich T, Blustein J. Variation in Payment Rates under Medicare’s Inpatient Prospective Payment System. Health Serv Res. 2016;52:676–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oseran AS, Howard SE, Blumenthal DM. Factors Associated With Participation in Cardiac Episode Payments Included in Medicare’s Bundled Payments for Care Improvement Initiative. JAMA Cardiol. 2018; 3:761–766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joynt Maddox KE, Reidhead M, Hu J, Kind AJH, Zaslavsky AM, Nagasako EM, Nerenz DR. Adjusting for social risk factors impacts performance and penalties in the hospital readmissions reduction program. Health Serv Res. 2019;54:327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta A, Allen LA, Bhatt DL, Cox M, DeVore AD, Heidenreich PA, Hernandez AF, Peterson ED, Matsouaka RA, Yancy CW, et al. Association of the Hospital Readmissions Reduction Program Implementation With Readmission and Mortality Outcomes in Heart Failure. JAMA Cardiol. 2018; 3:44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wadhera RK, Maddox KEJ, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the Hospital Readmissions Reduction Program With Mortality Among Medicare Beneficiaries Hospitalized for Heart Failure, Acute Myocardial Infarction, and Pneumonia. JAMA. 2018;320:2542–2552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chee TT, Ryan AM, Wasfy JH, Borden WB. Current State of Value-Based Purchasing Programs. Circulation. 2016;133:2197–2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Evaluation of Medicare’s Bundled Payments Initiative for Medical Conditions. N Engl J Med. 2018;379:260–269. [DOI] [PubMed] [Google Scholar]
- 16.Joynt KE, Jha AK. Thirty-Day Readmissions -- Truth and Consequences. N Engl J Med. 2012;366:1366–1369. [DOI] [PubMed] [Google Scholar]
- 17.Doimo S, Fabris E, Piepoli M, Barbati G, Antonini-Canterin F, Bernardi G, Maras P, Sinagra G. Impact of ambulatory cardiac rehabilitation on cardiovascular outcomes: a long-term follow-up study. Eur Heart J. 2018;21:664. [DOI] [PubMed] [Google Scholar]
- 18.Sandoval Y, Jaffe AS. Type 2 Myocardial Infarction: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;73:1846–1860. [DOI] [PubMed] [Google Scholar]
- 19.White HD, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, Edelberg JM, Erglis A, Goodman SG, Hanotin C, et al. Effects of alirocumab on types of myocardial infarction: insights from the ODYSSEY OUTCOMES trial. Eur Heart J. 2019;380:581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lambrakis K, French JK, Scott IA, Briffa T, Brieger D, Farkouh ME, White H, Chuang AM-Y, Tiver K, Quinn S, Kaambwa B, et al. The appropriateness of coronary investigation in myocardial injury and type 2 myocardial infarction (ACT-2): A randomized trial design. Am Heart J. 2019;208:11–20. [DOI] [PubMed] [Google Scholar]
- 21.Masoudi FA, Ponirakis A, de Lemos JA, Jollis JG, Kremers M, Messenger JC, Moore JWM, Moussa I, Oetgen WJ, Varosy PD, et al. Trends in U.S. Cardiovascular Care: 2016 Report From 4 ACC National Cardiovascular Data Registries. J Am Coll Cardiol. 2017;69:1427–1450. [DOI] [PubMed] [Google Scholar]
- 22.Díaz-Garzón J, Sandoval Y, Smith SW, Love S, Schulz K, Thordsen SE, Johnson BK, Driver B, Jacoby K, Carlson MD, et al. Discordance between ICD-Coded Myocardial Infarction and Diagnosis according to the Universal Definition of Myocardial Infarction. Clin Chem. 2016;63:415–419. [DOI] [PubMed] [Google Scholar]
- 23.Arora S, Strassle PD, Qamar A, Wheeler EN, Levine AL, Misenheimer JA, Cavender MA, Stouffer GA, Kaul P. Impact of Type 2 Myocardial Infarction (MI) on Hospital‐Level MI Outcomes: Implications for Quality and Public Reporting. J Am Heart Assoc. 2018;7:e008661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martin LM, Januzzi JL Jr., Thompson RW, Ferris TG, Singh JP, Bhambhani V, Wasfy JH. Clinical Profile of Acute Myocardial Infarction Patients Included in the Hospital Readmissions Reduction Program. J Am Heart Assoc. 2018;7:842–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goyal A, Gluckman TJ, Tcheng JE. What’s in a Name?: The New ICD-10 (10th Revision of the International Statistical Classification of Diseases and Related Health Problems) Codes and Type 2 Myocardial Infarction. Circulation. 2017;136:1180–1182. [DOI] [PubMed] [Google Scholar]
- 26.Goyal A, Gluckman TJ, Levy AE, Mariani D, Perez C, Rose GA, Sweeney S, Thompson RC, Waites T, Tcheng JE. Translating the Fourth Universal Definition of Myocardial Infarction into Clinical Documentation. Cardiology. 2018; 34–36. [Google Scholar]
- 27.McCarthy C, Murphy S, Cohen JA, Rehman S, Jones-O’Connor M, Olshan DS, Singh A, Vaduganathan M, Januzzi JL, Wasfy JH. Misclassification of Myocardial Injury as Myocardial Infarction: Implications for Assessing Outcomes in Value-Based Programs. JAMA Cardiol. 2019;4:460–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Decision Memo for Transcatheter Aortic Valve Replacement (TAVR) (CAG-00430R). Center for Medicare and Medicaid Services (cms.gov). Published June 21, 2019. Accessed June 5, 2020. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=293&bc=ACAAAAAAQAAA&
- 29.Center for Medicare and Medicaid Innovation (CMMI). BPCI Advanced (innovation.cms.gov). Published September 2019. Accessed June 5, 2020. https://innovation.cms.gov/files/fact-sheet/bpciadvanced-my3-modeloverviewfs.pdf
- 30.Cowie MR, Blomster JI, Curtis LH, Duclaux S, Ford I, Fritz F, Goldman S, Janmohamed S, Kreuzer J, Leenay M, et al. Electronic health records to facilitate clinical research. Clin Res Cardiol. 2017;106:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


