Abstract
Human exposure to radio-therapeutic doses of gamma rays can produce late effects, which negatively affect cancer patients’ quality of life, work prospects, and general health. This study was performed to explore the role of Piceatannol (PIC) in the process of “mitochondrial biogenesis” signaling pathway as possible management of disturbances induced in stressed animal model(s) either by gamma-irradiation (IR) or administration of reserpine (RES); as a mitochondrial complex-I inhibitor. PIC (10 mg/kg BW/day; orally) were given to rats for 7 days, after exposure to an acute dose of γ-radiation (6 Gy), or after a single reserpine injection (1 g/kg BW; sc). Compared to reserpine or γ-radiation, PIC has attenuated hepatic and renal mitochondrial oxidative stress denoted by the significant reduction in the content of lipid peroxides and NO with significant induction of SOD, CAT, GSH-PX, and GR activities. PIC has also significantly alleviated the increase of the inflammatory markers, TNF-α and IL-6 and apoptotic markers, cytochrome c, and caspase-3. The decrease of oxidative stress, inflammation, and apoptotic responses were linked to a significant amelioration in mitochondrial biogenesis demonstrated by the increased expression and proteins’ tissue contents of SIRT1/p38-AMPK, PGC-1α signaling pathway. The results are substantiated by the significant amelioration in mitochondrial function verified by the higher levels of ATP content, and complex I activity, besides the improvement of hepatic and renal functions. Additionally, histopathological examinations of hepatic and renal tissues showed that PIC has modulated tissue architecture after reserpine or gamma-radiation-induced tissue damage. Piceatannol improves mitochondrial functions by regulating the oxidant/antioxidant disequilibrium, the inflammatory and apoptotic responses, suggesting its possible use as adjuvant therapy in radio-therapeutic protocols to attenuate hepatic and renal injuries.
Keywords: gamma irradiation, mitochondrial impairment, piceatannol, reserpine
Introduction
Radiation therapy or radiotherapy is the use of ionizing radiation to destroy cancer cells and to control selected metastases. A large majority of cancer patients undergo radiation therapy as a part of cancer treatment including cancers of the breast, prostate, cervix, head and neck, lung, and brain, as well as sarcomas.1 Side effects come from damage to healthy cells and tissues near the treatment area. Therapeutic abdominal irradiation for the treatment of bowel cancer is usually associated with higher rates of non-specific abdominal pain than those observed in radiation-naïve patients, years after treatment.2 Goldberg and Lehnert3 stated that avoidance of damage to non-cancerous tissues outside the target zone is a major priority in using ionizing radiation (IR). Radiation-induced oxidative stress involves a variety of deleterious cellular injuries including alterations in gene expression, augmented intracellular ROS production, mitochondrial damage, and apoptosis. Similarly, various reports linked xenobiotics-induced hepatic injury to a distinct type of factors including oxidative stress, inflammatory response, and cell death.
Mitochondrial complex-I, the largest and most complicated enzyme of the electron transport chain and the entry point for electrons to the respiratory chain, is considered the rate-limiting step in overall respiration, and thus play a crucial role in energy metabolism.4 Mutations in its subunits lead to a wide range of inherited neuromuscular and metabolic disorders.5 Reserpine is documented to inhibit complex-I, stimulate reactive oxygen/nitrogen species associated with inflammation, and mitochondrial dysfunction in various vital organs.6
The cellular mitochondrial volume comprises about 4%–25% of the total cell volume; depending on the cell type and state, thus, the mitochondria represent a substantial target for cytoplasmic irradiation.7 Mitochondrion plays a crucial role in the tissue bioenergetics status; therefore, its dysfunction is considered a prime trigger of diseases.8 The peroxisome proliferator-activated receptor-gamma coactivator-1α (PGC-1α) is an important transcriptional co-activator that induces both mitochondrial metabolism and biogenesis at the molecular level. PGC-1α has been reported to possess a pivotal role in various diseases, where it showed an altered expression in many organs after chemo- and radiotherapy.9 However, its role in radiation-induced mitochondrial dysfunction is still unclear. The activation of PGC-1α is controlled via Peroxisome proliferator-activated receptors (PPARs), AMP-activated protein kinase (AMPK), and Sirtuin1 (SIRT1). Briefly, AMPK phosphorylation promotes the expression and activation of PGC-1α; likewise, SIRT1 deacetylates and activates PGC-1α, regulates mitochondrial biogenesis.10 Thus, agents activating the SIRT1-mediated PGC-1α signaling pathways might be of vital significance in regulating the antioxidants and mitochondrial functional states following the toxic destruction caused by certain exo or endotoxins.11 An example of such agents is piceatannol (PIC), a polyphenol belonging to the stilbenes group; a resveratrol analog, existing naturally in plants. For example, both red and white grapes contain PIC at concentrations of 374 and 43 ng/g, respectively.11 In addition, passion fruit and Vaccinium berries are rich in PIC.12,13 It was reported that PIC possesses a wide spectrum of biological activities including antidiabetic, neuroprotective, cardioprotective, anti-allergic, and anti-aging.14–16 It also protects retinal pigment epithelium cells against UV-B irradiation.17 In light of the above-detailed information, this study aimed to modulate the radiation-mediated mitochondrial dysfunction as compared to that induced by the classical mitochondrial toxin; reserpine, with a focus on the potential effect of piceatannol against both stressors-induced liver and kidney injuries.
Materials and methods
Materials: Reserpine (methylreserpate 3,4,5-trimethoxybenzoic acid), piceatannol (3,3′,4,5′-tetrahydroxy stilbene) and all other chemical reagents, solvents, and buffers were obtained from Sigma-Aldrich Chemical Co. (St. Louis, MO, USA).
Animals: Male Wister Albino rats weighing 150–180 g were used in the present study; they were purchased from the breeding unit of Egyptian Holding Company for Biological Products and Vaccines. The animals were housed in standard cages and had free access to water and standard laboratory diet; all animals were subjected to the standard conditions of temperature and light-dark cycle. The present study was carried out according to the guidelines stated by the Research Ethics Committee of the National Centre for Radiation Research and Technology (NCRRT), Cairo, Egypt (Ref. No: 195/7/2020), which conformed to the international guidelines for the proper care and use of laboratory animals and complied with relevant legislation stated in the Guide for the Care and Use of Laboratory Animals (NIH publication No. 85–23, 1996).
Irradiation process: A single dose of 6 Gray (Gy) gamma-radiation was delivered to the whole body of rats at a dose rate of 0.67 Gy/min, was performed at the NCRRT (Cairo, Egypt) using a Canadian gamma cell-40 (137Cesium). The dose of radiation was calculated by the Dosimetry specialists in the NCRRT, based on the dose rate emitted by the 137Cesium source which was 0.67 Gy/min as confirmed by the NCRRT routine scheduled dose mapping and validation studies.
Experimental design: To assess the effects of PIC on the reserpine/radiation-induced mitochondrial dysfunction, rats were randomly assorted into six experimental groups; each group consisted of eight animals. Control (C) group: normal rats. PIC group: rats received piceatannol for seven successive days at a dose of 10 mg/kg/day orally. IR group: irradiated rats exposed to an acute dose of 6 Gy. IR + PIC group: rats orally received PIC as mentioned above following γ-irradiation (6 Gy). RES group; rats received a single reserpine injection; s.c., at a dose of 1 g/kg. RES + PIC group; rats orally received PIC following reserpine injection (as previously mentioned). PIC, IR, and RES doses administered in the present study were based on earlier studies18–20 respectively.
Blood and tissue sampling: At the end of the experimental period, rats were anaesthetized by intraperitoneal injection of Urethane (1.2 g/kg b.w.),21 then sacrificed by cervical decapitation. Blood was collected in heparinized and non-heparinized tubes to separate plasma and serum; respectively, by centrifugation at 3000 × g for 15 min using Hettich Mikro 22R centrifuge UP8U’I (Tuttlingen, Germany). Dissected liver and kidney tissues samples were collected and divided into two portions each; the first of which was stored at −80 °C for the further assessment of antioxidant biomarkers, pro-inflammatory mediators, apoptotic markers, and gene expressions. The second portion of liver and kidney samples were fixed in 10% neutral formalin and prepared for histopathological examination.
Methods
Separation of mitochondrial fraction: The liver and kidney mitochondrial fractions were prepared according to the method described by Lampl et al.22 Briefly, tissues were homogenized on ice using a Teflon pestle homogenizer in a medium containing 250 mM sucrose, 10 mM Tris–HCl, and 1 mM ethylene diamine tetra acetic acid (EDTA), pH 7.2 at 4°C. The homogenate was centrifuged at 600 × g for 10 min and then the supernatant was centrifuged for 5 min at 15,000 × g to obtain the mitochondrial pellet. The protein content of the mitochondrial fractions was determined using the method of Bradford.23
Assessment of mitochondrial oxidative stress status: The extent of lipid peroxidation was assessed using the thiobarbituric acid test for malondialdehyde (MDA), used as described by Yoshioka et al.24 Nitric oxide (NO) was measured according to the method of Miranda et al.25 Superoxide dismutase (SOD), catalase (CAT), glutathione reductase (GR), and glutathione peroxidase (GSH-PX) levels were determined according to the methods of Kakkar et al.,26 Bergmeyer et al.,27 Goldberg and Spooner,28 and Gross et al.,29 respectively.
Assessment of mitochondrial function: The activity of respiratory chain complex I was determined spectrophotometrically and expressed as µmoles of reduced or oxidized substrate per minute per milligram of mitochondrial protein. Complex I (NADH-ubiquinone oxidoreductase) activity was assayed using 100 μmol l−1 decyl ubiquinone as the electron acceptor and 200 μmol l−1 NADH as the donor, in a 10 mmol l−1 KH2PO4/K2HPO4 buffer, pH 7.5, containing 3.75 mg·mL−1 BSA, 2 mmol l−1 KCN, and 7.5 μmol l−1 antimycin A. Oxidation of NADH was then measured at 340 nm.30 The concentration of ATP was measured using Kit (Cat. No. S0027, Beyotime Biotechnology, Jiangsu, China) according to the manufacturer’s instructions.
Assessment of liver and kidney functions: Serum activities of aspartate aminotransferase (AST, Cat. No. 261 002), alanine aminotransferase (ALT, Cat. No. 263 002) and alkaline phosphatase (ALP, Cat. No. 217 002) were determined as biomarkers for liver function using commercial kits (Spectrum Diagnostics Co., Cairo, Egypt) according to the manufacturer’s protocol. Similarly; to assess kidney function, serum urea, and creatinine levels were quantified using Bio-Mid Diagnostics Kits (Cat. No. URE118100 and CRE106100, Cairo, Egypt), respectively according to the manufacturer’s instructions.
Assessment of the inflammatory markers: In rat serum, the pro-inflammatory cytokines; tumor necrosis factor alpha (TNF-α, Cat. No. RTA00) and interleukin 6 (IL-6, Cat. No. SR6000B) was investigated using kits purchased from R&D Systems, Inc., Minneapolis, USA.
Assessment of the apoptotic markers: The protein levels of cytochrome-c (Cyt-c, Cat. No. MITOISO1, Sigma Aldrich, St Louis, MO, USA), and Caspase-3 (CSB, Cat. No. -E08857r, Cusabio Biotech, Ltd, China) in the liver and kidney homogenates were quantified using ELISA technique according to the manufacturer’s instructions.
Molecular assessment of mitochondrial PGC-1α: The protein content of PGC-1α in liver and kidney rat homogenates was determined using an ELISA kit (CSB-EL018425RA, Cusabio Biotech, Ltd., China), all procedures were performed according to the manufacturer’s instruction.
Detection of SIRT1 and PGC-1α mRNA gene expressions in liver and kidney tissues by quantitative real time pcr (qRT-PCR): Total RNA was extracted from the hepatic and renal tissue homogenate using RNeasy Purification Reagent (Qiagen, Valencia, CA), according to the manufacturer’s instructions. Gel electrophoresis was used to assess the extracted RNA quality. First-strand cDNA was synthesized from 4 μg of total RNA using an Oligo (dT)12-18 primer and Superscript™ II-RNase Reverse Transcriptase. This mixture was then incubated at 42°C for 1 h, the kit was purchased from SuperScript Choice System (Life Technologies, Breda, the Netherlands). Using real time PCR (RT–PCR) with SYBR Green PCR Master Mix (Applied Biosystems, Foster City, CA USA) according to the method stated by Livak and Schmittgen,31 the gene expression for each sample was normalized to the expression of β-actin as follows:
Immunoblotting analysis: Rat liver and kidney homogenates were used for Western blotting analysis as previously defined by Mingone et al.32 using homogenization lysis buffer (Sigma-Aldrich, St. Louis, MD, USA). BCA assay kit (Thermo Fisher Scientific) was used to quantify the total protein content in the lysate, then each sample was loaded onto 8% sodium dodecyl sulphate–polyacrylamide gel electrophoresis (SDS–PAGE) and transferred to a nitrocellulose membrane (Amersham Bioscience, Piscataway, New Jersey, USA) using a semidry transfer apparatus (Bio-Rad, Hercules, California). The membranes were incubated with 5% non-fat milk blocking buffer containing 10 mmol Tris–HCl (pH 7.4), 150 mmol NaCl, and Tris-buffered saline with 0.05% Tween-20 (TBST) at 4°C, overnight. The membranes were then washed with TBST and incubated with antibodies of each of anti-SIRT1, anti-p-38, and anti-p-p-38 (Thr180/Tyr182) antibodies (1:500, Cell Signaling Technologies, Danvers, MA), for overnight on a roller shaker at 4°C. Immunoblotting was performed utilizing the indicated primary antibody followed by the appropriate horseradish peroxidase (HRP)-conjugated goat immunoglobulin (Amersham Biosciences). Chemiluminescence detection was performed using the Amersham detection kit, according to the manufacturer’s protocols, and exposed to X-ray film.
Protein levels were quantified by densitometric analysis of the autoradiograms using a scanning laser densitometer (Biomed Instruments). Results were determined after normalization for β-actin protein expression (as the housekeeping protein).
Histopathological examination
Samples of liver and kidney tissues were fixed in 10% formaldehyde solution and inserted in paraffin using standard methods. Sectioned tissues at 3-μm, were treated with hematoxylin-eosin (H&E) stain. Under a light microscope, the stained sections were inspected.33. The histopathological changes of hepatocytes and degree of periportal lymphocyte infiltration were recorded according to Ramos et al.34 The histopathological findings of renal lesions were scored according to Zhang et al.35
The hepatic lesions were scored according to the following criteria:
| Score | Description |
|---|---|
| 0 | Indicates minimal or no evidence of injury |
| I | Hydropic degeneration |
| II | Micro-vesicular steatosis |
| III | Necrosis (hypo-stained or absent nucleus, intense cytoplasmic eosinophilia, and destruction or loss of the architecture of the hepatocyte cord) |
| IV | Apoptosis |
The renal lesions were scored according to the following criteria:
| Score | Lesion |
|---|---|
| 0 | Normal histology |
| 1 | Tubular epithelial cell degeneration, without significant necrosis or apoptosis |
| 2 | Tubular epithelial cell necrosis and apoptosis <25% |
| 3 | Tubular epithelial cell necrosis and apoptosis <50% |
| 4 | Tubular epithelial cell necrosis and apoptosis <75% |
| 5 | Tubular epithelial cell necrosis and apoptosis ⩾75% |
Statistical analyses
Comparisons among different groups were performed by one way analysis of variance (ANOVA). It is a parametric statistical analysis that compares between- and within-groups variance to measure differences between two or more groups. All statistical analysis were performed by using statistical package SPSS (Statistical Program for Social Science) (SPSS® Chicago, IL, USA) version 15.0 software program. Each value represents the mean ± standard deviation collected from eight animals in each group. The difference between means were considered significant at P < 0.05.
Results
Influence of PIC on hepatic and renal mitochondrial oxidative stress
As for RES and IR effects on the hepatic oxidative stress status, a notable increase in liver MDA content associated with an obvious inhibition in the mitochondrial activities of SOD, CAT, GSH-Px, and GR were observed in RES and IR groups in comparison to the control group. PIC treatment has significantly attenuated the RES and IR-induced rise in hepatic MDA contents and restored the hepatic mitochondrial activities of SOD, CAT, GSH-Px, and GR observed in PIC + RES and PIC + IR groups as compared to those of the RES and IR untreated groups (Table 1).
Table 1.
Effect of PIC on hepatic and renal mitochondrial redox status in rats exposed to RES or γ-radiation.
| Parameters | Control | PIC | RES | RES + PIC | IR | IR + PIC |
|---|---|---|---|---|---|---|
| Hepatic oxidative stress status | ||||||
| MDA (nmol/g protein) | 288 ± 16a | 279 ± 13a | 399 ± 29b | 307 ± 24c | 465 ± 21d | 334 ± 29e |
| NO (nmol/g protein) | 13.5 ± 2.6a | 14.2 ± 1.4a | 5.8 ± 1.2b | 8.2 ± 1.8c | 4.9 ± 0.9b | 9.2 ± 0.7d |
| SOD (U/mg protein) | 8.8 ± 0.8a | 9.3 ± 0.6a | 3.7 ± 0.9b | 6.7 ± 1.8c | 4.1 ± 1.2b | 8.8 ± 0.5a |
| CAT (U/mg protein) | 2.5 ± 0.4a | 3.0 ± 0.3a | 0.3 ± 0.03b | 1.4 ± 0.2c | 0.4 ± 0.07b | 2.1 ± 0.3a |
| GSH-PX (U/mg protein) | 21.2 ± 0.8 a | 22.3 ± 0.8a | 7.2 ± 1.1b | 14.2 ± 0.7c | 9.1 ± 0.5d | 19.9 ± 1.1e |
| GR (U/g protein) | 759 ± 13a | 756 ± 10a | 426 ± 14b | 645 ± 19c | 331 ± 15d | 622 ± 18c |
| Renal oxidative stress status | ||||||
| MDA (nmol/g protein) | 291 ± 32a | 283 ± 22a | 393 ± 28b | 300 ± 31c | 457 ± 19d | 304 ± 30c |
| NO (nmol/g protein) | 18.8 ± 0.6a | 17.8 ± 1.2a | 9.7 ± 1.6b | 15.2 ± 0.6c | 7.1 ± 0.4b | 13.9 ± 1.3d |
| SOD (U/mg protein) | 7.0 ± 0.6a | 7.1 ± 2.3a | 2.4 ± 1.1b | 5.1 ± 3.6c | 3.2 ± 1.9d | 7.7 ± 3.0a |
| CAT (U/mg protein) | 2.3 ± 0.4a | 2.5 ± 0.5a | 0.3 ± 0.2b | 2.2 ± 0.2a | 0.5 ± 0.2c | 2.3 ± 0.8a |
| GPX (U/mg protein) | 11.3 ± 1.2a | 12.3 ± 1.4a | 5.2 ± 0.8b | 9.2 ± 0.7c | 4.4 ± 0.3d | 10.7 ±1.2a |
| GR (U/g protein) | 164 ± 13a | 160 ± 11a | 72 ± 8b | 105 ± 29c | 65 ± 9b | 139 ± 12a |
Data are presented as means ± SD (n = 8). Groups with different letters are significantly different, at P ⩽ 0.05. Groups with similar letters are not significantly different, at P ⩽ 0.05.
Regarding the effects of PIC against RES and IR-induced renal injury, nephrotoxicity biomarkers; serum urea and creatinine levels, were assessed. Results displayed in Table 1 revealed a marked elevation in serum urea and creatinine levels, accompanied by an elevation in renal MDA contents, together with the inhibition of renal mitochondrial SOD, CAT, GSH-Px, and GR activities in RES and IR groups as compared to the control group. On the other hand, PIC reversed those effects as it significantly reduced serum urea and creatinine levels as well as the renal MDA content. Moreover, PIC administration induced a significant elevation of renal mitochondrial SOD, CAT, GSH-Px, and GR activities in PIC + RES and PIC + IR groups, compared to RES and IR groups (Table 1).
| Gene symbol | Sequence of the primers used for real-time PCR | Accession number |
|---|---|---|
| SIRT1 | F: 5’-GTCTGTGCCTTCCAGTTGCT-3’ | NM_001372090.1 |
| R: 5’-CTGCTTGCTGTCCATACCTG-3’ | ||
| PGC-1α | F: 5’-ACATCgCAATTCTCCCTT-3’ | NM_031347.1 |
| R: 5’-CTCTTgAgCCTTTCgTgCTC-3’ | ||
| β-actin | F: 5’ CCAGGCTGGATTGCAGTT3’ | XM_017604191.1 |
| R: 5’GATCACGAGGTCAGGAGATG3’ |
Piceatannol effect on inflammatory markers and hepatic and renal functions
Serum liver enzymes activities; AST, ALT and ALP, were performed to determine the extent of liver injury induced by reserpine (RES) administration and ionizing radiation (IR) exposure. In Table 2, a significant increase in serum AST, ALT, and ALP activities in RES and IR groups; as compared to the control, is displayed. On the other hand, treatment of RES and IR rats with PIC significantly corrected the hepatic injury induced by each of the toxicants in serum AST and ALT activities as compared to the untreated RES and IR groups (Table 2). As displayed in Table 2, RES and IR groups showed a marked rise in serum levels of IL-6 and TNF-α, as compared to the control rats. Remarkably, administration of PIC to RES and IR groups significantly decreased serum IL-6 and TNF-α levels in PIC + RES and PIC + IR groups, compared to their corresponding control group.
Table 2.
Effect of PIC on inflammatory markers and hepatic and renal functions status in rats exposed to RES or γ-radiation.
| Parameters | Control | PIC | RES | RES + PIC | IR | IR + PIC |
|---|---|---|---|---|---|---|
| Inflammatory markers | ||||||
| TNF-α (pg/mL serum) | 26 ± 2a | 22 ± 4a | 125 ± 10b | 44 ± 6c | 121 ± 10b | 56 ± 12d |
| IL-6 (pg/mL serum) | 37 ± 4a | 35 ± 5a | 113 ± 30b | 43 ± 11a | 119 ± 16b | 57 ± 12c |
| Hepatic functions | ||||||
| ALT (U/mL serum) | 32 ± 5a | 31 ± 10a | 104 ± 8b | 49 ± 6c | 130 ± 19d | 71 ± 13e |
| AST (U/L serum) | 72 ± 9a | 70 ± 8a | 213 ± 5b | 90 ± 14c | 225 ± 18d | 105 ± 15e |
| ALP (U/L serum) | 110 ± 17a | 113 ± 12a | 164 ± 5b | 118 ± 7a | 159 ± 8b | 120 ± 6c |
| Renal functions | ||||||
| Urea (mg/dL serum) | 52 ± 5a | 49 ± 10a | 60 ± 8b | 37 ± 4c | 88 ± 12d | 55 ± 6a |
| Creatinine (mg/dL serum) | 0.66 ± 0.10a | 0.67 ± 0.15a | 0.90 ± 0.39b | 0.51 ± 0.25c | 0.78 ± 0.33d | 0.68 ± 0.36a |
Data are presented as means ± SD (n = 8). Groups with different letters are significantly different, at P ⩽ 0.05. Groups with similar letters are not significantly different, at P ⩽ 0.05.
Influence of PIC treatment on hepatic and renal mitochondrial changes in rats exposed to RES or γ-radiation
The activity of the mitochondrial Complex I enzyme and the ATP content were assessed as markers for both hepatic and renal mitochondrial functions. Each of reserpine injection and radiation exposure induced a significant decrease in hepatic and renal mitochondrial ATP contents and complex I activity, compared to untreated groups (Table 3). However, PIC-treated groups showed a significant increment in both the mitochondrial dehydrogenase (complex-1) activity and ATP content.
Table 3.
Effect of PIC on markers of hepatic and renal mitochondrial function in rats exposed to RES or γ-radiation.
| Parameters | Control | PIC | RES | RES + PIC | IR | IR + PIC |
|---|---|---|---|---|---|---|
| Hepatic mitochondrial function | ||||||
| ATP (µmol/mg protein) | 0.93 ± 0.45a | 0.97 ± 0.23a | 0.25 ± 0.19b | 0.68 ± 0.05c | 0.37 ± 0.04d | 0.87 ± 0.16e |
| Complex I (µmol NADH/min/mg protein) | 79 ± 10a | 78 ± 11a | 58 ± 6b | 68 ± 15c | 22 ± 5d | 57 ± 9b |
| Renal mitochondrial function | ||||||
| ATP (µmol/mg protein) | 0.98 ± 0.07a | 1.05 ± 0.06a | 0.39 ± 0.26b | 0.71 ± 0.15c | 0.47 ± 0.06d | 0.90 ± 0.45a |
| Complex I (µmol NADH/min/mg protein) | 68 ± 13a | 69 ± 9a | 50 ± 7b | 58 ± 14c | 19 ± 5d | 49 ± 10b |
Data are presented as means ± SD (n = 8). Groups with different letters are significantly different, at P ⩽ 0.05. Groups with similar letters are not significantly different, at P ⩽ 0.05.
Influence of PIC on hepatic and renal apoptotic markers
The mitochondrial dysfunction was also reflected in an obvious status of hepatic and renal cellular apoptosis. Data displayed in Table 4 indicated that each of RES and IR significantly increased the tissue contents of hepatic and renal cytochrome c and caspase-3 as compared to control group. Significant decrements were recorded in PIC + IR group (Table 4). In case of PIC + RES group, partial yet statistically significant improvements were observed, compared to RES group.
Table 4.
Effect of PIC on hepatic and renal apoptotic markers in rats exposed to RES or γ-radiation.
| Parameters | Control | PIC | RES | RES + PIC | IR | IR + PIC |
|---|---|---|---|---|---|---|
| Hepatic apoptotic markers | ||||||
| Caspase-3 (ng/mg protein) | 11.0 ± 2.5a | 10.4 ± 1.8a | 39.8 ± 3.5b | 22.3 ± 7.5c | 37.6 ± 9.1d | 15.7 ± 7.1e |
| Cytochrome-c (ng/mg) | 0.82 ± 0.49a | 0.77 ± 0.43a | 4.78 ± 0.6b | 1.8 ± 0.22c | 4.93 ± 0.79d | 0.91 ± 0.18b |
| Renal apoptotic markers | ||||||
| Caspase-3 (ng/mg protein) | 2.3 ± 0.4a | 2.1 ± 0.5a | 9.2 ± 1.4b | 5.3 ± 0.9c | 8.4 ± 1.9d | 3.4 ± 0.5a |
| Cytochrome-c (ng/mg) | 0.62 ± 0.11a | 0.59 ± 0.15a | 4.03 ± 0.52b | 1.75 ± 0.75c | 2.56 ± 0.98d | 0.81 ± 0.06b |
Data are presented as means ± SD (n = 8). G\groups with different letters are significantly different, at P ⩽ 0.05. Groups with similar letters are not significantly different, at P ⩽ 0.05.
PIC treatment upregulated the hepatocellular PGC-1α/p38 signaling molecules
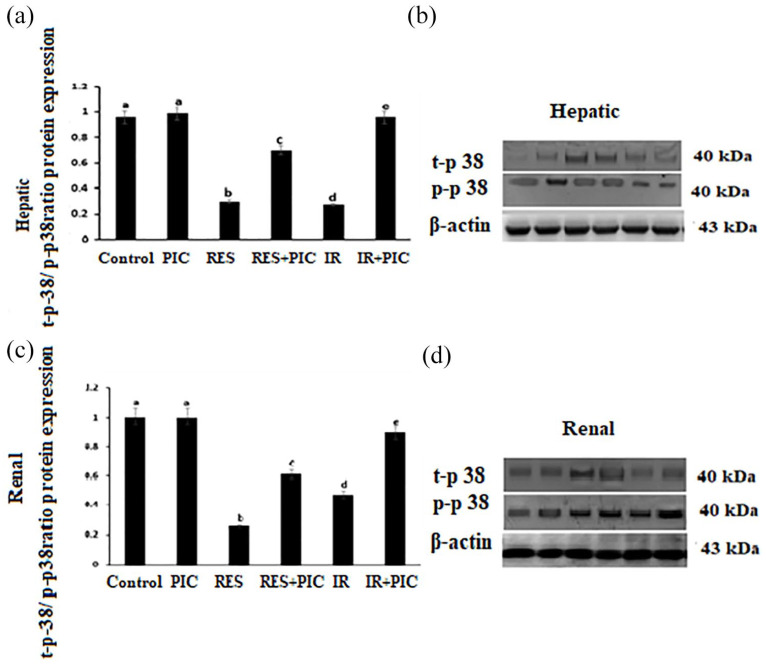
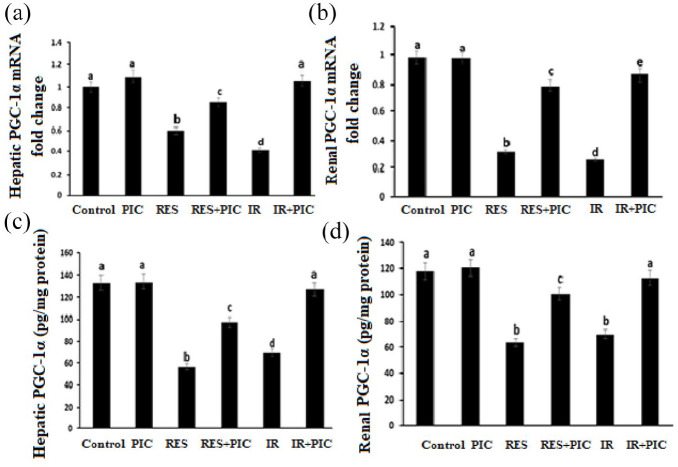
As shown in Figure 1a to d, each of RES and IR induced a profound reduction in protein expression of hepatic and renal active p38 (p-p38Thr180/Tyr182) as indicated by the decrement in p-p38/t-p38 expression. This was accompanied by a significant decline in hepatic and renal PGC-1α gene expression and protein level as seen in RES and IR groups, compared to the control group. PIC treatment improved the RES and IR-induced disruption expression of hepatic and renal active p38 and PGC-1α proteins when compared to RES and IR untreated groups; respectively (Figure 2a–d).
Figure 1.
Effect of whole body γ-irradiation (IR), reserpine (RES), and piceatannol (PIC) treatment on: rat hepatic and renal t-p-38/p-p38ratio protein expression (a and c), and the corresponding representative western blotting SDS-PAGE of hepatic and renal t-p38 and p-p-38 (40 kDa) normalized to β-actin (43 kDa) protein expression (b and d).
Data are presented as means ± S.E. (n = 8). Groups denoted with different letters are significantly different, at P ⩽ 0.05. Groups denoted with similar letters are not significantly different, at P ⩽ 0.05.
Figure 2.
Effect of whole body γ-irradiation (IR), reserpine (RES), and piceatannol (PIC) treatment on: hepatic and renal PGC-1α mRNA fold change (a and b), hepatic and renal PGC-1α protein level (c and d).
Data are presented as means ± S.E. (n = 8). Groups denoted with different letters are significantly different, at P ⩽ 0.05. Groups denoted with similar letters are not significantly different, at P ⩽ 0.05.
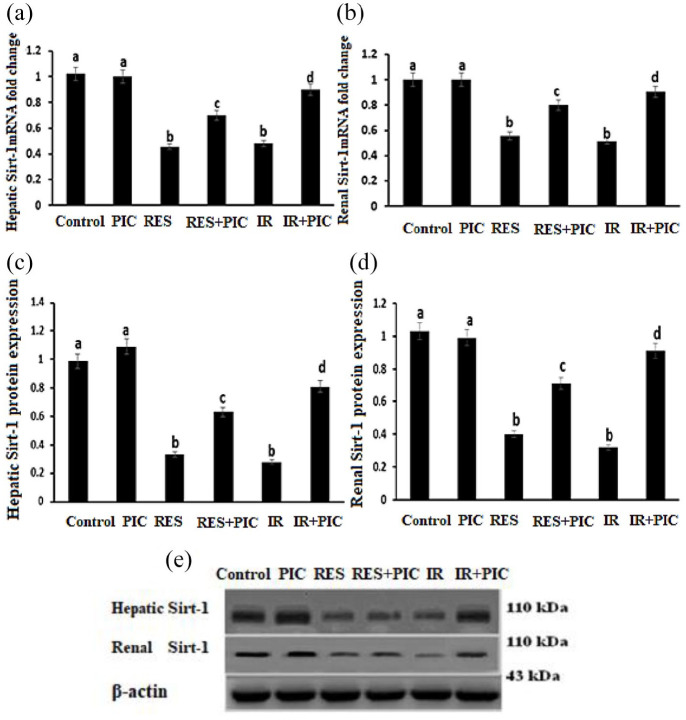
On the molecular level, SIRT-1 mRNA and protein expression levels were markedly decreased in RES and IR treated groups, compared to the control group. Noteworthy, PIC administration induced an improvement in hepatic and renal SIRT-1 gene expression and protein levels, compared to RES or IR groups (Figure 3a–e).
Figure 3.
Effect of whole body γ-irradiation (IR), reserpine (RES), and piceatannol (PIC) treatment on: rat hepatic and renal SIRT-1 mRNA fold change (a and b), hepatic and renal SIRT1 protein expression (c and d), and the corresponding representative western blotting SDS-PAGE of hepatic and renal SIRT-1 (110 kDa) normalized to β-actin (43 kDa) protein expressions (e).
Data are presented as means ± S.E. (n = 8). Groups denoted with different letters are significantly different, at P ⩽ 0.05. Groups denoted with similar letters are not significantly different, at P ⩽ 0.05.
Discussion
The current study investigated the alterations in mitochondrial biogenesis machinery induced by a single dose of radiation exposure, in comparison to that produced by the classical mitochondrial toxin; reserpine, intoxication via the induction of a state of oxidative stress along with subsequent changes of both liver and kidney mitochondrial functions. Other than oxidative stress, there are a variety of proposed mechanisms that may cause tissue injuries, such as the amplification of inflammatory reactions, the alternation in gene expression and cellular signaling pathways, and the induction of apoptosis.36
In the present study, the significantly higher tissue contents of lipid peroxides and NO with significant inhibition of SOD, CAT, GPX, and GR activities indicated both radiation and reserpine-induced physiological toxicities in liver and kidney tissues. Such disruptions in the redox signaling status induced a consequent dysfunction in each liver and kidney as reflected by the observed changes in liver function biomarkers; ALT, AST, and ALP as well as those of renal function; serum urea, and creatinine as compared to control group. Comparable results were reported in the study of Moustafa et al.37
A possible mechanism of those elevations is the RES-induced disruption of plasma membrane permeability hepatocytes leakage of these enzymes into serum.38 On the same line, a recent study39 reported that radiation-induced nephrotoxicity was triggered by ROS-mediated depression in Cyclin D1 expression in the renal nuclei and cells, thus inducing changes in the intracellular signaling with a consequent renal injury.
Following its systemic administration, reserpine is distributed to tissues based on their blood flow and easily penetrate cell membranes and then bind to the intracellular membrane components, particularly those rich in phospholipids, forming adducts inducing a nonstoichiometric inhibition of monoamine uptake,40 with a consequent oxidative stress status due to the oxidation processes of those monoamines by monoamine oxidases.41 Also, accumulation of tissue lipid peroxides induces an inflammatory status interfering with the mitochondrial functions in multiple organs including the liver and kidney.
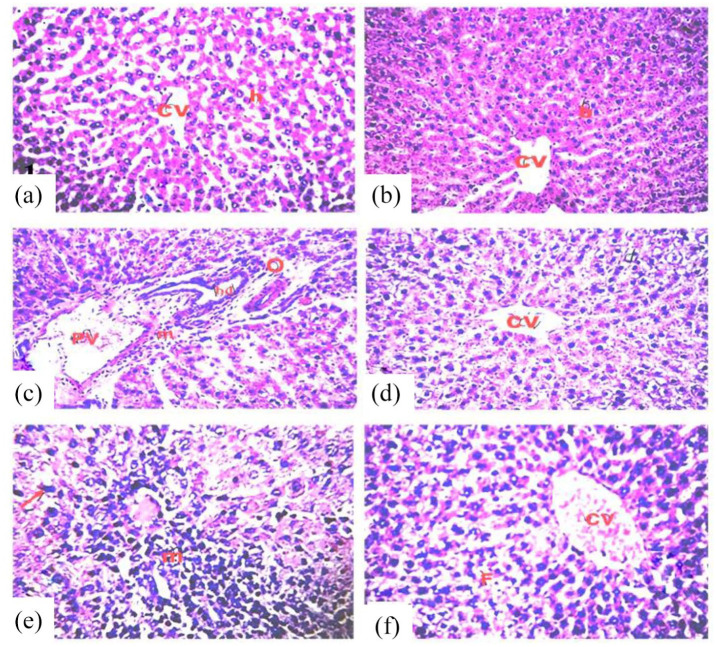
In the current work, the overproduction of ROS; resulting from IR-induced tissue water radiolysis, and RES-induced oxidative mitochondrial injury, can react with macromolecules and other essential targets inducing pronounced autolysis in mitochondria42 which results in mitochondria-mediated apoptosis of hepatocytes43 as confirmed by the significant increase in hepatic and kidney cytochrome c and caspase-3 activity shown in the present results. Furthermore, the hepatotoxicity and nephrotoxicity in RES and IR treated rats were herein confirmed by histopathological findings (Figures 4 and 5).
Figure 4.
Photomicrographs of sections in the liver of rats in the different groups, stained with hematoxylin and eosin (H&E), magnification ×400. (a) Control group. (b) PIC group showing normal architecture of hepatic lobule (h), and normal central vein (CV) (score 0). (c) RES group showing congested vessels, dilated portal vein (PV) with infiltration of inflammatory cells (m) in portal area (score IV). (d) RES + PIC group showing improved hepatic lobule and portal area (score I). (e) IR group showing disorganization of hepatic cords and necrotic changes of hepatocytes with apoptotic hepatocytes (arrow) (score IV). (f) IR + PIC group showing some improvement in hepatic architecture and reduction in portal lymphocytic infiltration (score I).
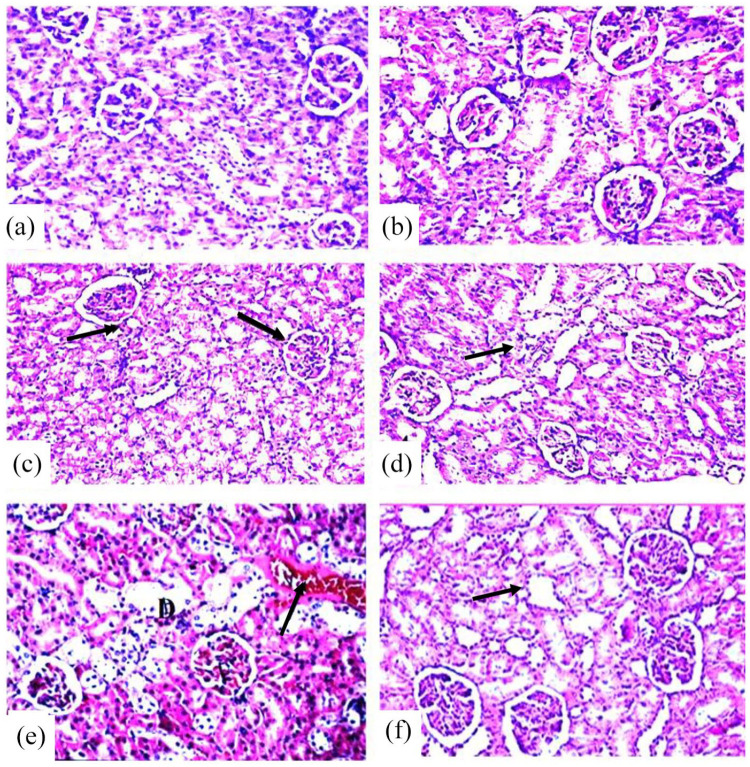
Figure 5.
Photomicrographs of sections in the kidney of rats in the different groups stained with hematoxylin and eosin (H&E), magnification ×400. (a) Control group. (b) PIC group showing normal histological structure of renal parenchyma characterized by circumscribe glomeruli with normal structure of capillary tufts and Bowman’s capsule. The renal tubules of both proximal and distal convoluted tubules showed intact epithelial lining with empty lumen (score 0). (c) RES group showing tubular epithelial lining with granulo-vacuolar degeneration (arrows) and narrowing of tubular lumen. The epithelial lining of both proximal and distal convoluted tubules lining showed necrosis and apoptosis (score 4). (d) RES + PIC group showing improvement of the kidney architecture with some swelling of tubular epithelial lining (score 1). (e) IR group showing leukocytic infiltration, degeneration in lying epithelium (D) of some tubules with congestion of blood vessels (score 4). (f) IR + PIC group showed mild swelling of tubular epithelial lining without significant pathological alteration (score 1).
In agreement with the above, we have shown in this study that, reserpine significantly reduced the level of ATP and the activities of succinate-dependent Complex I, Sirt-1, PGC-1α, and p38 MAPK, indicating an impaired function in the mitochondrial respiratory chain in the liver and renal tissues. This could be attributed to an increased lipid accumulation inducing down-regulation of SIRT1, which in turn reduces the expression of β-oxidation genes in the liver and kidney.44
The mitogen-activated protein kinases (MAPK) are involved in an activation loop consisting of ERK-1, ERK-2, JNKs, and the p38 kinase, a loop that is regulated by cellular environment-dependent mechanism affected by potentially injurious abiotic stress stimuli.45 A recent investigation of Park et al.46 stated that RES considerably induced MAPK, but inhibited p38 phosphorylation, which was noticed in the current data of hepatic and kidney tissues.
PIC is a potential candidate for the mitigation of hepatic and renal histological alterations in rats exposed to RES or γ-radiation
Altered levels of circulating cytokines might be non-invasive predictive biomarkers for radiotherapy-induced and clinical outcomes of cancer patients.47 Various studies have reported that under inflammatory conditions the cytokines have a key role in changeable p38/PGC-1α axis levels.48 In our study, RES and IR stimulated an inflammatory response reflected by the rise of TNF-α and IL-6 cytokines with reduced levels of p38/PGC-1α as compared to the corresponding control, suggesting the involvement of p38 AMPAK in hepatic and kidney injury. Thabet et al.49 reported that PPAR-α/p38 inhibition in hepatocytes resulted in an increased cytokines activation, with a consequent rise in chemokine’s expression for the recruitment of inflammatory cells, leading to hepatocytes apoptosis. Mechanisms proposed; RES may induce hepatocytes injury via the integration of smooth endoplasmic reticulum proliferation, ribosomes, and mitochondrial damage.38
PGC-1α plays a pivotal role in mitochondrial biogenesis in skeletal muscle50 and liver.51 Its deletion leads to reduced mitochondrial content.52 PGC-1α functions as an activating transcription factor and is involved in the coordinated regulation of nuclear and mitochondrial genes such as nuclear respiratory factors 1 and 2 and mitochondrial transcription factor-A.53
In the current study, piceatannol treatment was investigated for its regulatory and inducing effects on Sirt-1/PGC-1α involved in mitochondrial biogenesis and thus affecting its integrity and functions. The results revealed that piceatannol reduced lipid peroxidation and NO contents and increased GSH-PX, GR, SOD, and CAT activity in the liver and kidney. These effects of piceatannol could be attributed to its structural similarity with resveratrol and pterostilbene whose comparable effects have been reported in various studies. For example, resveratrol and pterostilbene were reported to augment the antioxidant status in diabetic animals.54,55 Similarly, the antioxidant effects of pterostilbene were attributed to its unique structure with one hydroxylic group and two methoxylic groups that scavenge ROS56; which are implicated in the initiation and pathogenesis of several diseases.
The results revealed also that piceatannol was able to attenuate the inflammatory and apoptotic responses against IR and RES toxicities in the liver and kidney. Piceatannol diminished the increase of the inflammatory markers, TNF-α and IL-6 and the apoptotic markers, cytochrome c and caspase-3. Furthermore, piceatannol boosted the expressions and proteins’ tissue contents of p-p38, SIRT1, PGC-1α. In this context, pterostilbene structurally similar to piceatannol was found to protect rats against diabetic myocardial oxidative stress and apoptosis via increased phosphorylation of adenosine monophosphate-activated protein kinase (AMPK).57 Moreover, pterostilbene has been reported to decrease cardiac oxidative stress through stimulation of AMPK/nuclear factor erythroid 2-related factor-2 (Nrf2)/heme-oxygenase (HO-1) pathway,58 and to possess neuroprotective properties against β-amyloid-induced inflammation through the inhibition of NLRP3/caspase-1 inflammasome pathway in the brain.59
PGC-1α is the “main key” of mitochondrial biogenesis that stimulates the mitochondrial gene expression and mitochondrial DNA replication.10 In the current study the results revealed that PIC treatment indorses deacetylation of PGC-1α and target gene expression, with increased protein levels of PGC-1α, which the SIRT1-dependent pathway activation such as a resveratrol analog on SIRT1 mRNA activation in the kidneys of diabetic nephropathy rats.53
The increased PGC-1α expression elicited by piceatannol; herein, was associated with enhanced activity of the antioxidant enzymes. In agreement with this observation, Rius-Pérez et al.,60 Valera-Alberni and Canto59 reported that PGC-1α is involved in the induction of ROS detoxifying enzymes. Thus, we speculated that the ability of piceatannol to suppress ROS improved antioxidant and reduced inflammatory and apoptotic responses might function through the SIRT1/p38-AMPK signaling pathway.
In rats treated with PIC after exposure to IR and RES, the decrease of oxidative stress, inflammatory, and apoptotic markers was accompanied by an amelioration in mitochondrial biogenesis. The higher levels of ATP content, and complex I activity indicates improved mitochondrial function. The modulator role of PIC in liver and kidney injury was confirmed by the improvement of liver and kidney functions and histopathological examinations. Because of its outstanding antioxidant function, piceatannol (PIC) is a beneficial compound. PIC derived its antioxidant property from the ethylene double bonds and phenolic hydroxyl groups.61 Li et al.62 found that PIC showed strong antioxidant activity in scavenging hydroxyl radicals, due to its four phenolic hydroxyl groups on the benzene ring. Setoguchi et al.63 have demonstrated that piceatannol revealed higher metabolic stability than resveratrol since, under their experiment; the pharmacokinetic curve for piceatannol was 2.1 times higher than that for resveratrol.
The results obtained in the current study go in line with the previous findings of who reported that strawberry fruits are a rich source of phytochemicals activates AMP-activated protein kinase (AMPK) signaling pathway, involved in mitochondrial biogenesis and antioxidant defenses.64–66 In addition, Wahdan et al.67 demonstrated that, PIC at a dose of 10 mg/kg was effective to cure kidney injury and the results obtained corroborate also that PIC (10 mg/kg BW) treatment of rats exposed to Cadmium-induced toxicity revealed inhibition of oxidative stress via upregulation in mRNA- and protein expression levels of Nrf2 pathway.18 In this study, we provide a new mechanism for PIC-mediated protection by demonstrating that PIC could protect against gamma radiation-induced oxidative stress, mitochondrial dysfunction and apoptosis via decreasing the tissue contents of lipid peroxides, NO and inducing SOD, CAT, GPX, and GR activities, together with the regulation of SIRT1/p38-AMPK, PGC-1α signaling pathway. Yet, our research has some limitations; for instance, the assessment of mitochondrial permeability transition, the assessment of complex II and inflammatory cytokines tissues contents, biochemical and transmission electron microscopy (TEM) of mitochondrial morphology would have been supportive parameters to describe the mechanisms of action of PIC in more details.
Conclusion
It could be concluded that piceatannol improve mitochondrial biogenesis and functions by regulating the oxidant/antioxidant disequilibrium, the inflammatory, and apoptotic responses, suggesting that the protective action of piceatannol might be a step forward in the development of adjuvant therapy for patients undergoing radiotherapy.
Acknowledgments
The authors would thank Prof. Dr. Ahmad Othman (Professor of Pathology, Pathology Department, Faculty of Veterinary Medicine, Cairo University) for the histopathological preparation, examinations, and reviewed of hepatic and renal tissue sections in this work.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: Ethical approval for this study was obtained from *the Ethical Committee of the National Centre for Radiation Research and Technology (NCRRT), Cairo, Egypt (Ref. No.: 195/7/2020)*.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Animal welfare: The present study followed international, national, and/or institutional guidelines for humane animal treatment and complied with relevant legislation.
ORCID iD: Enas Mahmoud Moustafa  https://orcid.org/0000-0003-0484-5759
https://orcid.org/0000-0003-0484-5759
References
- 1. Barton MB, Jacob S, Shafiq J, et al. (2014) Estimating the demand for radiotherapy from the evidence: A review of changes from 2003 to 2012. Radiotherapy and Oncology 112(1): 140–144. [DOI] [PubMed] [Google Scholar]
- 2. Savoie MB, Laffan A, Brickman C, et al. (2019) A multi-disciplinary model of survivorship care following definitive chemoradiation for anal cancer. BMC Cancer 19(1): 906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goldberg Z, Lehnert BE. (2002) Radiation-induced effects in unirradiated cells: A review and implications in cancer. The International Journal of Oncology 21(2): 337–349. [PubMed] [Google Scholar]
- 4. Sharma LK, Lu J, Bai Y. (2009) Mitochondrial respiratory complex I: Structure, function and implication in human diseases. Current Medicinal Chemistry 16(10): 1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brandt U. (2006) Energy converting NADH:quinone oxidoreductase (complex I). Annual Review of Biochemistry 75: 69–92. [DOI] [PubMed] [Google Scholar]
- 6. Singh D, Cho WC, Upadhyay G. (2015) Drug-induced liver toxicity and prevention by herbal antioxidants: An overview. Frontiers in Physiology 6: 363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cruz CD, Kang M-J. (2018) Mitochondrial dysfunction and damage associated molecular patterns (DAMPs) in chronic inflammatory diseases. Mitochondrion 41: 37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang Y, An H, Liu T, et al. (2019) Metformin improves mitochondrial respiratory activity through activation of AMPK. Cell Reports 29(6): 1511–1523.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gureev AP, Shaforostova EA, Popov VN. (2019) Regulation of mitochondrial biogenesis as a way for active longevity: Interaction between the Nrf2 and PGC-1α signaling pathways. Frontiers in Genetics 10: 435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhou YW, Li S, Yu Y, et al. (2018) SIRT1/PGC-1α signaling promotes mitochondrial functional recovery and reduces apoptosis after intracerebral hemorrhage in rats. Frontiers in Molecular Neuroscience 10: 443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Viñas P, Martínez-Castillo N, Campillo N, et al. (2011) Directly suspended droplet microextraction with in injection-port derivatization coupled to gas chromatography-mass spectrometry for the analysis of polyphenols in herbal infusions, fruits and functional foods. Journal of Chromatography A 1218(5): 639–646. [DOI] [PubMed] [Google Scholar]
- 12. Matsui Y, Sugiyama K, Kamei M, et al. (2010) Extract of passion fruit (Passiflora edulis) seed containing high amounts of piceatannol inhibits melanogenesis and promotes collagen synthesis. Journal of Agricultural and Food Chemistry 58(20): 11112–11118. [DOI] [PubMed] [Google Scholar]
- 13. Rimando AM, Kalt W, Magee JB, et al. (2004) Resveratrol, pterostilbene, and piceatannol in Vaccinium berries. Journal of Agricultural and Food Chemistry 52(15): 4713–4719. [DOI] [PubMed] [Google Scholar]
- 14. Piotrowska H, Kucinska M, Murias M. (2012) Biological activity of piceatannol: Leaving the shadow of resveratrol. Mutation Research 750(1): 60–82. [DOI] [PubMed] [Google Scholar]
- 15. Upadhyay S, Dixit M. (2015) Role of polyphenols and other phytochemicals on molecular signaling. Oxidative Medicine and Cellular Longevity 2015: 504253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Evans LW, Stratton MS, Ferguson BS. (2020) Dietary natural products as epigenetic modifiers in aging-associated inflammation and disease. Natural Product Reports 37(5): 653–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hao Y, Liu J, Wang Z, et al. (2019). Piceatannol protects human retinal pigment epithelial cells against hydrogen peroxide induced oxidative stress and apoptosis through modulating PI3K/Akt signaling pathway. Nutrients 11(7): 1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shi X, Fu L. (2019) Piceatannol inhibits oxidative stress through modification of Nrf2-signaling pathway in testes and attenuates spermatogenesis and steroidogenesis in rats exposed to cadmium during adulthood. Drug Design, Development and Therapy 13: 2811–2824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yamazaki H, Matsumoto K, Inoue T, et al. (1996) Induction of hepatocyte growth factor in the liver, kidney and lung following total body irradiation in rat. Cytokine 8(12): 927–932. [DOI] [PubMed] [Google Scholar]
- 20. Osubor CC, Nwanze EA. (1994) Inhibition of rat mitochondrial functions in vivo by 6-OHDA and reserpine. Research in Experimental Medicine 194(2): 109–117. [DOI] [PubMed] [Google Scholar]
- 21. Abd-El-Fattah AA, El-Sawalhi MM, Rashed ER, et al. (2010) Possible role of vitamin E, coenzyme Q10 and rutin in protection against cerebral ischemia/reperfusion injury in irradiated rats. International Journal of Radiation Biology 86(12): 1070–1078. [DOI] [PubMed] [Google Scholar]
- 22. Lampl T, Crum JA, Davis TA, et al. (2015) Isolation and functional analysis of mitochondria from cultured cells and mouse tissue. Journal of Visualized Experiments 97(97): 52076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bradford MM. (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Analytical Biochemistry 72: 248–254. [DOI] [PubMed] [Google Scholar]
- 24. Yoshioka T, Kawada K, Shimada T, et al. (1979) Lipid peroxidation in maternal and cord blood and protective mechanism against activated oxygen toxicity in the blood. American Journal of Obstetrics and Gynecology 135(3): 372–376. [DOI] [PubMed] [Google Scholar]
- 25. Miranda KM, Espey MG, Wink DA. (2001) A rapid, simple spectrophotometric method for simultaneous detection of nitrate and nitrite. Nitric Oxide 5(1): 62–71. [DOI] [PubMed] [Google Scholar]
- 26. Kakkar P, Das B, Viswanathan PN. (1984) A modified spectrophotometric assay of super oxide dismutase. Indian Journal of Biochemistry and Biophysics 21(2): 130–2. [PubMed] [Google Scholar]
- 27. Bergmeyer HU, Bergmeyer J, Grassl M. (eds.) (1986) Enzymes 1: Oxidoreductases, transferases. In: Methods of Enzymatic Analysis, 3rd edn, vol. 3. Weinheim, Germany: VCH. [Google Scholar]
- 28. Goldberg DM, Spooner RJ. (1983) Methods of enzymatic analysis. In: Bergmeyen HV. (ed.) 3rd edn., vols. 258–265. Deerfield Beach: Verlag Chemie, F1; p.3. [Google Scholar]
- 29. Gross R, Bracci R, Rudolph N, et al. (1967) Hydrogen peroxide toxicity and detoxification in the erythrocytes of newborn infants. Blood 29(4): 481–493. [PubMed] [Google Scholar]
- 30. William S, Immo E, Allison W, et al. (2009) Methods in enzymology. In: Mitochondrial function, part à mitochondrial electron transport complexes and reactive oxygen species, London: Elsevier Inc, pp.174–179. [Google Scholar]
- 31. Livak KJ, Schmittgen TD. (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta C(T)) method. Methods 25(4): 402–408. [DOI] [PubMed] [Google Scholar]
- 32. Mingone CJ, Gupte SA, Quan S, et al. (2003) Influence of heme and hemeoxygenase-1 transfection of pulmonary microvascular endothelium on oxidant generation and cGMP. Experimental Biology and Medicine (Maywood) 228(5): 535–559. [DOI] [PubMed] [Google Scholar]
- 33. Bancroft JD, Stevans A, Turner DR. (2013) Theory and Practice of Histological Techniques, 4th edn. Edinburgh: Churchill Livingstone. [Google Scholar]
- 34. Ramos CAF, Sá RCDS, Alves MF, et al. (2015) Histopathological and biochemical assessment of d-limonene-induced liver injury in rats. Toxicology Reports 2(2): 482–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang J, Brown RPS, Shaw M, et al. (2008) Immunolocalization of KIM-1, RPA-1, and RPA-2 in kidney of gentamicin-, mercury-, or chromium-treated rats: Relationship to renal distributions of iNOS and nitrotyrosine. Toxicologic Pathology 36(3): 397–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McKelvey KJ, Hudson AL, Back M, et al. (2018) Radiation, inflammation and the immune response in cancer. Mammalian Genome 29(11–12): 843–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Moustafa EM, Rashed ER, Rashed RR. (2021) Pterostilbene inhibits dyslipidemia-induced activation of progenitor adipose gene under high-fat diet and radiation stressor. Natural Product Communications 16(3): 1–12. [Google Scholar]
- 38. Al-Bloushi S, Safer AM, Afzal M, et al. (2009) Green tea modulates reserpine toxicity in animal models. Journal of Toxicological Sciences 34(1): 77–87. [DOI] [PubMed] [Google Scholar]
- 39. Moustafa EM, Hassan AA, El-Khashab IH, et al. (2020) The role of garcinol in abrogating cyclophosphamide/radiation nephrotoxicity via suppressing Mincle/Syk/NF-κB signaling pathway. Toxin Reviews 2020: 1–12. [Google Scholar]
- 40. Mandela P, Chandley M, Xu YY, et al. (2010) Reserpine-induced reduction in norepinephrine transporter function requires catecholamine storage vesicles. Neurochemistry International 56(6–7): 760–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yao X, Li L, Kandhare AD, et al. (2020) Attenuation of reserpine-induced fibromyalgia via ROS and serotonergic pathway modulation by fisetin, a plant flavonoid polyphenol. Experimental and Therapeutic Medicine 19(2): 1343–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Miller MA, Zachary JF. (2017) Mechanisms and morphology of cellular injury, adaptation, and death. Pathologic Basis Veterinary Disease 2017: 2–43. [Google Scholar]
- 43. Liu Z, Li T, Zhu F, et al. (2019) Regulatory roles of miR-22/Redd1-mediated mitochondrial ROS and cellular autophagy in ionizing radiation-induced BMSC injury. Cell Death Disease 10(3): 227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Opazo-Ríos L, Mas S, Marín-Royo G, et al. (2020) Lipotoxicity and diabetic nephropathy: Novel mechanistic insights and therapeutic opportunities. International Journal of Molecular Sciences 21(7): 2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kumar D, Jugdutt BI. (2003) Apoptosis and oxidants in the heart. Journal of Laboratory and Clinical Medicine 142(5): 288–297. [DOI] [PubMed] [Google Scholar]
- 46. Park R, Lee KI, Kim H, et al. (2017) Reserpine treatment activates AMP activated protein kinase (AMPK). Natural Product Sciences 23(3): 157–161. [Google Scholar]
- 47. Singh J, Sohal SS, Lim A, et al. (2019) Cytokines expression levels from tissue, plasma or serum as promising clinical biomarkers in adenocarcinoma of the prostate: A systematic review of recent findings. Annals of Translational Medicines 7(11): 245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cheng CF, Ku HC, Lin H. (2018) PGC-1α as a pivotal factor in lipid and metabolic regulation. International Journal of Molecular Sciences 19(11): 3447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Thabet NM, Abdel-Rafei MK, Moustafa EM. (2020) Boswellic acid protects against bisphenol-A and gamma radiation induced hepatic steatosis and cardiac remodelling in rats: role of hepatic PPAR-α/P38 and cardiac calcineurin-A/NFATc1/P38 pathways. Archives of Physiology and Biochemistry 14: 1–19. [DOI] [PubMed] [Google Scholar]
- 50. Zhang L, Zhang Y, Chang X, et al. (2020) Imbalance in mitochondrial dynamics induced by low PGC-1α expression contributes to hepatocyte EMT and liver fibrosis. Cell Death Disease 11(4): 226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Leone TC, Kelly DP. (2011) Transcriptional control of cardiac fuel metabolism and mitochondrial function. Cold Spring Harbor Symposium on Quantitative Biology 76: 175–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Choi HI, Kim HJ, Park JS, et al. (2017) PGC-1α attenuates hydrogen peroxide-induced apoptotic cell death by upregulating Nrf-2 via GSK3β inactivation mediated by activated p38 in HK-2 Cells. Scientific Reports 7(1): 4319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sedlak L, Wojnar W, Zych M, et al. (2018) Effect of resveratrol, a dietary-derived polyphenol, on the oxidative stress and polyol pathway in the lens of rats with streptozotocin-induced diabetes. Nutrients 10(10): 1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Millán I, Desco MDC, Torres-Cuevas I, et al. (2019) Pterostilbene prevents early diabetic retinopathy alterations in a rabbit experimental model. Nutrients 12(1): 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ullah O, Li Z, Ali I, et al. (2019) Pterostilbene alleviates hydrogen peroxide-induced oxidative stress via nuclear factor erythroid 2 like 2 pathway in mouse preimplantation embryos. Journal of Reproduction and Development 65(1): 73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kosuru R, Cai Y, Kandula V, et al. (2018) AMPK contributes to cardioprotective effects of pterostilbene against myocardial ischemia–reperfusion injury in diabetic rats by suppressing cardiac oxidative stress and apoptosis. Cellular Physiology and Biochemistry 46(4): 1381–1397. [DOI] [PubMed] [Google Scholar]
- 57. Tang T, Duan Z, Xu J, et al. (2020) Pterostilbene reduces endothelial cell injury in vascular arterial walls by regulating the Nrf2-mediated AMPK/STAT3 pathway in an atherosclerosis rat model. Experimental and Therapeutic Medicine 19(1): 45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Li Q, Chen L, Liu X, et al. (2018) Pterostilbene inhibits amyloid-β-induced neuroinflammation in a microglia cell line by inactivating the NLRP3/caspase-1 inflammasome pathway. Journal of Cellular Biochemistry 119(8): 7053–7062. [DOI] [PubMed] [Google Scholar]
- 59. Kershaw J, Kim KH. (2017) The therapeutic potential of piceatannol, a natural stilbene, in metabolic diseases: A review. Journal of Medicinal Food 20(5): 427–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Rius-Pérez S, Torres-Cuevas I, Millán I, et al. (2020) PGC-1α, inflammation, and oxidative stress: An integrative view in metabolism. Oxidative Medicine and Cellular Longevity 2020: 1452696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Valera-Alberni M, Canto C. (2018) Mitochondrial stress management: A dynamic journey. Cell Stress 2(10): 253–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Li XX, Yan RA, Duan HY. (2011) Synthesis and antioxidant activity of piceatannol. Food Fermentation Industries 37: 78–81. [Google Scholar]
- 63. Setoguchi Y, Oritani Y, Ito R, et al. (2014) Absorption and metabolism of piceatannol in rats. Journal of Agricultural and Food Chemistry 62(12): 2541–2548. [DOI] [PubMed] [Google Scholar]
- 64. Martin H, Burgess EJ, Smith WA, et al. (2015) NB. JAK2 and AMP-kinase inhibition in vitro by food extracts, fractions and purified phytochemicals. Food Functional 6(1): 305–312. [DOI] [PubMed] [Google Scholar]
- 65. Giampieri F, Alvarez-Suarez JM, Cordero MD, et al. (2017) Strawberry consumption improves aging-associated impairments, mitochondrial biogenesis and functionality through the AMP-activated protein kinase signaling cascade. Food Chemistry 234: 464–471. [DOI] [PubMed] [Google Scholar]
- 66. Forbes-Hernández TY, Giampieri F, Gasparrini M, et al. (2017) Lipid accumulation in HepG2 cells is attenuated by strawberry extract through AMPK activation. Nutrients 9(6): 621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Wahdan SA, Azab SS, Elsherbiny DA, et al. (2019) Piceatannol protects against cisplatin nephrotoxicity via activation of Nrf2/HO-1 pathway and hindering NF-κB inflammatory cascade. Naunyn-Schmiedeberg’s Archives of Pharmacology 392(11): 1331–1345. [DOI] [PubMed] [Google Scholar]