Abstract
Background
Of 133 million births globally, 3.7 million died in the neonatal period and 3 million are stillborn. The perinatal mortality rate in Ethiopia is 46 per 1000 pregnancies. However, area-specific information is limited in this regard. Therefore, this study aimed to determine the magnitude and determinants of adverse perinatal outcomes in Northern Ethiopia.
Method
An institution-based cross-sectional study was conducted by reviewing the medical records of mothers who gave birth between September 2015 and August 2016. The completeness and consistency of data were checked. Descriptive statistics were computed. A multinomial logistic regression model was fitted to identify determinants of adverse perinatal outcomes. Odds ratio with 95%CI was used and variables that had a P-value of < 0.05 in the final model were considered statistically significant.
Result
The magnitude of adverse perinatal outcomes was 214/799(27.47 %). Out of that, 10.8% had a perinatal mortality outcome, and 16.7% had a perinatal morbidity. Not using modern contraceptives(AOR = 1.7, 95% CI: 1.1-2.7), labor induction or augmentation(AOR = 3.0, 95% CI: 1.2-7.8), obstetric complications(AOR = 2.2, 95% CI: 1.1-4.5), attending antenatal care(AOR = 0.4, 95% CI: 0.2-0.8), primigravida (AOR = 0.5, 95% CI: 0.3-0.9), had no history of medical illness(AOR = 0.5, 95% CI: 0.3-0.8), and urban residency(AOR = 1.9, 95% CI, 1.1-2.9) were the significant determinants of perinatal outcome.
Conclusion
The magnitude of adverse perinatal outcomes was considerable and 1 in 5 neonates either had morbidity conditions or died. Improving family planning utilization, ANC, referral linkage, and management of obstetric complications could help to reduce the undesirable consequences of perinatal outcomes.
Keywords: low birth weight, prematurity, perinatal mortality, stillbirth, Ethiopia
Introduction
Worldwide it is estimated that there are 133 million live births annually, 5.9 million under-five deaths with 3.7 deaths during the neonatal period, and 3 million stillborn. A total of 98% of these deaths occur in the developing world. The average neonatal mortality rate in developing countries is 31/1000 live births while it is 4/1000 live births in developed countries. In Africa, the sub-Saharan regions of eastern, western, and central Africa have neonatal mortality between 40 and 46/1000 live births. Stillbirth rates have also remained high in sub-Saharan Africa with the rate of 38/1000 live births.1
In Ethiopia, 1 in every 35 children dies within the first month, 1 in every 21 children dies before celebrating the first birthday, and 1 in every 15 children dies before reaching the fifth birthday. According to Ethiopian Demographic and Health Survey (EDHS) 2016, the perinatal mortality in Ethiopia is 30/1000 live births and it is 44/1000 births in Amhara regional state where this study is conducted.2 In a household survey done in the Amhara region, North Gondar on the prevalence and associated factors of neonatal mortality among 3600 mothers, the neonatal mortality rate was 43.8 per 1000 live births.3
Fetal and extrauterine life forms a continuum during which human growth and development are influenced by genetic, environmental, and social factors. Perinatal mortality (PNM) refers to the death of a fetus after the age of viability (28 weeks), until the first seventh day of life.4
Of the global magnitude of 2.6 million stillbirths around 1.6 million stillbirths occur during labor in the low/middle-income countries where a significant proportion of women give birth at home usually in the absence of an attendant.5 Neonatal mortality is highest during the first 24 hours of life and it accounts for 65% of all infant deaths (deaths before 1 year of age).6,7 Nowadays, the widespread application of neonatal intensive care improved the survival of low birth weight (LBW) infants remarkably.8
Perinatal mortality rate could be affected by parity, gestational age, birth weight, congenital anomalies, infections, and exposure to adverse factors during pregnancy, labor, and/or delivery.9-11 Generally, it is influenced by prenatal, maternal, and fetal conditions and by circumstances surrounding delivery. Perinatal deaths are associated with intrauterine growth restriction (IUGR) which is a condition that predisposes the fetus to asphyxia and neonatal infections.12,13 Generally, the predictors of adverse perinatal outcomes could be maternal factors such as multiparty, multiple pregnancies, hypertensive disorders, uterine rupture, trauma, abnormal labor, diabetes, sepsis, post-term pregnancy, drugs and Rhesus incompatibility, maternal age (both high and low), and preterm delivery; fetal factor, for instance, non-vertex presentation, gestational age, prematurity, chromosomal anomalies, and non-chromosomal birth defects; placental factors such as feto-maternal hemorrhage, abruption, placenta previa, cord accident, placental insufficiency, intrapartum asphyxia, twin-to-twin transfusion, and chorioamnionitis.10,14,15
The essential elements of a focused approach to antenatal care are recognizing and managing pregnancy-related complications, screening for conditions and diseases, taking preventive measures, and planning a birth. According to WHO guidelines, a higher frequency of antenatal contacts reduced the likelihood of stillbirths. Eight or more contacts for antenatal care can reduce perinatal deaths by up to 8 per 1000 births when compared to 4 visits.12 However, an inequity exists and young, rural, poor, and less educated women may not benefit from ANC services or may drop out due to lack of health care access and low-quality services.13
Although there is information about perinatal mortality in Ethiopia, and there is limited information specific to the study area. Therefore, this study aimed to determine the magnitude and determinants of adverse perinatal outcomes in Northern Ethiopia and this would ultimately contribute to overcoming the prevailing challenges in the control of perinatal mortality in Ethiopia.
Methods and Materials
Study Design and Setting
An institution-based cross-sectional study was conducted by reviewing medical records of mothers who gave birth from September 2015 to September 2016 in Tefera Hailu Metasebia Hospital (THMH), Wag Himra zone, Amhara Regional State, Ethiopia. The hospital has 128 health professionals in different fields including a surgeon, emergency surgical officers, general practitioners, health officers, nurses, laboratory technicians, and 52 supporting staff. Also, it has 32 inpatient beds (14 gynecology and 18 obstetrics) and 6 delivery beds in the gynecology and obstetrics departments. Currently, the gynecology obstetrics department runs by emergency surgical officers and midwives.
Study Population
The study population includes all neonates born in Tefera Hailu Memorial Hospital from September 2015 to August 2016. Records with grossly incomplete data with relevant information were excluded from the study. The total sample size of the study was 836. Data were extracted from registration books, delivery registration, and maternal and neonatal cards. The data were collected by 2 trained midwives under the supervision of the research team.
Operational Definitions
Adverse perinatal outcome: morbidity or mortality that happens after 28 weeks of gestation and within 7 days of birth. In this study, perinatal outcomes had 3 categories described as favorable, morbidity, or mortality outcomes. A favorable outcome was considered in the absence of morbidity or mortality.
Neonatal morbidity: when a neonate has at least one of the following clinical presentations diagnosed by a physician within 7 days of birth such as perinatal asphyxia, thermoregulation, prematurity, infection in neonates, jaundice, metabolic disorder, meconium aspiration syndrome, neonatal seizure, neonatal hematologic problems, birth trauma, shock in the neonates, congenital malformations, and acute or emergent surgical conditions.
Perinatal Mortality (PM): the death of a fetus after the age of viability (28 weeks of gestation) until the seventh day after birth (including stillbirth).
Stillbirth or fetal death: birth after 28 completed weeks of gestation with the absence of signs of life at or after birth (death happened before or during labor and birth).
Neonatal mortality (NM): Neonatal death within the first 28 days after birth. It can also be divided into the death of a live-born baby within the first 7 days of age (early neonatal mortality-ENM) and death after 7 days until the 28th day of age (late neonatal mortality-LNM).
Low birth weight (LBW): a birth weight of <2500 g.
Very low birth weight: a birth weight of <1500 g.
Preterm birth was defined as a birth before 37 completed weeks; term birth was defined when a mother gives birth between 37 and 42 completed weeks; post-term was defined as delivery after 42 completed weeks.
A cord accident was defined as an event that happened during labor and delivery that includes cord prolapse, cord presentation, cord entanglement, and cord knot.
Antepartum hemorrhage (APH) was defined as bleeding from the genital tract of the pregnant mother after the fetus has reached the age of viability (which is after 28 completed weeks or fetal weight of 1000 gm or more), and before the fetus is delivered.
Data Management and Analysis
Data were first entered into an Excel spreadsheet and exported to SPSS version 20. Descriptive statistics were computed, and multinomial logistic regression analysis was used to identify determinants of adverse perinatal outcomes. Factors that had a P-value of ≤.20 in the bivariable analysis and variables with well-known clinical significance with adverse perinatal outcomes were fitted into the final model of multivariable multinomial logistic regression. The odds ratio with 95% CI was used to declare the presence and strength of association. Variables with a P-value of < .05 in the final model were considered statistically significant.
Results
Socio-Demographic Characteristics
A total of 836 newborns were delivered at Tefera Hailu Memorial Hospital from September 2015 to August 2016, and 57 of them were excluded due to the incompleteness of the information on the medical records. The median age of mothers was 25 years with a range of 16 to 45. Of all the new-borns, 429 (55.1%) were males and 408 (52.8%) were from urban residents (Table 1).
Table 1.
Socio-Demographic Characteristics of New-Borns and Their Mothers in Tefera Hailu Memorial Hospital from September 2015 to August 2016 (n = 779).
| Socio-demographic characteristics | 95% CI | ||||
|---|---|---|---|---|---|
| Variable | Category | Frequency | Percentage | Lower | Upper |
| Residence | Urban | 412 | 52.8 | 49.6 | 56.5 |
| Rural | 367 | 47.1 | 43.5 | 50.5 | |
| Sex of newborn | Male | 429 | 55 | 51.3 | 58.9 |
| Female | 350 | 45 | 41.1 | 48.7 | |
| Age of mother | Age <18 | 41 | 5.3 | 3.7 | 6.9 |
| Age 18-35 | 671 | 86.1 | 83.7 | 88.7 | |
| Age >35 | 67 | 8.6 | 6.7 | 10.5 | |
Obstetric Characteristics
The total number of neonates delivered from mothers who had 1 or more obstetric complications was 69 (8.8 %). It includes antepartum hemorrhage 33 (4.2 %), premature rupture of membrane 28 (3.6%), oligohydramnios 9 (1.1%), polyhydramnios 7 (0.9 %), and malpresentation 46 (5.9 %). Of the mothers, 340 (43.6 %) were primigravida and 127(16.3 %) had a poor obstetric history. Before the current pregnancy, 315 (40.4 %) had used modern contraceptives. The median duration of labor was 11 hours, and 49 (6.3 %) of the labor was induced. Two-hundred-ninety (36.3 %) of the mothers had never attended ANC.
The mode of delivery was vaginal for 611 (78.4 %), cesarean section or laparotomy for 146 (18.7 %), and instrument-assisted for 20 (2.6 %) mothers. A congenital anomaly was present among 12 (1.5 %) births (Figure 1).
Figure1.
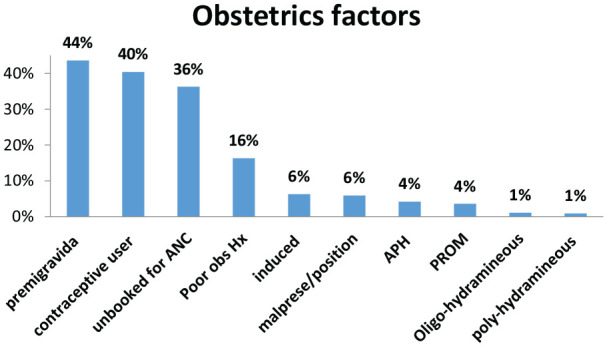
Obstetrics related conditions of mothers who gave birth in THMH, Amhara region, Ethiopia; September 2015 to September 2016 (n = 779).
Medical Factors
The total number of newborns delivered from mothers who had a medical illness was 96 (12 %). The medical problems were HIV 34 (4.3 %), anemia 24 (3.1 %), hypertensive disorders of pregnancy 19 (2.4 %), and others (urinary tract infection (UTI), acute gastroenteritis (AGE), and an acute febrile illness (AFI)) 23 (2.9 %).
Perinatal Outcomes
Out of the total births, 565 (72.5 %) had favorable perinatal outcomes, 84 (10.8 %) had a perinatal mortality outcome, and 130 (16.7 %) had perinatal morbidity. Overall, the magnitude of adverse perinatal outcomes (mortality and morbidity) was 214 (27.5 %).
Perinatal Morbidity Outcomes
The commonest causes of morbidity were preterm delivery, which affected 114 (14.5 %) neonates, low birth weight 120 (15.3 %), low Apgar score 92 (11.7 %), and congenital anomalies 12 (1.5%).
Perinatal Mortality Outcome
The total number of perinatal deaths was 84 (10.8 %, 95 % CI: 8.9-13.2), and out of this 63 (8.1 %) were stillbirth and 21 (2.7 %) early neonatal loss. Reasons for perinatal mortality in the hospital were: low Apgar score, which affected 73 (86.9 %) neonates, prematurity 42 (50.0 %), low birth weight 38 (45.2 %), early onset of neonatal sepsis 7 (8.3 %), asphyxia 2 (2.4 %), meconium aspiration syndrome 3 (3.6 %), and others 4 (4.8 %) (Figure 2).
Figure 2.
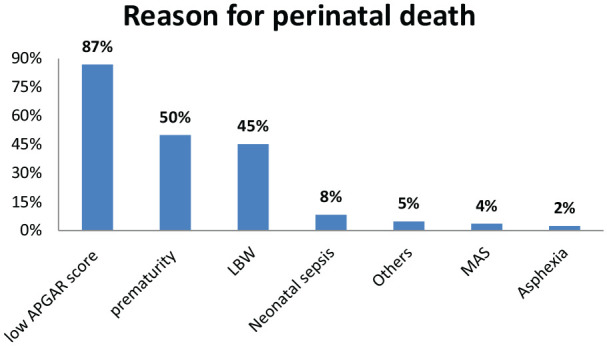
Reasons for perinatal mortality in THMH from September 2015 to August 2016.
Determinants of Perinatal Outcomes
In the bivariable multinomial logistic regression model residence, antenatal attendance, parity, history of modern contraceptive use, poor obstetric history, the status of labor, mal-presentation, mode of delivery, medical illness, and obstetrics complication were fitted. Factors that had a P-value of ≤ 0.20 on crude analysis and variables with well-known clinical significance with perinatal outcomes were fitted into the final model of multivariable multinomial logistic regression (Table 2).
Table 2.
Multinomial Logistic Regression for Factors Associated with Perinatal Outcomes in Waghimra Zone Tefera Hailu Memorial Hospital from September 2015 to August 2016 (n = 779).
| Variable | Perinatal outcomes | ||||
|---|---|---|---|---|---|
| Favorable | Mortality | ||||
| COR 95% CI | AOR 95% CI | COR 95% CI | AOR 95% CI | ||
| Residence | Urban | 1.9 (1.3-2.8) | 1.9 (1.1-2.9)** | 0.3 (0.2-0.6) | 0.5 (0.3-1.1) |
| Rural | 1 | 1 | 1 | 1 | |
| ANC attendance | Yes | 1.4 (0.8-1.9) | 0.9 (0.5-1.4) | 0.3 (0.2-0.5)* | 0.4 (0.2-0.8)** |
| No | 1 | 1 | 1 | 1 | |
| Parity | Primi | 0.8 (0.6-1.3) | 0.8 (0.5-1.2) | 0.5 (0.3-0.9)* | 0.5 (0.3-0.9)** |
| Multi | 1 | 1 | 1 | 1 | |
| Poor obstetric history | Yes | 1.0 (0.6-1.8) | 0.9 (0.5-1.7) | 1.4 (0.7-2.9) | 0.8 (0.3-1.8) |
| No | 1 | 1 | 1 | 1 | |
| Contraceptive use | Yes | 1.9 (1.2-2.8) | 1.7 (1.1-2.7)** | 0.7 (0.4-1.3) | 1.2 (0.6-2.5) |
| No | 1 | 1 | 1 | 1 | |
| Mode of delivery | Operative | 1.2 (0.7-1.9) | 1.6 (0.9-2.8) | 2.3 (1.2-4.4)* | 1.4 (0.7-3.0) |
| SVD | 1 | 1 | 1 | 1 | |
| Status of labor/delivery | Induced/augmented | 0.6 (0.3-1.5) | 0.7 (0.3-1.7) | 3.6 (1.5-8.8) | 3.0 (1.2-7.8) |
| Spontaneous | 1 | 1 | 1 | 1 | |
| Mal-presentation | Yes | 0.8 (0.3-1.9) | 0.6 (0.2-1.6) | 3.5 (1.4-9.1) | 2.5 (0.8-7.5) |
| No | 1 | 1 | 1 | 1 | |
| Medical disorder | Yes | 0.6 (0.4-1.0) | 0.5 (0.3-0.8) | 0.6 (0.2-1.3) | 0.6 (0.2-1.4) |
| No | 1 | 1 | 1 | 1 | |
| Obstetrics complication | Yes | 0.3 (1.3-0.5) | 0.4 (0.2-0.8) | 2.3 (1.2-4.5) | 2.2 (1.1-4.5)** |
| No | 1 | 1 | 1 | 1 | |
Reference category is morbidity outcome. **P-value of <.05.
The multivariable analysis using multinomial logistic regression showed the following findings.
Compared to neonates born to mothers from rural settings, neonates born to mothers from urban settings were 1.9 times more likely to have a favorable outcome than morbidity outcomes (AOR = 1.9, 95 % CI, 1.1-2.9). Compared to mothers who had not used modern contraceptives, neonates born to mothers who had used modern contraceptives were 1.7 times more likely to have a favorable outcome than morbidity outcomes (AOR = 1.7, 95% CI: 1.1-2.7). Neonates born from mothers who had a history of medical illness compared to mothers who had no medical illness were 50 % less likely to have a favorable outcome than morbidity outcomes (AOR = 0.5, 95% CI: 0.3-0.8). Neonates born from mothers with obstetric complications compared to neonates born from mothers without obstetric complications were 60 % less likely to have a favorable outcome than morbidity outcomes (AOR = 0.4, 95% CI: 0.2-0.8).
Neonates born from mothers who had ANC attendance compared to mothers who did not have ANC attendance were 60% less likely to have mortality outcomes than morbidity outcomes (AOR = 0.4, 95% CI: 0.2-0.8). Neonates born from primigravida mothers compared to multi-gravida mothers were 50 % less likely to have mortality outcomes than morbidity outcomes (AOR =0.5, 95% CI: 0.3-0.9). As compare to neonates born from mothers whose labor was spontaneous, neonates born from mothers who had labor induction or augmentation by oxytocin were 3 times (AOR = 3.0, 95% CI: 1.2-7.8) more likely to have mortality outcome than morbidity outcomes. Neonates born from mothers with obstetric complications compared to neonates born from mothers without obstetric complications were 2.2 times more likely to have mortality outcomes than morbidity outcomes (AOR = 2.2, 95% CI: 1.1-4.5).
Discussion
This study was conducted to assess the magnitude and factors affecting perinatal outcomes at Tefera Hailu Memorial hospital. The magnitude of the perinatal mortality rate in this study was 10.8% (95% CI: 8.9-13.2). It is consistent with the findings from a systemic review done on 16 hospitals in Ethiopia,14 and other studies done in Tanzania,16 and Jimma, western Ethiopia.15 However, it is higher than a study done in the North East of Iran.17 This could be explained by a difference in the socio-demographic and economic condition of the study participants. Tefera Hailu Memorial Hospital is the only hospital in the zone that gives comprehensive obstetrics care and each Woreda in the Zone has a poor infrastructure for transportation.
The magnitude of perinatal morbidity in this study was 16.7%. This is consistent with a study done in Holland.18 However, it is lower than a study done in Australia.19 This could be explained by the socioeconomic difference between the settings.
According to the multivariable analysis using multinomial logistic regression, neonates whose mothers were urban residence were 90% more likely to have a favorable outcome than morbidity outcomes compared to neonates whose mothers were rural residence. This is consistent with studies done in Canada.20-22 This is because urban mothers have better educational status and access to health facilities. They are more likely able to reach health facilities before complications happen. Moreover, urban women have a very limited problem with transportation to health facilities which could avoid delays in accessing medical care.
Neonates born to mothers who had ANC attendance compared to mothers who did not have ANC attendance were 60% less likely to have mortality outcomes than morbidity outcomes. It is consistent with studies done in Zimbabwe,23 Ethiopia,24 and the United States of America.25 As it is known that when mothers have ANC, they get an adequate evaluation and health-related problems can be detected early. Also, they discuss their birth plan with health care providers during their ANC and they could plan to have facility delivery and would go to a health facility when their labor starts. Therefore, they are less likely to delay and to be victims of poor birth outcomes.
Neonates born to primigravida mothers compared to multi-gravida mothers were 50% less likely to have mortality outcomes than morbidity outcomes. This is consistent with a study done in Uganda.26 When parity increases, the risk of developing obstetric complications increases.27 Besides, multi-gravida women are most of the time older and are at a greater risk of obstetric complications.26,28,29
Compared to mothers who had not used modern contraceptives, neonates born from mothers who had used modern contraceptives were 70% more likely to have a favorable outcome than morbidity outcomes. This is consistent with a study done in the United States.30 Women who use modern contraceptives have better knowledge and they are more likely to have a planned pregnancy. Moreover, mothers could have a better health condition due to the planned pregnancy and that would help them to have a healthier outcome.31,32
Neonates born to mothers whose labor was either induced or augmented by oxytocin compared to mothers whose labor was spontaneous were 3 times more likely to have mortality outcomes than morbidity outcomes. Women could have augmentation by oxytocin following a uterine atonia that can happen due to different reasons. When women have power failure especially after the fetus is engaged, it could prolong the labor and make the fetus asphyxiated and exacerbate the adverse birth outcomes among newborns.33-35 Also, women are going to have other alternative management following their power failure, and the alternatives could be surgical or instrumental delivery or augmenting the labor by oxytocin. These alternatives have their effect in altering the birth outcomes.
Neonates born to mothers who had a history of medical illness compared to mothers who had no medical illness were 50% less likely to have a favorable outcome than morbidity outcomes. Understandably, maternal illness is a risk factor for adverse birth outcomes.35 When a mother has an illness, that could affect the physiology of mothers during labor, and also the disease might be transmitted to the newborn and worsen his/her condition.
Neonates born to mothers with obstetric complications compared to neonates born to mothers without obstetric complications were 2.2 times more likely to have mortality outcomes than morbidity outcomes. Neonates born to mothers with obstetric complications compared to neonates born to mothers without obstetric complications were 60% less likely to have a favorable outcome than morbidity outcomes. This is consistent with studies done in Kenya, Tanzania, and Norway.27,35,36 Mothers who have obstetric complications are at risk of having poor birth outcomes and the complications would lead the newborns to have bad outcomes.
This study can be used as a baseline for other researchers and will be a source of information for planning and decision-making. However, mothers who live in the rural part of the study area are mostly giving birth at home and the findings of this study might not represent women who deliver in the community. Since we used secondary data, the result might be affected by some incomplete records.
Conclusions
The magnitude of adverse perinatal outcomes in the study area was considerable. The commonest determinants of poor perinatal outcomes were low birth weight and prematurity. Urban residence, ANC, parity, and modern contraceptive use had a protective effect on perinatal mortality while labor induction/augmentation, medical illness, and obstetric complications were risk factors of adverse perinatal outcomes. Increasing modern family planning service utilization, encouraging antenatal care follow-up service; identifying and referring clients with medical illness and obstetrics complications early is strongly recommended.
Acknowledgments
First and foremost we are very much thankful to the Ethiopian Public Health Association for supporting and facilitating the data collection process. Also, we would like to thank the data collectors and staff of Tefera Hailu Memorial Hospital for their support during data collection.
Footnotes
Abbreviations: AOR: adjusted odds ratio; COR: crude odds ratio; CSA: central statistical agency; CI: confidence interval; EDHS: Ethiopian Demographic and Health Survey; SD: Standard deviation; WHO: World Health Organization.
Authors’ Contributions: ES initiated the research. ES, SB, AB, and AT contributed to the proposal writing, data entry, and analysis. SB drafted the manuscript and all the other authors read and approved the final version of the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Ethical approval was obtained from an institutional review board of the Ethiopian Public Health Association. Additionally, a letter of permission was obtained from Tefera Hailu Memorial Hospital. Since patient records were reviewed, informed consent was waived. Names of patients were not recorded, and the information gathered was not accessible to anyone except the principal investigator and was kept locked and protected by a password.
ORCID iD: Simon Birhanu  https://orcid.org/0000-0002-7852-5902
https://orcid.org/0000-0002-7852-5902
Availability of Data and Materials: All data generated or analyzed during this study are included in this manuscript.
References
- 1. World Health Organization. Neonatal and perinatal mortality Country, Regional and Global Estimates. 2007. Accessed December 30, 2020. https://apps.who.int/iris/handle/10665/43444
- 2. Central Statistical Agency. Ethiopia demographic and health survey. 2016. Accessed December 30, 2020. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf
- 3. Kebede B, Gebeyehu A, Sharma HR, Yifru S. Prevalence and associated factors of neonatal mortality in North Gondar Zone, Northwest Ethiopia. Ethiop Jhealth Dev. 2012;26:66-71. [Google Scholar]
- 4. Kliegman RM, Behrman RE, Jenson HB, et al. Overview of mortality and morbidity. Nelson Textbook of Pediatrics. 18th ed. Saunders and Elsevier; 2007. [Google Scholar]
- 5. Yakoob MY, Ali MA, Ali MU. The effect of providing stillbirth attendance and emergency obstetrics care in preventing stillbirth. BMC Public Health. 2011;11:S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. El-Mowafi D. High risk pregnancy In: EI-Mowafi DM, ed. Obstetrics Simplified, 1st ed. Egypt: Burg Abu-Samra, El-Happy Land Square; 1997. [Google Scholar]
- 7. Corton MM, Gary Cunningham F, Leveno KJ, et al. Preterm birth. Williams’s Obstetrics, 23rd ed. New York, USA: McGraw-Hill Professional Publishing; 2005. [Google Scholar]
- 8. Keirse MJ, Rush RW, Howat P, et al. Contribution of preterm delivery to perinatal mortality. Br Med J 1976;2:965-968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yirgu R, Molla M, Sibley L, et al. Perinatal mortality, magnitude, determinant and cause in west Gojam: Population-based nest case control study. PLoS One. 2016;11:e0159390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Malewzi KJ, Muluzi KT, Chihana BH. Factors responsible for perinatal mortality in womans giving birth in health facility. Afr J Nurs Midewifery 2015;2:121-130. [Google Scholar]
- 11. Gaym A. Perinatal mortality audit. Ethiop J Health Dev. 2000;14(3):335-343. [Google Scholar]
- 12. World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. 2016. ISBN 978 92 4 154991 2. Accessed January 2, 2021. https://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf [PubMed]
- 13. Lincetto O, Mothebesoane-Anoh S, Gomez P, et al. Opportunities for Africa’s Newborns. Antenatal care. 2012. Published 2006. Accessed January 2, 2021. www.who.int/entity/pmnch/media/publications/aonsectionIII_2.pdf
- 14. Berhan Y, Berhan A. Perinatal mortality trend in Ethiopia. Ethiop J Health Sci. 2014;29:29-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yesuf A. Perinatal mortality and associated factor. Gynecol Obstet. 2016;6:409. doi: 10.4172/2161-0932.1000409 [DOI] [Google Scholar]
- 16. Schmiegelow C, Minja D, Oesterholt M, et al. Factors associated with and causes of perinatal mortality in northeastern Tanzania. Acta Obstet Gynecol Scand. 2012;91:1061-1068. [DOI] [PubMed] [Google Scholar]
- 17. Ghorat F, Ghafarzadeh R, Esfehani RJ. Perinatal mortality and its associated factors. Iran J Neonatol. 2016;7(1): 47-51. doi: 10.22038/ijn.2016.6665 [DOI] [Google Scholar]
- 18. Vos AA, Denktaş S, Borsboom GJ, Bonsel GJ, Steegers EA. Differences in perinatal morbidity and mortality on the neighbourhood level in Dutch municipalities: a population based cohort study. BMC Pregn Childbirth. 2015;15:201. doi: 10.1186/s12884-015-0628-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Morris JM, Totterdell J, Bin YS, Ford JB, Roberts CL. Contribution of maternal age, medical and obstetric history to maternal and perinatal morbidity/mortality for women aged 35 or older. Aust N Z J Obstet Gynaecol. 2018;58:91-97. doi: 10.1111/ajo.12674 [DOI] [PubMed] [Google Scholar]
- 20. Lisonkova S, Haslam MD, Dahlgren L, Chen I, Synnes AR, Lim KI. Maternal morbidity and perinatal outcomes among women in rural versus urban areas. CMAJ. 2016;188:E456-E465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shankardass K, O’Campo P, Dodds L, et al. Magnitude of income-related disparities in adverse perinatal outcomes. BMC Pregn Childbirth. 2014;14:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lisonkova S, Sheps SB, Janssen PA, Lee SK, Dahlgren L, Macnab YC. Birth outcomes among older mothers in rural versus urban areas: a residence-based approach. J Rural Health. 2011;27:211-219. [DOI] [PubMed] [Google Scholar]
- 23. Feresu SA, Harlow SD, Welch K, Gillespie BW. Incidence of stillbirth and perinatal mortality and their associated factors among women delivering at Harare Maternity Hospital, Zimbabwe: a cross-sectional retrospective analysis. BMC Pregn Childbirth. 2005;5:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Worku AG, Yalew AW, Afework MF. The contributions of maternity care to reducing adverse pregnancy outcomes: a Cohort study in Dabat district, Northwest Ethiopia. Matern Child Health J. 2014;18:1336-1344. [DOI] [PubMed] [Google Scholar]
- 25. Partridge S, Abenhaim HA, Balayla J, Holcroft CA. Inadequate prenatal care utilization and risks of infant mortality and poor birth outcome: a retrospective analysis of 28,729,76 5U.S. deliveries over 8 years. Am J Perinatol. 2012;29:787-794. [DOI] [PubMed] [Google Scholar]
- 26. Kujala S, Waiswa P, Kadobera D, Akuze J, Pariyo G, Hanson C. Trends and risk factors of stillbirths and neonatal deaths in Eastern Uganda (1982–2011): a cross-sectional, population-based study. Trop Med Int Health. 2017;22:63-73. [DOI] [PubMed] [Google Scholar]
- 27. Linde LE, Rasmussen S, Kessler J, Ebbing C. Extreme umbilical cord lengths, cord knot and entanglement: risk factors and risk of adverse outcomes, a population-based study. PLoS One. 2018;13:e0194814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lisonkova S, Potts J, Muraca GM, et al. Maternal age and severe maternal morbidity: a population-based retrospective cohort study. PLoS Med. 2017;14: e1002307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ogawa K, Urayama KY, Tanigaki S, et al. Association between very advanced maternal age and adverse pregnancy outcomes: a cross sectional Japanese study. BMC Pregn Childbirth. 2017;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Goldthwaite LM, Duca L, Johnson RK, Ostendorf D, Sheeder J. Adverse birth outcomes in Colorado: assessing the impact of a statewide initiative to prevent unintended pregnancy. Am J Public Health. 2015;105:e60-e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sutton MY, Zhou W, Frazier EL. Unplanned pregnancies and contraceptive use among HIV- positive women in care. PLoS One. 2018;13:e0197216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Engjom HM, Morken N-H, Høydahl E, Norheim OF, Klungsøyr K. Increased risk of peripartum perinatal mortality in unplanned births outside an institution: a retrospective population-based study. Am J Obstet Gynecol. 2017;217:210.e1-210.e12. [DOI] [PubMed] [Google Scholar]
- 33. Laughon SK, Berghella V, Reddy UM, Sundaram R, Lu Z, Hoffman MK. Neonatal and maternal outcomes with prolonged second stage of labor. Obstet Gynecol. 2014;124:57-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bayou G, Berhan Y. Perinatal mortality and associated risk factors: a case control study. Ethiop J Health Sci. 2012;22:153-62. [PMC free article] [PubMed] [Google Scholar]
- 35. Mmbaga BT, Lie RT, Olomi R, Mahande MJ, Olola O, Daltveit AK. Causes of perinatal death at a tertiary care hospital in Northern Tanzania 2000–2010: a registry based study. BMC Pregn Childbirth. 2012;12:139. doi: 10.1186/1471-2393-12-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Weiner R, Ronsmans C, Dorman E, Jilo H, Muhoro A, Shulman C. Labor complications remain the most important risk factors for perinatal mortality in rural Kenya. Bull World Health Organ. 2003;81:561-566. [PMC free article] [PubMed] [Google Scholar]


