Abstract
The Covid-19 pandemic has exposed the difficulty of the US public health system to respond effectively to vulnerable subpopulations, causing disproportionate rates of morbidity and mortality. New York Haredi-Orthodox Jewish communities represent a group that have been heavily impacted by Covid-19. Little research has examined their experience or perceptions toward Covid-19 and vaccines. We conducted a cross-sectional, observational study to explore the experience of Covid-19 among Haredim. Paper surveys were self-administered between December 2020 and January 2021 in Haredi neighborhood pediatricians’ offices in Brooklyn, New York. Of 102 respondents, 43% reported either a positive SARS-CoV-2 viral or antibody test. Participants trusted their physicians, Orthodox medical organizations, and rabbinic leaders for medical information. Knowledge of Covid-19 transmission and risk was good (69% answered ≥ 4/6 questions correctly). Only 12% of respondents would accept a Covid-19 vaccine, 41% were undecided and 47% were strongly hesitant. Independent predictors of strong vaccine hesitancy included believing natural infection to be better than vaccination for developing immunity (adjusted odds ratio [aOR] 4.28; 95% confidence interval [CI] 1.23–14.86), agreement that prior infection provides a path toward resuming communal life (aOR 4.10; 95% CI 1.22–13.77), and pandemic-related loss of trust in physicians (aOR 5.01; 95% CI 1.05–23.96). The primary disseminators of health information for self-protective religious communities should be stakeholders who understand these groups' unique health needs. In communities with significant Covid-19 experience, vaccination messaging may need to be tailored toward protecting infection-naïve individuals and boosting natural immunity against emerging variants.
Keywords: COVID-19, Vaccine hesitancy, Orthodox Jewish, Survey
Introduction
Coronavirus Disease-19 (Covid-19) has disproportionately affected communities with socioeconomic and political deprivation in the United States (US), bringing health care disparities into sharp relief. It has highlighted vulnerabilities in groups with complex tensions with the state, public health authorities, and medical establishment, such as undocumented immigrants, Black Americans, Native Americans, rural Americans and prisoners [1–5]. At a fundamental level, the pandemic has exposed the failure of the public health system to respond effectively in localized contexts and sufficiently safeguard vast segments of our population.
Orthodox Jewish communities have been disproportionately impacted by Covid-19. In the US, an Orthodox Jewish community in Westchester County and the Bronx, New York was the first to experience state-mandated quarantine [6]. In a multicity seroprevalence study among Orthodox communities, over 30% of individuals had SARS-CoV-2 antibodies after the first Covid-19 wave in New York [7]. Covid-19 has particularly affected Hasidic and Litvish groups collectively known as Haredim, who live in close-knit communities and are less engaged with secular traditions than Modern Orthodox and other forms of Judaism. In early summer 2020, seropositivity rates at clinics serving Hasidic patients in Brooklyn were reported as between 40 and 60%, approaching 75% among men aged 18–34 [8]. In January 2021, self-reported prior infection was 57% among 91 Hasidic respondents in a national internet-based survey [9]. In that survey, approximately 85% of Haredi respondents personally knew someone who had died of Covid-19. Though the New York City Department of Health does not publicly report data on SARS-CoV-2 by religion, the seroprevalence rate in the largest Haredi neighborhood in Brooklyn, Boro Park, exceeded 45% in February 2021, the city’s second highest seroprevalence neighborhood [10].
Foreshadowing Covid-19’s devastating effect on the New York Haredi community, a measles outbreak occurred within Hasidic groups in the greater New York City area in 2018–2019. 93% percent of the measles cases during that outbreak were in the Orthodox Jewish community and 72% occurred within one Hasidic-predominant neighborhood of Brooklyn [11]. Of the cases for whom vaccination history was known, 85.8% were unvaccinated. To increase vaccination rates in these pockets, New York City government officials took actions that the Haredim experienced as curtailing individual liberties and threatening the integrity of the affected community. Unvaccinated children were banned from public places, including places of worship and schools. Schools that permitted entry of unvaccinated students were temporarily closed, and violations and fines were issued to those noncompliant with vaccination [12]. Though partnerships were formed between the local department of health and community stakeholders to enhance mutual understanding, the speed and ferocity with which Covid-19 took hold of Haredi communities less than a year later outpaced the public health response.
The significant impact of Covid-19 in Haredi-Orthodox Jewish areas has been attributed to high population density with large households and the maintenance of a highly communal lifestyle involving group prayer, learning and celebrations. Among the Haredim, extended families gather weekly to share meals at the Sabbath, men are obligated to pray in groups at synagogue three times daily, and children are schooled in-person given the paramount importance of student-educator and peer relationships in Torah education [13]. Despite Covid-19’s impact, little formal research has been conducted to elucidate how the Haredim perceive and negotiate the pandemic. Illuminating how these communities understand and prioritize Covid-19 can assist in the creation of sensitive recommendations that support community relationships with the public health establishment.
We conducted an observational study with a scored, closed-ended question survey within two primarily Hasidic neighborhoods in Brooklyn to explore responses of Haredi individuals to the Covid-19 pandemic and vaccines. We report on participants' personal experiences of Covid-19, knowledge about Covid-19 transmission and risk, sources of medical information, and perceptions surrounding Covid-19 and vaccines.
Methods
Study Oversight
The study protocol was approved by the NYU Langone Health Institutional Review Board. Before inclusion, those eligible were given the opportunity to review key study information and verbally consent prior to participating.
Study Design
This was a cross-sectional study design involving analysis of questionnaire data. We distributed paper quantitative surveys between December 7, 2020 and January 20, 2021 to a convenience sample of 100 Haredi individuals in the waiting rooms of physicians’ offices in predominantly Hasidic neighborhoods in Brooklyn, New York. All individuals in the waiting rooms on the dates of study who were 18 years or older who spoke and read English and identified as Haredi/Orthodox were eligible to participate.
Survey
The scored, closed-ended questionnaire had three components: an initial section characterizing participants and their personal experiences with Covid-19, a section examining what sources of information participants use and trust to learn about Covid-19, and a final section on knowledge, attitudes and practices. We assessed participants’ knowledge of Covid-19 transmission and vulnerability, attitudes regarding Covid-19 risk, immunity, vaccines and health authorities, and practices surrounding Covid-19 risk mitigation. The survey was distributed in English and developed with recommendations from Haredi individuals, physicians who work in the surveyed communities, and were shaped in part by Covid-19 vaccine hesitancy themes trending in 2020 [14]. The primary endpoints reported were, for knowledge, the proportion of answers in line with current understanding about Covid-19 and, for attitudes, Likert scores to direct questions.
Study Procedures
Potential participants were offered a key information form to gauge interest in study participation. If they expressed interest, eligibility was verified, and verbal consent obtained. Surveys were participant-administered. Participants were considered enrolled after filling out any portion of the survey.
Statistical Analysis
We used descriptive statistics to summarize respondent characteristics. Missing data did not invalidate participants’ remaining responses. Analysis was adjusted for number of missing responses, except for the knowledge section, where missing responses were classified as incorrect if at least one question in the section was answered.
Descriptive data was expressed as mean ± standard deviation for continuous data, median and interquartile range for ordinal data, and frequency and percentages for categorical data. Five-point Likert scales were reported as frequencies with percent for each answer-type on the scale. We tested associations between different demographic, knowledge and attitudes variables using chi-squared tests. Likert responses were dichotomized between “agree and strongly agree” and “neutral, disagree or strongly disagree” to all questions except for Covid-19 vaccine hesitancy, where the neutral category was grouped with those who agreed or strongly agreed that they would receive the vaccine. If p was less than 0.05 on chi-squared tests of association, we performed multiple logistic regression with forward selection to quantify independent associations with adjusted odds ratios (aOR). We conducted quantitative data analysis using SPSS, version 25. Statistical significance was set at alpha = 0.05.
Results
A total of 102 surveys were collected. Demographic characteristics and personal experience with Covid-19 are shown in Table 1. Participants were representative of the clientele of selected practices, primarily women of child-bearing age who were bringing a child for a pediatrician visit. Most lived in nuclear families with a spouse and 2–6 children, and very few lived with older adults. 43% had either a positive SARS-CoV-2 viral or antibody test. A significant percentage of respondents (8%) had an immediate family member who died of Covid-19.
Table 1.
Characteristics of participants
| Survey location (N = 102) | |
| Boro Park—no. (%) | 95 (93) |
| Williamsburg—no. (%) | 7 (7) |
| Gender (N = 101) | |
| Female—no. (%) | 88 (87) |
| Male—no. (%) | 13 (13) |
| Median Age (IQR)—year (N = 101) | 32 (25–38) |
| Neighborhood of Residence (N = 101) | |
| Williamsburg—no. (%) | 7 (7) |
| Boro Park—no. (%) | 75 (74) |
| Midwood—no. (%) | 14 (14) |
| Monsey/New Square—no. (%) | 2 (2) |
| Other—no. (%) | 3 (3) |
| Median Number of Household Members (IQR) | 6 (4–8) |
| Median Number of Household Children (IQR) | 4 (2–5.5) |
| Median Number of Household Adults > 65 (IQR) | 0 (0–0) |
| SARS-CoV-2 PCR Positive—no. (%) (N = 102) | 16 (16) |
| SARS-CoV-2 Antibody Positive—no. (%) (N = 93) | 41 (44) |
| Median Household Members Who Were Lab Covid-19 Positive for Households that Reported > 0 cases (N = 41) | 2 (1–3) |
| Participant or Immediate Family Member was Hospitalized with Covid-19—no. (%) (N = 96) | 8 (8) |
| Immediate Family Member Died of Covid-19—no. (%) (N = 99) | 8 (8) |
| Participant or Someone Close to Them Donated Covid-19 Plasma—no. (%) (N = 96) | 12 (13) |
Sources of Information
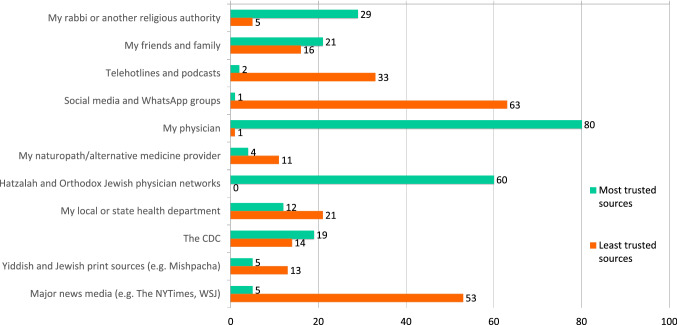
Participants reported obtaining information on Covid-19 from a diversity of sources, with in-person interactions (48%), social media/websites (47%) and person-to-person texts, calls and video chat (34%), being the most common. Figure 1 depicts participants’ most and least trusted sources of medical information. Most trusted sources were personal physicians, Orthodox medical organizations and rabbinic leaders. Government sources were seldom trusted. One in five participants considered their local or state health department among the least trusted sources of medical information. Respondents demonstrated a significant skepticism toward social media and major secular news media as outlets for medical information.
Fig. 1.
Most trusted and least trusted sources of medical information (number of responses, participants selected up to three for each)
Knowledge
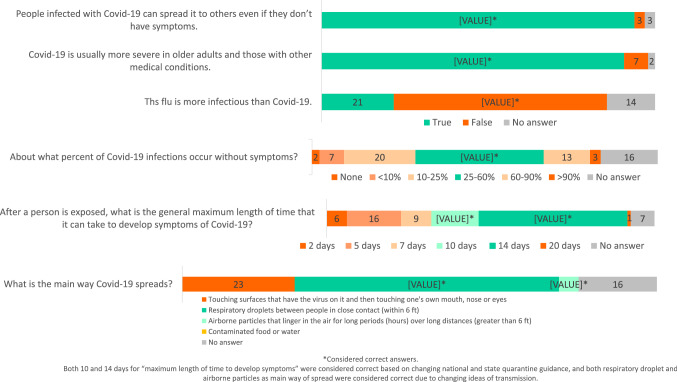
Figure 2 shows the responses and percent correct to survey questions about Covid-19 transmission and risk. The mean score was 4.05 of 6 questions correct (SD 1.28). Of respondents, 69% answered ≥ 4 questions correctly, which we defined as “good” knowledge of Covid-19 transmission and risk. A substantial percentage of participants (28.4% of respondents) incorrectly answered that the main mechanism of Covid-19 transmission was through touching surfaces and then touching mucous membranes, likely reflecting the confusion early in the pandemic around the role of surfaces in transmission.
Fig. 2.
Knowledge of Covid-19: transmission and risk (N = 97)
There was no significant association observed between gender, age, survey location, neighborhood of residence, or history of Covid-19 with level of knowledge. However, data suggested that women had higher odds of possessing a “good” knowledge level (≥ 4 questions correctly) than men in the multivariate model (odds ratio [OR] 3.6), though the confidence interval included 1 (95% confidence interval [CI] 0.986–13.1; p = 0.053). When attitudes were examined in a regression model as predictors of knowledge, those who believed that routine vaccines were essential and those who had not lost trust in physicians had higher odds of possessing “good” knowledge about Covid-19 transmission (aOR 5.74; CI 1.57–20.92 and aOR 6.34; CI 1.45–27.7, respectively).
Attitudes
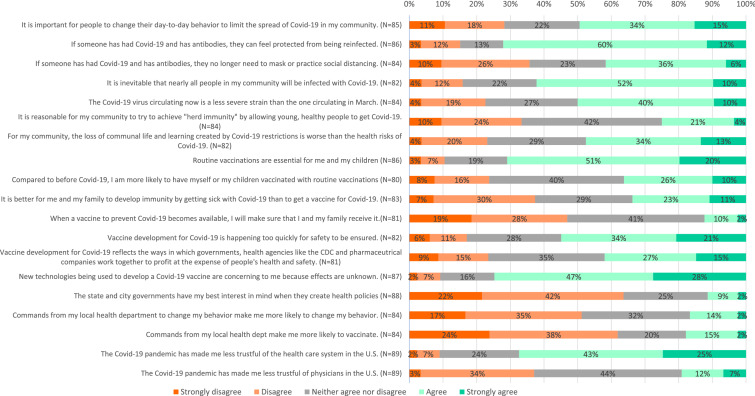
Figure 3 displays the responses to questions assessing perceptions of Covid-19 risk mitigation, immunity, Covid-19 vaccine acceptability, routine vaccination acceptability and trust in government and the health care system. 50% of participants agreed that it was important to modify behavior to limit spread of Covid-19 in their community, approximately 25% felt neutral, and 25% disagreed. Nearly 75% of respondents felt that Covid-19 antibodies were protective against re-infection. 62% agreed that it was inevitable and another 22% did not disagree that nearly all people in the community would be infected. There was no consensus on whether it was reasonable for the community to achieve herd immunity by allowing young, healthy people to get Covid-19. For half, the loss of communal life and learning created by Covid-19 restrictions was perceived as worse than the health risks of Covid-19.
Fig. 3.
Perceptions of Covid-19, routine vaccines and Covid-19 vaccines (percent responses)
Only 12% of respondents would accept a Covid-19 vaccine for themselves and their family, but a substantial percentage were undecided (41%) at this early phase of vaccine distribution. A much higher percentage (70%) agreed that routine vaccinations were essential. Though most were not swayed, 36% responded that they were more likely to obtain routine vaccination for themselves or their children compared to before Covid-19. Apprehension about new vaccine technology was the most prevalent concern about the Covid-19 vaccines. Respondents indicated a lack of confidence in local and state governments and health officials, and very few agreed that mandates from the local health department would make them change their behavior (16%) or vaccinate (17%). The majority had lost trust in the health care system in the US during the Covid-19 pandemic. This loss of trust extended to a lesser degree to physicians.
To examine predictors of Covid-19 vaccine hesitancy vs favorability, responses to the question “When a vaccine to prevent Covid-19 becomes available, I will make sure that I and my family receive it” were dichotomized. Those who disagreed or strongly disagreed were considered “strongly hesitant” and those who neither agreed nor disagreed, agreed, or strongly agreed were considered “more accepting.” There was no significant association observed between gender, age, survey location, neighborhood of residence, personal history of Covid-19 or level of knowledge and Covid-19 vaccine hesitancy. Table 2 displays the significant univariate associations between attitudes and vaccine hesitancy. In a logistic regression model including attitudes associated with Covid-19 vaccine hesitancy, sentiments that remained independent predictors of strong Covid-19 vaccine hesitancy were: the feeling that natural infection was better than vaccine for developing immunity (aOR 4.28, 95% CI 1.23–14.86), agreement that prior Covid-19 with antibodies obviates need to mask or practice social distancing (aOR 4.1, 95% CI 1.22–13.77), and loss of trust in US physicians resulting from the pandemic (aOR 5.01, 95% CI 1.05–23.96).
Table 2.
Attitudes associated with strong vaccine hesitancy
| No plans to receive Covid-19 vaccinea | Univariate Odds Ratio (95% Confidence Interval) | P value | Adjusted Odds Ratio (95% Confidence Interval) | P value |
|---|---|---|---|---|
| If someone has had Covid-19 and has antibodies, they no longer need to mask or practice social distancing | 5.84 (2.16–15.78) | < 0.001 | 4.10 (1.22–13.77) | .022 |
| Covid strain circulating now is less severe than the one circulating in March | 2.67 (1.07–6.64) | 0.033 | ||
| For my community, the loss of communal life and learning created by Covid-19 restrictions is worse than the health risks of Covid-19 | 3.68 (1.42–9.49) | 0.006 | ||
| It is better for me and my family to develop immunity by getting sick with Covid-19 than to get a vaccine for Covid-19 | 8.25 (2.81–24.24) | < 0.001 | 4.28 (1.23–14.86) | .022 |
| Vaccine development for Covid-19 is happening too quickly for safety to be ensured | 3.75 (1.48–9.52) | 0.004 | ||
| Vaccine development for Covid-19 reflects the ways in which governments, health agencies like the CDC and pharmaceutical companies work together to profit at the expense of people’s health and safety | 3.17 (1.24–8.09) | 0.014 | ||
| New technologies being used to develop a Covid-19 vaccine are concerning to me because their effects are unknown | 6.61 (1.73–25.28) | 0.003 | ||
| Commands from my local health department to have myself or my children vaccinated make me more likely to vaccinate | 0 (0.0-undefined) | < 0.001 | ||
| The Covid-19 pandemic has made me less trustful of physicians in the US | 4.35 (1.24–15.25) | 0.016 | 5.01 (1.05–23.96) | .044 |
aInput variables for logistic regression model consist of all those in table above other than “commands from my local health department to have myself or my children vaccinate make me more likely to vaccinate” based on non-computable odds ratio for this variable since one cell contained “0” value. Computed final model included those variables with adjusted odds ratios presented above
The bold values have the significance listed as the P value in the last column
Discussion
To our knowledge, this is the first peer-reviewed report examining perceptions toward Covid-19 and vaccines in individuals from Haredi communities in the US. Our findings among a sample of mainly younger, adult women in two Hasidic-predominant neighborhoods of Brooklyn reveal a community deeply impacted by Covid-19, both in terms of overall seropositivity and significant proportion of deaths among immediate family members. When seeking medical information, participants turn toward physicians, Orthodox Jewish medical groups and religious leaders that understand their community’s cultural cues. Few participants trusted mainstream media, most lacked confidence in government institutions and lost trust in the US medical system because of the pandemic. Most were wary about Covid-19 vaccines. Decisions around Covid-19 vaccines hinged on beliefs about the immune protection offered from natural infection and to a less certain degree, trust in physicians over the course of the Covid-19 pandemic.
Our findings of Haredi perceptions of Covid-19 vaccines demonstrated similar, if not more hesitant, views as those found in a national internet-based survey conducted January 2021 among the American Jewish community [9]. In that report, 31% of Hasidic and 53% of Litvish respondents planned to receive or had already received the Covid-19 vaccine. For comparison, in a New York City poll in December 2020, 55% of New York City residents intended to get the vaccine [15]. The significant proportion in our study who were undecided may become more receptive as vaccine experience grows. Overall, 57% of 91 Hasidic and 78% of 265 Litvish respondents in the above cited study held positive vaccine sentiments (in contrast, 93% of Modern Orthodox and 95% of Non-Orthodox held positive vaccine sentiments). When joined together, the proportion of Haredim with positive vaccine sentiments (70%) was quite similar to the percent who viewed routine vaccinations as essential in our study (70%) and of the American population in December 2020 (69%) [16].
The lack of participants’ confidence that local and state governments have their best interests in mind when they create health policies, and the articulated erosion of trust in the health care system demonstrate the failure of the public health establishment to sensitively engage, message and support these communities. The history of Haredi groups in New York has involved friction with state and city health officials, beginning even prior to the measles outbreak and punctuated during Covid-19, where Haredim have felt unfairly singled out and misunderstood. Hypothesizing from our data, when public health restrictions are antithetical to the social fabric of communities, the existential risk to the collective brought forth by restrictions outweighs their proposed public health benefits. This is particularly true when recommendations are put forth by government authorities that provide conflicting guidance amid scientific uncertainty and, as the Haredim perceive, have a limited understanding of their way of life. Individuals make their own calculations based on available, observable information, tolerating these risks because they believe they cannot meaningfully exist otherwise.
Perhaps the most evident incongruity between public health messaging and the Haredi experience of Covid-19 has been that around natural infection and immunity. By prescribing equivalent behaviors and vaccine strategies in those who have had Covid-19 with those who are SARS-CoV-2-naïve, public health messaging effectively equates risk of acquiring disease between these two groups. Members of Haredi communities observed early on that this risk is not equivalent: there is a relative consensus that if people have had Covid-19 and have antibodies, they can feel protected from being reinfected. Emerging evidence supports this perspective of protection after previous SARS-CoV-2 infection. Several large cohort studies have reported that reinfection is rare, and that the risk of reinfection with SARS-CoV-2 is reduced by 80–95% for at least 5–7 months with no signs of waning immunity [17–19], though protection may be less robust in the elderly [20]. There are implications to giving broad instruction to everyone and discounting natural immunity, despite a recognized difference in disease risk. In communities having low confidence in government and public health officials, this uniform messaging may backfire. Messaging on Covid-19 immunity may need to be tailored, validating that people believe and have observed that natural immunity to Covid-19 is usually protective. For example, vaccine messaging could focus on protecting those vulnerable individuals without prior Covid-19 through vaccination, and on “boosting” immunity in the elderly and protecting against emerging variants for those with previous Covid-19. With scientific justification emerging [21–23], studies on whether one dose of mRNA vaccine is sufficiently protective in individuals with prior Covid-19 will be important, as a one-dose boost concept may significantly promote vaccine uptake.
This study has limitations. Nearly all our participants were from one site, and few were men. Because we wished to protect the identity of participants, we did not inquire whether they were Litvish or Hasidic, or if they identified with a particular Hasidic group. Given these features and the small size of our sample, this study is not by any means intended to be representative of the vast diversity of American Haredim. Another limitation was that our sites were physician practices that require vaccination, so we may have overestimated the degree of acceptance of routine vaccines in the wider community. We did not examine some vaccine hesitancy themes around Covid-19 vaccines, particularly misinformation regarding infertility, which grew in circulation in January and February 2021. The limits of our sample size led to wide confidence intervals in our regression analysis.
Despite our small sample, our findings have broad implications. They imply that religiously affiliated stakeholders that understand the unique context of health needs situated within socio-religious obligations should be the primary vehicles for tailoring health information to more insular communities. This finding is supported by previous literature that advocates that religious authorities should be involved in the distribution of health messages to self-protective religious minority groups [24]. The Haredi response to Covid-19 provides an example of how it is critical to understand local context to develop effective interventions within vulnerable communities. Future studies ought to evaluate whether uniform public health strategies are appropriate or if more resources should be put into culturally and demographically specific strategies, particularly in those communities with complex relationships with the state and public health authorities. Resources could be pre-emptively put in place to better study these communities’ dynamic health attitudes and practices to develop more effective public health policies. Qualitative studies are needed to fully understand vaccine hesitancy in various groups. Such studies will enable the medical community to meet the health needs of vulnerable communities during this and future pandemics.
Acknowledgements
Research supported by The Louis and Rachel Rudin Foundation, Inc. Rudin Medical Ethics & Humanities Fellowship at NYU Grossman School of Medicine. The authors would like to thank Israel Zyskind, MD, Moshe Felberbaum and Jacob Levenson for their review of the manuscript, Robert S. Holzman, MD for his review of statistical analyses and all participants for their contribution to the research.
Author Contribution
All authors contributed to study conception and design. Data collection was performed by EC. Data analysis was performed by EC and DZ. Resources were compiled by EK. The first draft of the manuscript was written by EC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The Louis and Rachel Rudin Foundation, Inc. Rudin Medical Ethics & Humanities Fellowship at NYU Grossman School of Medicine.
Data Availability
By request.
Declarations
Ethics Approval
NYU Langone Health Institutional Review Board.
Informed Consent
Verbal consent obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Greenaway C, Hargreaves S, Barkati S, et al. COVID-19: Exposing and addressing health disparities among ethnic minorities and migrants. Journal of Travel Medicine. 2020 doi: 10.1093/jtm/taaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muñoz-Price LS, Nattinger AB, Rivera F, et al. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Network Open. 2020 doi: 10.1001/jamanetworkopen.2020.21892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.IDSA. (2020, July 7). COVID-19 policy brief: Disparities among native American Communities in the United States. Retrieved from https://www.idsociety.org/globalassets/idsa/public-health/covid-19/covid19-health-disparaties-in-native-american-communities-final.pdf
- 4.Mueller JT, McConnell K, Burow PB, Pofahl K, Merdjanoff AA, Farrell J. Impacts of the COVID-19 pandemic on rural America. Proceedings of the National Academy of Sciences. 2021 doi: 10.1073/pnas.2019378118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawks L, Woolhandler S, McCormick D. COVID-19 in prisons and jails in the United States. JAMA Internal Medicine. 2020;180(8):1041–1042. doi: 10.1001/jamainternmed.2020.1856. [DOI] [PubMed] [Google Scholar]
- 6.Weinberger-Litman SL, Litman L, Rosen Z, Rosmarin DH, Rosenzweig C. A look at the first quarantined community in the USA: Response of religious communal organizations and implications for public health during the COVID-19 pandemic. Journal of Religion and Health. 2020;59(5):2269–2282. doi: 10.1007/s10943-020-01064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zyskind I, Rosenberg AZ, Zimmerman J, et al. SARS-CoV-2 seroprevalence and symptom onset in culturally linked orthodox Jewish communities across multiple regions in the United States. JAMA Network Open. 2021;4(3):e212816. doi: 10.1001/jamanetworkopen.2021.2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brooklyn’s Hasidic Jews are acting like they have herd immunity. Could they be right? (2020, July 8). Jewish Telegraphic Agency. Retrieved from https://www.jta.org/2020/07/08/health/brooklyns-hasidic-jews-are-acting-like-they-have-herd-immunity-could-they-be-right
- 9.Social Research | Nishma Research. (n.d.). Retrieved March 17, 2021, from http://www.nishmaresearch.com/social-research.html
- 10.COVID-19: Data Totals - NYC Health. (n.d.). Retrieved March 17, 2021, from https://www1.nyc.gov/site/doh/covid/covid-19-data-totals.page#antibody
- 11.Zucker JR, Rosen JB, Iwamoto M, et al. Consequences of undervaccination—Measles outbreak, New York City, 2018–2019. New England Journal of Medicine. 2020;382(11):1009–1017. doi: 10.1056/NEJMoa1912514. [DOI] [PubMed] [Google Scholar]
- 12.Otterman, S. (2019, September 3). Get vaccinated or leave school: 26,000 N.Y. Children face a choice. The New York Times. Retrieved from https://www.nytimes.com/2019/09/03/nyregion/measles-vaccine-exemptions-ny.html
- 13.Pirutinsky S, Cherniak AD, Rosmarin DH. COVID-19, mental health, and religious coping among American Orthodox Jews. Journal of Religion and Health. 2020;59(5):2288–2301. doi: 10.1007/s10943-020-01070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smyser, J. (2020, August). COVID-19 and vaccine opposition. Presented at the Project VCTR. Retrieved from www.projectvctr.com
- 15.Zucker, J. R. (2021). ABNY COVID vaccine survey. Retrieved from https://abny.org/
- 16.Muñana, C. (2020, December 15). KFF COVID-19 vaccine monitor: December 2020. KFF. Retrieved from https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/
- 17.Hall, V., Foulkes, S., Charlett, A., et al. (2021). Do antibody positive healthcare workers have lower SARS-CoV-2 infection rates than antibody negative healthcare workers? Large multi-Centre prospective cohort study (the SIREN study), England: June to November 2020. medRxiv. 10.1101/2021.01.13.21249642
- 18.Lumley SF, O’Donnell D, Stoesser NE, et al. Antibody status and incidence of SARS-CoV-2 infection in health care workers. New England Journal of Medicine. 2021;384(6):533–540. doi: 10.1056/NEJMoa2034545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abu-Raddad, L. J., Chemaitelly, H., & Coyle, P., et al. (2021). SARS-CoV-2 reinfection in a cohort of 43,000 antibody-positive individuals followed for up to 35 weeks. medRxiv. 10.1101/2021.01.15.21249731
- 20.Hansen CH, Michlmayr D, Gubbels SM, Mølbak K, Ethelberg S. Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: A population-level observational study. The Lancet. 2021 doi: 10.1016/S0140-6736(21)00575-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krammer F, Srivastava K, Alshammary H, et al. Antibody responses in seropositive persons after a single dose of SARS-CoV-2 mRNA vaccine. New England Journal of Medicine. 2021 doi: 10.1056/NEJMc2101667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manisty C, Otter AD, Treibel TA, et al. Antibody response to first BNT162b2 dose in previously SARS-CoV-2-infected individuals. The Lancet. 2021 doi: 10.1016/S0140-6736(21)00501-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Samanovic, M. I., Cornelius, A. R., Wilson, J. P., et al. (2021). Poor antigen-specific responses to the second BNT162b2 mRNA vaccine dose in SARS-CoV-2-experienced individuals. medRxiv. 10.1101/2021.02.07.21251311
- 24.Kasstan B. Vaccines and vitriol: An anthropological commentary on vaccine hesitancy, decision-making and interventionism among religious minorities. Anthropology & Medicine. 2020 doi: 10.1080/13648470.2020.1825618. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
By request.