Abstract
A 6-year-old girl with a history of chronic immunosuppression following small bowel and colon transplantation for tufting enteropathy presented with a diffuse, facial-predominant eruption composed of pink-to-skin-colored papules with central white dystrophic spicules. Histology from a punch biopsy and polymerase chain reaction (PCR) from plucked spicules confirmed a diagnosis of trichodysplasia spinulosa (TS). Additional molecular studies identified several strains of the trichodysplasia spinulosa–associated polyomavirus infecting multiple tissues of the patient, confirming the systemic nature of trichodysplasia spinulosa infections.
Keywords: diagnosis, pediatric, trichodysplasia spinulosa, trichodysplasia spinulosa–associated polyomavirus
1. CASE PRESENTATION
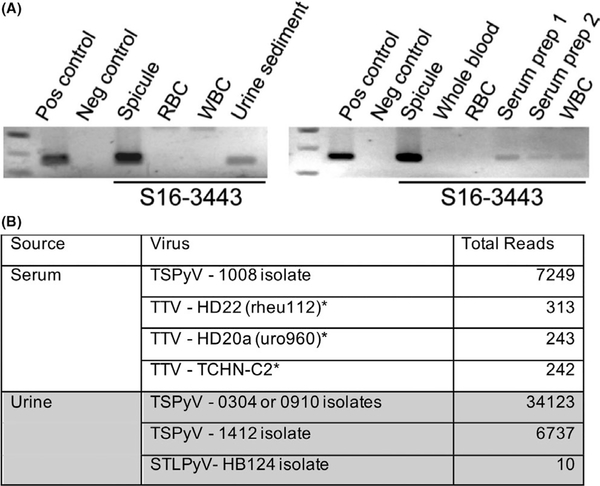
A 6-year-old girl presented with a several-month history of a papular eruption on the face, trunk, and extremities. She had a history of tufting enteropathy confirmed by genetic testing, treated with small bowel and colon transplantation, which was complicated by severe graft rejection requiring chronic immunosuppression with prednisolone, tacrolimus, and sirolimus. On examination, she had multiple follicular-based papules on the central face, trunk, and extremities with white dystrophic hairs protruding from the center of the papules (Figure 1A). A punch biopsy from the right thigh lacked a well-defined hair shaft and showed a dilated infundibulum filled with keratinaceous and apoptotic debris (Figure 1B). Detection of the trichodysplasia spinulosa–associated polyomavirus (TSPyV) by polymerase chain reaction (PCR) from plucked spicules confirmed the diagnosis. TSPyV was also detected in blood and urine. Purification, rolling circle amplification, and high-throughput sequencing identified abundant strains of TSPyV in the serum and urine in addition to St. Louis polyomavirus and several torque tenoviruses (Figure 2). The patient was treated with topical 1% cidofovir cream but was lost to follow-up as her family left the country.
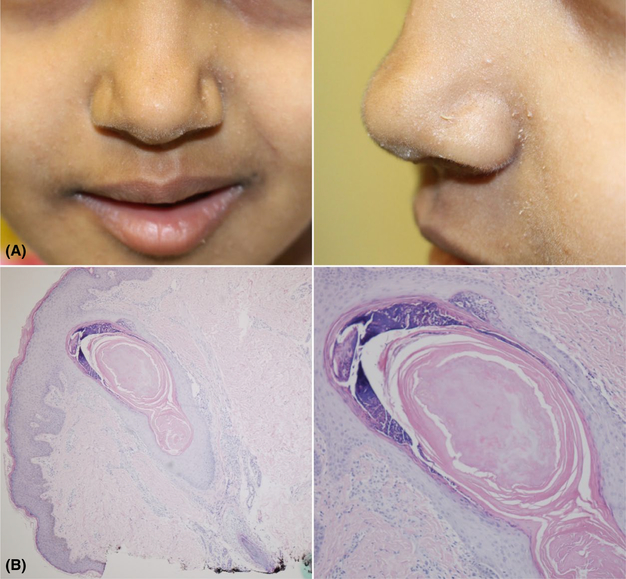
FIGURE 1.
Clinical and histologic images of trichodysplasia spinulosa. A, Multiple follicle-based papules on the central face with white dystrophic hairs protruding from the center of the papules. B, Biopsy lacked a well-defined hair shaft and showed a dilated infundibulum filled with keratinaceous and apoptotic debris
FIGURE 2.
A, Polymerase chain reaction and B, next-generation sequencing of trichodysplasia spinulosa–associated polyomavirus in hair (Spicule), urine, and serum. STLPyV, St. Louis polyomavirus; TSPyV, trichodysplasia spinulosa–associated polyomavirus; TTV, torque tenovirus; *Torque tenoviruses with > 200 total reads listed
2. DISCUSSION
Trichodysplasia spinulosa (TS) is a rare skin eruption caused by a human polyomavirus TSyPV.1 Most cases occur with immunosuppression after solid organ transplant and rarely, blood dyscrasias.2 It has been reported in a wide range of patient ages, from 20 months to 70 years old.3 Clinical diagnosis may be confirmed by the characteristic histopathology, electron microscopy, or molecular demonstration of virus in affected hairs.1,4 Similar to a previously reported case,4 we were able to confirm the diagnosis by PCR from plucked spicules and suggest that this noninvasive method could be used as a diagnostic test in children or adults when a biopsy is not preferred.
Trichodysplasia spinulosa–associated polyomavirus has been detected in the skin, urine, blood, respiratory secretions, and cerebrospinal fluid of TS patients.4,5 Although our patient had clear evidence of a systemic TSPyV infection with virus detectable in the blood and urine, the skin was the only site of end-organ dysfunction. In the general population, seroprevalence against TSPyV is high (70%-80%), and the virus has been isolated from tonsillar tissue, suggesting that it could remain latent in lymphoid tissue.3 However, primary infection by TSPyV in a naïve patient has also been proposed as the mechanism for disease development in TS.5
Next-generation sequencing performed in this case allowed for the detection of multiple unique strains of TSPyV in this patient's blood and urine. These studies suggest that the virus is undergoing active selection and mutation during the infection process. Although the clinical relevance of the various strains is not understood, it may be of clinical value to determine whether only one or multiple strains may cause the cutaneous eruption. Finally, the clinical relevance of torque tenoviruses (TTV) (TTV-HD22, TTV-HD20a, TTV-TCHN-C2) and St. Louis polyomavirus coinfecting this patient with TS remains unclear. Both PyV and TTV have been described as part of the “human virome,” but their contribution to normal or disease tissues states has not been defined.
REFERENCES
- 1.van der Meijden E, Janssens RW, Lauber C, Bouwes Bavinck JN, Gorbalenya AE, Feltkamp MC. Discovery of a new human polyomavirus associated with trichodysplasia spinulosa in an immunocompromized patient. PLoS Pathog. 2010;6:e1001024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Osswald SS, Kulick KB, Tomaszewski M-M, Sperling LC. Viral-associated trichodysplasia in a patient with lymphoma: a case report and review. J Cutan Pathol. 2007;34:721–725. [DOI] [PubMed] [Google Scholar]
- 3.Sadeghi M, Aaltonen LM, Hedman L, Chen T, Soderlund-Venermo M, Hedman K. Detection of TS polyomavirus DNA in tonsillar tissues of children and adults: evidence for site of viral latency. J Clin Virol. 2014;59:55–58. [DOI] [PubMed] [Google Scholar]
- 4.Barton M, Lockhart S, Sidbury R, Wang R, Brandling-Bennett H. Trichodysplasia spinulosa in a 7-year-old boy managed using physical extraction of keratin spicules. Pediatr Dermatol. 2017;34:e74–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Meijden E, Horvath B, Nijland M, et al. Primary polyomavirus infection, not reactivation, as the cause of trichodysplasia spinulosa in immunocompromised patients. J Infect Dis. 2017;215:1080–1084. [DOI] [PubMed] [Google Scholar]