Abstract
Care for non-communicable diseases, including hypertension and diabetes (HTN/DM), is recognized as a growing challenge in humanitarian crises, particularly in low- and middle-income countries (LMICs) where most crises occur. There is little evidence to support humanitarian actors and governments in designing efficient, effective, and context-adapted models of care for HTN/DM in such settings. This article aimed to systematically review the evidence on models of care targeting people with HTN/DM affected by humanitarian crises in LMICs. A search of the MEDLINE, Embase, Global Health, Global Indexus Medicus, Web of Science, and EconLit bibliographic databases and grey literature sources was performed. Studies were selected that described models of care for HTN/DM in humanitarian crises in LMICs. We descriptively analysed and compared models of care using a conceptual framework and evaluated study quality using the Mixed Methods Appraisal Tool. We report our findings according to PRISMA guidelines. The search yielded 10 645 citations, of which 45 were eligible for this review. Quantitative methods were most commonly used (n = 34), with four qualitative, three mixed methods, and four descriptive reviews of specific care models were also included. Most studies detailed primary care facility-based services for HTN/DM, focusing on health system inputs. More limited references were made to community-based services. Health care workforce and treatment protocols were commonly described framework components, whereas few studies described patient centredness, quality of care, financing and governance, broader health policy, and sociocultural contexts. There were few programme evaluations or effectiveness studies, and only one study reported costs. Most studies were of low quality. We concluded that an increasing body of literature describing models of care for patients with HTN/DM in humanitarian crises demonstrated the development of context-adapted services but showed little evidence of impact. Our conceptual framework could be used for further research and development of NCD models of care.
Keywords: Non-communicable disease, conflict, disasters, refugee health, displaced populations, complex emergencies, programmes, implementation
KEY MESSAGES.
This systematic review identified an increasing body of literature documenting models of care for hypertension and diabetes (HTN/DM) management in humanitarian settings, but studies remain of limited quality.
The majority of studies described primary care-level, physician-delivered HTN/DM services in middle-income countries affected by the Syrian crisis.
Our use of a model of care conceptual framework allowed the comparison of studies from diverse regions and crises and may prove useful to guide further research and evaluation and programme design.
Introduction
The burden of non-communicable diseases (NCDs) has received increasing global attention in the last decade, and NCD care has been included as a specific target of the Sustainable Development Goals (Nugent et al., 2018). Low- and middle-income countries (LMICs) bear most of the burden of NCD mortality and morbidity, and it is estimated this burden will continue to rise and cause a greater financial burden on health systems and households, particularly in LMICs (Kankeu et al., 2013). Achieving the global target of reducing premature deaths due to NCDs by one-third will not be possible without health policies and programmes that reach the most vulnerable communities such as those affected by conflict or disaster (Tangcharoensathien et al., 2015). However, to date, there has been limited evidence to guide interventions for NCD prevention and care in LMICs and even less for humanitarian contexts (Kane et al., 2017; Allen et al., 2018).
In 2017, there were an estimated 180 million people affected by armed conflicts, including a record 68.5 million refugees and internally displaced people (IDPs) (United Nations High Commissioner for Refugees, 2018). An additional 95 million were affected by natural disasters (Centre for Research on the Epidemiology of Disasters, 2018). LMICs hosted the majority of these populations. Managing NCDs is particularly challenging in humanitarian crises due to insecurity and weakened or damaged health systems that are often under-capacitated and poorly aligned to address chronic care needs (Woodward et al., 2016). Humanitarian actors are now increasing their focus on NCDs, an area until recently neglected compared to other emergency health policies and measures (Amara and Aljunid, 2014; Massey et al., 2017; Slama et al., 2017). These actors recognize the need for context-adapted approaches based on the local epidemiology, population demographics and sociocultural characteristics, and health system composition and quality (Jobanputra et al., 2016). They can also draw on lessons learned from decades of implementing chronic HIV/AIDS treatment, such as incorporating task sharing while avoiding a vertical approach that neglects primary health care (Rabkin et al., 2018).
Studies on NCD interventions in humanitarian settings in LMICs have been limited to date (Ruby et al., 2015; Jobanputra et al., 2016; Aebischer Perone et al., 2017; Blanchet et al., 2017; Ansbro et al., 2021). A 2015 systematic review examining the effectiveness of NCD interventions in humanitarian settings identified only eight studies meeting inclusion criteria (Ruby et al., 2015). The review found that implementation of algorithm-based interventions for specific NCDs and cohort monitoring was successful in improving programmatic outcomes, but the included studies were of limited quality overall. None of the selected studies focused on NCD prevention, and none was conducted in Sub-Saharan Africa. Another recent review, describing diabetes care in humanitarian crises, found a paucity of existing evidence describing the burden, access to care and utilization of services for diabetes patients in such settings (Kehlenbrink et al., 2019). The review highlighted the need to address financial and other barriers to patient access and to develop cost-effective models of care.
Implementing NCD care in humanitarian crises requires the development of a context-adapted approach or ‘model of care’. A model of care may be characterized as a conceptual and pragmatic framework that describes how services are delivered within a health system (Davidson et al., 2006; Agency for Clinical Innovation, 2013). Several authors have proposed that robust primary care services are an essential part of the model of care for screening and management of hypertension, diabetes, and other NCDs in LMICs (Maher et al., 2012; Jobanputra et al., 2016; Aebischer Perone et al., 2017). A systematic review of primary care-based models of care for NCDs in Sub-Saharan Africa proposed a modified conceptual framework to understand and compare these models based on evidence from these settings (Kane et al., 2017). The authors identified the key health systems roles of NCD screening, prevention, and control, and they described model inputs, such as dedicated NCD health workers, strong communication with medical specialists, and patient treatment adherence support.
There are unique challenges to implementing similar models of NCD care in humanitarian crises. These include forced displacement, which may lead to the disruption of treatment and support, and interrupted health services due to the movement and attrition of health care workers (HCWs), insecurity, destruction of infrastructure, or breakdown in supply chains and data processes (Jobanputra et al., 2016; Aebischer Perone et al., 2017; Slama et al., 2017;). NCD screening has not been recommended during an emergency response in settings without programmes for disease management and treatment (Aebischer Perone et al., 2017). Furthermore, the fragmentation of care between governmental and non-governmental organizations (NGOs) can lead to the creation of parallel health systems and programmes, further complicating the delivery of continuous, integrated care as well as the sustainability of such programmes when NGO actors depart (Blanchet et al., 2016). Primary-level models of care for NCDs in humanitarian settings should be designed to take account of these specific challenges.
In order to inform the development of effective and patient-centred models of care for NCDs in humanitarian settings, it is essential to explore the currently available evidence and identify gaps to guide urgently needed research in this area. This systematic review focused on two conditions, hypertension and diabetes (HTN/DM), that contribute significantly to the global burden of NCDs and that are amenable to being managed using a primary care model. Our review used broader inclusion criteria than previous studies, encompassing quantitative, qualitative, and mixed methods studies. We developed a model of care conceptual framework for NCD care in humanitarian crises to guide our review.
The aim of this systematic review was to examine the evidence on models of care for HTN/DM in humanitarian crises in LMICs. The objectives were to: (1) describe the key characteristics and findings of eligible studies; (2) analyse the models of care for patients with HTN/DM in humanitarian crises using a model of care conceptual framework; (3) evaluate the quality of the evidence for models of care; and (4) provide policy and research recommendations for the implementation of NCD models of care in humanitarian crises.
Methods
This systematic review followed the reporting items for systematic reviews as described in the PRISMA statement (Moher et al., 2009).
Eligibility criteria
Populations of study
The study populations were defined as people affected by humanitarian crises including refugees, IDPs, and non-displaced persons, as well as host communities when the former groups were also included in the study. Only crises that occurred in LMICs, as defined by the World Bank, were included (World Bank, 2018). Studies set in the protracted health crises caused by HIV/AIDS and tuberculosis, in the absence of another humanitarian crisis, were excluded. Studies examining NCD care of refugees and IDPs residing or resettled in high-income countries, as well as active and former combatants, were excluded because high-income country health systems tend to have long-established programs and guidelines for NCDs and different resources available for NCD care compared to those in LMICs.
Health conditions
We included studies examining models of care for NCDs (either unspecified NCDs or a limited number of highly prevalent NCDs); models specific to hypertension and/or diabetes; or models managing complications from these diseases. Studies and reports that described models of care for specific NCDs other than HTN/DM were excluded, such as programmes for cancer care.
Interventions and levels of care
Health intervention modalities included those spanning the disease course from preventative care, screening, healthy behaviour promotion, disease management, and treatment to rehabilitation and palliation. In order to encompass the spectrum of potential interventions at the individual and population levels, sites and levels of care ranged from community- and home-based programmes to facility-based primary, secondary, and tertiary level programmes. Studies that only described disease prevalence or health-seeking behaviours without describing a modality of care, such as how interventions were delivered, were excluded.
Types of studies and outcome measures
This review included quantitative, qualitative, mixed methods studies, policy analyses, and case study articles, which offered additional descriptive detail on specific models of care referred to in the included empirical studies. Thus, neither the presence of a control group nor the presence of outcome data was an inclusion requirement. When present, patient clinical outcome and process outcome data, described below, were reviewed as well as information on patient and providers’ perceptions of the model of care.
Search strategy
This search included the MEDLINE, Embase, Global Health, Global Indexus Medicus, Web of Science (Science Citation Index Expanded, Social Sciences Citation Index, and Emerging Sources Citation Index), and EconLit bibliographic databases and was conducted in November 2020. Search terms were related to humanitarian crises, NCDs, and models of care. The MEDLINE search strategy shown (see Supplementary File S1) was originally created in MEDLINE and then modified for the other databases. We developed search terms for ‘model of care’ from previous literature reviews of NCD care and in discussion with experts (Ruby et al., 2015; Kane et al., 2017). Search terms were also mapped to subject headings of each bibliographic database, and LMIC search terms were used to narrow results (World Bank, 2018). We included studies published after January 1990 until 31 December 2019, since previous reviews did not find studies on NCD care in humanitarian emergencies prior to 1997 (Ruby et al., 2015; Blanchet et al., 2017). No language restrictions were applied in the search, and no studies were excluded based on language alone. We also reviewed grey literature for any original research that described HTN/DM models of care. We searched the websites of larger humanitarian NGOs and supranational organizations including United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA), United Nations High Commissioner for Refugees, Médecins Sans Frontières (MSF) and MSF Field Research, International Rescue Committee, International Committee of the Red Cross, International Federation of Red Cross and Red Crescent Societies, Mercy Corps, International Medical Corps, ReliefWeb, Humanity & Inclusion—Handicap International, and HelpAge International.
Study selection and data extraction
After the removal of duplicates, six authors independently reviewed the citation title and abstract for inclusion in the full-text review. Citations with titles that appeared to meet inclusion criteria but without an available abstract were also included for full-text review. The analysis of full-text articles for final inclusion was conducted by two authors, and disagreements were moderated by a third author. We contacted the authors of relevant papers if the full-text article was not available.
Data were extracted from all included studies by two authors using an Excel spreadsheet based on the model of care conceptual framework. A third author conducted the extraction on a random sample each of the final selected papers for quality control purposes. Data extraction variables included study characteristics, type of humanitarian crisis, study population, research methods, key findings according to the conceptual framework domains, and outcomes if available. Any relevant outcome measures were included, such as patient intermediate clinical outcomes (achieving target measures for blood pressure and glycaemic control), treatment default or non-adherence rates, and significant cardiovascular disease events or mortality. Process or programmatic outcomes included the fidelity of implementation of standardized protocols or guidelines for diagnosis, treatment and monitoring, outcomes related to training of physicians and other medical staff in NCD care (numbers trained, change in knowledge), and availability of essential supplies and medications.
Model of care conceptual framework
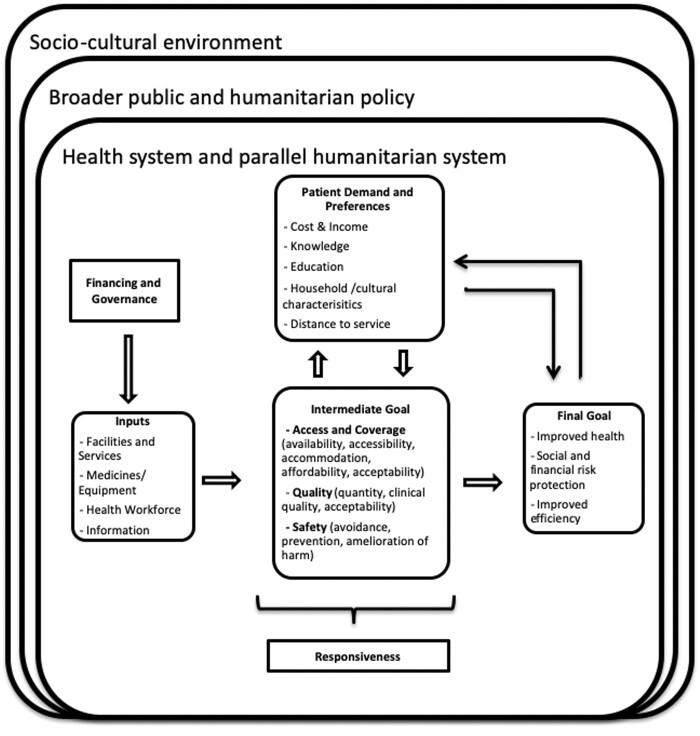
In order to describe and compare diverse implementation models of NCD care across different humanitarian programmes and settings, we developed a conceptual framework based on the World Health Organization (WHO) health systems building blocks framework and other existing models of care in LMICs (Figure 1) (World Health Organization, 2007; Kane et al., 2017; Kruk et al., 2018). Acknowledging the criticism that the building blocks approach to health system appraisal is somewhat mechanistic in evaluating each block separately, our study framework was modified to enable an analysis of the relationship between the various resources and components of a health system. It was informed by the ‘systems thinking’ approach that addresses the complexity of health systems and the interactions of components or sub-systems leading to changes in the whole (Kruk et al., 2018).
Figure 1.
Conceptual framework for model of care for NCDs in humanitarian crises.
For this framework, we added the domain of patient demand and preferences to capture the concept of ‘patient centredness’ and the interaction between the formal health system and community-based formal or informal systems. The sub-themes in this domain were drawn from economic models and social systems approaches to describing health systems and were influenced by the recent discourse on the prioritization of quality in healthcare (Kruk et al., 2018). These sub-themes were cost and income, knowledge, education, household characteristics, and distance from the facility.
The intermediate health goals in this framework reflected those in the WHO health systems framework, highlighting the interaction of health system inputs with these patient needs and preferences (World Health Organization, 2007). The domains of access—availability, affordability, accessibility, accommodation, and acceptability—were derived from previously described measures of coverage (Penchansky and Thomas, 1981; Hernández-Quevedo and Papnicolas, 2013; Levesque et al., 2013). Availability was defined as the volume and type of existing services and whether this was adequate for the volume and needs of service users. Affordability constituted the patient’s capacity to use financial resources to obtain care balanced against their income and the perceived worth of the service. Accessibility addressed the match between the location of services vs the location of people in need, including transport, travel time, distance, and cost. The accommodation was defined as the organization of service delivery, such as opening times and ability of service users to accommodate to this. Acceptability was considered as the relationship between the services and the patient’s expectations of appropriate care.
The goal of health care quality was described by the quantity of intended care, quality of services provided, patient-perceived experience, and safety of health care processes. We included three additional intermediate health goals: system responsiveness, continuity of care, and integration of services. Responsiveness has been defined as the ability of health services meet a patient’s holistic needs; in this framework, it also encompassed a model of care’s ability to respond to changing patient needs in a volatile context (Hernández-Quevedo and Papnicolas, 2013; Kruk et al., 2018). Integration described the linkage between different levels and sites of care, such as facility-based care and community-based support as well as coordination between providers and institutions, while continuity of care referred to uninterrupted care throughout the patient’s disease and life course. They were included as another intermediate health goal to emphasize the chronic, integrated care required for HTN/DM. These intermediate goals directly impact the final goals of improved health, social financial risk protection and improved efficiency. For NCDs, we considered that measures of effective care leading to improved health may include improved intermediate clinical outcomes such as improved blood pressure control, decreased complications and deaths, behavioural outcomes such as reduced smoking and improved diet and exercise, and patient-level outcomes such as improved quality of life.
The model of care framework also placed the health system within the broader array of issues present during a humanitarian crisis. The first was sociocultural context, defined as the economic and social environment of the country where the health system is located. Contributing factors included cultural health beliefs and health-seeking behaviours. The second was the public and humanitarian policy context, which included tobacco and alcohol regulation and other health policies. The model of care framework was used to create a data extraction tool for use during full-text review, to guide the descriptive analysis of heterogeneous studies and synthesize the results.
Critical appraisal
The Mixed Methods Appraisal Tool (MMAT) was used on all studies presenting primary data. The MMAT is a critical appraisal tool that was designed for the appraisal stage of systematic reviews of empirical mixed studies that include qualitative, quantitative, and mixed methods studies. It allows appraisal of the methodological quality of five categories of studies: qualitative research, randomized controlled trials, non-randomized studies, quantitative descriptive studies, and mixed methods studies. We applied the 2018 version, which was updated on the basis of findings from a literature review of critical appraisal tools, interviews with MMAT users, and an e-Delphi study with international experts (Hong et al., 2018). An initial screening question was applied to determine if the study presented empirical data. Using the MMAT 2018 guidance document, each included study was assigned a study category within MMAT and was rated ‘don’t know/yes/no’ for each criterion of the chosen category (see Supplementary Table S3). MMAT discourages the calculation of an overall score and screening out of low-quality studies. Thus, ratings were presented along with a descriptive analysis of study strengths and weaknesses. Three authors performed the appraisal.
Ethics
The authors’ institution provided ethical approval for the conduct of this study.
Results
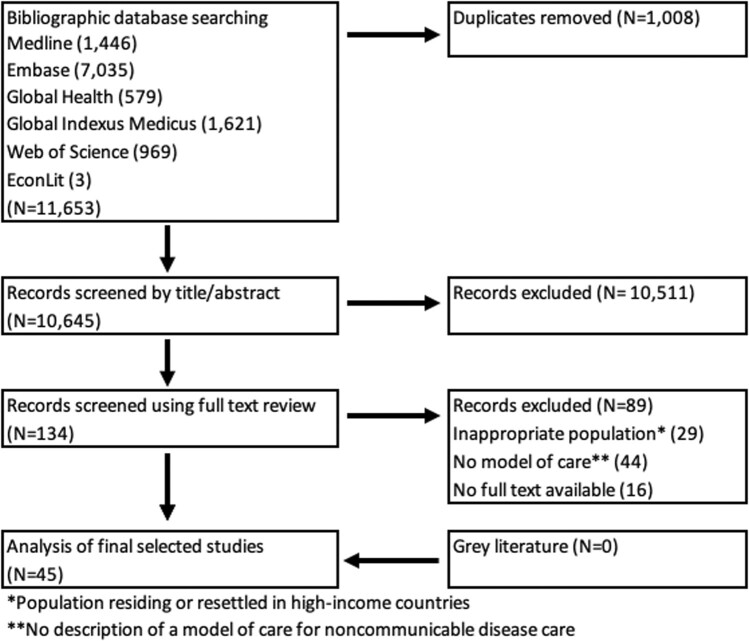
Study selection
The bibliographic databases yielded 10 645 citations after duplicates were removed (Figure 2). Based on English-language citation title or abstract, we selected 134 for a full-text review; 45 were eligible for data extraction. The other citations were excluded because there was neither description of how interventions were delivered nor of a specific care model (n = 44), the study populations resided in high-income countries (n = 29), or the full text was not available (n = 16). The grey literature search yielded no additional papers.
Figure 2.
PRIMSA flowchart from literature search and article screening.
Study characteristics
A summary of the 45 included records is shown in Table 1. The studies were published between 2000 and 2019, and the median year of publication was 2016. The majority (n = 37, 82%) involved populations living in or fleeing from conflict-affected countries while only eight were of populations affected by natural disasters (Ramachandran, 2005; Chan and Kim, 2011, 2010; Hung et al., 2013; Sun et al., 2013; Martinez et al., 2015; Mobula et al., 2016; Adrega et al., 2018). Among the studies from conflict-affected contexts, almost half (n = 18, 49%) concerned the protracted displacement of Palestinian populations served by UNRWA in their five fields of operation within the MENA region (Yusef, 2000; Mousa et al., 2010; Khader et al., 2012a,b, 2013, 2014a,b,c; Alabed et al., 2014; Saadeh et al., 2015; Shahin et al., 2015; Santoro et al., 2016; Radwan et al., 2017; Damiri et al., 2018; Saleh et al., 2018a,b,c; Abu Kishk et al., 2019); 10 concerned Syrian refugees in the host countries Jordan, Lebanon, and Turkey (Kallab, 2015; Collins et al., 2017; Doocy et al., 2017; Hyatt, 2017; Sethi et al., 2017; Elliott et al., 2018; Alawa et al., 2019; Kayali et al., 2019; McNatt et al., 2019; Boulle et al., 2019b); three described forcibly displaced Iraqis in Iraq and Jordan (Mateen et al., 2012; Istepanian et al., 2014; Baxter et al., 2018); five concerned protracted conflicts in Mali, Democratic Republic of Congo (DRC), or Myanmar (Burma) and one described an acute conflict setting in the Philippines (Besancon et al., 2015; Murphy et al., 2017; Naing and Bakker, 2018; Saito et al., 2018; Salazar et al., 2018; Ansbro et al., 2019). No studies were found from the Europe and Central Asia or Latin America and the Caribbean regions.
Table 1.
Summary of study characteristics
| Authors, date, reference | Title | Setting and population | Study designa and size |
|---|---|---|---|
| Abu Kishk et al. (2019) | Model to improve cardiometabolic risk factors in Palestine refugees with diabetes mellitus attending UNRWA health centres | Non-camp- and camp-based Palestinian refugees enrolled for DM care UNRWA PHCCs in the five fields of operation | Observational cohort study with 1598 participants |
| Adrega et al. (2018) | Prevalence of cardiovascular disease risk factors, health behaviours and atrial fibrillation in a Nepalese post-seismic population: a cross-sectional screening during a humanitarian medical mission | Camp and village-based rural population 18 months post-earthquake in Nepal | Cross-sectional analytical study with 270 participants comparing two sites |
| Alabed et al. (2014) | An assessment of diabetes care in Palestinian refugee camps in Syria | Palestinian refugees enrolled for DM in care at UNRWA PHCCs in Syria | Descriptive cross-sectional survey of 154 participants |
| Alawa et al. (2019) | Evaluating the provision of health services and barriers to treatment for chronic diseases among Syrian refugees in Turkey: a review of literature and stakeholder interviews | Syrian refugees in both non-camp- and camp-based settings in Turkey | Qualitative semi-structured interviews with 61 patients and staff members, and document review |
| Ansbro et al. (2019) | Management of diabetes and associated costs in a complex humanitarian setting in the Democratic Republic of Congo: a retrospective cohort study | General population attending a diabetes outpatient service in a rural conflict-affected region of the Democratic Republic of Congo | Mixed methods design. Retrospective cohort study with 243 participants and descriptive costing study |
| Baxter et al. (2018) | Access to care for non-communicable diseases in Mosul, Iraq between 2014 and 2017: a rapid qualitative study | Displaced Iraqis presenting to clinics in camp-based setting | Qualitative semi-structured interviews with 15 physicians |
| Besancon et al. (2015) | Diabetes in an emergency context: the Malian case study | General urban population affected by acute outbreak of conflict in Mali | Descriptive case study |
| Boulle et al. (2019b) | Cardiovascular disease among Syrian refugees: a descriptive study of patients in two Médecins Sans Frontières clinics in northern Lebanon | Syrian refugees and local communities with atherosclerotic cardiovascular disease presenting to NCD clinics in Lebanon | Retrospective cohort study with 1286 participants with cross-sectional survey of subset of 514 participants |
| Chan and Kim (2010) | Remote mobile health service utilization post 2005 Kashmir-Pakistan earthquake | General rural population presenting to mobile clinics during a 3-month post-earthquake period in Pakistan | Descriptive cross-sectional study with 3084 participants comparing two sites |
| Chan and Kim (2011) | Chronic health needs immediately after natural disasters in middle-income countries: the case of the 2008 Sichuan, China earthquake | General urban population presenting to a single hospital during a 2-week period post-earthquake in China | Cross-sectional descriptive design with 182 participants |
| Collins et al. (2017) | Cardiovascular disease risk and prevention amongst Syrian refugees: mixed methods study of Médecins Sans Frontières programme in Jordan | Non-camp-based Syrian refugees and host population attending non-governmental organization clinics in north Jordan | Mixed methods design. Quantitative retrospective cohort with 2901 participants and qualitative key informant staff interviews |
| Damiri et al. (2018) | Metabolic syndrome among overweight and obese adults in Palestinian refugee camps | Camp-based refugees attending camp-based UNRWA clinics in the West Bank | Cross-sectional survey with 689 participants |
| Doocy et al. (2017) | Guidelines and mHealth to improve quality of hypertension and type 2 diabetes care for vulnerable populations in Lebanon: longitudinal cohort study | Non-camp-based Syrian refugees and host population attending primary care clinics in Lebanon | Observational cohort with 793 participants, structured interviews with 761 participants |
| Elliott et al. (2018) | A cross-sectional assessment of diabetes self-management, education and support needs of Syrian refugee patients living with diabetes in Bekaa Valley Lebanon | Non-camp-based rural Syrian refugees and host population attending NGO primary care clinic in Bekaa, Lebanon | Cross-sectional survey with 292 participants |
| Hung et al. (2013) | Disease pattern and chronic illness in rural China: the Hong Kong Red Cross basic health clinic after 2008 Sichuan earthquake | General rural population presenting to field clinic during a three-week post-earthquake period in China | Descriptive cross-sectional design with 2034 participants |
| Hyatt (2017) | Tackling non-communicable disease among Syrian refugees and vulnerable host communities in Jordan | Non-camp-based Syrian refugees and local population accessing community-based organisations’ services in Jordan | Descriptive case study |
| Istepanian et al. (2014) | The potential of m-health systems for diabetes management in post conflict regions a case study from Iraq | Patients attending an urban hospital outpatient diabetic clinic in conflict-affected Iraq | Non-blinded randomized control design with 12 participants |
| Kallab (2015) | Management of hypertension and diabetes for the Syrian refugees and host community in selected health facilities in Lebanon | Non-camp-based Syrian refugees and host population attending PHCCs and mobile units in Lebanon | Descriptive case study |
| Kayali et al. (2019) | Treating Syrian refugees with diabetes and hypertension in Shatila refugee camp, Lebanon: Médecins Sans Frontières model of care and treatment outcomes | Syrian refugees with DM or HTN presenting to an urban, camp-based NCD clinic in Lebanon | Retrospective cohort analysis of 2644 patients |
| Khader et al. (2012b) | Cohort monitoring of persons with diabetes mellitus in a primary healthcare clinic for Palestine refugees in Jordan | Non-camp- and camp-based Palestinian refugees enrolled for DM care in one UNRWA PHCC in Amman, Jordan | Retrospective cohort study with 2851 cases, using closed and open cohort approaches. |
| Khader et al. (2012a) | Cohort monitoring of persons with hypertension: an illustrated example from a primary healthcare clinic for Palestine refugees in Jordan | Non-camp- and camp-based Palestinian refugees enrolled for HTN care at six UNRWA PHCCs in Jordan | Retrospective cohort study with 4130 cases |
| Khader et al. (2013) | Diabetes mellitus and treatment outcomes in Palestine refugees in UNRWA primary health care clinics in Jordan | Non-camp- and camp-based Palestinian refugees enrolled for DM care at six UNRWA PHCCs in Jordan | Retrospective cohort study with 12 548 cases |
| Khader et al. (2014a) | What happens to Palestine refugees with diabetes mellitus in a primary healthcare centre in Jordan who fail to attend a quarterly clinic appointment? | Non-camp- and camp-based Palestinian refugees ever enrolled for DM care at single UNRWA PHCC in Amman, Jordan | Retrospective cohort design with 2974 participants |
| Khader et al. (2014b) | Treatment outcomes in a cohort of Palestine refugees with diabetes mellitus followed through use of E-Health over 3 years in Jordan | Non-camp- and camp-based Palestinian refugees; new patients with DM entered into E-Health system with DM in a 3-month period at one UNRWA PHCC in Jordan | Retrospective cohort study with 119 participants |
| Khader et al. (2014c) | Hypertension and treatment outcomes in Palestine refugees in United Nations Relief and Works Agency primary health care clinics in Jordan | Non-camp- and camp-based Palestinian refugees ever enrolled for HTN care at six UNRWA PHCCs in Jordan | Retrospective cohort study with 18 881 participants |
| Martinez et al. (2015) | Use of the WHO Package of Essential Noncommunicable Disease Interventions after Typhoon Haiyan | General population presenting to health facilities in a 1-year post-hurricane period in the Philippines | Descriptive case study |
| Mateen et al. (2012) | Medical conditions among Iraqi refugees in Jordan: data from the United Nations Refugee Assistance Information System | Non-camp- and camp-based Iraqi refugees registered in Jordan | Retrospective descriptive cross-sectional study with 7642 participants |
| McNatt et al. (2019) | “What's happening in Syria even affects the rocks”: a qualitative study of the Syrian refugee experience accessing noncommunicable disease services in Jordan | Syrian refugees in both non-camp- and camp-based settings in Jordan | Qualitative structured in-depth interviews 68 participants |
| Mobula et al. (2016) | Prevalence of Hypertension among Patients Attending Mobile Medical Clinics in the Philippines after Typhoon Haiyan | Patient presenting to a mobile medical unit following a tropical cyclone in the Philippines | Retrospective cohort analysis of 3730 patients |
| Mousa et al. (2010) | Hyperglycaemia, hypertension and their risk factors among Palestine refugees served by UNRWA | Palestinian refugees who received targeted HTN/DM screening as part of routine activities during a 1-month period in three PHCCs selected from each of the five UNRWA fields of operation | Descriptive cross-sectional study across multiple clinical sites with 7762 patients |
| Murphy et al. (2017) | Diabetes care in a complex humanitarian emergency setting: a qualitative evaluation | General population attending a DM outpatient service in a rural conflict-affected region of the Democratic Republic of Congo | Qualitative investigation with focus group discussions with 16 patients and staff members and individual interviews with 17 participants |
| Naing and Bakker (2018) | Challenges for migrant and cross-border populations with diabetes mellitus at Mae Tao Clinic in the Mae Sot-Myawaddy border region of Thailand and Myanmar | Myanmar refugees with diabetic complications presenting comprehensive clinic in Thailand near the Myanmar border | Descriptive case study |
| Radwan et al. (2017) | Influence of organizational culture on provider adherence to the diabetic clinical practice guideline: using the competing values framework in Palestinian Primary Healthcare Centres | Health care workers at UNRWA PHCCs for Palestinian refugees in the Gaza Strip | Cross-sectional study of health workers from different facilities with 323 participants |
| Ramachandran (2005) | Experiences of the WHO Collaborating Centre for Diabetes in India in managing tsunami victims with diabetes | Patients with diabetes in medical relief camps following a tsunami in India | Descriptive case study |
| Saadeh et al. (2015) | Trends in the utilization of antihypertensive medications among Palestine refugees in Jordan, 2008-2012 | Non-camp- and camp-based Palestinian refugees diagnosed with HTN attending UNRWA PHCCs in Jordan 2008-2012. | Retrospective review of procurement data and retrospective cohort analysis. |
| Saito et al. (2018) | Challenges to primary healthcare services in the management of non-communicable diseases in marginalised populations on the Thailand-Myanmar border: a pilot survey | Non-camp- and camp-based Myanmar refugees and local population registered for NCD care at comprehensive clinic in Thailand near the Myanmar border | Retrospective cohort analysis of 238 patients |
| Salazar et al. (2018) | Health Consequences of an Armed Conflict in Zamboanga, Philippines Using a Syndromic Surveillance Database | General urban population presenting to health facilities in an acute conflict lasting 7 months in the Philippines | Retrospective cross-sectional study of 49 health facilities’ records |
| Saleh et al. (2018c) | Using Mobile Health to Enhance Outcomes of Noncommunicable Diseases Care in Rural Settings and Refugee Camps: Randomized Controlled Trial | Palestinian refugees and host population in catchment areas of five rural MOPH and three camp-based UNRWA PHCCs and those enrolled in HTN/DM care at those clinics and eight comparator clinics. | Randomized control design randomized at health facility level with 8 intervention and 8 control clinics and 2359 participants |
| Saleh et al. (2018a) | eHealth as a facilitator of equitable access to primary healthcare: the case of caring for non-communicable diseases in rural and refugee settings in Lebanon | Palestinian refugees and local communities receiving community-based screened for HTN/DM and referred to selected ministry or UNRWA PHCCs in Lebanon. | Descriptive cross-sectional study with 3481 participants |
| Saleh et al. (2018b) | mHealth use for non-communicable diseases care in primary health: patients' perspective from rural settings and refugee camps | Palestinian refugees and host community enrolled for HTN/DM care in selected camp-based UNRWA or rural MOPH PHCCs and those diagnosed/high risk on community-based screening in the PHCC catchment areas in Lebanon | Mixed methods design. Cross-sectional telephone survey with 1000 participants. Focus group discussions with 39 participants |
| Santoro et al. (2016) | Primary healthcare reform in the United Nations Relief and Works Agency for Palestine Refugees in the Near East | Non-camp- and camp-based Palestinian refugees enrolled in HTN/DM care in UNRWA PHCCs in the five fields of operation | Case study of health system reform using a chronic care model |
| Sethi et al. (2017) | Community-Based Noncommunicable Disease Care for Syrian Refugees in Lebanon | Syrian refugees in informal tented settlements and low-income host population in rural Lebanon | Cross-sectional analytical study with 2000 participants |
| Shahin et al. (2015) | Diabetes care in refugee camps: the experience of UNRWA | Non-camp- and camp-based Palestinian refugees enrolled for HTN/DM care UNRWA PHCCs in the five fields of operation | Case study of NCD care system citing primary quantitative research |
| Sun et al. (2013) | Clinical characteristics of hypertension among victims in temporary shield district after Wenchuan earthquake in China | Temporary shelter-based urban population displaced during a 1-year post-earthquake period China | Descriptive cross-sectional survey of 3230 participants |
| Yusef (2000) | Management of diabetes mellitus and hypertension at UNRWA primary health care facilities in Lebanon | Palestinian refugees enrolled for HTN/DM in care at all 24 UNRWA PHCCs in Lebanon | Descriptive cross-sectional study of 2202 participants |
DM, diabetes; HTN, hypertension; NCD, non-communicable disease; PHCCs, primary health care clinics; UNRWA, United Nations Relief and Works Agency for Palestine Refugees in the Near East.
Study design assigned based on MMAT 2018 guidance (Hong et al., 2018).
In terms of target NCD condition, the majority of included studies (19) described a combined model for HTN/DM care (most referring to a single model implemented by UNRWA, described below). Nine studies described services specific to diabetes care, of which three included children under 16 years old with Type 1 diabetes (Alabed et al., 2014; Besancon et al., 2015; Kayali et al., 2019). Eight studies described services providing ad hoc primary-level or immediate-response post-disaster care that included any NCD presenting to the service, while four studies described services focusing on three of the WHO-defined ‘big five’ NCDs (cardiovascular disease including hypertension, diabetes and/or chronic respiratory disease, but excluding cancer and mental health disorders). An additional four studies described screening activities for hypertension alone or broader cardiovascular disease risk factors.
The most common type of study design was a quantitative cross-sectional approach, used in 15 (33%) of studies, while 10 (22%) used a retrospective, descriptive cohort analysis using quantitative methods to characterize a model of care for a specific patient population. Seven papers (15%) presented research intervention studies, including two implementation studies measuring the impact of an NCD intervention, and three others using mixed methods for evaluation. Three studies used a qualitative approach of semi-structured interviews with patients or key stakeholders that focused on barriers to NCD care (Baxter et al., 2018; Alawa et al., 2019; McNatt et al., 2019). Baxter et al. (2018) and McNatt et al. (2019) specifically elicited the patient perception of NCD care. Other papers presented operational research, 1 (2%) using qualitative methods alone (Murphy et al., 2017) and 3 (7%) using a mixed methods approach (Collins et al., 2017; Saleh et al., 2018b; Ansbro et al., 2019). In general, the mixed methods studies complemented quantitative data from medical records with qualitative focus group discussions (FGDs) with patients or interviews with HCWs. Two papers, Murphy et al. (2017) and Ansbro et al. (2019), formed part of the same mixed methods programme evaluation. Eight (18%) studies were largely descriptive accounts of a case study or specific model of care (Ramachandran, 2005; Besancon et al., 2015; Kallab, 2015; Martinez et al., 2015; Shahin et al., 2015; Santoro et al., 2016; Hyatt, 2017; Naing and Bakker, 2018).
The health outcomes reported in these studies are given in Supplementary Table S2. The UNRWA descriptive cohort studies and the intervention studies reported on intermediate clinical outcomes (blood pressure and glycaemic control) (Yusef, 2000; Mousa et al., 2010; Khader et al., 2012a,b, 2013, 2014a,b,c; Shahin et al., 2015). Two of the cohort studies described clinically important ‘hard’ outcomes such as deaths or rates of cardiovascular disease complications (Khader et al., 2014c; Boulle et al., 2019b). Two studies investigating interventions for promoting a healthy diet and physical activity described patient-reported behaviour change (Saleh et al., 2018b; Abu Kishk et al., 2019). No other studies reported on clinically important effectiveness outcomes, behavioural outcomes, or patient-level outcomes, and none reported on other major adverse events. Systems or programmatic outcomes reported included the number of patients reached by the model of care, patient retention or loss to follow up, and referral rates (Kallab, 2015; Hyatt, 2017; Saito et al., 2018; Ansbro et al., 2019; Kayali et al., 2019;). Other studies measured the availability of essential medications and supplies or health care worker adherence to clinical guidelines such as whether a test was performed at the correct time interval (Alabed et al., 2014; Besancon et al., 2015; Martinez et al., 2015; Saadeh et al., 2015; Collins et al., 2017; Doocy et al., 2017; Radwan et al., 2017).
Models of care
We found that there was no single unifying model of care for HTN/DM care in humanitarian crises, and the variance in care models included in this review was highly dependent on context. In order to descriptively synthesize the diverse models presented in the included studies, we created a typology based on the type of crisis, region and integration with the health system, since these factors likely influenced model design. These are presented in Table 2. Most papers described models in settings of protracted, conflict-related displacement in the Middle East and North Africa (MENA) region (Yusef, 2000; Mousa et al., 2010; Khader et al., 2012a,b, 2013, 2014a,b,c; Mateen et al., 2012; Alabed et al., 2014; Kallab, 2015; Saadeh et al., 2015; Shahin et al., 2015; Santoro et al., 2016; Collins et al., 2017; Doocy et al., 2017; Hyatt, 2017; Radwan et al., 2017; Sethi et al., 2017; Baxter et al., 2018; Damiri et al., 2018; Elliott et al., 2018; Saleh et al., 2018a,b,c; Abu Kishk et al., 2019; Alawa et al., 2019; Boulle et al., 2019b; Kayali et al., 2019; McNatt et al., 2019). Fewer papers involved populations displaced by chronic conflict in non-MENA regions (Murphy et al., 2017; Naing and Bakker, 2018; Saito et al., 2018; Ansbro et al., 2019). A single study focused on a non-displaced population in the chronic conflict setting of Iraq (Istepanian et al., 2014). A third typology referred to responses to acute conflict and a fourth to responses to natural disasters (Ramachandran, 2005; Chan and Kim, 2011, 2010; Hung et al., 2013; Sun et al., 2013; Mobula et al., 2016; Adrega et al., 2018; Salazar et al., 2018).
Table 2.
Models of care by crisis type and region
| Relevant papers (authors, date) | Setting and population | Model of care description |
|---|---|---|
| CONFLICT—PROTRACTED DISPLACEMENT | ||
| Camp- and non-camp-based Palestinian refugees > 40 years enrolled for HTN/DM care in UNRWA PHCCs in five fields of operation: Syria, Jordan, Lebanon, Gaza and West Bank |
UNRWA Model UNRWA primary health care centres (PHCCs) operating in parallel to host country health systems, providing free HTN/DM screening and management since 1990s
|
|
| Non-camp-based Syrian refugees in Lebanon and both urban-based Syrian refugees and the vulnerable host population in Jordan and Lebanon | JORDAN and LEBANON NGO Programme Models
|
|
| Non-camp- and camp-based Palestinian refugees and host communities > 40 years in care at UNRWA PHCCs and MOPH PHCCs in rural area of Lebanon | LEBANON UNRWA and MOPH PHCCs—Intervention Study
|
|
| Doocy et al. (2017) | Non-camp-based Syrian refugees and host population > 40 years attending 10 NGO-supported PHCCs in Lebanon | LEBANON NGO-Supported MOPH PHCCs—Intervention Study
|
| Kallab (2015) | Non-camp-based Syrian refugees and local population > 40 years presenting to specific primary care clinics and mobile units in Lebanon | LEBANON NGO PHCC and Community Outreach Programme
|
| Sethi et al. (2017) | Syrian refugees in informal tented settlements in Lebanon and low-income host population | LEBANON NGO PHCC and Community Outreach Programme
|
| Hyatt (2017) | Non-camp-based Syrian refugees and local population in Jordan | JORDAN NGO Community Education Programme
|
| Mateen et al. (2012) | Non-camp- and camp-based Iraqi refugees registered with UNHCR in Jordan | JORDAN UNHCR Coordinated Medical care for Iraqi refugees
|
| Non-camp- and camp-based Syrian refugees in Jordan and Turkey | JORDAN and TURKEY
|
|
| Baxter et al. (2018) | Displaced Iraqis presenting to clinics in camp-based setting | IRAQ
|
| Non-camp- and camp-based Burmese refugees and local population in Thailand | THAILAND NGO provided comprehensive primary care
|
|
| CONFLICT—NON-DISPLACED POPULATIONS | ||
| Istepanian et al. (2014) | Patients attending urban hospital diabetes clinic in Iraq | IRAQ Diabetes Outpatient Intervention Study
|
| General population in a rural conflict-affected region of the Democratic Republic of Congo | NGO supported diabetes outpatient clinic in MOH hospital
|
|
| CONFLICT—ACUTE CRISIS | ||
| Besancon et al. (2015) | General urban population affected by conflict in Mali | NGO-supported continuity of care for DM during acute conflict
|
| Salazar et al. (2018) | Urban population attending health facilities in acute conflict in the Philippines | Surveillance of Presentations to Reporting Facilities
|
| NATURAL DISASTER | ||
| Chan and Kim (2010) | Rural population attending mobile clinics 3 months after an earthquake in Pakistan | PAKISTAN Ad Hoc primary-level healthcare provided by NGO
|
| Chan and Kim (2011) | Urban population evacuated to a hospital in a 2-week period post-earthquake in China | CHINA Hospital Triage Post Helicopter Evacuation
|
| Hung et al. (2013) | Rural population presenting to field clinics within three weeks of an earthquake in China | CHINA Red Cross Basic Health Clinic Ad Hoc Healthcare
|
| Sun et al. (2013) | Urban population displaced 1 year after an earthquake in China | CHINA Cross-sectional NCD Survey of IDPs
|
| Ramachandran (2005) | Urban population in medical relief camps following a tsunami in India | INDIA
|
| Mobula et al. (2016) | Urban and remote populations following a tropical cyclone in the Philippines | PHILIPPINES
|
| Martinez et al. (2015) | General population presenting to health facilities 1 year after a hurricane in the Philippines | PHILIPPINES Health System Strengthening During Recovery Phase
|
| Adrega et al. (2018) | Camp and village-based rural population 18 months post-earthquake in Nepal | NEPAL Opportunistic NCD Screening as part of ad hoc medical care
|
BP, blood pressure; DM, diabetes mellitus; HCWs, health care workers; HTN, hypertension; MMU, Mobile Medical Unit; NGO, non-governmental organization; OHG, oral hypoglycaemic agent; PEN, Package of Essential Non-communicable Disease Interventions; PHCC, primary health care clinic; UNRWA, United Nations Relief and Works Agency for Palestinians in the Near East.
In terms of the models from protracted displacement MENA settings, most described primary-level facility-based models of care for HTN/DM delivered by non-specialist doctors. The UNRWA model, described in 16 studies, has evolved in parallel to host country health systems since the 1990s, providing screening and treatment of HTN/DM to Palestinian refugees in their five fields of operation. Four studies described vertical, primary care level models developed by MSF in Jordan and Lebanon, which served Syrian refugees and the vulnerable host population (Collins et al., 2017; Elliott et al., 2018; Boulle et al., 2019b; Kayali et al., 2019). Three intervention studies from Lebanon documented approaches to strengthen the host country health system primary health care clinics (PHCCs) for Syrian refugees and the host population using eHealth tools and/or extending access through the use of mobile medical units (MMUs) (Saleh et al., 2018a,b,c). Three additional studies from the MENA region highlighted community-based services, with two describing the evolution from using MMUs to reach marginalized populations living in informal tented settlements in Lebanon to later supporting local PHCCs, linking these to the community through refugee outreach volunteers (Kallab, 2015; Sethi et al., 2017). The third, from Jordan, described a community educator programme that conducted NCD awareness sessions through a network of 11 community-based organizations (Hyatt, 2017). Prior to the Syrian crisis, the fragmented provision of NCD care for Iraqi refugees in Jordan via a mix of public and NGO primary and hospital-level providers was described in another study (Mateen et al., 2012). Alawa et al. (2019) tracked the evolution of refugee and health policy in Turkey in response to the Syrian crisis with the implementation of a Family Medicine model and the creation of migrant health centres.
The studies involving populations displaced by chronic conflict in non-MENA regions also described facility-based services: primary care services providing ad hoc care to Myanmar refugees on the Thai border and a nurse-led, vertical outpatient service focused on diabetes care in the DRC (Murphy et al., 2017; Naing and Bakker, 2018; Saito et al., 2018; Ansbro et al., 2019). Two studies involved responses to acute conflict: acute violence in northern Mali where an NGO supported the public service to provide diabetes care, through the evacuation of Type 1 diabetics, performance of a rapid needs assessment and provision of emergency kits and medications (Besancon et al., 2015). In the Philippines, the NCD needs at multiple health system levels were documented using a surveillance tool following the outbreak of armed conflict in one region (Salazar et al., 2018).
Eight studies described models of care implemented after natural disasters, five describing the acute response phase (Ramachandran, 2005; Chan and Kim, 2011, 2010; Hung et al., 2013; Mobula et al., 2016), while three described the recovery phase over 1-year post-disaster (Sun et al., 2013; Martinez et al., 2015; Adrega et al., 2018). In the acute settings, the models of care consisted of non-specialist doctors providing ad hoc care to all patients, including those presenting with NCDs, at a mobile clinic or field hospital, while one actively screened any patient over 14 years of age for hypertension (Hung et al., 2013). Post-disaster cross-sectional screening surveys were performed among urban internally displaced people following an earthquake in China (Sun et al., 2013), while rural and camp-based Nepalese were opportunistically screened for CVD risk factors 18 months post-earthquake (Adrega et al., 2018). An additional study described opportunistic hypertension screening and treatment after Typhoon Haiyan (Mobula et al., 2016), and Martinez et al. (2015) documented efforts to implement the WHO Package of Essential NCD care interventions in six Philippine provinces following health system destruction during the same event. Ramachandran et al. (2005) described a team of hospital-based diabetes specialists providing case finding, technical support (particularly diabetic foot care), insulin and family therapy for diabetic patients displaced by the 2004 tsunami in eastern India.
Specific framework elements
The elements of our model of care conceptual framework that were addressed in the included studies are given in Table 3. All elements of the framework were included in at least one study; however, no single study addressed every element, and there was a wide range of focus on each component.
Table 3.
Results by model of care framework elements
The symbol denotes that this component is present.
Health system inputs
All studies described at least one input for NCD care. Most studies described the cadre of health workforce who provided consultations. The majority, including all MENA facility-based models, involved non-specialist physicians supported by nurses (Yusef, 2000; Mousa et al., 2010; Mateen et al., 2012; Khader et al., 2012a,b, 2013, 2014a,b,c; Sun et al., 2013; Alabed et al., 2014; Istepanian et al., 2014; Besancon et al., 2015; Martinez et al., 2015; Collins et al., 2017; Doocy et al., 2017; Hyatt, 2017; Radwan et al., 2017; Baxter et al., 2018; Elliott et al., 2018; Saleh et al., 2018a,b,c; Abu Kishk et al., 2019; Alawa et al., 2019; Boulle et al., 2019b; Kayali et al., 2019). Santoro et al. (2016) specifically highlighted task shifting the care of uncomplicated patients to nurses under the latest UNRWA family health team reform. In another MENA region model, community health workers (CHWs) or volunteers were trained to conduct screening and/or awareness sessions (Saleh et al., 2018b,c), while, in two Lebanese studies, volunteers were recruited from the refugee community itself (Hyatt, 2017; Sethi et al., 2017). Studies from other regions with different availabilities of trained health workers (DRC and Thailand), described non-physician clinicians carrying out the roles of patient evaluation and management (Murphy et al., 2017; Saito et al., 2018; Ansbro et al., 2019). As discussed above, all studies described either community- or facility-based services within the model of care for each type of setting.
The procurement and utilization of essential, generic medications or equipment was emphasized in several studies, most basing their lists on WHO or host country guidance (Yusef, 2000; Khader et al., 2012a,b, 2013, 2014a,b,c; Besancon et al., 2015; Kallab, 2015; Martinez et al., 2015; Saadeh et al., 2015; Collins et al., 2017; Sethi et al., 2017; Elliott et al., 2018; Saito et al., 2018). In many cases, drugs were provided free to patients (Yusef, 2000; Kallab, 2015; Santoro et al., 2016; Collins et al., 2017; Sethi et al., 2017; Elliott et al., 2018; Saito et al., 2018; Boulle et al., 2019b; Kayali et al., 2019), and in many studies onsite laboratory testing was done to facilitate patient access (Yusef, 2000; Kallab, 2015; Hyatt, 2017; Elliott et al., 2018). One study emphasized the utility of examining procurement records to investigate prescribing practices and guideline adherence (Saadeh et al., 2015). Perhaps reflecting a lack of health system readiness to manage NCDs, the intervention studies strengthening existing primary care in Lebanon involved providing medicines and equipment to PHCCs, while during the Mali conflict and the response to the tsunami in India, NGOs provided both medicines and kits to the responding facilities. Two Lebanese papers mentioned drug stock outs posing a challenge, linking this to the unstable environment with fluctuant beneficiary populations, limited buffer stocks, delayed requests, and transport of supplies (Kallab, 2015; Sethi et al., 2017). Others mentioned lack of funding limiting their use of preferred medications and equipment such as insulin and glycated haemoglobin testing, respectively (Shahin et al., 2015; Saito et al., 2018), while the insulin supplied in the Indian tsunami study was donated from abroad (Ramachandran, 2005).
The use of information was discussed in 27 studies (Mateen et al., 2012; Khader et al., 2012a,b, 2013, 2014a,b,c; Istepanian et al., 2014; Besancon et al., 2015; Kallab, 2015; Martinez et al., 2015; Saadeh et al., 2015; Shahin et al., 2015; Mobula et al., 2016; Santoro et al., 2016; Collins et al., 2017; Doocy et al., 2017; Murphy et al., 2017; Sethi et al., 2017; Salazar et al., 2018; Saleh et al., 2018a,b,c; Alawa et al., 2019; Ansbro et al., 2019; Boulle et al., 2019b; Kayali et al., 2019). Many described the use of evidence-based, adapted guidelines often influenced by WHO guidance (Collins et al., 2017; Murphy et al., 2017; Ansbro et al., 2019; Kayali et al., 2019; Boulle et al., 2019b), training of HCWs (Doocy et al., 2017; Sethi et al., 2017; Naing and Bakker, 2018) and inclusion of healthy living education in their interventions (Doocy et al., 2017; Naing and Bakker, 2018; Saleh et al., 2018b; Abu Kishk et al., 2019). However, a number mentioned a lack of available guidelines and collection of basic routine health data as barriers to delivery of good quality care (Chan and Kim, 2011; Kallab, 2015). Several studies used paper-based records from individual programmes or electronic databases compiling reports from multiple facilities to characterize the NCD burden in a given crisis-affected population (Mateen et al., 2012; Saito et al., 2018; Salazar et al., 2018), while an adapted rapid assessment tool determining diabetes needs was created during the acute conflict response in Mali (Besancon et al., 2015). A small number of intervention studies explored the use of technological innovations for provider support and training or patient education, self-management, and appointment reminders (Istepanian et al., 2014; Doocy et al., 2017; Saleh et al., 2018a,b,c). These interventions were linked to improved blood pressure and glycaemic control (Istepanian et al., 2014; Saleh et al., 2018c) or improved clinician- and patient-reported clinical interactions (Doocy et al., 2017). The UNRWA studies emphasized the utility of an electronic medical record system (EMR) to track patient care and outcomes, facilitate clinical and programmatic monitoring, plan workload, and forecast drug needs (Khader et al., 2012a,b, 2013, 2014a,b,c).
Financing and governance were infrequently discussed and mainly in relation to the limitations of international funding (n = 13, 29%). In the study in Mali, the NGO had difficulty raising international donor funds for diabetes care as it was not seen as a priority (Besancon et al., 2015), while others mentioned the unsustainability of funding NCD care for NGOs and intergovernmental organizations as well as the general decrease in funding for the Syrian crisis (Mateen et al., 2012; Kallab, 2015; Alawa et al., 2019). Authors writing on the UNRWA HTN/DM model emphasized that services were provided within a narrow budget, limiting provision of certain tests and the implementation of successfully piloted community services (Shahin et al., 2015; Santoro et al., 2016). The only study to report on cost described the incremental costs from the provider perspective of introducing a formal outpatient diabetes programme in an NGO-supported hospital in the DRC. Annual total costs decreased after introduction of training and clinical and programmatic guidelines and cost per patient per year was found to be similar to the costs of HIV programs in Sub-Saharan Africa (Ansbro et al., 2019).
Patient demand and preferences
Patient demand and preferences (needs, knowledge, education, sociocultural characteristics, income, distance from care, and trust in services) was not commonly discussed, and mixed methods studies used qualitative methods mainly in an explanatory way to understand intervention outcomes (Chan and Kim, 2011; Istepanian et al., 2014; Kallab, 2015; Doocy et al., 2017; Hyatt, 2017; Murphy et al., 2017; Elliott et al., 2018; Salazar et al., 2018; Saleh et al., 2018b,c). Only Sethi et al. (2017) in describing an NCD programme for Syrian refugees in Lebanon, described involving patients in intervention design. Four studies explored patients’ disease knowledge and understanding, eliciting findings such as poor appointment adherence when patients felt well and beliefs that NCDs could be cured (Alabed et al., 2014; Murphy et al., 2017; Elliott et al., 2018; Saleh et al., 2018b). Diabetes self-management and support were improved by higher education status, previous diabetes education, and, in two examples, by having social supports in place (Murphy et al., 2017; Elliott et al., 2018). In McNatt et al.(2019), patients highlighted the aspects of different models that they valued, such as home visit services, set appointment times, and in-home monitoring equipment; patients also expressed preferences for certain drugs, with many obtaining them directly from pharmacies, forgoing consultation in order to minimize costs. They expressed frustration with the lack of access to specialists and also the potentially limited services available at NGO clinics. Sociocultural characteristics affected NCD self-management in the MENA region, whereby people were unable to follow exercise advice due to security concerns, psychological stress, or the cultural limitations to exercising outdoors, especially for women (Mateen et al., 2012; Kallab, 2015; Santoro et al., 2016; Collins et al., 2017; Sethi et al., 2017). The specific needs and provision for older people were emphasized in one paper (Kallab, 2015), while patient preferences for traditional, plant-based medicines and the use of traditional healers were described in another (Murphy et al., 2017).
Intermediate health system goals
The intermediate goals (access and coverage, quality and safety, responsiveness) received more attention. In terms of access and coverage, availability of NCD services was most commonly described (Yusef, 2000; Mousa et al., 2010; Chan and Kim, 2010, 2011; Hung et al., 2013; Sun et al., 2013; Besancon et al., 2015; Kallab, 2015; Santoro et al., 2016; Doocy et al., 2017; Hyatt, 2017; Murphy et al., 2017; Sethi et al., 2017; Adrega et al., 2018; Baxter et al., 2018; Saito et al., 2018; Salazar et al., 2018; Saleh et al., 2018a; Alawa et al., 2019; Ansbro et al., 2019; McNatt et al., 2019). Authors stressed that ensuring the presence of NCD programmes and trained HCWs was the first step in making HTN/DM services accessible. The volume of NCD services was described in a negative light, with studies referring to long waiting times causing stress for patient and providers (due to the complexities of NCD consultations or the sudden influx of a newly displaced population) or in positive terms, that is achieving the decreased volume of consultations and workload for doctors via task shifting of routine follow-up to nurses (Yusef, 2000; Kallab, 2015; Santoro et al., 2016). While multiple studies mentioned NGO-supported programmes providing free or subsidized consultations and medications to patients (Ramachandran, 2005; Shahin et al., 2015; Murphy et al., 2017; Sethi et al., 2017; Boulle et al., 2019b; Kayali et al., 2019), a number expressly addressed vulnerable groups’ ineligibility or limited affordability of accessing care through the existing health system, costs of transport and healthy diet options, or of indirect costs of clinic attendance (Ramachandran, 2005; Khader et al., 2013; Kallab, 2015; Murphy et al., 2017; Baxter et al., 2018; Naing and Bakker, 2018; Saito et al., 2018). In the Thai chronic care clinics serving Myanmar refugees, high rates of loss to follow up were attributed to the direct and opportunity costs of attending, despite offering free care, and to the refugees’ mobility, economic vulnerability, and poor understanding of the need for regular follow-up (Naing and Bakker, 2018; Saito et al., 2018).
Accessibility for remote and vulnerable communities, including the elderly, were addressed via interventions such as mobile clinics and community health workers (Yusef, 2000; Mousa et al., 2010; Chan and Kim, 2011, 2010; Sun et al., 2013; Kallab, 2015; Mobula et al., 2016; Santoro et al., 2016; Murphy et al., 2017; Sethi et al., 2017; Adrega et al., 2018; Saito et al., 2018; Salazar et al., 2018; Saleh et al., 2018a). These were particularly important for isolated communities after natural disasters (Chan and Kim, 2011, 2010; Mobula et al., 2016; Adrega et al., 2018). Three studies described the negative impact of insecurity on patient access to services (Kallab, 2015; Murphy et al., 2017; Ansbro et al., 2019); others described additional support to accommodate patient needs to attend health facility visits (Besancon et al., 2015; Murphy et al., 2017; Sethi et al., 2017; Saleh et al., 2018a; Alawa et al., 2019; Kayali et al., 2019) while limited clinic opening hours may have failed to accommodate patients, especially working males, in some settings (Kallab, 2015; Saito et al., 2018; Saleh et al., 2018a; McNatt et al., 2019). Two papers from the MENA region commented on gender-related barriers, where having predominantly male medical officers was identified as a potential cultural barrier to providing quality care, while training female refugee volunteers was seen as an advantage (Santoro et al., 2016; Sethi et al., 2017).
Patient acceptability was measured in only five included studies and was mentioned in a further five (Istepanian et al., 2014; Kallab, 2015; Hyatt, 2017; Murphy et al., 2017; Baxter et al., 2018; Saleh et al., 2018b,c; Alawa et al., 2019; Ansbro et al., 2019; McNatt et al., 2019). Syrian refugees in Lebanon reported high satisfaction with NCD care during exit interviews because services were free and provided the opportunity for screening (Kallab, 2015). High patient satisfaction was found with mobile messaging, and patients reportedly found the messages useful and easy to understand (Istepanian et al., 2014; Saleh et al., 2018b,c). In the DRC, Murphy et al. (2017) found that patients were more satisfied with diabetes care if they participated in group support sessions coordinated by the NCD clinic.
Quality (defined here as quantity, clinical quality and safety) was more widely covered (Mousa et al., 2010; Khader et al., 2013, 2014a,b,c, 2012a,b; Istepanian et al., 2014; Kallab, 2015; Martinez et al., 2015; Saadeh et al., 2015; Collins et al., 2017; Doocy et al., 2017; Murphy et al., 2017; Radwan et al., 2017; Sethi et al., 2017; Baxter et al., 2018; Damiri et al., 2018; Saito et al., 2018; Saleh et al., 2018a,b,c; Abu Kishk et al., 2019; Ansbro et al., 2019; McNatt et al., 2019). Quantity of care (the amount of care required to achieve the desired results) was not specifically discussed other than referencing a lack of adequate referral options and frequency of follow up visits (Alabed et al., 2014; Besancon et al., 2015; Ansbro et al., 2019; Boulle et al., 2019b). Those studies that examined clinical quality (skills and training of provider, his/her decision-making) focused on guideline adherence and intermediate clinical outcomes (Alabed et al., 2014; Collins et al., 2017; Doocy et al., 2017; Murphy et al., 2017; Radwan et al., 2017; Sethi et al., 2017; Saleh et al., 2018b; Boulle et al., 2019b; Ansbro et al., 2019). Safety (avoiding or ameliorating harm, including having adequate stocks of good quality medications) was rarely mentioned: Elliot et al. (2018) specifically mentioned hypoglycaemia prevention as part of diabetes self-management for patients using insulin, while several described medication stock outs.
Responsiveness of health systems to patient needs and patient centredness was relatively well covered, particularly in the papers from UNRWA (Ramachandran, 2005; Khader et al., 2012a,b, 2013; Kallab, 2015; Santoro et al., 2016; Doocy et al., 2017; Hyatt, 2017; Sethi et al., 2017; Baxter et al., 2018; Naing and Bakker, 2018; Alawa et al., 2019; Ansbro et al., 2019; McNatt et al., 2019). Examples included tailoring health awareness messages to specific audiences (men, adolescents, women) following participant feedback in Jordan (Hyatt, 2017); a program in Lebanon focusing on elderly and frail patients, minimizing the frequency of clinic interactions and travel distance, and responding to the growing NCD needs among their patient cohort by iteratively revising their care model (Kallab, 2015); and a PHCC eliciting patient priorities in designing their facility services and community outreach (Sethi et al., 2017).
Integration between and continuity within NCD care services received greater attention (Yusef, 2000; Ramachandran, 2005; Chan and Kim, 2011; Mateen et al., 2012; Khader et al., 2012a,b, 2013; Hung et al., 2013; Alabed et al., 2014; Istepanian et al., 2014; Besancon et al., 2015; Kallab, 2015; Martinez et al., 2015; Mobula et al., 2016; Santoro et al., 2016; Doocy et al., 2017; Hyatt, 2017; Murphy et al., 2017; Sethi et al., 2017; Naing and Bakker, 2018; Saito et al., 2018; Saleh et al., 2018a,b,c; Alawa et al., 2019; Ansbro et al., 2019; McNatt et al., 2019). In the emergency setting, acute referral to secondary or tertiary care following triage was mentioned (Chan and Kim, 2011; Hung et al., 2013; Mobula et al., 2016). However, several papers from the MENA region commented on the historic centralization of NCD care, fragmentation of primary care provision, and lack of continuity between health system levels and between the public and private sectors (Yusef, 2000; Istepanian et al., 2014; Kallab, 2015; Santoro et al., 2016; McNatt et al., 2019). Several Lebanon- and Jordan-based intervention studies attempted to address this issue by strengthening continuity between community-level activities and PHCCs, although only Saleh et al. (2018a) evaluated the impact of their intervention on continuity in Lebanon, finding low attendance rates at the referral PHCC appointment generated via their eHealth referral tool. While one Lebanese intervention study described successfully collaborating with a group of NGOs to strengthen primary-level NCD care delivery (Kallab, 2015), most models in the region appeared to operate in isolation from the host health system or other NGOs services. McNatt et al. (2019) emphasized the emotional, physical, and financial burden experienced by Syrian refugees as they navigated a fragmented system in Jordan, visiting several providers to fashion their own package of care. In an effort to promote consistency of care in Thailand, Burmese Border Guidelines were developed to standardize NCD and other health services among local institutions providing health services (Saito et al., 2018).
Broader policy and sociocultural context
Few studies described the broader themes surrounding national health and humanitarian policy, and sociocultural context. The existence of a national public health policy on tobacco control or action plans to tackle NCDs, diet and obesity was mentioned in a number of studies (Martinez et al., 2015; Hyatt, 2017; Murphy et al., 2017; Alawa et al., 2019). The recent evolution of the broader humanitarian NCD policy response was highlighted by the Malian response in 2012 where access to diabetes care was considered a low priority (Besancon et al., 2015), whereas, only 4 years later, Sethi et al. (2017) responded to the joint Lebanon Crisis Response Plan by transitioning from mobile medical clinics to more sustainable forms of health systems strengthening including access to NCD services. Another contrast was seen in national policy in Turkey that enabled Syrian healthcare workers who were refugees to be integrated in the health system, whereas this was not permitted in other host countries (Alawa et al., 2019). Policies promoting refugee access to NCD and other health services were also given attention in other studies from the MENA region (Mateen et al., 2012; Kallab, 2015; Santoro et al., 2016; Hyatt, 2017). The transience of certain humanitarian models was highlighted by HCWs interviewed for three MSF studies. They reported dependence on NGO expertise and expressed concern regarding the sustainability of the programme model and the potential impact of the organization’s departure (Collins et al., 2017; Murphy et al., 2017; Ansbro et al., 2019). As mentioned, several studies described cultural limitations and the impact of stress, insecurity, and poverty on the ability to exercise and access healthy food (Mateen et al., 2012; Khader et al., 2012a,b; Kallab, 2015; Collins et al., 2017; Murphy et al., 2017; Radwan et al., 2017; Abu Kishk et al., 2019), while gender roles were also discussed in relation to the appropriateness of HCWs in the MENA setting (Santoro et al., 2016; Sethi et al., 2017).
Critical appraisal
Applying the MMAT criteria to these studies revealed strengths and deficiencies in each of the different methodological approaches. There was a wide range of scores, representing the percentage of criteria met, among the studies (see Supplementary Table S4).
Quantitative studies
The majority of the quantitative studies were simple, descriptive retrospective cohort studies using routinely collected data of clinic-based cohorts. While some followed the same cohort over time, conclusions regarding intervention effectiveness were limited by a lack of comparison groups who were not receiving the intervention. No studies utilized quasi-experimental designs, such as step-wedged or interrupted time series. Only two studies justified sample size using statistical calculations (Doocy et al., 2017; Elliott et al., 2018). The second most common type of quantitative study was cross-sectional surveys. These studies generally used convenience sampling of populations attending for acute care, limiting their generalizability to the target populations and rendering them at high risk for non-response bias. Appropriate measures for HTN/DM screening and management were generally used, but some of the quantitative descriptive studies lacked statistical analysis of the outcomes reported.
Only two studies used more robust study designs: one non-blinded randomized control study involving only 12 patients tested the feasibility of the intervention (Istepanian et al., 2014), and one interventional study randomized at the facility level involving a total of 16 facilities (Saleh et al., 2018c). In the second study, the intervention and control catchment areas did not share the same baseline characteristics. Both studies reported complete outcome data and participant adherence to the assigned intervention.
Qualitative studies
Four exclusively qualitative studies were included in this review. Three used semi-structured interviews to explore issues surrounding access to NCD models of care (Baxter et al., 2018; Alawa et al., 2019; McNatt et al., 2019). An additional paper, Murphy et al. (2017), analysed a diabetes programme at a single health facility in the DRC. The researchers used approaches appropriate to the research question with well-described methods for FGDs and key informant interviews. In general, the findings from the thematic analyses of these papers appeared adequately derived from and substantiated by the data. However, the sample sizes were often small, with the exception of McNatt et al. (2019) with 68 participants. Although external interviewers were used in all except Baxter et al. (2018), the reporting did not consider whether the findings could have been influenced by the researchers’ interactions with participants.
The qualitative arms of the two mixed methods studies used appropriate qualitative approaches including FGDs (Saleh et al., 2018b) and key informant interviews (Collins et al., 2017). These studies used independent interviewers to conduct data collection, and coding and thematic analysis were performed by multiple researchers in each study. However, there were limited amounts of qualitative data analysis presented to substantiate the results.
Mixed methods studies
Among the three mixed methods studies, two used qualitative approaches combined with analytical cross-sectional methods (Collins et al., 2017; Saleh et al., 2018b), and the third used a retrospective cohort (Ansbro et al., 2019). There were shortcomings in each of quantitative and qualitative components of all three studies except for the qualitative arm of Collins et al. (2017). Although all three studies presented an appropriate rationale for using a mixed methods approach, only Collins et al. (2017) appropriately utilized and adequately reported the study’s inclusion of explanatory FGDs and key informant interviews to further explore the quantitative findings of the poor patient and provider adherence to treatment guidelines. One of the mixed methods studies provided little detail on the content or interpretation of their explanatory FGDs or patient interviews to enable us to draw conclusions on the quality of the findings or the integration of the methodologic approaches (Saleh et al., 2018b). None of the included mixed methods studies considered the limitations or possible divergence between qualitative and quantitative data.
Discussion
This systematic literature review sought to examine models of care for patients with HTN/DM in humanitarian crises. We believe it is the first review to analyse health interventions in humanitarian contexts using a ‘model of care’ conceptual framework. This framework allowed us to explore diverse models of care, using both health systems and patient-centred lenses, to provide a structured answer to calls made in previous papers to explore models of NCD service delivery for crisis-affected populations (Jobanputra et al., 2016; Aebischer Perone et al., 2017). The most common model of care described was primary care-level, physician-delivered HTN/DM services in acute and protracted conflicts in countries in the MENA region.
Despite the large increase in relevant published articles, with more than half of our included studies published since 2015, most were descriptive studies with few experimental or quasi-experimental study designs, a lack of robust study designs (or limitation to facility-based cohorts), and no studies measuring cost effectiveness (Ruby et al., 2015). The preponderance of descriptive studies and cross-sectional studies documenting the burden of NCDs among crisis-affected populations reflects, in part, the lack of basic evidence around NCD prevalence in LMICs but also the difficulties in performing high quality, longitudinal or experimental research studies in dynamic and potentially insecure humanitarian contexts (Buttenheim, 2009; Blanchet et al., 2017; Puri et al., 2017). Our inclusion of qualitative and mixed methods studies allowed examination of patient demand and experience, provider preferences, and quality in so far as these issues were covered in the literature. However, despite authors offering anecdotal lessons learned around the need for better training, the importance of data collection and analysis to support the provision of high-quality care, and the potential roles of task sharing and of community care, limited robust evidence was presented on what worked, for whom and why.
Few papers examined effectiveness. Most presented positive intermediate clinical outcome data (improved blood pressure and glycaemic control), and very few presented behavioural outcomes or hard clinical outcomes, such as death. The examples we found illustrated the benefits of eHealth, particularly use of an EMR to perform regular cohort analyses, the introduction of decision support tools to improve guideline adherence and use of SMS-based patient education and appointment reminders (Santoro et al., 2016; Doocy et al., 2017; Saleh et al., 2018b).
Our model of care framework enabled the exploration of the interactions between various health system inputs, patient factors, and intermediate and final health system goals, and it built on the primary care NCD model elements proposed by Kane et al. (2017). Elements of the framework that were common to previous conceptual frameworks, such as health system inputs, were most frequently described. This may reflect the fact that the humanitarian response has relatively recently turned its attention to the delivery of NCD care, thus most publications are describing specific, sometimes ad hoc interventions. Our findings are in agreement with previous reviews that identified gaps in reporting on intermediate goals such as quality of care (Ruby et al., 2015; Woodward et al., 2016). As the evidence base evolves, we hope to see a greater focus on quality and safety, responsiveness, and health outcomes.
Most of the models described in our review included disease screening or management delivered by medical staff at primary care facilities in MENA middle-income settings; they focused on the availability of the input components of our framework including facilities and services, essential diagnostics, medications and equipment, workforce and training of HCWs, as well as information, describing the use of standardized guidelines to improve clinical quality. Routine HTN/DM screening that was described in the UNRWA model of care and other protracted displacement contexts in the MENA region is a controversial element in the prevention and care of NCDs in humanitarian crises as there may be limited capacity to manage identified patients in an already overstretched health system in conflict and volatile contexts (Aebischer Perone et al., 2017). In the two models from Sub-Saharan Africa, routine diabetes screening was not performed, and patients were most commonly referred to the programmes after hospitalization (Besancon et al., 2015; Murphy et al., 2017).
Community-based care was not included in previous NCD models of care frameworks. Our review identified services delivered by MMUs, community health workers and outreach volunteers, which were especially useful in the emergency response setting or to serve hard-to-reach populations, such as the elderly, rural dwellers, or those in informal settlements (Chan and Kim, 2011; Kallab, 2015; Mobula et al., 2016; Sethi et al., 2017; Saleh et al., 2018c). Again, health system inputs involved in the delivery of care at the community level were most commonly described, focusing on facilities and services, medicines and equipment, and the health workforce. The utility for MMUs in crisis response we found in this review aligns with a previous non-systematic review that found that MMUs cannot be a primary model of care for the delivery of health services and should be a last resort to provide carefully chosen priority services (Du Mortier and Coninx, 2007). The role of community health workers or refugee volunteers in screening, referral, and adherence support, and it highlights the essential need to integrate these services with PHCCs and ensure continuity of care. However, all such described models were undertaken on a short-term pilot or research basis rather than being routinely integrated into care delivery, and the only study to assess the impact of community-facility referral pathways showed a poor rate of patient attendance at PHCC referral appointments (Kallab, 2015; Saleh et al., 2018a). Equally, referral pathways to hospital-level care for complications screening or management were rarely described, perhaps reflecting the high cost and poor availability of NCD referral services, which has been described in the humanitarian literature (Jobanputra et al., 2016; Slama et al., 2017; Akik et al., 2019; Boulle et al., 2019a).
The most commonly reported intermediate health system goal was access and coverage, highlighting the limited access to NCD care in affected countries, exacerbated by humanitarian crisis. The challenges in delivering chronic care that are specific to humanitarian settings were discussed in a limited number of papers. These included the interruption of care by outbreaks of acute conflict, difficulties in accessing vulnerable patient groups, and the fragmentation of the response when delivered by multiple actors, often in parallel to host health systems (Blanchet et al., 2016; Jobanputra et al., 2016; Woodward et al., 2016; Naing and Bakker, 2018; McNatt et al., 2019; Boulle et al., 2019a). We found examples of health system resilience, that is, the prioritization of interventions that allow a health system to absorb shocks, in the descriptions of the Malian acute conflict intervention and the Chinese earthquake responses (Chan and Kim, 2011; Besancon et al., 2015).
Few studies addressed the broader humanitarian or public health policy context, host health system responsiveness, or financing. Each of these components was omitted in more than half the studies. While NCDs had been neglected until recently, changing global burdens of disease and the relative increase in conflicts in the MENA region and other middle-income countries have catalyzed an increased focus on NCDs by the humanitarian sector and within the public health systems of affected countries. The development of tools such as evidence-based clinical and programmatic guidelines, training materials, and indicators has followed.
By contrast, four papers from host countries affected by the Syrian crisis discussed the changing national and humanitarian policy responses in favour of health system strengthening approaches (Hyatt, 2017; Sethi et al., 2017; Alawa et al., 2019; McNatt et al., 2019). Financing has perhaps not kept pace, reflecting the lack of donor development funding for NCDs more generally in LMICs, where most humanitarian crises occur (Spiegel et al., 2014; Nugent et al., 2018). While there is a consensus that delivery of NCD care in humanitarian settings is expensive, one study in this review included costing and illustrated the potential affordability of primary level, nurse-led diabetes care (Ansbro et al., 2019). However, further cost effectiveness, especially focusing on cost savings by preventing long-term HTN/DM complications, and patient-perspective studies documenting direct and indirect costs of NCD care, are sorely needed and patient affordability must be considered in NCD programme design.
Patient demand and needs, their experience and trust in services, and services’ accommodation to their needs were not commonly mentioned. However, some valuable lessons around care seeking, the burden experienced by patients in navigating their own care in fragmented systems, and the influence of patient or provider preferences on the fidelity of guideline implementation and patient adherence were elicited by qualitative studies that emphasized the need to understand local medical culture and context when designing care models (Collins et al., 2017; Murphy et al., 2017; McNatt et al., 2019). The need to adapt diet and exercise advice to the financial and cultural constraints of the context was highlighted, and peer support and education sessions were identified as potential solutions to supporting patient dietary and medication adherence.
Similarly, despite the growing literature advocating the development of person-centred, responsive, high quality, primary-level NCD care in LMICs, these aspects of our conceptual framework received little attention, other than in the suite of UNRWA papers (Kruk et al., 2015, 2018). Over decades, UNRWA’s primary care level HTN/DM model has evolved in response to the increasing NCD burden among their target population to encompass an integrated, family-based approach. A recent study conducted in Lebanon found that NCDs were the first cause of consultation among women of reproductive age and advocated for a family-based and life cycle approach to NCD care (Truppa et al., 2019). However, efforts to incorporate a community-based aspect, patient empowerment, and peer support have been sporadic, reportedly due to short-term project-based financing and general budgetary constraints (Santoro et al., 2016; Zoughbie et al., 2019). In this literature review, we did not focus on the integration of HTN/DM care into HIV/AIDS or tuberculosis programmes in stable LMIC humanitarian settings. As other authors have commented, there are lessons to be learned from the chronic care models and person-centred care delivery humanitarian actors have developed in response to these protracted public health crises (Harries et al., 2009; Rabkin et al., 2018). These include opportunities for HTN/DM screening (Anand et al., 2018), task sharing to nurses (Some et al., 2016), introduction of community adherence groups (Sobry et al., 2014), the need for a holistic ‘one-stop shop’ visit (Ansbro et al., 2017) as well as the need for specific guidelines, training, and consulting time for staff engaged in medical consultation, patient support, education, and counselling activities.
The Office for the Coordination of Humanitarian Affairs (OCHA) reports that more people in decades will require assistance beyond 2020, with Yemen proving the worst humanitarian crisis and Syria generating the worst refugee crisis (UNOCHA, 2019). Lessons applicable to static populations affected by prolonged crises may be learned from UNRWA and the Lebanese and Jordanian intervention studies. More work is still needed to understand how best to serve people with NCDs during an acute emergency and in unstable contexts with mobile populations.
The sustainability of some current models was questioned in a number of studies included in this review. Humanitarian actors have varying approaches regarding host health system integration and strengthening vs parallel programming. Some have called for the sustainability of NCD interventions to be considered and for handover to local health structures to occur during protracted crises (Aebischer Perone et al., 2017). Similarly, WHO has also recently emphasized the need to ‘build back better’ post-crisis (Banatvala and Small, 2020).
Implications for future research and policy
This review highlighted the need for continued research and evaluation of models of HTN/DM care in low-income countries, particularly in Sub-Saharan Africa, where availability of health system inputs such as a shortage of trained HCWs, facilities, affordable and accessible high-quality medicines and diagnostic equipment may be more limited. Prospective experimental or quasi-experimental studies, including interrupted time series studies, are needed to measure the impact of HTN/DM interventions such as community-based peer support and broader use of data-protected eHealth tools. There is still a paucity of cost-effectiveness evaluations in this field that can be used to advocate for further funding and resources for NCD care. We found few studies that addressed the domains of health system financing, broader humanitarian or public health policy context, and host system responsiveness. These are important areas for further investigation due to the increased costs in conflicts and disasters, the possibility of opposing policy stances or sociocultural beliefs, and potentially shifting health needs. NCD care in humanitarian crises may also benefit from implementation research that uses quantitative and qualitative methods that are context specific, multidisciplinary, and focus both on patient-reported outcomes and on service delivery process and outcome indicators that can help policy makers and programme implementers determine the most effective models of patient-centred care (Theobald et al., 2018).
Limitations
The focus of this review was on models of care for HTN/DM. Our search was limited to literature from 1990 onwards, due to previous reviews indicating no available studies on NCD care in humanitarian emergencies prior to 1997 (Ruby et al., 2015; Blanchet et al., 2017). Limiting to LMIC settings means we may not have reported on successful models of care for HTN/DM during natural disasters in high-income settings. The review used synthesis analysis (using the conceptual framework) and did not include a meta-analysis due to the heterogeneous study designs and methods, models of care, and outcomes of interest.
Conclusions
This systematic review described the growing body of literature studying models of care for HTN/DM in humanitarian crises. We found increasing descriptive evidence around models of NCD care. However, there were few high-quality studies and limited evidence of the impact of interventions such as guideline implementation and eHealth. The model of care conceptual framework used to guide this review allowed comparison and evaluation of diverse NCD care models across many settings and crises although there were few studies from Sub-Saharan Africa. The conceptual framework, identification of core care model components and gaps, and the results of this literature review may serve as a tool for the design, implementation, and evaluation of future NCD interventions for people with HTN/DM in humanitarian crises.
Supplementary data
Supplementary data are available at HEALTH POLICY AND PLANNING online.
Funding
This work was supported by a grant from Novo Nordisk. The funder had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Supplementary Material
Acknowledgements
We would like to thank Mr. Russell Burke, Assistant Librarian at the London School of Hygiene and Tropical Medicine, for his support in developing the systematic review search.
Conflict of interest statement. None declared.
Ethical approval: The authors’ institution provided ethical approval for the conduct of this study.
Contributor Information
Michael S Jaung, Department of Health Services Research & Policy and Centre for Global Chronic Conditions, Faculty of Public Health & Policy, London School of Hygiene & Tropical Medicine, 15-17 Tavistock Place, London, WC1H 9SH, UK; Department of Emergency Medicine, Baylor College of Medicine, 1504 Ben Taub Loop, Houston, 77030, TX, USA.
Ruth Willis, Department of Health Services Research & Policy and Centre for Global Chronic Conditions, Faculty of Public Health & Policy, London School of Hygiene & Tropical Medicine, 15-17 Tavistock Place, London, WC1H 9SH, UK.
Piyu Sharma, Department of Health Services Research & Policy and Centre for Global Chronic Conditions, Faculty of Public Health & Policy, London School of Hygiene & Tropical Medicine, 15-17 Tavistock Place, London, WC1H 9SH, UK.
Sigiriya Aebischer Perone, Health Unit, international Committee of the Red Cross, Avenue de la Paix 19, 1202 Geneva, Switzerland.
Signe Frederiksen, Danish Red Cross, Blegdamsvej 27 2100 Copenhagen Ö, Denmark.
Claudia Truppa, Health Unit, international Committee of the Red Cross, Avenue de la Paix 19, 1202 Geneva, Switzerland.
Bayard Roberts, Department of Health Services Research & Policy and Centre for Global Chronic Conditions, Faculty of Public Health & Policy, London School of Hygiene & Tropical Medicine, 15-17 Tavistock Place, London, WC1H 9SH, UK.
Pablo Perel, Department of Non-Communicable Disease Epidemiology and Centre for Global Chronic Conditions, Faculty of Epidemiology and Population Health, Keppel Street, London WC1E 7HT, UK.
Karl Blanchet, Geneva Centre of Humanitarian Studies, University of Geneva, 24 rue du Général-Dufour, Geneva, Switzerland.
Éimhín Ansbro, Department of Health Services Research & Policy and Centre for Global Chronic Conditions, Faculty of Public Health & Policy, London School of Hygiene & Tropical Medicine, 15-17 Tavistock Place, London, WC1H 9SH, UK.
References
- Abu Kishk N, Shahin Y, Mitri J. et al. 2019. Model to improve cardiometabolic risk factors in Palestine refugees with diabetes mellitus attending UNRWA health centers. BMJ Open Diabetes Research & Care 7: e000624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adrega T, Ribeiro J, Santos L, Santos JA.. 2018. Prevalence of cardiovascular disease risk factors, health behaviours and atrial fibrillation in a Nepalese post-seismic population: a cross-sectional screening during a humanitarian medical mission. Nepalese Heart Journal 15: 9–13. [Google Scholar]
- Aebischer Perone S, Martinez E, Du Mortier S. et al. 2017. Non-communicable diseases in humanitarian settings: ten essential questions. Conflict and Health 11: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agency for Clinical Innovation. 2013. Understanding the Process to Develop a Model of Care: An ACI Framework. Agency for Clinical Innovation. Chatswood. [Google Scholar]
- Akik C, Ghattas H, Mesmar S. et al. 2019. Host country responses to non-communicable diseases amongst Syrian refugees: a review. Conflict and Health 13: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alabed S, Guul A, Crighton C. et al. 2014. An assessment of diabetes care in Palestinian refugee camps in Syria. Avicenna Journal of Medicine 4: 66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alawa J, Zarei P, Khoshnood K.. 2019. Evaluating the provision of health services and barriers to treatment for chronic diseases among Syrian refugees in Turkey: a review of literature and stakeholder interviews. International Journal of Environmental Research and Public Health 16: 2660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen LN, Pullar J, Wickramasinghe KK. et al. 2018. Evaluation of research on interventions aligned to WHO ‘Best Buys’ for NCDs in low-income and lower-middle-income countries: a systematic review from 1990 to 2015. BMJ Global Health 3: e000535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amara AH, Aljunid SM.. 2014. Noncommunicable diseases among urban refugees and asylum-seekers in developing countries: a neglected health care need. Globalization and Health 10: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand T, Kishore J, Isaakidis P. et al. 2018. Integrating screening for non-communicable diseases and their risk factors in routine tuberculosis care in Delhi, India: a mixed-methods study. PLoS One 13: e0202256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansbro E, Meyer I, Okello V. et al. 2017. Evaluation of NCD service integrated into a general OPD and HIV service in Matsapha, Eswatini, 2017. Medecins Sans Frontieres Field Research, accessed 13 Dec 2020.
- Ansbro É, Homan T, Prieto-Merino D. et al. 2021. Clinical outcomes in a primary level non-communicable disease programme for Syrian refugees and the host population in Jordan: a retrospective cohort analysis using routine data. PLoS Medicine 18: e1003279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansbro ÉM, Biringanine M, Caleo G. et al. 2019. Management of diabetes and associated costs in a complex humanitarian setting in the Democratic Republic of Congo: a retrospective cohort study. BMJ Open 9: e030176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banatvala N, Small R.. 2020. Responding to Non-communicable Diseases during and beyond the COVID-19 Pandemic. https://blogs.bmj.com/bmj/ 2020/09/11/responding-to-non-communicable-diseases- during-and-beyond-the-covid-19-pandemic/, accessed 1 December 2020.
- Baxter LM, Eldin MS, Mohammed AA. et al. 2018. Access to care for non-communicable diseases in Mosul, Iraq between 2014 and 2017: a rapid qualitative study. Conflict and Health 12: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besancon S, Fall IS, Dore M. et al. 2015. Diabetes in an emergency context: the Malian case study. Conflict and Health 9: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchet K, Fouad FM, Pherali T.. 2016. Syrian refugees in Lebanon: the search for universal health coverage. Conflict and Health 10: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchet K, Sistenich V, Ramesh A. et al. 2017. An evidence review of research on health interventions in humanitarian crises. The Lancet 6736: 1–10. [DOI] [PubMed] [Google Scholar]
- Boulle P, Kehlenbrink S, Smith J, Beran D, Jobanputra K.. 2019a. Challenges associated with providing diabetes care in humanitarian settings. The Lancet Diabetes & Endocrinology 7: 648–56. [DOI] [PubMed] [Google Scholar]
- Boulle P, Sibourd-Baudry A, Ansbro E. et al. 2019b. Cardiovascular Disease among Syrian refugees: a descriptive study of patients in two Medecins Sans Frontieres clinics in northern Lebanon. Conflict and Health 13: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttenheim A. 2009. Impact Evaluation in the Post-disaster Setting: A Conceptual Discussion in the Context of the 2005 Pakistan Earthquake. International Initiative for Impact Evaluation. Washington, D.C.
- Centre for Research on the Epidemiology of Disasters. 2018. Natural Disasters 2017. Centre for Research on the Epidemiology of Disasters. Brussels.
- Chan EYY, Kim JJ.. 2010. Remote mobile health service utilization post 2005 Kashmir-Pakistan earthquake. European Journal of Emergency Medicine: Official Journal of the European Society for Emergency Medicine 17: 158–63. [DOI] [PubMed] [Google Scholar]
- Chan EYY, Kim J.. 2011. Chronic health needs immediately after natural disasters in middle-income countries: the case of the 2008 Sichuan, China earthquake. European Journal of Emergency Medicine 18: 111–4. [DOI] [PubMed] [Google Scholar]
- Collins DRJ, Jobanputra K, Frost T. et al. 2017. Cardiovascular disease risk and prevention amongst Syrian refugees: mixed methods study of Medecins Sans Frontieres programme in Jordan. Conflict and Health 11: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damiri B, Abualsoud MS, Samara AM, Salameh SK.. 2018. Metabolic syndrome among overweight and obese adults in Palestinian refugee camps. Diabetology & Metabolic Syndrome 10: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson P, Halcomb E, Hickman L, Phillips J, Graham B.. 2006. Beyond the rhetoric: what do we mean by a ‘model of care’? The Australian Journal of Advanced Nursing: A Quarterly Publication of the Royal Australian Nursing Federation 23: 47–55. [PubMed] [Google Scholar]
- Doocy S, Paik KE, Lyles E. et al. 2017. Guidelines and mHealth to improve quality of hypertension and type 2 diabetes care for vulnerable populations in Lebanon: longitudinal cohort study. JMIR Mhealth and Uhealth 5: e158–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott JA, Das D, Cavailler P. et al. 2018. A cross-sectional assessment of diabetes self-management, education and support needs of Syrian refugee patients living with diabetes in Bekaa Valley Lebanon. Conflict and Health 12: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harries AD, Billo N, Kapur A.. 2009. Links between diabetes mellitus and tuberculosis: should we integrate screening and care? Transactions of the Royal Society of Tropical Medicine and Hygiene 103: 1–2. [DOI] [PubMed] [Google Scholar]
- Hernández-Quevedo C, Papnicolas I.. 2013. Conceptualizing and comparing equity across nations. In: Papanicolas I, Smith PC (eds). Health System Performance Comparison: An Agenda for Policy, Information, and Research. Open University Press. New York, 183–222. [Google Scholar]
- Hong Q, Pluye P, Fàbregues S. et al. 2018. Mixed Methods Appraisal Tool (MMAT), version 2018. Registration of Copyright (#1148552), Canadian Intellectual Property Office, Industry Canada. Montreal.
- Hung KKC, Lam ECC, Chan EYY, Graham CA.. 2013. Disease pattern and chronic illness in rural China: the Hong Kong Red Cross basic health clinic after 2008 Sichuan earthquake. Emergency Medicine Australasia 25: 252–9. [DOI] [PubMed] [Google Scholar]
- Hyatt L. 2017. Tackling non-communicable disease among Syrian refugees and vulnerable host communities in Jordan. Field Exchange - Emergency Nutrition Network ENN 54: 69–72. [Google Scholar]
- Istepanian RSH, Mousa A, Haddad N. et al. 2014. The potential of m-health systems for diabetes management in post conflict regions a case study from Iraq. Annu Int Conf IEE Eng Med Biol Soc.. 3650–3. [DOI] [PubMed] [Google Scholar]
- Jobanputra K, Boulle P, Roberts B, Perel P.. 2016. Three steps to improve management of noncommunicable diseases in humanitarian crises. PLoS Medicine 13: e1002180–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kallab MG. 2015. Management of hypertension and diabetes for the Syrian refugees and host community in selected health facilities in Lebanon. Field Exchange - Emergency Nutrition Network ENN 68–72. [Google Scholar]
- Kane J, Landes M, Carroll C, Nolen A, Sodhi S.. 2017. A systematic review of primary care models for non-communicable disease interventions in Sub-Saharan Africa. BMC Family Practice 18: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kankeu H, Saksena P, Xu K, Evans DB.. 2013. The financial burden from non-communicable diseases in low- and middle-income countries: a literature review. Health Research Policy and Systems 11: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayali M, Moussally K, Lakis C. et al. 2019. Treating Syrian refugees with diabetes and hypertension in Shatila refugee camp, Lebanon: medecins Sans Frontieres model of care and treatment outcomes. Conflict and Health 13: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehlenbrink S, Smith J, Ansbro É. et al. 2019. The burden of diabetes and use of diabetes care in humanitarian crises in low-income and middle-income countries. The Lancet Diabetes and Endocrinology 8587: 30082–8. [DOI] [PubMed] [Google Scholar]
- Khader A, Ballout G, Shahin Y. et al. 2013. Diabetes mellitus and treatment outcomes in Palestine refugees in UNRWA primary health care clinics in Jordan. Public Health Action 3: 259–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khader A, Ballout G, Shahin Y. et al. 2014a. What happens to Palestine refugees with diabetes mellitus in a primary healthcare centre in Jordan who fail to attend a quarterly clinic appointment? Tropical Medicine & International Health 19: 308–12. [DOI] [PubMed] [Google Scholar]
- Khader A, Ballout G, Shahin Y. et al. 2014b. Treatment outcomes in a cohort of Palestine refugees with diabetes mellitus followed through use of E-Health over 3 years in Jordan. Tropical Medicine & International Health 19: 219–23. [DOI] [PubMed] [Google Scholar]
- Khader A, Farajallah L, Shahin Y. et al. 2012a. Cohort monitoring of persons with hypertension: an illustrated example from a primary healthcare clinic for Palestine refugees in Jordan. Tropical Medicine & International Health 17: 1163–70. [DOI] [PubMed] [Google Scholar]
- Khader A, Farajallah L, Shahin Y. et al. 2012b. Cohort monitoring of persons with diabetes mellitus in a primary healthcare clinic for Palestine refugees in Jordan. Tropical Medicine & International Health 17: 1569–76. [DOI] [PubMed] [Google Scholar]
- Khader A, Farajallah L, Shahin Y. et al. 2014c. Hypertension and treatment outcomes in Palestine refugees in United Nations Relief and Works Agency primary health care clinics in Jordan. Tropical Medicine & International Health 19: 1276–83. [DOI] [PubMed] [Google Scholar]
- Kruk ME, Gage AD, Arsenault C. et al. 2018. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health 6: e1196–e1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk ME, Nigenda G, Knaul FM.. 2015. Redesigning primary care to tackle the global epidemic of noncommunicable disease. American Journal of Public Health 105: 431–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levesque JF, Harris M, Russell G.. 2013. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. International Journal for Equity in Health 12: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher D, Ford N, Unwin N.. 2012. Priorities for developing countries in the global response to non-communicable diseases. Globalization and Health 8: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez RE, Quintana R, Go JJ, Villones MS, Marquez MA.. 2015. Use of the WHO package of essential noncommunicable disease interventions after Typhoon Haiyan. Western Pacific Surveillance and Response Journal 6: 18–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey E, Smith J, Roberts B.. 2017. Health needs of older populations affected by humanitarian crises in low- and middle-income countries: a systematic review. Conflict and Health 11: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mateen FJ, Carone M, Al-Saedy H. et al. 2012. Medical conditions among Iraqi refugees in Jordan: data from the United Nations Refugee Assistance Information System. Bulletin of the World Health Organization 90: 444–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNatt ZZ, Freels PE, Chandler H. et al. 2019. ‘What’s happening in Syria even affects the rocks’: a qualitative study of the Syrian refugee experience accessing noncommunicable disease services in Jordan. Conflict and Health 13: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobula LM, Fisher M, Lou Lau N. et al. 2016. Prevalence of hypertension among patients attending mobile medical clinics in the Philippines after Typhoon Haiyan. PLoS Currents 8: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Mortier S, Coninx R.. 2007. Mobile Health Units in Emergency Operations. Humanitarian Practice Network. London.
- Mousa HSA, Yousef S, Riccardo F, Zeidan W, Sabatinelli G.. 2010. Hyperglycaemia, hypertension and their risk factors among Palestine refugees served by UNRWA. Eastern Mediterranean Health Journal 16: 609–14. [PubMed] [Google Scholar]
- Murphy A, Biringanine M, Roberts B. et al. 2017. Diabetes care in a complex humanitarian emergency setting: a qualitative evaluation. BMC Health Services Research 17: 431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naing AL, Bakker M.. 2018. Challenges for migrant and cross-border populations with diabetes mellitus at Mae Tao Clinic in the Mae Sot-Myawaddy Border Region of Thailand and Myanmar. The International Journal of Lower Extremity Wounds 17: 195–6. [DOI] [PubMed] [Google Scholar]
- Nugent R, Bertram MY, Jan S. et al. 2018. Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. The Lancet 391: 2029–35. [DOI] [PubMed] [Google Scholar]
- Penchansky R, Thomas JW.. 1981. The concept of access: definition and relationship to consumer satisfaction. Medical Care 19: 127–40. [DOI] [PubMed] [Google Scholar]
- Puri J, Aladysheva A, Iversen V, Ghorpade Y, Brück T.. 2017. Can rigorous impact evaluations improve humanitarian assistance? Journal of Development Effectiveness 9: 519–42. [Google Scholar]
- Rabkin M, Fouad FM, El-Sadr WM.. 2018. Addressing chronic diseases in protracted emergencies: lessons from HIV for a new health imperative. Global Public Health 13: 227–33. [DOI] [PubMed] [Google Scholar]
- Radwan M, Sari AA, Rashidian A. et al. 2017. Influence of organizational culture on provider adherence to the diabetic clinical practice guideline: using the competing values framework in Palestinian Primary Healthcare Centers. International Journal of General Medicine 10: 239–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramachandran A. 2005. Experiences of the WHO Collaborating Centre for Diabetes in India in managing Tsunami victims with diabetes. Practical Diabetes International 22: 98–9. [Google Scholar]
- Ruby A, Knight A, Perel P, Blanchet K, Roberts B.. 2015. The effectiveness of interventions for non-communicable diseases in humanitarian crises: a systematic review. PLoS One 10: e0138303–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saadeh R, Qato D, Khader A, Shahin Y, Seita A.. 2015. Trends in the utilization of antihypertensive medications among Palestine refugees in Jordan, 2008-2012. Journal of Pharmaceutical Policy and Practice 8: 1–8: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito M, Keereevijit A, San TD. et al. 2018. Challenges to primary healthcare services in the management of non-communicable diseases in marginalised populations on the Thailand-Myanmar border: a pilot survey. Tropical Doctor 48: 273–7. [DOI] [PubMed] [Google Scholar]
- Salazar MA, Law R, Winkler V.. 2018. Health consequences of an armed conflict in Zamboanga, Philippines using a syndromic surveillance database. International Journal of Environmental Research and Public Health 15: 2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleh S, Alameddine M, Farah A. et al. 2018a. eHealth as a facilitator of equitable access to primary healthcare: the case of caring for non-communicable diseases in rural and refugee settings in Lebanon. International Journal of Public Health 63: 577–88. [DOI] [PubMed] [Google Scholar]
- Saleh S, Farah A, El Arnaout N. et al. 2018b. mHealth use for non-communicable diseases care in primary health: patients’ perspective from rural settings and refugee camps. Journal of Public Health 40: ii52–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleh S, Farah A, Dimassi H. et al. 2018c. Using mobile health to enhance outcomes of noncommunicable diseases care in rural settings and refugee camps: randomized controlled trial. JMIR Mhealth and Uhealth 6: e137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santoro A, Abu-Rmeileh N, Khader A, Seita A, McKee M.. 2016. Primary healthcare reform in the United Nations Relief and Works Agency for Palestine Refugees in the Near East. Eastern Mediterranean Health Journal 22: 417–21. [DOI] [PubMed] [Google Scholar]
- Sethi S, Jonsson R, Skaff R, Tyler F.. 2017. Community-based noncommunicable disease care for Syrian refugees in Lebanon. Global Health, Science and Practice 5: 495–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahin Y, Kapur A, Seita A.. 2015. Diabetes care in refugee camps: the experience of UNRWA. Diabetes Research and Clinical Practice 108: 1–6. [DOI] [PubMed] [Google Scholar]
- Slama S, Kim H-JJ, Roglic G. et al. 2017. Care of non-communicable diseases in emergencies. The Lancet 389: 326–30. [DOI] [PubMed] [Google Scholar]
- Sobry A, Kizito W, Van den Bergh R. et al. 2014. Caseload, management and treatment outcomes of patients with hypertension and/or diabetes mellitus in a primary health care programme in an informal setting. Tropical Medicine & International Health 19: 47–57. [DOI] [PubMed] [Google Scholar]
- Some D, Edwards JK, Reid T. et al. 2016. Task shifting the management of non-communicable diseases to nurses in Kibera, Kenya: does it work? PLoS One 11: e0145634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel P, Khalifa A, Mateen FJ.. 2014. Cancer in refugees in Jordan and Syria between 2009 and 2012: challenges and the way forward in humanitarian emergencies. The Lancet Oncology 15: e290–7. [DOI] [PubMed] [Google Scholar]
- Sun X-C, Zhou X-F, Chen S. et al. 2013. Clinical characteristics of hypertension among victims in temporary shield district after Wenchuan earthquake in China. European Review for Medical and Pharmacological Sciences 17: 912–6. [PubMed] [Google Scholar]
- Tangcharoensathien V, Mills A, Palu T.. 2015. Accelerating health equity: the key role of universal health coverage in the Sustainable Development Goals. BMC Medicine 13: 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theobald S, Brandes N, Gyapong M. et al. 2018. Health Policy Implementation research: new imperatives and opportunities in global health. The Lancet 392: 2214–28. [DOI] [PubMed] [Google Scholar]
- Truppa C, Leresche E, Fuller AF. et al. 2019. Utilization of primary health care services among Syrian refugee and Lebanese women targeted by the ICRC program in Lebanon: a cross-sectional study. Conflict and Health 13: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations High Commissioner for Refugees. 2018. Global Trends: Forced displacement in 2017. UNHCR. Geneva, Switzerland.
- UNOCHA. 2019. Global Humanitarian Overview 2020, accessed 05 Jan 2020
- Woodward A, Sondorp E, Witter S, Martineau T.. 2016. Health systems research in fragile and conflict-affected states: a research agenda-setting exercise. Health Research Policy and Systems 14: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. 2018. World Bank Country and Lending Groups Data. https://datahelpdesk.worldbank.org/ knowledgebase/articles/906519-world-bank-country-and-lending-groups, accessed 17 March 2019.
- World Health Organization. 2007. Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes. Geneva: World Health Organization.
- Yusef JI. 2000. Management of diabetes mellitus and hypertension at UNRWA primary health care facilities in Lebanon. Eastern Mediterranean Health Journal 6: 378–90. [PubMed]
- Zoughbie DE, Rushakoff JA, Watson KT. et al. 2019. A social-network behavioral health program on sustained long-term body weight and glycemic outcomes: 2-year follow-up of a 4-month Microclinic Health Program in Jordan. Preventive Medicine Reports 13: 160–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.