Abstract
The 2017 declaration of the opioid overdose epidemic as a public health emergency in the United States enhanced a national focus on effective and sustainable treatments for opioid use disorder (OUD), including multiple options utilizing medication. Despite clinical studies demonstrating efficacy, numerous reports suggest that medication for opioid use disorder (MOUD) has been underutilized, leaving many questions about specific barriers and facilitators. This study examines factors impacting attitudes and perspectives related to MOUD that influence its utilization and acceptance in a state where support for harm reduction and treatment policy has been limited. With consideration for the contextual cultural factors of this region, we conducted twelve individual interviews with people seeking treatment for OUD at a detoxification facility in Tampa, Florida. This study called attention to the perspectives of patients regarding their unique self-identified needs and beliefs around MOUD as it relates to their addiction treatment. We evaluated the perspectives collected in the interviews (N = 12) based on three main themes: 1) positive perceptions of MOUD; 2) negative perceptions of MOUD; and 3) overall perceptions of treatment and recovery. Findings suggest that participants’ varying levels of positive and negative perspectives about MOUD are informed by nuances in their social networks and varying levels of exposure or education. For example, participants held more negative opinions of MOUD than positive, accounting mostly for a view that it serves as a direct substitute for illicit opioids rather than a sustainable or supportive solution addressing the underlying causes of addiction. These opinions may be largely dependent on geographic location that dictates policy, practice, funding, and, in turn, cultural acceptance of MOUD. The findings in this qualitative study may help to inform future education efforts, initiatives addressing patient-level concerns, and provide decision-makers with meaningful information to tailor programmatic policy and procedures specific to local area social inputs and resource exposure.
Keywords: Opioid use disorder, Medication-assisted treatment (MAT), Medication for opioid use disorder (MOUD), Detoxification, Patient perspectives
1. Introduction
1.1. Background
Over the past 20 years, the number of individuals that opioid use disorder (OUD) has affected has risen dramatically. In 2017, 2.4 million individuals over the age of 12 qualified as having an opioid use disorder (Substance Abuse & Mental Health Services Administration (SAMHSA)., 2018). Also in 2017, opioid-related overdoses caused more than 47,000 deaths nationwide; a rising death toll that prompted the United States’ government to declare the opioid epidemic a public health emergency (Barocas et al., 2019; Centers for Disease Control and Prevention, 2018; Miclette et al., 2018). In 2018, opioids were a contributing factor in the death of 5576 individuals in Florida (Florida Department of Law Enforcement, 2019). While other states have seen a slight decrease in opioid-related overdose deaths, Florida’s count has continued to rise (Florida Department of Children and Families, 2018).
Florida has been historically slow in its policy responses for OUD-related harm reduction and treatment services. For example, only in 2017 did Florida become the 41st state to allow for the distribution of naloxone without a physician’s prescription, the same year that law enforcement became permitted to carry naloxone. In June 2019, after years of deliberation, legislators approved state-wide legalization of syringe exchange programs; nearly 30 years after states such as Massachusetts had allowed such programs (Infectious Disease Elimination Act (IDEA), 2019). It was not until March 2019 that the state’s attorney general publicly endorsed medication for opioid use disorder (MOUD) as a component of the state’s plan to combat OUD. Still, less than half of Florida’s substance use treatment facilities offer MOUD.
SAMHSA tracks the number of practitioners that a state certifies, who are eligible to provide buprenorphine treatment for OUD. Nationally, there are 115,086 practitioners with this waiver, but only 5422 in Florida (4.7%). To compare, in New York, a state with roughly the same population as Florida, there are 10,117; nearly double the number of eligible practitioners in Florida (SAMHSA, 2020). Additionally, as of 2018, there are only 52 opioid treatment programs (OTPs) that offer any form of MOUD in Florida. The 52 OTPs are unevenly spread among Florida’s 67 counties, with only one OTP located in a rural county. In the 10 counties with the highest opioid-related deaths, there are 30 OTPs, representing 58% of all OTPs in the state (Florida Medical Examiners Commission, 2018) but only 2 OTPs exist in the 10 counties with the highest opioid prescription rates (E-FORCSE®, 2017). OTPs in Florida are concentrated mainly in the central and southern part of the state and along the coastal regions, leaving a large portion of the state without access. More than half of the currently licensed OTPs (52%) do not accept Medicaid (Florida Department of Children and Families, 2018). In these ways, Florida is only recently applying MOUD services in ways that evidence has long supported elsewhere. The limited access to evidence-based MOUD treatment strategies may indicate a difference in cultural and community norms around MOUD acceptance and integration.
The far-reaching impact of OUD on a nationwide and statewide level has charged providers, researchers, and policy-makers with the task of finding adaptable and sustainable solutions to an issue already over-burdening the economy and disrupting communities. Engaging stakeholders across the spectrum of care in conversations about the most effective treatment approaches is an important step toward seeking solutions. Particularly, understanding the needs and perspectives of those who OUD directly impacts may help communities to contextualize and adapt evidence-based approaches in their communities with varying histories, policies, cultures, and beliefs regarding OUD treatment.
1.2. Medication solutions and barriers
MOUD (Wakeman, 2017), also referred to in the literature as medication-assisted treatment (MAT) (Connery, 2015), is an efficacious means of improving recovery outcomes for people with OUD. Used not only to manage withdrawals, MOUD also reduces the risk of relapse, improve treatment retention, improve social functioning, and reduce the risk of opioid overdose (Fullerton et al., 2014; Hser et al., 2014; Pierce et al., 2016). The Food and Drug Administration (FDA) has approved the use of three medications to treat OUD: methadone, buprenorphine, and naltrexone (Leshner & Dzau, 2019).
The positive and negative impacts of these medications can differ between individuals depending on treatment adherence and factors such as physiological dependence and withdrawal severity. Feasibility issues, such as a lack of accessibility to a provider, distance to clinic (Beardsley et al., 2003), transportation to a dosing facility, high costs, and patient or provider negative perceptions (Volkow et al., 2014), may inhibit adherence to an MOUD treatment plan. Furthermore, when adherence to the medication is interrupted, negative side-effects such as increased withdrawal symptoms or cravings may be intensified; factors that may deter patient MOUD acceptance and initial engagement (Timko et al., 2016).
With evidence that MOUD improves treatment outcomes (Fullerton et al., 2014; Hser et al., 2014; Joseph et al., 2000; Pierce et al., 2016; Sullivan et al., 2019; Volkow et al., 2014), researchers have indicated a need for a cultural shift toward patients’ and providers’ fully adopting medications as treatment, such has taken place for other chronic diseases (Kelly et al., 2015). Leaders in the field have suggested that this change could be supported with consistent use of inclusive and person-first language among practitioners. This acts as the rationale for transitioning away from terminology such as “medication-assisted treatment”, which indicates that medication does not qualify as complete treatment, to “medication for opioid use disorder”, which indicates medication as a stand-alone treatment approach (Wakeman, 2017).
Several other factors impact patients’ of MOUD (Uebelacker et al., 2016), including an individual’s comprehension of their treatment options, the feasibility of their treatment plan requirements, and their level of acceptance for using medication to support their recovery. Despite evidence of clinical efficacy, patients and providers have long seen medication as a controversial treatment modality (Jerry & Collins, 2013). Social and self-stigma associated with the etiology of addiction (i. e., addiction as a result of choices or values [Heyman, 2013] versus the idea that addiction is a disease [Volkow et al., 2016]) have fueled this controversy. Such controversy is also charged with the belief that recovery is achieved through abstinence that would be precluded with the use of agonist-based medication (Notley et al., 2015). A lack of public education around the mechanisms and efficacy of MOUD may also account for the decreased awareness and increased stigma associated with medication for a person addicted to substances (White, 2012).
1.3. A call to improve MOUD programs
Existing literature has stated the need for work that focuses on the beliefs and perspectives of people with OUD about the use of MOUD. For example, Uebelacker et al. (2016) suggests that MOUD program enrollment could benefit from a deeper understanding of individuals’ beliefs to more accurately address misconceptions and challenges associated with it. Others suggest that future qualitative research should address personal and social stigma associated with the intervention option, and involve people who are in need of feasible treatment solutions (Madden, 2019). This could help treatment providers to better attend to and understand their own patients’ attitudes to improve medication engagement and adherence. Efforts to facilitate increased patient autonomy, accountability, and involvement in treatment decisions, could result in improved treatment outcomes (Gruman et al., 2010; Mullins et al., 2004; Warden et al., 2012).
One study has focused on the perspectives of people transitioning from OUD detoxification to aftercare services, but it only provides a limited evaluation of individual-level facilitators and barriers specific to the use of medication (Stein et al., 2017). An in-depth qualitative analysis devoted specifically to patient perspectives is important for contextualizing the existing quantitative evaluations of MOUD. Specifically, a deeper understanding of these perspectives may allow providers to tailor efforts to engage patients in MOUD program enrollment and retention following detoxification (Rieckmann et al., 2007; Roman et al., 2011; Uebelacker et al., 2016). Such efforts may also help to inform more systematic interventions intended to improve patients’ buy-in. The current study, then, functions as an initial phase in understanding patients’ views about MOUD before researchers conduct larger studies that test novel approaches for advancing the acceptance of and engagement and retention in MOUD programs. Prior efforts in the field and gaps in the existing literature have informed the questions that this study addresses.
1.4. Current study
We conducted this qualitative study at a locked inpatient detoxification facility in Tampa, Florida, at which the facility initiated in July 2017 a new “medication assisted treatment” program to support patients with OUD during detoxification and after-care treatment. We conducted this study with an additional intention of providing pilot data for a randomized controlled trial (RCT) that the Centers for Disease Control and Prevention (CDC) was to fund at the same treatment site. The larger RCT tests an innovative technology and person-centered intervention for addressing engagement and retention in buprenorphine-based MOUD (Schuman-Olivier et al., 2018). The information collected from this current study is intended to inform patient-centered education and engagement efforts in preparation for the implementation of the intervention the CDC was to evaluate. The research questions addressed in this study focus on patients’ perceptions of MOUD in general, not limited to any one type of medication (i.e., methadone, buprenorphine, or naltrexone.) The research questions are: 1) What are the perspectives of patients in a detoxification facility in an area of low MOUD access? and 2) What are the barriers and facilitators of MOUD utilization for patients in treatment for OUD? We hypothesized that: 1) there will be a higher frequency of negative perspectives than positive perspectives concerning the use of MOUD; 2) MOUD will primarily be perceived as useful for detoxification but as a substitute for illicit drugs when used as a maintenance therapy; and 3) familial, social, and cultural influences will be key indicators of patients’ positive perceptions of MOUD.
2. Methods
2.1. Study design
We selected a qualitative design to directly collect and evaluate patient perspectives as a means to provide insight on the factors that contribute to their negative or positive perceptions of MOUD. We conducted twelve (N = 12) one-on-one semi-structured interviews, allowing for participants to speak to their recovery choices and considerations of post-detoxification next-steps and treatment planning, including MOUD options. All procedures that we performed in studies involving human participants were in accordance with the ethical standards of the University of South Florida’s Institutional Review Board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. We obtained informed consent through recorded verbal consent from all individual participants involved in the study. All participation was voluntary, and we did not compensate participants in an effort to avoid undue inducement of responses or perceptions of coercion.
2.2. Setting
The MOUD program at the study site, referred to as their “MAT” program, consists of two options for people with OUD upon discharge from the detoxification facility; 1) monthly long-acting naltrexone injections; or 2) daily, in-person, on-site supervised buprenorphine (BUP) dosing. (Methadone is available at other treatment facilities in the area though not at the study site.) In theory, these two medication options are made available to all eligible patients with OUD. However, the majority of these patients do not adhere to their treatment plans after discharge from inpatient detoxification, particularly when the treatment plan involves MOUD. The study location, based on intake data from 2018, admitted approximately 2000 patients to inpatient detoxification with an opioid use disorder, consisting of about 500 involuntary patients and 1500 voluntary patients, approximately 25% of whom were homeless. Nearly half of the total 2000 opioid use disorder patients who were admitted to inpatient detoxification left inpatient detoxification against medical advice and therefore were ineligible for outpatient MOUD treatment. According to an evaluation of electronic health records for the first 10 months of the “MAT” program, only approximately 8% of all OUD patients enrolled in the BUP program for any length of time. Nationally, the average rate of BUP retention is 50% at 6 months, significantly higher than what we observed at this treatment site (Pierce et al., 2016). This comparison offers rationale for the current study, demonstrating the need to more deeply understand how perceptions of MOUD may be uniquely affecting utilization and treatment engagement.
2.3. Participants
We conducted a total of twelve individual interviews between November 2018 to May 2019. We recruited participants through convenience sampling. They were adults (18+), four females and eight males, within the inpatient detoxification program, and we identified them through the daily patient census by their drug of choice (opioids), physical well-being, and willingness to participate in interviews. An agency employee asked each participant if they would like to be interviewed and the interviewer asked them again before the interview commenced. We excluded potential participants if their primary drug of choice was not opioids, or they vocalized any unwillingness or hesitation to participate. The study sought to explore the general perspectives of a diverse set of patients, without intent to stratify results based on specific demographic or individual descriptive factors. Given this generalized enrollment strategy, we conducted interviews until we achieved saturation of topics, which repetition of responses indicated (Fusch & Ness, 2015; Guest et al., 2006; Saunders et al., 2018). This resulted in 12 completed participant interviews.
2.4. Data analysis
A third-party secure transcription company professionaly transcribed the recorded interviews (ranging between a length of just more than 10 min to 27 min). The research team made edits to the transcripts and uploaded the finalized transcripts of all 12 individual interviews to Atlas.TI, a qualitative data analysis software (Dowling, 2008). Through a grounded theory approach (Creswell & Poth, 2016), we used an inductive thematic analysis to evaluate the interviews and transcriptions for meaningful themes and concepts based on reflections from existing empirical evidence (Guest et al., 2012). In addition to a thematic analysis, a content analysis allowed for an assessment of participant perceptions based on the frequency and context of the emerging concepts (Vaismoradi et al., 2013). While not a proxy for significance, and not within the traditional scope of grounded theory methodology, the content analysis has been offered as a quantitative supplement to contribute to a deeper understanding of participants’ perceptions.
The analysis took place through a six-phase process that included familiarization with the data, open coding and defining axial codes, achieving inter-rater reliability, coding all transcripts, establishing themes, and finally identifying quantitative patterns through analyses of code frequencies. First, three members of the research team (A.S., M.C., and V.H.) listened to the audio recordings of each interview at least once and read through the transcripts at least twice to familiarize themselves with the data. Through this process, they created a list of open codes. They compared and contrasted open codes to remove redundancy and account for unique patterns resulting in a list of mutually agreed upon axial codes with definitions. Before they coded transcripts, they achieved inter-rater reliability at 90% by individually coding the first four pages of the first transcript and then comparing results. All three researchers collectively coded the transcripts to achieve unanimity and full immersion in the content of the interviews for a thorough analysis process. They discussed discrepancies in coding until they came to a unanimous decision and made clarifications, as needed. During the axial coding process, it became clear that in addition to just negative or positive perceptions of MOUD, participants had meaningful perceptions about recovery in general that may play a role in their perceptions of MOUD even if not directly stated. In response, with consideration to the research questions and a review of the literature, the team identified the three overarching themes, 1) Positive perceptions of MOUD; 2) Negative perceptions of MOUD; and 3) Overall perceptions of treatment and recovery. We further evaluated the frequency of codes to reveal patterns in participants’ perceptions and we identified explicative quotes and earmarked them for use in the results section.
Using the codebook of 70 codes, we coded a total of 533 separate quotations within the 12 individual interviews. There was a frequency distribution between themes of the following: negative perceptions of MOUD with 180 utterances (33.8%), positive perceptions of MOUD with 134 utterances (25.1%), and overall perceptions of treatment and recovery with 219 utterances (41.1%). The themes and the most frequently occurring axial codes can be seen in Fig. 1.
Fig. 1.
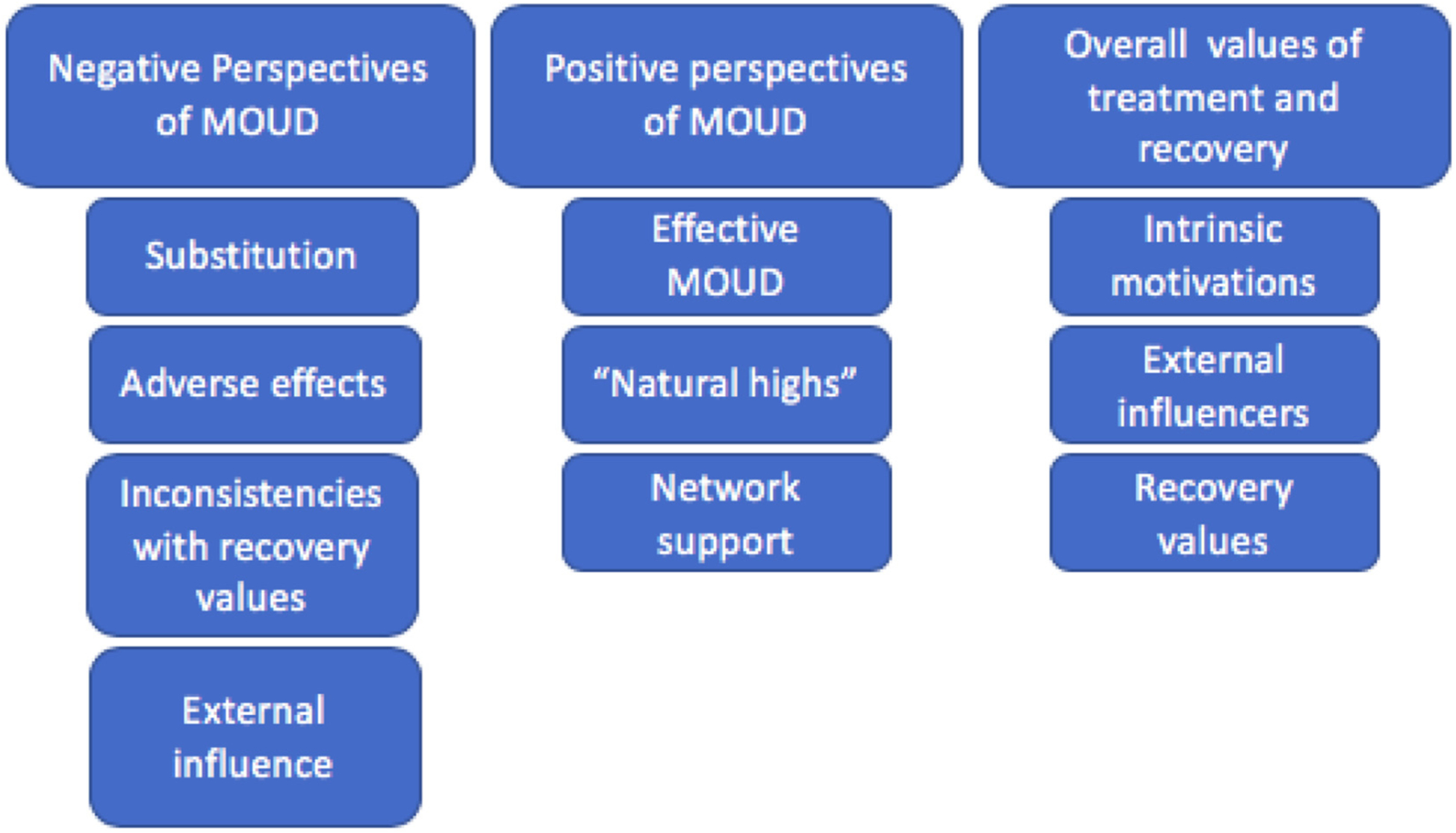
Themes and axial codes.
3. Results
Of the 12 participant interviews, seven of them had a higher frequency of codes for negative perceptions of MOUD than positive perceptions of MOUD. Additionally, for seven of the participant interviews, the highest frequency of codes was for general perceptions of treatment and recovery (see Table 1). The negative perspectives of MOUD theme evaluated the perceived challenges and barriers preventing the utilization and acceptance of MOUD as a recovery modality. The main codes that we explored in the results for this theme were: substitution (mentally and physically), adverse effects, recovery values, and external influence.
Table 1.
Proportion of codes by theme per participant.
| Participant # | Negative codes | Positive codes | General codes | Total | |||
|---|---|---|---|---|---|---|---|
| Count | % of total | Count | % of total | Count | % of total | ||
| 1 | 9 | 60% | 4 | 27% | 2 | 13% | 15 |
| 2 | 7 | 24% | 10 | 34% | 12 | 41% | 29 |
| 3 | 1 | 7% | 9 | 60% | 5 | 33% | 15 |
| 4 | 8 | 44% | 0 | 0% | 10 | 56% | 18 |
| 5 | 2 | 25% | 5 | 63% | 1 | 13% | 8 |
| 6 | 4 | 14% | 11 | 39% | 13 | 46% | 28 |
| 7 | 5 | 25% | 2 | 10% | 13 | 65% | 20 |
| 8 | 10 | 45% | 2 | 9% | 10 | 45% | 22 |
| 9 | 8 | 42% | 7 | 37% | 4 | 21% | 19 |
| 10 | 0 | 0% | 7 | 33% | 14 | 67% | 21 |
| 11 | 10 | 38% | 5 | 19% | 11 | 42% | 26 |
| 12 | 6 | 29% | 5 | 24% | 10 | 48% | 21 |
The positive perceptions of MOUD theme evaluates how MOUD supported the participants’ lives and treatment experience, highlighting the perceived benefits and acceptance of MOUD as an option. While coded utterances within the positive theme had the lowest frequency among all three themes, the code “belief that MOUD works” still accounted for 4.9% of the overall codes and was indicative of a participant’s positive perception of MOUD. The three main codes that we explored within this theme included: effective MOUD (physically and mentally), “natural highs”, and network support.
Participants’ perspectives categorized into the overall values of treatment and recovery theme emerged as a significant component of all conversations even when not directly related to their experiences with or beliefs about MOUD. The findings related to this theme were integral to understanding the mindset from which participants’ beliefs about MOUD originated and contextualized participants’ intentions regarding their own individualized treatment processes. This theme accounted for the highest frequency and included coded utterances that described each participant’s overall recovery process, needs, challenges, and goals not necessarily related to MOUD. The codes for this theme consisted of: intrinsic motivations, external influencers, and recovery values. Findings from all three themes and their codes, along with exemplary quotations, are described in depth in the following sections.
3.1. Negative perceptions of MOUD
3.1.1. Negative perceptions - substitution (mentally and physically)
The code “MOUD as a substitute” had the highest frequency, accounting for 26.1% of the coded utterances within the negative theme and 8.8% of the overall coded utterances. The perspective that MOUD served as a substitute to illicit drugs was most common but involved complex nuances and we established it as a separate grouping within the analysis process. First, participants presented the idea of substitution as a psychological challenge; MOUD allowed a person to function but seemed to do so at the cost of dependence on external means and misaligned with perceptions of complete rehabilitation. Some participants explained that they or others would use medications to supplement illicit drug use in pursuit of a high. There were references to MOUDs as “just another drug” and the idea that opting into MOUD was a “crutch”, a means to continue drug using behaviors, and a distraction from tending to the root causes of their addiction. Some participants valued MOUD as a substitute for other drugs during a period of detoxification in transition to abstinence but felt negatively about using it as a means of maintenance therapy.
I didn’t like the way it gave me the same feeling. It was the same routine as when I go get me a heroin bag in the morning. I can’t function and I can’t walk, but I can walk to the spot and get me a ten-dollar bag. A bag, you know? It was the same thing. Waking up, I can’t walk, but I’m going to go get my dose and come back. It’s the same thing.
In the end of the day, you’re trading one for another, and you’re still on a leash. You’re still controlled by this opiate, so all that it is, is an opiate. At the end of the day, you’re taking an opiate. The day you get them all out of your system, and learn to live life without them, then that’d be the best thing. That’s what I think.
It is a substitute. It’s not a solution. It’s not a fix-all. It’s not going to fix anything. It’s more or less a pharmaceutical company’s way of gaining more money through this epidemic, in my opinion. I mean, I would rather someone take Kratom than take a pharmaceutical pill that’s basically the exact same thing as the heroin that they’re putting in their body, or the Oxys that they’re taking, I mean it’s the same thing. Buprenorphine is an extremely powerful opiate, so what’s the difference?
Seven of the participants acknowledged that MOUD served as a substitute in a way that detracted from their recovery goals. Of these seven participants, six of them had a greater frequency of negative perceptions of MOUD than positive perceptions. One participant did have a greater frequency of negative perceptions than positive perceptions but did not acknowledge substitution as a contributing factor to this negative perception (participant 11).
3.1.2. Negative perceptions - adverse effects
Many of the coded utterances highlighted concerns about the adverse effects of MOUD. These concerns included practical implications such as the high cost of the medications as well as physical side effects such as amplified withdrawals, struggles with appropriate titration, and feelings of dependence or cravings. Several participants distinguished the significant physical impacts specifically when trying to titrate off of MOUD; they compared withdrawals to being worse than what they experienced during the detoxification process from their drug of choice. Some took pride in successfully detoxing from other drugs and felt that reverting to the use of MOUD would set them back after they had already accomplished what they felt was “the hardest part.”
So, if you take that for at least a month, now it’s built up in your systems. It’s connected to your bones. It’s attached itself to places to where it’s going to be there for at least a month after you stop taking it. So, for a month, you’re going to go through a severe withdrawal. Heroin’s withdrawal isn’t shit compared to Methadone and Buprenorphine withdrawal. So, imagine what the person is going to do within that months’ time. We only have to withdraw for a week off of heroin, Oxys, Percs, Vicodins. It’s a week, a week max. Now, theirs is going to be a month of that. So, just imagine, what do you think that person is going to do? Do you think they’re going to go get high? Do you think they’re going to want to take that pain away, knowing it’s going to be a month long?
Eight of the twelve participants acknowledged the physical adverse effects of MOUD, which consisted of all seven of the participants who voiced their perceptions of MOUD as being primarily negative and included one participant who had a primarily positive perception of MOUD (participant two).
3.1.3. Negative perceptions - recovery values
The third grouping within the negative theme was based on participants’ idea that MOUD was inconsistent with recovery values. This included perspectives that MOUD manifested a reliance on external means that were inessential and not dependable. They questioned what would happen if their access was limited, if they suddenly could not pay, or even if it became illegal; they were wary of a version of recovery that required so many stipulations and trust in a system that they could not control.
Yeah, I mean, it might bring you joy while you’re on it, while you’re taking a maintenance program, but like I said, what if the clinic disappears? What if you can’t afford your daily dose? There’s so many variables or factors that play into it that just, as opposed to you coming here, going to rehab, and just being done.
Four of the 12 participants spoke directly to MOUD being inessential, not dependable, or influenced by a corrupted system. All four of those who mentioned these factors had a greater frequency of negative attitudes than positive (participants number one, eight, nine, and eleven.)
3.1.4. Negative perceptions - external influences
The fourth grouping, external influence, included participants’ idea that their family or other social support would disapprove of their use of MOUD. Some participants stated that the stability of their basic needs was reliant on their familial support that would be in jeopardy should they pursue a treatment modality that was not approved. In this way, they did not feel like the choice to pursue MOUD was theirs to make. The concept of disapproval from others was tied to statements about the social stigmas associated with a non-abstinence-based recovery as well as practical access to groups or programs that accepted an MOUD approach. Participants stated that community-based treatment programs and groups like AA and NA did not allow people on MOUD to participate.
Anything that brought you joy in life, prior to use of drugs, no longer brings you joy without the presence of drugs, and then eventually even with the drugs, those things no longer bring you joy. The only thing that brings you joy is the drug. So, it’s the same thing with Methadone, Buprenorphine, and all that. So, how does it really help somebody get back to a normal healthy life if they need these things to bring them joy?
I even called my dad to see if he could bring the $40 up, so I could do the suboxone instead of the other one that they give you [in inpatient detoxification]. And he talked to my stepmom, and my stepmom basically just told him, and he told me that I was changing out one drug for another one, is how they looked at it. Because that can be addictive, too, and so he was like, “You’re going to feel shitty, whatever, you know, just deal with it.”
There were four participants who spoke to challenges related to external influences such as family or network disapproval. Three of those four were more likely to report a majority of negative perceptions of MOUD over positive perceptions (participants number seven, eight, and eleven) with one participant voicing external influence as a negative factor but still having an overall positive perception of MOUD (participant number two).
3.2. Positive perceptions of MOUD
3.2.1. Positive perceptions - effective MOUD (physically and mentally)
Some participants perceived the effectiveness of MOUD as a physical and mental benefit. Most commonly, participants voiced that they perceived, observed, or experienced MOUD to prevent relapse by helping to avoid craving, making them feel safer from overdose, and managing withdrawal during or after inpatient detoxification. Participants also described MOUD as being helpful in facilitating rehabilitation for daily functioning and improved quality of life. For example, they perceived it to support job acquisition and sustainability, renewed relationships with loved ones, and a realignment with personal and moral values.
Well, for me it’s just withdrawals. I really don’t like withdrawing and I feel like Suboxone just helps with that a lot. And then, when you withdraw from Suboxone it’s not as … the withdrawals from Suboxone is not as bad as opiate withdrawals.
It helps the cravings go down a bunch, and it’s safe, very safe. So, there’s not a need to go out into the street and go shopping, to self-medicate. It’s also affordable. Three dollars a day is not bad. It’s beneficial. It’d be something, with the buprenorphine, that I would recommend it to a lot of people.
Eleven of the twelve participants, all but participant number four, acknowledged the efficacy of MOUD as a positive factor.
3.2.2. Positive perceptions - “natural highs”
The grouping “natural highs” was derived from participant’s descriptions of the type of life they hoped to lead with MOUD. Participants framed their mission to attain joy, success, meaningful relationships, contributions to society, and stability as the pursuit of a “natural high” or non-drug-related means of sustainable quality of life. Among those participants who vocalized that MOUD could help them to achieve such goals, there was a specific recognition that it may improve their daily functioning by providing accountability and a structured routine. Despite that MOUD involves the use of a medication-based solution, the intention to seek fulfilment and life satisfaction without the desire to get high was a distinguishing factor between those who perceived MOUD to be negative versus those who perceived it to be positive. “Success. Money. Family. Civility. No longer a need for drugs. Just a natural high.”
It worked great. I didn’t have the urges throughout the day that I would normally. Like, being at work, or even being at the gym. The gym, especially after I left the gym, that was my biggest time because your endorphins are down, your insulin drops after you work out, so you’re looking for something to boost yourself back up. It’s just a way I used to maintain… When I was on methadone, I didn’t have the urge. I’d leave, I’d go back to work, I’d stay focused. My mind, it wasn’t pulling on the back of my head, like, I need to go use, I need to go use, I need to go use.
Seven of the participants spoke to these factors, three of whom had a greater overall perception of MOUD as positive (participants number three, six, and ten). Four of those who acknowledged the benefits of MOUD for this theme had an overall greater frequency of negative perceptions of MOUD (participants number eight, nine, eleven, and twelve).
3.2.3. Positive perceptions - network supports
Network support was the third and final grouping within the positive theme. For those who found MOUD to be a positive component of their recovery or a potentially viable solution described having familial or social networks that were supportive of the use of medication in treatment. Some participants described knowing others or having loved ones who had benefited greatly from MOUD and had encouraged them to pursue it themselves. “I had a grudge against my mother. She put me on this. Every day I wake up, I’m just like, this is for the best.” “I mean, it’s been good. I’ve met some nice people here, to keep in contact… They’re trying to stay clean too.”
There were four participants who acknowledged that family or social networks were positive influences, three of whom had a greater frequency of overall positive perception of MOUD than negative perceptions (participants number three, five, and ten) with one participant who had an overall negative perceptions of MOUD over positive perceptions (participant number one).
Participants also perceived as a benefit the idea that therapeutic support was a component of an MOUD program. As mentioned previously, participants commonly described participation in therapeutic services as a facilitator of general recovery success; some participants recognized that a key component of their engagement in an MOUD program would include either group or one-on-one counseling support.
The first time I did it, it was a very important part of my life because of the fact that I was accounted for, coming here every single day, and doing the group, and getting medication, which was important too.
Three participants described the therapeutic component of MOUD as a positive factor, two of whom had an overall greater positive perception of MOUD (participants number two and 10) and one who had an overall greater negative perception of MOUD (participant number nine). Outside of these three subgroups of positive perceptions of MOUD, the data indicated that participants who vocalized internal motivations as well as personal accountability or a readiness to change when expressing their general perceptions about treatment, also vocalized a higher prevalence of positive perceptions of MOUD as a maintenance therapy. Six participants acknowledged this internal motivation, four of whom had overall higher positive perceptions of MOUD than negative perceptions (participants number two, three, six, and ten). There were two participants who acknowledged these positive factors but still had an overall higher negative perception of MOUD than positive (participants eleven and twelve.)
3.3. Overall values of treatment and recovery
3.3.1. Overall values - intrinsic motivations
First, intrinsic motivations described the participant’s internal reasons for pursuing addiction treatment, including feelings of readiness; a sense of accountability for their actions in the past and desires to change in the future; as well as desires for normalcy, stability, and productivity
Tired of being lonely, tired of wondering how you’re going to get the next fix. You’re tired … you’re just tired of all the bullshit. You got to be tired, that’s it. It’s a mental thing. I mean, it’s like people eat too much, people shop too much. You got to be tired of seeing those final notices or seeing the way people look at you when you walk through the mall. You got to be tired of it. You have to want to change. You just have to want it. That’s it.
Yeah I want to live life bro. You know how long it’s been since I sat down and went to the movie theaters? Or I’ve sat down in a restaurant and ate a meal? You know how long it’s been since I’ve done that? Or gone to the beach and just walked it. You know? Nothing. Nothing. Nothing. My life is boring. I get high, I close the door at my house, I stay home all day, that’s it. That’s no life.
Ten of the twelve participants discussed components of their intrinsic motivation in reference to their general plans and desires for treating their OUD.
3.3.2. Overall values - external influences
Participants described external stressors, such as financial and housing instability, as barriers to treatment access and retention but also as reasons for wanting to pursue treatment in the first place. Similarly, participants cited familial support, the expectations of others, and social norms as being limiting in certain circumstances but as facilitating in others. Participants widely cited mental health issues as a challenge to treatment and an underlying cause of addiction. Participants commonly cited the need for their mental health treatment to take precedence over treatment for their addiction but recognized a causational relationship between them. “Like I said, I take psych medications and they improve me… And that’s one of my problems, I always relapse. So I stopped taking them, and I need them.”
Nine of the twelve participants discussed external influences that impacted their pursuit of treatment and recovery either negatively or positively. They recognized family influence as both a motivator for changing their behaviors and as a root cause of the challenges that brought them to addiction in the first place.
3.3.3. Overall values - recovery values
The third grouping within this theme was related to recovery values. Participants described their perspectives on what is required and expected to achieve addiction recovery for themselves and for others. For example, participants had a common conception that recovery required abstinence, though there was not a consensus about whether MOUD was acceptable in an abstinence-based treatment approach. Participants repeatedly voiced a use of therapeutic support as a primary resource for recovery. Participants did not make a distinction between group therapy or one-on-one therapy, rather they recognized any means to intentionally address mental and emotional well-being as a priority independent of a participant’s disclosure about their own mental illness.
Getting the therapy, talking with the therapist, getting on psych meds for my depression, and just being able to, I guess, figure out my trigger points. Which I know was mostly all my depression, was what it was. So just getting that controlled, and then making sure that I’m not going around back where I was when I leave there.
Additionally, many participants noted the utility of groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA). A few participants relied on the groups as consistent recovery communities and found success through the support of their sponsors. Others found that the mutual-help groups were misaligned with their values and noticed that the expertise of their sponsors was limited (Kelly & Yeterian, 2011).
It’s just the simple fact that you have AA. You have NA, and it’s actually a very strong unity. It’s what I took, so … And I’ve seen it help a lot of people. I’ve seen people I didn’t believe would stay sober, still sober.
That’s the other problem is you go like, they’re like, “Go to NA, go to AA, go to NA,” but then you get a sponsor and they’re like, “Oh you’re on suboxone? Well I don’t know if I can sponsor you because you’re on suboxone.”
Ten out of the twelve participants discussed their recovery values and specific beliefs around the type of recovery that was best suited for them.
4. Discussion
Findings from this study highlight the complexity of factors that influence the perspectives and attitudes of patients toward MOUD. Existing literature that considers patients’ attitudes toward MOUD has similarly found a variation in stated preferences for the use of medication (Bergman et al., 2019; Hewell et al., 2017). Some concluded that these preferences influence the likelihood of initiation in MOUD, particularly in engagement after detoxification (Uebelacker et al., 2016; Yarborough et al., 2016). Preference for utilizing a particular form of MOUD compared to others has been shown as a predictor of more positive attitudes for MOUD in general (Uebelacker et al., 2016), and studies show a significant preference for buprenorphine treatments over methadone treatments (Schwartz et al., 2008). A reason for this preference is the structural barriers that result from the methadone treatment program design that typically requires more in-person dosing and monitoring, the associated stigma, and the fear of methadone withdrawal (Uebelacker et al., 2016; Yarborough et al., 2016). Notably, the program under consideration in this study offers a buprenorphine option that is structured similarly to a traditional methadone maintenance program, with daily witnessed in-person dosing, posing similar structural barriers such as time, transportation, scheduling conflicts, child-care needs, and so on. This study found that the rigidity of the programmatic dosing procedures, support and wrap-around services being inaccessible, and a sense of unreliability left patients with a feeling of distrust in the system of care and particularly distrust of MOUD. Prior work—which has showed that patients’ skepticism of MOUD can be grounded in stigma and real inconsistencies in service delivery—supports this finding (Bergman et al., 2019; Rieckmann et al., 2017; Wakeman & Rich, 2018).
Prior research has also already explored whether gender, race and ethnicity, and history of using medication are indicators of preferences for MOUD. For example, one study found that women were more likely to be interested in methadone and naltrexone treatment options over buprenorphine compared to men, and that African Americans were more likely to state a preference for methadone or naltrexone over buprenorphine than other racial/ethnic groups. This same study did not find a significant association for any of the three medication options for those with a history of using that medication (Uebelacker et al., 2016). While past research has emphasized a need for improving access and education for MOUD and indicated individual-level factors that may predict preferences for MOUD, the current study contributes to the need for a deeper understanding of patients’ perceptions based on their values, relationships, experiences, and cultural norms (Schwartz et al., 2008; Uebelacker et al., 2016).
People seeking meaningful treatment for an active OUD are often marginalized and stigmatized rather than engaged in problem-solving efforts (Madden, 2019). The diversity of patients’ recovery priorities, social and support networks, accessibility and resources, and personal values all potentially impact their utilization and acceptance of MOUD (Knudsen et al., 2011; Kumar et al., 2020; Rieckmann et al., 2007; Rigg & Murphy, 2013; Sigmon, 2014). This study provided an in-depth exploration of these factors, underscoring patients as key stakeholders in this conversation. The data collected in this study countered common societal perceptions that people with OUD may not know what is best for themselves; findings demonstrated their self-awareness and accountability, their acknowledgement of a system that does not always work in their favor, and the deep work necessary to sustain a meaningful and fulfilling life of recovery.
We had hypothesized the following: 1) there will be a higher frequency of negative perceptions than positive perceptions concerning the use of MOUD; 2) MOUD will primarily be perceived as useful for detoxification but as a substitute for illicit drugs when used as a maintenance therapy; and 3) familial, social, and cultural influences will be key indicators of a patient’s positive perceptions of MOUD. Our findings strongly supported hypotheses one and three and although our findings did not strongly support the second hypothesis, our findings still meaningfully contribute to existing and future literature.
The higher frequency of negative perceptions of MOUD compared to positive perceptions supported the first hypothesis, thereby highlighting the need for targeted interventions aimed at improving the acceptability of MOUD. The relationship among community attitudes toward MOUD, the attitudes’ effect on patient demand for MOUD, and availability of prescribers willing to get waivers to prescribe buprenorphine in regions like the ones we studied need to be further examined (Louie et al., 2019).
Results related to the second hypothesis were more complex; some participants preferred the use of MOUD only as a facilitator of safe and comfortable detoxification, while others found it to be acceptable as a maintenance therapy. Although some voiced that the use of medication for maintenance was not their personal choice, they stated that they would not disparage or judge others who might choose a medication maintenance option. The overall perception was that medication maintenance would be best in cases where all other treatment options had been exhausted. Research should further explore this cognitive dissonance between treatment options that participants prefer for their own recovery versus what they thought would be best for other people.
Last, the third hypothesis was repeatedly indicated in the findings that familial and social relationships influenced patients’ acceptance of MOUD. Future work should acknowledge the cultural norms of patients’ communities, and the influence of peers, providers, and family members as key factors affecting integration of MOUD into local policy and practice. We recommend that future efforts be made to engage the social networks of people seeking treatment and that providers educate family.
4.1. Limitations
One major limitation of this study is the lack of participant demographic or descriptive variables. Although demographic information would have enriched the individual-level analysis, the focus of the study at the time of data collection was on the elicitation of beliefs and responses to inform practices around patient engagement and education. It may have strengthened findings to have documentation of participants’ addiction, drug of choice, prior treatment history, and type of admission (i.e., voluntary or court-ordered treatment). This additional information may have contributed to a deeper understanding of how past experiences influenced their shared perspectives and intentions for moving forward with or without MOUD. This study also took place at only one inpatient detox facility. However, since this is the only locked inpatient detoxification facility in the county, it serves a wide variety of patients who are both court mandated and self-referred, as well as insured vs. uninsured, allowing us to include people seeking recovery with diverse backgrounds and referral sources.
There are a few considerations that should be made when evaluating the methodological rigor of this study. First, a process for systematically analyzing and defining saturation would have contributed to methodological rigor. Standardization of the saturation assessment process would be particularly important for replication of this study in other settings. Additionally, there are conflicting notions in the literature regarding the methodological rigor of combining a grounded theory approach or thematic analysis with a content analysis approach (Vaismoradi et al., 2013).
Finally, as the terminology in this field changes to reflect best practices indicated in the literature, it is sometimes only in retrospect that we recognize the implications of the language we use. While the questions in the interview protocol did not explicitly use the phrase “medication-assisted treatment”, both the participant and the interviewer used this term within interview discussions due to the program’s use of this term. Knowing what we do about the implicit indications of this phrase being tied to a temporary or partial approach to treatment (Wakeman, 2017), we must acknowledge that the use of the term may have portrayed unintended biases about the usefulness or acceptance of medication to treat opioid use disorders that could have impacted participants’ perceptions. Future research should use only the most up-to-date person-centered language or to mutually define terms with participants in the data collection phase. Attention to language in these processes may help to avoid unintended consequences of cultural norms and language that may perpetuate stigma. This is particularly important for research aimed at understanding, more deeply, the personal perceptions of patients who may have already been marginalized in their pursuit for treatment.
4.2. Implications
This study offers a deeper look into this community’s culture through its evaluation of the perspectives from people whom an MOUD program hopes to serve. In areas where societal pressures, stigmas, resources, or expectations might vary from clinical standards elsewhere, MOUD programs should consider cultural norms and social influences. Programs tailor MOUD engagement and education to assuage concerns and barriers unique to the cultural norms of the setting and population (Bergman et al., 2019). Studying regions (e.g., urban vs. rural) where exposure to and resources for MOUD have been limited, with a focus on attitudes and stigmas, may help to more accurately identify distinctive risks and reduce overdoses.
A shift in the organizational culture can mitigate barriers to acceptance and use of MOUD. Programs should place a premium on accurate and adequate information sharing with staff, patients, and patients’ social networks. First, programs can prioritize individualized treatment efforts that leverage internal and external motivators. Second, programs can integrate personal experiences and preferences in the treatment planning stage to help to strengthen a patient’s commitment to their MOUD treatment. For example, participants in this study acknowledged the importance of integrated therapeutic services that would support them in managing their mental health though behavioral interventions in concurrence with their MOUD. Also, acknowledging and addressing local infrastructural challenges, such as cost, transportation, and continuity of care in treatment planning stages would likely help patients to establish more trust and confidence in the program’s delivery of their treatment plan. Last, we found patients’ relationships to influence their willingness or apprehension to engage in MOUD. Programs should make efforts to incorporate into treatment and educate the social networks of those considering MOUD programs.
Programs’ reluctance or skepticism for integrating MOUD into treatment norms exists, at least partially, due to a lack of interest from patients, local stigma, community standards, and social network concerns. All these factors reduces supply and demand for MOUD despite high levels of OUD. Nevertheless, the circumstances, experiences, and worldviews of people seeking MOUD vary across distinct populations and regions; as a result, providers, researchers, and decision-makers must make intentional efforts to avoid the homogenization of treatment delivery. All stakeholders should prioritize integrating the needs of individuals as they seek to develop feasible and sustainable recovery options grounded in clinical best practice.
4.3. Future research
Future research might compare patients’ perspectives from other regions to determine the impact of external factors and regional cultural norms. Evaluating differences between states, counties, or urban and rural areas might help to identify specific factors that contribute to variatious views of MOUD treatment integration and acceptance. Future research might also seek to correlate patients’ perspectives of MOUD with patients’ participation and outcomes in MOUD or other treatment services. Clinicians’, family members or friends’, policy-makers’, and community members’ perspectives could also contribute to a deeper understanding of the challenges and facilitators that impact the utilization and acceptance of MOUD. Including patient treatment history and medical records in future research might also support research that focuses on incorporating patients’ perspectives into treatment. A provider’s understanding of associations between treatment history and MOUD experiences could benefit efforts to further tailor treatment interventions for individuals.
Additionally, research continues to emerge that indicates the power of language in decreasing stigma and preventing unintended bias (Wakeman & Rich, 2018; Zwick et al., 2020). In response to the increased emphasis on person-centered language, particularly in the area of OUD treatment, research could compare patients’ responses based on the language that researchers use to identify what type of language, if any, influenced OUD patients’ perspectives. Such work could provide insight into whether the language that a provider uses changes a patient’s positive or negative associations of MOUD.
Last, future work could focus on strategies to address patients’ negative perceptions of MOUD. Interventions that are psychoeducational, leveraging internal locus of control and motivation, or providing peer-based support, have shown promise in other areas of recovery and medication management (Mooney et al., 2020; Mullins et al., 2004; Palacio et al., 2016). Particularly for people at a crossroads in their treatment or transitioning from detox, additional research examining the utility and efficacy of these types of interventions holds promise for transforming negative perceptions of MOUD for more effective treatment.
Acknowledgments
The Centers for Disease Control and Prevention United States Grant ID: 1 R01CE003039-01-00.
Appendix A. Semi-structured interview protocol
Brief Introduction. Example: “I’m here to gather information about your experience with medication assisted treatment such as buprenorphine, methadone, or naltrexone and to understand a little bit about your process in transitioning from detox into the next step, whatever that might mean for you. We want to understand what you need and what would be most useful for you.”
- What would work for you or what has worked in the past?
- What is it about that approach that worked for you?
- What wouldn’t work for you or what has not worked in the past?
- What is it about that approach that didn’t work for you?
- Have you used medication for treatment before?
- How did it work for you?
- What worked/didn’t work for you?
How are you feeling about your transition after detox?
Are there steps you feel like you need to take in order to help yourself stay on track after detox?
With the challenges you are facing, what do you do to keep yourself safe as you prepare for this transition?
References
- Barocas JA, Wang J, Marshall B, LaRochelle MR, Bettano A, Bernson D, … Walley AY (2019). Sociodemographic factors and social determinants associated with toxicology confirmed polysubstance opioid-related deaths. Drug and Alcohol Dependence, 200, 59–63. 10.1016/j.drugalcdep.2019.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardsley K, Wish ED, Fitzelle DB, O’Grady K, & Arria AM (2003). Distance traveled to outpatient drug treatment and client retention. Journal of Substance Abuse Treatment, 25(4), 279–285. 10.1016/s0740-5472(03)00188-0. [DOI] [PubMed] [Google Scholar]
- Bergman BG, Ashford RD, & Kelly JF (2019). Attitudes toward opioid use disorder medications: Results from a US national study of individuals who resolved a substance use problem. Experimental and Clinical Psychopharmacology, 28(4), 449–461. 10.1037/pha0000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Drug overdose mortality by state. Retrieved from CDC/National Centers for Health Statistics; https://www.cdc.gov/nchs/pressroom/sosmap/drug_poisoning_mortality/drug_poisoning.htm. [Google Scholar]
- Connery HS (2015). Medication-assisted treatment of opioid use disorder: Review of the evidence and future directions. Harvard Review of Psychiatry, 23(2), 63–75. 10.1097/hrp.0000000000000075. [DOI] [PubMed] [Google Scholar]
- Creswell JW, & Poth CN (2016). Qualitative inquiry and research design: Choosing among five approaches. Sage Publications. [Google Scholar]
- Dowling M (2008). The SAGE encyclopedia of qualitative research methods. Thousand Oaks, CA: SAGE Publications, Inc. [Google Scholar]
- E-FORCSE®. (2017). the Florida Prescription Drug Monitoring Program. http://www.floridahealth.gov/statistics-anddata/e-forcse/index.html.
- Florida Department of Children and Families. (2018). Patterns and trends of the opioid epidemic in Florida (Retrieved from Tallahassee, FL: ). [Google Scholar]
- Florida Department of Law Enforcement. (2019). Drugs Identified in Deceased Persons by Florida Medical Examiners (2018 Annual Report).
- Florida Medical Examiners Commission. (2018). Drugs identified in deceased persons by Florida Medical Examiners. http://www.fdle.state.fl.us/MEC/Publications-and-Forms/Documents/Drugs-in-DeceasedPersons/2017-Annual-Drug-Report.aspx (12 E-FORCSE®, the Florida Prescription Drug).
- Fullerton CA, Kim M, Thomas CP, Lyman DR, Montejano LB, Dougherty RH, & Delphin-Rittmon ME (2014). Medication-assisted treatment with methadone: Assessing the evidence. Psychiatric Services, 65(2), 146–157. 10.1176/appi.ps.201300235. [DOI] [PubMed] [Google Scholar]
- Fusch PI, & Ness LR (2015). Are we there yet? Data saturation in qualitative research. The Qualitative Report, 20(9), 1408–1416. [Google Scholar]
- Gruman J, Rovner MH, French ME, Jeffress D, Sofaer S, Shaller D, & Prager DJ (2010). From patient education to patient engagement: Implications for the field of patient education. Patient Education and Counseling, 78(3), 350–356. 10.1016/j.pec.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Guest G, Bunce A, & Johnson L (2006). How many interviews are enough?: An experiment with data saturation and variability. Field Methods, 18(1), 59–82. 10.1177/1525822X05279903. [DOI] [Google Scholar]
- Guest G, MacQueen KM, & Namey EE (2012). Applied thematic analysis. Thousand Oaks, CA: SAGE Publishing. 10.4135/9781483384436. [DOI] [Google Scholar]
- Hewell VM, Vasquez AR, & Rivkin ID (2017). Systemic and individual factors in the buprenorphine treatment-seeking process: A qualitative study. Substance Abuse Treatment, Prevention, and Policy, 1. 10.1186/s13011-016-0085-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heyman G (2013). Addiction and choice: Theory and new data. Frontiers in Psychiatry, 4 (31). 10.3389/fpsyt.2013.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Saxon AJ, Huang D, Hasson A, Thomas C, Hillhouse M, … Wiest K (2014). Treatment retention among patients randomized to buprenorphine/naloxone compared to methadone in a multi-site trial. Addiction-Abingdon, 109(1), 79–87. 10.1111/add.12333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infectious Disease Elimination Act (IDEA). (2019). SB 366. The Florida Senate. [Google Scholar]
- Jerry JM, & Collins GB (2013). Medication-assisted treatment of opiate dependence is gaining favor. Cleveland Clinic Journal of Medicine, 80(6), 345–349. [DOI] [PubMed] [Google Scholar]
- Joseph H, Stancliff S, & Langrod J (2000). Methadone maintenance treatment (MMT): A review of historical and clinical issues. Mount Sinai Journal of Medicine, 67 (5–6), 347–364. [PubMed] [Google Scholar]
- Kelly JF, Wakeman SE, & Saitz R (2015). Stop talking “dirty”: Clinicians, language, and quality of care for the leading cause of preventable death in the United States. American Journal of Medicine, 128(1), 8–9. 10.1016/j.amjmed.2014.07.043. [DOI] [PubMed] [Google Scholar]
- Kelly JF, & Yeterian JD (2011). The role of mutual-help groups in extending the framework of treatment. Alcohol Research & Health: The Journal of the National Institute on Alcohol Abuse and Alcoholism, 33(4), 350–355. [PMC free article] [PubMed] [Google Scholar]
- Knudsen HK, Abraham AJ, & Roman PM (2011). Adoption and implementation of medications in addiction treatment programs. Journal of Addiction Medicine, 5(1), 21–27. 10.1097/ADM.0b013e3181d41ddb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar N, Howell BA, Oles W, Janmohamed K, Lee ST, Connor PG, & Alexander M (2020). The role of social network support on treatment outcomes for medication for opioid use disorder: A systematic review. medRxiv. 10.1101/2020.07.18.20156950 (2020.2007.2018.20156950). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leshner AI, & Dzau VJ (2019). Medication-based treatment to address opioid use disorder. JAMA, 321(21), 2071–2072. [DOI] [PubMed] [Google Scholar]
- Louie DL, Assefa MT, & McGovern MP (2019). Attitudes of primary care physicians toward prescribing buprenorphine: A narrative review. BMC Family Practice, 20(1), 157. 10.1186/s12875-019-1047-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden EF (2019). Intervention stigma: How medication-assisted treatment marginalizes patients and providers. Social Science and Medicine, 232, 324–331. [DOI] [PubMed] [Google Scholar]
- Miclette MA, Leff JA, Cuan I, Samet JH, Saloner B, Mendell G, & Meisel ZF (2018). Closing the gaps in opioid use disorder research, policy and practice: Conference proceedings. Addiction Science & Clinical Practice, 13(1), 22. 10.1186/s13722-018-0123-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney LJ, Valdez J, Cousins SJ, Yoo C, Zhu Y, & Hser Y-I (2020). Patient decision aid for medication treatment for opioid use disorder (PtDA-MOUD): Rationale, methodology, and preliminary results. Journal of Substance Abuse Treatment, 108, 115–122. 10.1016/j.jsat.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullins SM, Suarez M, Ondersma SJ, & Page MC (2004). The impact of motivational interviewing on substance abuse treatment retention: A randomized control trial of women involved with child welfare. Journal of Substance Abuse Treatment, 27(1), 51–58. 10.1016/j.jsat.2004.03.010. [DOI] [PubMed] [Google Scholar]
- Notley C, Blyth A, Maskrey V, Pinto H, & Holland R (2015). Exploring the concepts of abstinence and recovery through the experiences of long-term opiate substitution clients. Substance Abuse, 36(2), 232–239. 10.1080/08897077.2014.941085. [DOI] [PubMed] [Google Scholar]
- Palacio A, Garay D, Langer B, Taylor J, Wood BA, & Tamariz L (2016). Motivational interviewing improves medication adherence: A systematic review and meta-analysis. Journal of General Internal Medicine, 31(8), 929–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M, Bird SM, Hickman M, Marsden J, Dunn G, Jones A, & Millar T (2016). Impact of treatment for opioid dependence on fatal drug-related poisoning: A national cohort study in England. Addiction-Abingdon, 111(2), 298–308. 10.1111/add.13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieckmann T, Daley M, Fuller BE, Thomas CP, & McCarty D (2007). Client and counselor attitudes toward the use of medications for treatment of opioid dependence. Journal of Substance Abuse Treatment, 32(2), 207–215. 10.1016/j.jsat.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieckmann T, Gideonse N, Risser A, DeVoe J, Abraham A, Rieckmann TR, … Abraham AJ (2017). Treating opioid dependence with buprenorphine in the safety net: Critical learning from clinical data. Journal of Behavioral Health Services & Research, 44(3), 351–363. 10.1007/s11414-017-9553-z. [DOI] [PubMed] [Google Scholar]
- Rigg KK, & Murphy JW (2013). Understanding the etiology of prescription opioid abuse: Implications for prevention and treatment. Qualitative Health Research, 23(7), 963–975. 10.1177/1049732313488837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roman PM, Abraham AJ, & Knudsen HK (2011). Using medication-assisted treatment for substance use disorders: Evidence of barriers and facilitators of implementation. Addictive Behaviors, 36(6), 584–589. 10.1016/j.addbeh.2011.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, & Jinks C (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52(4), 1893–1907. 10.1007/s11135-017-0574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuman-Olivier Z, Borodovsky JT, Steinkamp J, Munir Q, Butler K, Greene MA, Goldblatt J, Xie HY, & Marsch LA (2018). MySafeRx: A mobile technology platform integrating motivational coaching, adherence monitoring, and electronic pill dispensing for enhancing buprenorphine/naloxone adherence during opioid use disorder treatment: A pilot study. Addiction Science & Clinical Practice, 13 (1), 1–14. 10.1186/s13722-018-0122-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz RP, Kelly SM, O’Grady KE, Mitchell SG, Peterson JA, Reisinger HS, & Brown BS (2008). Attitudes toward buprenorphine and methadone among opioid-dependent individuals. The American Journal on Addictions, 17(5), 396–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigmon SC (2014). Access to treatment for opioid dependence in rural America: Challenges and future directions. JAMA Psychiatry, 71(4), 359–360. 10.1001/jamapsychiatry.2013.4450. [DOI] [PubMed] [Google Scholar]
- Stein MD, Flori JN, Risi MM, Conti MT, Anderson BJ, & Bailey GL (2017). Overdose history is associated with post-detoxification treatment preference for persons with opioid use disorder. Substance Abuse, 38(4), 389–393. 10.1080/08897077.2017.1353570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health. Retrieved from Rockville, MD: https://www.samhsa.gov/data/. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2020). Number of DATA-Waived practitioners. Retrieved from Rockville, MD: https://www.samhsa.gov/medication-assisted-treatment/practitioner-program-data/certified-practitioners?field_bup_us_state_code_value=FL. [Google Scholar]
- Sullivan MA, Bisaga A, Pavlicova M, Carpenter KM, Choi CJ, Mishlen K, & Nunes EV (2019). A randomized trial comparing extended-release injectable suspension and oral naltrexone, both combined with behavioral therapy, for the treatment of opioid use disorder. American Journal of Psychiatry, 176(2), 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timko C, Schultz NR, Cucciare MA, Vittorio L, & Garrison-Diehn C (2016). Retention in medication-assisted treatment for opiate dependence: A systematic review. Journal of Addictive Diseases, 35(1), 22–35. 10.1080/10550887.2016.1100960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uebelacker LA, Bailey G, Herman D, Anderson B, & Stein M (2016). Patients’ beliefs about medications are associated with stated preference for methadone, buprenorphine, naltrexone, or no medication-assisted therapy following inpatient opioid detoxification. Journal of Substance Abuse Treatment, 66, 48–53. 10.1016/j.jsat.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaismoradi M, Turunen H, & Bondas T (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing & Health Sciences, 15(3), 398–405. 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Frieden TR, Hyde PS, & Cha SS (2014). Medication-assisted therapies - Tackling the opioid-overdose epidemic. The New England Journal of Medicine, 370(22), 2063–2066. 10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Koob GF, & McLellan AT (2016). Neurobiologic advances from the brain disease model of addiction. The New England Journal of Medicine, 374(4), 363–371. 10.1056/NEJMra1511480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakeman SE (2017). Medications for addiction treatment: Changing language to improve care. Journal of Addiction Medicine, 11(1), 1–2. 10.1097/adm.0000000000000275. [DOI] [PubMed] [Google Scholar]
- Wakeman SE, & Rich JD (2018). Barriers to medications for addiction treatment: How stigma kills. Substance Use and Misuse, 53(2), 330–333. 10.1080/10826084.2017.1363238. [DOI] [PubMed] [Google Scholar]
- Warden D, Subramaniam GA, Carmody T, Woody GE, Minhajuddin A, Poole S. a., Potter J, Fishman M, Bogenschutx M, Patkar A, & Trivedi MH (2012). Predictors of attrition with buprenorphine/naloxone treatment in opioid dependent youth. Addictive Behaviors, 37(9), 1046–1053. 10.1016/j.addbeh.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White WL (2012). Medication-assisted recovery from opioid addiction: Historical and contemporary perspectives. Journal of Addictive Diseases, 31(3), 199–206. [DOI] [PubMed] [Google Scholar]
- Yarborough BJH, Stumbo SP, McCarty D, Mertens J, Weisner C, & Green CA (2016). Methadone, buprenorphine and preferences for opioid agonist treatment: A qualitative analysis. Drug and Alcohol Dependence, 160, 112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwick J, Appleseth H, & Arndt S (2020). Stigma: How it affects the substance use disorder patient. Substance Abuse Treatment, Prevention, and Policy, 15(1), 1–4. 10.1186/s13011-020-00288-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


