Abstract
Objective:
Research suggests that sociopolitical stressors connected with the 2016 presidential election were associated with increases in preterm birth among Latina women. This study determined whether periviable births (<26 weeks gestation), which exhibit extremely high rates of infant morbidity and mortality, among US Latina women increased above expected levels after the 2016 US presidential election.
Methods:
We assigned singleton live births among Latina and non-Latina white women in the US to 96 monthly conception cohorts conceived from January 2009 through December 2016. We constructed risk ratios by dividing the rate of periviable birth among Latina women by the rate among non-Latina white women. We used time-series methods to determine if the risk ratio of periviable births in cohorts conceived by Latina women and exposed to the election of 2016 exceeded those expected from autocorrelation and calendar effects.
Results:
We found an outlying sequence of risk ratios among Latina women starting with the cohort conceived in April and ending with that conceived in November 2016. Increases in the ratios ranged from 0.07 above an expected of 1.61 for the cohort conceived in June, to 0.39 above an expected of 1.27 for the cohort conceived in April.
Conclusion:
We find that pregnancies among Latina women in gestation at the time of the 2016 election yielded more than expected periviable births. These findings support the argument that the prospect of anti-immigrant policies promised by the Trump campaign sufficiently stressed Latina women to affect the timing of birth.
Keywords: preterm birth, periviable birth, Latina/Hispanic women, immigrants, sociopolitical stressors
INTRODUCTION
Recent research suggests that sociopolitical stressors associated with the 2016 presidential election, such as the use of highly racialized and anti-immigrant rhetoric, may play a critical role in shaping maternal and child health among targeted populations.1,2 Gemmill et al. find a 3.2–3.6% increase in the number of preterm infants born to Latina women in the US in the 9 months following the election.2 The increase was observed after controlling for preterm birth in the larger population, suggesting that Latina mothers were particularly vulnerable to the changing social and political environment. Indeed, the 2016 presidential campaign has been linked with heightened fear and anxiety among the US Latino population,3–5 including decreased prenatal care utilization among foreign-born Latina women in some regions of the country.6 Moreover, recent evidence from survey experiments shows that exposure to information about President Trump’s immigration agenda is associated with increased reports of deportation anxiety among both native-born and foreign-born Latinos, further supporting the notion that the 2016 election was associated with a “climate of threat” for certain populations in the US.5
The observed population-level increase in preterm birth following the presidential election may have profound implications for the health of individuals and their families. Infants born preterm show elevated risk for both short- and long-term complications, including higher risk of infant death, impaired neurodevelopment, and severe medical disabilities.7–9 These risks are greatest for those born at the limits of viability. These “periviable” births, defined as live births that occur between 20 0/7 to 25 6/7 weeks gestation,10 account for most neonatal deaths and nearly 40% of infant deaths in the US.9,11,12 Moreover, among periviable infants who survive their first year, almost half have at least one marker of impaired neurodevelopment, which includes conditions such as moderate or severe cerebral palsy, profound hearing loss or visual impairment, difficulty performing gross motor skills like walking or running, and cognitive impairment.9
The negative outcomes associated with periviable birth not only increase the psychological and emotional burden for individuals and families, but also exact a large financial toll to society at large.13,14 Although <1% of live births occur during the periviable period,10 they account for at least 20% of all birth hospitalization costs.15 Hospital discharge data from California, for example, indicate that the mean cost for extremely preterm infants (<28 weeks gestation) in 2009–2011 was approximately $320,000.15
Either of two theories leads to the hypothesis that the stressful nature of the election of 2016 could have increased the incidence of periviable births among Latina women. The first, and more clinically oriented, assumes that a complex interaction of developmental mechanisms, regulated by hormonal signaling, sets the timing of parturition at about the 40th week of gestation. The hormonal cascade associated with the stress response “dysregulates” developmental mechanisms by disrupting normal signaling.16–19 Clinical manifestations of this dysregulation include abnormal acceleration of the “pregnancy clock” that, in turn, causes preterm births, including those before 26 complete weeks of gestation.
A second, and more evolutionary based, theory assumes that normal, well-regulated mechanisms protect maternal fitness by spontaneously aborting pregnancies unlikely to yield offspring who would thrive in the prevailing environment.20 Most of these spontaneous abortions come early in gestation and affect fetuses with abnormalities that would preclude maturation to reproductive age even in benign environments. Some, however, come after the 20th week of gestation and often involve small for gestational age (SGA) but otherwise normal fetuses.21 These late spontaneous abortions increase among stressed women because natural selection would have conserved mutations that suppressed reproduction in environments that threaten maternal investment in frail infants.21 In recent decades, advances in neonatal care have converted some of what would have previously been late spontaneous abortions (i.e., stillbirths) into periviable births.22
The literature includes no attempts to determine whether periviable births increased among Latino infants exposed in utero to the election of 2016. This void remains despite the research described above, as well as the dire clinical sequelae and high social cost of periviable birth. Here we test the hypothesis that the election of 2016 sufficiently perturbed gestations among Latina mothers to induce periviable births among cohorts exposed in utero to the election. The methods we use improve on earlier work by using conception, rather than birth, cohorts and by controlling not only trends, but also month-of-year effects and other autocorrelation. These changes provide greater confidence in specifying the population at risk as well as in identifying, among live births, the most vulnerable period in gestation.
METHODS
Data and Measures
Data for this analysis came from restricted-use birth data files from the National Center for Health Statistics (NCHS) National Vital Statistics System. Only singleton births were included in analysis. We constructed month-year conception cohorts for all live births conceived in 2009–2016. We subtracted the length of gestation from the month and year of birth for live births that occurred in 2009–2017. Each resulting conception cohort, therefore, represents all observed live births that were likely conceived in the same month and year. We defined gestational age based on the date of the last menstrual period (LMP) to ensure consistency across time; alternative measures of gestational age based on the best obstetric estimate were not standardized across states until 2014.23 Maternal race/ethnicity was self-reported and classified in accordance with the 1997 Office of Management and Budget Standards.24 We identified Latina women from birth certificates that indicated any Hispanic ethnicity, regardless of reported race. In sensitivity analysis, we further disaggregated Latina women by nativity status based on whether women were born in the US or abroad.
We conducted all analyses and report results in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cohort studies.25 Institutional review board approval and informed consent were not required because the deidentified data were made available through a data use agreement with NCHS.
Statistical Analysis
Our analyses proceeded through 7 steps. First, we constructed our dependent variable as a time-series of risk ratios for 96 monthly conception cohorts conceived during the Obama presidency (i.e., January 2009 through December 2016). We calculated the risk ratios by dividing the rate of periviable birth (i.e. 20 0/7 to 25 6/7 weeks gestation) among Latina women by the rate among non-Latina white women.26 A risk ratio of 1 implies equal rates while ratios above and below 1 imply, respectively, a higher or lower rate among Latina women.
Second, we used Box-Jenkins methods27 to identify autocorrelation in the risk ratio time series of the 87 cohorts conceived from January 2009 through March 2016. These cohorts, conceived during the Obama presidency, could not have been in gestation for 26 or fewer weeks at the time of November 8 election (i.e., at risk of periviable birth). Box-Jenkins methods detect trends, cycles (e.g., true seasonality), and the tendency of a series to remain elevated or depressed, or to oscillate, after high or low values.
Third, we estimated a Box-Jenkins “transfer function” formed by adding 11 binary variables scored 1 for each calendar month, excluding January, and 0 otherwise to the Box-Jenkins model identified in Step 2. This step detects and controls for month-of-year effects that can appear over and above seasonality. True seasonality, detected by Box-Jenkins methods, refers to the circumstance in which the value of a monthly time series at t- 12 months reliably predicts the value at month t similarly for all months. A calendar effect refers to the circumstance in which a given month appears predictably high or low while the values of other months may not.
Fourth, we applied Box-Jenkins methods to the residuals of the transfer function estimated in step 3 to detect and specify autocorrelation revealed by control of calendar effects.27
Fifth, we added any Box-Jenkins parameters indicated by the results of Step 4 to the transfer function specified in Step 3 and estimated it for the same 87 cohorts analyzed in steps 2 and 3. The fitted values of this model estimate the risk ratio expected in the 87 cohorts conceived during the Obama presidency but not exposed to the election of November 2016. We used these months to “train” the model because we assume that Latina women had adapted to the immigration policies of the Obama presidency.2 Candidate Trump explicitly promised more hostile policies should he be elected.28,29
Sixth, we used the model estimated in step 5 to predict the number of periviable births to Latina mothers for all 96 conception cohorts. The predictions for the 88th through 95th cohorts serve as our counterfactuals or values expected had the election not occurred or had no effect on periviable births to Latina mothers.
Lastly, as described in more detail in the Supplement, we used the methods of Alwan and Roberts30 to identify any outlying sequences among the 96 residuals of the model estimated in step 6 and to describe the shape of any such sequences. All analyses were conducted with Scientific Computing Associates software.31
In a sensitivity analysis, we examined whether our findings were similar for both US-born and foreign-born Latina women, as it is unclear whether threats of anti-immigrant policies and associated rhetoric would similarly impact both groups of women.32,33 To do so, we repeated our test separately for native-born and immigrant Latina women.
The argument that the election of 2016 sufficiently perturbed gestations among Latina mothers to induce periviable births predicts a higher-than-expected outlying sequence among the cohorts conceived from April through November 2016. Those conceived in March, though in gestation at the time of the election, could not produce periviable births consistent with the argument because those cohorts’ gestational age exceeded 26 completed weeks by early November.
RESULTS
U.S. Latina and non-Latina white women gave birth to 7,053,231 and 16,002,240 live singletons nationwide, respectively, during the study period. The periviable rates were 0.31% for Latina and 0.21% for non-Latina white women. The 96 monthly cohort rates for Latina women ranged from 0.26% to 0.38% and from 0.18% to 0.26% for non-Latina white women. The points in Figure 1 show our dependent variable (i.e., ratio of the rate for Latina women divided by the rate for non-Latina white women) plotted over the test cohorts.
Figure 1.
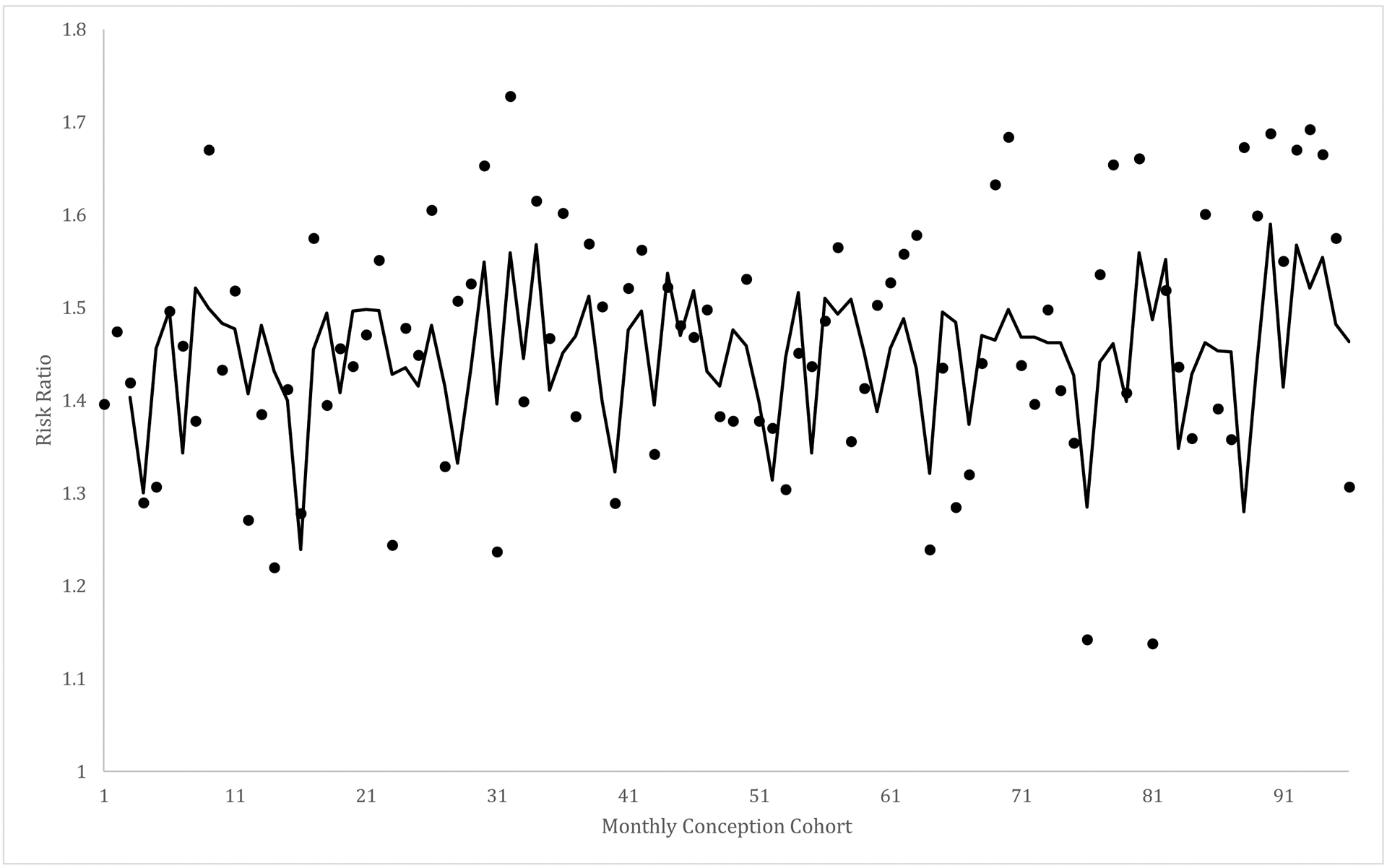
Observed (points) and expected (from autocorrelation and month of year) risk ratios of periviable birth to Latina women compared to non-Latina white women for 96 monthly conception cohorts starting with January 2009 and ending December 2016.
We describe the step by step results of our test in the Supplement. Table 1 shows the values of the transfer function for the 87 “training months,” estimated in Step 5, that included the 11 month-of-year binary variables and a Box-Jenkins parameter that controls autocorrelation. As shown, the risk ratio for cohorts conceived in Aprils appear predictably low over the test period. The Box-Jenkins moving average parameter at t-2 for all Latina women indicates that high or low values in the risk ratio tend to “echo” two cohorts later.
Table 1.
Coefficients and standard errors (SE) for transfer functions predicting the risk ratio of periviable births to all Latina women, as well as to foreign and native-born Latina women, compared to non-Latina white women in 87 monthly conception cohorts (Janauary 2009 through March 2016).
| All Latina women | Foreign-born Latina women | Native-born Latina women | ||||
|---|---|---|---|---|---|---|
| Predictor | Coefficient | SE | Coefficient | SE | Coefficient | SE |
| Constant | 1.451** | 0.037 | 1.359** | 0.034 | 1.338** | 0.065 |
| Month of year | ||||||
| February | 0.018 | 0.053 | −0.030 | 0.048 | −0.031 | 0.064 |
| March | −0.035 | 0.045 | −0.062 | 0.048 | −0.071 | 0.061 |
| April | −0.152** | 0.055 | −0.132** | 0.050 | −0.156** | 0.072 |
| May | 0.002 | 0.055 | 0.017 | 0.050 | −0.003 | 0.067 |
| June | 0.048 | 0.055 | −0.025 | 0.050 | −0.051 | 0.076 |
| July | −0.071 | 0.055 | −0.054 | 0.050 | −0.060 | 0.074 |
| August | 0.070 | 0.055 | 0.023 | 0.050 | 0.019 | 0.076 |
| September | 0.028 | 0.055 | −0.007 | 0.050 | −0.009 | 0.068 |
| October | 0.066 | 0.055 | 0.036 | 0.050 | 0.033 | 0.072 |
| November | −0.024 | 0.048 | −0.059 | 0.050 | −0.043 | 0.064 |
| December | −0.023 | 0.055 | 0.031 | 0.050 | 0.010 | 0.064 |
| Box-Jenkins Parameters |
MA(2) = −0.298** | 0.104 | AR(12)=−0.409** | 0.121 | MA(8)= 0.239** AR(1) = 0.313** AR(2) = 0.101** |
0.115 0.099 0.100 |
p < .05, 2-tailed test;
p < .01, 2-tailed test.
The line plotted in Figure 1 shows the fitted values predicted by applying the model shown in Table 1 for all Latina women to the 96 cohorts. The line from cohort 88 onward traces the counterfactuals, or the values expected if the election of 2016 had not occurred, for our tests. The differences between the expected and observed values appear in Figure 2.
Figure 2.
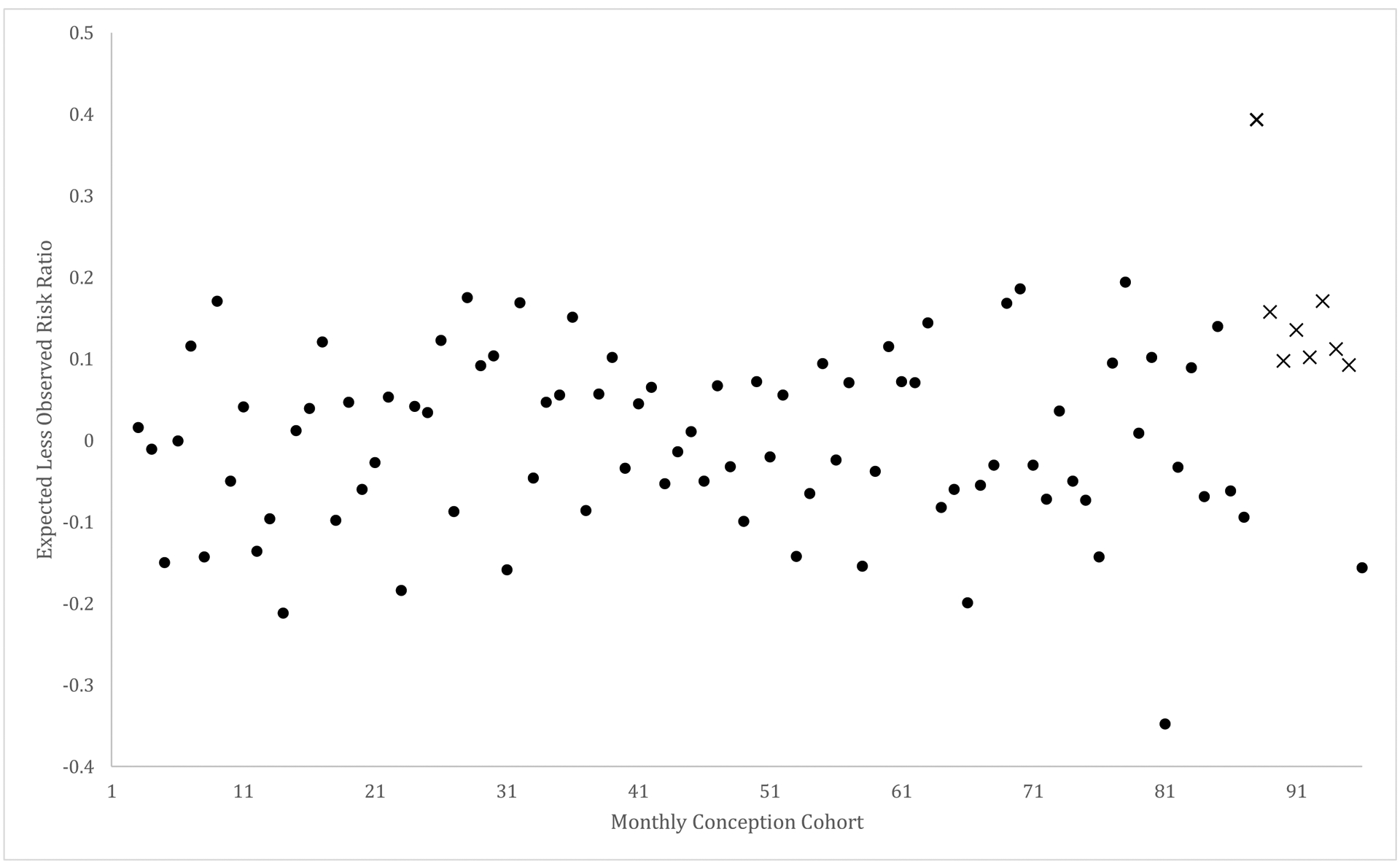
Expected (from autocorrelation and month of year) less observed risk ratios for 96 monthly conception cohorts starting with January 2009 and ending December 2016. Alwan and Roberts sequence marked with X.
Alwan and Roberts outlier detection routines applied to the residuals estimated in step 5, and shown in Figure 2, detected an outlying sequence of values for all Latina women beginning with the cohort conceived in April 2016 and persisting, though declining, through the cohort conceived in November. Table 2 shows the increases in risk ratios for the 8 cohorts in the sequence. Figure 2 shows the outlying sequence of cohorts with X’s. Increases in the ratios ranged from 0.07 above an expected of 1.61 for the cohort conceived in June, to 0.39 above an expected of 1.27 for the cohort conceived in April.
Table 2.
Increase in risk ratio for periviable birth for the 8 cohorts conceived by all Latina women, as well as by foreign- and native-born Latina women, compared to the risk among non-Latina white women, from April through November 2016.
| Month of conception | Increase in risk | ||
|---|---|---|---|
| All Latina women | Foreign-born Latina women | Native-born Latina women | |
| April 2016 | 0.392 | 0.278 | 0.334 |
| May | 0.173 | 0.214 | 0.039 |
| June | 0.072 | 0.166 | −0.193 |
| July | 0.119 | 0.090 | −0.105 |
| August | 0.127 | 0.048 | −0.070 |
| September | 0.177 | 0.071 | 0.070 |
| October | 0.110 | 0.184 | 0.026 |
| November | 0.095 | 0.204 | 0.019 |
Tables 1 and 2 also show results from our sensitivity analysis, where we present results separately for foreign-born and native-born Latina women. As shown in Table 2, applying steps 2 through 7 above yielded an outlying sequence for foreign-born Latina women very similar to that for all Latina women (e.g., the outlying sequence beginning with the cohort conceived in April persisted through the cohort conceived in November). Native-born women also exhibited a “spike” for the cohort conceived in April; however, no elevated sequence appeared among cohorts conceived closer in time to the election.
DISCUSSION
We find higher rates of periviable birth among cohorts conceived by Latina women, and exposed during pregnancy to the election of 2016, than expected from history and from cohorts conceived by non-Latina white women. These results appear consistent with the argument that the anti-immigrant rhetoric of the Trump campaign may have triggered the mechanisms that control the timing of parturition. The results extend previous findings of an upward shift in preterm birth among Latina women by showing an increase in preterm births with the highest likelihood of infant mortality and early life morbidity. Although we did not examine the survival of periviable infants in our study, given the high risk of neonatal death among these gestations, we would expect that more than half of the excess periviable births that we identified would have likely died shortly following birth.9
Previous research could not determine whether the 2016 Presidential election per se or events following the election (e.g., January 2017 inauguration, passage of immigration-related Executive Orders) coincided with an elevated risk of preterm birth.2 Our results build on this work in that we find an outlying sequence of periviable births among cohorts conceived from April through November. These cohorts would have been delivered in the periviable range from November 2016 (pregnancies conceived in April 2016) through May 2017 (pregnancies conceived in November 2016). The timing of this sequence indicates that the Presidential election per se may have been sufficiently stressful to accelerate the timing of parturition among Latina mothers. This circumstance indicates that the anticipation of imminent threats to security34,35—even in advance of any legislative action—may affect the biology of pregnant women. Indeed, these findings align with prior work by Torche and Sirois (2019) showing that the mere passage of an anti-immigrant law in Arizona, rather than the implementation of the law itself, was associated with lower birth weight among Latina immigrant women.33
Interestingly, in sensitivity analysis we observed a spike in periviable birth among both foreign-born and native-born Latina women, indicating potential spillover effects of anti-immigrant rhetoric and policies on US-born individuals. Indeed, most US Latino individuals know someone who is undocumented, and one-third know someone who has experienced immigration detention or deportation.36 However, these spillover effects are not necessarily limited to those with the closest ties to historically targeted communities. Importantly, recent research finds that deportation fears have increased for Latino citizens since the 2016 election, suggesting that “among all Latino US citizens, fears may magnify under a racialized U.S. immigration regime.”37
Despite its importance as an outcome for obstetrics, pediatrics, and population health, we have limited knowledge of the risk factors for periviable birth.20,38 Our test cannot discern what mechanisms linking stress and periviable birth, such as the dysregulated and well-regulated gestation mechanisms described above, explain our findings. The fact that the Alwan and Roberts routines detected a sequence of high-risk cohorts suggests that both mechanisms could have been at work. Indeed, we do not find the theories mutually exclusive. Nevertheless, the current findings suggest that environmental stressors likely contribute to the incidence of this rare yet consequential outcome.
Additional research that would logically follow our analysis includes efforts to refine and test hypotheses of regional pregnancy responses, following the 2016 Presidential election, to immigrant-related rhetoric and enforcement. States and cities show large variation in the extent to which they cooperate with federal immigration authorities. Demographic factors, (e.g., residential mixing among Latino and non-Latino populations, density of social networks among immigrant Latinos and US-born co-ethnic family members) may also affect perceived risk of deportation and stress-related responses to anti-immigration sentiment. We encourage additional measurement of these variables as well as refinement of hypotheses which would identify a priori particular at-risk subgroups.
Strengths of our analysis include use of rigorous time-series methods which control for well-documented patterns (e.g., seasonality) in perinatal outcomes. In addition, use of non-Latina white women as a comparison population ensures that results do not arise from a generally occurring variation in adverse outcomes shared broadly across other racial/ethnic groups.
Limitations include that we lack detailed clinical information on the periviable births and therefore could not determine the fraction yielded by spontaneous as opposed to clinically anticipated deliveries. We also did not account for other types of adverse outcomes, such as fetal deaths or maternal morbidities, that could shed additional light on the relationship we observe. Such detail would allow testing speculation about the etiology of periviable births induced by stressful events. Moreover, because the beginning of our study period predates a shift in how gestational age is measured in national data, we rely on an LMP-based measure of gestational age rather than a measure based the obstetric estimate (OE). Although births are more likely to be classified as preterm using the LMP-based measure, data from 2013 show that the percentage of deliveries that occur before 28 weeks gestation is largely similar using both measures (0.70% using OE and 0.73% using LMP),39 so misclassification due to gestational age reporting is likely not large. Third, it is plausible the election and subsequent presidency may have stressed other immigrant groups. We note that our risk ratio denominator did not exclude immigrant non-Latina white women who may have also been negatively affected by anti-immigrant rhetoric (e.g. immigrants from the Middle East and North Africa).40 This inclusion may have led to conservative estimates if these women were similarly impacted by the election. Finally, our model was “trained” using all 96 months of the Obama presidency, but we acknowledge that anti-immigrant policies fluctuated over this time. However, anti-immigrant rhetoric, generally, was less overt during the Obama presidency than the Trump presidency, providing an appropriate baseline for our model. Indeed, as noted previously, our study design tests whether the data appear consistent with the argument that threats would increase if Trump were to be elected.
This study demonstrates, in general, the importance of sociopolitical contexts in maternal and child health. In particular, xenophobic and racist rhetoric, coupled with credible threats of xenophobic and racist policies, may have a deleterious impact on the health of marginalized groups, like pregnant Latina women.41 Because sociopolitical stress may negatively impact expectant mothers, providers, clinics, and hospitals that serve populations impacted by this stress should consider stress mitigation programs among affected populations. Finally, it is important to note that the stress and anxiety associated with the November 2016 election existed against a background of other sociopolitical stressors that may impact Latina women, including policies that prevent undocumented or recent unlawful permanent residents from receiving government benefits such as Medicaid.42 As such, policies and rhetoric that exclude or stigmatize immigrants or Latinos must be examined in order to reduce the burden of sociopolitical stress among Latina women, irrespective of the president in power.
Supplementary Material
Funding:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of Interest Statement: None declared.
REFERENCES
- 1.Krieger N, Huynh M, Li W, Waterman PD, Van Wye G. Severe sociopolitical stressors and preterm births in New York City: 1 September 2015 to 31 August 2017. J Epidemiol Community Health. 2018;72(12):1147–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gemmill A, Catalano R, Casey JA, Karasek D, Alcalá HE, Elser H, Torres JM. Association of preterm births among US Latina women with the 2016 presidential election. JAMA Network Open. 2012;2(7):e197084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pew Research Center. More Latinos have serious concerns about their place in America under Trump. https://www.pewLatina.org/wp-content/uploads/sites/5/2018/10/Pew-Research-Center_Latinos-have-Serious-Concerns-About-Their-Place-in-America_2018-10-25.pdf. Published October 25, 2018. Accessed June 17, 2019. [Google Scholar]
- 4.Krupenkin M, Hill S, Rothschild D, Yom-Tov E. President Trump stress disorder: partisanship, ethnicity, and expressive reporting of mental distress after the 2016 election. SAGE Open. [published online March 27, 2019]. doi: 10.1177/2158244019830865 [DOI] [Google Scholar]
- 5.Jones BS, Sherman JW, Rojas NE, Hosek A, Vannette DL, Rocha RR, et al. Trump-induced anxiety among Latina/os. Group Processes & Intergroup Relations. [published online December 25, 2019]. doi: 10.1177/1368430219889132 [DOI] [Google Scholar]
- 6.Chu DM, Aagaard J, Levitt R, et al. Cohort analysis of immigrant rhetoric on timely and regular access of prenatal care. Obstet Gynecol. 2019;133(1):117–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allen MC. Neurodevelopmental outcomes of preterm infants. Curr Opin Neurol. 2008;21(2):123–128. [DOI] [PubMed] [Google Scholar]
- 8.Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N Engl J Med. 2008;359(3):262–273. [DOI] [PubMed] [Google Scholar]
- 9.Younge N, Goldstein RF, Bann CM, Hintz SR, Patel RM, Smith PB, et al. Survival and neurodevelopmental outcomes among periviable infants. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. N Engl J Med. 2017;376:617–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American College of Obstetricians and Gynecologists (ACOG). Periviable birth. Obstetric Care Consensus No. 6. Obstet Gynecol. 2017;130:e187–99. [DOI] [PubMed] [Google Scholar]
- 11.Lau C, Ambalavanan N, Chakraborty H, Wingate MS, Carlo WA. Extremely low birth weight and infant mortality rates in the United States. Pediatrics. 2013;131(5):855–860. [DOI] [PubMed] [Google Scholar]
- 12.Raju TN, Mercer BM, Burchfield DJ, Joseph GF. (2014). Periviable birth: executive summary of a Joint Workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists. Journal of Perinatology. 2014;34(5):333–342. [DOI] [PubMed] [Google Scholar]
- 13.Caughey AB, Burchfield DJ. Costs and cost-effectiveness of periviable care. Semin Perinatol. 2014;38(1):56–62. [DOI] [PubMed] [Google Scholar]
- 14.Cheah IGS. Economic assessment of neonatal intensive care. Transl Pediatr. 2019;8(3):246–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Phibbs CS, Schmitt SK, Cooper M, Gould JB, Lee HC, Profit J, Lorch SA. Birth Hospitalization Costs and Days of Care for Mothers and Neonates in California, 2009–2011. J Pediatr. 2019;204:118–125.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dunkel Schetter C Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology. 2011;62:531–558. [DOI] [PubMed] [Google Scholar]
- 17.Menon R, Bonney EA, Condon J, Mesiano S, Taylor RN. Novel concepts on pregnancy clocks and alarms: redundancy and synergy in human parturition. Human Reproduction Update. 2016;535–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bonney EA. Alternative theories: Pregnancy and immune tolerance. Journal of Reproductive Immunology. 2017;123:65–71. [DOI] [PubMed] [Google Scholar]
- 19.Karoutsos D, Karoutsos P, Karoutsou E. The Biological Clock and Vascular Disease: Application to Pregnancy. Journal of Clinical Epigenetics. 2017;3:1. [Google Scholar]
- 20.Catalano R, Bruckner T, Avalos LA, Stewart H, Karasek D, Kariv S, Gemmill A, Saxton K, Casey J. Understanding periviable birth: A microeconomic alternative to the dysregulation narrative. Social Science & Medicine. 2019;233:281–284. [DOI] [PubMed] [Google Scholar]
- 21.Bruckner TA, Catalano R. Selection in utero and population health: Theory and typology of research. SSM – Population Health. 2018;5:101–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elser H, Gemmill A, Casey JA, Karasek D, Bruckner T, Mayo JM. Stillbirths and live births in the periviable period. Annals of Epidemiology. 2020;49:8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin JA, Osterman MJK, Kirmeyer SE, Gregory ECW. Measuring gestational age in vital statistics data: Transitioning to the obstetric estimate. National vital statistics reports; vol 64 no 5. Hyattsville, MD: National Center for Health Statistics. 2015. [PubMed] [Google Scholar]
- 24.Office of Management and Budget. Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity. https://obamawhitehouse.archives.gov/omb/fedreg_1997standards. Published October 30, 1997. Accessed October 21, 2019. [Google Scholar]
- 25.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. [DOI] [PubMed] [Google Scholar]
- 26.Cummings P The relative merits of risk ratios and odds ratios. Archives of Pediatrics & Adolescent Medicine. 2009;163:438–445. [DOI] [PubMed] [Google Scholar]
- 27.Box G, Jenkins G, Reinsel G. Time Series Analysis: Forecasting and Control. 4th ed. Hoboken, NJ: Wiley; 2008. [Google Scholar]
- 28.Pierce S, Bolter J, Selee AUS. Immigration policy under Trump: deep changes and lasting impacts. https://www.migrationpolicy.org/research/us-immigration-policy-trump-deep-changes-impacts. Published July 2018. Accessed June 17, 2019. [Google Scholar]
- 29.Patler C, Hamilton E, Meagher K, Savinar R. Uncertainty about DACA may undermine its positive impact on health for recipients and their children. Health Aff (Millwood). 2019;38(5):738–745. [DOI] [PubMed] [Google Scholar]
- 30.Alwan LC, Roberts HV. Time-series modeling for statistical process control. Journal of Business & Economic Statistics. 1988;6(1):87–95. [Google Scholar]
- 31.Scientific Computing Associates Statistical System. SCA forecasting and time series analysis. http://www.scausa.com/scapc.php. Accessed May 9, 2019. [Google Scholar]
- 32.Novak NL, Geronimus AT, Martinez-Cardoso AM. Change in birth outcomes among infants born to Latina mothers after a major immigration raid. International Journal of Epidemiology. 2017;46(3):839–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Torche F, Sirois C. Restrictive immigration law and birth outcomes of immigrant women. Am J Epidemiol. 2019;188(1):24–33. [DOI] [PubMed] [Google Scholar]
- 34.García SJ. Living a deportation threat: Anticipatory stressors confronted by undocumented Mexican immigrant women. Race and Social Problems. 2018;10:221–234. [Google Scholar]
- 35.Gómez Cervantes A, Menjívar C. Legal violence, health, and access to care: Latina immigrants in rural and urban Kansas. Journal of Health and Social Behavior. 2020. doi: 10.1177/0022146520945048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanchez GR, Pedraza FI, Vargas ED. Health care in the shadows: Latino National Health and Immigrant Survey 2015. https://www.latinodecisions.com/blog/healthcare-in-the-shadows/. Published May 27, 2015. Accessed June 17, 2019. [Google Scholar]
- 37.Asad AL. Latinos’ deportation fears by citizenship and legal status, 2007 to 2018. Proceedings of the National Academy of Sciences. 2020;16:8836–8844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carmichael S, Blumenfeld YJ, Mayo JA, Profit J, Shaw GM, Hintz SR, Stevenson DK. Stillbirth and live birth at periviable gestational age: A comparison of prevalence and risk factors. Am J Perinatol 2019;36(5):537–544. [DOI] [PubMed] [Google Scholar]
- 39.Martin JA, Osterman MJK, Kirmeyer SE, Gregory ECW. Measuring gestational age in vital statistics data: Transitioning to the obstetric estimate. National vital statistics reports; vol 64 no 5. Hyattsville, MD: National Center for Health Statistics. 2015. [PubMed] [Google Scholar]
- 40.Islamaphobia Samari G. and public health in the United States. American Journal of Public Health. 2016;106:1920–1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Montoya-Williams D, Fuentes-Afflick E. Political Determinants of Population Health. JAMA Network Open. 2019;2(7):e197063. [DOI] [PubMed] [Google Scholar]
- 42.Healthcare.gov. Coverage for lawfully present immigrants. Baltimore, MD: U.S. Centers for Medi- care & Medicaid Services; 2012. Available from: https://www.healthcare.gov/immigrants/lawfully-present-immigrants/Accessed November 8, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


