Abstract
Patients in the US are more likely to receive out-of-network behavioral health care, including treatment for mental health or substance use disorders, than they are to receive other medical and surgical services out-of-network. To date, out-of-network and in-network trends in the prices and use of ambulatory behavioral health care have been seldom described. Here we compare levels and growth of insurer-negotiated prices (allowed amounts), patient cost-sharing, and use of psychotherapy services in-network with levels and growth out-of-network in a large, commercially insured, US population from 2007 to 2017. For both adult and child psychotherapy, prices and cost-sharing were substantially higher out-of-network than they were in-network. These gaps widened during the eleven-year period. Prices and cost-sharing for in-network psychotherapy decreased during this period, whereas prices and cost-sharing for out-of-network psychotherapy increased. Use of adult and child psychotherapy increased during this period, driven by growth of in-network use, rather than out-of-network use. The increasing gap in prices and cost-sharing between out-of-network psychotherapy and in-network psychotherapy, viewed in the context of a shortage of behavioral health providers who accept insurance, may limit access to ambulatory behavioral health care.
Stakeholders are increasingly recognizing a shortage of behavioral health providers in the United States. Across patients of all age groups, these shortages, especially of providers who accept insurance, are expected to worsen in the coming years.1–4 Although almost one in five adults reported suffering from mental illness in the United States in 2016, less than 50 percent accessed treatment.5,6 For those who do seek care, in many areas the wait for behavioral health services, particularly outpatient appointments, can be up to several months.7–9 This wait delays potentially effective treatments, as three quarters of people who receive psychotherapy have been shown to demonstrate benefit.10 In addition to experiencing long wait times when pursuing care, patients also may struggle to obtain appointments as a result of outdated insurance databases (for example, “ghost networks”).11,12
Access to behavioral health care, including treatment for mental health or substance use disorders, can differ substantially on the basis of whether the provider is within an insurer’s network or is an out-of-network provider. Insurers encourage patients to seek in-network providers, as prices paid by the insurer and out-of-pocket cost-sharing paid by the patient are generally both lower in-network than out-of-network.
Patients are three to six times more likely to seek care out-of-network for behavioral health concerns, including for psychotherapy (one of the most common treatments for many psychiatric conditions), than they are for medical concerns.13–15 One possible reason for this phenomenon is the decline in participation of psychiatrists in insurance networks, particularly commercial insurance networks, during the past decade.16,17 Psychiatrists do not account for the majority of behavioral health service use, but a variety of other health care providers1,18 from whom patients receive behavioral health services also may not participate in insurance networks.19 As the cost of care rises for patients, this lack of in-network providers may affect who is able to access behavioral health care.
Lawmakers in the US are increasingly seeking ways to protect patients from high out-of-network prices, particularly as out-of-network prices and cost-sharing have risen in some areas of medical care during the last decade.20–23 At the federal level, this has been an area of bipartisan effort, as US senators from across the political spectrum have proposed legislation to protect patients from the high cost-sharing for out-of-network services, notably when patients receive unexpected bills.24,25 Despite growing concern about the cost of out-of-network behavioral health services, little is known about how prices and cost-sharing for behavioral health services, and in particular psychotherapy, have evolved in recent years.26 To address this gap in knowledge, we examined longitudinal data among a large nationwide commercially insured population to examines prices, cost-sharing, and use of ambulatory psychotherapy out-of-network compared with in-network during the past decade.
Study Data And Methods
We analyzed outpatient claims data from the IBM MarketScan Commercial Claims and Encounters Database, a large, nationwide sample of individuals with employer-sponsored health insurance that provides information on negotiated prices, patient cost-sharing, and use.27,28
We studied all medical claims from 2007 through 2017 with a primary procedure code of psychotherapy, defined using Current Procedural Terminology codes (for example, 90804, 90805, and 90806; for a full list, see online appendix exhibit 1).29–35 The price was defined as the paid amount on a claim, reflecting negotiated allowed amounts between insurer and provider. Cost-sharing was defined as the sum of deductibles, copayments, and coinsurance paid by the patient. We excluded claims with zero or negative prices or negative cost-sharing. Given that a small number of outlier claims with high prices may be a result of errors in claims processing, and because outliers may disproportionately affect averages, prices and cost-sharing at the claims level were capped at the ninety-ninth percentile. All values were adjusted for inflation to 2016 US dollars. An indicator variable on each claim signified whether it was paid in-network or out-of-network.
We gathered characteristics of the patient, including age, sex, and Diagnostic Cost Groups risk score from Verisk Health.36 The Diagnostic Cost Groups risk score uses demographic information and diagnoses to predict expected spending; such a score is widely used by public and private insurers in risk adjustment. Individuals were defined as adults if their age was greater than eighteen years, and as children otherwise. Eighteen-year-olds were categorized as children because these individuals are commonly seen by child psychiatrists and are typically still in high school. Use of psychotherapy was evaluated at the person-year level among individuals with at least one year of continuous enrollment. The number of psychotherapy visits per hundred individuals was assessed, as well as the average number of visits per enrollee among those receiving any psychotherapy.
Changes in price and cost-sharing over time were assessed separately for in-network and out-of-network services, with the ratios of out-of-network to in-network prices and cost-sharing compared over time. Average price and cost-sharing were analyzed separately for adult and child psychotherapy. Subgroup analyses were conducted by site of care (office versus on-campus hospital outpatient departments) and by population size of metropolitan statistical areas, representing urbanicity.
Linear regressions were used to estimate average changes in annual spending, cost-sharing, and use, controlling for the Diagnostic Cost Groups risk score and plan type fixed effects (appendix exhibit 2).35
In secondary analyses, we examined psychotherapy delivered by psychiatrists, nonpsychiatrist behavioral health providers (psychotherapists, psychologists, and psychiatric nurses), and all other providers (for example, oncologists and palliative care physicians). Given that physicians may set different prices than nonphysicians and that the proportions of provider types was not constant across time, average price and cost-sharing could be affected by changes in the distribution of provider types. Therefore, we calculated the average prices and cost-sharing weighted by fixed proportions of provider types throughout the period, using the 2007 proportions of provider types in all years. All analyses used Stata, version 15. This study was approved by the Institutional Review Board at Harvard Medical School.
This study has several important limitations. First, it is a descriptive study using claims data from a convenience sample of individuals with employer-sponsored insurance. Employers may enter and exit the data each year. We were unable to identify a continuously enrolled cohort of employers across the eleven years, which means their composition could affect prices. Nevertheless, this data set is one of the largest in the country and maintained fairly broad geographic coverage throughout the study period.
Second, although we examined only psychotherapy (by definition a fixed basket of services), the average price can be influenced by the mix of provider types, given that psychiatrists may command slightly higher prices than nonphysician providers for the same service. Changes in the distribution of provider types could result from multiple factors. The composition of providers, employers, and enrollees may change. Patients may substitute from one provider type to another (for example, psychiatrist to nonpsychiatrist) because of price or various clinical reasons. Employers may change their provider networks, plan design (for example, coverage of out-of-network services or of certain specialties), and other incentives that affect the mix of providers in the claims. In secondary analyses, we studied the data by specialty, finding similar price trends for psychiatrists, other behavioral health providers, and all other providers. Results holding proportions of provider types constant were qualitatively similar to the main findings using all provider types.
Third, payments made outside of insurance (for example, private payments from patients to providers or balance billing of patients by providers) could not be observed. Therefore, to the extent that additional costs such as balance billing would further increase the cost of behavioral health care to patients, especially out-of-network, our findings represent a lower bound or conservative estimate of patients’ out-of-pocket costs.
Fourth, in this study, we focused on examining per visit prices of psychotherapy and the rate of psychotherapy visits, rather than total spending on behavioral health.
Last, we were unable to evaluate the clinical or personal reasons patients sought care and do not provide any normative judgment about whether the number of visits received was high or low.
Study Results
From 2007 through 2017, a total of 90,900,831 psychotherapy claims met criteria for inclusion in our study. These included 73,209,596 (80.5 percent) psychotherapy visits for adults and 17,691,235 (19.5 percent) psychotherapy visits for children (exhibit 1). The total number of unique enrollees in the population was 53,519,876 (data not shown).
Exhibit 1:
Characteristics of the study population and average prices and cost-sharing for psychotherapy claims for children and adults, 2007–17
| Adults (older than 18 years) | Children (0–18 years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IN (n = 53,876,473) | OON (n = 19,333,123) | OON/IN ratio | IN (n = 13,311,534) | OON (n = 4,379,701) | OON/IN ratio | |||||
| Mean/% | SD | Mean/% | SD | Mean/% | SD | Mean/% | SD | |||
| Age (years) | 41.7 | 12.2 | 42.4 | 12.5 | —a | 13.0 | 3.8 | 13.0 | 3.8 | —a |
| Female (%) | 66.6 | —a | 65.2 | —a | —a | 51.9 | —a | 50.2 | —a | |
| Risk score | 2.4 | 3.8 | 2.3 | 3.7 | —a | 1.3 | 2.6 | 1.4 | 2.5 | —a |
| Price ($) | 88.89 | 28.25 | 133.27 | 53.78 | 1.5 | 88.24 | 31.25 | 127.08 | 50.88 | 1.4 |
| Office | 88.56 | 27.57 | 133.72 | 53.26 | 1.5 | 87.75 | 30.17 | 128.04 | 50.74 | 1.5 |
| HOPD | 114.67 | 69.32 | 160.67 | 110.42 | 1.4 | 118.34 | 76.52 | 143.06 | 87.21 | 1.2 |
| Cost-sharing ($) | 22.33 | 19.38 | 46.74 | 41.75 | 2.1 | 23.84 | 21.42 | 51.47 | 44.13 | 2.2 |
| Office | 22.42 | 19.13 | 47.28 | 41.64 | 2.1 | 23.95 | 21.07 | 51.95 | 43.82 | 2.2 |
| HOPD | 22.46 | 28.7 | 41.6 | 52.53 | 1.9 | 24.43 | 30.57 | 53.96 | 53.88 | 2.2 |
SOURCE Authors’ analysis of data from the IBM Watson Truven MarketScan Commercial Claims and Encounters Database, 2007-2017. NOTES Values in the Mean/% column are means unless otherwise indicated. Prices are adjusted to 2016 US dollars. The Diagnostic Cost Groups risk score is a measure of health status, calculated using age, sex, and diagnosis codes. Diagnostic Cost Groups is similar to the Medicare Hierarchical Condition Category risk score and is commonly used for risk adjustment by private insurers. Higher scores denote greater expected spending. OON is out-of-network. IN is in-network. SD is standard deviation. HOPD is hospital outpatient department (on-campus).
Not applicable.
Exhibit 1 shows the characteristics of patients receiving psychotherapy. The mean age (±standard deviation) of adults receiving psychotherapy was 41.9 ± 12.3 years, and for children it was 13.0 ± 3.8 years. Adult psychotherapy claims comprised a greater proportion of women (66.2 percent) than men and represented patients with mean Diagnostic Cost Groups scores of 2.4 ± 3.8. For children, 51.5 percent were girls and the mean Diagnostic Cost Groups risk scores were 1.4 ± 2.6. These characteristics and risk scores were similar between in-network and out-of-network claims. The numbers presented here are weighted averages of the in-network and out-of-network numbers presented in exhibit 1.
Adult Psychotherapy
Unadjusted trends in in-network and out-of-network psychotherapy prices and cost-sharing for adults and children are shown in exhibit 2. For in-network adult psychotherapy, negotiated prices declined by 13.9 percent across the eleven-year period, going from $98.10 in 2007 to $84.47 in 2017 (p < 0.001). In-network patient cost-sharing among adults declined by 15.4 percent, going from $25.22 to $21.33 over the same period (p < 0.001).
Exhibit 2.
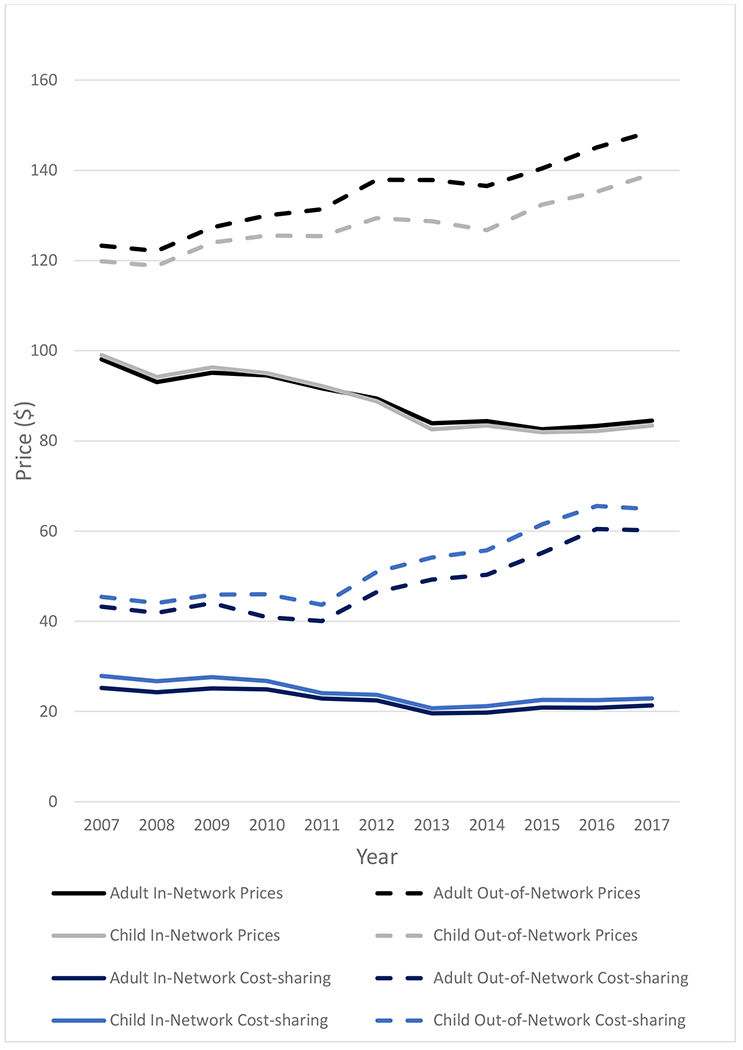
Prices and Cost-Sharing In-Network and Out-of-Network for Psychotherapy, 2007-2017
For out-of-network adult psychotherapy, prices increased from $123.30 in 2007 to $148.64 in 2017, a 20.6 percent increase (p < 0.001). Similarly, out-of-network cost-sharing grew from $43.23 to $60.15 during the study period, an increase of 39.1 percent (p < 0.001) (exhibit 2). The ratio of out-of-network prices to in-network prices rose from 1.28 to 1.76 over the course of the eleven years. During the same period, the ratio of out-of-network cost-sharing to in-network cost-sharing increased more, going from 1.71 to 2.82 (appendix exhibit 3).35
Child Psychotherapy
Trends in in-network and out-of-network psychotherapy prices and cost-sharing for children were qualitatively similar to trends for adults (exhibit 2). In-network prices decreased 15.7 percent (going from $98.98 in 2007 to $83.42 in 2017) and in-network cost-sharing decreased 17.9 percent (going from $27.90 in 2007 to $22.90 in 2017), whereas out-of-network prices increased 16.1 percent (going from $119.83 in 2007 to $139.18 in 2017; p < 0.001) and out-of-network cost-sharing increased 42.8 percent (going from $45.43 in 2007 to $64.89 in 2017; p < 0.001). The ratio of out-of-network prices to in-network prices for child psychotherapy increased from 1.21 to 1.67, and the ratio of out-of-network to in-network cost-sharing increased from 1.63 to 2.83 during this period (appendix exhibit 4).35
Subgroup Analyses
In the site-of-care analysis, the ratio of out-of-network to in-network prices for psychotherapy provided in both the outpatient office and hospital outpatient department settings increased for both adults and children from 2007 to 2017 (going from 1.26 to 1.75 for adults and 1.22 to 1.69 for children in the outpatient office, and analogously, from 1.12 to 1.78 for adults and 1.01 to 1.25 for children in the hospital outpatient department; appendix exhibits 5 and 6).35
The ratio of out-of-network to in-network cost-sharing in the office and hospital outpatient department settings for both adults and children increased more substantially (going from 1.72 to 2.83 for adults and 1.63 to 2.84 for children in provider offices and from 1.55 to 2.40 for adults and 1.39 to 2.96 for children in hospital-outpatient departments; appendix exhibits 5 and 6).35
In the analysis by size of metropolitan statistical area, changes in prices and cost-sharing were similar across metropolitan statistical areas during the eleven-year period, with comparable trends seen in each quartile of population size (appendix exhibits 7 and 8).35 Results were qualitatively similar when nonbehavioral health providers who billed behavioral health services (a small portion of the claims) were excluded. Results were qualitatively similar when codes introduced in Current Procedural Terminology coding guideline changes made in 2013 that allowed billing of add-on codes were excluded from the pricing and cost-sharing analyses (data not shown).
Secondary Analyses
Prices and cost-sharing for adult and child psychotherapy by provider type are shown in appendix exhibits 9 and 10.35 Across psychiatrists, nonpsychiatrist behavioral health providers, and all other providers, the average price could differ, but the change from 2007 to 2017 was qualitatively similar. When the overall average price was calculated using fixed proportions of providers, results were similar to those using observed proportions in the data. Analyses of cost-sharing demonstrated an analogous pattern.
Use
During the eleven-year study period, the use of adult psychotherapy increased from an average of 34.4 visits per 100 enrollees in 2007 to 54.3 visits per 100 enrollees in 2017 (p < 0.001; exhibit 3 and appendix exhibit 11).35 During this period, there was a trend toward increasing use of in-network adult psychotherapy from 22.4 visits per 100 enrollees in 2007 to 42.7 visits per 100 enrollees in 2017 (p < 0.001) and a corresponding decrease in observable out-of-network psychotherapy visits, going from 12.0 per 100 enrollees in 2007 to 11.5 per 100 enrollees in 2017 (p < 0.001; exhibit 3 and appendix exhibit 11).35 Among patients who received any adult psychotherapy, the mean number of visits per year increased across the period both in-network (going from 8.3 visits in 2007 to 9.4 visits in 2017, for a 13.3 percent increase) and out-of-network (going from 9.7 visits in 2007 to 13.6 visits in 2017, for a 40.2 percent increase) (appendix exhibit 11).35
Exhibit 3.
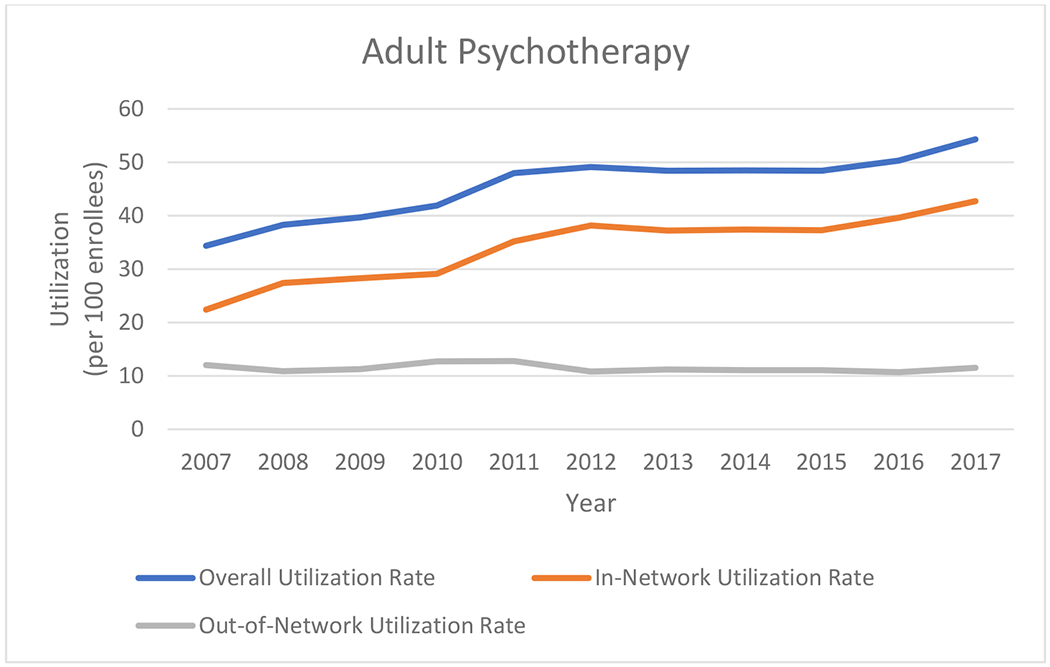
Utilization of Adult Psychotherapy, 2007-2017
For children, psychotherapy use increased from 21.2 visits per 100 enrollees in 2007 to 48.6 visits per 100 enrollees in 2017 (p < .001), with a similar increase seen in in-network use (going from 13.7 visits per 100 enrollees in 2007 to 38.8 visits per 100 enrollees in 2017; p < 0.001), whereas out-of-network use only increased slightly (going from 7.5 visits per 100 enrollees in 2007 to 9.8 visits per 100 enrollees in 2017; p < 0.001) (exhibit 4 and appendix exhibit 11).35 Among children who received any psychotherapy, mean visits per year increased across the period both in-network (going from 6.3 visits in 2007 to 8.4 visits in 2017, for a 33.3 percent increase) and out-of-network (going from 7.2 visits in 2007 to 10.9 visits in 2017, for a 51.4 percent increase) (appendix exhibit 11).35
Exhibit 4.
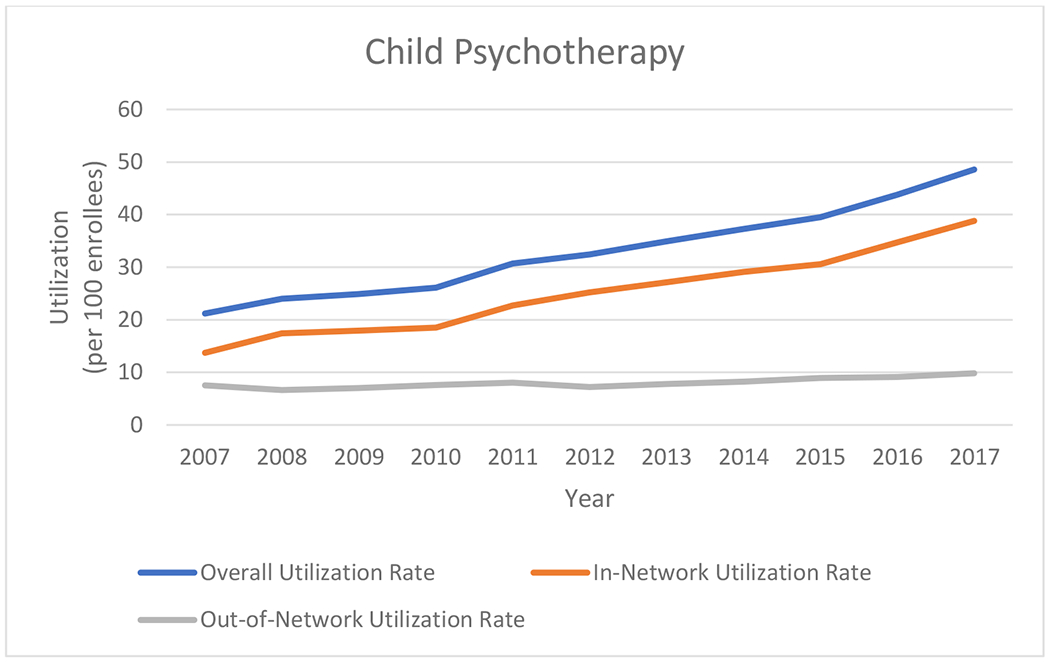
Utilization of Child Psychotherapy, 2007-2017
Discussion
During the past eleven years, the average price of psychotherapy paid by insurers has decreased for in-network care and increased for out-of-network care. Similarly, the average cost-sharing for psychotherapy paid by patients has decreased for in-network care and increased for out-of-network care. Thus, the gap between in-network and out-of-network costs for both insurers and patients has widened.
Several factors may help explain rising out-of-network prices relative to in-network prices. First, the shortage of behavioral health providers in the US affords psychiatrists, psychologists, and other providers some degree of market power in negotiations with private insurers. This may enable such providers both to stay out of insurance networks and to charge higher prices when the demand for behavioral health care grows. The number of psychiatrists per hundred thousand people in the United States declined 10 percent from 2003 to 2013 and the overall workforce is projected to continue to decline through 2024.2 Similarly, psychologists are in short supply, with 37 percent of US counties having no psychologists.37
Second, behavioral health is unique relative to most medical and surgical specialties in part because of the relatively low fixed costs of the facility infrastructure needed to establish an office-based practice. For example, providers may set up a private practice in a home office. Such flexibility may render it less necessary for behavioral health providers to practice within large physician organizations or delivery systems, in contrast to procedural or other specialists who may need such organizations or systems to supply facility resources or incur the fixed costs of practice. This freedom to choose the location and style of practice, as well as the patients who are seen, may enable behavioral health providers to more easily practice outside of insurance networks and to charge higher prices. This hypothesis is supported by evidence suggesting that behavioral health providers negotiate in-network prices with private insurers less frequently than do other medical specialties.16
Third, insurance reimbursement to behavioral health providers for behavioral health services, largely cognitive services through evaluation and management codes (although psychotherapy codes are distinct from standard office visit codes), is less favorable than for peer specialties. For example, in 2014, the median in-network reimbursement for a midlevel office visit (Current Procedural Terminology code 99213) for a commercially insured patient was $76 for a nonpsychiatrist medical doctor compared with $66 for a psychiatrist.38 These differences in unit prices potentially motivate behavioral health providers to charge higher out-of-network prices. In addition, declining in-network prices over time (12.2 percent for adults and 15.7 percent for children) may discourage providers from participating in insurance networks; for example, psychologists have reported low reimbursement rates as a primary deterrent to participating in Medicare.19
As out-of-network prices and cost-sharing for psychotherapy grew during the past decade, average in-network use increased while out-of-network use decreased or remained relatively stable population-wide. This is consistent with increased prices of out-of-network psychotherapy potentially encouraging fewer out-of-network visits and substitution toward in-network visits. With widening price differences between out-of-network and in-network care, patients could be more likely to choose in-network providers and insurance plans could be more likely to steer patients toward in-network providers. Among patients who received any psychotherapy, the mean number of in-network visits per patient increased during the eleven-year period, as did the mean number of out-of-network visits per patient. However, overall out-of-network use decreased slightly for adults (appendix exhibit 9),35 suggesting that fewer adults were receiving psychotherapy out-of-network, but those who did still used an increasing number of visits.
Despite increasing out-of-pocket costs, total use of psychotherapy increased during the study period within this commercially insured population. This suggests that access to behavioral health services was largely maintained. As services become more expensive, however, other, more vulnerable, populations who do not have commercial insurance or any insurance may fare differently. Moreover, if psychotherapy providers are practicing at full capacity, then increased access among commercially insured patients may mean that those with fewer financial resources or public insurance may face fewer options for treatment. We were unable to examine these potential offsetting or spillover effects.
Patients seeking behavioral health care commonly cite cost in general and, to a lesser degree, concerns that insurance will not fully cover the cost of their care as barriers to seeking treatment.6,39 These factors may restrict access to care, especially for disadvantaged or vulnerable populations. Furthermore, given that patients are more likely to seek behavioral health care out-of-network than other types of medical care,22 the burden of patient out-of-pocket spending for this type of care is comparably higher than that for other medical services.13,40 These services and associated costs may contribute to greater cost-sharing for patients with behavioral health conditions compared with those with chronic physical conditions.41 Our results build on the limited existing data and provide longitudinal, national evidence of these concerning trends in the increasing burden to patients, employers, and their insurers of out-of-network costs for psychotherapy.
Studies have been mixed as to the impact of the Mental Health Parity and Addiction Act of 2008 on out-of-network mental health service use, spending, and patients’ cost burden.42 The act took effect in 2010 and required insurers to provide similar benefits for mental health as for medical services. Some studies have suggested that spending on out-of-network mental health care did not change, whereas others reported increased spending in some areas.14,43–45 In addition, the Affordable Care Act introduced changes to the private insurance market through mandated coverage of essential health benefits that included mental health and substance use disorder services, including behavioral health treatment. Although our data cannot assess the effect of the parity law or the Affordable Care Act on prices of behavioral health care because of the lack of a counterfactual or control group, they do suggest that growth in out-of-network prices for behavioral health services existed before these federal laws and continued to exist after they went into effect. Whether such laws accelerated this trend or slowed what otherwise could have been faster growth remains unknown. With the 2013 Current Procedural Terminology code changes, we might have expected to see sharp use or price changes; however, the trends observed were fairly smooth across the study period. Further research should consider how federal policies may have affected the overall rising trend in out-of-network prices and patient cost-sharing during the past decade.
Conclusion
Psychotherapy is costlier to insurers and patients when obtained out-of-network than in-network, and this gap in prices and cost-sharing has widened during the past eleven years. These trends are evident across adult and child patient populations and affect both office-based and hospital-based practices. The evolution of out-of-network behavioral health care will have important policy implications for ensuring access to this essential service.
Supplementary Material
Acknowledgment
Preliminary findings were presented at the Academy Health Annual Research Meeting, June 2019, in Washington, DC. This work was supported by a grant from the Office of the Director, National Institutes of Health (NIH Director’s Early Independence Award No. DP5-OD024564 to Zirui Song). Nicole Benson receives support from the National Library of Medicine Biomedical Informatics and Data Science Research Training Grant (T15 LM007092). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or National Library of Medicine. The authors acknowledge Andrew Hicks for the derivation of risk scores using the Diagnostic Cost Groups risk adjustment model.
Biographies
BIOS:
Bio 1: Nicole M. Benson is an instructor in psychiatry at Harvard Medical School, and psychiatrist at Massachusetts General Hospital and McLean Hospital, in Belmont, Massachusetts.
Bio 2: Zirui Song (song@hcp.med.harvard.edu) is an assistant professor of health care policy and medicine at Harvard Medical School and Massachusetts General Hospital, and a faculty member in the Center for Primary Care at Harvard Medical School, in Boston, Massachusetts.
Notes
- 1.National Council Medical Director Institute. The psychiatric shortage: causes and solutions [Internet]. Washington (DC): National Council for Behavioral Health; 2017. March 28 [cited 2020 Apr 28]. Available from: https://www.thenationalcouncil.org/wp-content/uploads/2017/03/Psychiatric-Shortage_National-Council-.pdf [Google Scholar]
- 2.Satiani A, Niedermier J, Satiani B, Svendsen DP. Projected workforce of psychiatrists in the United States: a population analysis. Psychiatr Serv. 2018;69(6):710–3. [DOI] [PubMed] [Google Scholar]
- 3.Bishop TF, Seirup JK, Pincus HA, Ross JS. Population of US practicing psychiatrists declined, 2003-13, which may help explain poor access to mental health care. Health Aff (Millwood). 2016;35(7):1271–7. [DOI] [PubMed] [Google Scholar]
- 4.Raphelson S Severe shortage of psychiatrists exacerbated by lack of federal funding. National Public Radio [serial on the Internet]. 2018. March 9 [cited 2020 Apr 28]. Available from: https://www.npr.org/2018/03/09/592333771/severe-shortage-of-psychiatrists-exacerbated-by-lack-of-federal-funding
- 5.National Institute of Mental Health. Mental illness [Internet]. Bethesda (MD): NIMH; [updated 2019. February; cited 2020 Apr 28]. Available from: https://www.nimh.nih.gov/health/statistics/mental-illness.shtml [Google Scholar]
- 6.Walker ER, Cummings JR, Hockenberry JM, Druss BG. Insurance status, use of mental health services, and unmet need for mental health care in the United States. Psychiatr Serv. 2015;66(6):578–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freyer FJ. Wait for mental health treatment in Mass. can take months, study says. Boston Globe [serial on the Internet]. 2017. October 31 [cited 2020 Apr 28]. Available from: https://www.bostonglobe.com/metro/2017/10/31/wait-for-mental-health-treatment-can-take-months-study-says/EyfSBNea93rOaptHAFmqDP/story.html
- 8.Dampier C Mental health care appointments often come with a long wait. 3 ways to cope while help is delayed. Chicago Tribune [serial on the Internet]. 2018. October 25 [cited 2020 Apr 28]. Available from: https://www.chicagotribune.com/lifestyles/sc-fam-mental-health-wait-times-1030-story.html
- 9.Sirkin JT, McClellan SR, Hunt M, Sheedy K, Hoffman C, Olsho L. Quantifying wait times for outpatient mental health services in massachusetts: provider and organizational characteristics associated with access [Internet]. Boston (MA): Blue Cross Blue Shield of Massachusetts Foundation; 2017. October [cited 2020 Apr 28]. Available from: https://www.bluecrossmafoundation.org/sites/default/files/download/publication/Quant_MH_Wait_Times_REPORT_v07_final.pdf [Google Scholar]
- 10.Parekh R, Givon L. What is psychotherapy? [Internet]. Washington (DC): American Psychiatric Association; 2019. January [cited 2020 Apr 28]. Available from: https://www.psychiatry.org/patients-families/psychotherapy [Google Scholar]
- 11.Malowney M, Keltz S, Fischer D, Boyd JW. Availability of outpatient care from psychiatrists: a simulated-patient study in three U.S. cities. Psychiatr Serv. 2015;66(1):94–6. [DOI] [PubMed] [Google Scholar]
- 12.Busch SH, Kyanko KA. Incorrect Provider Directories Associated With Out-Of-Network Mental Health Care And Outpatient Surprise Bills. Health Aff (Millwood). 2020;39(6):975–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kyanko KA, Curry LA, Busch SH. Out-of-network provider use more likely in mental health than general health care among privately insured. Med Care. 2013;51(8):699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melek SP, Perlman D, Davenport S. Addiction and mental health vs. physical health: analyzing disparities in network use and provider reimbursement rates [Internet]. Seattle (WA): Milliman; 2017. December [cited 2020 Apr 28]. Available from: https://milliman-cdn.azureedge.net/-/media/milliman/importedfiles/uploadedfiles/insight/2017/nqtldisparityanalysis.ashx [Google Scholar]
- 15.Claxton G, Rae M, Cox C, Levitt L. An analysis of out-of-network claims in large employer health plans [Internet]. San Francisco (CA): Peterson-KFF Health System Tracker; 2018. August 13 [cited 2020 Apr 28]. Available from: https://www.healthsystemtracker.org/brief/an-analysis-of-out-of-network-claims-in-large-employer-health-plans/ [Google Scholar]
- 16.Bishop TF, Press MJ, Keyhani S, Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cummings JR. Rates of psychiatrists’ participation in health insurance networks. JAMA. 2015;313(2):190–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629–40. [DOI] [PubMed] [Google Scholar]
- 19.Hamp A, Stamm K, Lin L, Christidis P. 2015 APA survey of psychology health service providers [Internet]. Washington (DC): American Psychological Association, Center for Workforce Studies; 2016. September [cited 2020 Apr 28]. Available from: https://www.apa.org/workforce/publications/15-health-service-providers/ [Google Scholar]
- 20.Massachusetts Health Policy Commission. 2017 Annual health care cost trends report [Internet]. Boston (MA): Massachusetts Health Policy Commission; 2018. March [cited 2020 Apr 28]. Available from: https://www.mass.gov/files/documents/2018/03/28/Cost%20Trends%20Report%202017.pdf [Google Scholar]
- 21.Hall MA, Adler L, Ginsburg PB, Trish E. Reducing unfair out-of-network billing-integrated approaches to protecting patients. N Engl J Med. 2019;380(7):610–2. [DOI] [PubMed] [Google Scholar]
- 22.Song Z, Johnson W, Kennedy K, Biniek JF, Wallace J. Out-Of-Network Spending Mostly Declined In Privately Insured Populations With A Few Notable Exceptions From 2008 To 2016. Health Aff (Millwood). 2020;39(6):1032–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson WC, Kennedy K, Biniek JF, Song Z, Wallace J. Out-of-Network Spending: Why Growing Attention Is Focused On A Small Share Of Medical Spending. Health Affairs Blog; 2020. June 2 [cited 2020 Jun 2] Available from: https://www.healthaffairs.org/do/10.1377/hblog20200601.723677/full/ [DOI] [PMC free article] [PubMed]
- 24.Shaheen J, McCaskill C, Baldwin T, Hassan M. Reducing Costs for Out-of-Network Services Act of 2018 [Internet]. Washington (DC): 115th Congress; [cited 2020 Apr 28]. Available from: https://www.shaheen.senate.gov/imo/media/doc/Shaheen%20Out-of-Pocket%20Costs%20Bill%2010.3.2018.pdf [Google Scholar]
- 25.Cassidy W Protecting Patients from Surprise Medical Bills Act [Internet]. Washington (DC): 115th Congress; [cited 2020 Apr 28]. Available from: https://www.cassidy.senate.gov/imo/media/doc/Discussion%20Draft-%20Protecting%20Patients%20from%20Surprise%20Medical%20Bills%20Act.pdf [Google Scholar]
- 26.Busch SH, McGinty EE, Stuart EA, Huskamp HA, Gibson TB, Goldman HH, et al. Was federal parity associated with changes in Out-of-network mental health care use and spending? BMC Health Serv Res. 2017;17(1):315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adamson DM, Chang S, Hansen LG. Health research data for the real world: the MarketScan Databases. Ann Arbor (MI): Thomson Reuters; 2008. January. [Google Scholar]
- 28.IBM. IBM MarketScan Commercial Claims and Encounters Database [Internet]. Armonk (NY): IBM Watson Health; [cited 2020 Apr 28]. Available from: https://www.ibm.com/products/marketscan-research-databases [Google Scholar]
- 29.Busch AB, Frank RG, Lehman AF. The effect of a managed behavioral health carve-out on quality of care for medicaid patients diagnosed as having schizophrenia. Arch Gen Psychiatry. 2004;61(5):442–8. [DOI] [PubMed] [Google Scholar]
- 30.American Psychiatric Association, Office of Healthcare Systems and Financing. CPT primer for psychiatrists [Internet]. Washington (DC): American Psychiatric Association; 2013. [cited 2020 Apr 28]. Available for download from: https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Practice-Management/Coding-Reimbursement-Medicare-Medicaid/Coding-Reimbursement/cpt-primer-for-psychiatrists.pdf [Google Scholar]
- 31.Swann DR, Falcone AJ. CPT code changes: E/M 102, level selection, and documentation support [Internet]. Washington (DC): National Council for Behavioral Health; 2013. January 9 [cited 2020 Apr 28]. Available from: https://www.thenationalcouncil.org/webinars/cpt-code-changes-em-102-level-selection-and-documentation-support/ [Google Scholar]
- 32.American Academcy of Child and Adolescent Psychiatry. CPT code training module. Washington (DC): American Academcy of Child and Adolescent Psychiatry; 2012. August. [Google Scholar]
- 33.Office of Healthcare Systems and Financing, American Psychiatric Association. Current Procedural Terminology (CPT): code changes for 2013 overview [Internet]. Washington (DC): American Psychiatric Association; 2013. [cited 2020 Apr 28]. Available for download from: https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Practice-Management/Coding-Reimbursement-Medicare-Medicaid/Coding-Reimbursement/cpt-overview.pdf [Google Scholar]
- 34.National Council for Community Behavioral Healthcare. Major changes to CPT codes for psychiatry and psychotherapy in 2013 [Internet]. Washington (DC): NationalCouncil; 2012. September [cited 2020 Apr 28]. Available from: https://www.bcbst.com/providers/Nat-council-CPT-code-changes.pdf [Google Scholar]
- 35.To access the appendix, click on the Details tab of the article online.
- 36.DxCG Risk Solutions. DxCG science guide. Waltham (MA): Verisk Health; 2012. [Google Scholar]
- 37.Andrilla CHA, Patterson DG, Garberson LA, Coulthard C, Larson EH. Geographic variation in the supply of selected behavioral health providers. Am J Prev Med. 2018;54(6 Suppl 3):S199–207. [DOI] [PubMed] [Google Scholar]
- 38.Mark TL, Olesiuk W, Ali MM, Sherman LJ, Mutter R, Teich JL. Differential reimbursement of psychiatric services by psychiatrists and other medical providers. Psychiatr Serv. 2018;69(3):281–5. [DOI] [PubMed] [Google Scholar]
- 39.Kowalczyk L For many, a struggle to find affordable mental health care. Boston Globe [Internet]. 2018. October 20 [cited 2020 Apr 28]. Available from: https://www.bostonglobe.com/metro/2018/10/20/for-many-struggle-find-affordable-mental-health-care/AAK3aYmk89sRLicmTFpn6O/story.html
- 40.Pelech D, Hayford T. Medicare Advantage and commercial prices for mental health services. Health Aff (Millwood). 2019;38(2):262–7. [DOI] [PubMed] [Google Scholar]
- 41.Xu WY, Song C, Li Y, Retchin SM. Cost-sharing disparities for out-of-network care for adults with behavioral health conditions. JAMA Netw Open. 2019;2(11):e1914554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thalmayer AG, Friedman SA, Azocar F, Harwood JM, Ettner SL. The Mental Health Parity and Addiction Equity Act (MHPAEA) Evaluation Study: impact on quantitative treatment limits. Psychiatr Serv. 2017;68(5):435–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McGinty EE, Busch SH, Stuart EA, Huskamp HA, Gibson TB, Goldman HH, et al. Federal parity law associated with increased probability of using out-of-network substance use disorder treatment services. Health Aff (Millwood). 2015;34(8):1331–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Horgan CM, Hodgkin D, Stewart MT, Quinn A, Merrick EL, Reif S, et al. Health plans’ early response to federal parity legislation for mental health and addiction services. Psychiatr Serv. 2016;67(2):162–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Friedman SA, Thalmayer AG, Azocar F, Xu H, Harwood JM, Ong MK, et al. The Mental Health Parity and Addiction Equity Act Evaluation Study: impact on mental health financial requirements among commercial “carve-in” plans. Health Serv Res. 2018;53(1):366–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


