Abstract
Multiple studies have reported the increased risk of pulmonary complications and mortality in patients undergoing surgery with perioperative COVID-19 infection. With several reports of long-term sequelae in patients recovered from COVID-19 infection, this survey was conducted to collect the opinions of anesthesiologists regarding modifications to pre-anesthesia checkup (PAC) when COVID-19 survivors are posted for elective surgeries. We designed, validated and distributed a detailed online questionnaire, about various modifications in PAC in different patient populations like asymptomatic patients, patients with mild, moderate or severe hypoxia, significant cardiac complaints during COVID-19 and also geriatric, pediatric and pregnant patients with a history of COVID-19. We received 154 responses. Majority of responders agree that 0–2 weeks from the date of negative for SARS-CoV-2, is the ideal duration for all elective surgeries. Greater than 50% responders agree that a fresh PAC evaluation should be done for such patients which should include documentation of current functional status, fresh chest X-ray, electrocardiogram and coagulation profile. All patients who had hypoxia or cardiac symptoms during COVID-19 infection and even recovered asymptomatic geriatric patients should undergo cardiorespiratory evaluation with investigations such as HRCT chest, ABG, PFT, echocardiography and troponin I levels. Patients’ PAC should be individualized, factoring in the severity of COVID-19 infection, post recovery functional status, associated co-morbidities and the urgency as well as the risk of surgical intervention.
Supplementary Information
The online version contains supplementary material available at 10.1007/s13193-021-01347-z.
Keywords: COVID-19, Elective surgery, Preoperative anesthesia check-up, PAC
Introduction
Coronavirus disease (COVID-19) pandemic created a havoc with healthcare systems all over the world and brought elective surgeries to almost a standstill for many months during the year 2020. With reduction in fresh COVID-19 cases and shutting down of several COVID-19 centres across India, many beds reserved for COVID-19 patients are increasing being utilized for non-COVID-19 patients. Elective surgeries which had been on hold since the beginning of lockdown, show a cautious resumption. A subset of these patients coming up for elective surgeries may have recently recovered from SARS-CoV-2 infection. This necessitates the need to evaluate or re-evaluate (if already evaluated earlier) these patients by the concerned anesthesiologists in the preoperative period.
There is increasing evidence that recovery from COVID-19 infection is complicated by several sequelae. It has been observed that the virus affects multiple organs, primarily the pulmonary and cardiac systems apart from the brain and neuro-cognitive system, digestive tract, renal system, etc. Additionally, post viral symptoms such as brain fog, memory deficits, headaches and depression have been observed in covid recovered patients, all clubbed under the umbrella term of ‘Post COVID Syndrome’ [1]. COVID-19 infection has been implicated in having long term effects, the nature of which is still evolving and not yet completely predictable or understood. All of this may have implications for the management of such COVID-19 survivors in the perioperative period.
A gamut of anesthesia and surgical societies have come up with general recommendations for resumption of elective surgical workload after easing of the restrictions due to COVID-19 pandemic [2–5]. None of them have suggested a detailed guideline regarding preoperative assessment and risk stratification of COVID-19 recovered patients coming up for elective surgeries. There is only one article on a framework for preoperative evaluation of previously COVID-19 positive patients which is an experience from a single centre in Oregon, USA [1].
This national electronic survey was conducted to collect the opinions of anesthesiologists regarding modifications to both in-patient pre-anesthesia checkup (PAC) or TelePAC (over videoconferencing) when COVID-19 survivors are posted for elective surgeries.
Methods
Institutional Ethics Committee exempted the review of this online, cross-sectional survey. We designed a detailed questionnaire about various modifications in PAC or TelePAC in different patient populations like asymptomatic patients, patients with mild, moderate or severe hypoxia, significant cardiac complaints during COVID-19 and also geriatric, pediatric and pregnant patients with a history of COVID-19. This questionnaire consisted of eighteen semi-open and multiple-choice questions. In the first section, the participants’ demographic information including age, sex, anesthesiology experience, type of practice and institute of practice were collected. In the next section, we collected data on the ideal duration between COVID-19 negative report and conduct of elective surgeries, safety measures during conduct of such PAC, modifications in PAC depending on the severity of COVID-19 infections, need for major surgeries and vulnerable populations namely pediatric, geriatric and obstetric. (ESM_1.pdf).
The content validity of the questionnaire was performed by ten anesthesiologists from all over India, who rated each question on a four-point Likert scale on the basis of simplicity, clarity, ambiguity and relevance for each question. The questionnaire was designed and distributed using Google Forms. The questionnaire was disseminated across the country using snowball sampling technique between 25th December 2020 and 7th February 2021. The Google Forms survey link was sent by email and WhatsApp social media network to anesthesiologists all over India. They were further requested to recommend the survey to other anesthesiology communities known to them. At the end of one and a half month, all the responses were collated, tabulated and analyzed.
The categorical variables were expressed as number and percentages. For the purpose of this study, we have considered the opinions of more than 50% of the responders as significant.
Results
We received a total of 154 responses. There were no incomplete responses. Age and sex distribution, anesthesiology experience and type of practice of the responders are mentioned in Table 1. Maximum responders are in the age group of 31–40 years (33.8%), 53.9% responders have an anesthesiology experience ranging from 5 to 25 years and 59.1% responders are working in government/trust/public healthcare institutes.
Table 1.
Demographic Data
| Parameters | Categories | Number (%) |
|---|---|---|
| Age | < 30 years | 37 (24%) |
| 31–40 years | 52 (33.8%) | |
| 41–50 Years | 41 (26.6%) | |
| 51–60 Years | 16 (10.4%) | |
| > 61 Years | 8 (5.2%) | |
| Sex | Female | 83 (53.9%) |
| Male | 71 (46.1%) | |
| Anaesthesiology experience | Resident | 30 (19.5%) |
| < 5 years | 21 (13.6%) | |
| 5–25 Years | 83 (53.9%) | |
| > 25 Years | 20 (13%) | |
| Type of Practice | Government/Trust/Public healthcare | 91 (59.1%) |
| Corporate/Private | 34 (22.1%) | |
| Freelancer | 29 (18.8%) |
A total of 54.5%, 58.4% and 42.8% responders agree that 0–2 weeks is the ideal duration between COVID-19 negative report and date of elective surgery, when posted for minor or daycare surgeries, time sensitive major surgeries and purely elective major surgeries respectively. (Table 2).
Table 2.
Ideal duration of electives surgery from the time of COVID-19 negative report
| Minor/ Day-care procedures | Time sensitive major surgeries | Purely elective major surgeries | |
|---|---|---|---|
| 0–2 weeks | 84 (54.5%) | 90 (58.4%) | 66 (42.8%) |
| 2–4 weeks | 28 (18.2%) | 35 (22.7%) | 28 (18.2%) |
| 4–8 weeks | 33 (21.4%) | 23 (14.9%) | 34 (22.1%) |
| > 8 weeks | 9 (5.8%) | 6 (3.6%) | 26 (16.9%) |
A total of 55.2% responders feel that conduct of in-person PAC with use of N95 mask, gown, shield and gloves is safe. (Fig. 1).
Fig. 1.
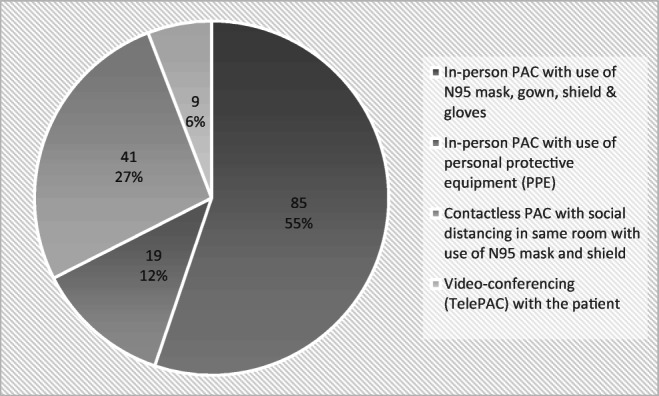
Requirements for safe conduct of PAC
Majority of the responders agree that a post COVID-19 PAC along with optimization of co-morbidities and re-assessment of functional capacity is necessary. Estimation of effort tolerance, breath holding time and 6-min walk test should be done in all patients as applicable. (Table 3) Greater than 50% responders feel that fresh chest X-ray, electrocardiogram and coagulation profile, as applicable, should be done for all COVID-19 recovered patients.
Table 3.
Survey Responses
| Asymptomatic | Mild Hypoxia | Moderate Hypoxia | Severe Hypoxia | Cardiac symptoms | Major surgeries | Geriatric | Pediatric | Obstetric | |
|---|---|---|---|---|---|---|---|---|---|
| No modification | 9 (5.8%) | 1 (0.6%) | 1 (0.6%) | 3 (1.9%) | 3 (1.9%) | 3 (1.9%) | 4 (2.6%) | 20 (13%) | 4 (2.6%) |
| Fresh PAC | 123 (79.9%) | 129 (83.8%) | 133 (86.4%) | 137 (89%) | 140 (90.9%) | 140 (90.9%) | 136 (88.3%) | 133 (86.4%) | 137 (89%) |
| Effort Tolerance | 96 (62.3%) | 123 (79.9%) | 124 (80.5%) | 136 (88.3%) | 134 (87%) | 135 (87.7%) | 128 (83.1%) | ||
| BHT | 99 (64.3%) | 111 (72.1%) | 114 (74%) | 118 (76.6%) | 106 (68.8%) | 110 (71.4%) | 105 (68.2%) | ||
| 6 MWT | 86 (55.8%) | 101 (65.6%) | 113 (73.4%) | 109 (70.8%) | 107 (69.5%) | 110 (71.4%) | 87 (56.5%) | ||
| Chest X-ray | 110 (71.4%) | 115 (74.7%) | 113 (73.4%) | 111 (72.1) | 100 (64.9%) | 115 (74.7%) | 115 (74.7%) | 124 (80.5%) | |
| ECG | 85 (55.2%) | 107 (69.5%) | 118 (76.6%) | 128 (83.1%) | 140 (90.9%) | 133 (86.4%) | 131 (85.1%) | 115 (74.7%) | |
| Coagulation profile | 82 (53.2%) | 95 (61.7%) | 110 (71.4%) | 127 (82.5%) | 121 (78.6%) | 131 (85.1%) | 112 (72.7%) | 80 (51.9%) | 120 (77.9%) |
| ABG | 23 (14.9%) | 60 (39%) | 98 (63.6%) | 127 (82.5%) | 115 (74.7%) | 113 (73.4%) | 85 (55.2%) | 34 (22.1%) | 55 (35.7%) |
| HRCT chest | 37 (24%) | 83 (53.9%) | 115 (74.7%) | 142 (92.2%) | 122 (79.2%) | 119 (77.3%) | 93 (60.4%) | 38 (24.7%) | |
| PFT | 29 (18.8%) | 71 (46.1%) | 98 (63.6%) | 126 (81.8%) | 103 (66.9%) | 117 (76%) | 83 (53.9%) | 36 (23.4%) | |
| Troponin I | 19 (12.3) | 24 (15.6%) | 40 (26%) | 65 (42.2%) | 118 (76.6%) | 79 (51.3%) | 58 (37.7%) | 10 (6.5%) | 27 (17.5%) |
| 2D echocardiography | 36 (23.4%) | 68 (44.2%) | 92 (59.7%) | 119 (77.3%) | 146 (94.8%) | 134 (87%) | 129 (83.8%) | 27 (17.5%) | 81 (52.6%) |
BHT: Breadth holding time, 6 MWT: 6 Minute Walk Test, ECG: Electrocardiogram, ABG: Arterial Blood Gases, HRCT: High resolution computer tomography, PFT: Pulmonary function test
With regard to the assessment of the pulmonary status post COVID-19, more than 50% responders feel that arterial blood gases, high resolution computer tomography scan (HRCT) of chest and pulmonary function tests need to be recorded in all patients who had moderate to severe hypoxia or significant cardiac symptoms during COVID-19; in patients posted for major abdominal, thoracic, cardiac or vascular surgeries and geriatric patients. HRCT chest also needs to be done in patients who had mild hypoxia (53.9%).
For assessing the cardiac status post COVID, troponin I levels need to be recorded in patients who had significant cardiac symptoms during COVID-19 (76.6%) and patients posted for major abdominal, thoracic, cardiac and vascular surgery (51.3%). Greater than 50% responders agree that two-dimensional echocardiography should be done in patients who had moderate to severe hypoxia and significant cardiac symptoms during COVID-19 infection as also those posted for major surgeries, geriatric and obstetric patients. A few responders (1.9%) suggested NT proBNP as a requirement for patients who had significant cardiac symptoms, followed by cardiac consultation and further testing as suggested by the results of the above investigations.
Discussion
Multiple studies have reported the increased risk of pulmonary complications and mortality in patients undergoing surgery with perioperative COVID-19 infection. [6–8] Data is scarce on patients who undergo surgery after recovery from COVID-19. There are several reports arising about deleterious effects of COVID-19 on multiple organs, especially the cardiopulmonary systems, even after recovery from COVID-19 infection. This survey was conducted from 25th December 2020 to 7th February 2021 when the first wave of COVID-19 pandemic was on the wane and elective surgeries received a fillip. We observed that COVID-19 survivors were a large subset of these patients coming up for elective surgeries. Intending to cater to the PAC needs of this cadre of patients, we designed our questionnaire accordingly.
Majority of our responders are in the age group of 31 to 50 years, having 5–25 years of anesthesiology experience, with maximum response from those working in government/trust/public healthcare institutes.
Greater than 50% responders feel that the conduct of in-person PAC with use of N95 mask, gown, shield and gloves is safe in COVID-19 recovered patients. Above mentioned safety measures are the general recommendations for conduct of PAC during the COVID-19 pandemic, which is also applicable to assessment of COVID-19 survivors [2, 4]. Since COVID-19 cases are on a rise again (second and subsequent waves) and since TelePAC may be a norm in some settings for quite a long time, modifications to the PAC are applicable to both in-person and TelePAC [9].
Majority of our responders feel that all elective surgeries, whether minor/daycare or major, in COVID-19 survivors can be performed within two weeks after COVID-19 negative reports, following a PAC re-evaluation and optimization. American Society of Anesthesiologists and Anesthesia Patient Safety Foundation Joint Statement on Elective Surgery and Anesthesia for Patients after COVID-19 Infection recommend a symptom and severity-based categorization to address the timing of elective surgery post recovery [3]. They recommend a delay of four to six weeks for asymptomatic or mildly symptomatic patients who did not require hospitalization; eight to ten weeks for symptomatic patients who were diabetic, immunocompromised or hospitalized; and twelve weeks for patients admitted to an intensive care unit due to COVID-19 infection. In view of lack of evidence-based recommendations, these guidelines are derived from the cardiopulmonary recovery rates extrapolated from similar human coronavirus infections in the past such as Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS). A study from Brazil has reported that in a small cohort of forty nine asymptomatic COVID-19 recovered patients who underwent oncological surgeries, around 25 days post COVID-19 diagnosis (range 12–84 days), were not at a higher risk of postoperative complications as compared to patients with no COVID-19 history [10]. The study from UK found that both pulmonary complications and mortality after curative cancer surgery were at their lowest with the interval of four weeks after the first COVID-19 positive swab [11]. Our survey was performed well before the publication of the COVIDSurg Collaborative and GlobalSurg Collaborative on the timing of surgery following SARS-CoV-2 infection, which found that a ≥ 7 week delay after COVID-19 diagnosis, was associated with a similar mortality risk as baseline [12]. Even after this 7 week delay, patients with ongoing symptoms had a higher mortality as compared to patients who were asymptomatic or those whose symptoms had resolved. The various societys’ or Institute’s recommendations are unanimous in recommending a comprehensive preoperative evaluation and optimization of co-morbidities and physiologic status of all COVID-19 recovered patients, especially those with residual symptoms, prior to posting them for elective surgery [1–4].
Majority of the responders agree that a fresh or re-evaluation of PAC of all COVID-19 survivors should include functional capacity testing with documentation of post covid recovery effort tolerance, breath holding time and six-minute walk test. These are simple bedside cardiopulmonary function tests which can give us an idea about the immediate preoperative cardiovascular reserve of these patients and may allow comparison to pre-covid baseline, if such data is available. While post COVID-19 effort tolerance is subjective, both breath holding time and 6-min walk test are fairly objective. These can be performed during the conduct of PAC and do not require any additional expenditure on the part of the patients. It may not be possible to perform these tests in young pediatric or obstetric population and hence have not been included as PAC modifications for this population. Apart from above mentioned tests, Bui et al. have also recommended a frailty assessment on the Edmonton Frail scale for all such patients above 65 years of age or those who were hospitalized for COVID-19 [1].
Most of our responders also feel that a chest X-ray, electrocardiogram and a coagulation profile post COVID-19, should be done as part of the PAC for all COVID-19 recovered patients irrespective of the severity. COVID-19 causing a procoagulant state, with cardiopulmonary system being the primarily affected organs, these are baseline investigations commonly requested prior to any surgery. Further assessment of cardiopulmonary status depends on the severity of COVID-19 infection, residual symptoms post COVID-19, potential for reversibility of any complications and prognostication of postoperative complications.
Since respiratory system is the most significantly affected organ in COVID-19, post recovery assessment of pulmonary system becomes paramount. A review article has presented a detailed narrative on pathogenesis of pulmonary fibrosis after coronavirus infections, including COVID-19, SARS and MERS [13]. They report that the presence of initial ground glass opacities on CT chest progressed to interlobular septal thickening and traction bronchiectasis (features suggestive of pulmonary fibrosis) in 30–62% of the patients recovered form SARS. They found that during 12-month follow up, many of these patients progressed to lung fibrosis and diffusion abnormalities which progressively improved over the one-year period. None of the patients showed any abnormalities on pulmonary function tests. The article reports that although fibrotic changes have been noted on chest CT scans of COVID-19 patients, further literature is awaited on whether these changes are reversible or progress to fixed pulmonary fibrosis. Elective surgery in such patients may further complicate the scenario with the recovering lungs being vulnerable to secondary injury due to perioperative anesthesia and critical care needs. They also report that pulmonary fibrosis is more frequently observed in geriatric patients following SARS and MERS. The study from UK found that in a propensity score matched model, postoperative pulmonary complications were higher in COVID-19 recovered patients as compared to those with no COVID-19, when undergoing curative cancer surgery [11]. Bui et al. have included a complete metabolic panel and an ambulatory pulse oximetry measurement in their PAC protocol along with chest X-ray [1]. They do not recommend pulmonary function tests and arterial blood gases due to unclear data on clinical significance with regard to perioperative outcomes.
Myocarditis, myocardial infarction, cardiomyopathies, arrythmias, shock and cardiac arrest are some of the complications associated with COVID-19 infection, necessitating cardiac status evaluation in COVID-19 recovered patients [14, 15]. Both SARS and MERS have been associated with myocardial injury and myocarditis with elevated troponin levels. A few studies with small cohorts, have reported an elevated troponin levels in 5–17% of patients hospitalized with COVID-19 and 22–31% of those admitted to intensive care unit with COVID-19 [14]. Patients with myocardial injury may present a range of findings in the electrocardiogram such as ST-T wave changes, T wave inversions and PR abnormalities. Echocardiography helps differentiate myocarditis from acute myocardial infarcts with a focus on regional wall motion abnormalities. Further cardiac evaluations along with NT proBNP and stress tests may be indicated depending on the current status and results of the above tests. Cardiac complications have been found to be progressively higher in patients with worsening severity of respiratory symptoms. Apart from electrocardiogram and echocardiography, Bui et al. have included NT proBNP assessment for all symptomatic (during COVID-19) patients posted for minor and all patients posted for major surgeries [1]. Akin to pulmonary fibrosis, the cardiovascular complications are more likely to occur in geriatric populations [15]. Studies performed in pediatric populations with COVID-19 reveal a normal cardiac laboratory profile [4, 15]. There is no specific data of outcomes of obstetric patients who have recovered from COVID-19. Although cardiac complications are likely during COVID-19 infections, literature is scarce on the long-term morbidity and mortality from these cardiac complications.
Eventually every patients’ PAC should be individualized, factoring in the severity of COVID-19 infection, post recovery functional status, associated co-morbidities and the urgency as well as the risk of surgical intervention. A few anesthesia societies recommend the formation of a prioritization policy or an operating schedule control committee constituting the surgical, anesthesia/critical care and nursing leadership to develop a strategy to streamline the whole process [2, 4]. The various anesthesia societies stress that the protocols and policies should be re-evaluated frequently, based on emerging COVID-19 outcomes related data.
Conclusion
The COVID-19 recovered patients can be posted for elective surgeries within 0–2 weeks from the date of negative for SARS-CoV-2 report. The increase in the number of COVID-19 recovered patients coming up for elective surgery lends itself to a comprehensive preoperative evaluation and risk assessment prior to posting them. Integration of good clinical skills and an array of diagnostic investigations may help us to assess each patient in the absence of clear scientific data on outcomes of these patients after elective surgeries.
Supplementary Information
(PDF 163 kb)
Code Availability
Nil
Authors’ Contributions
All authors whose names appear on the submission made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; drafted the work or revised it critically for important intellectual content; approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Data Availability
Included in Tables and supplementary files.
Declarations
Ethics Approval
This is an online survey. Ethical approval was waived by the Institutional Ethics Board-II (TMC).
Consent to Participate
Included in survey form.
Consent for Publication
Obtained.
Conflicts of Interest/Competing Interests
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bui N, Coetzer M, Schenning KJ, O’Glasser AY. Preparing previously COVID-19-positive patients for elective surgery: a framework for preoperative evaluation. Perioper Med. 2021;10:2–5. doi: 10.1186/s13741-020-00172-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Society of Anesthesiologists [homepage on the Internet]. Joint Statement: Roadmap for Resuming Elective Surgery after COVID-19 Pandemic. [updated on 2020 Apr 17; cited on 2021 Apr 15]. Available from: https://www.asahq.org/about-asa/newsroom/news-releases/2020/04/joint-statement-on-elective-surgery-after-covid-19-pandemic
- 3.American Society of Anesthesiologists [homepage on the Internet]. American Society of Anesthesiologists and Anesthesia Patient Safety Foundation Joint Statement on Elective Surgery and Anesthesia for Patients after COVID-19 Infection. [updated on 2020 Dec 08; cited on 2021 Apr 15]. Available from: https://www.asahq.org/about-asa/newsroom/news-releases/2020/12/asa-and-apsf-joint-statement-on-elective-surgery-and-anesthesia-for-patients-after-covid-19-infection
- 4.Velly L, Gayat E, Quintard H, Weiss E, De Jong A, Cuvillon P, et al. Guidelines: Anaesthesia in the context of COVID-19 pandemic. Anaesth Crit Care Pain Med. 2020;39:395–415. doi: 10.1016/j.accpm.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solanki SL, Thota RS, Garg R, Pingle AA, Goswami J, Ranganath N, Mukherjee S, Gupta S, Patkar S, Chikkalingegowda RH, Jindal T, Ray MD, Upadhye SM, Divatia JV (2020) Society of Onco-Anesthesia and Perioperative Care (SOAPC) advisory regarding perioperative management of onco-surgeries during COVID-19 pandemic. Indian J Anaesth 64(Suppl 2):S97–S102 [DOI] [PMC free article] [PubMed]
- 6.COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet (London, England) 2020;396(10243):27–38 [DOI] [PMC free article] [PubMed]
- 7.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, Zhan LY, Jia Y, Zhang L, Liu D, Xia ZY, Xia Z. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jonker PKC, Van Der Plas WY, Steinkamp PJ. Perioperative SARS-CoV-2 infections increase mortality, pulmonary complications, and thromboembolic events: a Dutch, multicenter, matched-cohort clinical study. Surgery. 2020;169:264–274. doi: 10.1016/j.surg.2020.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Srivastava D, Solanki SL, Ambasta S, Chandra A. Tele-Preanesthetic check-ups (TelePAC) during COVID-19: apprehensions and possibilities. J Anaesthesiol Clin Pharmacol. 2020;36:415–417. doi: 10.4103/joacp.JOACP_343_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baiocchi G, Aguiar S, Duprat JP, Coimbra FJF, Makdissi FB, Vartanian JG, et al. Early postoperative outcomes among patients with delayed surgeries after preoperative positive test for SARS-CoV-2: A case-control study from a single institution. J Surg Oncol 2021;(Mar):823–33 [DOI] [PMC free article] [PubMed]
- 11.COVIDSurg Collaborative. Delaying surgery for patients with a previous SARS-CoV-2 infection. Br J Surg 2020;107(12):e601–e602 [DOI] [PMC free article] [PubMed]
- 12.COVIDSurg Collaborative, GlobalSurg Collaborative. Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia 2021; Mar 09. Epub ahead of print [DOI] [PMC free article] [PubMed]
- 13.Ojo AS, Balogun SA, Williams OT, Ojo OS. Pulmonary fibrosis in COVID-19 survivors: predictive factors and risk reduction strategies. Pulm Med. 2020;2020:6175964. doi: 10.1155/2020/6175964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Long B, Brady WJ, Koyfman A, Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020;38:1504–1507. doi: 10.1016/j.ajem.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Petrovic V, Radenkovic D, Radenkovic G, Djordjevic V, Banach M. Pathophysiology of cardiovascular complications in COVID-19. Front Physiol. 2020;11:1–11. doi: 10.3389/fphys.2020.575600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 163 kb)
Data Availability Statement
Included in Tables and supplementary files.


