Abstract
BACKGROUND AND PURPOSE: Although diagnostic lumbar selective nerve root blocks are often used to confirm the pain-generating nerve root level, the reported accuracy of these blocks has been variable and their usefulness is controversial. The purpose of this study was to evaluate the accuracy of diagnostic lumbar selective nerve root blocks to analyze potential causes of false results in a prospective, controlled, single-blinded manner.
Materials and METHODS: A total of 105 block anesthetics were performed under fluoroscopic guidance in 47 consecutive patients with pure radiculopathy from a single confirmed level: 47 blocks were performed at the symptomatic level, and 58 were performed at the adjacent asymptomatic “control” level. Contrast and local anesthetics were injected, and spot radiographs were taken in all cases. We calculated the diagnostic value of the block anesthetics using concordance with the injected level. We analyzed the potential causes of false results using spot radiographs.
RESULTS: On the basis of a definition of a positive block as 70% pain relief, determined by receiver-operator characteristic (ROC) analysis, diagnostic lumbar selective nerve root block anesthetics had a sensitivity of 57%, a specificity of 86%, an accuracy of 73%, a positive predictive value of 77%, and a negative predictive value of 71%. False-negatives were due to the following causes identifiable on spot radiographs: insufficient infiltration, insufficient passage of the injectate, and intraepineural injections. On the other hand, false-positives resulted from overflow of the injectate from the injected asymptomatic level into either the epidural space or symptomatic level.
CONCLUSION: The accuracy of diagnostic lumbar selective nerve root blocks is only moderate. To improve the accuracy, great care should be taken to avoid inadequate blocks and overflow, and to precisely interpret spot radiographs.
Diagnostic selective nerve root blocks (DSNRB) are often used to confirm the pain-generating root level. Despite its widespread use, the reported accuracy of such blocks at determining the symptomatic level varies from 31% to 100%.1–11 In addition to the wide range in the accuracy, unfortunately, most of these studies1–9 have been retrospective in nature, have had a small sample size,7–9 and have failed to describe their methodologies in detail.5 Furthermore, in all studies on the topic to date, the definition of a positive or negative result based on the degree of pain relief has been arbitrarily set between 50% and 100% or has not been clearly described.1–11 In addition, none of these studies1–11 have analyzed the sensitivity, specificity, accuracy, and predictive values because they focus on the results of DSNRB on the presumed lesion level alone, and none of the studies used injections at unaffected “control” roots.
Because of the technical difficulty in selectively anesthetizing a single root and the shortcomings of the studies published to date, the diagnostic accuracy of selective nerve root blocks has been questioned by some authors.12–14 Despite the limitations, others4,14,15 have supported the use of DSNRBs. Given this controversy, we decided to perform a prospective, controlled, blinded study to evaluate the sensitivity, specificity, accuracy, and predictive value of these blocks on unaffected, as well as affected, roots. More specifically, the purpose of this study was threefold: first, to determine the cutoff value of percent relief of the radiating pain for defining a positive and a negative block result; second, to evaluate the diagnostic value of selective nerve root blocks with use of a prospective, controlled, single-blinded design in consecutive patients with a single-level lumbosacral radiculopathy; and third, to identify the potential factors for improvement of the diagnostic value by analyzing spot radiographs. By performing the study and understanding the value of DSNRBs in the treatment of single-level radiculopathy, we would then gain a better appreciation of the role DSNRBs may play in determination of the pain-generating root level in patients with multilevel radiculopathy.
Methods
DSNRBs have been used by the authors before initiating this study in patients with both multilevel and single-level radiculopathy in an attempt to localize and confirm the source of pain, and if possible, to try to avoid surgery. Once it became clear that our study was needed, we recruited potential candidates and instructed to them that control blocks on unaffected levels were not a routine prerequisite for surgery and that their participation in the study was strictly voluntary. Only those patients who volunteered to participate in the study were enrolled. Associated expenses were paid for by a grant obtained specifically to carry out this study. The study received the approval of our institutional review board, and written informed consents were obtained from all enrolled patients.
Patient Selection and Determination of the Monoradiculopathy Level
To determine the diagnostic capability of blocks, we had to first establish a criterion standard for a monoradiculopathy. We took multiple steps to try to ensure that we selected only patients with true monoradicular leg pain.
First Step.
Patients who underwent an operation between January 2005 and April 2006 with a single-level, unilateral lumbosacral radiculopathy confirmed by clinical, radiographic, and MR imaging findings were initially included as potential candidates for the study. Exclusion criteria included multilevel or bilateral neural compression on MR imaging, incompatible or infrequent clinical findings (incompatible distribution of sensory change or pain; infrequent motor weakness, such as decreased power of ankle dorsiflexor in a patient having an L5 lesion on MR imaging; and decreased straight-leg raising or normal femoral stretching test in L4 radiculopathy), transitional vertebrae, coexisting extraspinal lesion or peripheral neuropathy, and previous history of any lumbar surgeries. We did not exclude patients with an annular tear (high-intensity zone), mild disk bulging without neural compression, or minimal facet arthropathy in the same or other levels, as long as the monoradiculopathy at the index level was clearly confirmed by clinical, radiographic, and MR imaging findings. Electromyelography was not used in patient selection except in a few patients who were excluded because of peripheral neuropathy. The patients who fulfilled the above criteria and accepted participation in this study were sent for DSNRBs performed in the manner described below.
Second Step.
Patients who had prolonged relief of pain after the first injection that precluded proper evaluation of the next block or those whose operations were canceled because of persistent pain relief after DSNRB were excluded from the study. Those passing the second step then went on to their operations, as planned. Only a single-level root decompression or diskectomy was performed in each patient.
Third Step.
The operative findings had to correlate with the images to verify the cause-effect relationship. We further excluded any patients who, in their opinion, failed to obtain complete or nearly complete relief of their radiating pain immediately after the operation, because we could not clearly determine if the poor surgical result was from the failed operation, picking the wrong level, missing hidden extraspinal causes of neural compression, or other causes.
Fourth Step.
An independent review of all data by spine surgeons uninvolved in the care of the patients was performed within 1 to 2 weeks of surgery to recheck and exclude any patients whose conditions were inappropriate for this study. The group determined if the patient indeed had a monoradiculopathy that was caused by the level that was operated on. If unanimous agreement was not achieved on any patient, that patient was excluded.
DSNRB Procedure and Assessment of Its Effect
At 1 or 2 days preoperatively, an attending spinal radiologist, who had experience performing several thousand lumbar nerve root blocks, and his 2 colleagues performed DSNRBs using published techniques.15 In brief, the injections were performed in an angiography suite equipped with biplanar fluoroscopy (Integris Allura 12 & 12 Biplane; Phillips Medical Systems, Best, the Netherlands) while the patient lay prone. After sterile preparation, draping, and local anesthesia with 1% lidocaine, a 12-cm, 22-gauge spinal needle was advanced and positioned near the target nerve root. The target point was around the neural foramen. The needle position was checked by biplanar fluoroscopy. Pain provocation with nerve root irritation by needle contact was not carried out. After injecting 1 mL of iohexol myelographic contrast agent (Omnipaque 300; Amersham Health, Princeton, NJ), anteroposterior and lateral digital spot radiographs were taken and stored in the PACS server. Then, 1 mL of 2% lidocaine was injected.
DSNRBs were done at the presumed pain-generating level and also on 1 or 2 adjacent control levels in a random-sequence fashion. A minimum of 6 hours elapsed between blocks. In patients with an S1 radiculopathy, only an L5 block was used as a control. In patients with a pathologic lesion in other levels, control blocks on both cranial and caudal levels were performed serially, unless patients' refusal, prolonged pain relief after the second block, or limited time before surgery precluded a third block. Although the patients were blinded as to the levels of the blocks, blinding obviously could not be applied to the physicians administering the injections. Therefore, this was a single-blinded study.
An orthopedic research nurse, blinded to the injection level, asked the patients to rate the percentage of decrease in their radiating pain compared with the preinjection state at 30 minutes after the injection. Although the level of pain before the injection was assessed with use of a 10-point visual analog scale (VAS) with 0 defined as no pain and 10 defined as the worst pain, patients were asked to assess the block results by using a percentage decrease in the preinjection pain, because, in our experience, we found this method to be a more accurate method of assessing the degree of pain improvement.
Diagnostic Value
To calculate the diagnostic value of DSNRB, we first had to define a “cutoff value” of percentage decrease in radiating pain for a “positive” block. We performed a receiver-operator characteristic (ROC) analysis to determine the optimal value of this cutoff. True-positives were defined as a positive effect on the affected root and false-positives, as a positive effect on a control root. True-negatives were defined as a negative effect on the control root and false-negatives as a negative effect on the affected root. The sensitivity, specificity, accuracy, and positive and negative predictive values were calculated.
At 3 months after the data collection was completed, all radiographic studies were reviewed by the attending spinal radiologist, who was blinded to the degree of pain relief after DSNRB. For each block, he determined the presence or absence of the potential causes of false results on the spot radiographs. In a few cases, there were 2 or more spot radiographs with different needle tip positions for 1 block, which meant that the needle was repositioned. In those cases, the analyses were done with use of the findings seen only on the final radiographs, ignoring the distribution of the contrast media, which was also seen on the other radiographs.
Statistical Analysis
We performed statistical analyses with the SPSS 12.0 software (SPSS, Chicago, Ill). We analyzed the relationship between the findings on spot radiographs and the occurrence of false results using the Fisher exact test. The confidence interval was set at 95%.
Results
Patients
Ninety-five potential candidates were approached and asked if they would participate in the study. Of the 95 patients, 83 agreed to participate and were enrolled. Because of our strict inclusion and exclusion criteria, 15 were excluded after the DSNRB; 12 were excluded postoperatively; and an additional 9 were excluded after independent panel review, leaving a total of 47 patients in the study (28 men, 19 women; ages 18–76 years, mean age, 47 years). There were 4 patients who had foraminal stenosis, 3 with isthmic spondylolisthesis, and 40 with herniated disks (36 paracentral, 3 foraminal, 1 extraforaminal). Affected roots were L4 in 3, L5 in 31, and S1 in 13. The median duration of radiating pain was 3 months (range, 15 days to 3 years). Preinjection VAS averaged 8.0 (range, 6–10), and Oswestry disability index was 53.0 (range, 32–96). We performed 58 blocks at 1 or 2 control roots: 1 in L3, 18 in L4, 15 in L5, and 24 in S1. A total of 105 DSNRBs were performed.
ROC Analysis and Diagnostic Value of DSNRB
The results of an ROC analysis to determine the optimal cutoff value for the definition of a positive DSNRB are shown in Table 1. This shows that the higher the cutoff value, the higher the specificity, but the lower the sensitivity. We chose 70% pain relief because it had the highest accuracy (73%). With the 70% cutoff, there were 27 true-positives, 50 true-negatives, 8 false-positives, and 20 false-negatives. The sensitivity of the DSNRB was 57% (27/47), with a specificity of 86% (50/58), accuracy of 73% (77/105), positive predictive value of 77% (27/35), and negative predictive value of 71% (50/70) (Table 2).
Table 1:
Results of receiver-operator characteristic (ROC) analysis for cutoff value for the definition of a positive result
| Cutoff Value (%) | Sensitivity (%) | Specificity (%) | Accuracy (%) | Positive Predictive Value (%) | Negative Predictive Value (%) |
|---|---|---|---|---|---|
| ≥0 | 100 | 0 | 45 | 45 | - |
| ≥10 | 91 | 21 | 52 | 48 | 75 |
| ≥20 | 89 | 26 | 54 | 49 | 75 |
| ≥30 | 79 | 40 | 57 | 51 | 70 |
| ≥40 | 72 | 50 | 60 | 54 | 69 |
| ≥50 | 70 | 74 | 72 | 69 | 75 |
| ≥60 | 60 | 78 | 70 | 68 | 70 |
| ≥70 | 57 | 86 | 73 | 77 | 71 |
| ≥80 | 36 | 90 | 66 | 74 | 63 |
| ≥90 | 21 | 91 | 60 | 67 | 59 |
| =100 | 4 | 100 | 57 | 100 | 56 |
Note:—Cutoff value indicates the cutoff value of percent decrease in radiating pain compared with the pre-injection state.
Table 2:
Diagnostic value of DSNRB with the cutoff value for positive result set at 70%
| Estimate | All Patients | Patients Without Two Findings* on Spot Radiographs |
|---|---|---|
| Sensitivity | 57% (27/47) | 71% (25/35) |
| (42, 72)† | (54, 85)† | |
| Specificity | 86% (50/58) | 91% (43/47) |
| (75, 94)† | (80, 98)† | |
| Accuracy | 73% (77/105) | 83% (68/82) |
| (64, 81)† | (73, 90)† | |
| Positive predictive value | 77% (27/35) | 86% (25/29) |
| (60, 90)† | (68, 96)† | |
| Negative predictive value | 71% (50/70) | 81% (43/53) |
| (59, 82)† | (68, 91)† |
Two findings indicate inadequate blocks (including insufficient infiltration, insufficient passage, and intraepineural injection) and overflow.
Shown in parentheses are 95% confidence intervals.
Causative Findings of False Results on Spot Radiographs
On the spot radiographs, 10 of the 20 false-negative cases were deemed to be “inadequate blocks” (Table 3). There were 3 types of inadequate blocks (Figs 1 and 2). In 4 of these, the inadequate block was caused by “insufficient infiltration” of the affected areas with injectate leakage into the surrounding neighborhood tissues (Fig 1A) including the muscles and anterior S1–2 foramen in S1 root block. In the other 4 cases, the cause of the inadequate block was “insufficient passage” of injectate because of a blockade by a huge paracentral herniated disk (Fig 1B). In typical circumstances, the injectate spread medially to outline the caudal margin of the herniated disk and could spread even to the medial epidural space slightly, but it could not spread to a more cephalic portion, where the root was compressed by the herniated disk. In the other 2 cases, false-negatives were caused by intraepineural injections (Fig 2A).16 The causes of the remaining 10 false-negatives were not identified on spot radiographs.
Table 3:
Causative findings of false results on spot radiographs
| Findings | Numbers | |
|---|---|---|
| False-negative | ||
| Inadequate block | 10 | |
| Insufficient infiltration with injectate leakage | 4 | |
| Insufficient passage of injectate from a blockade by a huge herniated disk | 4 | |
| Intraepineural injection | 2 | |
| Not identified on spot radiographs | 10 | |
| False-positive | ||
| Overflow of injectate into the epidural space or into an adjacent affected level | 4 | |
| From an injected upper unaffected level | 2 | |
| From a injected lower unaffected level | 2 | |
| Not identified on spot radiographs | 4 | |
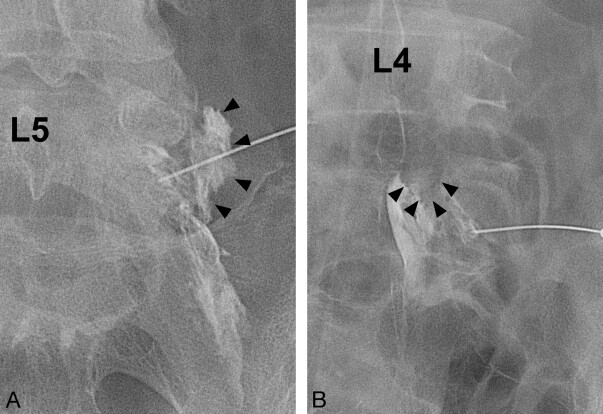
Fig 1.
Insufficient infiltration and insufficient passage. A, Insufficient infiltration of the root, compressed by the herniated L4–5 disk. Contrast leakage lateral to the neural foramen (arrowheads) is observed. B, Insufficient passage of the injectate from a blockade by a huge herniated disk. A filling defect of contrast media by an inferiorly migrated huge paracentral disk herniation at L4–5 is observed (arrowheads).
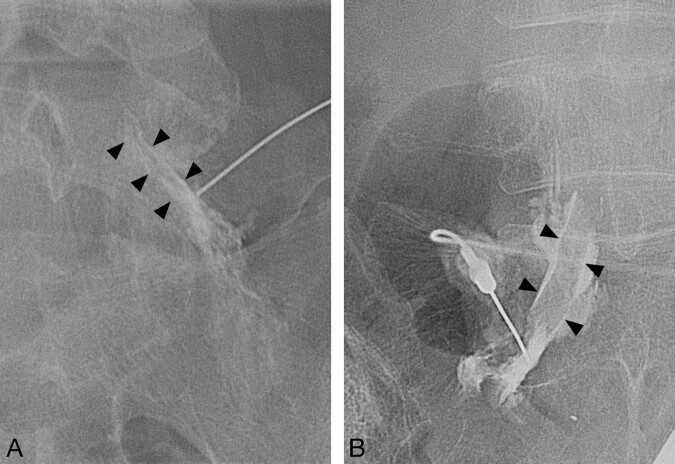
Fig 2.
Intraepineural and extraepineural injections. A, Intraepineural injection causing aggravation of the radiating pain during the procedure, resulting in a false-negative. Central feathery appearance within the tubular outline of the root (arrowheads) is observed. B, Extraepineural injection showing the root as a linear filling defect (arrowheads).
In 4 of 8 false-positive results, there was overflow of lidocaine from the control level into the epidural space or into the symptomatic level (Table 3). This overflow of injectate came from an upper level in 2 cases and a lower level in 2 (Fig 3). The causes of the remaining 4 false-positives were not identified on spot radiographs.
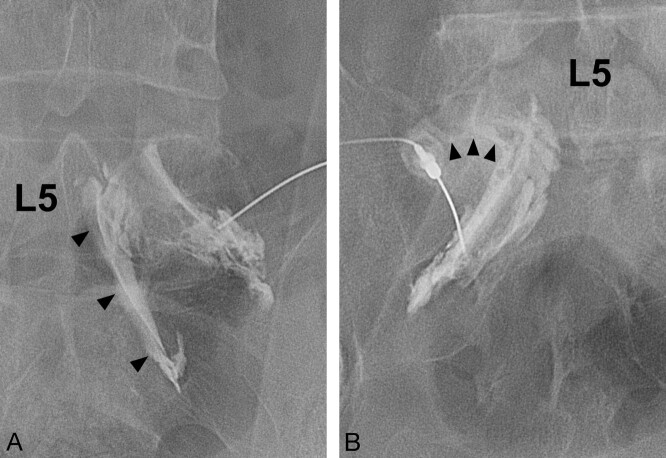
Fig 3.
Overflow of injectate. A, Injectate from the unaffected L5 root spreads caudally to the affected S1 nerve root (arrowheads), causing a false-positive result. B, Injectate from the unaffected S1 root spreads cranially to the affected L5 root (arrowheads), causing a false-positive result.
We performed additional statistical analyses on the relationship between the above spot radiographic findings and the occurrence of false results. Among 12 inadequate blocks, 10 were false-negatives and 2 were true-positives (Table 4). Although inadequate blocks did not always lead to a false-negative result, there was a statistically significant increase in the false-negative rate in the group with inadequate blocks than in the group without them (P = .002, Fisher exact test). Among 11 cases having overflow of the injectate into the epidural space or into the adjacent affected level from a control level, 4 were false-positives and 7 were true-negatives (Table 5). Although the overflow did not always lead to a false-positive result, there was a statistically significant increase in the false-positive rate in the group with the overflow compared with the group without it (P = .03, Fisher exact test).
Table 4:
Inadequate block and false-negative rate of diagnostic selective nerve root block
| Inadequate Block | Results of DSNRB |
False-Negative Rate | PValue (Fisher Exact Test) | |
|---|---|---|---|---|
| False-Negative | True-Positive | |||
| Present | 10 | 2 | 83% (10/12) | .002 |
| Absent | 10 | 25 | 29% (10/35) | |
Note:—DSNRB indicates diagnostic selective nerve root block.
Table 5:
Overflow of the injectate and false-positive rate of diagnostic selective nerve root block
| Overflow of the Injectate | Results of DSNRB |
False-Positive Rate | PValue (Fisher Exact Test) | |
|---|---|---|---|---|
| False-Positive | True-Negative | |||
| Present | 4 | 7 | 36% (4/11) | .03 |
| Absent | 4 | 43 | 6% (4/47) | |
Note:—DSNRB indicates diagnostic selective nerve root block.
When we again calculated the diagnostic value using 82 blocks, excluding the 23 blocks with the above 2 radiographic findings which might or might not lead to false results, the values improved as follows: sensitivity improved from 57% to 71%, specificity improved from 86% to 91%, accuracy improved from 73% to 83%, positive predictive value improved from 77% to 86%, and negative predictive value improved from 71% to 81% (Table 2).
Discussion
Lumbosacral DSNRBs are often used to identify the pain generator. However, there is controversy regarding the accuracy of these blocks, given the possibility of a negative block at a presumed pain-generating level or, alternatively, a positive block at a presumed innocent level. We decided to carry out a study to determine the diagnostic value of DSNRB including sensitivity, specificity, accuracy, and predictive values. To the best of our knowledge, this is the first prospective, controlled study to determine those values with use of control injections on unaffected adjacent levels as well as on the affected levels.
We found that the diagnostic value of DSNRB was only moderate. The diagnostic value was relatively low compared with previous reports,1–11 most of which did not measure false-positives on unaffected control roots. Often in clinical practice, the therapeutic effect is the most important aspect of a nerve root block, and attention is typically paid to assure sufficient infiltration rather than worrying about selectivity of the block. When performing a diagnostic block, however, selectively blocking a single level becomes paramount. Our radiologists assiduously tried to “selectively” block only 1 root to minimize false-positive results. The obvious potential disadvantage of this approach is that when one concentrates on lowering the false-positives, the unintended consequence may be to increase the false-negatives. This could be one of the reasons for our relatively low diagnostic value.
The identifiable cause of false-negatives was inadequate block because of insufficient infiltration with injectate leakage, insufficient passage of injectate resulting from a blockade by a huge herniated disk acting as a barrier, or intraepineural injection. Although “insufficient infiltration” is thought to be a technical error by the physicians, “insufficient passage of injectate” is thought to be a result of the characteristic of the lesion itself (eg, a huge herniated disk rather than a technical error such as inappropriate needle positioning). Although there has been no report on this phenomenon, we believe it could cause false-negative results because all of the 4 blocks with this spot radiographic finding resulted in false-negative results. Another cause of false-negative results was an intraepineural injection, which temporarily aggravated the radiating pain rather than alleviating it. Pfirrmann et al16, in their study on the therapeutic root block, reported that intraepineural injections were more commonly painful at the time of injection than were extraepineural injections.
In contrast to the false-negative results, there was only 1 identifiable cause for false-positive results. This was because of overflow of the injectate from an asymptomatic level into the adjacent affected one or into the epidural space, where it might nonselectively block several levels including the symptomatic one.
In previous studies1–11 the degree of pain relief required for a block to be considered positive was set arbitrarily between 50% and 100% or was not clearly described.1–11 Furthermore, none of the studies used ROC analysis to determine the ideal cutoff for a block to be considered positive. A higher cutoff increases true-negatives and false-negatives, and a lower one increases false-positives and true-positives. One might think that a 90% or 100% improvement with the block might be desirable. However, high values increase the specificity but significantly decrease sensitivity and accuracy. In our study, the ROC analysis demonstrated that 70% was the optimal cutoff value, having the largest number of DSNRBs with correct diagnoses. However, one could argue for the use of higher cutoff values in situations in which high specificity is desirable, at the expense of sensitivity and accuracy.
Limitations of Our Study and Possible Causes of Unexplained False Results
As with any study, there were a number of limitations with ours. First, defining a positive response to DSNRB had an inherent problem in that the degree of improvement in radiating pain depended on a subjective determination by the patient, and the same degree of pain alleviation might be judged differently by different patients. Nevertheless, this was done in clinical situations in which we ask patients how much they have improved.
The second limitation of our study was the lack of the pain provocation test to see whether root irritation by needle contact reproduces concordant pain. Requiring both pain reproduction by needle placement and relief after injection for the definition of positive DSNRB would decrease false-positive results in an unaffected level, but it will increase false-negative results in an affected level as well. In our daily practice, we do not perform pain provocation tests in diagnostic and therapeutic blocks and, actually, try to avoid this to minimize the chance of undesirable pain production. Furthermore, we prefer to avoid provoking pain in unaffected adjacent levels.
Third, 1 level of double-blinding would have been possible if the physicians performing the blocks were blinded to the presumptive site of pain or pathologic process. Such blinding could potentially be important because, without it, the physician might have consciously or subconsciously altered the technique used or discussed the procedure and findings with the patient. Despite this, we chose not to blind these physicians and, instead, let them review preinjection imaging studies before they performed the blocks. We believed that this more faithfully reproduced the real-world situation in which the physicians routinely review imaging studies before performing the procedure. Without proper knowledge of the specific anatomy and pathologic condition of an individual patient, we believe that there is an increased risk for injury during an interventional procedure on that patient.
A fourth limitation of our study was the lack of dose or concentration-response determination for lidocaine. Previous investigations used 0.2 to 3 mL.1–7,9–11 Huston and Slipman15 have suggested using 0.5 to 1 mL to avoid false-positives. We agree with Sasso et al4 that minimal volume with high concentration may provide a more reliable block. However, to the best of our knowledge, the effect of the amount and concentration of the anesthetics on diagnostic value has not been reported thus far. Additional studies with use of various doses and concentrations are needed.
Fifth, the spot radiographs were taken at the time of the block, but the questionnaires were administered at 30 minutes after the procedure. Between these gaps, lidocaine can diffuse into surrounding areas, causing unexpected results. For example, the injectate might be placed at the symptomatic level, but as it diffuses and dilutes with time, it might result in a false-negative 30 minutes later. In reality, we doubt that this is a frequent problem because the block occurs almost immediately, with the effect lasting for at least 1 hour. However, it is possible that 80% pain relief without dilution resulted in 60% relief with dilution resulting in a false-negative. Conversely, injectate from a control level could diffuse to a symptomatic root, resulting in a false-positive. Indeed, we found that on the radiographs obtained at 30 minutes after the injection, the contrast media had dispersed such that we could no longer delineate their total spread. This suggests that if too much anesthetic is used, false-positive results can occur. Although it is difficult to prove, we believe that diffusion might be a common cause of false-negative and false-positive results. In an ideal setting, the questionnaire should be administered immediately after the injection, but this is somewhat impractical and requires a verbal questionnaire. We are currently performing a study to determine if the response to the block differs at 1, 5, 15, and 30 minutes after the injection.
Sixth, we performed the ROC analysis in our study population and applied the results to the same population. Another, perhaps more accurate, method might have been to perform the ROC analysis in a separate group and then apply the results to the study population. Because of the difficulty of enrolling the requisite number of patients in such a study, we chose not to use this methodology. Our methodology could theoretically make the results of DSNRBs seem more accurate than they are. If anything, this bolsters our argument that DSNRBs are, at best, only moderately accurate.
A final limitation of this study was that the radiologist performing the injections reviewed his own work, though he was blinded to the block results and some time was permitted to elapse between the blocks and the radiologist's reading of the radiographs. It is not ideal to have the same radiologist read the images because there may be inherent bias by the physician to underreport mistakes. On the other hand, there might be an incentive to overreport mistakes, to make it seem as if blocks, when performed correctly, will yield accurate results. We believe that the 2 biases are likely to cancel each other out.
Strengths of the Study
Despite our limitations, we believe that this study had unique strengths. We rigorously selected patients with a monoradiculopathy and used them as criterion standards against which the accuracy of DSNRBs could be tested. We did blocks on unaffected, as well as affected roots. We tried to replicate real-world situations with the injections because an idealized methodology is less likely to be repeated in clinical situations. We used ROC analysis to determine the cutoff value of pain relief and were able to determine all of the statistical parameters that define the usefulness of the injections.
Lessons That We Learned from This Study
This study demonstrates that to precisely and correctly interpret the results of DSNRBs, it is necessary to take great care during the injection procedures to selectively block the target root, use contrast media, take spot radiographs, and examine them carefully for the distribution of the injectate. The technique of a diagnostic block should be different from that of a therapeutic block, in which a false-positive result is of no concern. In an ideal setting, the injection should be extraepineural, and the injection material should sufficiently bathe the pathologic region shown on MR imaging while not overflowing into the epidural space or to the adjacent roots. In cases in which these conditions are not met during the injection, special attention is needed to interpret the results. Although our radiologist and his colleagues did everything possible to perform the injections as accurately as possible, on reviewing their own work, they found errors that were not evident during the procedure. As a direct result of this study, we now routinely review such films and check them for accuracy.
This study also demonstrates that diagnostic value of DSNRB is not high. Many problems or questions need to be solved for it to be used as a highly reliable method for selection of an operative level in patients having multilevel pathologic conditions on MR imaging. Nevertheless, we still use these blocks because they represent one of the few diagnostic tests to determine if a level that is abnormal on an imaging study is indeed a pain-generating level. As with every diagnostic test, however, one must keep in mind that there are false-positive and false-negative results.
Additional studies are needed to determine the optimal amount and concentration of the local anesthetics and the optimal time after injection for determining the test result. The cutoff value of pain relief for determining the test result may need to be reevaluated by other authors as well. In addition, the cause of false results that could not be explained on spot radiographs needs to be investigated further.
Conclusion
As the first step toward deciding the applicability of DSNRB in determining the pain-generating root level in patients with “multilevel” pathologic processes, we investigated its diagnostic value in “single-level” radiculopathy using a prospective, controlled, single-blinded design. We found that the diagnostic value of DSNRB was only moderate, with a sensitivity of 57%, a specificity of 86%, an accuracy of 73%, a positive predictive value of 77%, and a negative predictive value of 71%. For improvement in the accuracy of DSNRBs, great care should be taken to avoid inadequate blocks (ie, insufficient infiltration, insufficient passage of the injectate, and intraepineural injections) or overflow of the injectate, and to precisely interpret spot radiographs. Additional investigations are required to determine the optimal amount and concentration of the local anesthetics, optimal time after injection for determining the test result, and the optimal cutoff value of pain relief to define the positive block results.
Footnotes
This study was supported by a Research Grant of Seoul National University Bundang Hospital (06-2005-056).
References
- 1.Dooley JF, McBroom RJ, Taguchi T, et al. Nerve root infiltration in the diagnosis of radicular pain. Spine 1988;13:79–83 [DOI] [PubMed] [Google Scholar]
- 2.Haueisen DC, Smith BS, Myers SR, et al. The diagnostic accuracy of spinal nerve injection studies. Their role in the evaluation of recurrent sciatica. Clin Orthop Relat Res 1985;198:179–83 [PubMed] [Google Scholar]
- 3.Herron LD. Selective nerve root block in patient selection for lumbar surgery: surgical results. J Spinal Disord 1989;2:75–79 [PubMed] [Google Scholar]
- 4.Sasso RC, Macadaeg K, Nordmann D, et al. Selective nerve root injections can predict surgical outcome for lumbar and cervical radiculopathy: comparison to magnetic resonance imaging. J Spinal Disord Tech 2005;18:471–78 [DOI] [PubMed] [Google Scholar]
- 5.Van Akkerveeken PF. The diagnostic value of nerve root sheath infiltration. Acta Orthop Scand Suppl 1993;251:61–63 [DOI] [PubMed] [Google Scholar]
- 6.Porter DG, Valentine AR, Bradford R. A retrospective study to assess the results of CT-directed peri-neural root infiltration in a cohort of 56 patients with low back pain and sciatica. Br J Neurosurg 1999;13:290–93 [DOI] [PubMed] [Google Scholar]
- 7.Krempen JF, Smith BS. Nerve-root injection: a method for evaluating the etiology of sciatica. J Bone Joint Surg Am 1974;56:1435–44 [PubMed] [Google Scholar]
- 8.North RB, Kidd DH, Campbell JN, et al. Dorsal root ganglionectomy for failed back surgery syndrome: a 5-year follow-up study. J Neurosurg 1991;74:236–42 [DOI] [PubMed] [Google Scholar]
- 9.Schutz H, Lougheed WM, Wortzman G, et al. Intervertebral nerve-root in the investigation of chronic lumbar disc disease. Can J Surg 1973;16:217–21 [PubMed] [Google Scholar]
- 10.North RB, Kidd DH, Zahurak M, et al. Specificity of diagnostic nerve blocks: a prospective, randomized study of sciatica due to lumbosacral spine disease. Pain 1996;65:77–85 [DOI] [PubMed] [Google Scholar]
- 11.Stanley D, McLaren MI, Euinton HA, et al. A prospective study of nerve root infiltration in the diagnosis of sciatica. A comparison with radiculography, computed tomography, and operative findings. Spine 1990;15:540–43 [DOI] [PubMed] [Google Scholar]
- 12.Saal JS. General principles of diagnostic testing as related to painful lumbar spine disorders: a critical appraisal of current diagnostic techniques. Spine 2002;27:2538–45 [DOI] [PubMed] [Google Scholar]
- 13.Furman MB, O'Brien EM. Is it really possible to do a selective nerve root block? Pain 2000;85:526. [DOI] [PubMed] [Google Scholar]
- 14.Slosar PJ Jr, White AH, Wetzel FT. Controversy. The use of selective nerve root blocks: diagnostic, therapeutic, or placebo? Spine 1998;23:2253–56 [DOI] [PubMed] [Google Scholar]
- 15.Huston CW, Slipman CW. Diagnostic selective nerve root blocks: indications and usefulness. Phys Med Rehabil Clin N Am 2002;13:545–65 [DOI] [PubMed] [Google Scholar]
- 16.Pfirrmann CW, Oberholzer PA, Zanetti M. Selective nerve root blocks for the treatment of sciatica: evaluation of injection site and effectiveness–a study with patients and cadavers. Radiology 2001;221:704–11 [DOI] [PubMed] [Google Scholar]