Abstract
Objectives:
To determine the incidence and risk factors of delirium in the cardiac care unit (CCU) and intensive care unit (ICU).
Methods:
This multicenter prospective observational study was conducted between July 2019 and November 2019 in the central region of Saudi Arabia. All patients admitted to the critical care units were enrolled, and their demographic data and risk factors of delirium were reported.
Results:
A total of 165 patients were included: 76 (46.1%) admitted to the CCU and 89 (53.9%) admitted to the ICU. The mean age was 55.1±18 years, and 45 (27.3%) were women. We found that 24/165 (14.5%) patients developed delirium during admission. Importantly, variables significantly associated with delirium group were female gender: (24.5% versus 10.8%, p=0.028), malnutrition (29.2% versus 5%, p<0.001), the presence of urinary catheter (75% versus 30.5%, p=0.001), septicemia (50% versus 14.9%, p<0.001), intubation (41.7% versus 10.6%, p=0.001), low hemoglobin (10.79±2.91 versus 12.05±2.77, p=048), and prolonged prothrombin time (PT) (15.87±5.17 versus 13.60±3.28, p=0.011).
Conclusion:
The incidence of delirium was 14.5% among patients admitted to critical care units in the central region of Saudi Arabia. Septicemia, prolonged PT, malnutrition, and urinary catheter are significant predictors of delirium.
Keywords: delirium, critical care, Saudi
Delirium is defined as an abrupt onset of inattention associated with the disturbance of awareness, perception, and cognitive function, which commonly has a transient fluctuation course.1 There are various definition of delirium, in the present study, we define delirium if the following 4 diagnostic criteria were met: first, consciousness disturbance that occurs in association with impairment of the ability to focus; second, cognitive changes (language or memory abnormalities); third, acute onset (over hours to days) with fluctuating pattern of the symptoms; forth, clinical or laboratory evidence that the symptoms are due to a physiologic effects of a medical disease, medication use, and substance intoxication. Admission to intensive care unit (ICU) and disease severity are the most important predisposing factors for delirium.2 Moreover, various predisposing factors for delirium, such as the length of hospital stay, alcoholism, hypertension, advanced age, infection, urinary catheterization, electrolyte disturbance, and malnutrition, have been reported.3,4 The incidence of delirium in ICU was reported in a study conducted on 332 patients as 26.1%.5 While the incidence of delirium in patients with acute cardiovascular diseases, including acute myocardial infarction and acute heart failure, was approximately 15% in a study conducted on 700 patients admitted in the cardiac care unit (CCU).6 A few risk factors are related to the CCU: the requirement of mechanical support, increasing immobility, anti-arrhythmic drugs, and heart failure.7 The first step in the management strategy of delirium is to recognize and then try to eliminate the predisposing factors. Although several reports investigated the incidence and prevalence of ICU delirium,8 data on the incidence of delirium in the ICU is lacking in the Middle East. Given the fact that, alcoholism is a common cause of delirium, alcohol consumption is prohibited in Saudi Arabia for religious reasons. Thus, our study aimed to determine the incidence of delirium in the ICU and to evaluate its predisposing factors in the central region of Saudi Arabia.
Methods
This multicenter prospective observational study was conducted between July 2019 and November 2019 in 4 hospitals in the central region of Saudi Arabia.
All conscious patients aged >18 years who were admitted to the ICU or CCU were included. Patients with a history of dementia, psychosis, significant baseline neurological diseases, younger than 18 years, or admitted with coma were excluded.
Patient demographic data including age, gender, the reason for admission, and risk factors of delirium such as moderate to severe pain (score ≥4 on numerical rating scale between 0-10), the length of stay, and infection diagnosed with cultures were reported. Although there are various scales in use for assessment of delirium in ICU, in this study, we used the following validated scale to estimate the incidence of delirium: the Richmond Agitation-Sedation Scale (RASS) and Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). The RASS was used as a first step to assess the level of consciousness as follows: at RASS -4 or -5 score, delirium cannot be assessed as patients are considered unresponsive; thus, the same were assessed using the CAM-ICU to analyze the content of consciousness. So, the patients were assessed as if they are delirious or not according to the criteria in the CAM-ICU which are 1) acute onset or fluctuating course, 2) inattention, 3) altered level of consciousness, and 4) disorganized thinking.1 Importantly, the patient was considered delirious if the first and second criteria were present with either the third or fourth. The institutional and regional ethical committee approved the study protocol. All enrolled patients signed a consent form.
Statistical analysis
Quantitative variables were expressed as means ± standard deviations, and categorical variables as frequencies. We compared patients with and without delirium by using a t-test analysis for continuous variables and the Chi-square test for categorical variables. In addition, we performed univariate and multivariate regression analyses including all variables to identify predictors of delirium.
Results
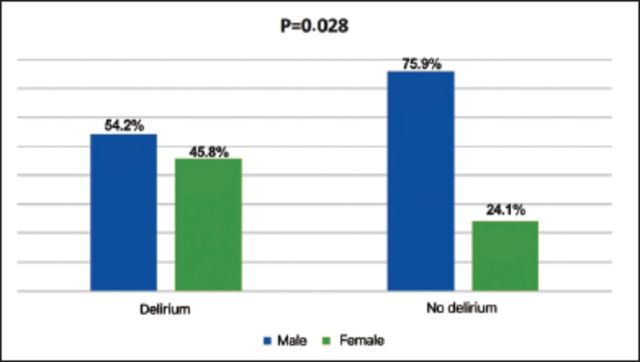
A total of 165 patients were included: 76 (46.1%) were admitted to the CCU and 89 (53.9%) to the ICU. The mean age was 55±18 years, and 45 (27.3%) were women (Figure 1). We found that 24/165 (14.5%) patients developed delirium during admission. We found that women were significantly associated with delirium when compared to men 11/45 (24.5%) versus 13/120 (10.8%), p=0.028. Delirium was significantly associated with malnutrition 7/24 (29.2%) versus 7/141 (5%) (p<0.001), the presence of urinary catheter 18/24 (75%) versus 43/141 (30.5%) (p=0.001), septicemia 12/24 (50%) versus 21/141 (15%) (p<0.001), intubation 10/24 (41.7%) versus 15/141 (10.6%) (p=0.001), a low hemoglobin level 10.79±2.91 versus 12.05±2.77 (p=0.048), and prolonged prothrombin time (PT) (15.87±5.17 versus 13.60±3.28, p=0.011) when compared with patients without delirium (Table 1). We found the length of stay did not differ between patient with and without delirium. We used a univariate regression module including all variables associated with delirium and found that malnutrition, urinary catheter, infection, hemoglobin level, and prolonged PT were significant predictors of delirium (Table 2).
Figure 1.
- Illustrates that delirium is more prevalent in women than in men.
Table 1.
- Baseline characteristics.
| Variables | All patients | Delirium | No delirium | P-value |
|---|---|---|---|---|
| Number of patients (%) | 165 (100) | 24 (14.5) | 141 (85.5) | - |
| Gender (male) (%) | 120 (72.7) | 13 (54.2) | 107 (75.9) | 0.028 |
| Age (years), mean±SD | 55 ± 18 | 60.0 ± 23 | 54 ± 17 | 0.147 |
| Marital status (married) (%) | 139 (84.2) | 20 (83.3) | 119 (84.4) | 0.45 |
| Height, mean±SD | 165 ± 9 | 166 ± 10 | 164 ± 9 | 0.95 |
| Weight, mean±SD | 75 ± 15 | 79 ± 22 | 74 ± 13 | 0.25 |
| Body mass index, mean±SD | 27.5 ± 5.6 | 28.8 ± 6.7 | 27.2 ± 5.6 | 0.35 |
| Educational level (illiterate)(%) | 41 (24.8) | 9 (37.5) | 32 (22.7) | 0.14 |
| Occupational status (employed) (%) | 61 (37.0) | 5 (20.8) | 56 (39.7) | 0.031 |
| Living status (with family) (%) | 104 (63.0) | 20 (83.3) | 84 (59.6) | 0.012 |
| Smoking (%) | 43 (26.1) | 6 (25.0) | 37 (26.2) | 0.54 |
| Pain (%) | 74 (44.9) | 10 (41.7) | 64 (45.4) | 0.26 |
| Malnutrition (%) | 14 (8.5) | 7 (29.2) | 7 (5.0) | 0.001 |
| Urinary catheter (%) | 61(37.0) | 18 (75.0) | 43 (30.5) | 0.001 |
| Infection (%) | 33 (20.0) | 12 (50.0) | 21 (14.9) | <0.001 |
| Invasive procedure (%) | 94 (57.0) | 15 (62.5) | 79 (56.0) | 0.45 |
| Surgery (%) | 13 (7.9) | 2 (8.3) | 11 (7.8) | 0.61 |
| Chronic kidney disease (%) | 26 (15.8) | 4 (16.7) | 22 (15.6) | 0.59 |
| Home medication (none) (%) | 21 (12.7) | 2 (8.3) | 19 (13.5) | 0.007 |
| Hypertension (%) | 83 (50.3) | 13 (54.2) | 70 (49.6) | 0.44 |
| Dyslipidemia %) | 25 (15.2) | 2 (8.3) | 23 (16.3) | 0.24 |
| Stroke (%) | 14 (8.5) | 2 (8.3) | 12 (8.5) | 0.61 |
| Heart failure (%) | 23 (13.9) | 4 (16.7) | 19 (13.5) | 0.52 |
| Liver failure (%) | 3 (1.8) | 2 (8.3) | 1 (0.7) | 0.004 |
| Acute renal failure (%) | 19 (11.5) | 4 (16.7) | 15 (10.6) | 0.057 |
| Intubation (%) | 25 (15.2) | 10 (41.7) | 15 (10.6) | 0.001 |
| Diabetes (%) | 67 (40.6) | 9 (37.5) | 58 (41.1) | 0.28 |
| White blood count, mean±SD | 12 ± 9 | 11 ± 4 | 13 ± 9 | 0.52 |
| Hemoglobin, mean±SD | 11.9 ± 3 | 10.8 ± 3 | 12.1 ± 3 | 0.048 |
| Sodium, mean±SD | 139 ± 7 | 139 ± 9 | 139 ± 7 | 0.87 |
| Potassium, mean±SD | 4.1 ± 0.7 | 4.1 ± 0.6 | 4.1 ± 0.7 | 0.75 |
| Calcium, mean±SD | 2.1 ± 0.4 | 2.0 ± 0.4 | 2.2 ± 0.3 | 0.23 |
| Random blood sugar, mean±SD | 158 ± 111 | 139 ± 82 | 161 ± 116 | 0.42 |
| PH, mean±SD | 7.39 ± 0.09 | 7.42 ± 0.14 | 7.38 ± 0.09 | 0.22 |
| Partial pressure of carbon dioxide, mean±SD | 39 ± 10 | 37 ± 7 | 39 ± 11 | 0.40 |
| Alanine aminotransferase, mean±SD | 46 ± 35 | 45 ± 29 | 46 ± 36 | 0.93 |
| Aspartate aminotransferase, mean±SD | 77 ± 124 | 73 ± 104 | 77 ± 127 | 0.91 |
| Creatinine, mean±SD | 124 ± 139 | 136 ± 174 | 122 ± 133 | 0.67 |
| Urea, mean±SD | 14.4 ± 41 | 10.2 ± 8 | 15 ± 44 | 0.60 |
| Prothrombin time, mean±SD | 13.9 ± 4 | 16 ± 5 | 14 ± 3 | 0.011 |
| Partial thromboplastin time, mean±SD | 42 ± 80 | 36 ± 12 | 43 ± 87 | 0.74 |
| International normalized ratio, mean±SD | 2 ± 9 | 1.4 ± 0.4 | 2.1 ± 9.5 | 0.74 |
| Bicarbonate, mean±SD | 24 ± 6 | 24 ± 7 | 24 ± 6 | 0.79 |
| Partial pressure of oxygen, mean±SD | 61 ± 39 | 78 ± 32 | 58 ± 4 | 0.068 |
| Absence of CAD (%) | 18 (10.9) | 6 (25.0) | 12 (8.5) | 0.009 |
| Ischemic cardiomyopathy (%) | 14 (8.5) | 2 (8.3) | 12 (8.5) | 0.47 |
| Valvular heart disease, n(%) | 3 (1.8) | 0 (0.00) | 3 (2.1) | 0.71 |
| Non-ischemic cardiomyopathy (%) | 10 (6.1) | 1 (4.2) | 9 (6.4) | 0.70 |
| Atrial fibrillation (%) | 3 (1.8) | 2 (8.3) | 1 (0.7) | 0.036 |
| Electrocardiogram, sinus rhythm (%) | 129 (78.2) | 19 (79.2) | 110 (78.0) | 0.56 |
| Ejection fraction, mean±SD | 39.5 ± 13 | 41.4 ± 16 | 39.4 ± 12 | 0.67 |
| Pulmonary artery systolic pressure, mean±SD | 35 ± 7 | 36 ± 6 | 34 ± 9 | 0.91 |
| Normal diastolic function (%) | 43 (26.1) | 6 (25.0) | 37 (26.2) | 0.35 |
Pain: score ≥4 on numerical rating scale between 0-10, infection: confirmed with positive culture, heart failure: EF <40%,CAD: coronary artery disease
Table 2.
- Univariate binary regression of variables of variable associated delirium with a p-value <0.05.
| Variablea | Univariant binary regression for delirium | |||
|---|---|---|---|---|
| 95% C. I. for OR | P-value | |||
| OR | Lower | Upper | ||
| Gender, male | 0.376 | 0.154 | 0.915 | 0.031 |
| Malnutrition | 8.462 | 2.561 | 27.953 | < 0.001 |
| Urinary catheter | 5.651 | 2.089 | 15.288 | 0.001 |
| Infection | 5.667 | 2.247 | 14.289 | < 0.001 |
| Home medication | 0.825 | 0.652 | 1.044 | 0.109 |
| Liver failure | 0.814 | 0.568 | 1.166 | 0.261 |
| Hemoglobin | 1.175 | 0.999 | 1.383 | 0.052 |
| Prothrombin time | 0.876 | 0.781 | 0.982 | 0.023 |
OR: odds ratio
Discussion
In the present study, we found that the incidence of delirium in critical care units was approximately 14.5%. In addition, we found that infection, intubation, and urinary catheter were strong predictors of delirium. We found that prolonged PT was significantly associated with delirium, which is probably explained by liver dysfunction or disseminated intravascular coagulopathy.
Delirium can result in poor outcomes, including prolonged mechanical ventilation, longer ICU and hospital stays, higher mortality, long-term cognitive impairment,1,2 and a higher cost of care.3 The length of stay, alcoholism, hypertension, advanced age, infection, urinary catheterization, electrolyte disturbance, and malnutrition are well-known predictors of delirium.4,6 Remarkably, the incidence of delirium in patients with acute cardiovasåcular diseases, including acute myocardial infarction and acute heart failure, was 15% in a study conducted on 700 patients admitted in the CCU.7 The authors concluded that important predictors of delirium were the requirement of mechanical support, increasing immobility, anti-arrhythmic drugs, and heart failure.8
In this study, the incidence of delirium (14.5%), which was similar to that reported in the literature.9-11 Moreover, we found that 36.8% of mechanically ventilated patients developed delirium, which was higher than that reported by Tilouche N et al.9 These differences may be explained by including cardiac patients in our study.9 Moreover, our results were similar to those of Bart et al12 demonstrating that coronary angiography was a significant risk factor for delirium in ICU patients.
Given that the most important step in the management of delirium is recognizing and controlling risk factors, our study has important clinical implications as it highlights the major risk factors of delirium in the ICU and CCU.
Study limitations
First, the number of patients included in the study was small. Second, we did not investigate the effects of sedation on patients; however, sedative influences on delirium were previously investigated in a large Saudi population.13 Third, we only included patients who developed symptoms during ICU/CCU admission, which may contribute to the low incidence of delirium in our study.
In conclusion, we found that 14.5% of patients admitted to the critical care unit developed delirium. Women, urinary catheter, prolonger PT, septicemia, and mechanical ventilation are strong predictors of delirium.
Acknowledgment
We thank Abdulaziz A. Aljomailan, Asma R. Alharbi, and Saleh A. Al-bahiji for their assistance with data collection.
Footnotes
References
- 1.Van den Boogaard M, Schoonhoven L, van der Hoeven JG,van Achterberg T, Pickkers P.. Incidence and short‑term consequences of delirium in critically ill patients: A prospective observational cohort study. Int J Nurs Stud 2012; 49: 775‑783. [DOI] [PubMed] [Google Scholar]
- 2.Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr., et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 2004; 291: 1753‑1762. [DOI] [PubMed] [Google Scholar]
- 3.Milbrandt EB, Deppen S, Harrison PL, Shintani AK, Speroff T, Stiles RA, et al. Costs associated with delirium in mechanically ventilated patients. Crit Care Med 2004; 32: 955‑962. [DOI] [PubMed] [Google Scholar]
- 4.Ouimet S, Kavanagh BP, Gottfried SB, Skrobik Y.. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med 2007; 33: 66-73. [DOI] [PubMed] [Google Scholar]
- 5.Kanova M, Sklienka P, Roman K, Burda M, Janoutova J.. Incidence and risk factors for delirium development in ICU patients - a prospective observational study. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2017; 161: 187-196. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed S, Leurent B, Sampson EL.. Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Ageing 2014; 43: 326-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Falsini G, Grotti S, Porto I, Toccafondi G, Fraticelli A, Angioli P, et al. Long-term prognostic value of delirium in elderly patients with acute cardiac diseases admitted to two cardiac intensive care units: a prospective study (DELIRIUM CORDIS). Eur Heart J Acute Cardiovasc Care 2018; 7: 661-670. [DOI] [PubMed] [Google Scholar]
- 8.Ibrahim K, McCarthy CP, McCarthy KJ, Brown CH, Needham DM, Januzzi JL Jr, McEvoy JW.. Delirium in the cardiac intensive care unit. J Am Heart Assoc 2018; 7: e008568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tilouche N, Hassen MF, Ali HBS, Jaoued O, Gharbi R, El Atrous SS.. Delirium in the intensive care unit: incidence, risk factors, and impact on outcome. Indian J Crit Care Med 2018; 22: 144-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: Validity and reliability of the confusion assessment method for the Intensive Care Unit (CAM-ICU). JAMA 2001; 286: 2703-2710. [DOI] [PubMed] [Google Scholar]
- 11.McNicoll L, Pisani MA, Zhang Y, Ely EW, Siegel MD, Inouye SK.. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc 2003; 51: 591-598. [DOI] [PubMed] [Google Scholar]
- 12.Van Rompaey B, Elseviers MM, Schuurmans MJ, Shortridge-Baggett LM, Truijen S, Bossaert L.. Risk factors for delirium in intensive care patients: a prospective cohort study. Crit Care 2009; 13: R77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rasheed AM, Amirah M, Abdallah M, Awajeh AM, Parameaswari PJ, Al Harthy A.. Delirium incidence and risk factors in adult critically ill patients in Saudi Arabia. J Emerg Trauma Shock 2019; 12: 30-34. [DOI] [PMC free article] [PubMed] [Google Scholar]