The case
A 7-year-old girl has a 2-month history of a mildly swollen and slightly painful knee, which her parents believe was caused by a fall at school. There is no other relevant history. Examination reveals a small swelling of the knee, with a small flexion contracture, loss of full flexion and some discomfort at the end of the range of motion. The results of the rest of the examination are normal. A complete blood count and the erythrocyte sedimentation rate are normal. A test for rheumatoid factor is negative, and an antinuclear antibody test is positive at a low titre (1:40). The child is referred to a pediatric rheumatologist with a provisional diagnosis of juvenile rheumatoid arthritis, although the referring physician is concerned about a possible injury to the knee caused by the fall.
Musculoskeletal pains in children are common, affecting 10%–20% of schoolchildren.1 In a recent school-based survey of adolescents in British Columbia, musculoskeletal pains were the second most common problem (after acne), and over 5% of these adolescents had limb pain of such severity that they believed that they had arthritis.2 Most of these pains are not the result of a serious underlying disease, although they can be a cause of significant morbidity. However, some children with musculoskeletal pains will have conditions that are either life-threatening or potentially crippling. The variety and relative frequencies of musculoskeletal conditions seen by pediatric rheumatologists have recently been documented.3
Diagnosis
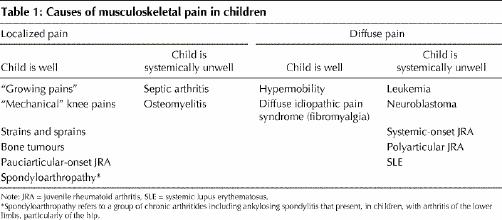
In trying to determine the diagnosis in a child with limb pains, it is helpful to categorize the pain as localized or diffuse, and then to decide whether the child is systemically unwell (febrile, anorexic, lethargic, and so on). Table 1 illustrates this approach, listing the most common and important causes of musculoskeletal pain. However, although these groupings are helpful, there will be exceptions. For example, although most children with pauciarticular-onset juvenile rheumatoid arthritis (JRA) seem quite healthy except for the swollen joint, some will have a lot of pain and will appear unwell, whereas some children with polyarticular JRA may have minimal systemic complaints. Similarly, a child with a bone tumour may have marked systemic features despite having a localized lesion. Although children with diffuse idiopathic pain syndrome (fibromyalgia-like disorder) complain bitterly of being fatigued and unwell, clinically they almost always appear to be thriving.
Table 1
When approaching a child with musculoskeletal pain, it is important for the physician to determine whether the problem could be caused by trauma, infection or a neoplastic condition before considering other possibilities, because a delay in diagnosing such conditions may have catastrophic consequences.
Trauma
Trauma is often incorrectly blamed for children's joint and limb pains. It is unlikely that a child will have a swollen, painful or tender limb as a consequence of trauma, if it was not serious enough to make the child immediately stop whatever activity he or she was engaged in. Usually, a swollen joint that is attributed by the child or parents to a fairly innocuous injury actually preceded the traumatic event and was merely brought to light by the injury.
An exception to this is the “overuse” type of injury often seen in enthusiastic young athletes. Although limb pains such as shin splints or stress fractures are not usually associated with significant swelling, they do occur following repetitive, relatively minor trauma. Careful history-taking should elicit the information that the adolescent is engaging in many hours of sport.
In the young child, it is always important to consider the possibility of physical abuse. Supporting evidence for this includes delay in bringing the child to medical attention following the “accident,” bruises of varying ages, torn frenula of the lips and retinal hemorrhages.
An acutely swollen joint after apparently minor trauma in a very young boy should raise the possibility of hemophilia. Children with underlying systemic disease may also develop pathological fractures due to osteoporosis; examples of these would be children taking chronic corticosteroid therapy, adolescents with anorexia nervosa and, more rarely, children with primary bone abnormalities.
Infection
A joint or bone infection should be suspected in any child who is unwell, febrile and has a very tender bone or the inability to move a joint. Erythema overlying the tender area is suggestive of infection and, conversely, is rarely seen in children with an idiopathic chronic arthritis. Usually, bone or joint infections affect only one area but, occasionally, several areas can be affected, particularly in the very young or immunosuppressed. In children with such infections, there is often a preceding history of minor trauma.
Tumours
Benign bone tumours, such as osteoid osteomas, and malignant tumours, such as osteogenic sarcoma and Ewing's sarcoma, are important causes of localized limb pain in children. Osteoid osteomas classically are associated with night pain that is relieved dramatically by small doses of nonsteroidal anti-inflammatory drugs (NSAIDs). A fairly large proportion of children with lymphoblastic leukemia or neuroblastoma have widespread musculoskeletal pain, and in children with leukemia there can actually be evidence of joint swelling presumably because of infiltration of the synovium by leukemic cells. Bony tenderness, which extends beyond the joint capsule, is suggestive of leukemia; although the idiopathic chronic arthritides, such as polyarticular-onset JRA, are accompanied by joint line tenderness, patients do not have bony tenderness. Such bone tenderness may be elicited at sites other than those about which a child is complaining.
The recording of a few symptoms and signs combined with some judicious investigations can be extremely helpful in determining whether the cause of a musculoskeletal complaint in a child is serious (Table 2).
Table 2
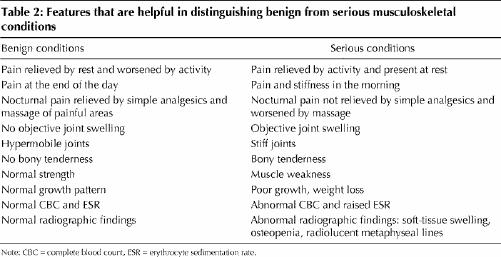
This division into “benign” and “serious” is only a guide, and no one feature can be considered in isolation. For example, although pains that are relieved by rest and exacerbated by activity are suggestive of “mechanical” causes, most of which are not serious in children, when these symptoms affect the back, they might be suggestive of a spondylolithesis or, if they affect the hip, they might be suggestive of a slipped capital femoral epiphysis, both of which are urgent problems. Pain is never benign; only the cause of the pain may be benign.
Understandably, parents often become increasingly anxious the longer a child has pains. However, a history of several weeks of episodic pains (even with a history of episodic joint swelling) that is not associated with any objective joint swelling or bony tenderness, but is associated with a normal complete blood count and erythrocyte sedimentation rate, is unlikely to be caused by a serious underlying disease.
Many children have minor developmental variants of the musculoskeletal system, such as knock knees, flat feet, or femoral or tibial torsion, that will be obvious to the examining physician. It is tempting to ascribe limb pain to these minor abnormalities, but this should be resisted because they rarely cause significant limb pain.
Specific joints
If a joint has been symptomatic for more than a day or two, minor trauma or sepsis are less likely to be causes of the complaint. Because the hip and knee are the most commonly affected areas, it is helpful to have a short list of conditions involving these joints. Similarly, because back pain in children, particularly in the very young, is caused by structural disease much more often than it is in adults, it is useful to be aware of some causes. Table 3 lists, by age, some conditions that are common or important causes of symptoms in specific joints.
Table 3
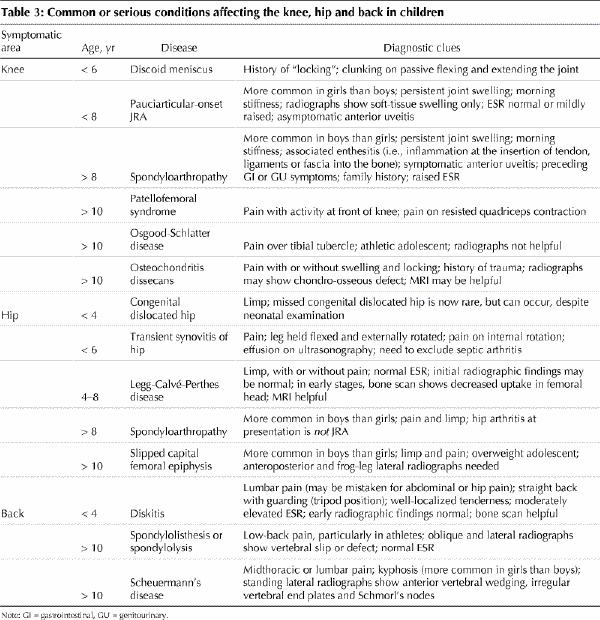
Pain in a joint may be referred from another area, especially in young children. Knee pain is not uncommonly referred from the hip. It is, therefore, always essential to examine the joints above and below the symptomatic joint, if there is no obvious abnormality in the painful area. This includes examining a child's back when he or she has a limp or is complaining of pain in the lower limbs.
Fallacy of the “rheumatology screen”
It is common to hear physicians talk about ordering a “rheumatology screen,” usually in reference to tests for antinuclear antibodies (ANAs) and rheumatoid factor. This is a false concept. The ANA test is positive in over 30% of children in whom it is ordered,4 making a positive test almost meaningless as an indication of rheumatic disease. Furthermore, many children with JRA and other rheumatic diseases test negative for ANAs. A negative ANA test would be unusual in a child with systemic lupus erythematosus (SLE) but, unless the ANA test is positive at a high titre (1:320 or more), a positive test alone is unlikely to indicate that the child has this condition. Rheumatoid factor tests are similarly of little value; they are rarely positive in children. When they are positive, only about half of these children have a chronic rheumatic disease. Furthermore, only about 10% of children with JRA test positive for rheumatoid factor.5
A few focused tests may be helpful, depending on the results of the clinical examination. A complete blood count (CBC) and erythrocyte sedimentation rate (ESR) are unlikely to be normal in a child with a bone or joint infection, a malignancy or an inflammatory rheumatic disease. Most children with an inflammatory rheumatic disease will have mild normochromic or hypochromic anemia and a raised platelet count. The exception might be a child with chronic arthritis affecting only 1 or 2 joints who might have a completely normal CBC and ESR. A normal or low platelet count or lymphopenia in the context of a raised ESR is suggestive of leukemia or SLE. A high level of lactate dehydrogenase in a child who is constitutionally unwell and has diffuse musculoskeletal symptoms would suggest the presence of leukemia or perhaps juvenile dermatomyositis.
Radiographs are often helpful and should always be ordered before arranging for bone scans, CT scans or MRI. Normal radiographic findings do not exclude the diagnosis of JRA or of osteomyelitis at an early stage, but radiographs are usually sensitive for bone tumours or fracture.
Urinalysis is a simple test, which is worth ordering if SLE is suspected, and the result will be available more quickly than for more specific tests (e.g., anti-DNA antibodies, C3 levels). Hematuria or significant proteinuria, with or without casts, in association with a raised ESR or lymphopenia would certainly increase the likelihood that the child has SLE. Determining muscle enzyme levels (creatine kinase, alanine transaminase, aspartate transaminase) is useful if the pain appears to be in the muscle, particularly if there is associated weakness; raised levels suggest juvenile dermatomyositis.
Chronic inflammatory rheumatic diseases
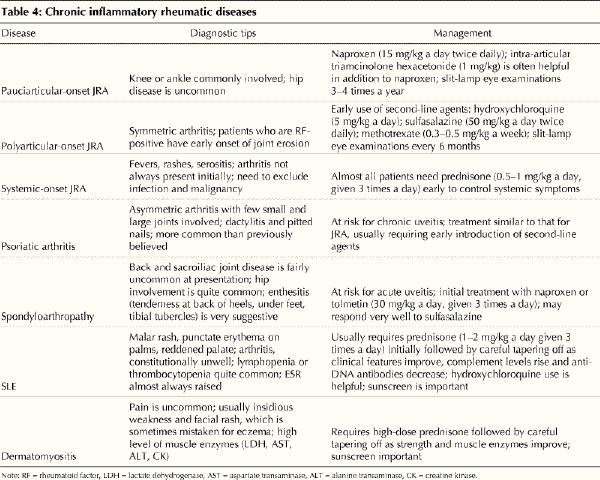
The childhood idiopathic arthropathies, systemic connective tissue diseases and vasculitides are probably more frequent than diabetes or epilepsy. Some of these conditions, with guides to their diagnosis and management, are listed in Table 4.
Table 4
If a child has had a swollen joint for more than a few days and there is no evidence of an infection, the diagnosis is probably a chronic pauciarticular (oligo) arthritis, which is the most common arthritis in children, usually affecting girls under 8 years of age. The most important task for the physician initially presented with a child with a swollen joint is to exclude sepsis. If there is any doubt (e.g., if the child is systemically unwell), a blood culture and joint aspiration should be performed, and the child should be administered intravenous antibiotics while awaiting the culture results. There is no excuse for failing to perform cultures and simply starting the child on oral antibiotics in case the joint is infected.
However, most children with chronic arthritis are managed without the need for diagnostic joint aspiration. Once a diagnosis of a chronic arthritis is made, it is appropriate to prescribe NSAIDs. We routinely use naproxen at 15 mg/kg daily, divided into 2 doses. Although the pain is usually at least partly alleviated within a day or two, it may take several weeks of consistent therapy before there is noticeable improvement in the joint swelling; thus, one would usually wait 6–8 weeks before considering other therapeutic options, unless it is clear that the condition is getting worse.
In a child with a monoarthritis, the use of intra-articular triamcinolone hexacetonide at a dose of about 1 mg/kg is often dramatically effective. Children with systemic-onset JRA usually require medium-dose to high-dose prednisone to control their systemic symptoms. Children with polyarticular arthritis often benefit from low-dose prednisone in the first few weeks of their treatment, before NSAIDs and other antirheumatic drugs begin to take effect.
There is increasing evidence that children with chronic arthritis have a high risk of continuing active arthritis over many years, often well into adult life. There is also increasing evidence that there is a “therapeutic window” in the first 2 years of disease when the chances are best for suppressing the inflammation and minimizing permanent joint damage. Because of this, pediatric rheumatologists are increasingly using so-called slow-acting antirheumatic drugs (particularly methotrexate) much earlier than before.
Children with chronic arthritis, particularly those with pauciarticular-onset JRA, are at risk of developing chronic uveitis (iritis); this is usually asymptomatic and can only by diagnosed by an ophthalmologist performing a slit-lamp eye examination regularly every few months over several years.
Canadians are in the fortunate position of perhaps having more pediatric rheumatologists per capita than anywhere else in the world. It is, therefore, probably the standard of care in Canada that all children with chronic arthritis or a systemic connective tissue disease will be seen by a pediatric rheumatologist within a few weeks of the onset of disease. Although it is appropriate for primary care physicians to start a child with a presumed chronic arthritis on NSAIDs, the other therapies discussed here, including intra-articular corticosteroid injections, should usually only be prescribed by a specialist. It is important, however, that the primary care physician remain closely involved in the child's care. There is always a risk that once children with chronic arthritis are referred to a specialist, they become “detached” from the family physician, whose important, continuing role in the child's health care is forgotten. The family physician is often the best person to help the child and family cope with the stresses of having a chronic illness. The child will also at times have illnesses that may or may not be related to the chronic arthritis or the side effects of the medications, and these will need to be evaluated and treated appropriately by the primary care physician.
Musculoskeletal pains are common in children. Although some are not serious, others can be harbingers of severe disease. A careful, focused approach can usually allow a rapid diagnosis to be reached, and the correct management instituted.
The case revisited
The pediatric rheumatologist concurred with the diagnosis of pauciarticular-onset JRA. The child was prescribed naproxen, 15 mg/kg daily, divided into 2 doses. The results of a slit-lamp examination performed by an ophthalmologist shortly after diagnosis were normal, as were repeat examinations performed every 3 months. Despite apparently good compliance with NSAIDs, the child continued to have a low-grade swelling of the knee, although the extent of the swelling appeared to fluctuate in a rather unusual manner. After 6 months, it was apparent that the swelling was localized mainly in the medial superior aspect of the knee. A repeat radiograph was still normal. Because of the poor response to treatment, the unusual localization of the swelling and its varying extent, MRI was performed. This examination demonstrated a moderately large vascular malformation in the vastus medialis muscle. Surgical excision led to complete resolution of the knee swelling.
This vignette demonstrates that, although monoarthritis of the knee is the most common presentation of JRA, other diagnoses must be borne in mind, particularly if the response to treatment is suboptimal; a history of trauma may be a red herring, an ANA test can be misleading and specialists can be wrong.
Key points .
Musculoskeletal pains affect 10%–20% of schoolchildren; although most musculoskeletal pains are not caused by a serious underlying disease, some may be life- threatening or potentially crippling.
When attempting to reach a diagnosis, it is helpful to categorize the pains as localized or diffuse and to decide whether the child is systemically unwell (febrile, anorexic, lethargic, and so on).
When examining a child with musculoskeletal pain, the physician should determine whether the symptoms might be due to trauma, infection or a tumour.
A red joint should be treated as a sign of infection until proven otherwise
The idea of a “rheumatology screen” is a fallacy; tests for antinuclear antibodies and rheumatoid factor are of little value in diagnosis.
A complete blood count and measurement of erythrocyte sedimentation rate are often useful as these are unlikely to be normal in a child with a serious bone or joint infection, a malignancy or an inflammatory rheumatic disease.
Plain radiographs should always be ordered before other imaging and may be useful in revealing bony conditions such as tumours that might mimic arthritis.
Radiographs are often more useful in excluding conditions than in making a positive diagnosis of chronic arthritis.
Urinalysis is an inexpensive, simple test that may help in the diagnosis of systemic lupus erythematosus.
If a child has had a swollen joint for more than a few days and there is no evidence of an infection, the diagnosis is probably a chronic pauciarticular arthritis, which is the most common arthritis in children.
Although monoarthritis of the knee is the most common presentation of juvenile rheumatoid arthritis, other diagnoses must be borne in mind, particularly if the response to treatment is suboptimal.
Children with chronic arthritis have a high risk of continuing active arthritis over many years, often well into adult life.
Early aggressive anti-inflammatory therapy provides the best chance of suppressing the inflammation and minimizing permanent joint damage.
CMAJ's rheumatology series .
This series is now complete.
Esdaile JM. Rheumatology: introduction to the series. CMAJ 2000;162(7):1007.
Ensworth S. Rheumatology: 1. Is it arthritis? CMAJ 2000; 162 (7): 1011-6.
Shojania K. Rheumatology: 2. What laboratory tests are needed? CMAJ 2000;162(8):1157-63.
Reid G, Esdaile JM. Rheumatology: 3. Getting the most out of radiology. CMAJ 2000;162(9):1318-25.
Cibere J. Rheumatology: 4. Acute monoarthritis. CMAJ 2000; 162(11):1577-83.
Klinkhoff A. Rheumatology: 5. Diagnosis and management of inflammatory polyarthritis. CMAJ 2000;162 (13): 1833-8.
Price GE. Rheumatology: 6. Localized therapy. CMAJ 2000; 163(2):176-83.
Huang SHK. Rheumatology: 7. Basics of therapy. CMAJ 2000; 163(4):417-23.
Lacaille D. Rheumatology: 8. Advanced therapy. CMAJ 2000; 163(6):721-8.
Clark BM. Rheumatology: 9. Physical and occupational therapy in the management of arthitis. CMAJ 2000; 163 (8): 999-1005.
Brady OH, Masri BA, Garbuz DS, Duncan CP. Rheumatology: 10. Joint replacement of the hip and knee — when to refer and what to expect. CMAJ 2000;163(10):1285-91.
Puttick MPE. Rheumatology: 11. Evaluation of the patient with pain all over. CMAJ 2001;164(2):223-7.
Tsang I. Rheumatology: 12. Pain in the neck. CMAJ 2001;164 (8): 1182-7.
Wing PC. Rheumatology: 13. Minimizing disability in patients with low-back pain. CMAJ 2001;164(10):1459-68.
Taunton JE, Wilkinson M. Rheumatology: 14. Diagnosis and management of anterior knee pain. CMAJ 2001;164 (11):1595-601.
Wade JP. Rheumatology: 15. Osteoporosis. CMAJ 2001; 165 (1): 45-50.
Malleson PN, Beauchamp RD. Rheumatology: 16. Diagnosing musculoskeletal pain in children. CMAJ 2001;165(2):183-8.
Supplementary reading .
Cassidy JT, Petty RE. Textbook of pediatric rheumatology. 4th ed. Philadelphia: WB Saunders; 2001.
Footnotes
This series has been reviewed and endorsed by the Canadian Rheumatology Association.
The Arthritis Society salutes CMAJ for its extensive series of articles on arthritis. The Society believes that this kind of information is crucial to educating physicians about this devastating disease.
This article has been peer reviewed.
Acknowledgements: We acknowledge the helpful comments of Dr. David Cabral.
Competing interests: None declared.
Correspondence to: Dr. Peter Malleson, Rm. 1A 16, British Columbia's Children's Hospital, 4480 Oak St., Vancouver BC V6H 3V4; fax 604 875-3649; pmalleson@cw.bc.ca
References
- 1.Goodman JE, McGrath PJ. The epidemiology of pain in children and adolescents: a review. Pain 1991;46:247-64. [DOI] [PubMed]
- 2.Adolescent health survey: province of British Columbia. Richmond (BC): New Leaf Computer Publishing and Printing Corporation; 1993.
- 3.Malleson PN, Fung MY, Rosenberg AM. The incidence of pediatric rheumatic diseases: results from the Canadian Pediatric Rheumatology Association Disease Registry. J Rheumatol 1996;23:1981-7. [PubMed]
- 4.Malleson PN, Sailer M, Mackinnon MJ. Usefulness of antinuclear antibody testing to screen for rheumatic diseases. Arch Dis Child 1997;77:299-304. [DOI] [PMC free article] [PubMed]
- 5.Eichenfield AH, Athreya BH, Doughty RA, Cebul RD. Utility of rheumatoid factor in the diagnosis of juvenile rheumatoid arthritis. Pediatrics 1986;78:480-4. [PubMed]


