Abstract
Summary
The study examined long-term direct and indirect economic burden of osteoporotic fractures among postmenopausal women. Healthcare costs among fracture patients were substantial in first year after fracture and remained higher than fracture-free controls for 5 years which highlight needs for early detection of high-risk patients and continued management for osteoporosis.
Introduction
This study compared direct and indirect healthcare costs between postmenopausal women and demographically matched controls in the 5 years after incident non-traumatic fracture, and by fracture type in commercially insured and Medicare populations.
Methods
Two hundred twenty-six thousand one hundred ninety women (91,925 aged 50–64 years; 134,265 aged ≥ 65 years) with incident non-traumatic fracture (hip, vertebral, and non-hip non-vertebral (NHNV)) from 2008 to 2017 were identified. Patients with fracture were directly matched (1:1) to non-fracture controls based on demographic characteristics. Direct healthcare costs were assessed using general linear models, adjusting for baseline costs, comorbidities, osteoporosis diagnosis, and treatment. Indirect costs associated with work loss due to absenteeism and short-term disability (STD) were assessed among commercially insured patients. Costs were standardized to 2018 US dollars.
Results
Osteoporosis diagnosis and treatment rates prior to fracture were low. Patients with fracture incurred higher direct costs across 5-year post-index compared with non-fracture controls, regardless of fracture type or insurance. For commercially insured hip fracture patients, the mean adjusted incremental direct healthcare costs in years 1, 3, and 5 were $59,327, $6885, and $3241, respectively. Incremental costs were lower, but trends were similar for vertebral and NHNV fracture types and Medicare-insured patients. Commercially insured patients with fracture had higher unadjusted indirect costs due to absenteeism and STD in year 1 and higher adjusted indirect costs due to STD at year 1 (incremental cost $5848, $2748, and $2596 for hip, vertebral, and NHNV fracture).
Conclusions
A considerable and sustained economic burden after a non-traumatic fracture underscores the need for early patient identification and continued management.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00198-020-05769-3.
Keywords: Absenteeism, Fractures, Long-term cost of fracture, Osteoporosis, Short-term disability
Introduction
Increased life expectancy and the aging of the baby boomer generation has resulted in a steady increase in the population of people aged 65 and older in the United States (US) [1]. As this population increases, so does the societal burden of medical conditions more prevalent in older adults, such as non-traumatic fractures [2, 3]. Non-traumatic fractures are commonly associated with osteoporosis, or low bone mass in patients with osteopenic femoral or spine bone mineral density (BMD), particularly when other risk factors are present [4, 5]. They are fractures that occur during routine daily activities or from a low-energy injury such as a fall from standing height. Moreover, non-traumatic fractures also impact the working population, as half of all women over the age of 50 are reported to have osteoporosis or low bone mass, and many will have a non-traumatic fracture during their lifetime [6].
A report from the National Osteoporosis Foundation estimated 441.7 new non-traumatic fractures per 10,000 Medicare beneficiaries in 2015 [7]. The leading sites for non-traumatic fractures are the hip and vertebra, but these only account for 31 to 40% of all non-traumatic fractures [8, 9]. Women are more likely to experience a non-traumatic fracture than men [2, 7], and this disparity increases with age [10]. Other risk factors for fracture include increasing age, lower BMD T-score, a history of fracture, and a history of falls [11, 12]. Conditions and medications associated with reduced bone density or an increased risk of falling, such as impaired mobility, poor self-assessed health, low body mass index, and dementia, have also been associated with increased fracture risk [11–13].
Among postmenopausal women, non-traumatic fractures are a leading source of healthcare burden, and in 2011, hospitalization costs alone were estimated to be $5.1 billion in the US [3]. Estimates of the US national expenditure on non-traumatic fractures range from $12.9 to $16.9 billion annually [2, 14], and Burge et al. projected that shifting demographics will drive direct spending on non-traumatic fractures up to $25.2 billion by 2025 [2]. In addition, non-traumatic fractures are associated with a loss of independence and reduced physical and mental quality of life [15, 16], which was linked to a decrease in workplace productivity and an increase in healthcare costs [17]. For women with hip and vertebral fractures, these reductions in quality-of-life can persist for many years post-fracture [18, 19].
The immediate high costs of non-traumatic fractures have been documented [2, 14, 20–24]; however, their findings reflected healthcare costs more than a decade ago. The only recent publication documenting short-term costs came from the 2019 Milliman Report, which captured costs only among Medicare patients [7]. Even less is known about the long-term effects on healthcare costs beyond 1-year post-fracture and among working-aged women in a commercial health plan. The objective of this study was to assess the 5-year direct and indirect healthcare costs of non-traumatic fracture among women age 50 years and older in commercial and Medicare US populations. Costs were analyzed among commercially and Medicare-insured patients for three fracture types (hip, vertebral, non-hip, non-vertebral (NHNV)).
Methods
Study design and data source
This observational retrospective cohort analysis utilized de-identified US administrative claims data from the IBM MarketScan Commercial Claims and Encounters database (Commercial), the MarketScan Medicare Supplemental and Coordination of Benefits database (Medicare), and the MarketScan Health and Productivity Management Database for the period from January 1, 2007, through December 31, 2017. The commercial and Medicare databases capture the inpatient medical, outpatient medical, and outpatient prescription drug data for their respective covered populations, and form a convenience sample of 155 million commercially insured employees and approximately 10.6 million Medicare enrollees.
The Health and Productivity Management database contains workplace absence, short-term disability (STD), and long-term disability data for a subset of employer clients that contribute data to the Commercial Database.
All database records are statistically de-identified and certified to be fully compliant with US patient confidentiality requirements set forth in the Health Insurance Portability and Accountability Act of 1996. Because this study used only de-identified patient records and did not involve the collection, use, or transmittal of individually identifiable data, this study was exempted from Institutional Review Board approval. All study data were obtained using International Classification of Diseases, Ninth and Tenth Revision, Clinical Modification (ICD-9-CM and ICD-10-CM) codes, Current Procedural Terminology 4th edition codes, Healthcare Common Procedure Coding System codes, and National Drug Codes.
Patient selection and cohort assignment
Using a method previously described by Bonafede et al. [12], patients with either (1) a primary or secondary diagnosis indicative of closed or pathologic hip, vertebral, or NHNV fracture on an inpatient claim, or (2) an outpatient claim with a diagnosis of closed or pathologic hip, vertebral, or NHNV fracture and a corresponding fracture treatment procedure for the same fracture site between January 1, 2008 and December 31, 2016, were identified. The earliest observed claim for a fracture was the index date.
Patients without evidence of fracture between January 1, 2008 and December 31, 2016, were eligible for inclusion in the control cohort. The index date of controls was assigned by identifying patients without a fracture event and randomly matching them with replacement to the pool of patients with a fracture event who had the same year of birth. Controls then were assigned the index date of their matched fracture patient.
To be included in the study, all patients were required to be female, at least 50 years old on the index date, and have at least 12 months of continuous enrollment with medical and pharmacy benefits before and after the index date. Patients were followed through the earliest of the following: 60-month post-index, end of continuous enrollment, or end of the study period (December 31, 2017). Patients with evidence of closed or pathological fracture at any time during continuous follow-up were excluded, as were patients with any of the following during the pre-index period: (1) indication of major trauma such as falls from a ladder, (2) transport accidents, or other causes that may imply traumatic fracture within ± 7 days of the index fracture, (3) Paget’s disease of the bone and other osteitis deformans and osteopathies, (4) osteogenesis imperfecta, (5) hypercalcemia, (6) cancers (excluding non-melanoma skin cancer), or (7) human immunodeficiency virus.
Fracture patients were stratified into three groups (hip, vertebral, or NHNV (defined as radius and ulna, humerus, tibia and fibula, ankle, pelvis, and clavicle)) based on the location of the index fracture. Patients with multiple fractures on their index date were assigned to one of the three fracture groups using the following hierarchical order: hip > vertebral > NHNV fracture. Patients with fractures were directly matched, using that same hierarchical order, to controls based on age at index, geographic region, insurance plan type, payer (commercial or Medicare), and total months of follow-up. For commercial patients, age was matched 1:1; whereas, for Medicare patients, age was matched 1:1 for ages 65 to 84 years, then in 5-year increments for ages 85 to 99 years, and then a single group for those aged 100 years and above. Matched pairs were grouped into five non-exclusive cohorts based on the duration of follow-up: ≥ 12 months, ≥ 24 months, ≥ 36 months, ≥ 48 months, and ≥ 60 months. The same method of 1:1 direct matching was used to match the subset of commercially insured fracture patients with workplace absenteeism or STD eligibility to controls with similar work-loss coverage. Matched pairs with absenteeism eligibility during the 5-year follow-up and those with STD eligibility during the 5-year follow-up were identified.
Patient characteristics
Patient demographics were measured on the index date and included age, geographic region, insurance plan type, and payer. Baseline clinical characteristics were measured during the 12-month pre-index period and included Deyo-Charlson Comorbidity Index (CCI) [25], diagnosis of osteoporosis or low bone mass, diagnosis of select conditions associated with an increased risk of fracture (chronic obstructive pulmonary disease (COPD), heart disease, multiple sclerosis, osteoarthritis, and Parkinson’s disease), and utilization of osteoporosis-related medications (oral and injectable bisphosphonates, calcitonin, denosumab, raloxifene, and teriparatide).
Healthcare utilization and costs
All-cause healthcare utilization and costs were measured during the pre- and post-index periods. Components of healthcare utilization and costs included inpatient admissions, emergency room (ER) visits, outpatient services and visits (such as outpatient office visits, skilled nursing facility (SNF) services, and other outpatient services), and outpatient pharmacy claims. All costs were adjusted for inflation using the medical care component of the Consumer Price Index and standardized to 2018 US dollars [26].
Indirect costs
Indirect costs from work loss due to absenteeism and STD were assessed among employed commercially insured patients linked to the MarketScan Health and Productivity Database. Patient eligibility was established independently for each outcome. For example, a patient only needed to have absenteeism coverage to be included in the absenteeism analysis. The number of days lost due to workplace absenteeism and STD was measured during the 5-year follow-up period. The minimum cohort size for data reporting was set at 30 patients. The sample size of the hip fracture cohort with absenteeism eligibility from year 2 to 5 post-index was less than 30 patients; thus, their results were not reported. The reason for work absence or STD is not recorded on the claim; therefore, these can be absences for any cause.
Indirect costs of absenteeism were calculated by multiplying the number of days absent during the follow-up period with the estimated daily age-, sex-, and region-specific wage based on the 2017 Current Population Survey conducted by the Bureau of Labor Statistics [27]. Indirect costs of STD were calculated by multiplying the number of days lost due to STD with 70% of the daily BLS wage to reflect the fact that the typical STD program benefit compensates for approximately 70% of an employee’s pay and benefits [28, 29].
Statistical analysis
Mean and standard deviation (SD) were reported for continuous variables, and statistical significance was determined using Student’s t tests. Frequencies and percentages were reported for categorical variables, and statistical significance was determined using chi-squared tests.
Multivariable analysis was used to examine the difference in annual total direct costs for each of the 5 years and indirect costs due to STD for the first year between fracture patients and controls following the index date while controlling for baseline costs and patient demographic and clinical characteristics. Costs differences were estimated using generalized linear regression models employing a log link and gamma error distribution. Separate models were constructed for Medicare and commercial patients and for hip, vertebral, and NHNV fracture patients, and for patients eligible for STD. The main explanatory variable of interest was the presence of a fracture. Each model adjusted for age, geographic region, insurance plan type, DCCI, baseline total healthcare costs, baseline comorbid conditions (osteoporosis, COPD, heart disease, multiple sclerosis, osteoarthritis, and Parkinson’s disease), and baseline osteoporosis-related medication utilization.
A p value of < 0.05 was set a priori as the threshold for statistical significance. Direct matching, descriptive analysis, and multivariable analyses were conducted using WPS version 4.1 (World Programming, UK).
Results
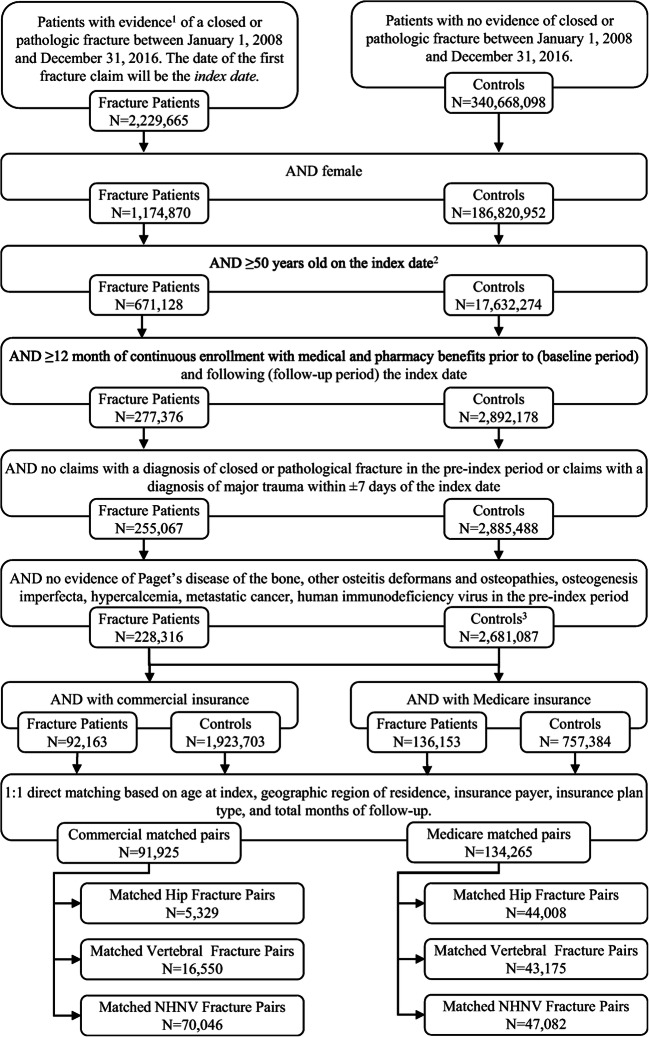
Of the 2,229,665 patients with a fracture between January 1, 2008 and December 31, 2016, 228,316 (10.2%) met all the inclusion and exclusion criteria (Fig. 1). Of these, 226,190 (99.1%) could be directly matched to control patients without a fracture event based on age, geographic region, insurance payer, insurance plan type, and duration of follow-up. Among the matched commercially insured patients were 5329 (5.8%) hip fracture patients, 16,550 (18.0%) vertebral fracture patients, and 70,046 (76.2%) NHNV fracture patients with at least 1 year of continuous follow-up. Among the matched Medicare-insured patients were 44,008 (32.8%) hip fracture patients, 43.175 (32.2%) vertebral fracture patients, and 47,082 (35.1%) NHNV fracture patients with at least 1 year of continuous follow-up (Table 1).
Fig. 1.
Patient selection. 1At least one primary or secondary diagnosis indicative of closed or pathologic fracture on an inpatient claim OR a non-diagnostic outpatient claim which carries a diagnosis of non-traumatic fracture along with the corresponding fracture treatment procedures for the same fracture site. 2Control patients were assigned index dates by pairing them to a randomly selected fracture patient (with replacement) based on insurance type and year of birth and then assigning the control patient the index date of the fracture patient. 3To ensure control, patients were excluded if they had a closed or pathological fracture at any time during the observation period; an additional 11,943 control patients were excluded because they had a fracture between December 31, 2016 and December 31, 2017
Table 1.
Baseline characteristics of patients with hip, vertebral, and non-hip non-vertebral (NHNV) fracture and their matched comparison cohorts stratified by insurance type
| Commercial | Medicare | Commercial | Medicare | Commercial | Medicare | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hip fracture | Controls | Hip fracture | Controls | Vertebral fracture | Controls | Vertebral fracture | Controls | NHNV fracture | Controls | NHNV fracture | Controls | |
| N = 5329 | N = 5329 | N = 44,008 | N = 44,008 | N = 16,550 | N = 16,550 | N = 43,175 | N = 43,175 | N = 70,046 | N = 70,046 | N = 47,082 | N = 47,082 | |
| Age, years (mean, SD) | 57.8 (3.6) | 57.8 (3.6) | 82.9 (7.0) | 82.8 (6.9) | 56.9 (3.8) | 56.9 (3.8) | 80.7 (7.1) | 80.7 (7.1) | 56.4 (3.7) | 56.4 (3.7) | 78.4 (7.4) | 78.4 (7.3) |
| Age categories (N, %) | ||||||||||||
| 50–64 | 5329 (100) | 5329 (100) | 120 (0.3) | 120 (0.3) | 16,550 (100) | 16,550 (100) | 238 (1) | 238 (1) | 70,046 (100) | 70,046 (100) | 592 (1) | 592 (1) |
| 65–74 | 5682 (12.9) | 5682 (12.9) | 8768 (20.3) | 8768 (20.3) | 15,094 (32.1) | 15,094 (32.1) | ||||||
| 75–84 | 19,034 (43.3) | 19,034 (43.3) | 20,481 (47.4) | 20,481 (47.4) | 20,788 (44.2) | 20,788 (44.2) | ||||||
| 85+ | 19,172 (43.6) | 19,172 (43.6) | 13,688 (31.7) | 13,688 (31.7) | 10,608 (22.5) | 10,608 (22.5) | ||||||
| Duration of follow-up | ||||||||||||
| ≥ 1 year | 5329 (100) | 5329 (100) | 44,008 (100) | 44,008 (100) | 16,550 (100) | 16,550 (100) | 43,175 (100) | 43,175 (100) | 70,046 (100) | 70,046 (100) | 47,082 (100) | 47,082 (100) |
| ≥ 2 years | 3284 (61.6) | 3284 (61.6) | 30,973 (70.4) | 30,973 (70.4) | 10,398 (62.8) | 10,398 (62.8) | 30,102 (69.7) | 30,102 (69.7) | 46,028 (65.7) | 46,028 (65.7) | 32,987 (70.1) | 32,987 (70.1) |
| ≥ 3 years | 2005 (37.6) | 2005 (37.6) | 21,556 (49.0) | 21,556 (49.0) | 6431 (38.9) | 6431 (38.9) | 20,719 (48.0) | 20,719 (48.0) | 29,963 (42.8) | 29,963 (42.8) | 23,264 (49.4) | 23,264 (49.4) |
| ≥ 4 years | 1229 (23.1) | 1229 (23.1) | 14,225 (32.3) | 14,225 (32.3) | 4019 (24.3) | 4019 (24.3) | 13,756 (31.9) | 13,756 (31.9) | 19,444 (27.8) | 19,444 (27.8) | 15,831 (33.6) | 15,831 (33.6) |
| ≥ 5 years | 754 (14.1) | 754 (14.1) | 8897 (20.2) | 8897 (20.2) | 2402 (14.5) | 2402 (14.5) | 8562 (19.8) | 8562 (19.8) | 12,334 (17.6) | 12,334 (17.6) | 10,362 (22.0) | 10,362 (22.0) |
| Deyo-Charlson Comorbidity Index (mean, SD) | 0.9 (1.5) | 0.3 (0.8)** | 1.2 (1.5) | 0.9 (1.3)** | 0.6 (1.1) | 0.3 (0.8)** | 1.2 (1.5) | 0.9 (1.3)** | 0.4 (0.9) | 0.3 (0.8)** | 1.1 (1.5) | 0.9 (1.3)** |
| Low bone mass (N, %) | 285 (5.3) | 180 (3.4)** | 1275 (2.9) | 1047 (2.4)** | 956 (5.8) | 593 (3.6)** | 2124 (4.9) | 1262 (2.9)** | 2674 (3.8) | 2394 (3.4)** | 2023 (4.3) | 1424 (3.0)** |
| Osteoporosis diagnosis (N, %) | 567 (10.6) | 169 (3.2)** | 5284 (12.0) | 3149 (7.2)** | 567 (10.6) | 169 (3.2)** | 5284 (12.0) | 3191 (7.4)** | 2783 (4.0) | 2229 (3.2)** | 4965 (10.5) | 3527 (7.5)** |
| Comorbid conditions (N, %) | ||||||||||||
| Chronic obstructive pulmonary disease | 840 (15.8) | 448 (8.4)** | 7713 (17.5) | 5447 (12.4)** | 2848 (17.2) | 1396 (8.4)** | 9238 (21.4) | 5567 (12.9)** | 8105 (11.6) | 5811 (8.3)** | 8297 (17.6) | 6030 (12.8)** |
| Heart disease | 1163 (21.8) | 616 (11.6)** | 21,253 (48.3) | 17,291 (39.3)** | 3363 (20.3) | 1978 (12.0)** | 21,596 (50.0) | 16,733 (38.8)** | 10,501 (15.0) | 8131 (11.6)** | 20,920 (44.4) | 17,319 (36.8)** |
| Multiple sclerosis | 155 (2.9) | 25 (0.5)** | 137 (0.3) | 52 (0.1)** | 199 (1.2) | 55 (0.3)** | 141 (0.3) | 59 (0.1)** | 697 (1.0) | 293 (0.4)** | 236 (0.5) | 83 (0.2)** |
| Osteoarthritis | 1240 (23.3) | 505 (9.5)** | 10,484 (23.8) | 8086 (18.4)** | 2699 (16.3) | 1558 (9.4)** | 11,619 (26.9) | 7981 (18.5)** | 8188 (11.7) | 6649 (9.5)** | 11,171 (23.7) | 8700 (18.5)** |
| Parkinson’s disease | 50 (0.9) | 10 (0.2)** | 1420 (3.2) | 559 (1.3)** | 63 (0.4) | 18 (0.1)** | 1007 (2.3) | 492 (1.1)** | 98 (0.1) | 75 (0.1) | 872 (1.9) | 492 (1.0)** |
| Osteoporosis-related medications1 (N, %) | 940 (17.6) | 539 (10.1)** | 10,358 (23.5) | 8106 (18.4)** | 2439 (14.7) | 1456 (8.8)** | 13,476 (31.2) | 7952 (18.4)** | 5775 (8.2) | 5931 (8.5) | 10,098 (21.4) | 8554 (18.2)** |
| All-cause healthcare costs (mean, SD) | $31,494 ($75,015) | $8093 ($15,184)** | $19,869 ($38,121) | $12,752 ($24,428)** | $23,446 ($52,847) | $8644 ($22,229)** | $21,912 ($39,022) | $12,675 ($24,508)** | $12,770 ($28,848) | $8445 ($21,879)** | $18,428 ($37,092) | $12,885 ($30,300)** |
*p < 0.05 **p < 0.001
1Includes oral and injectable bisphosphonates (alendronate, ibandronate, risedronate, zoledronic acid), calcitonin, denosumab, raloxifene, and teriparatide
On average, the hip fracture patients were older than vertebral patients who were older than NHNV fracture patients though this trend was more distinct in the Medicare-insured cohort than in the commercially insured cohort (Table 1). All comorbid conditions of interests were more common among fracture patients than comparison patients regardless of fracture type or insurance payer except for among commercially insured NHNV fracture patients whose incidence of Parkinson’s disease and use of bisphosphonates use was similar to comparison patients. Fracture patients were more likely to have a pre-index diagnosis of osteoporosis or low bone mass than controls; however, even in the older patient cohort (aged 65 or older), fewer than 12% of any cohort had a pre-index osteoporosis diagnosis and 21–31% of patients had osteoporosis-related medication prior to their index fracture.
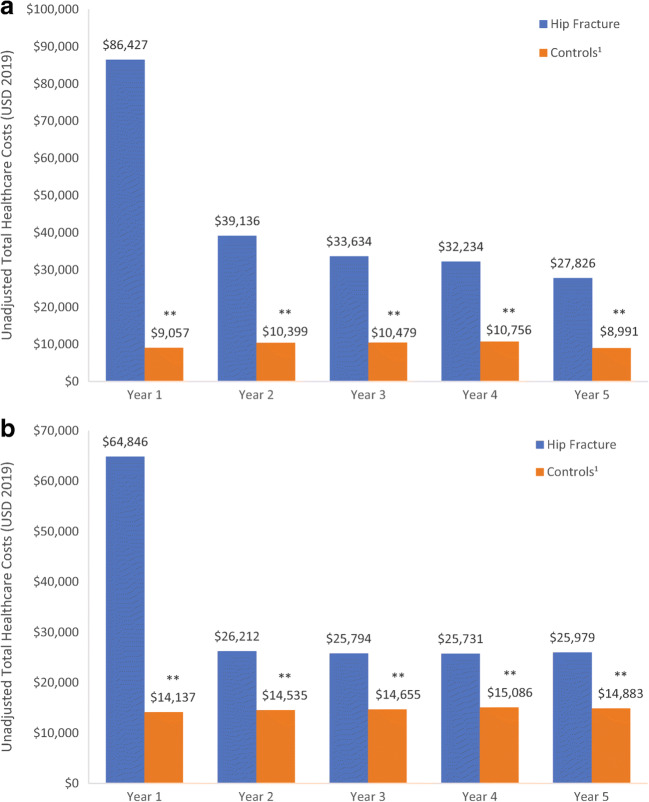
Total all-cause healthcare costs for patients with a non-traumatic fracture were significantly higher than matched controls regardless of the year of follow-up, fracture type, or insurance payer (all p < 0.001; Fig. 2 and Supplementary Table 1). In the commercially insured cohort, mean unadjusted year 1 costs were $75,505 higher for hip fracture patients, $38,649 higher for vertebral fracture patients, and $17,306 higher for NHNV fracture patients compared to controls. In the Medicare-insured cohort, mean unadjusted year 1 costs were $49,486 higher for hip fracture patients, $26,561 higher for vertebral fracture patients, and $22,965 higher for NHNV fracture patients compared to controls. The cost difference between matched hip, vertebral, and NHNV fracture patients and controls decreased from year 1 to year 5 but remained significant.
Fig. 2.
Total healthcare costs during year 1 to year 5 post-index among a commercially and b Medicare-insured patients with hip fracture and matched comparison patients. **p < 0.001 1Controls matched (1:1) to fracture patients on age at index, geographic region, insurance plan type, and total months of follow-up
The excess costs in fracture patients were driven by higher inpatient utilizations and costs. Among commercially insured patients, 93.5% with hip fracture, 33.3% with vertebral fracture, and 24.6% with NVNH fracture had at least one inpatient admission in the year 1 post-index year compared to 5.4%, 5.4%, and 5.6% of matched controls, respectively (Table 2). Whereas, among Medicare-insured patients, 90.2% with hip fracture, 50.9% with vertebral fracture, and 51.5% with NVNH fracture had at least one inpatient admission in the index year compared to 19.6%, 18.4%, and 17.0% of matched controls, respectively (Table 2). In year 1, inpatient admission costs comprised 63.4% ($54,772) of total costs for commercially insured patients with hip fracture and 50.5% ($32,719) of total costs for Medicare-insured patients with hip fracture compared to 21.2% ($1918) and 29.5% ($4172) for their respective control cohorts. For other cohorts, inpatient admissions in year 1 comprised 34.6 to 47.6% of costs for fracture patients and 19.8 to 29.5% of costs for controls. The utilization of inpatient services remained higher for fracture patients than controls during the long-term follow-up period (Supplementary Table 2).
Table 2.
All-cause total, inpatient, skilled nursing facility (SNF), and outpatient (OP) prescription utilization and costs in the first year following fracture
| Commercial | Medicare | |||
|---|---|---|---|---|
| Fracture patients | Controls | Fracture patients | Controls | |
| Hip fracture cohort | N = 5329 | N = 5329 | N = 44,008 | N = 44,008 |
| Total healthcare costs, US$ (mean, SD) | $86,427 ($107,474) | $9057 ($20,716)** | $64,846 ($66,818) | $14,137 ($28,987)** |
| Patients with an inpatient admission (N, %) | 4983 (93.5) | 290 (5.4)** | 39,687 (90.2) | 8619 (19.6)** |
| Admissions per patient (mean, SD) | 1.6 (1.3) | 0.1 (0.4)** | 1.3 (0.9) | 0.2 (0.6)** |
| Hospitalization days (mean, SD) | 5.2 (5.2) | 0.2 (1.1)** | 5.2 (6.1) | 0.9 (3.0)** |
| Inpatient costs (mean, SD) | $54,772 ($77,960) | $1918 ($14,516)** | $32,719 ($46,710) | $4172 ($17,754)** |
| Patients with a SNF visit (N, %) | 1370 (25.7) | 23 (0.4)** | 29,772 (67.7) | 6265 (14.2)** |
| SNF costs (Mean, SD) | $3510 ($10,743) | $47 ($1524)** | $14,869 ($22,119) | $1309 ($7200)** |
| Patients with an OP prescription (N, %) | 5199 (97.6) | 4672 (87.7)** | 42,166 (95.8) | 39,584 (89.9)** |
| OP prescription costs (Mean, SD) | $6453 ($12,921) | $2199 ($4789)** | $3823 ($6109) | $2901 ($3991)** |
| Patients with an osteo-related medications (N, %)1 | 1464 (27.5) | 509 (9.6)** | 11,552 (26.2) | 7042 (16.0)** |
| Vertebral fracture cohort | N = 16,550 | N = 16,550 | N = 43,175 | N = 43,175 |
| Total healthcare costs (mean, SD) | $49,165 ($95,332) | $9561 ($24,098)** | $41,445 ($63,625) | $14,229 ($33,212)** |
| Patients with an inpatient admission (N, %) | 5510 (33.3) | 901 (5.4)** | 21,962 (50.9) | 7947 (18.4)** |
| Admissions per patient (mean, SD) | 0.6 (1.1) | 0.1 (0.3)** | 0.7 (0.9) | 0.2 (0.5)** |
| Hospitalization days (mean, SD) | 1.8 (4.4) | 0.2 (1.4)** | 2.7 (5.1) | 0.9 (3.4)** |
| Inpatient costs (mean, SD) | $23,388 ($74,501) | $1892 ($13,773)** | $15,541 ($38,706) | $4214 ($22,428)** |
| Patients with a SNF visit (N, %) | 734 (4.4) | 60 (0.4)** | 12,471 (28.9) | 5152 (11.9)** |
| SNF costs (mean, SD) | $638 ($5172) | $28 ($906)** | $5059 ($14,262) | $1070 ($6250)** |
| Patients with an OP prescription (N, %) | 16,035 (96.9) | 14,599 (88.2)** | 41,849 (96.9) | 39,077 (90.5)** |
| OP prescription costs (mean, SD) | $5776 ($13,001) | $2234 ($5968)** | $4870 ($8602) | $2967 ($4356)** |
| Patients with an osteo-related medications (N, %)1 | 4432 (26.8) | 1364 (8.2)** | 17,228 (39.9) | 6952 (16.1)** |
| NHNV fracture cohort | N = 70,046 | N = 70,046 | N = 47,082 | N = 47,082 |
| Total healthcare costs (mean, SD) | $27,282 ($47,949) | $9549 ($25,818)** | $37,805 ($57,341) | $14,273 ($32,898)** |
| Patients with an inpatient admission (N, %) | 17,214 (24.6) | 3896 (5.6)** | 24,262 (51.5) | 8026 (17.0)** |
| Admissions per patient (mean, SD) | 0.3 (0.7) | 0.1 (0.3)** | 0.7 (0.8) | 0.2 (0.5)** |
| Hospitalization days (mean, SD) | 1.0 (3.2) | 0.2 (1.4)** | 2.5 (4.6) | 0.8 (2.7)** |
| Inpatient costs (mean, SD) | $9428 ($33,853) | $2016 ($15,196)** | $14,170 ($36,267) | $3971 ($17,952)** |
| Patients with a SNF visit (N, %) | 2387 (3.4) | 284 (0.4)** | 15,097 (32.1) | 4709 (10.0)** |
| SNF costs (mean, SD) | $441 ($3767) | $26 ($723)** | $6550 ($16,165) | $964 ($6074) |
| Patients with an OP prescription (N, %) | 66,626 (95.1) | 61,344 (87.6)** | 45,148 (95.9) | 42,828 (91.0)** |
| OP prescription costs (mean, SD) | $3282 ($10,417) | $2243 ($6699)** | $3930 ($6642) | $3003 ($4780)** |
| Patients with an osteo-related medications (N, %)1 | 7267 (10.4) | 5532 (7.9)** | 10,585 (22.5) | 7461 (15.8)** |
**p < 0.001
1Includes oral and injectable bisphosphonates (alendronate, ibandronate, risedronate, zoledronic acid), calcitonin, denosumab, raloxifene, and teriparatide
In Medicare patients, skilled nursing facility utilization and costs were much higher in fracture patients than controls throughout the follow-up time. The percentage of Medicare-insured hip, vertebral, and NHNV fracture patients with at least one visit to a SNF in year 1 was 67.7%, 28.9%, and 32.1%, respectively, compared to 14.2%, 11.9%, and 10.0% of matched controls (Table 2).
Among year 1, outpatient pharmacy costs comprised only 7.5% ($6297) of $86,427 total costs for commercially insured patients with hip fracture and only 5.9% ($3731) of $64,846 total costs for Medicare-insured patients with hip fracture. For vertebral and NHNV fracture cohorts, outpatient prescriptions in year 1 comprised 10.4 to 12.0% of costs for fracture patients and 20.9 to 23.5% of costs for controls. Among those with at least one outpatient prescriptions, only 10.4–27.5% of commercially insured fracture patients and 22.5–39.9% of Medicare-insured fracture patients had at least one osteoporosis-related medication (Table 2).
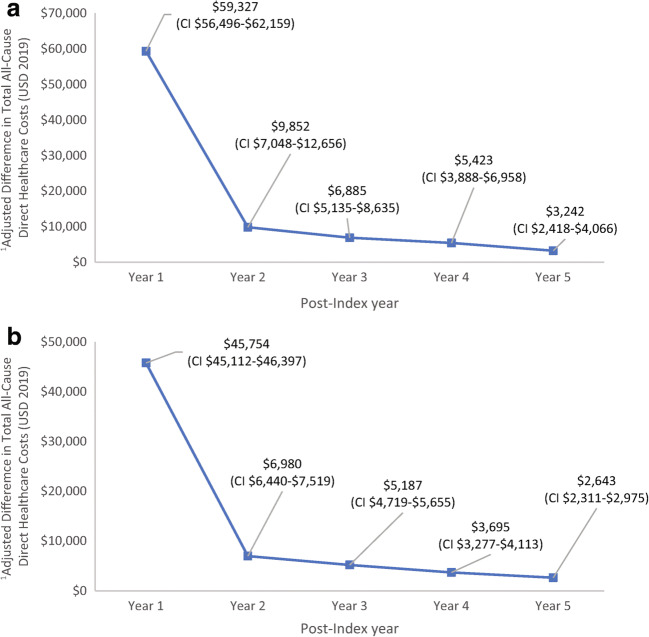
After adjusting for differences in demographic characteristics, clinical characteristics, and baseline healthcare costs, the difference in mean (95% CI) total healthcare costs between patients with hip fracture and matched controls in the first year post-index was $59,327 ($56,496–$62,159) for commercially insured patients and $45,754 ($45,112–$46,397) for Medicare-insured patients (Fig. 3). The difference in healthcare costs between patients with hip fracture and controls decreased substantially from year 1 to year 2 and gradually between year 2 and year 5 but remained significantly elevated for the full follow-up period. Trends were similar for patients with commercial insurance and those with vertebral and NHNV fractures (Supplementary Fig. 1).
Fig. 3.
Adjusted difference in total healthcare costs between patients with hip fracture and their matched controls with a commercial or b Medicare insurance. 1Adjusted for demographics, clinical characteristics, and baseline health care costs
The number of days lost due to workplace absenteeism in year 1 was significantly higher among commercially insured patients with fracture than matched controls regardless of fracture type (all p < 0.05) (Supplementary Table 3). Patients with hip fractures had 20 more days lost due to absenteeism compared to controls. Patients with vertebral and NHVN fracture respectively had 13.2 and 12.0 more absentee days than controls. Subsequently, patients with hip, vertebral, or NHNV fracture-incurred higher indirect costs due to workplace absenteeism, with the incremental costs ranging from $2511 to $4305. STD days and indirect costs due to STD in year 1 were significantly higher among patients with fracture than matched controls (all p < 0.001). The STD days were 43.1 days higher for patients with hip fracture, 20.9 days for vertebral fracture, and 18.9 days for NHNV fracture in year 1. The indirect costs due to STD were $6208 higher for patients with hip fracture, $3092 with vertebral fracture, $2773 with NHNV fracture than their control counterparts. After adjusting for covariates, patients with fracture had consistently higher adjusted mean (95% CI) indirect costs due to STD (incremental cost $5848 [$4854–$6841], $2748 [$2290–$3206], and $2596 [$2425–$2765] for hip, vertebral, and NHNV fracture, respectively) compared with controls during year 1 post-index. The adjusted costs due to STD during year 2 to 5 post-index were not significantly different between fracture patients and controls with the exception of patients with vertebral fracture incurring higher costs during year 3 ($679 [$148–$1210], p = 0.012) and year 4 ($449 [$17–$880], p = 0.041).
Discussion
This retrospective US claims analysis of women over 50 years of age found that non-traumatic fractures have a significant and sustained effect on healthcare costs. Over a 5-year post-fracture follow-up period, total all-cause healthcare costs were significantly higher for patients with a non-traumatic fracture than matched controls regardless of fracture location or insurance payer even after adjusting for the difference in baseline characteristics and costs. The incremental cost of fracture was highest in year 1 and, among patients with hip fracture, which was driven by high utilization of inpatient services. The use of skilled nursing facilities was higher among fracture patients than matched controls and, among Medicare-insured fracture patients, comprised 12.2–22.9% of total healthcare costs. Despite the considerable and sustained costs of fracture, less than a quarter of patients were diagnosed with osteoporosis or received osteoporosis-related treatment prior to their non-traumatic fracture. Even after non-traumatic fractures, only 10.4–27.5% of commercially insured fracture patients and 22.5–39.9% of Medicare-insured fracture patients received osteoporosis-related treatment.
These findings are consistent with the existing literature on the initial costs of non-traumatic fractures. A study of osteoporosis patients with a fracture event between 1997 and 2001, found that patients with fracture spent over twice that as patients with osteoporosis but without a fracture (US $15,942 vs $6476) and nearly three times that of the age- and sex-matched control group ($4658) [14]. The 2019 Milliman Report found the direct medical costs in year 1 following a new osteoporotic fracture were $21,844 among Medicare fee-for-service beneficiaries, with hip fracture incurring the highest costs (US $47,377) [6]. In a prior analysis of the MarketScan Databases, Shi et al. estimated the costs of hip, vertebral, and NHNV fractures to be $26,545, $14,977, and $9183 for commercially insured patients and $15,196, $6701, and $6106 for Medicare-insured patients in the first year following fracture (2006 USD) [20]. A more recent study of patients in a managed care population estimated the unadjusted 1-year healthcare costs of patients with hip, vertebral, and NHNV fractures to be $35,898, $23,634, and $12,918 for commercially insured patients and $32,919, $18,117, and $13,769 for Medicare-insured patients (2016 USD) [22]. The higher costs among commercially insured patients across these studies compared to Medicare-insured patients may be due to the lower reimbursement rates by Medicare. Hospital readmission and transfer to a skilled nursing facility are covered by the payment from the first admission in Medicare but are paid in full by commercial providers [20]. Because payment is not required from the Medicare supplemental side, which is our data source in MarketScan Medicare Database, no claim for services is incurred. Although the costs are underestimated in Medicare, the findings accurately reflected the costs to employers and health plans for Medicare patients.
Our findings on the indirect costs of non-traumatic fracture are supported by prior studies [30, 31]. A study of long bone fractures in working-age adults reported that, depending on fracture site and number, the incremental indirect cost of absenteeism ranged from $950 to $2600, and the incremental cost of STD ranged from $2050 to $4600 (2008 USD) [30]. An analysis of patients with osteoporosis and non-vertebral fractures (includes hip and NHNV) by Pike et al. found that fracture patients were nearly three times as likely to receive disability benefits (18.0% vs 6.5%, p < 0.05), and their mean disability period was twice as long as controls (16.0 vs 6.5 days, p < 0.05) [31]. Pike et al. also reported that the incremental cost due to absenteeism was $1875 for patients with NHNV fractures (2006 USD).
Hip fractures are among the most expensive fracture sites due to the high utilization of inpatient and skilled nursing facility services [2, 20, 32]. Over the past 3 decades, post-surgery care for hip fractures has been shifting from the inpatient setting to that of skilled nursing facilities. An analysis of Medicare claims found that while the median duration of hospitalization for hip fracture decreased from 12 to 5 days between 1988 and 2005, the percentage of patients being discharged into a skilled nursing facility increased from 34 to 54% over the same time frame [33].
In 2010, there were an estimated 53.6 million Americans over the age of 50 years with osteoporosis or low bone mass, with the number expected to grow by 33% by 2030 [34]. Despite being a leading modifiable risk factor for non-traumatic fractures and a chronic condition requiring continued treatment, osteoporosis and low bone mass are underdiagnosed and undertreated, which was also observed in our study [35–37]. The acute and sustained impact on healthcare costs observed in this study should be considered when evaluating pharmaceutical and non-pharmaceutical interventions to reduce non-traumatic fractures.
The primary limitation of this study is that it excludes the 20–30% of patients with hip fracture who die within 1 year [7, 33]. This study was designed to examine the long-term costs of non-traumatic fracture, but the initial acute costs for patients who die from their fracture may be substantial and not accounted for in this analysis due to the minimum 1-year follow-up. In addition, we do not capture what portion of patient attrition in subsequent years is due to mortality rather than other causes and cannot determine if there was excess mortality between the fracture and non-fracture patients.
Non-traumatic fractures were identified by the location of the fracture, the type of fracture, and the exclusion of patients with codes indicating major trauma. This approach may result in the inclusion of patients with fractures due to moderate trauma and miss patients whose fractures do not come to clinical attention. The latter is particularly a problem for vertebral fractures as these often go undiagnosed but may contribute to pain, disability, and costs [38]. In addition, our study did not differentiate patients with or without subsequent fractures or patients with multiple fractures on this index date, which may impact the long-term economic burden of fracture and identification of the subgroup most likely to benefit from additional intervention [39]. This study used data from patients with commercial insurance and Medicare supplemental insurance, and the findings may not be generalizable to the uninsured or those with other insurance. Finally, although we used multivariable analysis to control for baseline differences in cohorts, there are several factors that may influence fracture costs that are not captured in administrative claims and, therefore, could not be controlled for. In particular, the results of bone mineral density testing is not available in claims data and could not be incorporated into our analysis. The presence of osteoporosis and low bone mass was captured using ICD-9-CM and ICD-10-CM diagnosis codes, and likely underestimates the prevalence of these conditions as they are undercoded in claims data and underdiagnosed in clinical practice [7, 37, 40].
Conclusion
The cost difference between matched hip, vertebral, and NHNV fracture and comparison patients was largest during the year 1 post-index period and remained substantial during the year 2 to year 5 post-index. Total unadjusted and adjusted cost differences were highest for hip fracture patients compared to vertebral and NHNV fracture patients. Indirect costs due to workplace absenteeism and STD were markedly higher among the fracture patients relative to comparison patients. The study findings highlight the sustained economic burden of non-traumatic fractures in the short-term (1 year) and long-term (2–5-year post-fracture), and underscored the need for early patient identification and continued management.
Supplementary Information
(PDF 54 kb)
(PDF 17 kb)
(PDF 57 kb)
(PDF 44 kb)
Acknowledgments
Medical writing services were provided by Jessamine Winer-Jones PhD of IBM Watson Health. Programming services were provided by Christina Larson Chebili of IBM Watson Health. Statistical analysis services were provided by Virginia Noxon, Philip Chan, and David M Smith of IBM Watson Health. The study was supported by Amgen Inc.
Availability of data and material
The data that support the findings of this study are available from IBM Watson Health. Restrictions apply to the availability of these data, which were used under license for this study.
Funding
This study was funded by Amgen Inc.
Compliance with ethical standards
Conflicts of interest/competing interests
Xiaoqing Xu, Shravanthi Gandra, and Michele McDermott are employed by Amgen Inc. Oth Tran is employed by IBM Watson Health, which received funding from Amgen Inc. to conduct this study. Stuart Silverman is a consultant of Amgen Inc. Machaon Bonafede was employed by IBM Watson when the study was conducted, and is currently employed by Veradigm. Kathleen Fox is a consultant of Amgen, Inc..
Code availability
The codes that support the findings of this study are available from IBM Watson Health. Restrictions apply to the availability of these codes, which were used under license for this study.
Footnotes
The original online version of this article was revised: The last line of the Abstract Methods is as follows: “Costs were standardized to 2019 US dollars.” The text should be 2018 US dollars. The last line of the article Methods Healthcare utilization costs section reads as follows: “All costs were adjusted for inflation using the medical care component of the Consumer Price Index and standardized to 2019 US dollars”. The text should be 2018 US dollars. Table 1: The cells in the row headed Osteoporosis diagnosis contain the incorrect data.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/29/2022
A Correction to this paper has been published: 10.1007/s00198-022-06410-1
References
- 1.(2016) Federal Interagency Forum on Aging Related Statistics. Older americans 2016: key indicators of well-being. U.S. Government Printing Office. https://agingstats.gov/docs/LatestReport/Older-Americans-2016-Key-Indicators-of-WellBeing.pdf. Accessed 30 January 2020
- 2.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 3.Singer A, Exuzides A, Spangler L, O’Malley C, Colby C, Johnston K, Agodoa I, Baker J, Kagan R. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90:53–62. doi: 10.1016/j.mayocp.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 4.Lespessailles E, Cortet B, Legrand E, Guggenbuhl P, Roux C. Low-trauma fractures without osteoporosis. Osteoporos Int. 2017;28:1771–1778. doi: 10.1007/s00198-017-3921-7. [DOI] [PubMed] [Google Scholar]
- 5.Stone KL, Seeley DG, Lui L-Y, Cauley JA, Ensrud K, Browner WS, Nevitt MC, Cummings SR, Osteoporotic Fractures Research Group BMD at multiple sites and risk of fracture of multiple types: long-term results from the study of osteoporotic fractures. J Bone Miner Res. 2003;18:1947–1954. doi: 10.1359/jbmr.2003.18.11.1947. [DOI] [PubMed] [Google Scholar]
- 6.What women need to know. National Osteoporosis Foundation. https://www.nof.org/preventing-fractures/general-facts/what-women-need-to-know/#caucasian. Accessed 20 July 2020
- 7.Dane Hansen, Carol Bazell, Pamela Pelizzari, Pyenson B (2019) Medicare cost of osteoporotic fractures: the clinical and cost burden of an important consequence of osteoporosis. https://www.bonehealthpolicyinstitute.org/full-milliman-report. Accessed 27 January 2020
- 8.Amin S, Achenbach SJ, Atkinson EJ, Khosla S, Melton Iii LJ. Trends in fracture incidence: a population-based study over 20 years. J Bone Miner Res. 2014;29:581–589. doi: 10.1002/jbmr.2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Budhia S, Mikyas Y, Tang M, Badamgarav E. Osteoporotic fractures: a systematic review of U.S. healthcare costs and resource utilization. Pharmacoeconomics. 2012;30:147–170. doi: 10.2165/11596880-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 10.Odén A, McCloskey EV, Kanis JA, Harvey NC, Johansson H. Burden of high fracture probability worldwide: secular increases 2010–2040. Osteoporos Int. 2015;26:2243–2248. doi: 10.1007/s00198-015-3154-6. [DOI] [PubMed] [Google Scholar]
- 11.Hannan MT, Weycker D, McLean RR, Sahni S, Bornheimer R, Barron R, et al. Predictors of imminent risk of nonvertebral fracture in older, high-risk women: the Framingham Osteoporosis Study. JBMR Plus. 2019;3:e10129. doi: 10.1002/jbm4.10129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonafede M, Shi N, Barron R, Li X, Crittenden DB, Chandler D. Predicting imminent risk for fracture in patients aged 50 or older with osteoporosis using US claims data. Arch Osteoporos. 2016;11:26. doi: 10.1007/s11657-016-0280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Banefelt J, Åkesson KE, Spångéus A, Ljunggren O, Karlsson L, Ström O, Ortsäter G, Libanati C, Toth E. Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos Int. 2019;30:601–609. doi: 10.1007/s00198-019-04852-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orsini LS, Rousculp MD, Long SR, Wang S. Health care utilization and expenditures in the United States: a study of osteoporosis-related fractures. Osteoporos Int. 2005;16:359–371. doi: 10.1007/s00198-004-1694-2. [DOI] [PubMed] [Google Scholar]
- 15.Brenneman SK, Barrett-Connor E, Sajjan S, Markson LE, Siris ES. Impact of recent fracture on health-related quality of life in postmenopausal women. J Bone Miner Res. 2006;21:809–816. doi: 10.1359/jbmr.060301. [DOI] [PubMed] [Google Scholar]
- 16.Borgström F, Lekander I, Ivergård M, Ström O, Svedbom A, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jürisson M, Kallikorm R, Lesnyak O, McCloskey E, Nassonov E, Sanders KM, Silverman S, Tamulaitiene M, Thomas T, Tosteson ANA, Jönsson B, Kanis JA. The international costs and utilities related to osteoporotic fractures study (ICUROS)—quality of life during the first 4 months after fracture. Osteoporos Int. 2013;24:811–823. doi: 10.1007/s00198-012-2240-2. [DOI] [PubMed] [Google Scholar]
- 17.Fujiwara S, Zhao X, Teoh C, Jaffe DH, Taguchi Y. Disease burden of fractures among patients with osteoporosis in Japan: health-related quality of life, work productivity and activity impairment, healthcare resource utilization, and economic costs. J Bone Miner Metab. 2019;37:307–318. doi: 10.1007/s00774-018-0916-1. [DOI] [PubMed] [Google Scholar]
- 18.Silverman S, Viswanathan HN, Yang YC, Wang A, Boonen S, Ragi-Eis S, Fardellone P, Gilchrist N, Lips P, Nevitt M, Palacios Gil-Antuñano S, Pavelka K, Revicki D, Simon J, Macarios D, Siris ES. Impact of clinical fractures on health-related quality of life is dependent on time of assessment since fracture: results from the FREEDOM trial. Osteoporos Int. 2012;23:1361–1369. doi: 10.1007/s00198-011-1720-0. [DOI] [PubMed] [Google Scholar]
- 19.Rohde G, Haugeberg G, Mengshoel AM, Moum T, Wahl AK. Two-year changes in quality of life in elderly patients with low-energy hip fractures. A case-control study. BMC Musculoskelet Disord. 2010;11:226. doi: 10.1186/1471-2474-11-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shi N, Foley K, Lenhart G, Badamgarav E. Direct healthcare costs of hip, vertebral, and non-hip, non-vertebral fractures. Bone. 2009;45:1084–1090. doi: 10.1016/j.bone.2009.07.086. [DOI] [PubMed] [Google Scholar]
- 21.Castelli A, Daidone S, Jacobs R, Kasteridis P, Street AD. The determinants of costs and length of stay for hip fracture patients. PLoS One. 2015;10:e0133545. doi: 10.1371/journal.pone.0133545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Christensen L, Iqbal S, Macarios D, Badamgarav E, Harley C. Cost of fractures commonly associated with osteoporosis in a managed-care population. J Med Econ. 2010;13:302–313. doi: 10.3111/13696998.2010.488969. [DOI] [PubMed] [Google Scholar]
- 23.Gabriel SE, Tosteson ANA, Leibson CL, Crowson CS, Pond GR, Hammond CS, et al. Direct medical costs attributable to osteoporotic fractures. Osteoporos Int. 2002;13:323–330. doi: 10.1007/s001980200033. [DOI] [PubMed] [Google Scholar]
- 24.Nikitovic M, Wodchis WP, Krahn MD, Cadarette SM. Direct health-care costs attributed to hip fractures among seniors: a matched cohort study. Osteoporos Int. 2013;24:659–669. doi: 10.1007/s00198-012-2034-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 26.Consumer Price Index details report tables United States Department of Labor. https://www.bls.gov/cpi/home.htm. Accessed 1 October 2020
- 27.American Community Survey. The United States Census Bureau. https://data.census.gov/mdat/. Accessed 20 March 2020
- 28.Song X, Quek RG, Gandra SR, Cappell KA, Fowler R, Cong Z. Productivity loss and indirect costs associated with cardiovascular events and related clinical procedures. BMC Health Serv Res. 2015;15:245. doi: 10.1186/s12913-015-0925-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bonafede M, Sapra S, Shah N, Tepper S, Cappell K, Desai P. Direct and indirect healthcare resource utilization and costs among migraine patients in the United States. Headache. 2018;58:700–714. doi: 10.1111/head.13275. [DOI] [PubMed] [Google Scholar]
- 30.Bonafede M, Espindle D, Bower AG. The direct and indirect costs of long bone fractures in a working age US population. J Med Econ. 2013;16:169–178. doi: 10.3111/13696998.2012.737391. [DOI] [PubMed] [Google Scholar]
- 31.Pike C, Birnbaum HG, Schiller M, Sharma H, Burge R, Edgell ET. Direct and indirect costs of non-vertebral fracture patients with osteoporosis in the US. Pharmacoeconomics. 2010;28:395–409. doi: 10.2165/11531040-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 32.Schousboe JT, Paudel ML, Taylor BC, Kats AM, Virnig BA, Dowd BE, Langsetmo L, Ensrud KE. Pre-fracture individual characteristics associated with high total health care costs after hip fracture. Osteoporos Int. 2017;28:889–899. doi: 10.1007/s00198-016-3803-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29:2520–2526. doi: 10.1002/jbmr.2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flais J, Coiffier G, Le Noach J, Albert JD, Faccin M, Perdriger A, et al. Low prevalence of osteoporosis treatment in patients with recurrent major osteoporotic fracture. Arch Osteoporos. 2017;12:24. doi: 10.1007/s11657-017-0317-4. [DOI] [PubMed] [Google Scholar]
- 36.Gillespie CW, Morin PE. Osteoporosis-related health services utilization following first hip fracture among a cohort of privately-insured women in the United States, 2008–2014: an observational study. J Bone Miner Res. 2017;32:1052–1061. doi: 10.1002/jbmr.3079. [DOI] [PubMed] [Google Scholar]
- 37.Gillespie CW, Morin PE. Trends and disparities in osteoporosis screening among women in the United States, 2008-2014. Am J Med. 2017;130:306–316. doi: 10.1016/j.amjmed.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 38.Bottai V, Giannotti S, Raffaetà G, Mazzantini M, Casella F, De Paola G, et al. Underdiagnosis of osteoporotic vertebral fractures in patients with fragility fractures: retrospective analysis of over 300 patients. Clinical cases in mineral and bone metabolism : the official journal of the Italian Society of Osteoporosis, Mineral Metabolism, and Skeletal Diseases. 2016;13:119–122. doi: 10.11138/ccmbm/2016.13.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leslie WD, Schousboe JT, Morin SN, Martineau P, Lix LM, Johansson H, McCloskey EV, Harvey NC, Kanis JA. Fracture risk following high-trauma versus low-trauma fracture: a registry-based cohort study. Osteoporosis Int. 2020;31:1059–1067. doi: 10.1007/s00198-019-05274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cheng H, Gary LC, Curtis JR, Saag KG, Kilgore ML, Morrisey MA, Matthews R, Smith W, Yun H, Delzell E. Estimated prevalence and patterns of presumed osteoporosis among older Americans based on Medicare data. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2009;20:1507–1515. doi: 10.1007/s00198-009-0835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 54 kb)
(PDF 17 kb)
(PDF 57 kb)
(PDF 44 kb)
Data Availability Statement
The data that support the findings of this study are available from IBM Watson Health. Restrictions apply to the availability of these data, which were used under license for this study.