Introduction
Subcutaneous implantable cardioverter-defibrillators (S-ICD) have been shown to be noninferior to conventional transvenous ICDs with respect to device-related complications and inappropriate shocks.1 For patients who meet indications for an ICD and do not require bradycardia pacing, antitachycardia pacing, or cardiac resynchronization therapy, it is becoming an attractive option to avoid vascular complications. Complications such as lead malfunction and infection are more common with the transvenous ICD, whereas inappropriate shocks are more common with the S-ICD.1 The majority of inappropriate S-ICD therapies results from T-wave oversensing, but there are also reports of QRS double or triple counting, especially in times of electrolyte derangements. We report a case where oversensing of multiple components of a ventricular escape rhythm resulted in inappropriate shocks owing to a unique S-ICD algorithm.
Case report
We report a 58-year-old woman with a past medical history of hypertension, diabetes mellitus, dyslipidemia, end-stage renal failure on hemodialysis, peripheral vascular disease with previous right and left below-knee amputations, nonischemic cardiomyopathy diagnosed since 2011, and an S-ICD (Boston Scientific 1010 SQ-RX S-ICD) implanted since 2014. She presented to the emergency room for lethargy and drowsiness and reports of shocks from her S-ICD.
A device interrogation shows 4 treated episodes with 4 shocks delivered. Her S-ICD had been programmed with a shock zone at 220 beats per minute (bpm) and conditional shock zone at 200 bpm with postshock pacing turned on. Figure 1 shows episode 1 where there is a development of a broad complex tachycardia around 130 bpm (tachycardia cycle length about 460 ms) resembling a sinewave pattern. The device starts to double count each QRS complex, which is initially appropriately interpreted by the device, resulting in some beats being discarded. Subsequently, there is intermittent triple counting of the QRS complexes, satisfying tachycardia detection, resulting in charging and delivery of a shock at an acceptable shock impedance. The shock effectively converts the patient back to baseline rhythm with a few initial paced beats.
Figure 1.
Subcutaneous implantable cardioverter-defibrillator device electrograms; episode 1 showing the spontaneous development of a wide complex tachycardia followed by delivery of a shock.
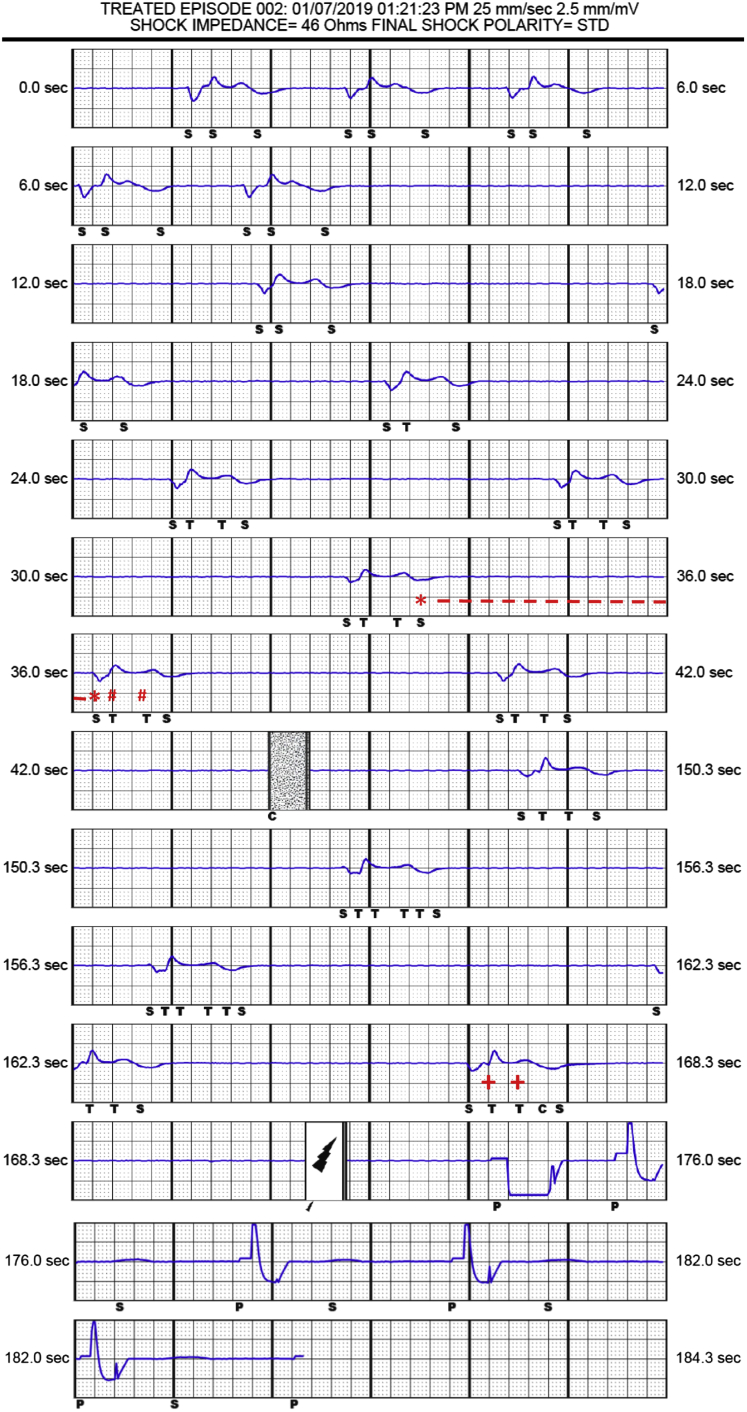
A second episode, depicted in Figure 2, occurs about 30 minutes following episode 1. There is significant bradycardia, likely a broad ventricular escape rhythm at 38 bpm with intermittent ventricular pauses. The device initially oversenses on 2 components of the QRS and the T wave, resulting in triple counting of each complex signal. Subsequently there is oversensing on 3 components of the QRS and T wave, which results in short intervals falling in the tachycardia zone, leading to charging and inappropriate shock delivery. Following this shock, there is back-up pacing from the device with persistence of oversensing. The patient continues to experience 2 further episodes of inappropriate shocks, similar to episode 2, before presenting to the emergency room.
Figure 2.
Subcutaneous implantable cardioverter-defibrillator device electrograms; episode 2 showing the development of bradycardia, likely ventricular escape rhythm, followed by delivery of a shock. The S-S interval labeled with ∗ represents one of the first certified intervals after a long pause, which is discarded while the subsequent intervals, ST and T-T intervals labeled with #, continue to contribute to tachycardia detection until the detection counter is fulfilled. The last 2 certified consecutive intervals, ST and T-T intervals labeled with +, confirm rhythm persistence before shock is delivered.
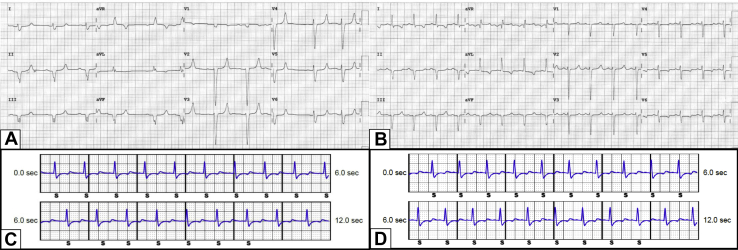
Figure 3A shows her presenting electrocardiogram at the emergency room. She was in normal sinus rhythm at about 75 bpm with isolated atrial ectopic beats and widened QRS duration at 135 ms, with delayed terminal depolarization. She was found to be have severe hyperkalemia, with a serum potassium of 9.7 mmol/L, and metabolic acidosis, with a serum bicarbonate level of 9.0 mmol/L. Her other laboratory investigations were within her baseline limits. She missed her last hemodialysis session, as no family member was available to bring her to the dialysis center. She underwent urgent hemodialysis and a recheck serum potassium and bicarbonate showed normalized values. Figure 3B shows a repeat electrocardiogram with sinus rhythm at 100 bpm and normalized QRS duration at 95 ms. Figure 3C and 3D shows the S-ICD electrograms at the time of presentation and following correction of electrolyte derangements, respectively. There were no perceivable differences in S-ICD sensing during normal sinus rhythm.
Figure 3.
A: The patient’s presenting electrocardiogram (ECG) with normal sinus rhythm and isolated atrial ectopic beats and widened QRS duration of 135 ms. There is also prolonged atrial conduction with flattened and broadened P waves, and prolonged PR interval. B: The patient’s ECG following hemodialysis with sinus rhythm, normalization of QRS duration to 95 ms, atrial conduction time, and PR interval. C, D: The S-ICD electrograms at the time of presentation (C) and following correction of electrolyte derangements (D), where there were no perceivable differences in subcutaneous implantable cardioverter-defibrillator sensing during normal sinus rhythm.
Discussion
This patient had severe hyperkalemia and metabolic acidosis as a result of missed hemodialysis, which led to an initial spontaneous episode of slow ventricular tachycardia with a sinewave pattern. Although this ventricular tachycardia was well below the programmed tachycardia zones, double and triple counting led to tachycardia detection and delivery of shock therapy. The shock effectively converted the rhythm back to baseline rhythm with a few beats of backup pacing with residual signs of oversensing. Despite the inappropriate tachycardia detection and the chance that this could have terminated with antitachycardia pacing, this is still considered an appropriate therapy.
In the second episode, despite long ventricular pauses, oversensing of multiple components of the escape beat led to tachycardia detection with an inappropriate shock. This is owing to an algorithm that is unique to the S-ICD. Owing to its subcutaneous nature and potential risk of undersensing during tachycardia, the S-ICD does not certify any sensed beat that is less than 30 bpm or being more than a 2-second interval apart.2 Nonetheless, the first sensed beat following a pause would still be labeled with an “S,” just like a certified beat would be. However, it will not be used to calculate the 4 R-R intervals that contribute to tachycardia detection.2 Using 2 complexes in Figure 2 for illustration, the first certified interval (S-S interval labeled with ∗) after a long pause is discarded, while the subsequent intervals (ST and T-T intervals labeled with #) continue to contribute to tachycardia detection. Hence, the detection counter is never reset and progressively increases until the 18 out of 24 criteria are met before capacitor charging is initiated. Rhythm persistence analysis is employed, which requires the x out of y condition to be maintained or exceeded in the last 2 certified consecutive intervals (ST and T-T intervals labeled with +) before shock is delivered.
Hyperkalemia can cause an increase in T-wave amplitude. Differences between the action potential characteristics of ventricular endocardial and epicardial tissues and predominant distribution of the Ik1 in the endocardial tissue lead to a strong association of extracellular potassium concentration with the repolarization process.3 In addition, the resting membrane potential becomes less negative with hyperkalemia, thereby reducing the rate of rise of phase 0, which causes widening of the QRS complex.4 As a result, patients with cardiac devices who develop hyperkalemia are vulnerable to T-wave oversensing and QRS overcounting.
It is interesting to note that oversensing only occurred during the ventricular escape rhythm and not during normal sinus rhythm, as demonstrated in Figure 3C and 3D. It is likely that hyperkalemia accentuated several components of the broad QRS complex escape rhythm and also attenuated the QRS-to-T-wave amplitude ratio, resulting in oversensing.
This patient had a first-generation S-ICD without a SMART Pass algorithm. However, SMART Pass would not have impacted the decision for delivering a shock for this episode because it was designed to reduce non-QRS signals and would have been disabled owing to long intervals between sensed events.2 The S-ICD only delivers therapies at tachycardia rates above 170 bpm, and adding a conditional zone has been shown to reduce inappropriate shocks, but this would not have changed the outcome in this case, as the arrhythmias were way below the therapy zone.
Hence, profound bradycardias in combination with oversensing can lead to tachycardia detection and inappropriate shocks, even from contemporary S-ICDs with SMART Pass.5,6 To our knowledge, this is the first case report of a patient presenting with inappropriate shocks owing to bradycardia. It is important that physicians recognize the limitations of the S-ICD in times of bradycardia, and perhaps future algorithms can be developed to mitigate such scenarios.
Key Teaching Points.
-
•
Hyperkalemia increases the amplitude of T waves and broadens QRS complexes, making the subcutaneous implantable cardioverter-defibrillator (S-ICD) vulnerable to both T-wave oversensing and QRS overcounting.
-
•
A unique algorithm in the S-ICD makes it susceptible to delivering inappropriate therapies in times of bradycardia and oversensing. Hence it should not be recommended to patients with significant bradycardia and pauses.
-
•
Contemporary S-ICDs with programmed SMART Pass algorithms and conditional zones will not mitigate scenarios of oversensing during bradycardia.
Acknowledgement
The authors acknowledge the assistance in analysis and interpretation of device decisions provided by Mr Luke Michael and Ms Rena Lim, Boston Scientific Technical Service.
Footnotes
Disclosures: All authors have no relevant disclosures pertaining to this case report.
References
- 1.Knops R.E., Olde Nordkamp L.R.A., Delnoy P.-P.H.M. Subcutaneous or transvenous defibrillator therapy. N Engl J Med. 2020;383:526–536. doi: 10.1056/NEJMoa1915932. [DOI] [PubMed] [Google Scholar]
- 2.Boston Scientific Emblem Subcutaneous Implantable Cardioverter Defibrillator User’s Manual. https://www.bostonscientific.com/content/dam/bostonscientific/Rhythm%20Management/portfolio-group/EMBLEM_S-ICD/Download_Center/359481-001%20EMBLEM%20S-ICD%20PTM_English.pdf
- 3.Aoki K., Okajima K., Kiuchi K., Yokoi K., Teranishi J., Shimane A. A case of inappropriate implantable cardioverter defibrillator therapy induced by T-wave oversensing due to hyperkalemia. J Arrhythm. 2015;31:395–397. doi: 10.1016/j.joa.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barold S.S., Herweg B. The effect of hyperkalaemia on cardiac rhythm devices. Europace. 2014;16:467–476. doi: 10.1093/europace/eut383. [DOI] [PubMed] [Google Scholar]
- 5.Wilson D., Yue A., Roberts P.R., Morgan J.M. Oversensing and shock delivery in the S-ICD: five shocks two mechanisms. Pacing Clin Electrophysiol. 2015;28:1009–1012. doi: 10.1111/pace.12532. [DOI] [PubMed] [Google Scholar]
- 6.Wiles B.M., Fitzsimmons S.J., Roberts P.R. Post mortem therapy from a subcutaneous ICD: What is the mechanism? Pacing Clin Electrophysol. 2017;40:735–737. doi: 10.1111/pace.13089. [DOI] [PubMed] [Google Scholar]