Abstract
Purpose
To determine whether active smokers have different patient-reported outcomes relative to nonsmokers for pain, function, and overall health at baseline and 1 or 2 years after an arthroscopic partial meniscectomy.
Methods
Patients who underwent arthroscopic partial meniscectomy were identified. Demographic data, including smoking status and patient-reported outcome measures (PROMs), were prospectively collected preoperatively and 3 months, 6 months, 1 year, and 2 years postoperatively. Statistical analysis was performed using the mixed-effects model to compare PROMs preoperatively and 1 or 2 years postoperatively between nonsmokers and active smokers.
Results
509 knees undergoing arthroscopic partial meniscectomy were divided into 2 cohorts: group I, nonsmokers (n = 470) and group II, active smokers (n = 39). There were statistically significant baseline differences in PROMs for nonsmokers versus smokers: visual analog scale (VAS), 5.0 ± 0.4 versus 6.3 ± 0.7, respectively (P = .001); Knee Injury and Osteoarthritis Outcome Score (KOOS) Pain scale, 50.3 ± 3.2 versus 42.5± 5.5 (P = .005); KOOS Symptoms scale, 50.0 ± 3.2 versus 43.6 ± 5.4 (P = .019); and Western Ontario and McMaster Universities Arthritis Index (WOMAC) Pain scale, 57.5 ± 3.4 versus 48.2 ± 6.1 (P = .003). There were also statistically significant differences in nonsmokers versus smokers regarding knee function at baseline shown by the KOOS Activites of Daily Living (ADL) scale: (61.1 ± 3.3 versus 53.5 ± 6.1; P = .015). Baseline mental health, as assessed by the Veterans Rand 12-Item Health Survey (VR-12) Mental Health questionnaire, was also statistically different between nonsmokers (55.4 ± 0.8) and smokers (51.5 ± 3.3; P = .020). Importantly, PROMs for pain and function were lower at all time points for smokers.
Conclusion
Patients who were active smokers at the time of partial meniscectomy had significantly worse baseline and postoperative PROMs compared with nonsmokers. Changes from baseline for smokers and nonsmokers were relatively consistent between groups 1 and 2 years postoperatively. Smokers will improve a relatively similar amount as nonsmokers after partial meniscectomy, but their overall PROM scores are lower.
Level of Evidence
III, retrospective comparative study.
Meniscal tears are the most common knee injury, with an incidence of 23.8/100,000 per year in the United States.1 Injury to the meniscus often causes pain and mechanical symptoms and can limit daily activities. Many patients fail nonoperative treatment measures and ultimately opt for surgical intervention.2, 3, 4
The current options for arthroscopic meniscal surgery are partial meniscectomy or meniscal repair.5 Indications for meniscectomy or meniscal repair are multifactorial and depend on the tear pattern, tear location, stability of the meniscus and knee, and patient factors.6 Many studies have documented uniformly good to excellent results in 80% to 95% of patients within the first 5 years after a partial meniscectomy.6
Knee complications, symptoms, function, and quality of life after a partial meniscectomy are often observed clinically and measured through patient-reported outcome measures (PROMs). Preoperative and intraoperative predictors of poor clinical outcomes and longer rehabilitation times after partial meniscectomy include female sex, lateral meniscal tears, degenerative meniscal tears, and increased body mass index.3,7, 8, 9, 10, 11, 12
Smoking is a known risk factor associated with significantly worse clinical outcomes in surgical procedures.11,13,14 Smoking has been shown to negatively impact clinical outcomes and increase complication rates in anterior cruciate ligament (ACL) reconstruction, total hip and knee arthroplasty, and rotator cuff repairs.9, 10, 11,15 Studies have identified smoking as a risk factor for poor outcomes and as a risk factor for healing after meniscal repair.3,12,16 Additionally, a recent study by Heyer et al.17 determined that smoking was an independent risk factor for complications after meniscectomy. The purpose of this study is to determine whether active smokers have different patient-reported outcomes for pain, function, and overall health at baseline and 1 or 2 years after an arthroscopic partial meniscectomy relative to nonsmokers. The authors hypothesized that patients who smoke at the time of partial meniscectomy will have lower baseline and postoperative PROMs.
Methods
Approval by the institutional review board was obtained before the initiation of the present study. All patients signed an informed consent. An electronic surgical outcomes registry was used for data collection. Data were collected prospectively on consecutive surgeries performed by a single surgeon at an academic medical center and retrospectively reviewed for the present study. Inclusion criteria were age ≥18 years, primary partial meniscectomy (medial and/or lateral) with or without chondroplasty during the study period, baseline data, and 1- and 2- year follow-up data. Exclusion criteria were age <18 years, repeat meniscectomy, ligamentous injury, and <1 follow-up time point. For patients with >1 surgery on the same knee, only the first surgery was included. Patients were indicated for surgery after magnetic resonance imaging (MRI)-confirmed meniscal pathology, and patients had either an acute meniscal tear or chronic/degenerative tears and failed nonoperative treatments including injections and physical therapy. Current smoking status was collected at each time point, and patients were considered smokers if they were smoking at the time of surgery. All patients followed the same standard postoperative rehabilitation protocol for knee arthroscopy and partial meniscectomy.
All participants were administered a preoperative survey consisting of the following validated outcome-measuring tools: visual analog scale (VAS), the Veterans Rand 12-Item Health Survey (VR-12), the Knee Injury and Osteoarthritis Outcome Score (KOOS), a standard preoperative form consisting of 4 questions regarding a patient’s expectations of recovery, a Single Assessment Numeric Evaluation (SANE) knee score, and the Western Ontario and McMaster Universities Arthritis Index (WOMAC). The same outcome measures were reassessed at 3 months, 6 months, 1 year, and 2 years postoperatively. At each data collection point, participants were emailed an electronic survey with 1 email reminder and 1 phone call reminder by a research assistant (K.D.G.) if outcome measures were not completed in a timely manner.
Statistical Analysis
The scores for all functional assessment metrics were tallied for each cohort at each of the time points of data collection preoperatively and postoperatively. Baseline differences in covariates were assessed using t test (continuous variables) and chi-squared test (categorical variables). A linear mixed-effects model to compare outcomes between the groups at each time point accounted for all available data and did not require that subjects have complete data at all time points. Multivariable models adjusted for covariates that were imbalanced at baseline (worker’s compensation status). Statistical analysis was performed using SAS version 9.4 (SAS Institute, Cary, NC) to determine whether there was any correlation between smoking status and functional outcome measures collected. Statistical significance was set at P < .05.
Results
Patient Characteristics
A total of 743 patients who underwent a partial meniscectomy and participated in the outcomes registry from 2012 to 2016 were identified. A total of 509 knees in 495 patients met the inclusion criteria. 481 patients had a single-knee partial meniscectomy, and 14 patients had bilateral knee partial meniscectomies at 2 different time points. There were a total of 470 knees in group I (nonsmokers) and 39 knees in group II (smokers) that underwent partial meniscectomy during the data collection period. Differences in baseline demographics and characteristics between smokers and nonsmokers are presented in Table 1. There were no statistically significant differences between the 2 groups in terms of age at treatment, mean body mass index (BMI), sex, ethnicity, or diabetes; however, there was a statistically significant difference between groups with regard to worker’s compensation status (P < .0001). The 2-year follow-up compliance was 296 patients (58%) with baseline and both year 1 and year 2 postoperative data.
Table 1.
Patient demographics
| Demographic Characteristics | Nonsmokers (n = 470) | Smokers (n = 39) | P Value |
|---|---|---|---|
| Age at treatment (y) | 46.98 ± 11.99 | 47.58 ± 9.97 | .7632 |
| Body mass index (kg/m2) | 29.81 ± 6.31 | 30.09 ± 5.63 | .8283 |
| Sex | .1587 | ||
| Male | 186 | 20 | |
| Female | 282 | 19 | |
| Race/ethnicity | .2179 | ||
| Hispanic | 22 | 4 | |
| Non-Hispanic white | 348 | 30 | |
| Non-Hispanic Black | 18 | 2 | |
| Other | 82 | 3 | |
| Diabetes | .7477 | ||
| No | 449 | 37 | |
| Yes | 19 | 2 | |
| Worker’s compensation | <.0001 | ||
| No | 452 | 32 | |
| Yes | 14 | 7 |
Data are mean ± standard deviation or n (%).
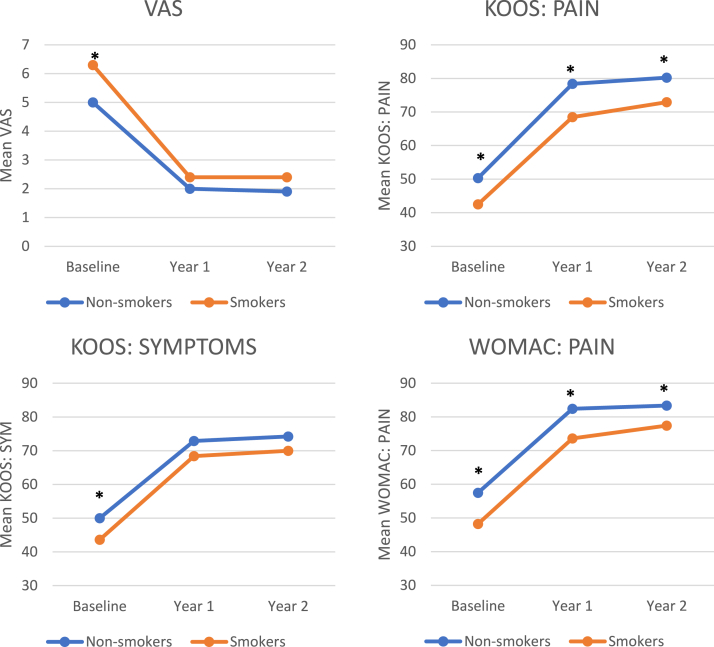
Baseline and Postoperative Knee Pain
The visual analog scale (VAS), Knee Injury and Osteoarthritis Outcome Score (KOOS) for Pain, KOOS for Symptoms, and Western Ontario and McMaster Universities Arthritis Index (WOMAC) for Pain were used to assess overall patient pain experienced at baseline, year 1, and year 2. After adjusting for worker’s compensation status, statistically significant differences at baseline were measured between nonsmokers (5.0 ± 0.4) and smokers (6.3 ± 0.7, P = .0006) for VAS and between nonsmokers (50.0 ± 3.2) and smokers (43.6 ± 5.4, P = .0190) for KOOS: Symptoms. WOMAC scores were transformed so that higher scores indicate improvement in pain, function, and stiffness. Statistically significant differences were measured at baseline by the WOMAC: Pain scale for nonsmokers (57.5 ± 3.4) and smokers (48.2 ± 6.1, P = .0029) and at year 1 for nonsmokers (82.4 ± 3.3) and smokers (73.6 ± 5.6, P = .0021). Statistically significant differences were measured for KOOS: Pain at baseline for nonsmokers (50.3 ± 3.2) and smokers (42.5± 5.5, P = .0047), year 1 for nonsmokers (78.4 ± 3.3) and smokers (68.5 ± 6, P = .0011), and year 2 for nonsmokers (80.2 ± 3.3) and smokers (72.9 ± 6.5, P = .0282) (Figure 1). Table 2 shows the changes from baseline to 1- and 2-year postoperative time points for nonsmokers and smokers in regard to each PROM. The changes from baseline at 1 and 2 years were not statistically significant between nonsmokers and smokers with regard to KOOS: Pain (P = .520 and P = .887 change from baseline at 1 and 2 years, respectively), KOOS: Symptoms (P = .575 and P = .567), or WOMAC: Pain (P = .874 and P = .356). Smokers had lower scores at all time points and improved the same amount for all PROMs except KOOS Sport (baseline to 1 year), in which nonsmokers had statistically significantly greater improvement.
Figure 1.
Mean pain-related patient-reported outcome scores comparing nonsmokers and smokers across study time points (baseline indicates preoperative time point). ∗Significant differences between nonsmokers and smokers.
Table 2.
Changes in PROMs from baseline to 1 and 2 Years postoperatively
| PROM | Time | Nonsmokers | Smokers | P Value |
|---|---|---|---|---|
| KOOS ADL | BL to 1 yr | 24.1 (22.4, 25.8) | 21.3 (15.4, 27.2) | .3648 |
| KOOS ADL | BL to 2 yr | 25.1 (23.2, 27.0) | 22.5 (15.9, 29.2) | .4673 |
| KOOS Pain | BL to 1 yr | 28.0 (26.2, 29.8) | 26.0 (19.9, 32.1) | .5342 |
| KOOS Pain | BL to 2 yr | 29.8 (27.8, 31.8) | 30.3 (23.2, 37.4) | .8838 |
| KOOS QOL | BL to 1 yr | 36.0 (33.6, 38.3) | 29.3 (21.3, 37.4) | .1234 |
| KOOS QOL | BL to 2 yr | 38.8 (36.0, 41.5) | 33.8 (24.0, 43.6) | .3361 |
| KOOS Sport | BL to 1 yr | 36.0 (33.3, 38.8) | 25.4 (16.0, 34.9) | .0346 |
| KOOS Sport | BL to 2 yr | 38.2 (35.0, 41.5) | 30.3 (18.6, 42.0) | .1991 |
| KOOS Symptoms | BL to 1 yr | 22.8 (21.1, 24.6) | 24.7 (18.6, 30.8) | .5599 |
| KOOS Symptoms | BL to 2 yr | 24.1 (22.0, 26.1) | 26.3 (19.1, 33.6) | .5597 |
| KOOS JR | BL to 1 yr | 21.8 (19.6, 24.0) | 17.5 (9.3, 25.8) | .3265 |
| KOOS JR | BL to 2 yr | 23.5 (21.0, 26.1) | 17.1 (7.4, 26.8) | .2076 |
| Marx Activity Rating Scale | BL to 1 yr | –1.7 (–2.2, –1.3) | –0.8 (–2.3, 0.8) | .2591 |
| Marx Activity Rating Scale | BL to 2 yr | –1.7 (–2.2, –1.2) | –1.9 (–3.6, –0.1) | .8673 |
| SANE | BL to 1 yr | 35.4 (30.4, 40.3) | 33.5 (13.2, 53.7) | .8574 |
| SANE | BL to 2 yr | 36.8 (31.7, 41.9) | 33.1 (11.9, 54.2) | .7322 |
| VAS | BL to 1 yr | –3.0 (–3.3, –2.8) | –3.9 (–4.8, –3.1) | .0397 |
| VAS | BL to 2 yr | –3.1 (–3.3, –2.8) | –3.9 (–4.8, –2.9) | .1061 |
| VR-12 Mental | BL to 1 yr | –0.3 (–1.2, 0.6) | –0.1 (–3.2, 3.1) | .9009 |
| VR-12 Mental | BL to 2 yr | 0.2 (–0.7, 1.2) | 1.8 (–1.5, 5.1) | .3745 |
| VR-12 Physical | BL to 1 yr | 13.0 (12.0, 14.0) | 11.3 (7.9, 14.8) | .3490 |
| VR-12 Physical | BL to 2 yr | 14.1 (13.0, 15.2) | 10.8 (6.8, 14.8) | .1167 |
| WOMAC Function | BL to 1 yr | 24.1 (22.4, 25.8) | 21.3 (15.4, 27.2) | .3648 |
| WOMAC Function | BL to 2 yr | 25.1 (23.2, 27.0) | 22.5 (15.9, 29.2) | .4673 |
| WOMAC Pain | BL to 1 yr | 24.9 (23.1, 26.6) | 25.4 (19.4, 31.4) | .8683 |
| WOMAC Pain | BL to 2 yr | 25.7 (23.8, 27.7) | 29.1 (22.3, 35.9) | .3544 |
| WOMAC Stiffness | BL to 1 yr | 20.4 (18.1, 22.6) | 20.4 (12.6, 28.2) | .9885 |
| WOMAC Stiffness | BL to 2 yr | 22.9 (20.3, 25.6) | 24.2 (14.7, 33.7) | .7984 |
Data are median (95% confidence interval).
Abbreviations: ADL, activities of daily living; BL, baseline; JR, joint replacement; KOOS, Knee Injury and Osteoarthritis Outcome Score; PROM, patient-reported outcome measure; QOL, quality of life; SANE, Single Assessment Numerical Evaluation; VAS, visual analog scale; VR-12, Veterans Rand 12-Item Health Survey; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
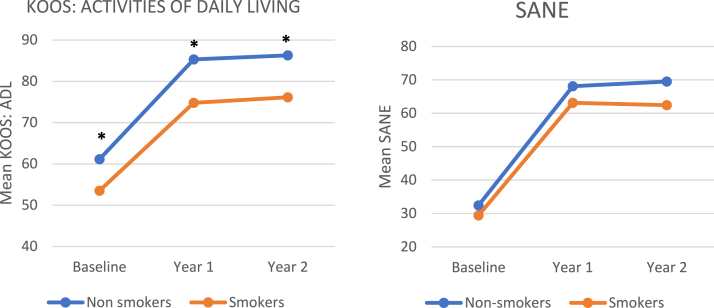
Baseline and Postoperative Knee Function
KOOS Activities of Daily Living (ADL) and SANE were used to assess patient-reported knee function. Statistically significant differences for KOOS ADL were measured at baseline for nonsmokers (61.1 ± 3.3) and smokers (53.5 ± 6.1), year 1 for nonsmokers (85.3 ± 3.1) and smokers (74.8 ± 5.2), and year 2 for nonsmokers (86.3 ± 3.2) and smokers (76.1 ± 5.7) (P = .0152, P < .00001, and P = .0005, respectively). SANE scores were measured at baseline for nonsmokers (32.4 ± 6.6) and smokers (29.4 ±16.6), year 1 for nonsmokers (68.1 ± 6.4) and smokers (63.1 ± 12.2), and year 2 for nonsmokers (69.5 ± 6.5) and smokers (62.4 ± 12.9) (P = .720, P = .418, and P = .280). There were no statistically significant differences for SANE scores at any time points (Figure 2). Additionally the changes from baseline at 1 and 2 years were not statistically significant between nonsmokers and smokers with regard to KOOS ADL (P = .352 and P = .461) or SANE (P = .849 and P = .714) (Table 2).
Figure 2.
Mean function-related patient reported outcome scores comparing nonsmokers and smokers across study time points (baseline indicates preoperative time point). ∗Significant differences between nonsmokers and smokers.
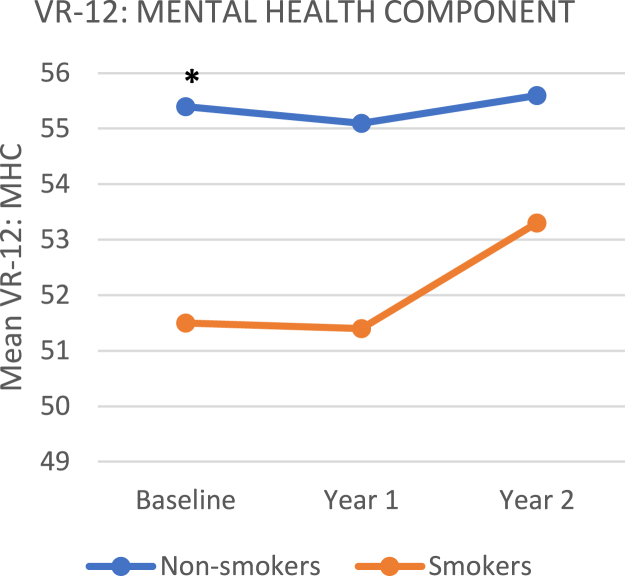
Overall Mental Health Score
Patient-reported mental health was assessed using the Mental Health Component (MHC) of the VR-12. After adjusting for worker’s compensation status, statistically significant differences were measured at baseline between nonsmokers (55.4 ± 0.8) and smokers (51.5 ± 3.3, P = .0199) for mental health (Figure 3).
Figure 3.
Mean mental health–related patient reported outcome scores comparing nonsmokers and smokers across study time points (baseline indicates preoperative time point). ∗Significant differences between nonsmokers and smokers.
Discussion
The most important finding of this study was that active smokers had significantly lower baseline and postoperative PROMs compared with nonsmokers. Active smokers were more likely to have significantly lower baseline mental health, as assessed by the VR-12 questionnaire. Smokers were also more likely to have statistically lower scores for knee pain, symptoms, and function as assessed by the KOOS and WOMAC questionnaires. The KOOS questionnaire showed there were statistically significant changes in knee function from baseline to 1 and 2 years after surgery. Importantly, smokers never reached the same postoperative outcome levels as nonsmokers with regard to knee pain, symptoms, or overall function. Given the significant health risks and poorer PROMs for smokers, surgeons should consider counseling smoking cessation before and after meniscectomy.
Overall, changes from baseline for smokers and nonsmokers were relatively consistent between the groups, given the absence of statistically significant changes from baseline at 1 and 2 years. These findings are consistent with others in the orthopaedic literature. Halawi et al.18 retrospectively reviewed 713 primary total hip and knee replacements with a minimum follow-up of 1 year. The authors showed that smoking status negatively affected baseline patient-reported outcomes, but that changes from baseline were relatively consistent between both groups before adjusting for baseline differences.18 Additionally, Bessette et al.19 queried 638 patients undergoing knee arthroscopy and found that smoking status had a significant impact on preoperative KOOS and VR-12 scores. In a study by Kowalchuk et al.20 that followed 402 patients undergoing ACL reconstruction, smoking along with obesity and severe chondrosis were the strongest predictors of significantly lower PROMs. Furthermore, the study showed that smokers were less likely to evaluate their knee function following ACL reconstruction as average or above average compared with nonsmokers.
Many previous studies have demonstrated that smoking is associated with significantly worse clinical outcomes in surgical procedures. A retrospective review by Blackwell et al.3 included 104 patients undergoing meniscal repair who were evenly divided between smokers and nonsmokers. The study found that smokers had a significantly increased risk of meniscal repair failure.3 Additionally, a recent study by Heyer et al.17 found that preoperative smoking was an independent risk factor for postoperative cardiac, renal, wound, pulmonary, and clotting complications after meniscectomy and ACL reconstruction. A systematic review conducted by Singh9 found that, compared with nonsmokers, current and former smokers had a 24% to 32% higher risk for any postoperative complication following total-hip or total-knee arthroplasty. Additionally, the risk of mortality was 62% higher in current smokers after total hip or knee arthroplasty compared with nonsmokers.9 Novikov et al.10 conducted a systematic review that concluded smoking was associated with significantly worse clinical outcome scores and higher complication rates after ACL reconstruction.
Limitations
There are several limitations to this current study, including the small sample size of active smokers. Further, smokers were not stratified by the amount of smoking or number of pack years. A power analysis was not performed, as the data were limited by the number of smokers, resulting in a type II error. The lack of covariable analysis, including type of meniscal tear, chondral lesion if present, degree of osteoarthritis, and mechanical axis, are additional limitations to this study. As with any retrospective review of prospectively collected data, there is the potential for nonresponse bias.
Conclusion
Patients who were active smokers at the time of partial meniscectomy had significantly worse baseline and postoperative PROMs compared with nonsmokers. Changes from baseline 1 and 2 years postoperatively were relatively consistent between the groups. Smokers will improve a relatively similar amount as nonsmokers after partial meniscectomy, but their overall PROM scores are lower.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Clayton R.A.E., Court-Brown C.M. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39:1338–1344. doi: 10.1016/j.injury.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 2.Maak M.D.T.G., Fabricant M.D.P.D., Wickiewicz M.D.T.L. Indications for meniscus repair. Clin J Sports Med. 2012;31:1–14. doi: 10.1016/j.csm.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 3.Blackwell R., Schmitt L.C., Flanigan D.C., Magnussen R.A. Smoking increases the risk of early meniscus repair failure. Knee Surg Sports Traumatol Arthrosc. 2016;24:1540–1543. doi: 10.1007/s00167-016-4002-8. [DOI] [PubMed] [Google Scholar]
- 4.Mezhov V., Teichtahl A.J., Strasser R., Wluka A.E., Cicuttini F.M. Meniscal pathology—The evidence for treatment. Arthritis Res Ther. 2014;16:206. doi: 10.1186/ar4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paxton E.S., Stock M.V., Brophy R.H. Meniscal repair versus partial meniscectomy: A systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27:1275–1288. doi: 10.1016/j.arthro.2011.03.088. [DOI] [PubMed] [Google Scholar]
- 6.Klimkiewicz J.J., Shaffer B. Meniscal surgery 2002 update: Indications and techniques for resection, repair, regeneration, and replacement. Arthroscopy. 2002;18:14–25. doi: 10.1053/jars.2002.36505. [DOI] [PubMed] [Google Scholar]
- 7.Haviv B., Bronak S., Kosashvili Y., Thein R. Which patients are less likely to improve during the first year after arthroscopic partial meniscectomy? A multivariate analysis of 201 patients with prospective follow-up. Knee Surg Sports Traumatol Arthrosc. 2016;24:1427–1431. doi: 10.1007/s00167-015-3590-z. [DOI] [PubMed] [Google Scholar]
- 8.Salata M.J., Gibbs A.E., Sekiya J.K. A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med. 2010;38:1907–1916. doi: 10.1177/0363546510370196. [DOI] [PubMed] [Google Scholar]
- 9.Singh J.A. Review smoking and outcomes after knee and hip arthroplasty: A systematic review. J Rheumatol. 2011;38:1824–1834. doi: 10.3899/jrheum.101221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Novikov D.A., Swensen S.J., Buza J.A., Gidumal R.H., Strauss E.J. The effect of smoking on ACL reconstruction: A systematic review. Phys Sports Med. 2016;44:335–341. doi: 10.1080/00913847.2016.1216239. [DOI] [PubMed] [Google Scholar]
- 11.Carbone S., Gumina S., Arceri V., Campagna V., Fagnani C., Postacchini F. The impact of preoperative smoking habit on rotator cuff tear: Cigarette smoking influences rotator cuff tear sizes. J Shoulder Elbow Surg. 2012;21:56–60. doi: 10.1016/j.jse.2011.01.039. [DOI] [PubMed] [Google Scholar]
- 12.Uzun E., Misir A., Kizkapan T.B., Ozcamdalli M., Akkurt S., Guney A. Factors affecting the outcomes of arthroscopically repaired traumatic vertical longitudinal medial meniscal tears. Orthop J Sport Med. 2017;5 doi: 10.1177/2325967117712448. 232596711771244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sedgh G., Finer L.B., Bankole A., Eilers M.A., Singh S. Adolescent pregnancy, birth, and abortion rates across countries: Levels and recent trends. J Adolescent Health. 2015;56:223–230. doi: 10.1016/j.jadohealth.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schmid M., Sood A., Campbell L., et al. Impact of smoking on perioperative outcomes after major surgery. Am J Surg. 2015;210:221–229.e6. doi: 10.1016/j.amjsurg.2014.12.045. [DOI] [PubMed] [Google Scholar]
- 15.Singh J.A., Houston T.K., Ponce B.A., et al. Smoking as a risk factor for short-term outcomes following primary total hip and total knee replacement in veterans. Arthritis Care Res. 2011;63:1365–1374. doi: 10.1002/acr.20555. [DOI] [PubMed] [Google Scholar]
- 16.Jones M.H., Spindler K.P. Risk factors for radiographic joint space narrowing and patient reported outcomes of post-traumatic osteoarthritis after ACL reconstruction: Data from the MOON cohort. J Orthop. 2017;35:1366–1374. doi: 10.1002/jor.23557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heyer J.H., Perim D.A., Amdur R.L., Pandarinath R. Impact of smoking on outcomes following knee and shoulder arthroscopy. Eur J Orthop Surg Traumatol. 2020;30:329–336. doi: 10.1007/s00590-019-02577-2. [DOI] [PubMed] [Google Scholar]
- 18.Halawi M.J., Allen D.A., Baron S., Savoy L., Williams V.J., Cote M.P. Tobacco smoking independently predicts lower patient-reported outcomes: New insights on a forgotten epidemic. J Arthroplasty. 2019;34(7 suppl):S144–S147. doi: 10.1016/j.arth.2018.10.036. [DOI] [PubMed] [Google Scholar]
- 19.Bessette M.C., Westermann R.W., Davis A., et al. Predictors of pain and function before knee arthroscopy. Orthop J Sport Med. 2019;7 doi: 10.1177/2325967119844265. 2325967119844265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kowalchuk D.A., Harner C.D., Fu F.H., Irrgang J.J. Prediction of patient-reported outcome after single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25:457–463. doi: 10.1016/j.arthro.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.