Abstract
Objective: Our aim was to explore the effect of multidisciplinary cooperative continuous nursing on the depression, anxiety and quality of life of gastric cancer (GC) patients. Methods: We recruited 128 hospitalized patients with GC in this prospective study. Sixty-four patients were randomly selected in the observation group given conventional continuous nursing care, and 64 patients in the control group given multidisciplinary cooperative continuous nursing care by the random number table. The anxiety status (assessed using self-rating anxiety scale), depression status (self-rating depression scale), quality of life (MOS SF-36 scale), postoperative pain (visual analogue scale), self-care agency (Exercise of Self-Care Agency scale), and nursing satisfaction were compared between the two groups. Results: The scores of pain intensity outside the hospital, and self-rating anxiety and depression scale were significantly lower (all P<0.05), and the dimension scores of both quality of life and self-care agency were markedly higher in the observation group than in the control group (all P<0.05). Besides, the observation group showed better satisfaction with continuous nursing care outside the hospital than the control group (P<0.05). Conclusion: Multidisciplinary cooperative continuous nursing exerts favorable effects in GC patients, and can ameliorate the depression, anxiety, postoperative pain and quality of life, and facilitate the self-care ability and satisfaction of patients. Thus, this nursing model is worthy of being promoted and applied clinically.
Keywords: Multidisciplinary cooperation, continuous care, quality of life, anxiety, depression
Introduction
Gastric cancer (GC) is a malignant tumor arising from the gastric mucosal epithelium with a high incidence in the digestive system [1,2]. Its etiology is complex and closely related to various factors such as Helicobacter pylori infection status, genetic factors, precancerous lesions, as well as living environment and habits [3]. It is reported that the incidence and mortality rate in gastric cancer patients were ranked 5th and 3rd respectively around the world in 2012 [4]. The onset of the disease is insidious. In the early stage, most patients develop no symptoms, and a few may have mild discomforts such as dyspepsia and fullness. By the time of hospital visiting, the discomforts have already progressed to advanced GC with a poor prognosis, seriously threatening the human health [5]. Surgery combined with chemotherapy is the main treatment for GC [6]. However, complications (e.g., gastrointestinal bleeding, pulmonary infection, postoperative depression, postoperative anxiety, and anastomotic leakage) may possibly occur after surgery. Severe physical and mental traumas caused by the decline of physical function can also result in negative emotions such as anxiety, fear and loss, which greatly affect the recovery and quality of life (QoL) of patients [7]. Eliminating or relieving depression and anxiety, and improving the QoL and prognosis of patients have become the focus of postoperative nursing.
Continuous nursing model, an extension of inpatient nursing model, provides medical, nursing, rehabilitation and health guidance services for discharged patients with medical demands, so as to meet their health care, psychological and supportive needs after discharge [8]. As for multidisciplinary cooperative continuous nursing care, multidisciplinary cooperation and continuous nursing are integrated to compensate for the limitations of professional skills and background, and ultimately achieve multiple guarantees. Hence, a comprehensive, all-round, patient-centered diagnosis and treatment plan as well as high-quality nursing service can be provided for discharged patients [9].
Currently, there are few reports on the effect of multidisciplinary cooperative continuous nursing on the depression, anxiety and QoL in GC patients at home and abroad. Therefore, we herein investigated the effect of multidisciplinary cooperative continuous nursing in improving the QoL and negative emotions of GC patients after surgery, and focused on its efficacy on postoperative pain, health behavior, health status and nursing satisfaction, in order to provide theoretical guidance for clinical nursing.
Materials and methods
General data
A prospective study was conducted on 128 GC patients who were hospitalized and underwent surgery in Nanjing Gaochun People’s Hospital from June 25, 2019 to July 30, 2020. The study subjects were randomly divided into the observation group (n=64) and the control group (n=64) by using the random number table method. The general data of the two groups are shown in the results section. This study was approved by the Medical Ethics Committee of Nanjing Gaochun People’s Hospital.
Inclusion criteria: Patients undergoing laparotomy surgery for GC; patients aged >18 years; patients with normal cognitive function; patients who agreed to participate in this study and signed the informed consent.
Exclusion criteria: Patients with major organ dysfunctions and systemic infectious diseases; patients with a history of mental illness or cognitive impairment; patients with other malignant tumors; patients with metastatic or unresectable tumors who could only receive palliative treatment.
Nursing methods
During the in-hospital period, both groups were given the same nursing methods, including prevention of postoperative complication, dietary guidance, disease monitoring, preoperative functional training, and psychological guidance. After discharge, two different continuous nursing programs were performed.
The control group received routine discharge instructions (e.g., precautions after discharge, introduction to possible complications and treatment methods), and telephone follow-ups once a week to understand the existing problems and give guiding opinions.
The control group received multidisciplinary cooperative continuous nursing care, and the specific measures are as follows:
(1) A multidisciplinary cooperative continuous nursing group was established, which was composed of 8 medical workers, including 2 doctors (1 chief physician and 1 attending physician), 1 nutritionist, 1 pharmacist, 1 psychological counselor, 1 head nurse and 2 nurses in charge.
(2) Specific measures: 1) Distribution of nursing services: The doctors were responsible for solving the surgery- and disease-related problems like postoperative wound redness and swelling; the nutritionist was responsible for formulating the dietary prescription; the pharmacist was responsible for making the medication plan after discharge; the psychological counselor was responsible for relieving psychological problems of the patients and their family members; the head nurse was responsible for coordinating and arranging the work of group members to ensure the work progress and quality; the nurses in charge were responsible for self-care guidance, health education and follow-up file establishment. 2) The multidisciplinary cooperative continuous nursing plans were formulated and completed as scheduled. 3) The patients’ general data were collected to establish continuous nursing files. 4) The WeChat group was established for communication. The patients and their family members participated in the group via scanning the code and shared knowledge on the medication for treating GC, rehabilitation, diet and self-care skills every day, and the doctors gave professional replies to consultations. 5) Telephone follow-up: The telephone follow-up was performed every 3 days according to the plan and relevant information was recorded. 6) Home visit: Face-to-face communications were made once a month based on the WeChat communications, telephone follow-ups and individual characteristics. During the process, scientific and reasonable guidances were given, including dietary guidance, medication guidance, pain control and mental health guidance, and introducing self-care knowledge, reexamination time, observation and treatment of postoperative complications, behavioral habits, and social behaviors. 7) Health education lectures for GC patients were held regularly in Nanjing Gaochun People’s Hospital, and the patients and their families were encouraged to be involved in obtaining stronger support.
(3) Effect evaluation: The effects of nursing intervention were evaluated weekly and the intervention plans were adjusted accordingly.
Outcome measures
Main outcomes
Pain intensity: The pain intensity at 7 days after discharge in both groups was quantified, using the visual analogue scale (VAS) [10]. The patients were asked to mark their pain sensation on the horizontal line and the position is then measured and coded from 0= no pain to 10= severe pain.
Anxiety status
The anxiety status at 3 months after discharge was compared between the two groups, using the self-rating anxiety scale (SAS) [11]. The SAS scores ≥50 indicated the presence of anxious symptoms with higher scores revealing more severe symptoms.
Depression status
The depression status at 3 months after discharge was compared between the two groups, using the self-rating depression scale (SDS) [12]. Higher scores indicate more severe depression (mild depression: 53~62 points, moderate depression: 63~72 points, severe depression: >72 points).
QoL: The QoL at 3 months after discharge was compared between the two groups, using the Medical Outcome Study (MOS) 36-item Short Form (SF-36), which includes five dimensions, namely, physical function, general health, social function, role-emotional, and mental health. The total score is 100 points in each dimension, with higher scores suggesting better QoL [13].
Secondary outcomes
Self-care agency
The self-care ability at 3 months after discharge in both groups was evaluated, using the Exercise of Self-Care Agency (ESCA) scale, which incorporates 4 dimensions: self-care skills, self-concept, self-responsibility, and health knowledge level. Higher scores indicate better self-care ability [14].
Nursing satisfaction
The self-made satisfaction scale was filled out by the patients at 3 months after discharge to assess the satisfaction with care, which was categorized into three levels: satisfied (90~100 points), basically satisfied (60~89 points), and dissatisfied (<60 points). Satisfaction rate = (satisfied cases + basically satisfied cases)/total number of cases × 100%.
Statistical analysis
All statistical analysis was performed using the SPSS 20.0. Chi-square test (χ2 test) was applied for the comparison of enumeration data expressed as case/percentages (n/%). The measurement data with normal distribution were expressed as mean ± standard deviation (x̅ ± sd), and independent t-test was adopted for the comparison between the two groups. Besides, the rank-sum test was used for the comparison of ranked data between the two groups. P values were judged significant if they were less than 0.05.
Results
Comparison of baseline data
As is shown in Table 1, there was no significant difference in the age, disease course, sex, tumor, node, metastasis staging, comorbidity, pathological type, etc. between the two groups, suggesting that the two groups were comparable (P>0.05).
Table 1.
Comparison of baseline data (n/%, x̅ ± sd)
| Index | Observation group (n=64) | Control group (n=64) | χ2/t | P |
|---|---|---|---|---|
| Age (year) | 61.4±3.1 | 60.6±3.8 | 1.305 | 0.194 |
| Disease course (year) | 2.61±0.35 | 2.50±0.33 | 1.829 | 0.070 |
| Sex | 0.127 | 0.721 | ||
| Male | 37 | 35 | ||
| Female | 27 | 29 | ||
| TNM staging | 0.129 | 0.937 | ||
| II | 12 | 11 | ||
| III | 34 | 36 | ||
| IV | 18 | 17 | ||
| Comorbidity | ||||
| Hypertension | 9 | 10 | 0.061 | 0.803 |
| Coronary heart disease | 8 | 8 | 0.000 | 1.000 |
| Diabetes mellitus | 6 | 7 | 0.086 | 0.769 |
| Pathological type | 0.151 | 0.927 | ||
| Tubular adenocarcinoma | 13 | 12 | ||
| Mucinous adenocarcinoma | 23 | 25 | ||
| Medullary carcinoma | 18 | 17 |
Note: TNM: tumor, node, metastasis.
Comparison of postoperative pain
The VAS score in the observation group was significantly lower than that in the control group (3.40±0.80 vs. 4.65±0.56, t=10.240, P<0.001). See Figure 1.
Figure 1.
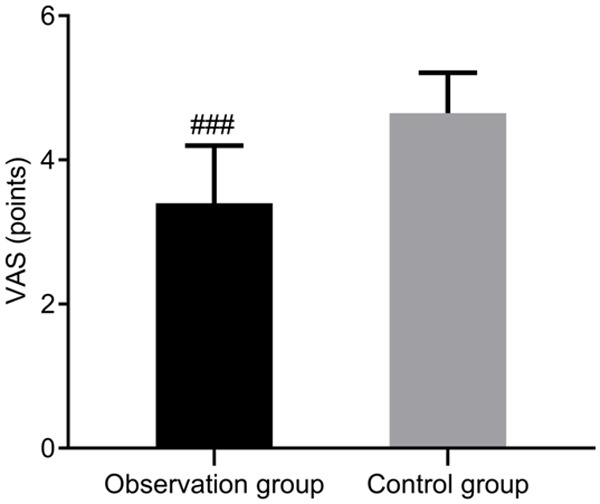
Comparison of VAS score. Compared with the control group, ###P<0.001. VAS: visual analogue scale.
Comparison of anxiety status
The SAS score in the observation group was markedly lower than that in the control group (47.14±5.40 vs. 51.13±5.09, t=4.301, P<0.001). See Figure 2.
Figure 2.
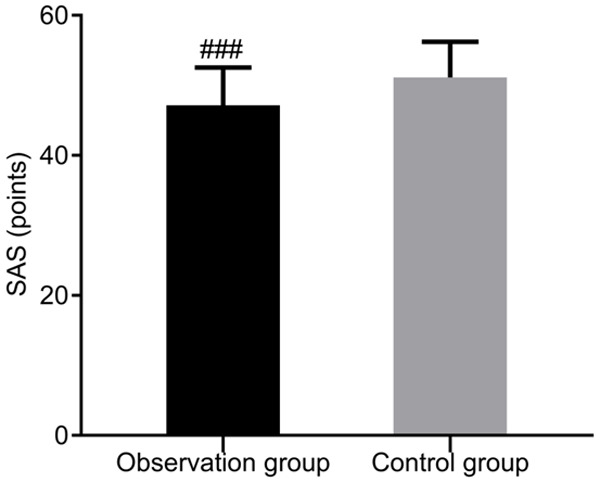
Comparison of SAS score. Compared with the control group, ###P<0.001. SAS: self-rating anxiety scale.
Comparison of depression status
The SDS score in the observation group was much lower than that in the control group (47.95±5.57 vs. 53.96±5.95, t=5.899, P<0.001). See Figure 3.
Figure 3.
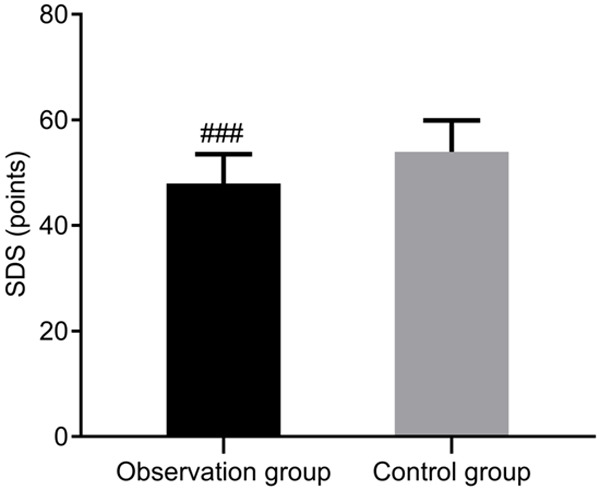
Comparison of SDS score. Compared with the control group, ###P<0.001. SDS: self-rating depression scale.
Comparison of QoL
The observation group showed significantly higher scores in terms of physical function, general health, social function, role-emotional, and mental health than the control group (all P<0.05). See Table 2.
Table 2.
Comparison of MOS SF-36 score (points, x̅ ± sd)
| Dimension | Observation group (n=57) | Control group (n=57) | t | P |
|---|---|---|---|---|
| Physical function | 78.18±10.24 | 65.88±9.20 | 7.148 | 0.000 |
| General health | 91.64±10.26 | 85.06±12.10 | 3.318 | 0.001 |
| Social function | 72.32±11.25 | 65.85±10.30 | 3.393 | 0.001 |
| Role-emotional | 63.83±9.20 | 55.56±7.31 | 5.630 | 0.000 |
| Mental health | 68.51±10.19 | 57.40±7.02 | 7.183 | 0.000 |
Note: MOS SF-36: medical outcome study 36-item short form.
Comparison of Self-care agency
As shown in Table 3, the observation group had much higher scores regarding self-care skills, self-concept, self-responsibility, and health knowledge level than the control group (all P<0.001).
Table 3.
Comparison of ESCA scale scores (points, x̅ ± sd)
| Dimension | Observation group (n=64) | Control group (n=64) | t | P |
|---|---|---|---|---|
| Self-care skills | 38.18±2.24 | 29.88±4.20 | 13.950 | 0.000 |
| Self-concept | 25.64±1.26 | 21.06±2.10 | 14.961 | 0.000 |
| Self-responsibility | 20.32±2.25 | 17.85±2.30 | 6.141 | 0.000 |
| Health knowledge level | 70.83±2.20 | 55.56±2.31 | 38.295 | 0.000 |
Note: ESCA: exercise of self-care agency.
Comparison of nursing satisfaction
In the observation group, 33 patients were satisfied with the continuous nursing, 26 were basically satisfied and 5 were dissatisfied, with the satisfaction rate of 92.19%. In the control group, 26 patients were satisfied with the continuous nursing, 25 were basically satisfied and 13 were dissatisfied, with the satisfaction rate of 79.69%. The observation group had a significantly higher satisfaction rate than the control group (P<0.05). See Table 4.
Table 4.
Comparison of Nursing satisfaction (n, %)
| Group | Satisfied | Basically satisfied | Dissatisfied | Satisfaction rate |
|---|---|---|---|---|
| Observation group (n=64) | 33 (51.56) | 26 (40.63) | 5 (7.81) | 59 (92.19) |
| Control group (n=64) | 26 (40.63) | 25 (39.06) | 13 (20.31) | 51 (79.69) |
| χ2 | 4.137 | |||
| P | 0.042 | |||
Discussion
In 2003, the concept of continuous care was formally and clearly defined by the American Geriatrics Society after being put forward by the study of the joint commission in 1947 [15,16]. Since continuous health care for discharged patients in the recovery period promotes rehabilitation and reduces needs for rehospitalization caused by deterioration of the condition, and decreases consumption of health service costs, continuous nursing care is widely used in clinical practice. In particular, postoperative nursing care for chronic and surgical diseases outside the hospital can achieve good results and improve the prognosis and nursing quality of patients [17,18]. Multidisciplinary cooperative continuous nursing is a model that combines multidisciplinary cooperation with continuous nursing. Since its establishment, the nursing model has made rapid development, been widely used in medical nursing, and achieved favorable practical results [19,20].
Pain is a subjective feeling of patients, and different individuals have different degrees of pain even with the same injury. Pain of advanced cancer is a common symptom in cancer patients, and the intensity is closely related to the individual psychological status. If the pain cannot be controlled in time, it may bring physical and psychological distress to the patients, and even result in postoperative adverse reactions and poor recovery [21]. Yan et al. divided 108 patients with multiple myeloma into the observation group given multidisciplinary cooperative continuous nursing model, and the control group given routine oral and written discharge instructions [22]. The results indicate that multidisciplinary cooperative continuous nursing model can be applied for bone pain relief. In our study, the VAS score was much lower in the observation group than in the control group, suggesting that the multidisciplinary cooperative continuous nursing can effectively alleviate the pain of the patients and facilitate the recovery, which was consistent with the above study. This may be due to the fact that in the continuous nursing process, patients are instructed to reduce the pain through WeChat group, home visit, and other methods (patient accompany, soothing music listening, TV watching, game playing, etc.). By this way, the patients’ attention is shifted, and they are encouraged to release the discomfort caused by the pain, and guided to master the mobility skills postoperatively, in order to promote intestinal peristalsis recovery, prevent intestinal adhesions, and ameliorate the pain resulting from flatulence.
Anxiety and depression are the most common psychological stress reactions in cancer patients. Anxiety, depression and pain are closely associated. The more severe the negative emotion, the lower the pain threshold. Zhang et al. enrolled 105 patients with breast cancer and classified them into the control group receiving routine discharge instructions, and the observation group receiving multidisciplinary cooperative continuous nursing care [23]. The results showed that the SAS and SDS scores were significantly lower in the observation group than in the control group, demonstrating that the multidisciplinary cooperative continuous nursing model could reduce the anxiety of patients. This may be because health education, psychological counseling, dietary guidance, etc. can ameliorate the negative emotions of patients by conducting the multidisciplinary continuous nursing methods such as WeChat, telephone, and face-to-face counseling.
Multidisciplinary cooperative continuous care model is essential for improving patients’ self-care ability and QoL. Wang et al. randomly divided 100 patients undergoing liver cancer surgery into the observation group and the control group [24]. The control group was given routine discharge instructions, while the observation group was given multidisciplinary cooperative continuous nursing measures. The results revealed that multidisciplinary cooperative continuous nursing was beneficial to facilitate the self-care ability and QoL. In our study, the self-care ability of the two groups was assessed by the ESCA scale. The scores of self-care skills, self-concept, self-care responsibility, and health knowledge level were significantly higher in the observation group than in the control group, suggesting that the patients had better self-care ability, which was consistent with the above study. Moreover, the scores of all dimensions of QoL in the observation group were higher than those in the control group, indicating that the QoL in the observation group was better than that in the control group. This may be due to the fact that multidisciplinary cooperative continuous nursing strengthened self-care ability, helps alleviate the pain, reduce the anxiety and depression of the patients, and thereby enhance the QoL of patients. Also, the results reconfirmed the advantages of multidisciplinary cooperative continuous nursing, which was in line with the above study.
Furthermore, our study identified that the satisfaction rate in the observation group was significantly higher than that in the control group, which may be because the multidisciplinary cooperative continuous nursing model can reduce the pain and anxiety, improve the nursing ability, QoL and prognosis of patients, and thus provide a better subjective experience for patients who seek for medical treatment. However, some limitations still exist in this study, e.g., the relapse situation after discharge and the incidence of complications were not observed. Therefore, studies with larger sample sizes and long-term assessment for nursing effect should be performed in the future to consolidate the feasibility and importance of multidisciplinary cooperative continuous nursing model in GC patients.
In summary, multidisciplinary cooperative continuous nursing in GC patients exerts a better effect, which can improve the depression, anxiety, postoperative pain and quality of life of patients as well as the self-care ability and satisfaction of patients. It is therefore worth of clinical promotion and application.
Disclosure of conflict of interest
None.
References
- 1.Spolverato G, Pawlik TM. Clinicopathological evaluation of recurrence in early gastric cancer. Am J Surg. 2019;157:202–207. [Google Scholar]
- 2.Bai T, Yokobori T, Altan B, Ide M, Mochiki E, Yanai M, Kimura A, Kogure N, Yanoma T, Suzuki M, Bao P, Kaira K, Asao T, Katayama A, Handa T, Gombodorj N, Nishiyama M, Oyama T, Ogata K, Kuwano H. High STMN1 level is associated with chemo-resistance and poor prognosis in gastric cancer patients. Br J Cancer. 2017;116:1177–1185. doi: 10.1038/bjc.2017.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fan JH, Wang JB, Wang SM, Abnet CC, Qiao YL, Taylor PR. Body mass index and risk of gastric cancer: a 30-year follow-up study in the Linxian general population trial cohort. Cancer Sci. 2017;108:1667–1672. doi: 10.1111/cas.13292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song Z, Wu Y, Yang J, Yang D, Fang X. Progress in the treatment of advanced gastric cancer. Tumour Biol. 2017;39:1010428317714626. doi: 10.1177/1010428317714626. [DOI] [PubMed] [Google Scholar]
- 5.Hu M, Qian C, Hu Z, Fei B, Zhou H. Biomarkers in tumor microenvironment? Upregulation of fibroblast activation protein-α correlates with gastric cancer progression and poor prognosis. OMICS. 2017;21:38–44. doi: 10.1089/omi.2016.0159. [DOI] [PubMed] [Google Scholar]
- 6.Yonemura Y, Fujimura T, Fushida S, Takegawa S, Kamata T, Katayama K, Kosaka T, Yamaguchi A, Miwa K, Miyazaki I. Hyperthermo-chemotherapy combined with cytoreductive surgery for the treatment of gastric cancer with peritoneal dissemination. World J Surg. 1991;15:530–535. doi: 10.1007/BF01675656. discussion 535-536. [DOI] [PubMed] [Google Scholar]
- 7.Hu X, Zhang C. Diagnosis and risk assessment of postoperative complications of gastric cancer in Japan and Korea. Zhonghua Wei Chang Wai Ke Za Zhi. 2017;20:129–134. [PubMed] [Google Scholar]
- 8.Razmjoee N, Ebadi A, Asadi-Lari M, Hosseini M. Does a “continuous care model” affect the quality of life of patients undergoing coronary artery bypass grafting? J Vasc Nurs. 2017;35:21–26. doi: 10.1016/j.jvn.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Xia YM, Wang J, Li JF. The effect of MDT continuous nursing on negative emotion, self-care ability and complications of rectal cancer patients undergoing stoma surgery. Int J Nurs Stud. 2020;39:2893–2897. [Google Scholar]
- 10.Maxwell C. Sensitivity and accuracy of the visual analogue scale: a psycho-physical classroom experiment. Dept. of Superintendence of the National Education Association of the United States; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry. 2017;17:329. doi: 10.1186/s12888-017-1489-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sepehry AA. In: Zung self-rating depression scale. Sepehry AA, editor. New York: Springer; 2011. [Google Scholar]
- 13.Vitorino D, Martins F, Souza A, Galdino D, Prado G. Utilizao do SF-36 em ensaios clínicos envolvendo pacientes fibromiálgicos: determinao de critérios mínimos de melhora clínica. Rev Neuroc. 2019;12:147–151. [Google Scholar]
- 14.Riesch SK, Hauck MR. The exercise of self-care agency: an analysis of construct and discriminant validity. Res Nurs Health. 1988;11:245–255. doi: 10.1002/nur.4770110406. [DOI] [PubMed] [Google Scholar]
- 15.Dong YJ, Shang SM, Mo L, Hou S. Research progress of continuous nursing models abroad. Chin Nurs Manage. 2012;12:22–23. [Google Scholar]
- 16.Qin GR. Current status and development trend of continued nursing care for discharged patients. J Nurs Sci. 2012;27:89–91. [Google Scholar]
- 17.Tian JL, Gong Ye HJ, Liu Y, Zhang S. Current research status of continuing nursing care for patients with chronic diseases. Chin Nurs Manage. 2017;17:108–111. [Google Scholar]
- 18.Ji CH, Guo HL, Xu XY. Investigation of current requirement of transitional care model on surgical patient. Chin J Mod Nurs. 2017;023:2346–2349. [Google Scholar]
- 19.Jiang Q, Ma P. Multidisciplinary cooperative nursing model of environmental pollution in hospitalised patients wards infected by multi-drug resistant bacteria in orthopaedics. J Environ Prot Ecol. 2019;20:1727–1732. [Google Scholar]
- 20.Zhang LY, Ni H, Yu GH, Ding WN, Wang XZ. Application effect of multidisciplinary team cooperation on continuous nursing care of patients with acute coronary syndrome after PCI. Prev Treat Card Cereb Dis. 2018;18:436–438. [Google Scholar]
- 21.Hu XX, Li MQ, Jiang JX. Application progress of multicultural nursing in patients with advanced cancer pain. Chin Cancer Clin Rehabil. 2018;25:509–512. [Google Scholar]
- 22.Yan Y, Geng CY, Zuo LH. Application effect of multidisciplinary cooperation continuation care in patients with multiple myeloma. Chin J Mod Nurs. 2017;23:1843–1847. [Google Scholar]
- 23.Zhang XC, Wang YH, Ge YH, Lu J, Wu X, Chen L. Effects of multidisciplinary cooperative extended care on psychological status and quality of life of breast cancer patients. Chin J Mod Nurs. 2018;24:199–202. [Google Scholar]
- 24.Wang HL, Xu CY, Zhang CP. The application effect of multidisciplinary cooperation model continuous nursing in patients after liver cancer surgery. Nurs Res. 2019;33:114–118. [Google Scholar]


