Abstract
Objective: This study was designed to explore the feasibility and effectiveness of patient-centered care (PCC) on basis of guidelines of Joint Commission on Accreditation of Healthcare Organizations (JCI) in patients with acute subarachnoid hemorrhage (SAH). Methods: A total of 180 SAH patients who received treatment in our hospital were selected as prospective research objects, and were divided into a study group (n=90) and a control group (n=90) by convenience sampling. Patients in the control group received conventional SAH-targeted care, and patients in the study group were additionally nursed with PCC on the basis of conventional SAH-targeted care. The general indicators, including Mini-Mental State Exam (MMSE) scores before and after intervention, activities of daily living (ADL), mental state, general self-efficacy scale (GSES), health knowledge, and incidence of complications were compared between the two groups. Results: The length of hospital stay, the time in bed, and the expenses of hospitalization in the study group were lower than those of the control group (P<0.05). The scores of MMSE, ADL, GSES, and health knowledge in the study group were higher than those in the control group (P<0.05), and the scores of each dimension of Symptom Checklist-90 (SCL-90) and the incidence of complications in the study group were lower than those in the control group (P<0.05). Conclusion: PCC for SAH patients based on the guidelines of JCI can not only improve the outcomes, cognitive function, self-efficacy, negative emotions and ADL of patients, but also help enhance their awareness of the disease and reduce the incidence of complications.
Keywords: Acute subarachnoid hemorrhage, patient-centered care, JCI, nursing, efficacy evaluation
Introduction
At present, the incidence rate of cerebrovascular diseases is on the rise, posing a major threat to human health. Cerebrovascular diseases are now the three most fatal diseases of human beings in addition to malignant tumors and coronary heart disease [1]. Subarachnoid hemorrhage (SAH) is a clinical syndrome caused by bleeding within the subarachnoid space. Its incidence rate accounts for 10% of cerebral stroke, and it is a common and critical hemorrhagic cerebrovascular disease in neurosurgery [2,3]. According to epidemiological investigations, the incidence rate of SAH in China is about 2 per 100,000, and the number of new cases can reach about 100,000 every year. Due to its acute onset, critical condition, and rapid progression, its mortality rate ranges from 22%-25%. Even with timely and effective treatment, most patients still need long-term care [4,5].
Many clinical studies have explored nursing methods for SAH patients. However, the traditional disease-centered model fails to meet the patients’ expectations [6]. The patient-centered care (PCC) on basis of guidelines of JCI is an emerging intervention concept and also a globally recognized medical service standard, which represents the highest level of hospital service and management. This concept is patient-centered, so it combines the hospital’s expertise flexibly to establish a targeted nursing model, achieving good results in practical applications [7]. A retrospective analysis of 100 SAH patients showed that PCC based on core concepts of JCI could effectively reduce the complication rate of SAH patients, improve their quality of life, and play a positive role in building a harmonious doctor-patient relationship [8]. It has also been found that SAH patients often experience negative emotion and aggravation of anxiety and depression due to a sudden onset of serious illness. The JCI concept can carry out targeted psychological interventions for patients and significantly alleviate the anxiety and depression of patients, which is of positive significance for clinical treatment [9].
The above results are the theoretical basis of this study. This study was designed to explore the feasibility and effectiveness of applying PCC based on core concepts of JCI in SAH patients, so as to provide theoretical references for improving their prognosis and quality of life.
Materials and methods
General materials
A total of 180 SAH patients admitted to our hospital from January 2019 to December 2019 were selected as the research objects, and were divided into a study group (n=90) and a control group (n=90) by convenience sampling.
Inclusion criteria: (1) All patients were clinically diagnosed with SAH [10] and presented with corresponding clinical symptoms; (2) The patients ranged in age from 18 to 70 years; (3) The survey was implemented with the approval of the Medical Ethics Committee; (4) The family members of the patents signed an informed consent.
Exclusion criteria: (1) Patients with mental illness; (2) Patients with open craniocerebral injury; (3) Patients with hemorrhage caused by craniocerebral tumor; (4) Patients with previous history of traumatic brain injury; (5) Patients with complications of endocrine disease, blood system disease, or severe liver and kidney dysfunction; (6) Pregnant or lactating women.
Rejection criteria: (1) Patients who lost follow-up during the survey; (2) Patients who voluntarily requested suspension or withdrawal during the survey.
Intervention methods
Patients in the two groups received the same treatment after admission, such as anti-infection, intracranial pressure reduction, medicines that nourished the nervous system, hemostasis, etc. Patients in the control group received routine interventions, such as taking medication as prescribed by doctors, nursing care of drainage tube, health education, etc., while on the basis of routine interventions, patients in the study group were additionally nursed with PCC as follows: (1) Checking the record, determining the difficulties in nursing of SAH and common complications of SAH patients, listing the cases and analyzing the causes one by one; (2) Analyzing the reasons for the high incidence of complications and poor prognosis in SAH patients according to literature review: (l) Insufficient attention was paid to psychological intervention. SAH patients are critically ill and progress rapidly. Most patients have obvious worries, anxiety, and depression. Traditional nursing often focuses on how to improve the condition, ignoring the patient’s feelings, leading to frequent adverse emotions; (ll) The posture exercise time was late. The patients under the traditional nursing started posture exercise time late, resulting in a significant decline in the patient’s extremity function; (lll) Less pain intervention. Pain is a common postoperative complication of SAH patients. If not taken seriously, it may affect the patient’s compliance and treatment effect; (3) Carrying out targeted nursing intervention: (l) Increasing the proportion of psychological intervention. Nursing staffs should pay attention to the psychological state of the patient, and fully consider their actual situation, family status, and social status, to carry out appropriate psychological counseling. They should ask the relatives of the patient to accompany and communicate with the patient to give them confidence in the treatment. (ll) Posture intervention should be carried out as soon as possible. According to the actual condition, the patients should carry out early physical rehabilitation exercises starting with passive and progressing to active, and getting on-bed to off-bed to restore the patients’ self-care ability as soon as possible. (lll) Carrying out appropriate pain intervention. Nursing staffs should pay attention to the patients’ pain nursing, which can reduce their pain and improve their treatment compliance by taking medication, and diverting attention; (lV) Carrying out complication-oriented nursing. Nursing staffs should combine common types of complications to carry out targeted nursing interventions, such as to aspirate sputum, replace the ventilator tubing, keep the vulva clean in a timely manner, and flush the bladder regularly. The two groups of patients underwent intervention for 30 days, and the family members of the patients or community medical institutions carried out continuous intervention after discharge.
Observation indicators and evaluation standards
Differences in general clinical treatment indicators after intervention
The duty nurses recorded the general clinical treatment indicators of the two groups, such as length of hospital stay, the time in bed, expenses of hospitalization, etc., and the differences between the groups were compared.
Analysis of cognitive function and activities of daily living (ADL) before and after intervention
The cognitive function and ADL of the patients in the two groups were evaluated before and after intervention. The Mini-Mental State Exam (MMSE) scale was selected for the evaluation of cognitive function, which is a common tool for clinical psychology testing and treatment, and can quickly reflect the degree of cognitive function impairment of subjects. The scale includes 30 items in 7 aspects, with a total score ranging from 0 to 30 points. A higher score indicates a lighter cognitive function impairment of the subjects [11]. The ADL scale was selected for the evaluation of ADL. The scale includes 10 items such as dining, bathing, dressing, and walking on the ground. The total score of the scale is the sum of the scores of each item, a higher score indicates a better independent living ability of the subjects [12].
Psychological analysis before and after intervention
The psychological states of the patients in the two groups were evaluated before and after intervention using SCL-90, which includes 90 items with a total of 9 sub-scales. The scale can evaluate subjects’ somatization, obsessive-compulsive symptoms, interpersonal relationships, depression, anxiety, hostility, phobia, paranoia, and psychosis. In this study, four sub-scales of somatization, depression, anxiety, and phobia were adopted as observation indicators [13].
Analysis of the score of self-efficacy and health knowledge before and after intervention
The self-efficacy of patients in the two groups was evaluated before intervention and at 30 days after intervention. General self-efficacy scale (GSES) was chosen for self-efficacy evaluation. The scale includes a total of 10 items, using the 1-4 grade scoring method. The total score of the scale is divided into the sum of the scores of each item, and a higher score indicates a better self-efficacy of the subject. The score of health knowledge was evaluated using a self-made scale in the hospital and was only evaluated at 30 days after intervention. The total score of the scale is 100 points. A higher score indicates a better knowledge of health of the subjects [14].
Comparison of the incidence of complications during the intervention
The incidence of various complications such as pulmonary infection, pressure ulcers, constipation, rebleeding, and urinary system infection during the intervention of the two groups were recorded, and differences between the two groups were compared.
Statistical method
Collected data were entered into EXCEL. The statistical analysis of data was processed by SPSS 22.0, and normal distribution test was carried out on the collected data. If the data conformed to a normal distribution, the counting data were expressed as [n (%)]. The Chi-square test was employed for intergroup comparisons. The measurement data were expressed as mean ± standard deviation. The t-test was used for intergroup comparisons. The graphic software used in this study was GraphPad Prism 8. P<0.05 was considered significant [15].
Results
Differences in general clinical data between the two groups
After analysis and comparison, there was little difference in general clinical data such as gender, age, average weight, cause of disease, education level, family income, etc. between the two groups (P>0.05), which were comparable (Table 1).
Table 1.
General clinical indicators in the two groups (x̅ ± s)/[n (%)]
| General clinical indicator | Study group (n=90) | Control group (n=90) | t/X2 | P | |
|---|---|---|---|---|---|
| Gender | Male | 61 | 46 | 1.883 | 0.17 |
| Female | 39 | 44 | |||
| Average age (years) | 38.29±2.33 | 38.34±2.41 | 0.142 | 0.887 | |
| Average weight (kg) | 63.29±4.11 | 64.19±3.98 | 1.492 | 0.137 | |
| Educational background | Bachelor’s or above | 30 | 32 | 1.228 | 0.231 |
| High school | 43 | 43 | |||
| Junior high school or below | 13 | 15 | |||
| Monthly income | <1000 CNY | 19 | 13 | 1.471 | 0.136 |
| 1000-5000 CNY | 31 | 30 | |||
| 5000 CNY and above | 40 | 43 | |||
| Cause of illness | Traffic accident | 34 | 30 | 0.819 | 0.345 |
| Fall from height | 43 | 35 | |||
| Fall accident | 10 | 20 | |||
| Others | 3 | 5 | |||
Differences in general clinical treatment indicators after intervention
The length of hospital stay, time spent in bed, and the expense of hospitalization in the study group were significantly shorter and lower than those in the control group, showing significant differences between the two groups (P<0.05) (Figure 1).
Figure 1.

Comparison of differences in general clinical treatment indicators between the two groups. The length of hospital stay, time in bed, and the expenses of hospitalization in the study group were significantly lower than those in the control group (P<0.05); # represents a significant difference between groups at the same indicator (P<0.05).
Analysis of cognitive function and ADL before and after intervention
There was no significant difference in scores of the MMSE and ADL scales of patients in the two groups before intervention (P>0.05). At 30 days after intervention, the scores of the MMSE and ADL scales in the study group were significantly higher than those in the control group (P<0.05). At the same time, the MMSE and ADL scores of the two the groups after intervention were significantly increased compared with those before intervention (P<0.05) (Figure 2).
Figure 2.

Differences in cognitive function and ADL of the two groups before and after intervention. After intervention, the MMSE and ADL scores of the study group were significantly higher than before intervention, compared to those of the control group, (P<0.05); the changes of the MMSE and ADL scores in the two groups before and after intervention showed that the changes in the MMSE and ADL scores in the study group were significantly larger than those in the control group (P<0.05); # represents statistically significant difference of the same indicator compared with the control group (P<0.05).
Psychological analysis before and after intervention
There was little difference in SCL-90 scale scores between the two groups before intervention (P>0.05). After intervention, the scores of the four sub-scales of somatization, depression, anxiety, and phobia in the study group were significantly lower than those in the control group, exhibiting significant differences between the two groups (P<0.05) (Figure 3).
Figure 3.
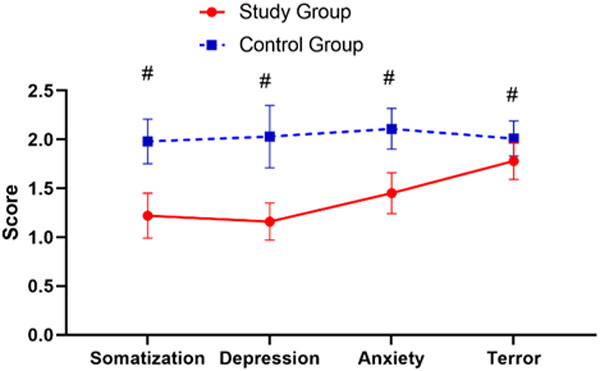
Analysis of the psychological states of the two groups after intervention. The scores of somatization, depression, anxiety, and phobia in the SCL-90 subscales of the study group patients were significantly lower than those of the control group at 30 days after intervention (P<0.05); # represents a significant difference between groups in the same indicator (P<0.05).
Analysis of the score of self-efficacy and health knowledge before and after intervention
There was little difference in GSES scores between the two groups before intervention (P>0.05). After intervention, the scores of the GSES of the two groups were significantly higher than those before intervention (P<0.05). After intervention, the health knowledge score of the study group was significantly higher than that of the control group (P<0.05) (Figure 4).
Figure 4.

Comparison of self-efficacy and health knowledge scores between the two groups before and after intervention. The GSES scores of the two groups had little difference before intervention, and the GSES scores of the two groups after intervention were significantly higher than those before intervention, and the difference was significant (A) (P<0.05); the health knowledge score of the study group after intervention was significantly higher than that of the control group (B) (P<0.05); # represents significant differences between groups at the indicator and at the same time (P<0.05).
Comparison of the incidence of complications during the intervention
There was 1 case of constipation in the study group during the intervention, and the total incidence of complications was 1.11%. There was 1 case of lung infection, 1 case of pressure ulcer, 3 cases of constipation, 1 case of rebleeding, and 1 case of urinary system infection in the control group during the intervention, and the total incidence of complications was 7.78%. The difference between the groups was significant (P<0.05) (Table 2).
Table 2.
Comparison of the incidence of complications during the intervention between the two groups [n (%)]
| Groups | n | Pulmonary infection | Pressure ulcer | Constipation | Rebleeding | Urinary system infection | Total incidence |
|---|---|---|---|---|---|---|---|
| Study group | 90 | 0 (0.00) | 0 (0.00) | 1 (1.11) | 0 (0.00) | 0 (0.00) | 1 (1.11) |
| Control group | 90 | 1 (1.11) | 1 (1.11) | 3 (3.33) | 1 (1.11) | 2 (2.22) | 7 (7.78) |
| X2 | - | - | - | - | - | - | 4.709 |
| P | - | - | - | - | - | - | 0.03 |
Discussion
Acute subarachnoid hemorrhage (SAH) is a general term for diseases in which blood flows into the subarachnoid space due to the rupture of cerebral blood vessels caused by various reasons. The typical clinical symptoms are nausea and vomiting, severe headache, unconsciousness, and convulsions. The disease is severe, progresses rapidly, and has poor prognosis. It is clinically advocated to carry out intervention as soon as possible to improve the quality of life of patients and reduce the incidence of neurologic deficits [16].
At present, the treatment principles of SAH are relatively standardized, mainly include timely hemostasis, infection prevention, and water and electrolyte balance adjustment. Although the principles of treatment have been established, clinical practice has found that some SAH patients still have poor prognosis. The reason may be related to the improper nursing intervention of the patients [17]. A survey has pointed out that the traditional nursing model advocates the condition as the center, and all nursing activities are based on the principle of improving the patients’ condition, which lacks humanity, is not conducive to improving patients’ unhealthy emotional state, and has poor practical application effects for patients with anxiety and depression [18]. Another survey of 176 SAH patients found that 43.18% of SAH patients scored higher on the anxiety and depression scale than the domestic norm, and the interview results showed that most patients were very worried about their own illness, had obvious fears, and desired to get care and help from others [19]. A survey from some scholars has pointed out that traditional SAH nursing is passive nursing, and its effect in preventing complications is not satisfactory; therefore, the initiative of nursing staff in intervention should be appropriately increased to provide prerequisites for improving the prognosis of patients [20].
The patient-centered care (PCC) based on core concepts of JCI is an emerging model of nursing intervention in recent years, which advocates interventions from the perspective of the patient to improve prognosis. The concept is significantly different from that of traditional nursing. A retrospective study of 100 stroke patients showed that the PCC based on concepts of JCI could significantly improve the quality of life of stroke patients and reduce the incidence of adverse cardiovascular events [21]. Another survey found that through training of the core concepts, the comprehensive nursing score of clinical departments had increased by 1.1%, the reporting rate of nursing hidden danger increased by 140%, and the incidence of adverse events decreased by 71.2%, indicating that the PCC based on core concepts of JCI had good practicality and effectiveness [22].
In this study, different groups were set up to analyze the feasibility of applying PCC based on core concepts of JCI for SAH patients. The results showed that patients in the study group with additional PCC of JCI had significantly shorter length of hospital stay and time in bed than those in the control group with routine nursing, indicating that PCC of JCI accelerated the recovery of SAH patients. Some scholars believe that the implementation of targeted nursing for SAH patients can significantly accelerate the treatment process. The reason may be that targeted nursing is more concise and effective. Besides, the comparison of medical expenses between the two groups showed that PCC based on core concepts of JCI not only helped optimize the allocation of medical resources, but also facilitated the development of medical management work [23]. Based on the analysis of cognitive function, life ability, and mental state of the two groups, patients in the study group had lower neurologic deficits, better self-care ability, and less unhealthy emotion after intervention. As mentioned above, unhealthy emotions will have an adverse effect on the treatment of SAH patients. The analysis of some scholars has pointed out that good nursing is an important basis for improving the prognosis of SAH patients. Timely and effective intervention can significantly improve the survival rate. Appropriate nursing can be patient-centered, which promotes the progress of treatment from multiple perspectives, and has significant effects [24]. In this study, it was found that PCC based on core concepts of JCI is actually a kind of team nursing, which can reflect the modern concept of holistic medical care. In the whole intervention process, the management of nursing staff and the implementation of nursing work were well planned, which significantly reduced the difficulty and improved the pertinence of nursing intervention, so as to achieve better implementation results.
The present study also compared the self-efficacy and health knowledge of patients in the two groups. The results showed that the self-efficacy and health knowledge scores of the patients in the study group were significantly higher than those in the control group after intervention, indicating that PCC based on core concepts of JCI could improve patients’ compliance and awareness of treatment. Some scholars have pointed out that self-efficacy is an important manifestation of patients’ subjective initiative in the treatment process. Patients with high self-efficacy are often able to cooperate with medical work actively, and the mastery of health knowledge affects the ability of patients to develop self-care after discharge from the hospital [25]. In this study, patients in the study group had significantly higher self-efficacy and health knowledge after intervention than those in the control group. This is because JCI, at its core, implements the philosophy of being patient-centered. It aims to establish the concept of self-care of patients, cultivate self-care abilities, stimulate the potential of self-care, and enable patients to participate in the nursing process actively, which can lay a good foundation for the development of patients’ nursing work after discharge from the hospital, and also meet the requirements of a new nurse-patient relationship [26]. As for the comparison of the incidence of complications, the authors of this study believe that the PCC based on concepts of JCI is a reverse-derivative intervention, which means to clarify the types of common complications of SAH, and then carry out targeted care. This model helps optimize the utilization of medical resources and improve the efficiency of nursing intervention.
In summary, the PCC based on core concepts of JCI for SAH patients can accelerate patient outcomes, improve the cognitive function, self-efficacy, unhealthy emotion and ADL of patients, and at the same time help improve their awareness of the disease and reduce the incidence of complications. The innovation of this study lies in exploring the feasibility of JCI in the nursing of SAH patients from multiple aspects such as self-efficacy, unhealthy emotion, cognitive function, ADL, and incidence of complications, which provides practical data support for other research. The shortcomings of this study lie in the lack of long-term follow-up of patients and lack of follow-up research on the development of patients’ ability after discharge. In the next step of the study, more detailed research discussions will be carried out with a view to providing references to improve the prognosis of SAH patients.
Disclosure of conflict of interest
None.
References
- 1.Nishikawa H, Suzuki H. Possible role of inflammation and galectin-3 in brain injury after subarachnoid hemorrhage. Brain Sci. 2018;8:30. doi: 10.3390/brainsci8020030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pawlowska E, Szczepanska J, Wisniewski K, Tokarz P, Jaskólski DJ, Blasiak J. NF-κB-mediated inflammation in the pathogenesis of intracranial aneurysm and subarachnoid hemorrhage. Does autophagy play a role? Int J Mol Sci. 2018;19:1245. doi: 10.3390/ijms19041245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coulier B. Pseudo-subarachnoid Hemorrhage. J Belg Soc Radiol. 2018;102:32. doi: 10.5334/jbsr.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu Q, Enkhjargal B, Huang L, Zhang T, Sun C, Xie Z, Wu P, Mo J, Tang J, Xie Z, Zhang JH. Aggf1 attenuates neuroinflammation and BBB disruption via PI3K/Akt/NF-κB pathway after subarachnoid hemorrhage in rats. J Neuroinflammation. 2018;15:178. doi: 10.1186/s12974-018-1211-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pearson TE, Frizzola MA, Priest MA, Rochman MF, Froehlich CD. Pediatric extracorporeal cardiopulmonary resuscitation patient with traumatic subarachnoid hemorrhage and takotsubo syndrome. Air Med J. 2018;37:64–66. doi: 10.1016/j.amj.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Al-Jehani H, Angle M, Marcoux J, Teitelbaum J. Early abnormal transient hyperemic response test can predict delayed ischemic neurologic deficit in subarachnoid hemorrhage. Crit Ultrasound J. 2018;10:1. doi: 10.1186/s13089-017-0079-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Toi H, Matsushita N, Ogawa Y, Kinoshita K, Satoh K, Takai H, Hirai S, Hara K, Matsubara S, Uno M. Utility of indocyanine green video angiography for sylvian fissure dissection in subarachnoid hemorrhage patients - sylvian ICG technique. Neurol Med Chir (Tokyo) 2018;58:85–90. doi: 10.2176/nmc.tn.2017-0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu Y, Zhang XS, Zhang ZH, Zhou XM, Gao YY, Liu GJ, Wang H, Wu LY, Li W, Hang CH. Peroxiredoxin 2 activates microglia by interacting with Toll-like receptor 4 after subarachnoid hemorrhage. J Neuroinflammation. 2018;15:87. doi: 10.1186/s12974-018-1118-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu FY, Cai J, Wang C, Ruan W, Guan GP, Pan HZ, Li JR, Qian C, Chen JS, Wang L, Chen G. Fluoxetine attenuates neuroinflammation in early brain injury after subarachnoid hemorrhage: a possible role for the regulation of TLR4/MyD88/NF-κB signaling pathway. J Neuroinflammation. 2018;15:347. doi: 10.1186/s12974-018-1388-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luo F, Wu L, Zhang Z, Zhu Z, Liu Z, Guo B, Li N, Ju J, Zhou Q, Li S, Yang X, Mak S, Han Y, Sun Y, Wang Y, Zhang G, Zhang Z. The dual-functional memantine nitrate MN-08 alleviates cerebral vasospasm and brain injury in experimental subarachnoid haemorrhage models. Br J Pharmacol. 2019;176:3318–3335. doi: 10.1111/bph.14763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anzabi M, Ardalan M, Iversen NK, Rafati AH, Hansen B, Østergaard L. Hippocampal atrophy following subarachnoid hemorrhage correlates with disruption of astrocyte morphology and capillary coverage by AQP4. Front Cell Neurosci. 2018;12:19. doi: 10.3389/fncel.2018.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miao YF, Peng T, Moody MR, Klegerman ME, Aronowski J, Grotta J, McPherson DD, Kim H, Huang SL. Delivery of xenon-containing echogenic liposomes inhibits early brain injury following subarachnoid hemorrhage. Sci Rep. 2018;8:450. doi: 10.1038/s41598-017-18914-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ido K, Kurogi R, Kurogi A, Nishimura K, Arimura K, Nishimura A, Ren N, Kada A, Matsuo R, Onozuka D, Hagihara A, Takagishi S, Yamagami K, Takegami M, Nohara Y, Nakashima N, Kamouchi M, Date I, Kitazono T, Iihara K. Effect of treatment modality and cerebral vasospasm agent on patient outcomes after aneurysmal subarachnoid hemorrhage in the elderly aged 75 years and older. PLoS One. 2020;15:e0230953. doi: 10.1371/journal.pone.0230953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brawanski N, Kashefiolasl S, Won SY, Tritt S, Berkefeld J, Senft C, Seifert V, Konczalla J. Does aneurysm side influence the infarction side and patients’ outcome after subarachnoid hemorrhage? PLoS One. 2019;14:e0224013. doi: 10.1371/journal.pone.0224013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu L, Su Z, Zha L, Zhu Z, Liu W, Sun Y, Yu P, Wang Y, Zhang G, Zhang Z. Tetramethylpyrazine nitrone reduces oxidative stress to alleviate cerebral vasospasm in experimental subarachnoid hemorrhage models. Neuromolecular Med. 2019;21:262–274. doi: 10.1007/s12017-019-08543-9. [DOI] [PubMed] [Google Scholar]
- 16.Ray B, Tinsley L, Ford L, Thompson DM, Sidorov EV, Bohnstedt BN. Trends of platelet volume index predicts delayed cerebral ischemia after subarachnoid hemorrhage. World Neurosurg. 2018;111:e624–e631. doi: 10.1016/j.wneu.2017.12.131. [DOI] [PubMed] [Google Scholar]
- 17.Chen J, Jin H, Xu H, Peng Y, Jie L, Xu D, Chen L, Li T, Fan L, He P, Ying G, Gu C, Wang C, Wang L, Chen G. The neuroprotective effects of necrostatin-1 on subarachnoid hemorrhage in rats are possibly mediated by preventing blood-brain barrier disruption and RIP3-mediated necroptosis. Cell Transplant. 2019;28:1358–1372. doi: 10.1177/0963689719867285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jang SH, Chang CH, Jung YJ, Kim SH, Seo JP. Optic radiation injury in patients with aneurismal subarachnoid hemorrhage: a preliminary diffusion tensor imaging report. Neural Regen Res. 2018;13:563–566. doi: 10.4103/1673-5374.228763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Engquist H, Rostami E, Enblad P. Temporal dynamics of cerebral blood flow during the acute course of severe subarachnoid hemorrhage studied by bedside xenon-enhanced CT. Neurocrit Care. 2019;30:280–290. doi: 10.1007/s12028-019-00675-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oka F, Chung DY, Suzuki M, Ayata C. Delayed cerebral ischemia after subarachnoid hemorrhage: experimental-clinical disconnect and the unmet need. Neurocrit Care. 2020;32:238–251. doi: 10.1007/s12028-018-0650-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolf S. Autoregulation monitoring is important: even after aneurysmal subarachnoid hemorrhage-isn’t it? Neurocrit Care. 2019;31:245–246. doi: 10.1007/s12028-019-00778-5. [DOI] [PubMed] [Google Scholar]
- 22.Juvela S. Reader response: association between aspirin dose and subarachnoid hemorrhage from saccular aneurysms: a case-control study. Neurology. 2019;92:1024–1025. doi: 10.1212/WNL.0000000000007550. [DOI] [PubMed] [Google Scholar]
- 23.Saand AR. CSF inflammatory and vasoactive mediators associated with poor functional outcome in subarachnoid hemorrhage (SAH) patients. 2019 [Google Scholar]
- 24.Wang G, Yu J. Remote acute subarachnoid hemorrhage after drainage of chronic subdural hematoma: a case report and review of the literature. Int J Surg Case Rep. 2018;44:202–206. doi: 10.1016/j.ijscr.2018.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ma L, Jiang Y, Dong Y, Gao J, Du B, Liu D. Anti-TNF-alpha antibody attenuates subarachnoid hemorrhage-induced apoptosis in the hypothalamus by inhibiting the activation of Erk. Neuropsychiatr Dis Treat. 2018;14:525–536. doi: 10.2147/NDT.S154809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vinas Rios JM, Sanchez-Aguilar M, Kretschmer T, Heinen C, Medina Govea FA, Jose Juan SR, Schmidt T. Predictors of hydrocephalus as a complication of non-traumatic subarachnoid hemorrhage: a retrospective observational cohort study in 107 patients. Patient Saf Surg. 2018;12:13. doi: 10.1186/s13037-018-0160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


