Abstract
Objective: To investigate the effect of a nursing protocol based on the KABP (Knowledge, Attitude, Belief and Practice) model in the cardiac rehabilitation (CR) of patients with acute myocardial infarction (AMI) after percutaneous coronary intervention (PCI). Methods: In this prospective study, a total of 76 patients with AMI who underwent PCI were selected as the research objects. Through random number table, the participants were divided into 41 cases in the KABP group (cardiac rehabilitation nursing based on KABP model) and 35 cases in the control group (conventional rehabilitation nursing). All patients underwent echocardiography within 48 hours after PCI and 3 months after the postoperative follow-up to determine the improvement of their cardiac function. The risk of falling out of bed for 7 days after surgery, the physical improvement and exercise endurance before and after the intervention, as well as the scores of Coronary Artery Disease Self-Management Scale (CSMS) and China Questionnaire of Quality of Life in Patients with Cardiovascular Diseases (CQQC) were compared between the two groups. Results: Within 48 hours after operation, there was no significant difference in the indicators of cardiac function between the two groups (all P>0.05). After 3 months of postoperative follow-up, the improvement of cardiac function of KABP group including left ventricular ejection fraction, stroke volume, and cardiac index were significantly better than those of the control group (all P<0.05), and NYHA class was also significantly better than that of the control group (P<0.001). On the 7th day after operation, the high risk of falling out of bed in the KABP group (17.07%) was significantly lower than that in the control group (74.29%; P<0.001). The metabolic equivalent, 6-minute walk test scores, and CQQC scores of the KABP group were significantly higher than those of the control group (all P<0.01). The total scores of daily life management, disease medical management, emotional cognitive management and self-management in CSMS were significantly higher than those of the control group (all P<0.01). Conclusion: Cardiac rehabilitation care based on the KABP model can improve the recovery of cardiac function of AMI patients after PCI, reduce the risk of falling out of bed, help patients recover their physical status and exercise endurance, and improve their management behavior and postoperative life quality.
Keywords: Nursing model of knowledge, attitude, belief and practice, acute myocardial infarction, percutaneous coronary intervention, cardiac rehabilitation, cardiac function
Introduction
Acute myocardial infarction (AMI) is a common critical cardiac disease caused by acute myocardial ischemia and necrosis due to coronary artery stenosis and occlusion [1]. With quick and obvious curative effects, percutaneous coronary intervention (PCI) technology can significantly increase the vascular recanalization rate of AMI, restore effective myocardial blood perfusion, and reduce its fatality rate, and thus the preferred treatment for AMI patients at present [2]. However, PCI can only temporarily relieve the mechanical stenosis or occlusion of coronary arteries, but not able to eliminate the cause to completely hinder the continued development of atherosclerosis. In addition, the risk of adverse cardiovascular events after PCI is extremely high. Therefore, other interventions need to be supplemented after surgery to consolidate its efficacy [3]. It was confirmed by a previous study that cardiac rehabilitation (CR) training was able to slow down the progression of atherosclerosis, promoted blood circulation, and enhanced the blood and oxygen supply to the heart [4]. At present, the effectiveness of the application of CR in AMI has been clinically confirmed, which can be carried out in stages, with a clear purpose of rehabilitation. It can correct the risk factors related to cardiac rehabilitation, alleviate patients’ symptoms, enhance their physical status, repair or even reverse the lesions, reduce the rate of recurrence and sudden death, and promote patients to resume normal life and return to society as soon as possible, which belongs to the secondary prevention of diseases [5].
Nevertheless, the implementation process of CR is relatively long, so patients still lack compliance during the implementation process. In the current clinical routine cardiac care, about 40% of patients show poor recovery of cardiac function during reexamination, which can then cause pulmonary dysfunction, insufficient exercise endurance, and even affect the patient’s ability to take care of themselves in daily life [6]. It has been reported that the KABP model can guide medical staff to improve patients’ awareness of the disease and establish positive rehabilitation beliefs, so that they can improve self-management behaviors and actively participate in the disease prevention [7]. The conceptual core of the KABP model is the hierarchical progression between knowledge, beliefs, and behaviors. Knowledge provides a solid foundation for behavior changes, and beliefs guide behavior changes. When applied to clinical care, it can be subdivided into three consecutive parts and integrated into the actual disease care process [8]. It has been used in the staged health education of patients with hypertension and coronary heart disease in previous studies, and the results have showed that it can effectively improve the self-efficacy and compliance behavior of patients, and it can effectively reduce the pain of patients with coronary heart disease after PCI [9,10]. At the same time, the 64-slice CT coronary vascular examination can also have a positive impact on the behavior, self-care and quality of life of patients with coronary heart disease [11]. The above reports all provided scientific evidence that the KABP could improve the compliance and care quality of patients with coronary heart disease. At present, there is few research report on the KABP nursing model in CR after PCI in patients with AMI. Thus, this study was to explore its application effects and provide guidance for clinical CR nursing.
Materials and methods
General information
In this prospective study, a total of 76 patients with AMI, who received PCI in our hospital, were selected as the research objects. The random number table was used to divide them into the KABP group including 41 cases (cardiac rehabilitation nursing based on KABP model) and the control group including 35 cases (conventional rehabilitation nursing). This study was approved by the hospital Medical Ethics Committee of our hospital.
The included subjects all met the diagnostic criteria for AMI in the ninth edition of Internal Medicine, and all successfully implemented PCI treatment [12]. Their Killip classification of cardiac function was lower than grade III and were aged between 40 and 70 years old. All patients and their families were agreed to participate in the study, and signed an informed consent form.
Those patients were excluded: patients who had extensive multi-site myocardial infarction or severe arrhythmia, cardiogenic shock, who accompanied severe liver, lung, kidney and other vital organ dysfunction; patients who suffered from tumors, who had obstacles in physical function or conscious communication; patients whose education level was lower than the level of elementary school.
Methods
After operation, both groups of patients were treated with blood pressure regulation, sedation and other treatments, symptomatic care such as oxygen and medication were also delivered.
Control group
Patients in the control group received routine rehabilitation care, including routine health education, psychological counseling, prevention and treatment of complications, diet and exercise intervention, etc. After PCI, patients should stay in bed and rest after insertion of the stent. The limbs should be fully immobilized for 12 hours, and ECG monitoring should be continued. From the next day onwards, the activity level will be considered according to the individual symptoms, such as attempting to sit up, standing up and walking out of bed after 3 days. After discharge from the hospital, they were given regular rehabilitation education and safety precautions, and the patient was instructed to continue to maintain physical activities every day until the previous daily activity was restored.
KABP group
To implement cardiac rehabilitation care based on the KABP model, the KABP intervention team was first established. The team member included one deputy chief physician, one head nurse (team leader) and six N2 Senior nurses. They were mainly responsible for the implementation and follow-up of training, as well as the training and feedback summary of intervention methods for rehabilitation nurses. The details were listed as follows.
Cognitive intervention: During the hospitalization period, the KABP team members would count and evaluate the basic conditions of the patient’s knowledge structure, self-management behavior, high-risk factors and so on. Then the KABP health file was established to facilitate subsequent implementation, follow-up and recording. Through knowledge lectures (video presentation), illustrated health manuals, public posters, electronic document promotion and other ways, AMI patients were helped to build up a disease knowledge system, understand the causes of disease development, pathological mechanisms, risk factors and complications caused by poor prognosis. The misconception that the cure depends on doctors’ surgery and medication would be correct, and the team would help patients eliminate negative ideas and misunderstandings of knowledge, and guide them to establish a positive and objective cognition of disease recovery. At the same time, the patient was informed that rehabilitation was a long-term process that requires the cooperation of doctors, nurses, and patients, especially for CR training in the post-discharge period. The patient’s cognition of the disease and the awareness of rehabilitation determine the patient’s compliance and the degree of harmony of nurse-patient cooperation.
Belief intervention: The sudden onset of the disease was often associated with complex emotions such as anxiety, fear, irritability and doubt. The initial recovery of the disease was accompanied by various physical and mental conditions such as fatigue, poor sleep quality and caution. Therefore, positive belief intervention was extremely important to help patients overcome the disease. Patients should be instructed to create a relaxing and comfortable resting environment, maintain a clean and tidy hospital or home environment, and enjoy happy music to reduce stress. The patient who was negatively pessimistic and skeptical about recovery should choose words that conveys an optimistic outlook on recovery, such as encouragement, hints, and successful case studies, to help him mentally and physically develop a healthy belief in recovery.
Behavioral intervention: We had a multidisciplinary team from many departments, including surgery, rehabilitation, psychology, nutrition, pharmacy and other departments, to review previous cases. A complete postoperative immediate CR training program was developed based on the energy consumption of each stage after PCI, the effectiveness of previous rehabilitation training and the post-hospital follow-up records, according to the American Heart Association’s guidelines for cardiac rehabilitation as a reference for the exercise program [13]. The program consisted of two phases (4 weeks after operation, the Brog Fatigue Scale was used to test its fatigue. As shown in Table 1. After the surgery, each patient was assigned with two rehabilitation nurses, who would assist and accompany the patient throughout the CR training under ECG monitoring or ECG telemetry in the hospital. During the training process, if there were any negative situations such as resistance, emotional instability and refusal to train, the designated rehabilitation nurse would give patient explanations and enlightenment, and seek the guidance and help of a psychotherapist in severe cases. The CR training after discharge were still followed up by one-to-one rehabilitation nurses through home visits, phone calls, WeChat, and text messages to supervise the continuation of CR. Telephone follow-up was conducted once a week, and the follow-up were conducted 3 months after discharge.
Table 1.
CR sports training schedule for KABP patients
| Stages | Timeline | Training content |
|---|---|---|
| During hospitalization | Within 12 hours after operation | The patient is mainly resting in bed, the nursing staff can assist patients to press the PCI puncture point after 6 hours and massage the lower back appropriately. Patients can raise the head of the bed and perform active or passive exercises, such as turning over, moving limbs, and performing major joint activities. They can gradually sit up in bed 1 or 2 times for 15-20 minutes per time, and also have the option to perform activities such as eating and washing. |
| 1 day after operation | The patient takes a sitting and standing position, changes the position when appropriate, and hangs his legs on the bed for 1 to 2 times, 15 to 20 minutes per time. The nursing staff massaged the patient’s waist and back twice a day, 10 minutes per time. | |
| 2 days after operation | The patient can try to get out of bed, and the nursing staff assists him to stand by the bed, sit on a chair for 2 to 3 times, and take care of defecation by the bed. | |
| 3 days after operation | The patient walks slowly on the bedside or indoors by supporting the wall 2-3 times per day, 10 minutes per time, and the time can be gradually increased according to their own physical ability. | |
| 4-6 days after operation | The patient can defecate and bathe by himself, walk slowly in the corridor outside the ward or in the hospital for 2-3 times, 15-20 minutes per time. | |
| 7 days after operation~Discharged | The patient walks slowly 3 times per day, no less than 15 minutes each time, and the nursing staff assists him to go up and down 2 to 3 stairs slowly, and he can take care of himself for basic life. | |
| After discharge | 1-2 weeks after operation | The patient can transition from walking slowly outdoors to a normal outdoor pace, 3 times/day, 15-20 minutes per time, and can slowly go up and down 10-20 steps. |
| 3-4 weeks after operation | The patient’s outdoor walking gradually increased slowly up and down the stairs 3 to 4 floors, fast walking, jogging and other items, 3 times per day, each time not less than 20 min, not more than 30 min. | |
| 4 weeks after operation | According to the patient’s recovery, the Brog Fatigue Scale was used to test its fatigue, and the exercise tolerance was tested by a flat test [14]. According to the results, the patient was guided to choose outdoor aerobic exercises, such as cycling, jogging, and Tai Chi. The starting point of the training intensity is when the patient’s self-conscious fatigue is 13-16, and the target heart rate is maintained in the range of (220-patient’s age) × (60% to 80%) during training, 3 times per day, no less than 20 min each time, no more than 30 min. | |
| 3 months after operation | Patients can participate in social activities and return to normal life and work. |
Note: CR: cardiac rehabilitation; KABP: knowledge, attitude, belief and practice; PCI: percutaneous coronary intervention.
During the training process, patients’ awareness of risk prevention should be raised. Measure and record blood pressure, pulse and heart rate before each training, and perform the following CR training after confirming normal. In case of force majeure factors such as weather changes outdoors, it could be converted to indoor sports, and the exercise intensity could be reduced as appropriate. After the training, record the number and time of daily training as well as the content and intensity of training. During the training period, if the patient developed pallor, palpitation, shortness of breath, chest tightness, neck tightness, numbness or pain in the limbs, dizziness and weakness, profuse sweating, slow or fast heart rate (>110 beats/min or <50 beats/min) and other abnormalities, the intensity of exercise should be reduced or stopped immediately. If the symptom didn’t get better or even worsens after adequate rest, the patient should be referred to the cardiology department immediately accompanied by family members.
Outcome measures and evaluation criteria
Comparison of cardiac function improvement: The left ventricular end systolic volume, left ventricular end diastolic volume, left ventricular ejection fraction (LVEF), stroke volume (SV), and cardiac index (CI) were measured by echocardiography within 48 hours after surgery and 3 months after postoperative follow-up. At the same time, the New York Heart Association (NYHA) classification was used to assess cardiac function after 3 months of postoperative follow-up and it was divided into grades I to IV [15]. Grade I referred to freedom of daily activities and basically unlimited. Grade II referred to slight limitation of daily activities, but no significant symptoms at rest. Grade III referred to the obvious limitation of daily life, palpitations, wheezing, angina and other symptoms caused by exercise or a small amount of physical activity, and the symptoms disappeared during rest. Grade IV referred to the limitation of any daily activities, and the above symptoms also occurred during rest.
Comparison of the risk of falling out of bed 7 days after operation: The inpatient fall risk assessment form was used to assess the falling risk [16]. The Cronbach’s α of the scale was 0.668, and the risk factor assessment specifically included age >65 years (1 point), consciousness impairment (1 point), visual impairment (1 point), mobility impairment or hemiplegia (3 points), sleep disorders or use of sedatives and analgesics (1 point), a history of unexplained falls or falling from bed in hospital within 1 year (1 point), physical weakness (dizziness, anemia, vertigo, hemorrhage, postural hypotension; 2 points). A total score of ≥4 was classified as high-risk falls/falling from bed and <4 as low-risk falls/falling from bed. The incidence of high/low risk of falling = (high/low risk of falling/falling from bed) number of people/total number of people * 100%.
Comparison of physical status improvement: The Freiburg physical status questionnaire was used for face-to-face survey, and the metabolic equivalent (MET) of the task and the patient’s self-reported physical activity status were recorded once before and 3 months of follow-up [17]. 1 MET was equivalent to a body energy expenditure of 4.2 kJ/kg/h while sitting still.
Comparison of the improvement of exercise endurance: The 6-minute walking test (6-MWT) test was used in the study [18]. After the patient rested for 15 minutes, the walking distance was measured at the fastest speed and walk straight for 6 minutes. If there was heart discomfort during the test, the patient should stop immediately, and tested once before and after 3 months of follow-up.
Comparison of self-management behavior scores: The Coronary Artery Disease Self-Management Scale (CSMS) was used in the study and the Cronbach’s α of the scale was 0.651-0.827 [19]. The scale had 3 major dimensions, 27 items, and was rated on a 5-point scale using a percentage system, including 8 items of daily life management, 15 items of disease medical management, and 4 items of emotional cognitive management. The average score for each dimension and the total average score for self-management were obtained. The score was the mean value of each dimension, and the score was proportional to the level of self-ability. It was evaluated once before and after 3 months of follow-up.
Comparison of quality of life scores: The China Questionnaire of Quality of Life in Patients with Cardiovascular Diseases (CQQC) was used in the study and the Cronbach’s α was 0.91 [20]. The questionnaire consisted of 6 items, divided into physical strength (2 questions), medical condition (6 questions), medical treatment (2 questions), general life (5 questions), psychosocial status (7 questions), work status (2 questions), evaluated once before and after 3 months of follow-up. The questionnaire score ranged from 0 to 154 points, and the score was directly proportional to the quality of life.
Statistical methods
All statistical data were analyzed using a professional statistical software named SPSS 21.0. Measurement data conforming to the normal distribution were expressed as mean ± standard deviation (x̅ ± sd). Denoted by t, the independent sample t test was used for the comparison between groups, and the paired sample t test was used for the before and after comparison within the group. All count data were expressed by the number of cases/percentage (n/%), which was evaluated by χ2 test and expressed by χ2. The difference was evaluated as statistically significant at P<0.05.
Results
Comparison of general information of the two groups of patients
There was no statistical difference in the general information of the two groups of patients (all P>0.05), as shown in Table 2.
Table 2.
Comparison of general information of the two groups of patients (x̅ ± sd, n/%)
| Items | Control group (n=35) | KABP group (n=41) | χ2/t | P |
|---|---|---|---|---|
| Gender (male/female) | 22/13 | 27/14 | 0.074 | 0.786 |
| Age (years) | 57.5±9.3 | 56.8±9.5 | 0.323 | 0.747 |
| Course of disease (month) | 10.2±2.7 | 9.8±2.3 | 0.698 | 0.488 |
| Smoking (n/%) | 29 (82.86) | 32 (78.05) | 0.276 | 0.600 |
| BMI (kg/m2) | 23.94±3.13 | 24.19±3.47 | 0.327 | 0.744 |
| Killip classification (n/%) | 0.549 | 0.458 | ||
| Grade I | 25 (71.43) | 26 (63.41) | ||
| Grade II | 10 (28.57) | 15 (36.59) | ||
| Coronary lesions (n/%) | 0.162 | 0.922 | ||
| Single branch lesion | 17 (48.57) | 20 (48.78) | ||
| Double branches lesion | 10 (28.57) | 13 (31.71) | ||
| Triple branches lesion | 8 (22.86) | 8 (19.51) | ||
| Complications (n/%) | ||||
| Hypertension | 7 (20.00) | 6 (14.63) | 0.383 | 0.536 |
| Diabetes | 6 (17.14) | 8 (19.51) | 0.071 | 0.791 |
| Hyperlipidemia | 11 (31.43) | 14 (34.15) | 0.063 | 0.802 |
Note: Killip classification: clinical classification of heart failure due to AMI; BMI index: body mass index; KABP: knowledge, attitude, belief and practice.
Comparison of cardiac function between the two groups of patients within 48 hours and 3 months after surgery
Within 48 hours after operation, there was no marked difference in the indicators of cardiac function between the two groups (all P>0.05). Three months after surgery, the improvement of cardiac function indexes including LVEF, SV, and CI in the KABP group was significantly better than that of the control group (all P<0.05). There was no significant difference between the two groups in left ventricular end systolic volume, left ventricular end diastolic volume (P>0.05), as shown in Table 3.
Table 3.
Comparison of cardiac function between the two groups of patients before and after intervention (x̅ ± sd, control group n=35, KABP group n=41)
| Items | Within 48 hours after surgery | 3 months after surgery | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Control group | KABP group | t | P | Control group | KABP group | t | P | |
| LVES (mL) | 47.43±12.19 | 48.76±11.54 | 0.488 | 0.627 | 51.45±15.32 | 47.12±13.67 | 1.302 | 0.197 |
| LVEDV (mL) | 100.24±27.25 | 98.53±23.13 | 0.296 | 0.768 | 103.65±25.37 | 105.38±29.66 | 0.271 | 0.787 |
| LVEF (%) | 45.46±3.61 | 44.24±3.24 | 1.552 | 0.125 | 50.57±5.62a | 58.35±5.73a | 5.952 | 0.000 |
| SV (mL) | 52.72±10.85 | 52.97±11.28 | 0.098 | 0.922 | 53.29±11.72 | 59.75±13.51a | 2.207 | 0.030 |
| CI (L/(min.m2)) | 2.65±0.57 | 2.67±0.42 | 0.176 | 0.861 | 2.98±0.66 | 3.36±0.74 | 2.344 | 0.022 |
Note: Compared with the data measured within 48 hours after operation in this group;
P<0.05.
KABP: knowledge, attitude, belief and practice.
Comparison of NYHA classification of the two groups of patients 3 months after surgery
Three months after the operation, the NYHA classification of the KABP group was significantly improved when compared with that of the control group (P<0.001), as shown in Table 4.
Table 4.
Comparison of NYHA classifications of the two groups of patients 3 months after surgery (n, %)
| Group | Grade I | Grade II | Grade III | Grade IV |
|---|---|---|---|---|
| Control group (n=35) | 3 (8.57) | 7 (20.00) | 15 (42.86) | 10 (28.57) |
| KABP group (n=41) | 18 (43.90) | 16 (39.02) | 5 (12.20) | 2 (4.88) |
| χ2 | 24.269 | |||
| P | 0.000 | |||
Note: KABP: knowledge, attitude, belief and practice.
Comparison of the risk of falls between the two groups of patients after getting out of bed
The high risk of falling out of bed in the KABP group 7 days after surgery (17.07%) was significantly lower than that of the control group (74.29%; P<0.001), as shown in Figure 1.
Figure 1.
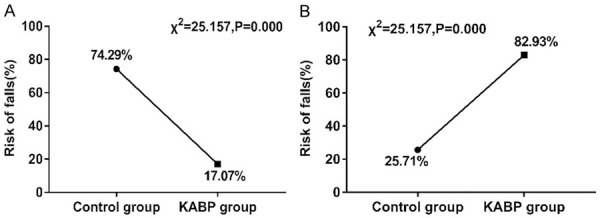
Comparison of the risk of falls between the two groups of patients after getting out of bed. A: High-Risk; B: Low-Risk. KABP: knowledge, attitude, belief and practice.
Comparison of physical status and exercise endurance between the two groups of patients before and after intervention
Before intervention, there was no significant difference in MET (2.34±0.72, 2.37±0.69) and 6-MWT score (255.34±27.92, 256.18±26.85) between the two groups of patients (all P>0.05). After the intervention, the MET (4.63±1.45, 6.13±1.67) and 6-MWT scores (375.56±27.34, 427.67±32.82) of the two groups of patients were significantly higher than those before the intervention (all P<0.05). Among them, the KABP group has a significantly higher increase than the control group (all P<0.001), as shown in Figures 2, 3.
Figure 2.
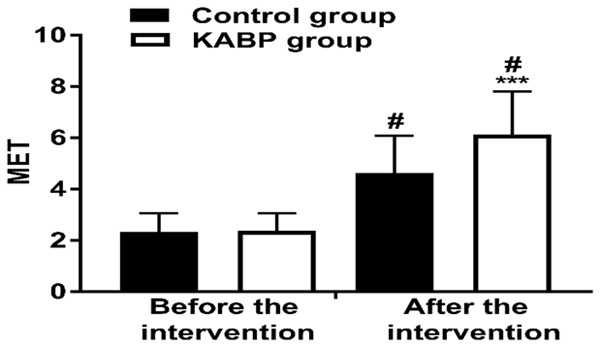
Comparison of the physical status of the two groups of patients before and after intervention. Compared with this group before intervention, #P<0.05; compared with the control group, ***P<0.001. MET: metabolic equivalent; KABP: knowledge, attitude, belief and practice.
Figure 3.
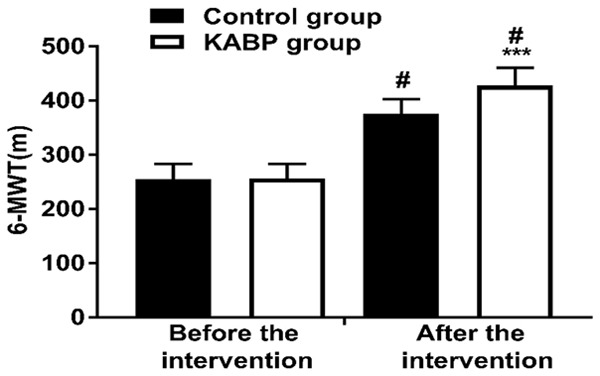
Comparison of exercise endurance between two groups of patients before and after intervention. Compared with this group before intervention, #P<0.05; compared with the control group, ***P<0.001. 6-MWT: 6-minute walk test; KABP: knowledge, attitude, belief and practice.
Comparison of CSMS scores before and after intervention between the two groups
Before the intervention, there were no significant differences in the CSMS scores and total scores between the two groups of patients (all P>0.05). After the intervention, the CSMS scores and total scores of the two groups of patients were significantly higher than those before intervention (all P<0.05), and the total scores of daily life management, disease medical management, emotional cognitive management, and self-management in CSMS of the KABP group were all significantly higher than that of the control group (all P<0.01), as shown in Table 5.
Table 5.
Comparison of CSMS scores before and after intervention between the two groups (x̅ ± sd, control group n=35, KABP group n=41)
| Items | Before intervention | After intervention | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Control group | KABP group | t | P | Control group | KABP group | t | P | |
| Daily life management | 67.24±14.75 | 68.01±15.26 | 0.227 | 0.824 | 75.47±16.34a | 87.29±11.25a | 3.611 | 0.000 |
| Disease medical management | 44.24±8.79 | 45.81±9.16 | 0.759 | 0.450 | 69.25±12.81a | 81.76±15.73a | 3.759 | 0.000 |
| Emotional cognitive management | 75.73±6.81 | 76.13±7.79 | 0.236 | 0.814 | 82.46±5.87a | 89.52±6.32a | 5.015 | 0.000 |
| Total score for self-management | 63.35±11.26 | 63.67±12.93 | 0.114 | 0.910 | 79.19±13.56a | 87.24±11.37a | 2.815 | 0.006 |
Note: Compared with this group before intervention;
P<0.05.
KABP: knowledge, attitude, belief and practice.
Comparison of CQQC scores before and after intervention between the two groups
Before the intervention, there was no significant difference between the two groups of patients in CQQC scores and total scores (all P>0.05). After the intervention, the scores and total scores of CQQC in the two groups were significantly higher than those before the intervention (all P<0.05). Among them, the physical strength, medical condition, medical treatment, general life, psychosocial status, work status and total score of CQQC in the KABP group were All were significantly higher than the control group (all P<0.001), as shown in Table 6.
Table 6.
Comparison of the quality of life scores of cardiovascular patients before and after intervention between the two groups (x̅ ± sd, control group n=35, KABP group n=41)
| Items | Before intervention | After intervention | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Control group | KABP group | t | P | Control group | KABP group | t | P | |
| Physical strength | 11.34±2.67 | 12.05±3.52 | 0.977 | 0.332 | 12.67±3.12a | 17.87±3.66a | 6.602 | 0.000 |
| Medical condition | 14.82±3.71 | 13.56±3.18 | 1.595 | 0.115 | 16.23±3.48a | 21.56±4.19a | 5.969 | 0.000 |
| Medical treatment | 2.45±0.72 | 2.39±0.46 | 0.425 | 0.673 | 3.57±0.47a | 5.92±0.73a | 16.912 | 0.000 |
| General life | 4.78±0.28 | 4.81±0.33 | 0.423 | 0.673 | 6.18±1.84a | 10.34±2.67a | 7.997 | 0.000 |
| Psychosocial status | 13.13±2.26 | 13.20±2.58 | 0.125 | 0.901 | 15.72±3.27a | 20.19±4.33a | 5.007 | 0.000 |
| Work status | 1.46±0.34 | 1.47±0.72 | 0.079 | 0.937 | 2.59±0.68a | 4.25±1.02a | 8.451 | 0.000 |
| Total score | 46.35±8.13 | 45.26±9.13 | 0.545 | 0.587 | 57.46±10.35a | 79.23±15.24a | 7.370 | 0.000 |
Note: Compared with this group before intervention;
P<0.05.
KABP: knowledge, attitude, belief and practice.
Discussion
The age of AMI patients is gradually getting younger. Meanwhile, there are more than 500,000 new patients with AMI each year in China, and its prevalence is increasing. What’s worse, the case fatality rate for patients over 60 years old is 38.4%, and it has risen significantly to 50% for patients over 80 years old [21]. Thus, it’s quite important to find an effective way to treat those patients. The current PCI technology provides a good medical guarantee for the rescue success rate of AMI, and the treatment also assists scientific nursing intervention to improve the prognosis of patients.
Studies have confirmed that CR training after PCI can regulate the body’s nervous system and inhibit bad emotions from causing adverse effects on the cardiovascular system [22]. Regular CR training can enhance the function of endothelial progenitor cells, repair blood vessel damage, and accelerate blood circulation. This training can also increase myocardial oxygen supply and coronary blood flow, which helps to ablate atherosclerotic plaques. It can also help the body’s energy metabolism to maintain a balance, reducing the risk of obesity and fat accumulation in patients, and obesity is an independent risk factor for cardiovascular disease. Zhang et al. discovered that taking simple and safe exercise for community CR could significantly improve the quality of life of patients with AMI after PCI, including improvement of cardiac ejection fraction, exercise endurance, etc. [23]. However, they also revealed that good treatment and rehabilitation results were the result of collaboration among cardiologists, general practitioners and nurses, as well as the cooperation of patients themselves and their families. It was found by Indian scholar Prabhakaran et al. that under the background of the relative lack of CR programs in India, yoga-based CR can improve the health of AMI patients and help their daily activities return to before the infarction [24]. Therefore, when conventional CR cannot be used or personal implementation was limited, yoga-based CR can be another option for AMI patients. Clinically, the cardiac rehabilitation created by Dr. Herman Hellerstein in the United States was divided into three phases: the hospitalization period, the early outpatient rehabilitation period after discharge, and the return to work period [25]. However, the implementation of CR in the entire treatment and rehabilitation process of AMI in China was still lagging behind, and it was still in the trial stage. Doctors, nurses and patients still do not pay enough attention to it. Most patients were disconnected from the hospital after they are discharged.
KABP is a progressive model of health behavior change based on personal knowledge and beliefs, with the goal of enabling patients to develop the correct perceptions, positive beliefs, self-management skills and compliance, and to change their behavior to achieve the desired treatment and recovery outcomes. In essence, KABP also helps patients to establish cognitive theory, cultivate positive beliefs and correct attitudes in health education, and form active and self-disciplined health promotion behaviors. Fatema et al. pointed out that knowledge and attitude were the main signs of consciousness, and enhancing the public’s cognitive awareness was the main determinant of preventing metabolic diseases and their complications [26]. Scholars such as Nivedita found that KABP can achieve ideal results in the prevention and control of the spread of infectious diseases [27]. And the KABP health education model can also alleviate the anxiety and pain of patients during laparoscopic perioperative period [28]. However, the current clinical application of KABP mode in the prognosis recovery of AMI patients after PCI was rare, and there was a lack of reports on the effect of cardiac rehabilitation on patients’ rehabilitation.
This study adopted the cardiac rehabilitation nursing based on the KABP model. It helps AMI patients to build a disease knowledge system, improves patients’ awareness and attention to the disease, and lays the foundation for subsequent behavior changes. Behavior change is a continuous process. In addition to cognitive intervention during hospitalization, follow-up after discharge is also important. Because the implementation of CR’s exercise plan is closely related to personal compliance and self-management. It is possible to improve the selfmanagement ability by changing the cognition of AMI patients, and cooperate with cardiac rehabilitation to achieve the improvement of cardiac function and quality of life. At the same time, belief interventions are based on cognitive interventions, where the patient understands and accepts the theoretically and cognitively the correct concept of disease recovery and can actively reject unhealthy consciousness and behaviors. This kind of change from the ideological level can directly guide them to establish a correct way of life with long lasting influence, and then provide a basis of thinking and action for the continuous progress of CR. In routine care after PCI, patients need to stay in bed early, but prolonged bed rest and passive posture may make the patient feel fatigue, irritable, with low back pain, and even venous thrombosis of the lower extremities, and thus increase the burden on the heart, and cause serious cardiovascular complications such as arrhythmia and ventricular fibrillation [29]. In this study, early CR rehabilitation care began to adjust the patient’s position before getting out of bed to relax the lower back muscles and relieve fatigue. This can effectively prevent venous thrombosis in the lower extremities, promote blood circulation and return, expand peripheral blood vessels, regulate gastrointestinal motility, and prevent constipation. At the same time, CR also helped to regulate the patient’s blood lipid level. Exercise can also increase the return blood volume and increase the contractility of the myocardium, which in turn can increase LVEF and restore heart function. The continuous CR care after discharge can improve the lung capacity of the patient, help the recovery of lung function, and enhance the patient’s exercise tolerance. In addition, the benefits of regular rehabilitation exercises were not only reflected in the recovery of physical functions, but also in the reduced the tension and anxiety of patients and maintenance of a good mental state. The results of this study showed that after 3 months of postoperative follow-up, the cardiac function of the KABP group including LVEF, SV, CI improvement, and NYHA classification were significantly better than those of the control group. This may be related to CR’s ability to enhance the adaptability of patients’ cardiac function, accelerate the recovery of patients’ myocardial function, increase coronary blood supply and improve cardiac function. The patients in the control group who received routine care should maintain strict immobilization after PCI, and have more irregular rehabilitation exercise plans after discharge, ignoring the recovery of patients’ heart function. At the same time, the MET value, 6-MWT, CSMS and CQQC scores of the KABP group were significantly higher than those of the control group. This may be due to the fact that the construction of the disease knowledge system based on the KABP model has changed the didactic intervention of nursing personnel in traditional health education, broken the shackles of knowledge that patients knew what they knew but did not know why, and improved patients’ self-management behaviors and CR compliance, while patients’ active cooperation and persistence in completing CR improved patients’ physical fitness, exercise endurance, and quality of life.
Previous studies have demonstrated that decreased muscle strength can lead to imbalances in patients’ gait, instability of foot strength, and damage to their balance ability, which is also an extremely important predictor of falls in patients [30]. In the traditional nursing concept, after PCI, patients need to stay in bed for at least 3 days, which greatly impaired the balance control of the patient’s muscle strength and peaceful activities. In the KABP group, patients received planned early in-hospital CR care after surgery, combined with muscle strength training to increase their maximum muscle strength, which was conducive to the control of the patient’s gait balance and to reduce the risk of falling out of bed after the operation. It was showed that the high risk of falling out of bed 7 days after operation in the KABP group (17.07%) was significantly lower than that in the control group, which was consistent with the above study. Our study was only aimed at stage I and stage II cardiac rehabilitation. In the later stage, the contents of stage III cardiac rehabilitation can be added to comprehensively prevent long-term cardiovascular disease and its recurrence. It is worth noting that cardiac rehabilitation is still in the early stage in China, and actually most hospitals are not able to provide cardiac rehabilitation services currently due to a variety of reasons. The actual participation rate in cardiac rehabilitation is low, and many people withdraw halfway through participation. Therefore, comprehensive improvement of medical services and national health management is still a long-way to go.
In summary, cardiac rehabilitation care based on the KABP model can improve the recovery of cardiac function in patients with AMI after PCI, reduce the risk of falling after getting out of bed, and help patients recover their physical fitness and exercise endurance. At the same time, it can improve self-management behavior and postoperative quality of life.
Disclosure of conflict of interest
None.
References
- 1.Hofmann R, James SK, Jernberg T, Lindahl B, Erlinge D, Witt N, Arefalk G, Frick M, Alfredsson J, Nilsson L, Ravn-Fischer A, Omerovic E, Kellerth T, Sparv D, Ekelund U, Linder R, Ekström M, Lauermann J, Haaga U, Pernow J, Östlund O, Herlitz J, Svensson L. Oxygen therapy in suspected acute myocardial infarction. N Engl J Med. 2017;377:1240–1249. doi: 10.1056/NEJMoa1706222. [DOI] [PubMed] [Google Scholar]
- 2.Luo L, Xu WQ, Zhong RX, Chen F, Fu YL, Zhang P, Xiao SH. Clinical efficacy and safety of percutaneous coronary intervention for acute myocardial infarction complicated with chronic renal insufficiency: a protocol of systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e16005. doi: 10.1097/MD.0000000000016005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holmes AA, Bangalore S. PCI or CABG for severe unprotected left main coronary artery disease: making sense of the NOBLE and EXCEL trials. J Thorac Dis. 2017;9:e451–e456. doi: 10.21037/jtd.2017.04.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kachur S, Chongthammakun V, Lavie CJ, De Schutter A, Arena R, Milani RV, Franklin BA. Impact of cardiac rehabilitation and exercise training programs in coronary heart disease. Prog Cardiovasc Dis. 2017;60:103–114. doi: 10.1016/j.pcad.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Risom SS. Cardiac rehabilitation in real life. Int J Cardiol. 2018;255:154–155. doi: 10.1016/j.ijcard.2017.12.084. [DOI] [PubMed] [Google Scholar]
- 6.Panovský R, Kukla P, Jancík J, Meluzín J, Dobsák P, Kincl V, Svobodník A. The prognostic effect of different types of cardiac rehabilitation in patients with coronary artery disease. Acta Cardiol. 2013;68:575–581. doi: 10.2143/AC.68.6.8000004. [DOI] [PubMed] [Google Scholar]
- 7.Pathak A, Rathore A, Dharani C. To asses the knowledge, attitude and practice (KAP) of paramedical staff towards chemotherapy drugs and their administration and effect of a capsule course on the same. Ann Oncol. 2016 [Google Scholar]
- 8.Zahiruddin WM, Arifin WN, Mohd-Nazri S, Sukeri S, Zawaha I, Bakar RA, Hamat RA, Malina O, Jamaludin T, Pathman A, Mas-Harithulfadhli-Agus AR, Norazlin I, Suhailah BS, Saudi SNS, Abdullah NM, Nozmi N, Zainuddin AW, Aziah D. Development and validation of a new knowledge, attitude, belief and practice questionnaire on leptospirosis in malaysia. BMC Public Health. 2018;18:331. doi: 10.1186/s12889-018-5234-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao S, Zhao H, Wang L, Du S, Qin Y. Education is critical for medication adherence in patients with coronary heart disease. Acta Cardiol. 2015;70:197–204. doi: 10.1080/ac.70.2.3073511. [DOI] [PubMed] [Google Scholar]
- 10.Aronov D, Bubnova M, Iosseliani D, Orekhov A. Clinical efficacy of a medical centre- and home-based cardiac rehabilitation program for patients with coronary heart disease after coronary bypass graft surgery. Arch Med Res. 2019;50:122–132. doi: 10.1016/j.arcmed.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Rahman H, Corcoran D, Aetesam-Ur-Rahman M, Hoole SP, Berry C, Perera D. Diagnosis of patients with angina and non-obstructive coronary disease in the catheter laboratory. Heart. 2019;105:1536–1542. doi: 10.1136/heartjnl-2019-315042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Q, Ma J, Jiang Z, Wu F, Ping J, Ming L. Identification of micrornas as diagnostic biomarkers for acute myocardial infarction in Asian populations: a systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e7173. doi: 10.1097/MD.0000000000007173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DuBose-Briski V, Yao X, Dunlay SM, Dhruva SS, Ross JS, Shah ND, Noseworthy PA. Evolution of the American college of cardiology and american heart association cardiology clinical practice guidelines: a 10-year assessment. J Am Heart Assoc. 2019;8:e012065. doi: 10.1161/JAHA.119.012065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cameron K, Williamson P, Short MA, Gradisar M. Validation of the flinders fatigue scale as a measure of daytime fatigue. Sleep Med. 2017;30:105–112. doi: 10.1016/j.sleep.2016.11.016. [DOI] [PubMed] [Google Scholar]
- 15.Caraballo C, Desai NR, Mulder H, Alhanti B, Wilson FP, Fiuzat M, Felker GM, Piña IL, O’Connor CM, Lindenfeld J, Januzzi JL, Cohen LS, Ahmad T. Clinical implications of the New York heart association classification. J Am Heart Assoc. 2019;8:e014240. doi: 10.1161/JAHA.119.014240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poe SS, Cvach M, Dawson PB, Straus H, Hill EE. The Johns Hopkins Fall risk assessment tool: postimplementation evaluation. J Nurs Care Qual. 2007;22:293–298. doi: 10.1097/01.NCQ.0000290408.74027.39. [DOI] [PubMed] [Google Scholar]
- 17.Li Y, Han J, Liu Y, Wang R, Wang R, Wu XP, Cao ZB. China survey of fitness trends for 2020. ACSMs Health Fit J. 2019;23:19–27. [Google Scholar]
- 18.Santos VB, Lopes CT, Dos Anjos LD, Begot I, Cassiolatto F, Guizilinni S, Moreira RSL. Accuracy of the defining characteristics of fatigue in patients with heart failure as identified by the 6-minute walking test. Int J Nurs Knowl. 2020;31:188–193. doi: 10.1111/2047-3095.12270. [DOI] [PubMed] [Google Scholar]
- 19.Barham A, Ibraheem R, Zyoud SH. Cardiac self-efficacy and quality of life in patients with coronary heart disease: a cross-sectional study from palestine. BMC Cardiovasc Disord. 2019;19:290. doi: 10.1186/s12872-019-01281-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu M, Li S, Li S, Li J, Xu H, Chen K. Baduanjin exercise for patients with ischemic heart failure on phase-II cardiac rehabilitation (BEAR trial): study protocol for a prospective randomized controlled trial. Trials. 2018;19:381. doi: 10.1186/s13063-018-2759-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xiao H, Zhang H, Wang D, Shen C, Xu Z, Zhang Y, Jiang G, Yang G, Wan X, Naghavi M. Impact of smoke-free legislation on acute myocardial infarction and stroke mortality: Tianjin, China, 2007-2015. Tob Control. 2020;29:61–67. doi: 10.1136/tobaccocontrol-2018-054477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sunamura M, Ter Hoeve N, Geleijnse ML, Steenaard RV, van den Berg-Emons HJG, Boersma H, van Domburg RT. Cardiac rehabilitation in patients who underwent primary percutaneous coronary intervention for acute myocardial infarction: determinants of programme participation and completion. Neth Heart J. 2017;25:618–628. doi: 10.1007/s12471-017-1039-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang Y, Cao H, Jiang P, Tang H. Cardiac rehabilitation in acute myocardial infarction patients after percutaneous coronary intervention: a community-based study. Medicine (Baltimore) 2018;97:e9785. doi: 10.1097/MD.0000000000009785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prabhakaran D, Chandrasekaran AM, Singh K, Mohan B, Chattopadhyay K, Chadha DS, Negi PC, Bhat P, Sadananda KS, Ajay VS, Singh K, Praveen PA, Devarajan R, Kondal D, Soni D, Mallinson P, Manchanda SC, Madan K, Hughes AD, Chathurvedi N, Roberts I, Ebrahim S, Reddy KS, Tandon N, Pocock S, Roy A, Kinra S. Yoga-based cardiac rehabilitation after acute myocardial infarction: a randomized trial. J Am Coll Cardiol. 2020;75:1551–1561. doi: 10.1016/j.jacc.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bethell HJ. Cardiac rehabilitation: from hellerstein to the millennium. Int J Clin Pract. 2000;54:92–97. [PubMed] [Google Scholar]
- 26.Fatema K, Hossain S, Natasha K, Chowdhury HA, Akter J, Khan T, Ali L. Knowledge attitude and practice regarding diabetes mellitus among nondiabetic and diabetic study participants in Bangladesh. BMC Public Health. 2017;17:364. doi: 10.1186/s12889-017-4285-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nivedita Knowledge, attitude, behaviour and practices (KABP) of the community and resultant iec leading to behaviour change about dengue in Jodhpur city, Rajasthan. J Vector Borne Dis. 2016;53:279–282. [PubMed] [Google Scholar]
- 28.Kesari D, Kovisman V, Cytron S, Benjamin J. Effects on pain and anxiety of patients viewing their cystoscopy in addition to a detailed explanation: a controlled study. BJU Int. 2003;92:751–752. doi: 10.1046/j.1464-410x.2003.04477.x. [DOI] [PubMed] [Google Scholar]
- 29.De Bacquer D, De Smedt D, Kotseva K, Jennings C, Wood D, Rydén L, Gyberg V, Shahim B, Amouyel P, Bruthans J, Castro Conde A, Cífková R, Deckers JW, De Sutter J, Dilic M, Dolzhenko M, Erglis A, Fras Z, Gaita D, Gotcheva N, Goudevenos J, Heuschmann P, Laucevicius A, Lehto S, Lovic D, Miličić D, Moore D, Nicolaides E, Oganov R, Pajak A, Pogosova N, Reiner Z, Stagmo M, Störk S, Tokgözoğlu L, Vulic D, Wagner M, De Backer G. Incidence of cardiovascular events in patients with stabilized coronary heart disease: the EUROASPIRE IV follow-up study. Eur J Epidemiol. 2019;34:247–258. doi: 10.1007/s10654-018-0454-0. [DOI] [PubMed] [Google Scholar]
- 30.Patterson BW, Repplinger MD, Pulia MS, Batt RJ, Svenson JE, Trinh A, Mendonça EA, Smith MA, Hamedani AG, Shah MN. Using the Hendrich II inpatient fall risk screen to predict outpatient falls after emergency department visits. J Am Geriatr Soc. 2018;66:760–765. doi: 10.1111/jgs.15299. [DOI] [PMC free article] [PubMed] [Google Scholar]


