Abstract
Objective: This research was designed to probe into the influencing factors of holistic nursing intervention under a social medical model on psychology and quality of life in advanced gastric cancer (GC) patients. Methods: Altogether 194 patients with advanced GC treated in our hospital from May 2017 to July 2018 were divided into two groups according to different nursing intervention methods. Where from, 86 were given routine nursing intervention and 108 were given holistic nursing intervention under a social medical model. The psychology, pain relief, sleep quality and self-nursing ability of patients were compared before and after intervention. The quality of life before and after intervention and the nursing satisfaction score after nursing were recorded. The factors affecting their quality of life were assessed by Logistic regression analysis. Results: The SAS, SDS, NRS and PSQI scores in the intervention group (IG) were obviously lower than those in the control group (CG) after nursing. The ESCA and EORTC QLQ-C30 scores after nursing in the IG were markedly higher than those in the CG. The total nursing satisfaction of patients in the IG after nursing was obviously higher than that in the CG. Logistic regression analysis revealed that age, lymph node metastasis, TNM stage, unimproved negative emotion, lack of self-nursing ability and routine nursing intervention all increased the risk of reduced quality of life. Conclusion: The decline in the quality of life of patients with advanced GC results from a comprehensive action of various risk factors, and holistic nursing under a social medical model can improve the psychology of patients, improve their self-nursing ability and quality of life.
Keywords: Holistic nursing under a social medical model, advanced gastric cancer, psychology, quality of life, influencing factors
Introduction
Gastric cancer (GC) is a serious worldwide health burden. It is the fourth most common cancer and the second largest cause of cancer-related mortality, which is related to a high morbidity [1]. Because the etiology and pathogenesis of GC have not yet been determined, although some pathogenic factors have been identified, primary prevention is still a major challenge [2]. A recent study has shown that 80-90% of GC patients are in advanced stages at the time of diagnosis, and most are prone to have negative emotions due to loss of body function and psychological factors after diagnosis [3]. In severe cases, patients will refuse to cooperate with treatment, which will lead to medical care work failure, thus reducing the treatment efficacy [4]. Most patients will suffer from cancer pain, which will cause great trouble and leads to loss of appetite, increased negative emotions and insomnia, seriously affecting the physical and mental health and quality of life of patients [5,6].
Clinically, treatment resistance for cancer patients can be caused by an anxious psychology and emotions and will impel them to refuse treatment intervention. Therefore, it is necessary to communicate deeply with patients, listen carefully to their complaints and concerns, and answer their questions patiently. It’s also essential to make patients understand the treatment effect, thus reducing their concerns and psychological conflicts as much as possible, enhancing their confidence in overcoming diseases and encouraging them to cooperate with clinical treatment [7]. However, the prognosis of advanced GC patients is poor, and chemotherapy intervention affects their quality of life [8]. Thus, this research included nursing intervention observations on the influencing factors of the quality of life of patients with advanced GC. Holistic nursing under the mode of social medicine is a comprehensive type of nursing directed by comprehensive concepts of biology, psychology and society, which pays attention to the disease assessment, social living conditions and psychological feelings of patients [9]. It helps patients deepen their recognition and confidence in medical staff, strengthen their cognition and understanding of diseases, thus actively cooperating with the work of nursing staff [10]. For example, He XL and others [11] have confirmed that giving high-quality nursing intervention to GC patients during the perioperative period can reduce their psychological barriers during the perioperative period and improve their quality of life after operation. Another study has shown that [12] effective nursing intervention for advanced GC patients can improve their mood and survival, and the nursing satisfaction score after intervention is higher.
The factors affecting the quality of life of advanced GC patients were analyzed, and the effects of holistic nursing under a social medical mode and nursing intervention methods on their psychological improvement and survival during the observation period were analyzed.
Materials and methods
General data
Altogether, 194 patients with advanced GC treated in the Huai’an Hospital of Chinese Medicine from May 2017 to July 2018 were selected and divided into two groups based on different nursing intervention methods. Where from, 86 patients were given routine nursing intervention and 108 were given holistic nursing intervention under a social medical mode. Inclusion criteria: patients were diagnosed as having advanced GC by gastric biopsy or pathological section [13]; patients had clear thinking and normal linguistic competence, so they could correctly understand the contents of the rating scale; patients had complete general clinical data. This research was approved by the Ethics Committee of our hospital. Both the subjects and their families have been informed, and they all signed the full informed consent. Exclusion criteria: Those who were complicated with severe anemia and systemic infection; those who could not complete the rating scale survey independently; those who were complicated with dysfunction of heart, kidney, liver and other organs; those who quit the experiment halfway; those who had a history of mental illness and were lost to follow up interview.
Nursing methods
Patients in the control group (CG) were given routine nursing: the medical staff gave routine testing guidance and simple safety education after patients were diagnosed and admitted to hospital. Patients were informed of matters needing attention when treating diseases, and given a targeted introduction of basic knowledge of diseases, so as to improve the awareness of diseases and treatment. The medical staff also gave patients a good ward environment, actively answered their questions, eliminated their doubts and promoted disease recovery.
Patients in the intervention group (IG) were given holistic nursing under the social medical model: (1) Disease cognition and psychological counseling: the medical staff strengthened communication with patients after admission, and give guidance on disease detection and matters needing attention at admission. After patients were admitted to hospital, their family, psychology, disease cognition degree and educational level were evaluated comprehensively, and then the nursing team gave psychological counseling and intervention on the basis of scientific evaluation of their psychology, and provided targeted psychological counseling in view of the psychological evaluation results. Nurses explained the disease knowledge to patients, and improved their unhealthy psychology, fear, despair and negative psychology in the face of treatment through daily condolences, observation of vital signs, multi-directional communication and other diversified ways. Besides, they also listed some similar cases with good treatment effect to the patients, so as to enhance their confidence in treatment, thus improving treatment compliance and promoting disease rehabilitation, so that they could actively cooperate with this nursing intervention and enhance self-nursing ability. (2) Pain intervention: the medical team strictly monitored patients’ condition, explained doctors’ advice (types of analgesic drugs, correct medication methods, and adverse reactions after medication), and distributed pain-related health manuals and materials to them, so as to comprehensively increase their awareness of pain management and drug use, and guided them to write pain treatment diaries to make pain management more standardized. (3) Sleep intervention: the nursing staff provided the patients with a comfortable, spacious and bright ward for relief, ensuring sufficient light in the ward and regular ventilating. At the same time, it was necessary for staff to operate, walk and talk lightly, so as to reduce the tension of patients caused by environmental factors, thus affecting their sleep. (4) Dietary guidance: the nursing staff informed patients to eat more high-vitamin, high-protein and high-calorie diets, and eat more fresh fruits and vegetables to supplement all vitamins and calories in their bodies, so as to enhance their resistance.
Outcome measures
1. Psychology scoring criteria of patients in both groups: self-rating depression scale (SDS) and self-rating anxiety scale (SAS) [14]: the SDS scale was divided into 20 items and the cut-off value was 53 points (53-62: mild depression, 62-72: moderate depression, ≥ 72: severe depression). The SAS scale was divided into 20 items, with a score of 50 points (50-59: mild anxiety, 60-69: moderate anxiety, ≥ 70: severe anxiety).
2. The pain degree was assessed by NRS [15], with the highest score of 10 points. The higher the score was, the more severe the pain degree was.
3. Pittsburgh Sleep Quality Index (PSQI) was employed [16], which had 7 dimensions and scores ranging from 0 to 21. The higher the score after evaluation was, the worse the sleep quality of patients was.
4. Self-care ability: self-nursing ability scale (ESCA) [17]: there were 4 different fields and 43 items in the scale, and the total score of the scale was 172. The higher the score was, the higher the self-care ability of patients was.
5. Quality of life assessment: EORTC QLQ-C30 [18] was adopted, which consisted of six single items: general health status, functional areas, symptom areas. The higher the score was, the higher the quality of life was.
6. Nursing satisfaction: patients were scored by the Satisfaction Questionnaire of our hospital, with three dimensions: very satisfied, satisfied and dissatisfied, and those were counted later.
7. The patients after nursing were divided into good prognosis and bad prognosis, and the factors affecting the quality of life of advanced GC patients were analyzed by logistics multivariate regression.
Statistical methods
SPSS 25.0 (Bioeasy Technology Co., Ltd., Beijing, China) was used for statistical analysis. The counting data were represented by cases/percentage (n/%) and inter-group comparison was analyzed through Chi-square test. When the theoretical frequency was less than 5, we employed continuous correction Chi-square test. The measurement data were expressed by (mean ± SD) and inter-group comparison was assessed via independent-samples t test. Intra-group comparison before and after nursing was analyzed via paired t test. The factors affecting the quality of life of advanced GC patients were analyzed via logistics multivariate regression, and the experimental data was illustrated via GraphPad Prism 6. The difference was statistically remarkable when P < 0.05.
Results
Comparison of general data of patients between both groups
There was no marked difference in gender, average age, body mass index, pathological type, lymph node metastasis, tumor size, TNM stage, history of smoking or drinking between both groups (P > 0.05) (Table 1).
Table 1.
General data of patients in intervention group and control group [n (%)] (mean ± SD)
| Classification | Intervention group (n=108) | Control group (n=86) | t/χ2 value | P value |
|---|---|---|---|---|
| Gender | 0.025 | 0.874 | ||
| Male | 59 (54.63) | 46 (53.49) | ||
| Female | 49 (45.37) | 40 (46.51) | ||
| Average age (years) | 48.79±4.13 | 49.16±4.08 | 0.623 | 0.534 |
| BMI (kg/m2) | 22.34±3.12 | 22.64±3.17 | 0.661 | 0.509 |
| Pathological typing | 0.515 | 0.916 | ||
| Poorly differentiated carcinoma | 36 (33.33) | 28 (32.56) | ||
| Moderately differentiated carcinoma | 33 (30.56) | 23 (26.74) | ||
| Mucinous adenocarcinoma | 21 (19.44) | 19 (22.09) | ||
| Signet-ring cell carcinoma | 18 (16.67) | 16 (18.60) | ||
| Lymph node metastasis | 0.015 | 0.901 | ||
| Yes | 38 (35.19) | 31 (36.05) | ||
| No | 70 (64.81) | 55 (63.95) | ||
| Tumor size (cm) | 0.174 | 0.678 | ||
| < 5 | 56 (51.85) | 42 (48.84) | ||
| ≥ 5 | 52 (48.15) | 44 (51.16) | ||
| TNM staging | 0.009 | 0.926 | ||
| I+II | 61 (56.48) | 48 (55.81) | ||
| III+IV | 47 (43.52) | 38 (44.19) | ||
| History of smoking | 0.017 | 0.895 | ||
| Yes | 58 (53.70) | 47 (54.65) | ||
| No | 50 (46.30) | 39 (45.35) | ||
| History of drinking | 0.216 | 0.642 | ||
| Yes | 63 (58.33) | 53 (61.63) | ||
| No | 45 (41.67) | 33 (38.37) |
Comparison of psychology scores of patients between both groups before and after nursing
There was no obvious difference in SAS and SDS scores of patients between both groups before nursing (P > 0.05). After nursing, the two scores were improved and obviously lower than those before nursing (P < 0.05), and the scores of the IG were markedly lower than those of the CG after nursing (P < 0.05) (Table 2).
Table 2.
Comparison of psychology scores of patients between both groups before and after nursing (mean ± SD)
| Group | Number of columns | SAS score | SDS score | ||
|---|---|---|---|---|---|
|
|
|
||||
| Before nursing | After nursing | Before nursing | After nursing | ||
| Intervention group | 108 | 59.54±5.41 | 35.32±3.17 | 54.67±5.21 | 27.79±2.48 |
| Control group | 86 | 58.73±5.38 | 49.82±4.39 | 55.04±5.17 | 45.33±4.01 |
| t | - | 1.039 | 26.690 | 0.493 | 37.370 |
| P | - | 0.300 | < 0.001 | 0.623 | < 0.001 |
Comparison of pain relief and sleep quality of patients between both groups before and after nursing
There was no remarkable difference in NRS and PSQI scores between both groups before nursing (P > 0.05). After nursing, the two scores were improved and obviously lower than those before nursing (P < 0.05), and the scores of the IG after nursing were markedly lower than those of the CG (P < 0.05) (Table 3).
Table 3.
Comparison of pain relief and sleep quality between both groups before and after nursing (mean ± SD)
| Group | Number of columns | NRS score | PSQI score | ||
|---|---|---|---|---|---|
|
|
|
||||
| Before nursing | After nursing | Before nursing | After nursing | ||
| Intervention group | 108 | 7.32±0.61 | 2.59±0.18 | 9.25±0.85 | 5.53±0.43 |
| Control group | 86 | 7.49±0.63 | 4.16±0.25 | 9.28±0.81 | 8.02±0.79 |
| t | - | 1.900 | 50.800 | 0.249 | 27.970 |
| P | - | 0.059 | < 0.001 | 0.803 | < 0.001 |
Comparison of ESCA scores of patients between both groups before and after nursing
There was no marked difference in health knowledge, self-concept, self-responsibility, self-nursing skills and total score of ESCA between both groups before nursing (P > 0.05), while the total score in the IG after nursing was remarkably higher than that in the CG (P < 0.05) (Figure 1).
Figure 1.
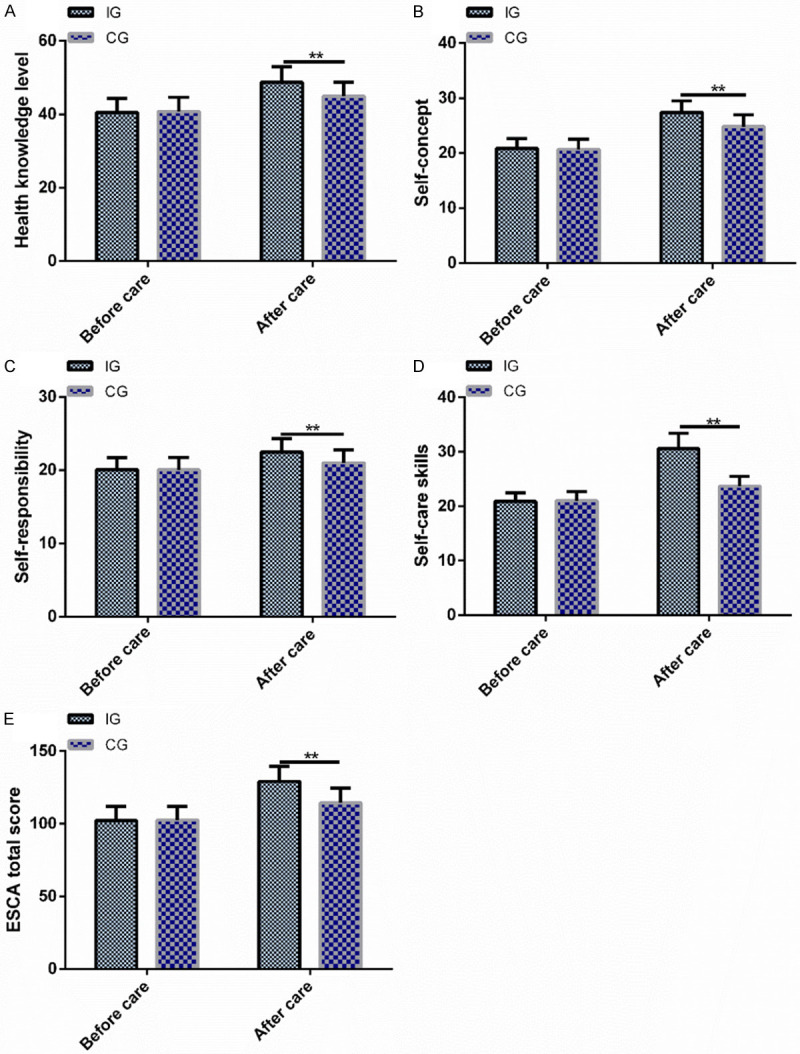
Comparison of ESCA scores of patients between both groups before and after nursing. A. There is no difference in the scores of health knowledge before nursing between both groups, but the scores after nursing in the intervention group are higher than those in the control group. B. There is no difference in the self-concept scores between both groups before nursing, but the scores of the intervention group after nursing are higher than those of the control group. C. There is no difference in the scores of self-responsibility before nursing between both groups, but the scores after nursing in the intervention group are higher than those in the control group. D. There is no difference in the scores of self-nursing skills before nursing between both groups, but the scores after nursing in the intervention group are higher than those in the control group. E. There is no difference in the total score of ESCA before nursing between both groups, but the total score after nursing in the intervention group is higher than that in the control group. Note: * < 0.05 compared with before nursing; # < 0.01 compared with two groups.
Comparison of EORTC QLQ-C30 scores of patients between both groups before and after nursing
There was no difference in scores of pre-nursing body function, emotional function, social function, cognitive function and general health condition between both groups (P > 0.05). After nursing, the improvement of EORTC QLQ-C30 score was markedly better than that before nursing (P < 0.05), and the scores of body function, emotional function, social function, cognitive function and general health condition in the IG after nursing ware markedly higher than those in the CG (P < 0.05) (Figure 2).
Figure 2.
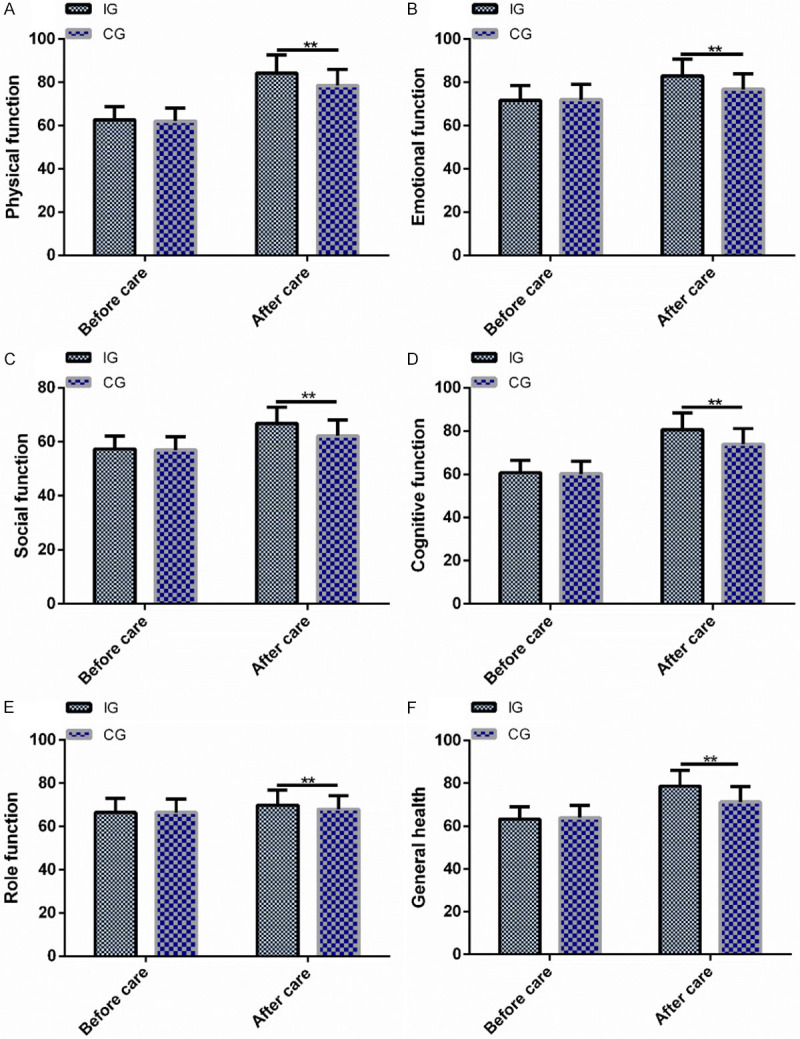
Comparison of EORTC QLQ-C30 scores between both groups before and after nursing. A. There is no difference in the scores of body function before nursing of patients between both groups, but the scores after nursing in the intervention group are higher than those in the control group. B. There is no difference in the scores of emotional function between both groups before nursing, but the scores of the intervention group after nursing are higher than those of the control group. C. There is no difference in the scores of social function between both groups before nursing, but the scores of the intervention group after nursing are higher than those of the control group. D. There is no difference in the scores of self-nursing skills before nursing between both groups, but the scores after nursing in the intervention group are higher than those in the control group. E. There is no difference in the scores of cognitive function between both groups before nursing, but the scores of the intervention group after nursing are higher than those of the control group. F. There is no difference in the scores of general health between both groups before nursing, but the scores of the intervention group after nursing are higher than those of the control group. Note: * < 0.05 compared with before nursing; # < 0.01 compared with two groups.
Comparison of nursing satisfaction evaluation of patients between both groups
After nursing, the total nursing satisfaction of patients in the IG was 91.67%, while that in the CG was 75.58%. The results revealed that the total nursing satisfaction of patients in the IG was obviously higher than that in the CG (P < 0.05) (Table 4).
Table 4.
Comparison of nursing satisfaction evaluation of patients between both groups [n (%)]
| Group | Number of cases | Very satisfied | Satisfied | Dissatisfied | Nursing satisfaction |
|---|---|---|---|---|---|
| Intervention group | 108 | 73 (67.59) | 26 (24.07) | 9 (8.33) | 99 (91.67) |
| Control group | 86 | 28 (32.56) | 37 (43.02) | 21 (24.42) | 65 (75.58) |
| χ2 | - | - | - | - | 9.476 |
| P | - | - | - | - | 0.001 |
Analysis of factors affecting quality of life of advanced GC patients
Comparing the differences of clinical reference and related indicators that affect patients’ quality of life after nursing intervention, we divided their quality of life differences into good prognosis (153 cases) and poor prognosis groups (42 cases). There were no marked differences in gender, tumor size, history of smoking and drinking (P > 0.05), but there were obvious differences in age, lymph node metastasis, TNM stage, negative emotion improvement, lack of self-nursing ability and nursing patterns (P < 0.05). Multivariate Logistic regression analysis showed that age (P=0.009), lymph node metastasis (P=0.008), TNM stage (P=0.006), negative emotion improvement (P=0.001), lack of self-nursing ability (P=0.007), nursing patterns (P=0.007) were the independent risk factors affecting the quality of life of advanced GC patients. Patients with age > 60, lymph node metastasis, TNM stage, unimproved negative emotion, lack of self-nursing ability and routine nursing intervention had increased risk of reduced quality of life (Tables 5, 6 and 7).
Table 5.
Analysis of factors affecting quality of life of advanced GC patients [n (%)]
| Classification | n | Good prognosis group (n=152) | Poor prognosis group (n=42) | t/χ2 value | P value |
|---|---|---|---|---|---|
| Gender | 0.629 | 0.428 | |||
| Male | 105 | 80 (76.19) | 25 (23.81) | ||
| Female | 89 | 72 (80.90) | 17 (19.10) | ||
| Average age | 27.211 | < 0.001 | |||
| 30-60 | 126 | 113 (89.68) | 13 (10.32) | ||
| > 60 | 68 | 39 (57.35) | 29 (42.65) | ||
| Lymph node metastasis | 17.261 | < 0.001 | |||
| Yes | 67 | 41 (61.19) | 26 (38.81) | ||
| No | 125 | 109 (87.20) | 16 (12.80) | ||
| Tumor size (cm) | 0.387 | 0.534 | |||
| < 5 | 98 | 75 (76.53) | 23 (23.47) | ||
| ≥ 5 | 96 | 77 (80.21) | 19 (19.79) | ||
| TNM staging | 5.374 | 0.020 | |||
| I+II | 109 | 92 (84.40) | 17 (15.60) | ||
| III+IV | 85 | 60 (70.59) | 25 (29.41) | ||
| History of smoking | 0.065 | 0.797 | |||
| Yes | 105 | 83 (79.05) | 22 (20.95) | ||
| No | 89 | 69 (77.53) | 20 (22.47) | ||
| History of drinking | 0.157 | 0.692 | |||
| Yes | 116 | 92 (79.31) | 24 (20.69) | ||
| No | 78 | 60 (76.92) | 18 (23.08) | ||
| Improvement of negative emotions | 51.001 | < 0.001 | |||
| Yes | 137 | 126 (91.97) | 11 (8.03) | ||
| No | 57 | 26 (45.61) | 31 (54.39) | ||
| Self-nursing ability | 78.6171 | < 0.001 | |||
| Yes | 157 | 143 (91.08) | 14 (8.92) | ||
| No | 37 | 9 (24.32) | 28 (75.68) | ||
| Nursing mode | 46.261 | < 0.001 | |||
| Holistic nursing | 108 | 104 (96.30) | 4 (3.70) | ||
| Routine nursing | 86 | 48 (55.81) | 38 (44.19) |
Table 6.
Logistic multivariate regression analysis assignment
| Factor | Variable | Assignment |
|---|---|---|
| Age > 60 | X1 | Continuous variable |
| Lymph node metastasis | X2 | Continuous variable |
| TNM staging | X3 | Continuous variable |
| Improvement of negative emotions | X4 | Yes=0; no=1 |
| Self-nursing ability | X5 | Yes=0; no=1 |
| Nursing mode | X6 | Holistic nursing=0, routine nursing=1 |
Table 7.
Multivariate Logistic regression analysis of influencing quality of life of advanced GC patients
| Variable | B | S.E | Wals | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| Age > 60 | 0.167 | 0.063 | 7.433 | 0.009 | 1.183 | 1.068-1.573 |
| Lymph node metastasis | 0.154 | 0.056 | 6.142 | 0.008 | 1.234 | 0.543-2.015 |
| TNM staging | 0.171 | 0.058 | 7.916 | 0.006 | 1.967 | 1.007-3.134 |
| Improvement of negative emotions | 0.573 | 0.176 | 13.683 | 0.001 | 1.753 | 1.278-2.472 |
| Self-nursing ability | 0.435 | 0.324 | 7.542 | 0.007 | 1.434 | 0.345-1.853 |
| Nursing patterns | 1.326 | 0.263 | 25.638 | 0.001 | 4.002 | 2.332-6.884 |
Discussion
GC is one of the most common malignancies found clinically, which not only threatens the life and safety of patients, but also seriously increases their family economic burden [19]. They not only suffer from diseases, but also bear tremendous psychological pressure [20]. With the progress of the disease, patients will have varying degrees of pain, which will have a serious impact on their psychology and sleep quality [21]. Therefore, it is particularly important to give psychological counseling to patients and improve their survival and treatment.
In this research, we adopted holistic nursing intervention in advanced GC patients under the social medical model, and found that patients’ conditions improved obviously. A recent research has shown that [22] cancer patients, especially advanced patients, have a higher incidence of depression, and the aggravation of negative emotions often leads to aggravation of illness or ineffective treatment; thus, psychological intervention is particularly critical. Another study has shown [23] that nursing intervention for patients undergoing GC surgery can improve their emotional and psychological state, which plays an important role in postoperative rehabilitation and prognosis. In this research, the SAS and SDS scores of patients after nursing were observed, and it was found that the two scores of patients in the IG after nursing were obviously lower than those in the CG. This shows that holistic nursing under the social medical model has targeted psychological intervention for patients, thus effectively alleviating their bad emotions, strengthening their enthusiasm for treatment and establishing a strong confidence in treatment. A new study has shown that [24] the peripheral nerve tissue of advanced GC patients easily causes cancer pain of different degrees under the compression of a tumor, which seriously affects health and quality of life. However, giving pain nursing to GC patients can effectively reduce their pain degree and prolong their sleep time, which is beneficial to physiological function recovery [25]. This research showed that the NRS and PSQI scores of patients in the IG were obviously lower than those in the CG after nursing. This revealed that effective nursing intervention could greatly reduce the pain of tumor patients and the physical and mental pain, and improve their sleep quality, thus promoting rehabilitation. A recent study has shown that [26] most patients undergoing gastric esophageal cancer surgery control their symptoms by changing their behavior and lifestyle. This study suggests that the ESCA scores of patients in the IG after nursing intervention are obviously higher than those in the CG, indicating that holistic nursing under the social medical model can help them establish good living conditions and habits, thus improving their self-monitoring and management ability. Hence, they will cooperate more with treatment and intervention, thereby promoting the rehabilitation of the disease.
Quality of life is a characteristic that describes personal subjective well-being, which is divided into psychological and physiological structures, and shows that quality of life is a a vital clinical endpoint [27]. Research shows that [28] the continuity of nursing should be strengthened to meet the health system and information needs of GC patients, so as to promote improvement of symptom management and reduce the negative impact on quality of life. We show that the improvement of EORTC QLQ-C30 score in the IG after nursing is obviously higher than that in the CG, which indicates that holistic nursing under the social medical model can better promote the recovery of the disease, help patients establish a good ability of self-management and good and healthy living habits and maintain a healthy physiological state, thus improving their quality of life. We also compared the recognition and evaluation of patients of the nursing intervention mode. The results showed that the total nursing satisfaction of patients in the IG was markedly higher than that in the CG, indicating that the holistic nursing under the social medical mode met the needs of patients; so, it won a lot of recognition compared with routine nursing. A new study has shown that [29] the quality of life of GC patients is related to their education level, age, disease stage, treatment method and time of diagnosis. In this research, the risk factors affecting patients’ quality of life were analyzed, and the results revealed that those with age > 60, lymph node metastasis, TNM staging, unimproved negative emotions, lack of self-nursing ability and routine nursing intervention increased the risk of lowering their quality of life.
Although this research confirmed that holistic nursing under the social medical model could bring better benefits to advanced GC patients, there is still room for improvement. For instance, we can further analyze the treatment compliance of patients, which will help to measure the treatment efficacy and we will gradually carry out supplementary research from the above perspectives in the days to come.
To sum up, the decline of the quality of life of advanced GC patients’ results from the accumulation of many risk factors; holistic nursing under the social medical model can improve the psychology, self-nursing ability and quality of life of patients.
Disclosure of conflict of interest
None.
References
- 1.Tan Z. Recent advances in the surgical treatment of advanced gastric cancer: a review. Med Sci Monit. 2019;25:3537–3541. doi: 10.12659/MSM.916475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu JY, Lee YC, Graham DY. The eradication of Helicobacter pylori to prevent gastric cancer: a critical appraisal. Expert Rev Gastroenterol Hepatol. 2019;13:17–24. doi: 10.1080/17474124.2019.1542299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo X, Zhao F, Ma X, Shen G, Ren D, Zheng F, Du F, Wang Z, Ahmad R, Yuan X, Zhao J, Zhao J. A comparison between triplet and doublet chemotherapy in improving the survival of patients with advanced gastric cancer: a systematic review and meta-analysis. BMC Cancer. 2019;19:1125. doi: 10.1186/s12885-019-6294-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim YI, Kim YA, Kim CG, Ryu KW, Kim YW, Sim JA, Yun YH, Choi IJ. Serial intermediate-term quality of life comparison after endoscopic submucosal dissection versus surgery in early gastric cancer patients. Surg Endosc. 2018;32:2114–2122. doi: 10.1007/s00464-017-5909-y. [DOI] [PubMed] [Google Scholar]
- 5.Zhang JK, Fang LL, Zhang DW, Jin Q, Wu XM, Liu JC, Zhang CD, Dai DQ. Type D Personality in gastric cancer survivors: association with poor quality of life, overall survival, and mental health. J Pain Symptom Manage. 2016;52:81–91. doi: 10.1016/j.jpainsymman.2015.12.342. [DOI] [PubMed] [Google Scholar]
- 6.Martin AN, Silverstein A, Ssebuufu R, Lule J, Mugenzi P, Fehr A, Mpunga T, Shulman LN, Park PH, Costas-Chavarri A. Impact of delayed care on surgical management of patients with gastric cancer in a low-resource setting. J Surg Oncol. 2018;118:1237–1242. doi: 10.1002/jso.25286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song W, Teng W, Shi X, Liu X, Cui Z, Tian Z. The relationship between RUNX3 expression, nursing strategies and nutritional status in elderly patients with advanced gastric cancer. Iran J Public Health. 2017;46:762–770. [PMC free article] [PubMed] [Google Scholar]
- 8.Smid D, Skalicky T, Fichtl J, Kubackova D, Dolezal J, Novak P, Svoboda T, Slouka D. The influence of palliative chemotherapy on the quality of life of patients with gastric cancer. Klin Onkol. 2016;29:279–286. doi: 10.14735/amko2016279. [DOI] [PubMed] [Google Scholar]
- 9.Huang KS, Wang SH, Chuah SK, Rau KM, Lin YH, Hsieh MC, Shih LH, Chen YH. The effects of hospice-shared care for gastric cancer patients. PLoS One. 2017;12:e0171365. doi: 10.1371/journal.pone.0171365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rajabpour S, Rayyani M, Mangolian Shahrbabaki P. The relationship between Iranian patients’ perception of holistic care and satisfaction with nursing care. BMC Nurs. 2019;18:48. doi: 10.1186/s12912-019-0374-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He XL, Cao ZM. Effect of high-quality nursing intervention on the psychological disorder in patients with gastric cancer during perioperative period: a protocol of systematic review and meta-analysis. Medicine (Baltimore) 2020;99:e20381. doi: 10.1097/MD.0000000000020381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scarpi E, Dall’Agata M, Zagonel V, Gamucci T, Berte R, Sansoni E, Amaducci E, Broglia CM, Alquati S, Garetto F, Schiavon S, Quadrini S, Orlandi E, Casadei Gardini A, Ruscelli S, Ferrari D, Pino MS, Bortolussi R, Negri F, Stragliotto S, Narducci F, Valgiusti M, Farolfi A, Nanni O, Rossi R, Maltoni M Early Palliative Care Italian Study Group (EPCISG) Systematic vs. on-demand early palliative care in gastric cancer patients: a randomized clinical trial assessing patient and healthcare service outcomes. Support Care Cancer. 2019;27:2425–2434. doi: 10.1007/s00520-018-4517-2. [DOI] [PubMed] [Google Scholar]
- 13.Kao YC, Fang WL, Wang RF, Li AF, Yang MH, Wu CW, Shyr YM, Huang KH. Clinicopathological differences in signet ring cell adenocarcinoma between early and advanced gastric cancer. Gastric Cancer. 2019;22:255–263. doi: 10.1007/s10120-018-0860-8. [DOI] [PubMed] [Google Scholar]
- 14.Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res. 2020;133:110102. doi: 10.1016/j.jpsychores.2020.110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karkkainen J, Selander T, Purdy M, Juvonen P, Eskelinen M. Patients with increased levels of the oxidative stress biomarker SOD1 appear to have diminished postoperative pain after midline laparotomy: a randomised trial with special reference to postoperative pain score (NRS) Anticancer Res. 2018;38:1003–1008. doi: 10.21873/anticanres.12315. [DOI] [PubMed] [Google Scholar]
- 16.Huang Y, Zhu M. Increased global PSQI score is associated with depressive symptoms in an adult population from the United States. Nat Sci Sleep. 2020;12:487–495. doi: 10.2147/NSS.S256625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guo L, Soderhamn U, McCallum J, Ding X, Gao H, Guo Q, Liu K, Liu Y. Testing and comparing two self-care-related instruments among older Chinese adults. PLoS One. 2017;12:e0182792. doi: 10.1371/journal.pone.0182792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Musoro JZ, Sodergren SC, Coens C, Pochesci A, Terada M, King MT, Sprangers MAG, Groenvold M, Cocks K, Velikova G, Flechtner HH, Bottomley A Eortc Quality of Life G-iG. Minimally important differences for interpreting the EORTC QLQ-C30 in patients with advanced colorectal cancer treated with chemotherapy. Colorectal Dis. 2020 doi: 10.1111/codi.15295. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Lee JE, Shin DW, Lee H, Son KY, Kim WJ, Suh YS, Kong SH, Lee HJ, Cho B, Yang HK. One-year experience managing a cancer survivorship clinic using a shared-care model for gastric cancer survivors in Korea. J Korean Med Sci. 2016;31:859–865. doi: 10.3346/jkms.2016.31.6.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim GM, Kim SJ, Song SK, Kim HR, Kang BD, Noh SH, Chung HC, Kim KR, Rha SY. Prevalence and prognostic implications of psychological distress in patients with gastric cancer. BMC Cancer. 2017;17:283. doi: 10.1186/s12885-017-3260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen Z, Liu H, Wang H, Wu C, Feng H, Han J. Effect of low-frequency rotary magnetic fields on advanced gastric cancer: survival and palliation of general symptoms. J Cancer Res Ther. 2018;14:815–819. doi: 10.4103/jcrt.JCRT_991_17. [DOI] [PubMed] [Google Scholar]
- 22.Ina K, Sugiyama A, Yuasa S, Koga C, Yamazaki E, Katayama Y, Nagaoka M, Nagao S. Depression screening test for patients with metastatic gastric and colorectal cancer. Gan To Kagaku Ryoho. 2010;37:1059–1063. [PubMed] [Google Scholar]
- 23.Jiang Y, Liu T. Effect of operating room care combined with home care for the postoperative rehabilitation and prognosis of gastric cancer patients with low PTEN gene expression. Oncol Lett. 2017;14:2119–2124. doi: 10.3892/ol.2017.6401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chau I, Fuchs CS, Ohtsu A, Barzi A, Liepa AM, Cui ZL, Hsu Y, Al-Batran SE. Association of quality of life with disease characteristics and treatment outcomes in patients with advanced gastric cancer: exploratory analysis of RAINBOW and REGARD phase III trials. Eur J Cancer. 2019;107:115–123. doi: 10.1016/j.ejca.2018.11.013. [DOI] [PubMed] [Google Scholar]
- 25.Zhang M, Li R, Chen H, Zhou J, Zhang Y. Application and efficacy evaluation of an NBASS-APS pain management model in postoperative analgesia for gastric cancer patients. J BUON. 2018;23:1426–1431. [PubMed] [Google Scholar]
- 26.Eng OS, Kim JY, Ruel N, Raz DJ, Erhunmwunsee L, Melstrom LG, Chao J, Woo Y, Kim J, Sun V. Quality of life, symptoms, and self-management strategies after gastroesophageal cancer surgery. J Pain Symptom Manage. 2018;56:e4–e8. doi: 10.1016/j.jpainsymman.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCall MD, Graham PJ, Bathe OF. Quality of life: a critical outcome for all surgical treatments of gastric cancer. World J Gastroenterol. 2016;22:1101–1113. doi: 10.3748/wjg.v22.i3.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rha SY, Lee HJ, Lee J. Unmet needs in the physical and daily living domain mediates the influence of symptom experience on the quality of life of gastric cancer patients. Support Care Cancer. 2020;28:1419–1431. doi: 10.1007/s00520-019-04954-3. [DOI] [PubMed] [Google Scholar]
- 29.Ngoc Thi Dang D, Ngoc Thi Nguyen L, Thi Dang N, Quang Dang H, Ta TV. Quality of life in vietnamese gastric cancer patients. Biomed Res Int. 2019;2019:7167065. doi: 10.1155/2019/7167065. [DOI] [PMC free article] [PubMed] [Google Scholar]


