Abstract
Objective: To assess the influence of PDCA-based nursing management model on the quality of life (QOL) and complications of patients with acute leukemia undergoing chemotherapy. Methods: In this study, we randomly divided 118 patients with acute leukemia undergoing chemotherapy in our hospital into an observation group (n=59) and a control group (n=59). The control group was implemented routine nursing while the observation group was implemented PDCA-based nursing management. The anxiety, depression, QOL, cancer fatigue, total complication rate, sleep quality, and patients’ satisfaction were compared between the two groups. Results: The SAS and SDS scores of the observation group were significantly lower than those of the control group (P<0.05). The scores of physical function, general health, social function, emotional role, and mental health of the observation group were superior to those of the control group (all P<0.05). The 4 dimensions of behavior/severity, sense, emotion and cognition/mood in the observation group were significantly lower than those of the control group (all P<0.05). The incidence of complications such as nausea and vomiting, infection, bleeding, phlebitis, bone marrow suppression and mucositis in the observation group was significantly lower than that in the control group (P<0.05). The scores of sleep quality in the observation group were significantly lower than those of the control group (all P<0.05). The observation group’s satisfaction with PDCA-based nursing management was markedly higher than that of the control group (P<0.05). Conclusion: The PDCA-based nursing management model applied to patients with acute leukemia undergoing chemotherapy has shown good effects, which can improve depression, anxiety, cancer fatigue, sleep quality and QOL. It also significantly reduced the incidence of complications and improved patients’ satisfaction, which was worth of clinical application.
Keywords: PDCA, nursing management, quality of life, cancer fatigue, complications
Introduction
Acute leukemia is a malignant clonal disease of one or more hematopoietic stem cells. The disease is characterized by abnormal proliferation of primary and naive cells, which inhibits the normal hematopoietic function of the bone marrow and can occur at different ages [1]. The etiology of acute leukemia is complex and unclear, and may be closely related to biological, chemical, genetic, and physical factors [2,3]. Studies have reported that the incidence of leukemia in China is 2.76/100,000 in recent years, showing increasing trend year by year [4]. The onset of the disease is of variety and it is not easy to detect. Patients may present with symptoms such as dizziness, fatigue, pallor, excessive menstruation, bleeding gums, sudden high fever or severe bleeding. When the diseased cells infiltrate into extra medullary organs such as liver, spleen and lymph nodes, it causes enlargement of the corresponding organs, which can be life-threatening if not treated in time [5].
Chemotherapy is the main treatment for acute leukemia, which can destroy the leukemia cell population, control the progression of the disease and relieve clinical symptoms. However, chemotherapy will also kill normal cells, and the adverse effects after the use of a large number of glucocorticoids and immunosuppressive drugs cause physical and mental pain to patients, leading to anxiety, fear, loss and other negative emotions. The psychological stresses may increase patient’s perception of pain and affect their quality of life (QOL) and disease outcomes [6]. Relieving patients’ pain and anxiety, improving their life quality and complications become the focus of acute leukemia.
PDCA management is a quality management model proposed in the field of management in America. It is a management process in which quality management is carried out in four stages: plan, do, check, action, and the cycle goes on and on [7]. The PDCA-based nursing management model is a new nursing model that combines PDCA management with nursing management in order to improve the quality of nursing care and clinical treatment outcomes [8]. There are a few reports on the impact of PDCA-based care management model on the QOL and complications of patients with acute leukemia undergoing chemotherapy at home and abroad, but neglect patients’ cancer fatigue and sleep quality [9]. Therefore, this study focused on the effectiveness of the PDCA-based nursing management model in so as to improve the QOL and to reduce complications of patients with acute leukemia undergoing chemotherapy. In order to provide theoretical guidance for clinical care, we analyzed the effects of the nursing model on patient’s anxiety, depression, cancer fatigue, complications, and satisfaction with nursing.
Materials and methods
General information
In this study, we randomly divided 118 patients with acute leukemia undergoing chemotherapy in Affiliated Hospital of Jiangnan University from March 13, 2019 to July 16, 2020 into an observation group (n=59) and a control group (n=59). Table 1 has shown the basic characteristics of patients in two groups. This study was approved by the medical ethics committee of Affiliated Hospital of Jiangnan University.
Table 1.
Comparison of general baseline data between the two groups of patients (n, %, x̅ ± sd)
| Indexes | Observation group (n=59) | Control group (n=59) | χ2/t | P |
|---|---|---|---|---|
| Age (years) | 56.4±4.1 | 55.6±4.8 | 0.973 | 0.332 |
| Course of disease (years) | 5.6±1.3 | 5.5±0.9 | 0.529 | 0.598 |
| Gender | 0.139 | 0.709 | ||
| Male | 24 | 26 | ||
| Female | 35 | 33 | ||
| Chemotherapy | 0.173 | 0.917 | ||
| IDA | 15 | 17 | ||
| CODP | 26 | 25 | ||
| HA | 18 | 17 | ||
| Comorbidity | ||||
| Hypertension | 11 | 12 | 0.054 | 0.816 |
| Coronary Heart Disease | 9 | 8 | 0.068 | 0.793 |
| Diabetes | 7 | 6 | 0.086 | 0.768 |
| Types of leukemia | 0.034 | 0.854 | ||
| Acute lymphocytic leukemia | 31 | 32 | ||
| Acute myeloid leukemia | 28 | 27 |
The included patients were suffering from acute leukemia diagnosed by the Criteria for Diagnosis and Efficacy of Hematology [10]. They had normal cognitive function. All of the enrolled subjects have agreed to participate in the study and signed informed consent.
Those patients were excluded: patients with a history of chemotherapy or mental illness; patients with vital organ dysfunction; patients with cognitive impairment; patients with other malignant tumors; patients who died during chemotherapy and withdrew from the study.
Methods
The control group received routine care. Before chemotherapy, patients were given routine health education, guided to a light diet, abstained from spicy and stimulating foods. After chemotherapy, patients were given medication and daily care.
The observation group implemented PDCA-based nursing management, which included a number of specific measures [11]. (1) Plan: To avoid the possible complications and catheter shedding of leukemia patients, a nursing plan would be formulated that included education of basic knowledge, psychological nursing methods, PICC intubation care and so on. (2) Do: ① We implemented disease-related health education, which included knowledge of acute leukemia-related pathology, diagnosis and treatment, PICC intubation protection and daily maintenance. ② We provided the knowledge of PICC catheterization management. We instructed patients to observe the condition of the catheter every day, such as blockage, folding, shifting, falling off, especially whether there was any bleeding or leakage at the puncture point, and change the dressing regularly. ③ We would conduct psychological counseling. Before chemotherapy, we tried to eliminate patients’ fears and worries about chemotherapy. After chemotherapy, we comforted the patient that physical discomfort was temporary to reduce patient’s anxiety. ④ Diet intervention referred to guiding the patient to eat scientifically, avoiding high-fat and spicy food, contraindicating tobacco and alcohol. ⑤ Discharge intervention included guiding patients to correctly care for PICC catheters, issuing acute leukemia related health education manuals to guide patients and their families in learning. (3) Check: We would set up a quality control team to conduct regular inspections on each intervention. Existing problems should be promptly raised, analyzed and discussed within the group to study rectification plans. (4) Action: At the end of patient’s treatment, we would conduct a comprehensive evaluation of all measures of the nursing process during the hospitalization period, mainly including PICC placement time, occurrence of complications or adverse events, QOL, quality of sleep, and satisfaction with nursing.
Outcome measures
After implementing systemic nursing, the intervention effects of the two groups were compared.
Main outcome measures
(1) The Self-Rating Anxiety Scale (SAS) was used to assess the status of anxiety between the two groups of patients [12]. The SAS score ≥50 points indicated that there were anxiety symptoms, and its degree became more serious as the score increased. (2) The Self-Rating Depression Scale (SDS) was used to assess the status of depression between the two groups of patients [13]. The degree of depression became more serious as the score increased (53-62 points was considered as mild depression, 63-72 points was considered as moderate depression, >72 points was considered as severe depression). (3) Medical Outcomes Study 36-Item Short-Form (MOS SF-36) was used to compare the QOL of the two groups of patients. The scale included five dimensions of physical function, general health, social function, emotional role, and mental health. The full score of each dimension was 100 points. The higher the score, the higher the QOL in the relevant dimensions was [14]. (4) The Pipers’ Fatigue Scale (PFS) scale was conducted to compare the status of cancer fatigue between the two groups. The scale included 4 dimensions of behavior/severity, sense, emotion and cognition/mood. The degree of cancer fatigue increased with the increase in scores [15]. (5) We compared the occurrence of complications such as nausea, vomiting, infection, bleeding, phlebitis, bone marrow suppression and mucositis between the two groups. If multiple complications occur in the same patient, the multiple complications were counted when calculating the total incidence of complications, that was, the total incidence of complications = the number of complications/total number of cases ×100%.
Secondary outcome measures
(1) The Pittsburgh Sleep Quality Index Rating Scale (PSQI) was conducted to compare the sleep quality of two groups of patients. The higher the score, the worse the sleep quality was [16]. (2) When discharged from the hospital, patients were asked to fill in the self-made satisfaction survey scale of Affiliated Hospital of Jiangnan University (the scale validity coefficient was 0.784, the reliability coefficient was 0.865) to evaluate nursing satisfaction. It was divided into satisfied (90-100 points), basically satisfied (60-89 points), dissatisfied (<60 points). Satisfaction rate = (satisfied + basically satisfied) number of cases/total number of cases × 100%.
Statistical analysis
In this study, SPSS 20.0 was adopted for data statistics. Counting data were presented as (n/%), and the comparison was tested by χ2 test. Measurement data were expressed as the mean ± standard deviation (x̅ ± sd) when conforming to normal distribution. The comparison between groups was tested by the independent-t test, comparison of the composition of grade data between groups was tested by rank sum test. P<0.05 was considered statistically significant.
Results
Comparison of general baseline data between the two groups
No statistically significant difference was discovered in age, course of disease, gender, chemotherapy, comorbidity, and types of leukemia between the two groups of patients (P>0.05), but they were comparable, as shown in Table 1.
Comparison of anxiety between the two groups
The SAS scores of the observation group was lower than that of the control group (48.13±6.38 vs. 52.18±5.68), which was markedly different (t=3.642, P<0.001), as shown in Figure 1.
Figure 1.
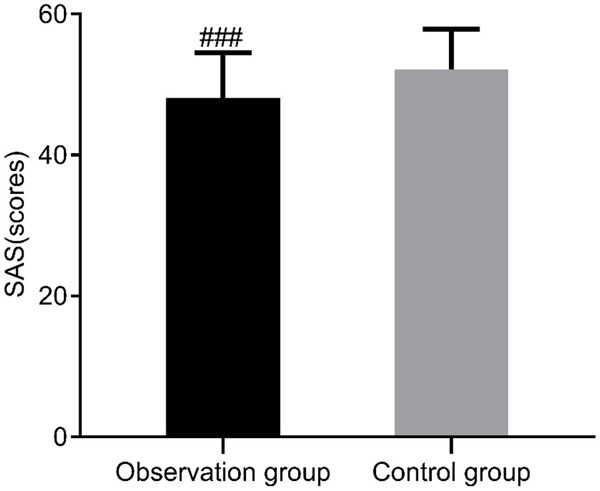
Comparison of SAS scores between the two groups. Compared with the control group, ###P<0.001. SAS: Self-Rating Anxiety Scale.
Comparison of depression in the two groups
The SDS scores of the observation group was lower than that of the control group (48.97±6.07 vs. 54.69±5.98; t=5.156, P<0.001), as shown in Figure 2.
Figure 2.
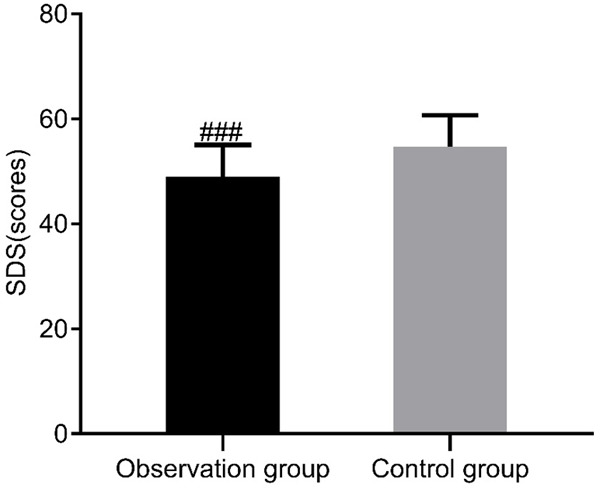
Comparison of SDS scores between the two groups. Compared with the control group, ###P<0.001. SDS: Self-Rating Depression Scale.
Comparison of the QOL of the two groups of patients
The scores of physical function, general health, social function, emotional role, and mental health of the observation group were higher than those of the control group (all P<0.01), as shown in Table 2.
Table 2.
Comparison of quality of life score MOS SF-36 between the two groups (points, x̅ ± sd)
| Quality of life score | Observation group (n=59) | Control group (n=59) | t | P |
|---|---|---|---|---|
| Physical function | 78.20±10.26 | 66.80±8.90 | 6.447 | 0.000 |
| General health | 91.76±10.15 | 85.17±12.21 | 3.188 | 0.002 |
| Social function | 72.34±11.43 | 65.87±10.26 | 3.236 | 0.002 |
| Emotional role | 64.81±9.32 | 55.54±7.29 | 6.018 | 0.000 |
| Mental health | 68.48±10.18 | 57.38±7.01 | 6.898 | 0.000 |
Comparison of cancer fatigue between the two groups
The observation group’s scores of 4 dimensions of behavior/severity, sense, emotion and cognition/mood were lower than those of the control group (all P<0.001), as shown in Table 3.
Table 3.
Comparison of cancer fatigue between the two groups (points, x̅ ± sd)
| Cancer fatigue status | Observation group (n=59) | Control group (n=59) | t | P |
|---|---|---|---|---|
| Behavior/severity | 2.18±0.34 | 5.18±0.94 | 23.053 | 0.000 |
| Sense | 1.94±0.26 | 5.06±0.80 | 28.490 | 0.000 |
| Emotion | 1.82±0.25 | 4.85±0.75 | 29.439 | 0.000 |
| Cognition/mood | 2.13±0.20 | 5.46±0.91 | 27.453 | 0.000 |
Comparison of the incidence of complications between the two groups
In the observation group, there were 4 cases of nausea and vomiting, 3 cases of infection, 3 cases of bleeding, 2 cases of phlebitis, 6 cases of bone marrow suppression, and 3 cases of mucositis. The total incidence of complications in the observation group was 35.59%. In the control group, there were 9 cases of nausea and vomiting, 7 cases of infection, 6 cases of bleeding, 6 cases of phlebitis, 7 cases of bone marrow suppression, and 4 cases of mucositis. The total complication rate of the control group was 66.10%. In the observation group, the total incidence of complications was markedly lower than that in the control group (P<0.01), as shown in Table 4.
Table 4.
Postoperative complications of the two groups of patients (n, %)
| Groups | Observation group (n=59) | Control group (n=59) | χ2 | P |
|---|---|---|---|---|
| Nausea and vomiting | 4 (6.78) | 9 (15.25) | ||
| Infection | 3 (5.08) | 7 (11.86) | ||
| Bleeding | 3 (5.08) | 6 (10.17) | ||
| Phlebitis | 2 (3.39) | 6 (10.17) | ||
| Bone marrow suppression | 6 (10.17) | 7 (11.86) | ||
| Mucositis | 3 (5.08) | 4 (6.78) | ||
| Total incidence of complications | 21 (35.59) | 39 (66.10) | 10.986 | 0.001 |
Comparison of sleep quality between the two groups
The PSQI scores in the observation group were significantly lower than those of the control group (10.97±2.07 vs. 14.69±3.38, t=7.209, P<0.001), as shown in Figure 3.
Figure 3.
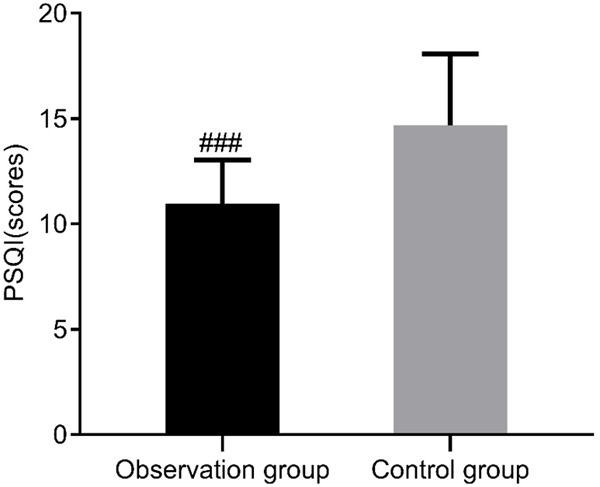
Comparison of PSQI scores between the two groups. Compared with the control group, ###P<0.001. PSQI: Pittsburgh Sleep Quality Index Rating Scale.
Comparison of patient care satisfaction between the two groups
In the observation group, 32 patients were satisfied with continuity care, 23 were basically satisfied, and 4 were dissatisfied. The satisfaction of the observation group was 93.22%. In the control group, 24 patients were satisfied with continuation care, 23 were basically satisfied, and 11 were dissatisfied. The satisfaction rate of the control group was 79.66%. The satisfaction rate of patients in the observation group with continuity care was significantly superior to that in the control group (P<0.05), as shown in Table 5.
Table 5.
Comparison of nursing satisfaction between the two groups of patients (n, %)
| Groups | Satisfied | Basically satisfied | Dissatisfied | Satisfaction rate |
|---|---|---|---|---|
| Observation group (n=59) | 32 (54.24) | 23 (38.98) | 4 (6.78) | 55 (93.22) |
| Control group (n=59) | 24 (40.68) | 23 (38.98) | 12 (20.34) | 47 (79.66) |
| χ2 | 4.627 | |||
| P | 0.031 | |||
Discussion
The PDCA (Plan, Do, Check, Action) cycle was a scientific quality management method, which was proposed by American quality management expert Deming in the 19-50s. It had standardized and scientific features that could promote the spiral improvement of quality level [17,18]. In recent years, since the PDCA cycle management method was introduced into the medical field, it had been widely used in the postoperative care management of cancer and surgical diseases. It had achieved good practical results and improved the prognosis of patients and the quality of care [19,20].
Patients with acute leukemia often suffered from anxiety and depression, which were the most common psychological stress reactions of patients. Jiang Xiaoling et al. took 120 patients with hypertensive as the study subjects [21]. The control group was delivered traditional nursing intervention while the observation group was implemented the PDCA cycle method for the nursing intervention. The study found that the observation group had significantly lower SAS and SDS scores than the control group. In the current study, the observation group was given a PDCA-based nursing management model and compared with the control group that was delivered a traditional nursing model. The results showed that the SAS and SDS scores of the observation group were lower than those of the control group, indicating that the PDCA-based nursing management model could reduce patients’ anxiety, improve their mental and emotional state.
PDCA-based nursing management model was important to improve patients’ QOL and reduce the complication rate. Lu et al. randomly divided 96 patients with acute leukemia into an observational group and a control group [9]. The control group was delivered routine care while the observation group implemented a PDCA-based nursing management model. The study concluded that the PDCA-based nursing management model was beneficial to improve the QOL and reduce the incidence of complications. In the current study, the QOL of the two groups of participants was evaluated by the MOS SF-36 scale. It was found that the observational group had significantly higher scores than the control group in each dimension of physical function, general health, social function, emotional role, and mental health, suggesting that the patients in the observation group had better QOL, which was consistent with the above findings. In addition, the complication rate of the observation group was lower than that of the control group, which may be due to the implementation of a PDCA-based care management model. It managed the risk of complications and adverse events after PICC placement by addressing the status of catheter use, the puncture point and the puncture vein, which was consistent with the above findings.
Cancer fatigue is one of the common symptoms of clinical malignant tumors. Caused by tumors or anti-tumor treatments, it is a disturbing, persistent status of physical, emotional and/or cognitive subjective fatigue and energy exhaustion. It interferes with daily life and functions, and the symptoms are non-specific weakness, weakness, general decline, lethargy, and fatigue. Patients with acute leukemia undergoing chemotherapy are often accompanied by fatigue, the incidence of which is about 75% to 96%, and the degree of fatigue is aggravated by the adverse reactions of chemotherapy [22]. In the current study, cancer-related fatigue was assessed in two groups of subjects through the PFS scale, and it was found that the behavior/severity, sense, emotion and cognition/mood dimensions scores were markedly lower in the observation group than in the control group, which was consistent with the above findings. This may be due to the fact that the observation group took appropriate exercises and activities, playing soothing music and so on to help patients relieve fatigue. In addition, the scores of sleep quality of the observation group were lower than those of the control group, indicating that the sleep quality of the observation group was better than that of the control group, once again proving the advantages of the PDCA-based care management model.
Finally, the current study also examined the nursing satisfaction of the two groups of patients during hospitalization, and found that the nursing satisfaction of the observation group was significantly superior to that of the control group. This may be because the PDCA-based nursing management model reduced patients’ anxiety and depression, improved patients’ sleep quality and QOL, reduced the incidence of complications, improved cancer fatigue, and patients have a better subjective experience in medical treatment. However, this study did not pay attention to negative emotions of the main caregivers. In the later stage, a large sample of long-term care effect research should be carried out to confirm the feasibility and importance of the PDCA-based nursing management model in patients with acute leukemia.
In summary, the PDCA-based nursing management model applied to patients with acute leukemia undergoing chemotherapy had better effects, which can improve patients’ depression, anxiety, cancer fatigue, sleep quality, and QOL. It also significantly reduced the occurrence of complications and improved patient satisfaction, which was worth of clinical application.
Disclosure of conflict of interest
None.
References
- 1.Ling Y, Xie Q, Zhang Z, Zhang H. Protein kinase inhibitors for acute leukemia. Biomark Res. 2018;6:8. doi: 10.1186/s40364-018-0123-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nichol JN, Assouline S, Miller WH. The etiology of acute leukemia. In: Wiernik P, Goldman J, Dutcher J, Kyle R, editors. Neoplastic diseases of the blood. New York: Springer; 2013. pp. 177–198. [Google Scholar]
- 3.Hu XX, Wang JM. Accurate treatment of acute myeloid leukemia: a new focus. J Second Mil Med Univ. 2018;39:465–468. [Google Scholar]
- 4.de Haas V, Ismaila N, Zhang L. Initial diagnostic workup of acute leukemia: ASCO clinical practice guideline endorsement summary of the CAP and ASH guideline. J Oncol Pract. 2019;15:101–105. doi: 10.1200/JOP.18.00613. [DOI] [PubMed] [Google Scholar]
- 5.Habringer S, Lapa C, Herhaus P, Schottelius M, Istvanffy R, Steiger K, Slotta-Huspenina J, Schirbel A, Hänscheid H, Kircher S, Buck AK, Götze K, Vick B, Jeremias I, Schwaiger M, Peschel C, Oostendorp R, Wester HJ, Grigoleit GU, Keller U. Dual targeting of acute leukemia and supporting niche by CXCR4-directed theranostics. Theranostics. 2018;8:369–383. doi: 10.7150/thno.21397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krull K, Kunstreich M, Bronsema A, Bleckmann K, Classen CF, Erdlenbruch B, Jorch N, Kolb R, Leipold A, Moser O, Prokop A, Scheurlen W, Steinbach D, Klasen-Sansone J, Klee D, Escherich G, Moericke A, Schrappe M, Borkhardt A, Kuhlen M. Osteonecrosis in children with acute lymphoblastic leukemia at initial diagnosis and prior to any chemotherapy. Leuk Lymphoma. 2019;60:78–84. doi: 10.1080/10428194.2018.1466292. [DOI] [PubMed] [Google Scholar]
- 7.Jiang Q, Zhang D, Majaw J, Zhao C, Chai Y, Xu Z, Wang R, Li X, Zou C, Huang L, Wu H, Hu P, Xiang P, Chen Q, Ma W, Zheng Z, Sun J, Liu T, Li W. Minimization of the perianal infection rate of hematological malignancies with agranulocytosis by quality control circle activity and patient-hospital-student win-win concept. J Int Med Res. 2018;46:2338–2345. doi: 10.1177/0300060517726863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wei W, Wang S, Wang H, Quan H. The application of 6S and PDCA management strategies in the nursing of COVID-19 patients. Crit Care. 2020;24:443. doi: 10.1186/s13054-020-03124-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lu XL, Yang ML, Chen CX, Zhang Y. Application of PDCA-based nursing management model in patients with acute leukemia undergoing chemotherapy. Chin J Mod Nurs. 2018;24:4428–4432. [Google Scholar]
- 10.Zhang ZN, Shen T. In: Diagnosis and treatment criteria for blood diseases. Zhang ZN, Shen T, editors. Beijing: China Science Press; 2007. [Google Scholar]
- 11.Zhu QH, Zhang Q, Zhang Y, Yang WP, Hu D, Du Y, Liao XQ, Li YP, Tan YL, Song ZF. A systematic review of the effect of PDCA nursing management in patients with leukemia undergoing PICC. J Clin Pathol. 2019;039:142–151. [Google Scholar]
- 12.Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry. 2017;17:329. doi: 10.1186/s12888-017-1489-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hunter EE, Murphy M. Zung Self-Rating Depression Scale. In: Kreutzer JS, DeLuca J, Caplan B, editors. Encyclopedia of Clinical Neuropsychology. New York: Springer; 2011. [Google Scholar]
- 14.Vitorino DFdM, Martins FLM, Souza ADC, Galdino D, Prado GFD. Utilizao do SF-36 em ensaios clínicos envolvendo pacientes fibromiálgicos: determinao de critérios mínimos de melhora clínica. Revista Neurociências. 2019;12:147–151. [Google Scholar]
- 15.Gledhill JA, Rodary C, Mahé C, Laizet C. French validation of the revised piper fatigue scale. Rech Soins Infirm. 2002:50–65. [PubMed] [Google Scholar]
- 16.Sun DL. Sinusitis-specific quality of life scale to evaluate the efficacy of chronic sinusitis after endoscopic sinus surgery. World Clinic Med. 2017;11:81, 83. [Google Scholar]
- 17.Wang WX, Zhang YY, Zhang XY, Yuan H. Application progress of PDCA cycle in nursing management. Chin J Mod Nurs. 2015;21:370–372. [Google Scholar]
- 18.Li C, Wang C, Liu CF, Zhang N, Ding J. The effect of PDCA-based nursing management in patients with stem cell transplantation complicated by oral mucositis. Chin J Mod Nurs. 2020;26:1486–1490. [Google Scholar]
- 19.Han JZ, Amina QH, Aiguli M, Yu XY. The effect of PDCA cyclic nursing management on secondary infection and self-efficacy in elderly patients with advanced lung cancer chemotherapy. China Med Herald. 2017:160–162. [Google Scholar]
- 20.Ye J, Yang Q, Liu DY. The application of PDCA cyclic nursing management model in the nursing of patients with cervical spine surgery. J Pract Clin Med. 2017;21:85–87. [Google Scholar]
- 21.Jiang XL. The effect of PDCA circulation method on blood pressure, anxiety, depression and self-efficacy in patients with essential hypertension. Lingnan J Cardiovasc Dis. 2018;v.24:100–102. [Google Scholar]
- 22.Lv L. Focus on solving the impact of nursing model on the poor mental state and coping styles of leukemia patients undergoing chemotherapy and cancer-related fatigue. Med clin Res. 2017;34:1036–1038. [Google Scholar]


