Abstract
Objective: The purpose of this study was to compare the effects of continuous intravenous infusions (CII) of fentanyl by pumping and ultrasound-guided continuous femoral nerve block (CFNB) with ropivacaine in terms of analgesic effects and postoperative cognitive function following total knee arthroplasty. Methods: The clinical data of 103 patients who underwent total knee arthroplasty were collected retrospectively and divided into group A (n = 51) receiving CII of fentanyl by pumping and group B (n = 52) receiving CFNB with ropivacaine. Mini-Mental State Examination (MMSE) scores, Visual analog scale (VAS) scores, knee joint flexion angle (KJFA), muscle strength, postoperative cognitive dysfunction (POCD), patient satisfaction, and adverse reactions of the two groups were compared. Results: The muscle strength scores in group B gradually improved at 6-48 h as compared with at 4 hours after operation (P < 0.05). Compared with group A, patients in group B had greater active motion of KJFA at 4, 6, and 12 h after operation (P < 0.05). In contrast to group A, patients in group B had lower VAS scores at rest or active and passive motion at 4-48 h after operation (P < 0.05). The MMSE scores of group B were higher than those of group A at 1, 4, and 7 d after operation (P < 0.05). The incidence of POCD at 4 d after operation was 1.92% in group B, lower than that of 15.69% in group A (P < 0.05). The incidence of adverse reactions was 5.77% in group B, lower than that of 29.41% in group A (P < 0.05). The satisfaction scores of group B were higher than those of group A (P < 0.05). Conclusion: Compared with CII of fentanyl by pumping, ultrasound-guided CFNB showed superior analgesic effects following total knee arthroplasty, which should reduce the incidence of POCD and adverse reactions.
Keywords: Ultrasound guidance, ropivacaine, continuous femoral nerve block, continuous infusion of fentanyl, total knee replacement, postoperative analgesia
Introduction
Osteoarthritis is a major orthopedic challenge that needs to be resolved in China. In recent years, the number of patients fracture caused by osteoarthritis has increased dramatically [1]. Patients with osteoarthritis are often accompanied by varying degrees of joint dysfunction, affecting the normal work and life of patients [2]. Total knee arthroplasty is one of the common surgical options for this type of fracture. Artificial knee prosthesis can replace the severely injured knee joint, eliminate pain, correct deformity, and effectively stabilize the affected limb to promote recovery [3].
Studies have shown that although total knee arthroplasty is an ideal treatment for knee osteoarthritis, 60% patients will experience severe postoperative pain, seriously affecting functional exercise and knee mobility [4,5]. The efficacy of knee osteoarthritis depends not only on surgical skills but also on postoperative rehabilitation exercises [6]. Therefore, it is essential to reduce postoperative pain and promote postoperative functional exercise for successful implementation of total knee arthroplasty [7]. Peripheral nerve block is a type of regional anesthesia. The anesthetic is injected near a specific nerve or bundle of nerves to block sensations of pain from a specific area of the body and exerts the anesthetic effects [8]. Nerve block is also widely used in analgesia after total knee arthroplasty, and the nerve stimulator during anesthesia improves the success rate of nerve block. However, this analgesic method also has some limitations, that is, it is difficult to directly observe the nerve structure, and the accuracy needs to be further improved. Other problems, such as incomplete analgesia and nerve damage, may also occur [10]. Therefore, continuous femoral nerve block (CFNB) under the guidance of ultrasound was popularized in clinical practice. Due to its strong ultrasonic penetration ability, good directivity and high resolution ultrasonic detection is widely applied with CFNB, improving the accuracy of nerve positioning and producing relatively ideal analgesic effects [11].
Effective analgesia is an essential part of postoperative management following total knee arthroplasty. Fentanyl is commonly prescribed as a slow-release patch for patients with chronic severe pain. In this study, its analgesic effects were compared for the first time with those of ropivacaine.
Materials and methods
Clinical data
The clinical data of 103 patients underwent total knee arthroplasty in our hospital were collected retrospectively and divided into two groups according to the analgesic method. The postoperative analgesic methods of group A (n = 51) and group B (n = 52) were continuous intravenous infusions (CII) of fentanyl by pumping and ultrasound-guided CFNB with ropivacaine, respectively. (1) Inclusion criteria: patients without contraindications for the surgical treatment and anesthetic drugs in this study; literal comprehension and reading ability; without coagulation dysfunction; with knee joint disease but without valgus knee deformity. This study was obtained approval of medical ethics committee. All patients signed the informed content. (2) Exclusion criteria: patients lack of clinical data; accompanied by severe respiratory diseases; low compliance; absolute surgical contraindications; presence of coagulopathy; preoperative neurological dysfunction and chronic pain.
Methods
Both groups were treated with general anesthesia by combined inhalation and intravenous anesthesia. The postoperative analgesia methods of groups A and B were continuous intravenous infusions (CII) of fentanyl by pumping and ultrasound-guided CFNB with ropivacaine.
Group A: 1.0 mg fentanyl (H20123297, National Pharmaceutical Group Industry Co., Ltd. Langfang Branch, 2 ml:0.1 mg) was added in 100 ml 0.9% sodium chloride injection (H20041076, Hebei Tiancheng Pharmaceutical Co., Ltd., 250 ml), which was injected into the disposable infusion pump. Patients received continuous pumping at 2 ml/h for 2 d.
Group B: At the end of the operation, ultrasound-guided CFNB with ropivacaine was performed. 200 ml of 0.2% ropivacaine hydrochloride injection (Guo Zhunzi) was added to the disposable infusion pump (200 ml) (H20173193, Guangdong Jiabo Pharmaceutical Co., Ltd., 20 ml:150 mg). The constant pumping speed was controlled at 4 ml/h. Under supine position and affected arm abducted 15°, femoral nerve block was performed using the color Doppler ultrasound diagnostic instrument. The skin puncture procedure was conducted at the site of puncture. The position of the inguinal ligament was determined, and the ultrasound transducer was placed 2 cm below the inguinal ligament. The position of femoral artery was explored and the ultrasound transducer was moved left and right, up and down until the cross-section of the femoral nerve, femoral artery and femoral vein could be clearly observed in the ultrasound image. By in plane needle approach, the needle was placed in line with and parallel to the transducer and advanced slowly toward the inside, and finally to the femoral nerve. Blood aspiration was observed. A small amount of 0.9% sodium chloride solution was injected to carefully observe the water separation. If physiological saline had diffused along the femoral nerve, 15 ml of 0.2% ropivacaine could be infused. The space around the femoral nerve was treated with hydro dissection technique. When the femoral nerve appeared to “float”, the catheter was placed in the position of the femoral nerve. The 0.9% sodium chloride solution was injected again through the catheter and the diffusion was carefully observed. If the fluid around the femoral nerve continued to diffuse, the catheter could be fixed and the disposable infusion pump could be connected. If a satisfactory diffusion effect was not observed, the catheter position could be adjusted and tried again, and then fixed the catheter and connected it with a disposable infusion pump. The infusion rate was controlled to 4 m/h for 2 d.
Observation measurement
(1) Muscle strength of affected limbs [12]: The muscle strength scores of the affected limbs were measured at postoperative 4 h, 6 h, 12, 24, and 48 h. In a supine position, the patients were instructed to flex knee joints of the affected limbs, and straighten them towards the back. Resistance was applied to carefully observe the strength of the quadriceps muscles. 0 points: the muscles are completely not moving or contracting; 1 point: muscle contraction can be observed without motion; 2 points: patients can move horizontally on the bed without anti-gravity; 3 points: anti-gravity without no resistance; 4 points: weak resistance; 5 points: normal muscle strength.
(2) Active motion of knee joint flexion angle (KJFA) [13]: The KJFA of the affected limbs in the two groups was evaluated at 4 h, 6, 12, 24, and 48 h after surgery. When in the flexed state, the knee joint was used as the axis, and the angle between the extension line of the front of the femur and the shank (posterior).
(3) Analgesic effect [14]: The analgesic effects of patients at rest, active, and passive motions were evaluated at 4, 6, 12, 24, and 48 h after surgery, covering 0-10 pozints. Severity of pain was proportional to the score.
(4) Mini-Mental State Examination (MMSE) score [15]: The cognitive function of the two groups was assessed on the 1, 4 and 7 d after surgery, including orientation to time, orientation to place, attention and calculation, and language, with a total score of 0-30 points. A score of 20 to 24 suggests mild dementia, 13 to 20 suggests moderate dementia, and less than 12 indicates severe dementia.
(5) The incidence of postoperative cognitive dysfunction (POCD) [16]: The incidence of POCD at 1, 4, and 7 d after surgery. POCD evaluation standard: MMSE score < 23 points.
(6) Incidence of adverse reactions in two groups.
(7) Satisfaction scores: The evaluation items included professionalism of medical service and attitude. The total score is 100 points. High scores denote high satisfaction.
Statistical analysis
SPSS 22.0 was used for data analysis. The measurement data were expressed as mean ± standard deviation (mean ± SD). The t test was used for data with normal distribution, and the Mann-Whitney U test was used for data that did not met normal distribution. Count data [n (%)] were compared by X 2 test. Graphpad software was used for plot drawing. P < 0.05 indicated significant differences.
Results
Comparison of baseline data
There was no statistically significant difference in sex ratio, age, BMI, and disease type between the two groups (P > 0.05) (Table 1).
Table 1.
Comparison of baseline data [n (%)]/(x̅ ± s)
| Data | Group A (n = 51) | Group B (n = 52) | t/X2 | P | |
|---|---|---|---|---|---|
| Gender (Case) | Male | 29 (56.86) | 32 (61.54) | 0.233 | 0.629 |
| Female | 22 (43.14) | 20 (38.46) | |||
| Age | 68.52 ± 2.18 | 68.59 ± 2.11 | 0.181 | 0.857 | |
| BMI (kg/m2) | 24.15 ± 0.15 | 24.19 ± 0.38 | 0.766 | 0.456 | |
| Disease type | |||||
| Traumatic arthritis | 20 (39.22) | 19 (36.54) | 0.015 | 0.859 | |
| Rheumatoid arthritis | 16 (31.37) | 17 (32.69) | |||
| Osteoarthritis | 15 (29.41) | 14 (26.92) | |||
Comparison of the muscular strength of the affected limb and KJFA
Compared with group A, group B had higher muscle strength scores and greater active motion of KJFA at multiple time-point after surgery (P < 0.05). The muscle strength scores and active motion of KJFA gradually increased at 4-48 h after surgery (P < 0.05) (Figure 1).
Figure 1.
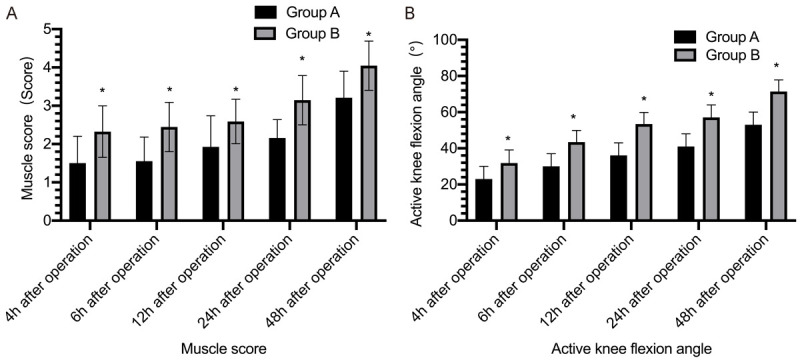
Comparison of the muscle strength score and the active motion of knee flexion angle of the affected limbs. A: Patients in group B (ropivacaine) all had higher scores of muscle strength in the affected limb at 4, 6, 12, 24, and 48 h, P < 0.05. B: Patients in group B had greater active motion of KJFA than that of group A at 4, 6, 12, 24, and 48 h after surgery. *Compared with group A, P < 0.05.
Comparison of postoperative analgesia
In contrast to group A, patients in group B had lower VAS scores at rest or under active and passive motions during 4-48 h after surgery (P < 0.05) (Figure 2).
Figure 2.
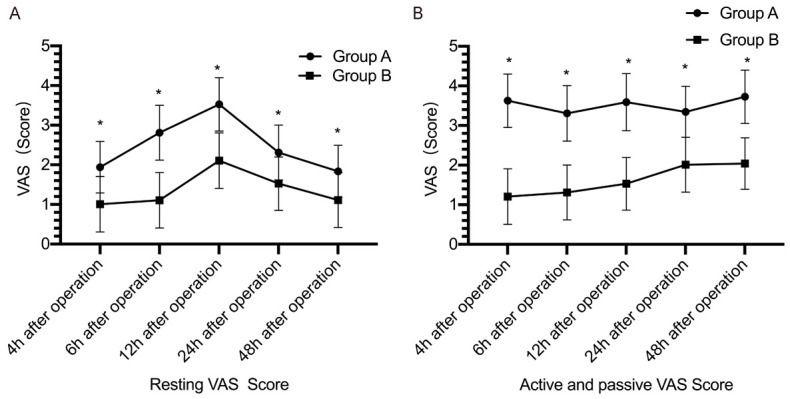
Comparison of the postoperative analgesia effect between the two groups. A: VAS scores at rest of patients in group B (ropivacaine) at 4-48 h after surgery were lower than those in group A (fentanyl), P < 0.05; B: VAS scores at active and passive motion of patients in group B at 4-48 h after surgery were lower than those in group A, P < 0.05. *Compared with group A, P < 0.05.
Comparison of incidence of POCD and adverse reactions
The incidence of POCD in group B at 1 d and 4 d after surgery was lower than that in group A (P < 0.05). There was no significant difference in the incidence of POCD at 7 days after surgery between the two groups (P > 0.05) (Table 2). Group A had 3 cases of hypoxia, 4 cases of vomiting, 5 cases of nausea and 3 cases of urinary retention, with the incidence of adverse reactions of 29.4%. Group B had 1 case of hypoxia, 1 case of vomiting, 1 case of nausea and 0 case of urinary retention, with the incidence of adverse reactions of 5.77%. The incidence of adverse reactions in group B was lower than that in group A (P < 0.05) (Table 3).
Table 2.
Comparison of the incidence of postoperative POCD between the two groups [n (%)]
| Group | Number of cases | 1 d after operation | 4 d after operation | 7 d after operation |
|---|---|---|---|---|
| Group A, fentanyl | 51 | 16 (31.37) | 8 (15.69) | 0 (0.00) |
| Group B, ropivacaine | 52 | 2 (3.82)* | 1 (1.92)* | 0 (0.00) |
| X2 | 13.638 | 4.797 | - | |
| P | 0.000 | 0.029 | - |
indicates comparison with group A, P < 0.05.
Table 3.
Comparison of the incidence of adverse reactions between the two groups [n (%)]
| Group | Number of cases | Hypoxia | Vomiting | Nausea | Urinary retention | Total |
|---|---|---|---|---|---|---|
| Group A, fentanyl | 51 | 3 (5.88) | 4 (7.84) | 5 (9.80) | 3 (5.88) | 15 (29.41) |
| Group B, ropivacaine | 52 | 1 (1.92) | 1 (1.92) | 1 (1.92) | 0 (0.00) | 3 (5.77)* |
| X2 | ||||||
| P |
indicates comparison with group A, P < 0.05.
Comparison of postoperative MMSE scores and satisfaction scores
The MMSE scores of group B patients were (26.98 ± 1.05) points, (25.96 ± 1.88) points, (27.98 ± 2.29) points at 1, 4, and 7 d respectively after surgery, which were higher than those in group A (P < 0.05) (Figure 3). The patient satisfaction score of group B was (95.68 ± 2.88), which was higher than (75.12 ± 2.36) of group A (P < 0.05) (Table 4).
Figure 3.
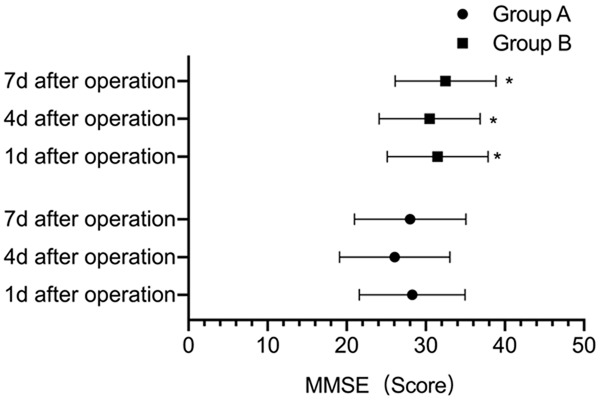
Comparison of postoperative MMSE scores of the two groups. The MMSE scores of group B (ropivacaine) patients were higher than those of group A (fentanyl) at 1, 4, and 7 d after operation, P < 0.05. *Compared with group A, P < 0.05.
Table 4.
Comparison of patient satisfaction scores between the two groups (x̅ ± s)
| Grouping | Satisfaction score |
|---|---|
| Group A, fentanyl (n = 51) | 75.12 ± 2.36 |
| Group B, ropivacaine (n = 52) | 95.68 ± 2.88* |
| t | 39.586 |
| P | 0.000 |
indicates comparison with group A, P < 0.05.
Discussion
The knee joint is one of the most complex joints in the human body and plays a key role in physical activities [17]. The knee joint has a great degree of mobility. Joint range of motion decreases with increasing age and it can easily be injured, leading to high incidence of knee diseases [18]. Total knee arthroplasty is one of the important surgical options for the clinical treatment of end-stage knee disease. Although it can obtain the ideal efficacy, postoperative pain is an important problem that needs to be solved urgently [19].
Postoperative pain is one of the common symptoms after total knee replacement. Without timely intervention, it can eventually develop into neuropathic and chronic pain [20]. Postoperative pain is a typical example of acute pain, which can lead to unpleasant feelings and can be easily ignored. Postoperative pain will also make the body’s metabolism and endocrine disorder, increase the patient’s pain, and affect the postoperative recovery effect [21]. Total knee arthroplasty has a large surgical trauma. Ligament and meniscus resection, tibial and femoral osteotomy may cause postoperative pain, seriously affecting the physical and mental health of patients [22]. Therefore, a high-quality postoperative pain management is necessary. Continuous epidural analgesia and venous analgesia (including continuous venous analgesia and venous self-controlled analgesia) are two traditional methods of analgesia after total knee replacement. Although continuous venous analgesia is simple to operate, it will seriously affect the affected limb. Although muscle strength and intravenous self-controlled analgesia can adjust the analgesic dose and time, they are very prone to drug dependence [23]. Continuous epidural analgesia has satisfactory analgesic effect, but it tends to cause adverse reactions such as urinary retention and hypotension, which limits its clinical application. In view of this, this study used ultrasound-guided CFNB with ropivacaine and compared its analgesic effect with continuous pumping of fentanyl. The results showed that patients in group B exhibited lower VAS scores than those in group A (P < 0.05), suggesting that ultrasound-guided CFNB with ropivacaine showed effective analgesia effects after total knee replacement. The reason may be that ropivacaine is a long-acting amide local anesthetic agent. It has lower incidence of motor block and fewer cardiovascular side effects, showing low toxicity [24]. It achieves successful nerve block, improving the pain and presenting ideal analgesic effects. Secondly, under the nerve block mode, drugs can directly act on the nerves, thereby exerting a blocking effect and achieving the ideal analgesic effect. Compared with the previous positioning of anatomical landmarks, the positioning accuracy under ultrasound guidance is higher, and the procedures can be played back. Next, ultrasound probe was used to monitor the entire anesthesia process to better determine the correlation between the femoral nerve and the surrounding tissues and blood vessels, which is beneficial to relieve pain [25]. Second, patients in group B had higher muscle strength scores and patient satisfaction at 6, 12, 24, and 48 h after surgery than those in group A, and the active motion of KJFA of affected limbs were all greater than those in group A (P < 0.05), which further confirmed the effectiveness of ultrasound-guided CFNB with ropivacaine. With expected analgesic effects of ultrasound-guided CFNB with ropivacaine, the muscle strength of the affected limb and knee function were less affected, promoting the rapid recovery of knee function and improving patient satisfaction.
POCD is postoperative cognitive dysfunction, which is one of the complications of the central nervous system, and mainly manifested as limited social function, personality changes, motor dysfunction, reduced concentration, impaired memory and confusion [26]. The MMSE scale is a common clinical method to evaluate postoperative cognitive dysfunction. The advantages of the MMSE include requiring no specialized equipment or training for administration. Due to its short administration period and ease of use, it is useful for cognitive assessment in the clinician’s office space or at the bedside [27]. In this study, patients in group B had higher MMSE scores at 1, 4, and 7 d after surgery, and the incidence of POCD was lower than that in group A (P < 0.05), suggesting that ultrasound-guided CFNB with ropivacaine could reduce the incidence of postoperative POCD. The reason may be that ultrasound-guided operation can not only avoid causing trauma to patients, but also accurately locate nerves and correctly guide the implementation of nerve block. Secondly, this analgesic method also effectively blocks the transmission of pain stimuli to the central system, thereby reducing the physiological changes and stress responses caused by pain stimuli, and thus decreasing the incidence of POCD [28].
In summary, compared with continuous pumping of fentanyl for analgesia, ultrasound-guided CFNB showed more effective analgesic effects following total knee arthroplasty, which helps reduce the incidence of POCD and adverse reactions.
Disclosure of conflict of interest
None.
References
- 1.Aksu C, Akay MA, Şen MC, Gürkan Y. Ultrasound-guided dorsal penile nerve block vs. neurostimulator-guided pudendal nerve block in children undergoing hypospadias surgery: a prospective, randomized, double-blinded trial. Paediatr Anaesth. 2019;29:1046–1052. doi: 10.1111/pan.13727. [DOI] [PubMed] [Google Scholar]
- 2.Kale A, Usta T, Basol G, Cam I, Yavuz M, Aytuluk HG. Comparison of ultrasound-guided transgluteal and finger-guided transvaginal pudendal nerve block techniques: which one is more effective? Int Neurourol J. 2019;23:310–320. doi: 10.5213/inj.1938112.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim YB, Park HY, Kim KM, Shin HJ, Kim SB, Lee MG. The effect of interfascial injection on obturator nerve block compared with nerve stimulating approach by ultrasound-guide: a randomized clinical trial. Urol J. 2019;16:407–411. doi: 10.22037/uj.v0i0.4386. [DOI] [PubMed] [Google Scholar]
- 4.Huang Z, Xia W, Peng XH, Ke JY, Wang W. Evaluation of ultrasound-guided genitofemoral nerve block combined with Ilioinguinal/iliohypogastric nerve block during inguinal hernia repair in the elderly. Curr Med Sci. 2019;39:794–799. doi: 10.1007/s11596-019-2107-2. [DOI] [PubMed] [Google Scholar]
- 5.Aslan R, Erbin A, Celik S, Ucpinar B, Eryilmaz R, Taken K. Periprostatic nerve block alone versus combined with perineal pudendal nerve block or intrarectal local anesthesia during transrectal ultrasound-guided prostate biopsy: a prospective randomized controlled trial. Int J Urol. 2019;26:833–838. doi: 10.1111/iju.14036. [DOI] [PubMed] [Google Scholar]
- 6.Anugerah A, Nguyen K, Nader A. Technical considerations for approaches to the ultrasound-guided maxillary nerve block via the pterygopalatine fossa: a literature review. Reg Anesth Pain Med. 2020;45:301–305. doi: 10.1136/rapm-2019-100569. [DOI] [PubMed] [Google Scholar]
- 7.Samerchua A, Leurcharusmee P, Panichpichate K, Bunchungmongkol N, Wanvoharn M, Tepmalai K, Khorana J, Chantakhow S. A prospective, randomized comparative study between ultrasound-guided posterior quadratus lumborum block and ultrasound-guided ilioinguinal/iliohypogastric nerve block for pediatric inguinal herniotomy. Paediatr Anaesth. 2020;30:498–505. doi: 10.1111/pan.13837. [DOI] [PubMed] [Google Scholar]
- 8.Murata S, Iwasaki H, Natsumi Y, Minagawa H, Yamada H. Vascular evaluation around the cervical nerve roots during ultrasound-guided cervical nerve root block. Spine Surg Relat Res. 2020;4:18–22. doi: 10.22603/ssrr.2019-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sinha C, Kumar A, Kumar A, Prasad C, Singh PK, Priya D. Pectoral nerve versus erector spinae block for breast surgeries: a randomised controlled trial. Indian J Anaesth. 2019;63:617–622. doi: 10.4103/ija.IJA_163_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferré F, Pommier M, Laumonerie P, Ferrier A, Menut R, Bosch L, Balech V, Bonnevialle N, Minville V. Hemidiaphragmatic paralysis following ultrasound-guided anterior vs. posterior suprascapular nerve block: a double-blind, randomised control trial. Anaesthesia. 2020;75:499–508. doi: 10.1111/anae.14978. [DOI] [PubMed] [Google Scholar]
- 11.Esparza-Miñana JM, Mazzinari G. Adaptation of an ultrasound-guided technique for pulsed radiofrequency on axillary and suprascapular nerves in the treatment of shoulder pain. Pain Med. 2019;20:1547–1550. doi: 10.1093/pm/pny311. [DOI] [PubMed] [Google Scholar]
- 12.Smith LM, Barrington MJ. Ultrasound-guided blocks for cardiovascular surgery: which block for which patient? Curr Opin Anaesthesiol. 2020;33:64–70. doi: 10.1097/ACO.0000000000000818. [DOI] [PubMed] [Google Scholar]
- 13.Tripathy S, Mandal I, Rao PB, Panda A, Mishra T, Kar M. Opioid-free anesthesia for breast cancer surgery: a comparison of ultrasound guided paravertebral and pectoral nerve blocks. A randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2019;35:475–480. doi: 10.4103/joacp.JOACP_364_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ryu JH, Shim JH, Yeom JH, Shin WJ, Cho SY, Jeon WJ. Ultrasound-guided greater occipital nerve block with botulinum toxin for patients with chronic headache in the occipital area: a randomized controlled trial. Korean J Anesthesiol. 2019;72:479–485. doi: 10.4097/kja.19145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corke PJ. Ultrasound-guided posterior antebrachial cutaneous nerve block utilising the ‘fat-filled flat tunnel’: description of technique and cutaneous sensory block area. Anaesth Intensive Care. 2019;47:532–540. doi: 10.1177/0310057X19888817. [DOI] [PubMed] [Google Scholar]
- 16.Arjun BK, Prijith RS, Sreeraghu GM, Narendrababu MC. Ultrasound-guided popliteal sciatic and adductor canal block for below-knee surgeries in high-risk patients. Indian J Anaesth. 2019;63:635–639. doi: 10.4103/ija.IJA_296_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu F, Tian J, Dong J, Zhang K. Tonic-clonic seizure during the ultrasound-guided stellate ganglion block because of an injection into an unrecognized variant vertebral artery: a case report. Medicine (Baltimore) 2019;98:e18168. doi: 10.1097/MD.0000000000018168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sir E, Eksert S, Zor M, Emin Ince M, Kaya E, Bedir S. The analgesic efficacy of ultrasound guided unilateral transversus abdominis plane block in the pain management of shock wave lithotripsy. Arch Esp Urol. 2019;72:933–938. [PubMed] [Google Scholar]
- 19.Siddeshwara A, Singariya G, Kamal M, Kumari K, Seervi S, Kumar R. Comparison of efficacy of ultrasound-guided pectoral nerve block versus thoracic paravertebral block using levobupivacaine and dexamethasone for postoperative analgesia after modified radical mastectomy: a randomized controlled trial. Saudi J Anaesth. 2019;13:325–331. doi: 10.4103/sja.SJA_25_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laumonerie P, Blasco L, Tibbo ME, Panagiotis K, Fernandes O, Lauwers F, Bonnevialle N, Mansat P, Ohl X. Ultrasound-guided versus landmark-based approach to the distal suprascapular nerve block: a comparative cadaveric study. Arthroscopy. 2019;35:2274–2281. doi: 10.1016/j.arthro.2019.02.050. [DOI] [PubMed] [Google Scholar]
- 21.Shah A, Morris S, Alexander B, McKissack H, Jones JR, Tedder C, Jha AJ, Desai R. Landmark technique vs. ultrasound-guided approach for posterior tibial nerve block in cadaver models. Indian J Orthop. 2020;54:38–42. doi: 10.1007/s43465-019-00012-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gritsenko K, Polshin V, Agrawal P, Nair S, Shaparin N, Gruson K, Tan-Geller M. Incidence of vocal cord paresis following ultrasound-guided interscalene nerve block: an observational cohort study. Best Pract Res Clin Anaesthesiol. 2019;33:553–558. doi: 10.1016/j.bpa.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 23.Kåsine T, Romundstad L, Rosseland LA, Ullensvang K, Fagerland MW, Hol PK, Kessler P, Sauter AR. Needle tip tracking for ultrasound-guided peripheral nerve block procedures-an observer blinded, randomised, controlled, crossover study on a phantom model. Acta Anaesthesiol Scand. 2019;63:1055–1062. doi: 10.1111/aas.13379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Osaka Y, Morita Y. A laser mount probe holder facilitates fixation of the optimized ultrasound image and needle alignment in-plane to the ultrasound beam during ultrasound-guided peripheral nerve block. J Anesth. 2019;33:620–622. doi: 10.1007/s00540-019-02666-w. [DOI] [PubMed] [Google Scholar]
- 25.Yang H, Dong Q, Liang L, Liu J, Jiang L, Liang H, Xu S. The comparison of ultrasound-guided thoracic paravertebral blockade and internal intercostal nerve block for non-intubated video-assisted thoracic surgery. J Thorac Dis. 2019;11:3476–3481. doi: 10.21037/jtd.2019.07.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karaca O, Pınar HU. Efficacy of ultrasound-guided bilateral erector spinae plane block in pediatric laparoscopic cholecystectomy: case series. Agri. 2019;31:209–213. doi: 10.14744/agri.2019.88896. [DOI] [PubMed] [Google Scholar]
- 27.Qian Y, Guo Z, Huang J, Zhang Q, An X, Hu H, Zhu F, Wang X. Electromyographic comparison of the efficacy of ultrasound-guided suprainguinal and infrainguinal fascia iliaca compartment block for blockade of the obturator nerve in total knee arthroplasty: a prospective randomized controlled trial. Clin J Pain. 2020;36:260–266. doi: 10.1097/AJP.0000000000000795. [DOI] [PubMed] [Google Scholar]
- 28.Gao Z, Xiao Y, Wang Q, Li Y. Comparison of dexmedetomidine and dexamethasone as adjuvant for ropivacaine in ultrasound-guided erector spinae plane block for video-assisted thoracoscopic lobectomy surgery: a randomized, double-blind, placebo-controlled trial. Ann Transl Med. 2019;7:668. doi: 10.21037/atm.2019.10.74. [DOI] [PMC free article] [PubMed] [Google Scholar]


