Abstract
Gynecological cancers especially endometrial cancer have put a huge burden on health care systems in different societies. In this regard, different studies have evaluated screening, diagnosis and treatments of endometrial cancer. Different survival rates, prognosis and recurrence rates have been reported by variable treatment methods. Laparotomy and laparoscopic radical hysterectomy (RH and LRH) are nowadays two most common surgical methods for endometrial cancer. In this systematic review, we investigated all article comparing two treatment techniques regarding RH and LRH in women with endometrial cancer who were classified as International Federation of Gynecology and Obstetrics (FIGO) stage I to III. Data regarding to blood loss and transfusion rate, operative time, duration of hospital stay, complications as intraoperative and postoperative, mean nodules counts, recurrent rate, adjuvant therapy were collected and analyzed. After reviewing five cohort studies, we indicated that laparoscopic procedures were better than laparotomy for managing endometrial cancer because the duration of hospitalization, blood loss and intraoperative and postoperative complications in laparoscopy procedure were lower than laparotomy procedures.
Keywords: Endometrial cancer, laparoscopy, laparotomy
Introduction
Endometrial cancer is known to be one of the most prevalent cancers among American women. Incidence of endometrial cancer is almost 64 new cases in every 100000 women with a mortality rate of 4.6 each year [1]. Prevalence of endometrial cancer in known to increase in higher ages and among obese women [2-4]. 75% of endometrial cancer occurs in postmenopausal women with the mean age of 70 years [5]. The 5 year survival rate of endometrial cancer is variable based on stages of the cancer from 96% in early stages to 17% in invasive stage [6,7].
Hysterectomy is one of the best methods in patients with non-metastatic endometrial cancer [8]. Hysterectomy could be associated with other surgical procedures such as oophorectomy. These surgeries could be performed using both laparoscopic and laparotomy methods each having their own advantages and complications [9,10]. Different lines of evidence have assessed the two procedures and their differences such as operation time, duration of hospitalization, post-operative pain and complications, requirements for blood transfusion and risks of infection. There are also different success and recurrence rates for both procedures, reported in different studies [11-13]. Studies believe that laparoscopic procedures are associated with better results especially by cosmetic evaluations but on the other hand, laparotomy hysterectomy might have better long-term results [14,15].
So in this study, we aimed to compare studies about comparison laparotomy and laparoscopic radical hysterectomy (RH and LRH) in patients with early stages of endometrial cancer.
Methods
Study design
The current study is a review based on Meta-analysis of observational studies in epidemiology (MOOSE) guideline (11). In this study keywords such as endometrial cancer, laparoscopic, laparotomy and radical hysterectomy were used and searched in the PubMed, Medline, Google Scholar, Embase and Cochrane library. The articles were searched between 2000 to 2020 and the language of these articles was English. In all search any software didn’t used. All article was original article (cohort or retrospectively) based on inclusion and exclusion criteria of study.
Assessments
Inclusion criteria for studies was all article comparing two treatment techniques regarding RH and LRH in women with endometrial cancer who were classified as International Federation of Gynecology and Obstetrics (FIGO) stage I to III. However, case report or case series studies, review, editorial and letter to editor studies and study about other management in patients of endometrial cancer were excluded.
In this regarding, these data were collected from studies that were included first authors last name, year of publication, participant, study design, sample size, age, body mass index (BMI), blood loss and transfusion rate, operative time, duration of hospital stay, complications as intraoperative and postoperative, mean nodules counts, recurrent rate, adjuvant therapy.
Statistical analysis
After collecting the data of articles, the quantitative data were showed as mean and qualitative data were showed as frequency and percent. The differences in the thickness and fit of the mouthguard fabricated by the vacuum-forming method and the pressure-forming method were analyzed using two-way analysis of variance (ANOVA) and a post-hoc test (Bonferroni method). Statistical analysis was performed using statistical analysis software (SPSS 24, IBM, USA), and differences of P<0.05 were decided significant.
Results
Demographical
We reviewed 5 study (Figure 1) including 3 cohorts, 1 prospective and 1 retrospective, all of these studies compared laparoscopy and laparotomy surgery in patients with endometrial cancer, so 716 cases were under laparoscopy and 360 cases were under laparotomy surgery. The mean age in the laparoscopy group was 56.31 years and in the laparotomy group was 55.54 years and the mean of BMI in the laparoscopy and laparotomy surgeries were 31.29 and 32.2 kg/m2, respectively.
Figure 1.
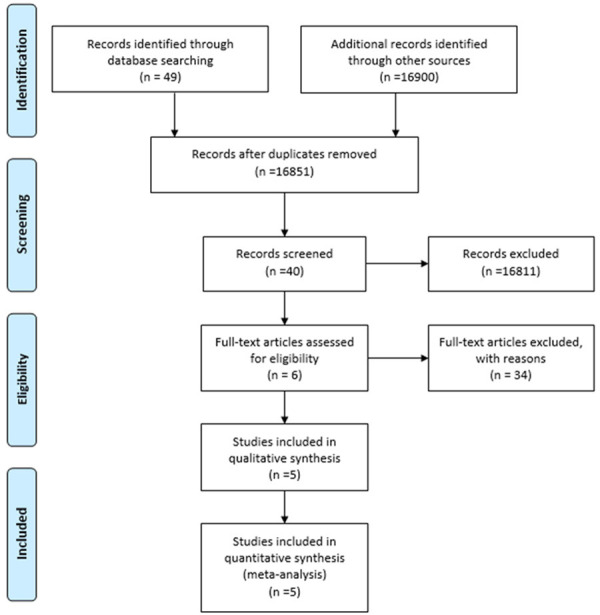
Literature search and screening flowchart.
Clinical information
The numbers of tumor staging in the laparoscopy (n=149) were 94 stage I (63.1%), 39 stage II (26.1%) and 16 stage III (10.8%) and in the laparotomy (n=189) were 123 stage I (65.1%), 42 stage II (22.2%) and 24 stage III (12.7%). The mean of lymph node numbers in the laparoscopy group was 18 and in the laparotomy group was 18.97. 27 of 58 cases (46.5%) in the laparoscopy group and 28 of 61 cases (45.9%) in the laparotomy group needed to adjuvant therapy. The mean of hospitalization in the laparoscopy and laparotomy groups were 4.63 and 8.67 days, respectively. The mean of operative time in the laparoscopy and laparotomy groups were 177.22 and 175.77 min.
Complications
There were some complications in both groups, the number of intraoperative complication in laparoscopy was 5 of 128 cases (3.9%) and in the laparotomy was 2 of 131 cases (1.5%) and the number of postoperative complication in the laparoscopy was 25 cases (3.4%) and in the laparotomy was 49 cases (13.6%). The mean of blood loss in the laparoscopy and laparotomy groups were 318.98 and 329.53 ml, respectively and 24 of 81 cases (29.6%) in the laparoscopy and 25 of 96 cases (26.04%) in the laparotomy groups needed to pack cells (Table 1).
Table 1.
Variables of studies that discussed
| Frist author | Year | Type | Group | Age (year) | Number | BMI* (kg/m2) | Staging | Lymph node | Adjuvant therapy | Hospitalization (days) | Operation time (min) | Complication | Blood loss (ml) | Pack cell need | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||||||
| I | II | III | Intraoperative | Postoperative | |||||||||||||
| Zorlu | 2005 | Cohort | Laparoscopy | 56.6 | 26 | 24.4 | 21 | 2 | 3 | 18.2 | 11 | 4.1 | 155 | 0 | 0 | - | 6 |
| Laparotomy | 54.9 | 26 | 26.2 | 14 | 4 | 8 | 21.1 | 10 | 8.2 | 144 | 0 | 5 | - | 8 | |||
| Api | 2013 | Cohort | Laparoscopy | 56 | 21 | 26.8 | 12 | 9 | - | 12.3 | - | 5 | 180.47 | - | 4 | 136.6 | - |
| Laparotomy | 54 | 58 | 26.7 | 42 | 14 | 2 | 13 | - | 8.5 | 169.65 | - | 9 | 245.6 | - | |||
| Yin | 2015 | Retro Cohort | Laparoscopy | 52.4 | 32 | - | 25 | 2 | 5 | 18.6 | 16 | 4.8 | 218.4 | 0 | 2 | 258.5 | - |
| Laparotomy | 51.6 | 35 | - | 27 | 2 | 6 | 18.3 | 18 | 7.7 | 203.5 | 1 | 3 | 304.7 | - | |||
| Bige | 2015 | prospective | Laparoscopy | 55.56 | 70 | 44.49 | 36 | 26 | 8 | 22.9 | - | 4.64 | 155.03 | 5 | 8 | 561.86 | 18 |
| Laparotomy | 56.24 | 70 | 45.9 | 40 | 22 | 8 | 23.53 | - | 10.36 | 185.94 | 1 | 21 | 438.29 | 17 | |||
| Schiavone | 2016 | retrospective | Laparoscopy | 61 | 567 | 29.5 | - | - | - | - | - | - | - | - | 11 | - | - |
| Laparotomy | 61 | 171 | 30 | - | - | - | - | - | - | - | - | 11 | - | - | |||
BMI: Body Mass Index.
Discussion
Based on results laparoscopy was better than laparotomy for management of women with endometrial cancer, the difference between these two methods are in hospitalization and complications following surgery. Our review was first review about selecting a choice method for management endometrial cancer.
Zorlu et al. in the 2005 was compared laparotomy and laparoscopy methods in patients with endometrial cancer for first time in a cohort, 52 patients were enrolled that 26 of them underwent laparotomy and other 26 cases underwent laparoscopic staging surgery, the means age were 54.9 years in the laparotomy group and 56.6 years in the laparoscopy group. The means gravidity were 3.8 in the laparotomy group and 3.6 in the laparoscopy group. There was no significant difference between groups based on age, gravidity, body mass index. 67.3% patients was stage I disease (54% in laparotomy group and 80.8% in laparoscopy). The means of lymph nodes were 18.2 in laparoscopy and 21.1 in laparotomy (P>0.05), two cases in laparoscopy and 4 cases in laparotomy had pelvic lymph nodes metastasis. 42.3% of laparoscopy and 38.5% of laparotomy had need to adjuvant radiation therapy. The mean of hospitalization in laparoscopy was significantly lower than laparotomy group (4.1 vs 8.2 days), but there was no significant difference between groups based on operative time. There was any complication in the laparoscopic method but 5 patients in the laparotomy group had wound complication which needed to reoperation for closure. 8 units red blood suspension in laparotomy group and 6 units in laparoscopy was used [16]. Based on present study the hospitalization time and postoperative in laparoscopy surgery was lower than laparotomy surgery.
Api et al. who was conducted a retrospective study in 2013, there was no significant difference between groups based on age, BMI and tumor grading (P>0.05), also 80.9 of laparoscopy and 91.3% of laparotomy were endometrioid (P=0.21). There was no significant difference between groups based on operative time (P=0.4). The mean of intraoperative blood loss and hospitalization in the laparotomy group was significantly higher than laparoscopy group (P<0.001 for both). All patients underwent pelvic lymphadenectomy and also paraaortic lymph nodes were in 28.5% of laparoscopy and 46.5% of laparotomy groups. The means of pelvic lymph nodes were 9.2 and 8.9 for laparoscopy and laparotomy procedures, respectively (P=0.80). The number of resected right lymph nodes in the laparoscopy was significantly higher than laparotomy procedure (P=0.039). Relapsing was occurred in 9.5% of laparoscopy and 8.6% of laparotomy groups. Any died was reported in this study [17]. The present study showed there was no difference between laparoscopy and laparotomy based on intraoperative blood loss and number of resected lymph nodes but the mean of hospitalization time in the laparoscopy surgery was lower than laparotomy.
A retrospectively study by Yin in 2015 which enrolled 26 patients underwent laparoscopy and 28 patients underwent laparotomy, there was no significant difference between groups based on age, lymph nodes, stage of disease and operative time. The mean of intraoperative blood loss in the laparoscopic procedure was significantly lower than laparotomy procedure (P<0.05). The mean of hospitalization and postoperative anal exhaust in the laparoscopy group was significantly lower than laparotomy group (P<0.05). Surgical complications such as intraoperative blood vessel rupture and bladder or ureteral injury was not in the laparoscopy group but one intraoperative blood vessel rupture was in the laparotomy group (P<0.05). One patient in the laparoscopy and one in the laparotomy group had postoperative fever. One patient in the laparotomy group had fat liquefaction but there was no patient in the laparoscopy group (P<0.05). There was no wound infection in each group. One case in the laparoscopy and one in the laparotomy groups had lymphatic cyst. There were 6.3% complication in laparoscopy and 11.4% in the laparotomy groups. There was no significant difference between groups based on adjuvant therapy (P>0.05). There were 3 recurred and 1 died in the laparoscopy group and 4 recurred and 1 died in the laparotomy group (P>0.05) [18]. The present study showed there are difference between two methods in the hospitalization and complication following surgery.
Bige et al. in a prospective at 2015, 140 morbidly obese women with early stage of endometrial carcinoma were enrolled into the study, there was no significant difference between groups based on demographics such as age and BMI and clinical such as grading of disease (P>0.05). The mean of operative time in the laparoscopy group was significantly lower than laparotomy and also the mean of blood loss in the laparoscopy was significantly higher than other (P<0.05). There was no significant difference between groups based on blood transfusion in intraoperative and postoperative, lymph nodes count and intraoperative complications (P>0.05). The postoperative complications in the laparoscopy group was significantly lower than laparotomy group (P=0.01). Also the postoperative pain in the laparoscopy procedure was significantly lower than laparotomy group (P<0.05). Mean time to resume full activity in the laparoscopy group was significantly lower than laparotomy group (P<0.001). One case in the laparotomy group had recurrence but there was no case in the laparoscopy (P>0.05). Two cases in the laparoscopy and 2 patients in the laparotomy group were died in the follow up period [19].
In a retrospective study by Schiavone and colleagues in 2016, 758 patients with endometrial cancer were enrolled, 567 cases underwent laparoscopic surgery with robotic and 171 underwent laparotomy, there was no significant difference between groups based on age, BMI and comorbidities (P>0.05). There were 11 cases (1.9%) in laparoscopy and 11 cases (6.4%) in laparotomy groups with herniation (P=0.002) [20]. Other data of this study not approved with inclusion of our study (Table 1). The low related studies were a main limitation for the present study so we need more related studies in this subject.
Conclusion
In this study we review five cohort study about different between laparoscopy and laparotomy procedures for management of women with endometrial cancer that based on these studies, laparoscopy was better than laparotomy to manage of these patients because the duration of hospitalization, blood loss and intraoperative and postoperative complications in laparoscopy procedure were lower than laparotomy procedure but based on our results collection the main differences between laparoscopy and laparotomy procedures were in the hospitalization and postoperative complications.
Disclosure of conflict of interest
None.
References
- 1.Hüsing A, Dossus L, Ferrari P, Tjønneland A, Hansen L, Fagherazzi G, Baglietto L, Schock H, Chang-Claude J, Boeing H. An epidemiological model for prediction of endometrial cancer risk in Europe. Eur J Epidemiol. 2016;31:51–60. doi: 10.1007/s10654-015-0030-9. [DOI] [PubMed] [Google Scholar]
- 2.Terry KL, Missmer SA. Epidemiology of ovarian and endometrial cancers. Pathology and Epidemiology of Cancer. Springer; 2017. pp. 233–246. [Google Scholar]
- 3.Creasman WT. Editor Endometrial cancer: incidence, prognostic factors, diagnosis, and treatment. Semin Oncol. 1997;24:1–140. [PubMed] [Google Scholar]
- 4.Rafiee Zadeh A, Ghadimi K, Mohammadi B, Hatamian H, Naghibi SN, Danaeiniya A. Effects of estrogen and progesterone on different immune cells related to multiple sclerosis. Caspian J Neurol Sci. 2018;4:83–90. [Google Scholar]
- 5.Mallozzi M, Leone C, Manurita F, Bellati F, Caserta D. Endocrine disrupting chemicals and endometrial cancer: an overview of recent laboratory evidence and epidemiological studies. I Int J Environ Res. 2017;14:334. doi: 10.3390/ijerph14030334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E. Endometrial cancer. Lancet. 2016;387:1094–1108. doi: 10.1016/S0140-6736(15)00130-0. [DOI] [PubMed] [Google Scholar]
- 7.Kumar S, Podratz KC, Bakkum-Gamez JN, Dowdy SC, Weaver AL, McGree ME, Cliby WA, Keeney GL, Thomas G, Mariani A. Prospective assessment of the prevalence of pelvic, paraaortic and high paraaortic lymph node metastasis in endometrial cancer. Gynecol Oncol. 2014;132:38–43. doi: 10.1016/j.ygyno.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Papadia A, Bellati F, Ditto A, Bogani G, Gasparri ML, Di Donato V, Martinelli F, Lorusso D, Benedetti-Panici P, Raspagliesi F. Surgical treatment of recurrent endometrial cancer: time for a paradigm shift. Ann Surg Oncol. 2015;22:4204–4210. doi: 10.1245/s10434-015-4504-5. [DOI] [PubMed] [Google Scholar]
- 9.Park D, Yun J, Kim S, Lee S. Surgical and clinical safety and effectiveness of robot-assisted laparoscopic hysterectomy compared to conventional laparoscopy and laparotomy for cervical cancer: a systematic review and meta-analysis. Eur J Surg Oncol (EJSO) 2017;43:994–1002. doi: 10.1016/j.ejso.2016.07.017. [DOI] [PubMed] [Google Scholar]
- 10.Magrina JF. Outcomes of laparoscopic treatment for endometrial cancer. Curr Opin Obstet Gynecol. 2005;17:343–346. doi: 10.1097/01.gco.0000175350.18308.73. [DOI] [PubMed] [Google Scholar]
- 11.Lim CS, Mowers EL, Mahnert N, Skinner BD, Kamdar N, Morgan DM, As-Sanie S. Risk factors and outcomes for conversion to laparotomy of laparoscopic hysterectomy in benign gynecology. Obstet Gynecol. 2016;128:1295–1305. doi: 10.1097/AOG.0000000000001743. [DOI] [PubMed] [Google Scholar]
- 12.Gaia G, Holloway RW, Santoro L, Ahmad S, Di Silverio E, Spinillo A. Robotic-assisted hysterectomy for endometrial cancer compared with traditional laparoscopic and laparotomy approaches: a systematic review. Obstet Gynecol. 2010;116:1422–1431. doi: 10.1097/AOG.0b013e3181f74153. [DOI] [PubMed] [Google Scholar]
- 13.Walker JL, Piedmonte MR, Spirtos NM, Eisenkop SM, Schlaerth JB, Mannel RS, Spiegel G, Barakat R, Pearl ML, Sharma SK. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: gynecologic oncology group study LAP2. J. Clin. Oncol. 2009;27:5331. doi: 10.1200/JCO.2009.22.3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghazali WAHW, Jamil SA, Sharin IA. Laparoscopic versus Laparotomy: staging surgery for endometrial cancer-malaysia’s early experience. GMIT. 2019;8:25. doi: 10.4103/GMIT.GMIT_25_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mourits MJ, Bijen CB, Arts HJ, ter Brugge HG, van der Sijde R, Paulsen L, Wijma J, Bongers MY, Post WJ, van der Zee AG. Safety of laparoscopy versus laparotomy in early-stage endometrial cancer: a randomised trial. Lancet Oncol. 2010;11:763–771. doi: 10.1016/S1470-2045(10)70143-1. [DOI] [PubMed] [Google Scholar]
- 16.Zorlu CG, Simsek T, Ari ES. Laparoscopy or laparotomy for the management of endometrial cancer. JSLS. 2005;9:442–6. [PMC free article] [PubMed] [Google Scholar]
- 17.Api M, Kayatas S, Boza AT, Nazik H, Adiguzel C, Guzin K, Eroglu M. Surgical staging of early stage endometrial cancer: comparison between laparotomy and laparoscopy. World J Clin Oncol. 2013;4:235. doi: 10.4021/wjon743w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yin X, Shi M, Xu J, Guo Q, Wu H. Perioperative and long-term outcomes of laparoscopy and laparotomy for endometrial carcinoma. Int J Clin Exp Med. 2015;8:19093. [PMC free article] [PubMed] [Google Scholar]
- 19.Bige Ö, Demir A, Saatli B, Koyuncuoğlu M, Saygılı U. Laparoscopy versus laparotomy for the management of endometrial carcinoma in morbidly obese patients: a prospective study. J Turk Ger Gynecol Assoc. 2015;16:164. doi: 10.5152/jtgga.2015.15128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schiavone MB, Bielen MS, Gardner GJ, Zivanovic O, Jewell EL, Sonoda Y, Barakat RR, Chi DS, Abu-Rustum NR, Leitao MM Jr. Herniation formation in women undergoing robotically assisted laparoscopy or laparotomy for endometrial cancer. Gynecol Oncol. 2016;140:383–386. doi: 10.1016/j.ygyno.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


