Abstract
Introduction: Endometriosis is an illness caused by the presence of foci of endometrial implants outside the uterine cavity. Laparoscopy (minimally invasive surgical method) is considered as the definitive treatment for Endometriosis. Method: Clinical data from January 2014 till December 2018, between the ages of 20 and 40 years were collected. A total of 175 women with pelvic Endometriosis complicated with infertility, underwent laparoscopy in our hospital, were followed up to assess fertility outcome. We analyzed using univariate logistic regression analysis as well as multivariate logistic analysis. Results: We analyzed the relationship between them by logistic regression analysis. Univariate logistic regression analysis indicated that the significant factors for influencing pregnancy were the following factors: age, infertility types: primary or secondary infertility, treatment with Gonadotrophin Releasing Hormone-agonist, r-AFS grade, operative method: excision or ablation. And multivariate logistic regression using all the factors also revealed that age, infertility types: primary or secondary, treatment with GnRH-a, revised- American Fertility Society grading and operative method: excision or ablation were positively correlated and were the significant factors to influence pregnancy outcome. While the other factors such as Body Mass Index, and endometriosis along with other gynecological pathology were not statistically significant. Conclusions: In this study, we found out that age, infertility type, treatment with Laparoscopy surgery, use of GnRH-a after the operation, grading of the disease, and different types of operative methods were found to be significant and were found to be the factors which influenced the pregnancy outcome.
Keywords: Endometriosis, infertility, laparoscopy, affecting factors
Introduction
Endometriosis is a recurrently seen ailment in the gynecological department among the generative age group of females and is distinguishing in character by the exhibition of endometriotic materials (glands and stroma) exterior to the uterine cavity, which is typically characterized by pelvic pain (dysmenorrhea, non-menstrual pain, and dyspareunia) and subfertility. The furthermost communal locations to get involved with this illness are ovaries and the pelvic peritoneum including the anterior and posterior cul de sacs. The exact cause of endometriosis to this day is unknown, although many theories have been developed regarding the pathophysiology. No single theory can enlighten the diversity of clinical presentations of endometriosis and most possibly the cause is multi-factorial. EMS has no pathognomonic signs or symptoms and is as a result hard to make a diagnosis. A proper link between infertility and endometriosis, albeit controversial, has been frequently described. In infertile women, 25-50% are considered to have endometriosis. In women with endometriosis, 30-50% is infertile [1]. About half of women with a surgical diagnosis of the disease successively be unsuccessful to accomplish natural pregnancy [2]. An unsuitable situation of the endometrium and its biochemical activity recruits an inflammatory response which outcomes in severe cyclical or non-cyclical pelvic pain. This pain strengthens during every menses, even while having sexual intercourse, straining while defecation, non-cyclical bleedings, and ailments related to the urinary and digestive systems. The illness also presents complications related to infertility [3-6]. The chief part of surgery to inflate the pregnancy rate in infertile women with EMS is much questioned. But many diverse studies suggested that at present, the treatment of infertility caused by endometriosis is mainly laparoscopic surgery, postoperative medication, and artificial assisted reproductive technology. EMS can only be diagnosed during laparoscopy, preferably established by histopathology, and can exist as a disease in the peritoneum with characteristic or indirect lesions, ovarian endometriotic cysts (endometriomas) or deeply infiltrative disease (DIE) or as a blend of these features. The European Society of Human Reproduction and Embryology [1], the American Society for Reproductive Medicine (ASRM) [7], and the Royal College of Obstetricians and Gynecologists [7] proposed surgery for stage I-II disease with partial advantage and stage III-IV disease with potential help. Operative laparoscopy for EMS comprises of electrocautery or laser demolition of endometriotic implants and adhesiolysis. At present, the “revised staging of endometriosis” proposed by AFS of the American Fertility Society in 1985 is the widely used staging system [8].
Occurrence of endometriosis has risen up to 50% in females with infertility [9]. Females with endometriosis have a low monthly fecundity rate (MFR) associated with the MFR in fertile controls. Monthly fecundity is from 0.02-0.10 in infertile females with endometriosis, however fecundity ranges from 0.15-0.20 per month in normal one [10]. The existence of endometriosis may negatively affect both the spontaneous chance of conception [11] and IVF pregnancy rates when associated with those of females with unexplained infertility or tubal factor controls [12].
In our manuscript, we intend to find the clinical factors that affected pregnancy outcome after laparoscopic treatment in endometriosis-associated Infertility.
Materials and methods
Selection of participants and collection of the data
Women who were surgically operated by the laparoscopic procedure for infertility to remove foci of EMS from January 2014 till December 2018 in the Gynecological ward of the Second affiliated hospital of Wenzhou medical university were retrospectively analyzed.
After the operative process, they were followed up for a one-year period during which the incidence of gestations was calculated. Women counted in this current study were diagnosed with primary infertility or with secondary infertility at an age not exceeding 40 years, who declared a willingness to conceive straight away, and whose male counterparts happened to fit in the ideals of normal semen analysis, were competent for the inquiry group.
Inclusion and exclusion criteria
Amongst our data, 175 women were carefully chosen for this retrospective study. They also fulfilled the inclusion criteria: infertile women (who were unable to conceive for > than 12 months) were diagnosed with EMS, by laparoscopy with histopathological confirmation, in the Second Affiliated Hospital of Wenzhou Medical University (Gynecology Department), Wenzhou, China.
1. Before the patients underwent the operation, they were not treated with hormonal drugs for three months. 2. They did not have any severe systemic diseases. 3. Male infertility issues were omitted. The husbands fit into the normal sperm count and their semen reports were average (agreeing to the fifth edition of World Health Organization WHO standards 2010 A.D). 4. Any abnormality related to coagulation was also excluded.
Patients were also excluded from the study if they were lost to follow-up (patients excluded) and also if they have any reproductive system malformations. Finally, a total of 175 patients were included in this study.
All women wanted to conceive a baby and were established postoperatively by histopathology as the disease. The average age of the patients was 20~40 years (29.3+4.1), including 56 cases of primary infertility and 119 cases of infertility with secondary types. 76 cases of Endometriosis along with Adenomyosis (43.4%).
Surgical procedure and postoperative management
The patients went through a laparoscopic tactic which is standard to eradicate the detectable endometriotic materials. General anesthesia was used for the operation and it was performed at 3~7 days of menses. Depending upon diverse sorts of the lesions observed during the operative process, we chose surgical methods such as by diathermy or laser vaporization, adhesion separation, electrocoagulation, internal lesion, oviduct repair, ovarian endometrioma cyst removal, and uterine suspension. All patients received treatment with methylene blue liquid in laparoscopic surgery. During operation, the grade and staging of the disease were also evaluated. After the operation, the abdominal cavity and the rinse solution are rinsed with saline. Intraperitoneal anti-adhesions were placed in patients with severe pelvic adhesions to prevent further adhesion after the operation. Intravenous antibiotics were injected into all patients, to prevent infection within 48 hours after the operation. After laparoscopy, the sample specimen collected during the procedure was directed for histopathological examination to approve the verdict of endometriosis. According to their judgment and economic situations, the patients were estimated to actively try to consider getting pregnant, either with ART or as expected naturally.
EMS diagnosis
All specimens were fixed by formalin solution (10%), then paraffin-embedded, sectioning, hematoxylin-eosin staining, and then pathologically established by 2 pathologists in the second affiliated hospital of Wenzhou medical university, Wenzhou, China.
Use of GnRH-agonist
After the operation, agreeing to the severity of the disease, GnRH-agonist was used for 3 to 6 cycles. Not all patients were given GnRH-agonist adjuvant therapy. According to their individual choices and economic situations, they were routinely managed or planned to receive ART.
Study members were telephoned to discover whether they conceived or not, and the patient’s last menstrual period date was noted. Pregnancy was demarcated as serum β-human chorionic gonadotropin >25 U/L and ultrasound proof of a gestational sac.
SPSS 23.0 was used to analyze hospital data. The information recovered included particulars of the patient’s age, type of infertility, infertility duration, body mass index, surgical methods, surgical staging (r-AFS grading), if joint with other gynecological disorders (such as Adenomyosis, Hydrosalpinx, endometrial polyps, or any other gynecological disorders), use of postoperative medication (that is whether the women were given GnRH-agonist adjuvant medicine for 3-6 months after they went through the surgical process of laparoscopy). And the patients were telephoned or followed up through outpatient department visits and outcomes of pregnancy results of 1 year after the surgical events were noted.
Statistical analysis
The statistics were performed using the statistical package for social sciences SPSS 23.0 (SPSS Inc., Chicago, IL, USA); statistical software. With normal distribution measurement data is expressed as - x + s, compared with t-test; count data were compared using the 2 tests. Multifactor logistic regression analysis of the potential factors was used to evaluate the factors affecting 1 year of pregnancy after laparoscopy (P<0.001 was statistically significant). The odds ratio and 95% confidence interval for each factor were calculated. In our study 72 patients who received GnRH-agonist conceived while 27 patients receiving GnRH-agonist didn’t conceive. And out of 68 patients who didn’t receive GnRH-agonist only 27 of them conceived.
Receiver operator characteristic (ROC) curves were plotted to determine an optimal cut-off point of the age. For all analyses, P<0.001 was considered as statistically significant.
Results
Clinical features and characteristics of patient
Out of 175 women included in our retrospective analysis (Table 1), the average age of the patients was 29.3+4.1 (range 20-20 years of age). Among them, 154 patients belonged to <35 years of age and 21 patients were over the age of 35.
Table 1.
Clinical features and patient’s characteristics
| Clinical features | values | |
|---|---|---|
| N (%) | ||
| Age (years) | 29.3±4.1 | |
| <35 | 154 (88.0) | |
| ≥35 | 21 (12.0) | |
| BMI (kg/m2) | 20.3±2.9 | |
| ≥24 | 14 (8.0) | |
| <24 | 161 (92.0) | |
| Fertility status | ||
| Conceived | Natural | 84 (48.0) |
| Assisted | 22 (12.6) | |
| Not conceived | 69 (39.4) | |
| Infertility type | ||
| secondary | 119 (68.0) | |
| primary | 56 (32.0) | |
| Operative methods | ||
| Excision | 54 (30.9) | |
| Ablation | 20 (11.4) | |
| excision + ablation | 101 (57.7) | |
| Grade | ||
| 1 | 34 (19.4) | |
| 2 | 56 (32.0) | |
| 3 | 43 (24.6) | |
| 4 | 42 (24.0) | |
| Other diseases (combined) | ||
| yes | 76 (43.4) | |
| no | 99 (56.6) | |
| GnRH-agonist | ||
| used | 99 (56.6) | |
| Not used | 75 (43.3) |
N = number of cases, BMI = body mass index.
The average body mass index of the infertile patients was 20.3±2.9. Among them 14 patients had a body mass index of more than 24 while, 161 patients had body mass index less than 24.
Among 175 women in this study, 84 women conceived naturally while 22 women conceived through the aid of assisted reproductive technique (In Vitro Fertilization or Intra Uterine Insemination). 119 patients were with secondary infertility and the remaining 56 patients had primary infertility.
54 of the patients underwent the laparoscopic procedure which included the excisional type of operation, 20 patients underwent an only excisional type of surgery while the remaining 101 underwent combined (excision + ablation both). According to the Revised-American Fertility Society staging [13] grade, 1 included 34 patients, grade 2 included 56, and grade 3 included 43, while grade 4 included 42 patients.
In the case of these patients, some of them had additional gynecological diseases (such as Adenomyosis, hydro-salpinx, polyps, etc.). 76 women had combined other gynecological diseases along with endometriosis and infertility while 99 women only had endometriosis with infertility. 99 patients got GnRH-agonist adjuvant drug after the operation while 75 of them didn’t have any hormonal therapy after the operation.
The relationship between clinical characteristics and reproductive outcomes in women
Out of the 175 patients who were followed up for the study, 106 were pregnant, and the overall rate of pregnancy was 60.57 percent. The clinical features of the patients are shown in (Table 2).
Table 2.
Correlations between the clinical characteristics and reproductive outcomes
| Clinical features | Pregnancy outcomes | P-value | |
|---|---|---|---|
|
| |||
| Conceived | Not conceived | ||
| Patients (n) | 106 | 69 | |
| Age (in years) | |||
| <35 | 101 | 53 | |
| ≥35 | 5 | 16 | <0.001 |
| BMI | |||
| ≥24 | 8 | 6 | |
| <24 | 98 | 63 | 0.784 |
| Infertility type | |||
| secondary | 82 | 37 | |
| primary | 24 | 32 | 0.001 |
| Operative method | |||
| Excision or ablation | 36 | 38 | 0.011 |
| Excision + ablation | 70 | 31 | |
| Grade of disease | |||
| 1+2 | 62 | 28 | |
| 3+4 | 44 | 41 | 0.021 |
| With other Gynecological Disease | |||
| present | 41 | 35 | |
| absent | 65 | 34 | 0.116 |
| Use of GnRH-agonist (postoperatively) | |||
| used | 72 | 27 | |
| Not used | 27 | 41 | <0.001 |
N = number of patients, P≤0.001.
Influence of various factors in the outcome of pregnancy in patients with endometriosis complicated with infertility. To discover whether the pregnancy result is influenced by the factors mentioned which are shown in (Table 1).
Furthermore, we analyzed univariate logistic and multivariate logistic regression to find out significant factors for pregnancy outcome in endometriosis associated infertile women.
Operative method of endometriosis was correlated with reproductive outcome
In order to know more about the relationship between operative method of endometriosis and reproductive outcome. We analyzed the affiliation between them by the logistic regression. Univariate logistic regression analysis (Table 3) indicated that the significant factors for pregnancy outcome after laparoscopy for endometriosis with infertility were age, infertility type, postoperative treatment with GnRH-a, r-AFS grade, and operative method.
Table 3.
Univariate logistic regression analysis of the potential factors to the reproductive outcome of infertile EMS women following surgery
| Univariate | |||
|---|---|---|---|
|
| |||
| Clinical features | OR | 95% CI | P-value |
| Age (year) | 6.098 | 2.117-17.562 | <0.001 |
| BMI (kg/m2) | 0.857 | 0.284-2.587 | 0.784 |
| Infertility type | 0.338 | 0.176-0.652 | 0.001 |
| Operative method | 1.544 | 1.131-2.107 | 0.006 |
| Grade of disease | 0.485 | 0.262-0.898 | 0.021 |
| Combined with other diseases | 0.613 | 0.332-1.131 | 0.117 |
| GnRH-agonist Adjuvant therapy | 3.216 | 1.705-6.064 | <0.001 |
OR = odds ratio; CI = confidence interval P≤0.001.
We analyzed the relationship between them by logistic regression analysis. Univariate logistic regression analysis point that the significant factors for influencing pregnancy were the following factors: age (<35 years, ≥35 years), (odds ratio [OR] 6.098, 95% CI 2.17-17.562, P<0.001), infertility types: primary or secondary infertility (odds ratio [OR] 0.338, 95% CI 0.176-0.652, P<0.001), treatment with GnRH-a (odds ratio [OR] 3.216, 95% CI 1.705-6.064, P<0.001), r-AFS grade (odds ratio [OR] 0.485, 95% CI 0.262-0.898, P = 0.021), operative method: excisional or ablation (odds ratio [OR] 1.544, 95% CI 1.131-2.107, P = 0.006).
Multivariate logistic regression (Table 4) using all the factors also revealed that age (odds ratio [OR] 11.599, 95% CI 3.274-41.089, P<0.001), infertility types: primary or secondary (odds ratio [OR] 0.22, 95% 0.099-0.491, P<0.001), treatment with GnRH-a (odds ratio [OR] 6.196, 95% CI 2.694-14.244, P<0.001), r-AFS grading (odds ratio [OR] 0.369, 95% CI 0.167-0.817, P = 0.014) and operative method: excisional or ablation (odds ratio [OR] 1.572, 95% CI 1.089-2.268, P = 0.016) were positively correlated and were the significant factors to influence pregnancy outcome. While the other factors such as BMI (odds ratio [OR] 0.857, 95% CI 0.284-2.587, P = 0.784), and endometriosis along with other gynecological pathology (odds ratio [OR] 0.613, 95% CI 0.332-1.131, P<0.117) were not statistically significant.
Table 4.
Multifactor logistic regression analysis of the potential factors to the reproductive outcome of infertile EMS women following surgery
| Multifactor | OR | 95% CI | P-value |
|---|---|---|---|
| Age (year) | 11.599 | 3.274-41.089 | <0.001 |
| Infertility type | 0.22 | 0.099-0.491 | <0.001 |
| Operative method | 1.572 | 1.089-2.268 | 0.016 |
| Grade | 0.369 | 0.167-0.817 | 0.014 |
| GnRH-agonist | 6.195 | 2.694-14.244 | <0.001 |
CI = confidence interval, OR = odds ratio, P≤0.001.
The factors such as age, infertility type, GnRH-a use after the operation, r-AFS staging, and operative method during laparoscopic surgery were found to be the influencing factors for pregnancy outcome after the laparoscopic procedure for patients with endometriosis complicated with infertility. According to the ROC curve, 26.15 is taken as the best cut-off value of Age, the sensitivity of the evaluation is 65%, and the specificity is 77.9% (Figure 1).
Figure 1.
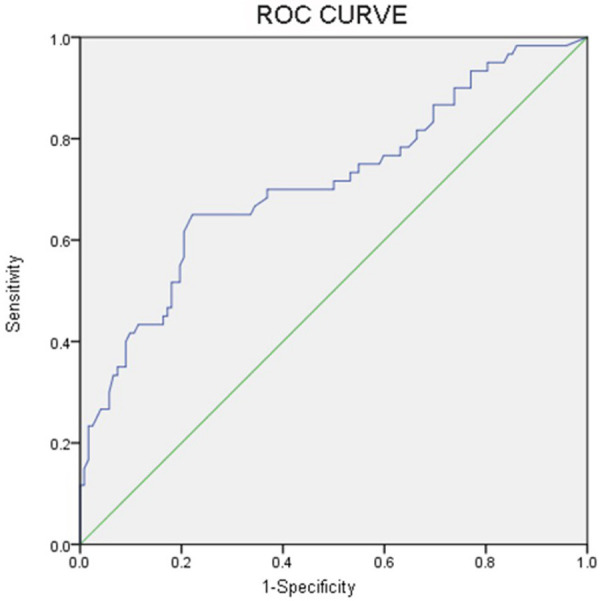
Receiver Operator Characteristic (ROC) curve showing the best cut-off value of Age was 26.15 (sensitivity 65%, specificity 77.9%).
Discussion
Endometriosis is an illness that is a benign condition but causes long-lasting inflammation leading to female childlessness which is marked by the occurrence of endometriotic matters (glands and endometrial stroma) exterior to the womb [1]. A causal association among EMS and infertility has been well-known through the application of evidence-based principles [14]. Women suffering from EMS not only experience a great deal of physical agony but also suffers mental and emotional pain. This disease is important because of its frequency, upsetting symptomatology, relationship with infertility, and potential for invasion of the surrounding organ system such as gastrointestinal and urinary tract. Women with EMS are expected to have an inferior monthly fecundity of about 0.02-0.1 per month [10,15]. Impact of EMS on quality of life and psychological health makes an enormous difference.
Laparoscopic surgery has persistently developed over the past years, advancing from an invasive diagnostic tool to an effectual tool for surgical management of the benign and malignant disease. Constant training, practice, and growth in imaging and laparoscopic instruments have helped extension of the purposes of laparoscopic surgery.
The overall advantage of minimizing trauma to the abdominal wall has been reproducible in many of the laparoscopic procedures compared with open surgery.
Faster convalescence, reduced hospital stays, and quicker return to regular activity are the most obvious benefits of the laparoscopic operation. The result, efficiency, decreased incidence of wound contaminations, and reduced perioperative morbidity of minimally invasive techniques have been revealed across different purposes, e.g., cholecystectomy, fundoplication, and adrenalectomy, etc. Despite the lack of randomized controlled trials to help laparoscopic applications, these techniques are acknowledged as the gold standard for surgical intervention. The laparoscopic surgeries are lengthier than open surgeries. Nevertheless, the period has reduced over the years through practice and the learning curve. There has been no indication that open surgery is superior to laparoscopic surgery in a relation to oncological short- and long-term results. Kasapoglu et al. assessed whether the endometriosis-associated drop in ovarian reserve is progressive in the absence of cure and superior in magnitude than the normal fall over time. They discovered that endometriosis was related with a quicker drop in serum AMH levels, which are a marker of the ovarian reserve, than the drop observed in healthy controls [16].
An analysis of 27 studies by Vercellini et al. discovered that no conclusive evidence of whether the number, size, or site of fibroids earlier to myomectomy influenced postoperative pregnancy rates [17]. Nevertheless, there are data which recommend that pregnancy rates are considerably lower in females when multiple fibroids are removed [18].
Age was found to have a clinically significant impact on postoperative pregnancy rate, with a lower spontaneous or assisted conception pregnancy rate over 35 years [19].
Advanced endometriosis with endometrioma is a usual cause of infertility, occasionally coexisting with other elements, however often presenting as a solitary reason for infertility.
In this study we retrospectively analyzed the aspects prompting the pregnancy results in the patients with infertility having EMS. The pregnancy rate in this study was found to be 60.57%. Hye Jun Lee et al. [20], in the year 2013 retrospectively analyzed 43 infertile women with surgically supported endometriosis and stated that the natural conception rate for the 12 months after the laparoscopy, was found to be 41.9% without any ART or hormone treatment. EMS not only affects adult but also adolescents. Symptoms in adolescents may perhaps exist as menstrual pain or acyclic pain, harsh pain in the pelvic cavity leading to the missed school, dysmenorrhea not or poorly reacting to medical therapy. Age is the single most important issue in evaluating an ovarian age as well as an ovarian reserve and mirrors both the quantity and quality of oocytes. From a pure fertility part, postponement in conception should be avoided. Our study also supports that women <35 years conceived more compared to women >35 years. Many studies advocate that in ladies age 35 or more, more aggressive treatment such as ovulation stimulation with IUI or IVF may be considered for superior results. Laparoscopy is deliberated the most prestigious technique for identifying EMS but in the situation where the disease is in the vagina or somewhere else, it is not considered a gold standard for diagnosing. Histopathological confirmation of at least one peritoneal lesion is perfect, and compulsory if DIE or a >3 cm sized endometrioma cyst exists. A gynecologist has to inspect the whole of the pelvis to record in detail the kind, size, and degree of all implants and adhesions, to make a proper diagnosis. The surgeon should save the surgical procedure in a disk. The good method is excision or/ablation of lesions depending upon the grade of EMS. The cure is not only to alleviate the disease process but also to reinstate the productiveness of a woman’s pregnancy outcome.
The principal management is mainly by surgery. Due to minor cost and little time duration of rehabilitation of patients after the minimally invasive laparoscopic procedure, with the advanced application of laparoscopic techniques, laparoscopic surgery is the best and chosen technique to manage EMS, and the equipment has benefits in the management of EMS on the more recognizable.
Marcoux et al. conducted a randomized controlled trial on 341 ladies to find out whether laparoscopic operation heightened fecundity in infertile patients with minimal-mild EMS. They established that either resection or ablation of minimal and mild EMS vividly heightened fecundity in infertile women when compared to diagnostic laparoscopy alone (cumulative probabilities, 30.7%, and 17.7%, respectively; P = 0.006). The equivalent fecundity rates were 4.7 and 2.4 per 100-person months, individually and the absolute upsurge in the 36-weeks likelihood of a conception passed past twenty weeks that was attributable to surgery was 13 percent. They also showed no significant difference between excisional vs. ablative techniques [21].
The results of our retrospective study found that the one-year pregnancy rate of infertile patients with endometriosis was 60.57%. But at the same time, many reports from many types of research works suggest that patients can be influenced by many factors in the process of laparoscopic surgery, and then it is still difficult to get pregnant after the operation. Xin Li et al. [22] in their study demonstrated that the prospect of spontaneous conception rate after the laparoscopic surgical practice for EMS associated infertility was found to be 46.5%, which reconfirmed the value of laparoscopic surgery.
Several biologic influences, such as a bigger height or smaller weight, have been conveyed to be connected with chances of having EMS [3,23-28]. Liu Yong et al. [29] conducted a meta-analysis that included a total of 11 studies (two different cohort studies and 9 case-control studies), which suggested that higher BMI may be related to a lesser possibility of endometriosis. Ayae Yamamoto et al. [30] directed a study which revealed that EMS was diagnosed in 9.5% of participants; 3.5% also recognized a diagnosis of ovarian endometrioma, EMS occurrence in Asians was ominously greater than in Caucasians (15.7 vs. 5.8%, P<0.01), Clinical pregnancy rates were ominously lower for Asian women, specifically in Indian (P<0.05), Japanese (P<0.05), and Korean (P<0.05) women, compared to Caucasian women, even after adjusting for EMS status. Within their study participants, BMI was not a significant independent predictor of EMS, they found BMI to be lower in Asian women compared to Caucasian women. This is reliable with many earlier studies that concluded BMI to be inversely related to EMS threat. Numerous EMS staging classifications were established in past but, the rAFS grading system is the utmost extensive in the modern practice because of its broader expression of EMS extension. However, some key aspects, like the age of a woman, duration of infertility, and family history, which might impact pregnancy consequences, are not well-thought-out by rAFS. Bearing in mind the restrictions of the rAFS grading system, for example, its’ incapability to foresee patients’ likelihood of getting pregnant after the operation, Adamson and Pasta formulated the EMS Fertility Index staging system, that is grounded on both ancient and surgical features to calculate the spontaneous Pregnancy Rate after the surgery for EMS. R-AFS is the most extensively used grading system. According to our research statistics, the clinical stage of EMS is closely related to postoperative pregnancy results. The higher the stage, the more severe the lesion is, the lower is the pregnancy rate. This may be the higher the stage of the disease, the more serious the adhesion, the more difficult to remove during the laparoscopic operation, and the higher the relapse rate after the operation. In accumulation, because most of the disease includes the ovary, so the advanced phase of EMS, may distress ovarian function thus distressing the postoperative pregnancy rate. For women with moderate and severe EMS, the spontaneous pregnancy rate after laparoscopic surgery is much higher compared with those treated by expectant management [31]. A French retrospective study [32] suggested that patients with moderate and severe EMS should try to conceive naturally for 8-12 and 6-8 months, respectively, before choosing for ART. Slabuszewska-Józwiak et al.’s [33] study reported that operative laparoscopy is an effective technique to cure infertility associated with EMS and that the period for expectant management after a surgical procedure must last for at least six months.
Mireia González-Comadran et al. [34], suggested in his retrospective cohort study work that reproductive results among women undergoing IVF and diagnosed with EMS-associated infertility do not differ expressively from women without the disease. Though women with EMS produce fewer oocytes, the fertilization rate is not compromised and the chances of accomplishing a live birth are not affected.
Earlier reports showed that the overall rate of pregnancy 3-5 years after surgery was 44-46% for those with stage III-IV EMS, while statistics from past 5 years of follow-up were not accessible [35]. With concern to management of minimal and mild endometriosis in infertile patients, only two findings can be preferred, and both display that laparoscopy with excision or ablation and ablation of adhesions is excellent to diagnostic laparoscopy alone also in terms of pregnancy rate [36].
Conclusion
Endometriosis is a leading source of infertility, not only affects women’s potency also gives a great deal of pain and so it is extremely imperative to know the elements influencing pregnancy to expand the pregnancy success rate. Age of women, infertility type, Laparoscopy, use of GnRH-a after the operation, EMS stage, and operative methods were found to be significant and were found to be the factors that influenced the pregnancy outcome. However, our retrospective study has limitations so further studies are required for detailed findings.
Limitations
Retrospective studies are not ideal methods to prove a hypothesis but may show trends and results in questions deserving further studies.
Small sample size: the precision of calculation of various variable was bargained by the small sample size.
The variables available to us lack the details desirable for more thorough analyses.
As the influencing factors lacked many aspects of infertility such as the total duration of the infertility period.
Since the study is done only on the patients who underwent surgery in our hospital, the results might lack generalization to the entire population.
Acknowledgements
We would like to thank all the doctors of the Reproductive Health Center Department of Second Affiliated Hospital of Wenzhou Medical University for providing all the necessary information required for this study. Without their help, this article would not have been possible. This study was subject to approval by the Ethics Committee Board of the Second Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, People’s Republic of China. This research was funded by the Science and Technology Project of Wenzhou Y20190257.
Disclosure of conflict of interest
None.
Abbreviations
- EMS
Endometriosis
- CI
confidence interval
- GnRH-a
Gonadotrophin-releasing hormone agonist
- IUI
intrauterine insemination
- IVF
in-vitro fertilization
- OR
odds ratio
- DIE
deeply infiltrative disease
References
- 1.Kennedy S, Bergqvist A, Chapron C, D’Hooghe T, Dunselman G, Greb R, Hummelshoj L, Prentice A, Saridogan E ESHRE Special Interest Group for Endometriosis and Endometrium Guideline Development Group. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod. 2005;20:2698–2704. doi: 10.1093/humrep/dei135. [DOI] [PubMed] [Google Scholar]
- 2.Somigliana E, Daguati R, Vercellini P, Barbara G, Benaglia L, Crosignani PG. The use and effectiveness of in vitro fertilization in women with endometriosis: the surgeon’s perspective. Fertil Steril. 2009;91:1775–1779. doi: 10.1016/j.fertnstert.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Giudice LC, Kao LC. Endometriosis. Lancet. 2004;364:1789–1799. doi: 10.1016/S0140-6736(04)17403-5. [DOI] [PubMed] [Google Scholar]
- 4.Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98:511–519. doi: 10.1016/j.fertnstert.2012.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bischoff FZ, Simpson JL. Heritability and molecular genetic studies of endometriosis. Hum Reprod Update. 2000;6:37–44. doi: 10.1093/humupd/6.1.37. [DOI] [PubMed] [Google Scholar]
- 6.Adamson GD, Baker VL. Subfertility: causes, treatment and outcome. Best Pract Res Clin Obstet Gynaecol. 2003;17:169–185. doi: 10.1016/s1521-6934(02)00146-3. [DOI] [PubMed] [Google Scholar]
- 7.Practice Committee of the American Society for Reproductive Medicine. Endometriosis and infertility. Fertil Steril. 2006;86:S156–160. doi: 10.1016/j.fertnstert.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Revised American Fertility Society classification of endometriosis: 1985. Fertil Steril. 1985;43:351–352. doi: 10.1016/s0015-0282(16)48430-x. [DOI] [PubMed] [Google Scholar]
- 9.D’Hooghe TM, Debrock S, Hill JA, Meuleman C. Endometriosis and subfertility: is the relationship resolved? Semin Reprod Med. 2003;21:243–254. doi: 10.1055/s-2003-41330. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz D, Mayaux MJ. Female fecundity as a function of age: results of artificial insemination in 2193 nulliparous women with azoospermic husbands. Federation CECOS. N Engl J Med. 1982;306:404–406. doi: 10.1056/NEJM198202183060706. [DOI] [PubMed] [Google Scholar]
- 11.Akande VA, Hunt LP, Cahill DJ, Jenkins JM. Differences in time to natural conception between women with unexplained infertility and infertile women with minor endometriosis. Hum Reprod. 2004;19:96–103. doi: 10.1093/humrep/deh045. [DOI] [PubMed] [Google Scholar]
- 12.Barnhart K, Dunsmoor-Su R, Coutifaris C. Effect of endometriosis on in vitro fertilization. Fertil Steril. 2002;77:1148–1155. doi: 10.1016/s0015-0282(02)03112-6. [DOI] [PubMed] [Google Scholar]
- 13.Rock JA ZOLADEX Endometriosis Study Group. The revised American Fertility Society classification of endometriosis: reproducibility of scoring. ZOLADEX Endometriosis Study Group. Fertil Steril. 1995;63:1108–1110. doi: 10.1016/s0015-0282(16)57556-6. [DOI] [PubMed] [Google Scholar]
- 14.Tomassetti C, D’Hooghe T. Endometriosis and infertility: Insights into the causal link and management strategies. Best Pract Res Clin Obstet Gynaecol. 2018;51:25–33. doi: 10.1016/j.bpobgyn.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Hughes EG, Fedorkow DM, Collins JA. A quantitative overview of controlled trials in endometriosis-associated infertility. Fertil Steril. 1993;59:963–970. [PubMed] [Google Scholar]
- 16.Kasapoglu I, Ata B, Uyaniklar O, Seyhan A, Orhan A, Yildiz Oguz S, Uncu G. Endometrioma-related reduction in ovarian reserve (ERROR): a prospective longitudinal study. Fertil Steril. 2018;110:122–127. doi: 10.1016/j.fertnstert.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 17.Vercellini P, Maddalena S, De Giorgi O, Aimi G, Crosignani PG. Abdominal myomectomy for infertility: a comprehensive review. Hum Reprod. 1998;13:873–879. doi: 10.1093/humrep/13.4.873. [DOI] [PubMed] [Google Scholar]
- 18.Sudik R, Husch K, Steller J, Daume E. Fertility and pregnancy outcome after myomectomy in sterility patients. Eur J Obstet Gynecol Reprod Biol. 1996;65:209–214. doi: 10.1016/0301-2115(95)02363-1. [DOI] [PubMed] [Google Scholar]
- 19.Li TC, Mortimer R, Cooke ID. Myomectomy: a retrospective study to examine reproductive performance before and after surgery. Hum Reprod. 1999;14:1735–1740. doi: 10.1093/humrep/14.7.1735. [DOI] [PubMed] [Google Scholar]
- 20.Lee HJ, Lee JE, Ku SY, Kim SH, Kim JG, Moon SY, Choi YM. Natural conception rate following laparoscopic surgery in infertile women with endometriosis. Clin Exp Reprod Med. 2013;40:29–32. doi: 10.5653/cerm.2013.40.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marcoux S, Maheux R, Berube S. Laparoscopic surgery in infertile women with minimal or mild endometriosis. Canadian Collaborative Group on Endometriosis. N Engl J Med. 1997;337:217–222. doi: 10.1056/NEJM199707243370401. [DOI] [PubMed] [Google Scholar]
- 22.Li X, Zeng C, Zhou YF, Yang HX, Shang J, Zhu SN, Xue Q. Endometriosis fertility index for predicting pregnancy after endometriosis surgery. Chin Med J (Engl) 2017;130:1932–1937. doi: 10.4103/0366-6999.211892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ashrafi M, Sadatmahalleh SJ, Akhoond MR, Talebi M. Evaluation of risk factors associated with endometriosis in infertile women. Int J Fertil Steril. 2016;10:11–21. doi: 10.22074/ijfs.2016.4763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peterson CM, Johnstone EB, Hammoud AO, Stanford JB, Varner MW, Kennedy A, Chen Z, Sun L, Fujimoto VY, Hediger ML, Buck Louis GM ENDO Study Working Group. Risk factors associated with endometriosis: importance of study population for characterizing disease in the ENDO Study. Am J Obstet Gynecol. 2013;208:451.e1–11. doi: 10.1016/j.ajog.2013.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moini A, Malekzadeh F, Amirchaghmaghi E, Kashfi F, Akhoond MR, Saei M, Mirbolok MH. Risk factors associated with endometriosis among infertile Iranian women. Arch Med Sci. 2013;9:506–514. doi: 10.5114/aoms.2013.35420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hemmings R, Rivard M, Olive DL, Poliquin-Fleury J, Gagne D, Hugo P, Gosselin D. Evaluation of risk factors associated with endometriosis. Fertil Steril. 2004;81:1513–1521. doi: 10.1016/j.fertnstert.2003.10.038. [DOI] [PubMed] [Google Scholar]
- 27.Signorello LB, Harlow BL, Cramer DW, Spiegelman D, Hill JA. Epidemiologic determinants of endometriosis: a hospital-based case-control study. Ann Epidemiol. 1997;7:267–741. doi: 10.1016/s1047-2797(97)00017-3. [DOI] [PubMed] [Google Scholar]
- 28.Upson K, Sathyanarayana S, Scholes D, Holt VL. Early-life factors and endometriosis risk. Fertil Steril. 2015;104:964–971. e965. doi: 10.1016/j.fertnstert.2015.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu Y, Zhang W. Association between body mass index and endometriosis risk: a meta-analysis. Oncotarget. 2017;8:46928–46936. doi: 10.18632/oncotarget.14916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yamamoto A, Johnstone EB, Bloom MS, Huddleston HG, Fujimoto VY. A higher prevalence of endometriosis among Asian women does not contribute to poorer IVF outcomes. J Assist Reprod Genet. 2017;34:765–774. doi: 10.1007/s10815-017-0919-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vercellini P, Fedele L, Aimi G, De Giorgi O, Consonni D, Crosignani PG. Reproductive performance, pain recurrence and disease relapse after conservative surgical treatment for endometriosis: the predictive value of the current classification system. Hum Reprod. 2006;21:2679–2685. doi: 10.1093/humrep/del230. [DOI] [PubMed] [Google Scholar]
- 32.Fuchs F, Raynal P, Salama S, Guillot E, Le Tohic A, Chis C, Panel P. Reproductive outcome after laparoscopic treatment of endometriosis in an infertile population. J Gynecol Obstet Biol Reprod (Paris) 2007;36:354–359. doi: 10.1016/j.jgyn.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 33.Slabuszewska-Jozwiak A, Ciebiera M, Baran A, Jakiel G. Effectiveness of laparoscopic surgeries in treating infertility related to endometriosis. Ann Agric Environ Med. 2015;22:329–331. doi: 10.5604/12321966.1152089. [DOI] [PubMed] [Google Scholar]
- 34.Gonzalez-Comadran M, Schwarze JE, Zegers-Hochschild F, Souza MD, Carreras R, Checa MA. The impact of endometriosis on the outcome of assisted reproductive technology. Reprod Biol Endocrinol. 2017;15:8. doi: 10.1186/s12958-016-0217-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang X, Liu D, Huang W, Wang Q, Feng X, Tan J. Prediction of Endometriosis Fertility Index in patients with endometriosis-associated infertility after laparoscopic treatment. Reprod Biomed Online. 2018;37:53–59. doi: 10.1016/j.rbmo.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 36.Ploteau S, Merlot B, Roman H, Canis M, Collinet P, Fritel X. Minimal and mild endometriosis: impact of the laparoscopic surgery on pelvic pain and fertility. CNGOF-HAS Endometriosis Guidelines. Gynecol Obstet Fertil Senol. 2018;46:273–277. doi: 10.1016/j.gofs.2018.02.004. [DOI] [PubMed] [Google Scholar]


