Abstract
Objective: To explore the effect of palliative care on the psychological well-being and sleep quality of the primary caregivers of elderly patients with terminal cancer. Methods: In this prospective study, a total of 102 elderly patients with terminal cancer and their primary caregivers were randomly divided into a study group and a control group of 51 patients each by a random number table. The control group was given routine end-of-life care and the study group was given palliative care. In this study, we compared adverse mood, sleep quality, psychological stress and satisfaction with care among primary caregivers before and after the intervention, as well as changes in patients’ quality of life. Results: The Hamilton Anxiety Scale (HAMA), the Hamilton Depression Scale (HAMD), the Pittsburgh Sleep Quality Index (PSQI), and RSS scores of the primary caregiver were significantly lower in both groups after the intervention, and significantly lower in the study group (all P<0.05). The Generic Quality of Life Inventory-74 (GQOLI-74) scores were significantly higher in both groups after the intervention, and significantly higher in the study group (all P<0.05). In addition, the primary caregiver’s satisfaction with care was significantly higher in the study group than that in the control group (96.08% vs. 82.35%, P<0.05). Conclusion: Palliative care for patients with terminal cancer can be effective in alleviating the poor psychological well-being of the primary caregivers, improving their sleep quality as well as improving nursing satisfaction and patients’ quality of life.
Keywords: Terminal patient, primary caregiver, palliative care, poor psychology, sleep quality
Introduction
Malignant tumors, especially advanced malignant tumors, have extremely limited survival time. For this special group of elderly patients with terminal tumors, their psychological, physical, care environment and social needs are different from those of patients with other diseases. Therefore, it has become a new challenge for medical institutions and medical personnel at all levels to take reasonable measures to improve the quality of life of terminal patients before they pass away [1,2]. For primary caregivers of terminal patients, factors such as the impending death of a loved one and the cost of treatment are sources of distress. Primary caregivers suffer physically and psychologically and often experience a variety of negative emotions [3,4]. Therefore, health care professionals should also focus on the psychological state and sleep quality of primary caregivers of terminal patients. Conventional end-of-life care focuses on the patient’s own condition and often neglects the psychological feelings of the primary caregiver, whereas palliative care can compensate for these deficiencies. Palliative care is a humanistic medical service model that focuses on terminal patients and their families, with multidisciplinary collaboration aimed at alleviating pain and improving the quality of life of patients and their families. It mainly includes the pain control, spiritual, psychological and social support, and comfortable care, and has attracted much attention in the medical community in recent years [5]. The aim of this study was to investigate the effect of palliative care on psychological well-being and sleep quality in primary caregivers of elderly patients with terminal cancer.
Materials and methods
General information
In this prospective study, a total of 102 elderly patients with terminal cancer and their primary caregivers who were admitted to Huiqiao Medical Center, Nanfang Hospital, Southern Medical University from July 2019 to July 2020 were divided into a study group and a control group of 51 patients each by random number table. The general information of the two groups of patients and their primary caregivers was shown in Table 1. This study was approved by the Medical Ethics Committee of Huiqiao Medical Center, Nanfang Hospital, Southern Medical University.
Table 1.
Comparison of general information between the two groups of patients (n, x̅ ± sd)
| Study group (n=51) | Control group (n=51) | χ2/t | P | |
|---|---|---|---|---|
| Gender (n) | 0.630 | 0.427 | ||
| Male | 29 | 25 | ||
| Female | 22 | 26 | ||
| Age (years) | 74.4±5.4 | 75.1±6.3 | 0.602 | 0.548 |
| BMI (kg/m2) | 22.72±2.01 | 22.43±2.14 | 0.705 | 0.482 |
| Cancer type (n) | 0.775 | 0.723 | ||
| Liver cancer | 13 | 15 | ||
| Stomach cancer | 11 | 8 | ||
| Lung cancer | 9 | 10 | ||
| Breast cancer | 5 | 6 | ||
| Ovarian cancer | 5 | 4 | ||
| Colorectal cancer | 4 | 5 | ||
| Other | 4 | 3 | ||
| Knowledge of the condition (n) | 0.706 | 0.703 | ||
| Understand all | 26 | 23 | ||
| Partial understanding | 22 | 23 | ||
| Don’t understand | 3 | 5 |
Patients had an age range of 65-85 years while the primary caregivers had an age range of 25-55 years. The immediate family members of the dying patient whose understanding and expression ability were normal can be the primary caregivers. All of the enrolled subjects have signed informed consent.
Exclusion criteria: patients with severe cognitive impairment and unable to complete the questionnaire independently; patients whose primary caregivers were accompanied by severe heart, liver, brain, or kidney disease.
Methods
The control group was given routine end-of-life care, such as room disinfection, 24-hour monitoring of vital signs, medication on time according to doctor’s orders, routine treatment such as nutritional support, immunotherapy or radiotherapy, and comfort for the primary caregivers to arrange work and rest properly and improve their mood.
On this basis, the study group was given the following palliative care [6]: (1) Health care providers built good relationships with patients and their primary caregivers through face-to-face communication, which was extremely important throughout the palliative care process. (2) Death education enabled patients to maintain a good attitude in the limited time before death, so that they and their primary caregivers could accept the reality calmly. (3) Medical staff instilled the concept of peaceful death to the primary caregivers of dying patients. Picture books, movies and videos were used to let family members understand that the end of life is a natural rule, or patients were suggested to set up “living will”, and relevant treatments were adopted before death according to the wishes of patients, so as to reduce the invasive treatment measures before death. (4) Medical staff actively adopted symptomatic conservative treatment to alleviate the suffering of terminal patients. (5) Medical personnel provided psychological guidance. It was almost impossible to cure elderly patients with terminal cancer, so it was inevitable that the primary caregivers would have excessive grief, and in severe cases, it might lead to depression and anxiety. Therefore, it was necessary to provide psychological guidance and appropriate comfort to the primary caregivers, listen to the pain in their hearts and empathize with them, help the family members to sort out the patient’s life story together, find positive events in the story, help patients construct the meaning of their life, assist the family members to conduct psychological reconstruction, and bid the best farewell.
Outcome measures
Primary outcome measures
In this study, the pre-intervention time was defined as the time between diagnosis of advanced malignancy and hospitalization for treatment. The post-intervention time was the days from clinician assessment to the death of the terminal patient. All scales were completed and collected on the spot with a 100% recovery rate.
The Hamilton Anxiety Scale (HAMA) and the Hamilton Depression Scale (HAMD) (17 items) were used to assess changes in the primary caregiver’s psychological state before and after the intervention [7,8]. The higher the score, the worse the anxiety and depression was.
Before and after the intervention, the Pittsburgh Sleep Quality Index (PSQI) was used to assess the sleep quality of the primary caregivers [9]. The PSQI has a total of 18 points, the lower the score, the better the sleep quality was.
Secondary outcome measures
Before and after the intervention, patients’ quality of life was assessed using the Generic Quality of Life Inventory-74 (GQOLI-74), which includes four dimensions of social function, psychological function, physical function, and material well-being, and the quality of life is improved with increasing scores [10].
Before and after the intervention, the Relative Stress Scale (RSS) was used to assess the psychological stress of the primary caregivers, including psychological distress, disrupted life, and negative emotions, with higher scores indicating higher levels of stress [11].
Nursing satisfaction survey scale was used to compare the satisfaction of the primary caregivers of the two groups of patients with regard to nursing care [12]. Satisfaction = (Satisfied + Basically Satisfied) number of cases/total number of cases × 100%.
Statistical analysis
With SPSS 20.0 for data statistics, counting data were expressed in the number of cases/percentage (n/%), and the comparison was performed by χ2 test. Measurement data conforming to normal distribution were expressed as the mean ± standard deviation (x̅ ± sd). The comparison between the same group before and after intervention was performed by paired t test, and the comparison between the two groups was performed by independent t test. P<0.05 was considered statistically significant.
Results
Comparison of general information of the two groups of patients and primary caregivers
The comparison of general data showed that the difference between the two groups of patients and their primary caregivers was not statistically significant (P>0.05), and there was comparability between the groups, as shown in Tables 1, 2.
Table 2.
Comparison of general information between the two groups of primary caregivers (n, x̅ ± sd)
| Study group (n=51) | Control group (n=51) | χ2/t | P | |
|---|---|---|---|---|
| Gender (n) | 0.639 | 0.424 | ||
| Male | 24 | 20 | ||
| Female | 27 | 31 | ||
| Age (years) | 36.4±3.7 | 37.5±4.2 | 1.403 | 0.164 |
| BMI (kg/m2) | 23.40±2.32 | 23.28±2.05 | 0.277 | 0.783 |
| Smoking habit (n) | 0.060 | 0.807 | ||
| Yes | 10 | 11 | ||
| No | 41 | 40 | ||
| Drinking habits (n) | 0.635 | 0.425 | ||
| Yes | 7 | 10 | ||
| No | 44 | 41 | ||
| Relationship with patients (n) | 0.706 | 0.401 | ||
| Spouse | 19 | 15 | ||
| Child | 32 | 36 | ||
| Family income (yuan/month) | 1.595 | 0.450 | ||
| <5000 | 7 | 9 | ||
| 5000-10000 | 36 | 30 | ||
| >10000 | 8 | 12 | ||
| Knowledge of routine care (n) | 0.088 | 0.767 | ||
| Yes | 6 | 7 | ||
| No | 45 | 44 |
HAMA, HAMD scores
The HAMA and HAMD scores of the primary caregivers were significantly lower in both groups after the intervention (all P<0.05) and significantly lower in the study group than the control group (P<0.001), as shown in Table 3.
Table 3.
Comparison of HAMA and HAMD scores between the two groups of primary caregivers before and after the intervention (x̅ ± sd)
| Group | Time | HAMA score | HAMD score |
|---|---|---|---|
| Study group (n=51) | Before intervention | 13.56±2.44 | 7.10±1.95 |
| After intervention | 9.44±2.53***,### | 4.55±1.17***,### | |
| Control group (n=51) | Before intervention | 13.10±2.94 | 7.40±2.11 |
| After intervention | 11.70±3.18* | 6.52±1.40* |
Note: Compared with before intervention;
P<0.05;
P<0.001.
Compared with control group after intervention;
P<0.001.
HAMA: the Hamilton Anxiety Scale; HAMD: the Hamilton Depression Scale.
PSQI scores
Before the intervention, the PSQI scores of the primary caregivers in the study and control groups were 14.30±2.55 and 13.96±2.40, respectively. After the intervention, the PSQI scores in the two groups were 10.32±2.06 and 12.53±2.31, respectively. Statistical analysis showed that the PSQI scores in both groups were significantly lower after the intervention (P<0.01), and significantly lower in the study group than the control group (P<0.001), as shown in Figure 1.
Figure 1.
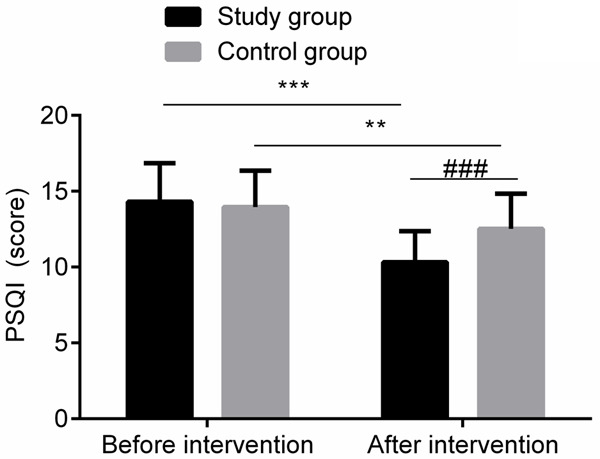
Comparison of PSQI scores between the two groups of primary caregivers before and after the intervention. Compared with before intervention, **P<0.01, ***P<0.001; Compared with control group after intervention, ###P<0.001. PSQI: the Pittsburgh Sleep Quality Index.
GQOLI-74 scores
After the intervention, the GQOLI-74 scores of the two groups of patients were significantly increased, and the study group was significantly higher than the control group (all P<0.05), as shown in Table 4.
Table 4.
Comparison of GQOLI-74 scores between the two groups of patients before and after intervention (x̅ ± sd, scores)
| Group | Social function | Psychological function | Physical function | Material well-being |
|---|---|---|---|---|
| Study group (n=51) | ||||
| Before intervention | 45.40±5.44 | 40.03±4.20 | 41.60±4.08 | 33.06±4.04 |
| After intervention | 48.96±4.39***,# | 45.30±5.30***,## | 45.96±4.39***,# | 37.94±4.29***,# |
| Control group (n=51) | ||||
| Before intervention | 45.14±4.85 | 40.12±5.33 | 42.04±4.20 | 33.85±4.85 |
| After intervention | 47.03±4.22* | 42.22±4.90* | 43.95±4.75* | 35.97±5.22* |
Note: Compared with before intervention;
P<0.05;
P<0.001.
Compared with control group after intervention;
P<0.05;
P<0.01.
GQOLI-74: the Generic Quality of Life Inventory-74.
RSS scores
After the intervention, the RSS scores of the primary caregivers of the two groups were significantly reduced, and the scores in the study group was significantly lower than the control group (all P<0.05), as shown in Table 5.
Table 5.
Comparison of RSS scores between the two groups of primary caregivers before and after the intervention (x̅ ± sd, scores)
| Group | Psychological distress | Disrupted life | Negative emotions |
|---|---|---|---|
| Study group (n=51) | |||
| Before intervention | 6.50±1.84 | 6.47±1.95 | 7.04±1.94 |
| After intervention | 5.04±1.52***,# | 5.08±1.19***,### | 5.86±1.10***,### |
| Control group (n=51) | |||
| Before intervention | 6.44±1.95 | 6.77±1.70 | 7.28±1.30 |
| After intervention | 5.64±1.20* | 6.12±1.05* | 6.69±1.09* |
Note: Compared with before intervention;
P<0.05;
P<0.001.
Compared with control group after intervention;
P<0.05;
P<0.001.
RSS: Relative Stress Scale.
Nursing satisfaction
The satisfaction of the primary caregivers in the study group was significantly higher than that of the control group (χ2=4.993, P=0.025), as shown in Table 6.
Table 6.
Comparison of satisfaction with nursing care between the two groups of primary caregivers (n, %)
| Group | Satisfied | Basically satisfied | Dissatisfied | Satisfaction |
|---|---|---|---|---|
| Study group (n=51) | 30 (58.82) | 19 (37.25) | 2 (3.92) | 49 (96.08)# |
| Control group (n=51) | 22 (43.14) | 20 (39.22) | 9 (17.65) | 42 (82.35) |
Note: Compared with the control group;
P<0.05.
Discussion
It is a fact that patients with terminal cancer have only a short time to live and will die in the near future, so they are a source of stress for the whole family especially for the primary caregivers [13]. The primary caregivers of elderly patients with terminal cancer are mostly their children or spouses, who are closely related to the patients. In the face of high treatment costs, their children need to suspend work in order to give their parents more comprehensive care and take care of their patients’ daily life, and additionally the pain of the impending death of their loved ones makes the primary caregivers physically and mentally exhausted. Stress from both psychological and spiritual burden often leads to varying degrees of anxiety, depression, and other adverse emotions in the primary caregivers of terminal patients with malignant tumors [14].
Pettifer et al. found that 5.7% to 11.3% of primary caregivers of terminal patients had psychological disorders of varying degrees, which not only affected their own physical health, but also indirectly affected the patients [15]. Therefore, clinical staff should not only take into account the patient’s condition and psychological changes, but also pay attention to the primary caregiver’s psychological changes and other problems, such as sleep disorders, stress reactions, etc. As soon as psychological fluctuations or sleep problems were obvious in the primary caregiver, interventions to ameliorate these problems should be implemented. Palliative care was a marginal cross-discipline and one of the most important symbols of the progress of human civilization and the advancement of health care. The essence of palliative care was philosophy for caring, the main purpose of which was to reduce the suffering of terminal patients before they die, to improve their quality of life, and to enable patients and their primary caregivers to face and accept the news of their impending death and face death correctly [16].
This study compared the psychological changes of the two groups of terminal patients and their primary caregivers (the study group was given palliative care and the control group was not). The results showed that the HAMA, HAMD and RSS scores of the primary caregivers of the two groups decreased after the intervention, and the scores in the study group were lower than those in the control group, suggesting that the application of palliative care can significantly improve the adverse psychological state and reduce the stress level of the primary caregivers of elderly patients with terminal cancer. This conclusion was consistent with report of related research, and it was speculated that indoctrination of death education, peaceful death and grief counseling in nursing care had improved the acceptance of the primary caregivers of terminal patients facing the fact that their relatives were about to leave [17]. This improved the primary caregiver’s acceptance of the impending death of their loved one, and allowed them to face the day with a calmer state of mind, thus improving the primary caregiver’s psychological mood and alleviating or reducing their stress response. The study by Lief et al. concluded that family members of terminal patients had more severe adverse psychological and stress states, and that the stress level of relatives was positively correlated with adverse emotions [18]. Chow et al. had similar findings, but they also found that adverse psychological and stress reactions were more severe when the primary caregivers were female [19]. This was not studied in the present study and was a point that needed to be further investigated in the future.
The primary caregivers of elderly terminal patients have great psychological and mental pressure, especially for those who are children. In order to take better care of their parents, children must take a break from work, but most of them are already mothers or fathers, so the pressures of living with the old and the young and dying parents in the hospital are important sources of stress. However, high levels of stress are an independent risk factor for sleep disorders, which can occur from time to time and are often severe for these individuals. Bernatchez et al. noted that the proportion of sleep disorders in the primary caregivers of terminal patients can be as high as 19.5% [20]. In this study, we compared the sleep quality of primary caregivers of terminal patients in two groups and found that the PSQI scores in the study group were lower than those of the control group after the intervention, suggesting that for elderly patients with terminal cancer, the use of palliative care can significantly improve their primary caregiver’s sleep quality, which was consistent with the findings reported by Bernatchez et al. [21]. In addition, it was also found in this study that the GQOLI-74 scores were higher in the study group than in the control group after the intervention, suggesting that palliative care helped to improve the quality of life of terminal patients before they passed away, and similar results were found in the study by Maree et al. [22]. Finally, the results of this study showed that the primary caregivers of the patients in the study group were more satisfied with their care, indicating that applying the palliative care to elderly patients with terminal cancer can improve their primary caregiver’s satisfaction with their care. However, the present study was a single-center study with limited sample size and limited observational parameters. In the future, a larger sample size is needed to conduct a multicenter, large-sample clinical randomized controlled study to demonstrate the benefits of the palliative care for terminal patients and their primary caregivers.
In summary, palliative care can significantly alleviate the adverse psychological well-being of the primary caregivers of elderly patients with terminal cancer, improve their sleep quality, increase nursing satisfaction, and at the same time improve the quality of life of patients, which is worthy of clinical promotion.
Disclosure of conflict of interest
None.
References
- 1.Peters CML, de Vries J, Lodder P, van der Laan L. Is a good quality of life and health status possible in older patients dying from critical limb-threatening ischemia: a prospective clinical study. Ann Vasc Surg. 2020;64:198–201. doi: 10.1016/j.avsg.2019.10.042. [DOI] [PubMed] [Google Scholar]
- 2.Verreault R, Arcand M, Misson L, Durand PJ, Kroger E, Aubin M, Savoie M, Hadjistavropoulos T, Kaasalainen S, Bédard A, Grégoire A, Carmichael PH. Quasi-experimental evaluation of a multifaceted intervention to improve quality of end-of-life care and quality of dying for patients with advanced dementia in long-term care institutions. Palliat Med. 2018;32:613–621. doi: 10.1177/0269216317719588. [DOI] [PubMed] [Google Scholar]
- 3.Weisse CS, Melekis K, Hutchins B. Providing end-of-life care: increased empathy and self-efficacy among student caregivers in residential homes for the dying. Am J Hosp Palliat Care. 2019;36:538–545. doi: 10.1177/1049909118820844. [DOI] [PubMed] [Google Scholar]
- 4.Carolan CM, Smith A, Forbat L. Conceptualising psychological distress in families in palliative care: findings from a systematic review. Palliat Med. 2015;29:605–632. doi: 10.1177/0269216315575680. [DOI] [PubMed] [Google Scholar]
- 5.Robinson MT, Holloway RG. Palliative care in neurology. Mayo Clin Proc. 2017;92:1592–1601. doi: 10.1016/j.mayocp.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Schlick CJR, Bentrem DJ. Timing of palliative care: when to call for a palliative care consult. J Surg Oncol. 2019;120:30–34. doi: 10.1002/jso.25499. [DOI] [PubMed] [Google Scholar]
- 7.Zimmerman M, Martin J, Clark H, McGonigal P, Harris L, Holst CG. Measuring anxiety in depressed patients: a comparison of the hamilton anxiety rating scale and the DSM-5 anxious distress specifier interview. J Psychiatr Res. 2017;93:59–63. doi: 10.1016/j.jpsychires.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 8.Raimo S, Trojano L, Spitaleri D, Petretta V, Grossi D, Santangelo G. Psychometric properties of the hamilton depression rating scale in multiple sclerosis. Qual Life Res. 2015;24:1973–1980. doi: 10.1007/s11136-015-0940-8. [DOI] [PubMed] [Google Scholar]
- 9.Del Rio João KA, Becker NB, de Neves Jesus S, Martins RIS. Validation of the portuguese version of the pittsburgh sleep quality index (PSQI-PT) Psychiatry Res. 2017;247:225–229. doi: 10.1016/j.psychres.2016.11.042. [DOI] [PubMed] [Google Scholar]
- 10.Zhou Y, Zhou RS, Li WJ, Lin YQ, Yao J, Chen J, Shen T. Controlled trial of the effectiveness of community rehabilitation for patients with schizophrenia in Shanghai, China. Shanghai Arch Psychiatry. 2015;27:167–174. doi: 10.11919/j.issn.1002-0829.215026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oh H, Lee S, Kim J, Lee E, Min H, Cho O, Seo W. Clinical validity of a relocation stress scale for the families of patients transferred from intensive care units. J Clin Nurs. 2015;24:1805–1814. doi: 10.1111/jocn.12778. [DOI] [PubMed] [Google Scholar]
- 12.McNicholas A, McCall A, Werner A, Wounderly R, Marinchak E, Jones P. Improving patient experience through nursing satisfaction. J Trauma Nurs. 2017;24:371–375. doi: 10.1097/JTN.0000000000000328. [DOI] [PubMed] [Google Scholar]
- 13.Kanno Y, Sato K, Shimizu M, Funamizu Y, Andoh H, Kishino M, Senaga T, Takahashi T, Miyashita M. Validity and reliability of the dying care process and outcome scales before and after death from the bereaved family members’ perspective. Am J Hosp Palliat Care. 2019;36:130–137. doi: 10.1177/1049909118785178. [DOI] [PubMed] [Google Scholar]
- 14.Kinoshita H, Maeda I, Morita T, Miyashita M, Yamagishi A, Shirahige Y, Takebayashi T, Yamaguchi T, Igarashi A, Eguchi K. Place of death and the differences in patient quality of death and dying and caregiver burden. J. Clin. Oncol. 2015;33:357–363. doi: 10.1200/JCO.2014.55.7355. [DOI] [PubMed] [Google Scholar]
- 15.Pettifer A, Froggatt K, Hughes S. The experiences of family members witnessing the diminishing drinking of a dying relative: an adapted meta-narrative literature review. Palliat Med. 2019;33:1146–1157. doi: 10.1177/0269216319859728. [DOI] [PubMed] [Google Scholar]
- 16.Davies EA. Why we need more poetry in palliative care. BMJ Support Palliat Care. 2018;8:266–270. doi: 10.1136/bmjspcare-2017-001477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klop HT, de Veer AJE, van Dongen SI, Francke AL, Rietjens JAC, Onwuteaka-Philipsen BD. Palliative care for homeless people: a systematic review of the concerns, care needs and preferences, and the barriers and facilitators for providing palliative care. BMC Palliat Care. 2018;17:67–72. doi: 10.1186/s12904-018-0320-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lief L, Berlin DA, Maciejewski RC, Westman L, Su A, Cooper ZR, Ouyang DJ, Epping G, Derry H, Russell D, Gentzler E, Maciejewski PK, Prigerson HG. Dying patient and family contributions to nurse distress in the ICU. Ann Am Thorac Soc. 2018;15:1459–1464. doi: 10.1513/AnnalsATS.201804-284OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chow K, Dahlin C. Integration of palliative care and oncology nursing. Semin Oncol Nurs. 2018;34:192–201. doi: 10.1016/j.soncn.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Bernatchez MS, Savard J, Savard MH, Aubin M. Feasibility of a cognitive-behavioral and environmental intervention for sleep-wake difficulties in community-dwelling cancer patients receiving palliative care. Cancer Nurs. 2019;42:396–409. doi: 10.1097/NCC.0000000000000603. [DOI] [PubMed] [Google Scholar]
- 21.Bernatchez MS, Savard J, Ivers H. Disruptions in sleep-wake cycles in community-dwelling cancer patients receiving palliative care and their correlates. Chronobiol Int. 2018;35:49–62. doi: 10.1080/07420528.2017.1381615. [DOI] [PubMed] [Google Scholar]
- 22.Maree JE, Van Rensburg JJ. Suitability of quality-of-life outcome measures in palliative care in the South African setting. Palliat Support Care. 2016;14:118–128. doi: 10.1017/S1478951515000036. [DOI] [PubMed] [Google Scholar]


