Abstract
Objective: This study aimed to investigate the effects of community-based rehabilitation (CBR) on the self-efficacy and quality of life in elderly patients with chronic obstructive pulmonary disease (COPD). Method: Eighty-one elderly patients with COPD admitted to our hospital were recruited as the study cohort and were randomly divided into a control group (n=41) and a study group (n=40). The control group underwent outpatient rehabilitative treatment, and the study group additionally underwent CBR. The treatment effects of the two groups at 1 month, 3 months, and 6 months of intervention were assessed using their pulmonary function and quality of life scores. Results: After completion of the CBR, the patients in the study group and the control group were scored using the CSES scale, which did not differ at 1 month of intervention, but the scores were higher in the study group than they were in the control group at 3 and 6 months of intervention (P < 0.05). The patients in the study group also scored higher on the WHOQOL-BREF scale than the control group (P < 0.05). Conclusion: CBR improves the self-efficacy and quality of life in elderly patients with COPD.
Keywords: Chronic obstructive pulmonary disease, community-based rehabilitation, self-efficacy, quality of life
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic, non-communicable disease characterized by airflow limitation and persistent respiratory symptoms, with common symptoms such as chest tightness, chronic cough, wheezing, dyspnea, and shortness of breath. Some patients experience multiple complications such as stroke, heart disease, skeletal muscle atrophy, and depression [1-3]. Chronic hypoxia can lead to shrunken lobes and cognitive functional changes [4], and, if uncontrolled, can advance to pulmonary heart disease and even respiratory failure. COPD is characterized by a complex etiology and a high morbidity and mortality, and it presents with progressive exacerbations which impose a heavy burden on the patients and their families. Currently, the treatment of COPD mainly focuses on the symptoms in the acute phase while neglecting the stable phase, which is the optimal period for patients to recover, and if the patients are treated actively and effectively during the stable phase, the treatment effect and efficacy can be greatly enhanced. Community-based rehabilitation (CBR) is a strategy within community development for the rehabilitation, equalization of opportunities, and social integration of all people with disabilities. CBR is implemented through the combined efforts of disabled people themselves, their families and communities, and the appropriate health, education, vocational and social services, which can improve lung function, quality of life, mitigate the risk of acute exacerbations, and reduce the consumption of medical resources.
The aim of this study was to apply CBR in the treatment of elderly patients with COPD, to analyze the dynamic effects of CBR on patients’ self-efficacy and quality of life, and to provide a theoretical basis for accelerating the rehabilitation as well as improving the prognoses of elderly patients with COPD.
Methods and materials
General information
A total of 81 elderly patients with COPD, admitted from January 2019 to January 2020 to the Respiratory Medicine Department of our hospital, aged 65-80 years, and meeting the diagnostic criteria of the Global Initiative for Chronic Obstructive Pulmonary Disease (2019 edition) [5] were enrolled, including 55 males and 26 females, aged 65-80 years, with an average age of (72.57 ± 4.98) years.
Exclusion criteria: patients with cerebral infarction, dementia, cerebral hemorrhage, or other serious neurological diseases, severe liver or kidney dysfunction, tumors, severe cardiovascular or cerebrovascular diseases, cognitive dysfunction, and patients who could not communicate normally.
The 81 subjects were randomly divided into the control group (n=41) and the study group (n=40) . Among them, there were 27 males and 14 females in the control group, with an average age of (72.54 ± 4.91) years, and 28 males and 12 females in the study group, with an average age of (72.32 ± 5.26) years. The two groups were comparable in terms of their baseline data (P > 0.05).
Personal files were established for all the patients, and an informed consent form was signed. This study was reviewed and approved by the ethics committee of Nantong Hospital of Traditional Chinese Medicine.
Intervention methods
After being discharged from the hospital, the control group received regular outpatient rehabilitative treatment.
At the same time, the study group was given CBR combined with outpatient rehabilitative treatment. Intervention measurements were developed according to the patients’ ages, physical conditions, and severity of COPD. The specific CBR measures were as follows.
Rehabilitation education
Professionals were invited to give lectures on the mechanism, clinical manifestations, and symptoms of COPD, to offer training on the use of expectorants and bronchodilators, to encourage patients to quit smoking and drinking alcohol, to avoid spicy, cold, and other stimulating foods, to encourage the patients to develop good habits, and to strengthen the patients’ confidence in the treatment [6,7].
Breathing exercises
The nursing staffs instructed the patients in breathing exercises and introduced the use of an assisted breathing apparatus. Pursed lip breathing was demonstrated and explained, i.e., you do this after inhaling by puckering your lips and exhaling through them slowly and deliberately, often to a count. Diaphragmatic breathing was performed, which is breathing that is done by contracting the diaphragm, a muscle located horizontally between the thoracic cavity and abdominal cavity. Air enters the lungs, the chest does not rise, and the belly expands during this type of breathing.
Exercise
According to the patients’ different conditions, the physical condition of each patient was evaluated to customize the personalized exercise plans. Exercise can take the form of regular walking, cycling, using a treadmill to exercise, etc. The 6 min walking distance can reflect the effectiveness of daily exercise.
Psychological counseling
Patients with negative emotions such as emotional anxiety, depression, and boredom can seek help from psychologists.
Observation indexes
Analysis of the changes in self-efficacy before and after the intervention
The self-efficacy of the two groups was assessed using the Self-Efficacy Scale (CSES) at pre-intervention, and at 1 month, 3 months, and 6 months of intervention, respectively. The COPD Patient Self-Efficacy Scale (CSES) was developed by scholars Wigal, Creer, and Kotses in 1991, and it is a self-administered tool used to assess self-efficacy in managing dyspnea in patients with COPD. The CSES scale consists of 34 items on a 5-likert scale, with Cronbach’s α=0.95 and retest reliability r=0.77. Patients rate their ability to confidently control their breathing in a variety of situations (including emotions, vulnerable environments, and physical exertion), with a score of 1 being not at all confident and 5 being very confident, the higher the score, the higher the level of self-efficacy [8-10].
Analysis of the changes in quality of life before and after the intervention
The quality of life was assessed using the World Health Organization Quality of Life Measurement Scale (WHOQOL-BREF) at pre-intervention, 1 month, 3 months, and 6 months, respectively. The WHOQOL-BREF scale, a simplified version of the WHOQOL-100 [11], is based on four domains, namely the physiological, psychological, social and environmental domains [12]. Although it is different from the original concept of the WHO6-domain model, it is consistent with the empirical results of the previous WHOQOL-100 Field Trial Version [13]. Higher scores indicate a better quality of life [14].
Statistical methods
The collected data were entered into IBM SPSS 21.0 software for statistical analysis. GraphPad Prism 8 was used to create the statistical plots. The measurement data (x̅ ± s) were tested using t-tests, with P < 0.05 indicating a significant difference [15].
Results
Comparison of the differences in the baseline data between the two groups of patients
It was found that the patients in the control and study groups were comparable in terms of their baseline data such as sex, age, weight, years of education, duration of the disease course, smoking history, income status, and marital status (P > 0.05) (Table 1).
Table 1.
Comparison of baseline data between the two groups (x̅ ± s)/[n (%)]
| General data | Control group (n=41) | Study group (n=40) | t/X2 | P | |
|---|---|---|---|---|---|
| Gender | Male | 27 | 28 | 0.148 | 0.712 |
| Female | 14 | 12 | |||
| Average age (years) | 72.54 ± 4.91 | 72.32 ± 5.26 | 0.176 | 0.861 | |
| Average duration (years) | 6.68 ± 3.86 | 6.49 ± 3.99 | 0.232 | 0.818 | |
| Average weight (kg) | 58.09 ± 7.50 | 57.65 ± 7.84 | 0.345 | 0.732 | |
| Education level | Below middle school | 21 | 22 | 0.378 | 0.742 |
| High school | 12 | 12 | |||
| University and above | 8 | 6 | |||
| Average smoking history (years) | 14.34 ± 11.05 | 13.63 ± 9.12 | 0.299 | 0.766 | |
| Monthly income | ≤ 3000 | 15 | 13 | 0.027 | 0.978 |
| 3000-5000 | 21 | 21 | |||
| ≥ 5000 | 5 | 6 | |||
| Marital status | Married | 34 | 31 | 0.115 | 0.741 |
| Single | 7 | 9 | |||
Changes in self-efficacy before and after the intervention
The CSES scores of the control group (3.02 ± 1.39) and the study group (2.98 ± 1.46) did not differ significantly before the intervention (P > 0.05), and both groups’ scores showed a significant improvement after the intervention. At 1 month of intervention, the difference in the CSES scores between the two groups was not significant (P > 0.05). At 3 and 6 months of intervention, the study group was (3.80 ± 0.97) and (4.03 ± 0.86), respectively, and the control group was (3.32 ± 1.19) and (3.35 ± 1.17), respectively, and the CSES scores were significantly higher in the study group than they were in the control group (P < 0.05) (Figure 1).
Figure 1.
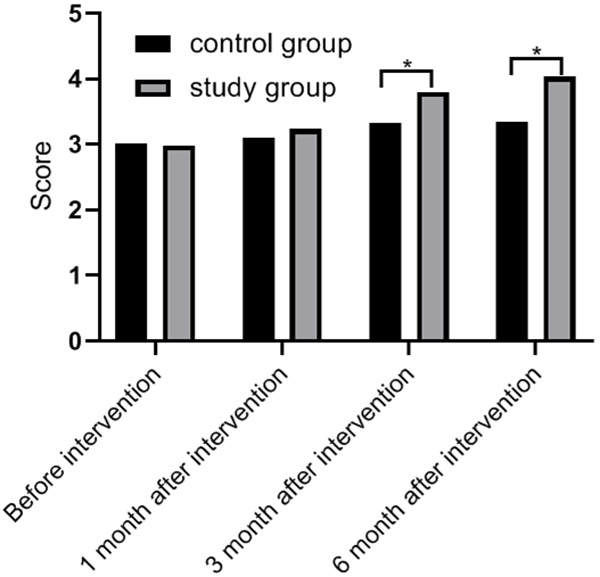
Analysis of the changes in the self-efficacy scores before and after the intervention in the two groups. *P < 0.05 compared with the control group.
Changes in the quality of life before and after the intervention
The WHOQOL-BREF scores were not significantly different (P > 0.05) in the four dimensions before the intervention.
On the physiological level, the study group scored (34.90 ± 3.20), (40.52 ± 4.03), and (50.52 ± 5.99) at 1, 3, and 6 months after the intervention, scores which were significantly higher than the scores of (31.54 ± 3.05), (32.91 ± 2.15) in the control group (P < 0.05) (Figure 2).
Figure 2.

Analysis of the changes in the quality of life-physiological scores before and after the intervention in the two groups. *P < 0.05 compared with the control group.
On the psychological level, the study group scored (54.39 ± 5.23), (57.39 ± 3.79), and (69.14 ± 3.20) at 1, 3, and 6 months after the intervention, scores which were significantly higher than the scores of (50.01 ± 2.04), (51.39 ± 1.51), and (51.39 ± 1.51) in the control group, respectively (P < 0.05) (Figure 3).
Figure 3.

Analysis of the changes in the quality of life-psychological factors scores before and after the intervention in the two groups. *P < 0.05 compared with the control group.
On the social level, the study group scored (30.41 ± 2.69), (36.16 ± 3.62), and (47.79 ± 3.92) at the three time points after the intervention, scores which were significantly higher than the scores of (28.41 ± 1.69), and (27.79 ± 1.78) and (29.54 ± 1.92) in the control group (P < 0.05) (Figure 4).
Figure 4.

Change analysis of the quality of life-social factor scores before and after the intervention in the two groups of patients. *P < 0.05 compared with the control group.
At the environmental level, the study group scored (67.54 ± 3.18) (1 month), (74.16 ± 5.44) (3 months), and (80.66 ± 6.23) (6 months), scores which were higher than the scores of (64.42 ± 1.90), (64.42 ± 1.90) and (66.42 ± 3.97) in the control group (P < 0.05) (Figure 5).
Figure 5.

Analysis of the changes in the quality of life-environmental factors scores before and after the intervention in the two groups. *P < 0.05 compared with control group.
Discussion
COPD has been increasing yearly as the population ages and as environmental pollution becomes more serious. The Global Initiative for Chronic Obstructive Pulmonary Disease (2019 edition) states that COPD has become the fourth most prevalent disease in the world in terms of morbidity and mortality [16]. During the course of COPD, symptoms such as chronic hypoxia and restricted motor function due to respiratory distress lead to hippocampal atrophy [17], decreased appetite and decreased physical fitness, and patients gradually lose their ability to work, which seriously affects their quality of life and increases the financial burden on their families.
This study evaluated the efficacy of CBR in the treatment of COPD patients. The results showed that, compared with the patients in the control group who underwent conventional outpatient rehabilitation treatment, the patients in the study group received CBR including rehabilitation education, breathing exercises, and psychological counseling. When comparing the data between the groups at the same time points, the differences were significant. The effects were more pronounced as the duration of the intervention progressed, and the patients’ self-efficacy improved significantly, and their quality of life improved significantly.
Studies have shown that only half of COPD patients can comply with medical advice to take their medication regularly, and only 10% of patients can correctly use inhaled drugs [18], and many patients do not know how to use drugs [19], leading to serious consequences such as recurrent episodes, a worsening of the condition, and an increased risk of re-hospitalization [20]. In recent years, many countries have begun to pay attention to improving the self-efficacy of COPD patients through education to stabilize the disease condition and improve the quality of life [21]. During the rehabilitation phase in patients with stable COPD, most time is spent at home. In this study, community-based rehabilitation including rehabilitation education, breathing exercises, and psychological counseling programs were utilized to provide adjunctive treatment to COPD patients who also underwent outpatient rehabilitative treatment. The study group underwent a combination of two nursing methods, which is more scientific. Especially when the patients are out of hospital, they are prone to lack condition monitoring and guidance. CBR promotes communication among patients, enables the patients to gain recognition as well as self-worth, which helps to reduce anxiety and depression and improve patients’ self-efficacy [22-24]. In this study, the comparison of the two groups at different time points after the intervention also confirmed this conclusion.
In summary, CBR can significantly improve self-efficacy and quality of life in patients with COPD, so it is worthy of clinical promotion. The innovation of this study is to abandon the concept of using conventional outpatient rehabilitative treatment or only physiotherapy for stable COPD patients, and to combine conventional outpatient rehabilitative treatment with CBR. The shortcomings of this study include the following: (1) The sample was small, resulting in a lack of generalizability of the results. (2) Short follow-up time. To address these shortcomings, the next step is to develop an intervention with a large sample size and a long follow-up period in order to provide a more detailed theoretical basis for the treatment of COPD.
Disclosure of conflict of interest
None.
References
- 1.Rothnie KJ, Müllerová H, Hurst JR, Smeeth L, Davis K, Thomas SL, Quint JK. Validation of the recording of acute exacerbations of COPD in UK primary care electronic healthcare records. PLoS One. 2016;11:e0151357. doi: 10.1371/journal.pone.0151357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128:2099–2107. doi: 10.1378/chest.128.4.2099. [DOI] [PubMed] [Google Scholar]
- 3.Ninane V, Corhay JL, Germonpré P, Janssens W, Joos GF, Liistro G, Vincken W, Gurdain S, Vanvlasselaer E, Lehouck A. Inhaled treatment of COPD: a Delphi consensus statement. Int J Chron Obstruct Pulmon Dis. 2017;12:793–801. doi: 10.2147/COPD.S125564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savage CC, Dixey PHA, Pennington C, Dodd JW. Visual rating assessment of cerebral atrophy and its relationship with cognitive function in chronic obstructive pulmonary disease. BMJ Open Respir Res. 2018;5:e000310. doi: 10.1136/bmjresp-2018-000310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Criner GJ, Frith P, Halpin DMG, Han M, López Varela MV, Martinez F, Montes de Oca M, Papi A, Pavord ID, Roche N, Sin DD, Stockley R, Vestbo J, Wedzicha JA, Vogelmeier C. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53:1900164. doi: 10.1183/13993003.00164-2019. [DOI] [PubMed] [Google Scholar]
- 6.Guilleminault L, Rolland Y, Didier A. Characteristics of non-pharmacological interventions in the elderly with COPD. Smoking cessation, pulmonary rehabilitation, nutritional management and patient education. Rev Mal Respir. 2018;35:626–641. doi: 10.1016/j.rmr.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Ambrosino N, Simonds A. The clinical management in extremely severe COPD. Respir Med. 2007;101:1613–1624. doi: 10.1016/j.rmed.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Siela D. Use of self-efficacy and dyspnea perceptions to predict functional performance in people with COPD. Rehabil Nurs. 2003;28:197–204. doi: 10.1002/j.2048-7940.2003.tb02060.x. [DOI] [PubMed] [Google Scholar]
- 9.Müller K, Niermann C, Einhorn N, Kotschy-Lang N, Wagner P. German translation of the COPD self-efficacy scale: development and validation of a short form. Psychother Psychosom Med Psychol. 2017;67:185–194. doi: 10.1055/s-0042-121803. [DOI] [PubMed] [Google Scholar]
- 10.Yu XQ, Wang MH, Li JS, Li SY, Xie Y, Bai YP, Zhang HL, Cao F, Hou CX, Ma LJ. Effect of comprehensive therapy based on Chinese medicine patterns on self-efficacy and effectiveness satisfaction in chronic obstructive pulmonary disease patients. Chin J Integr Med. 2019;25:736–742. doi: 10.1007/s11655-017-2417-9. [DOI] [PubMed] [Google Scholar]
- 11.Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 12.Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 13.Skevington SM. Measuring quality of life in Britain: introducing the WHOQOL-100. J Psychosom Res. 1999;47:449–459. doi: 10.1016/s0022-3999(99)00051-3. [DOI] [PubMed] [Google Scholar]
- 14.Liang WM, Chen JJ, Chang CH, Chen HW, Chen SL, Hang LW, Wang JD. An empirical comparison of the WHOQOL-BREF and the SGRQ among patients with COPD. Qual Life Res. 2008;17:793–800. doi: 10.1007/s11136-008-9326-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levi O, Bar-Haim Y, Kreiss Y, Fruchter E. Cognitive-behavioural therapy and psychodynamic psychotherapy in the treatment of combat-related post-traumatic stress disorder: a comparative effectiveness study. Clin Psychol Psychother. 2016;23:298–307. doi: 10.1002/cpp.1969. [DOI] [PubMed] [Google Scholar]
- 16.Leivseth L, Brumpton BM, Nilsen TI, Mai XM, Johnsen R, Langhammer A. GOLD classifications and mortality in chronic obstructive pulmonary disease: the HUNT study, Norway. Thorax. 2013;68:914–921. doi: 10.1136/thoraxjnl-2013-203270. [DOI] [PubMed] [Google Scholar]
- 17.Esser RW, Stoeckel MC, Kirsten A, Watz H, Taube K, Lehmann K, Petersen S, Magnussen H, von Leupoldt A. Structural brain changes in patients with COPD. Chest. 2016;149:426–434. doi: 10.1378/chest.15-0027. [DOI] [PubMed] [Google Scholar]
- 18.Restrepo RD, Alvarez MT, Wittnebel LD, Sorenson H, Wettstein R, Vines DL, Sikkema-Ortiz J, Gardner DD, Wilkins RL. Medication adherence issues in patients treated for COPD. Int J Chron Obstruct Pulmon Dis. 2008;3:371–384. doi: 10.2147/copd.s3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler R, Ståhl E, Vogelmeier C, Haughney J, Trudeau E, Löfdahl CG, Partridge MR. Patient understanding, detection, and experience of COPD exacerbations: an observational, interview-based study. Chest. 2006;130:133–142. doi: 10.1378/chest.130.1.133. [DOI] [PubMed] [Google Scholar]
- 20.Couillard S, Larivée P, Courteau J, Vanasse A. Eosinophils in COPD exacerbations are associated with increased readmissions. Chest. 2017;151:366–373. doi: 10.1016/j.chest.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Barr RG, Celli BR, Mannino DM, Petty T, Rennard SI, Sciurba FC, Stoller JK, Thomashow BM, Turino GM. Comorbidities, patient knowledge, and disease management in a national sample of patients with COPD. Am J Med. 2009;122:348–355. doi: 10.1016/j.amjmed.2008.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ninot G, Brun A, Queiras G, Segi A, Moullec G, Desplan J. Psychosocial support for pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Rev Mal Respir. 2003;20:549–557. [PubMed] [Google Scholar]
- 23.Klauser P, Baker ST, Cropley VL, Bousman C, Fornito A, Cocchi L, Fullerton JM, Rasser P, Schall U, Henskens F, Michie PT, Loughland C, Catts SV, Mowry B, Weickert TW, Shannon Weickert C, Carr V, Lenroot R, Pantelis C, Zalesky A. White matter disruptions in schizophrenia are spatially widespread and topologically converge on brain network hubs. Schizophr Bull. 2017;43:425–435. doi: 10.1093/schbul/sbw100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kunik ME, Veazey C, Cully JA, Souchek J, Graham DP, Hopko D, Carter R, Sharafkhaneh A, Goepfert EJ, Wray N, Stanley MA. COPD education and cognitive behavioral therapy group treatment for clinically significant symptoms of depression and anxiety in COPD patients: a randomized controlled trial. Psychol Med. 2008;38:385–396. doi: 10.1017/S0033291707001687. [DOI] [PubMed] [Google Scholar]


