Abstract
Purpose
The purpose of this study was to determine if the Single-Assessment Numeric Evaluation (SANE) score correlates with existing validated hip-specific patient-reported outcome measures (PROMs), including the Modified Harris Hip Score (mHHS), the International Hip Outcome Tool (IHOT-33), the Hip Outcome Score, Activities of Daily Living subscale (HOS-ADL), and the Hip Outcome Score, Sport-Specific subscale (HOS-SS), for patients preparing to undergo hip arthroscopy for treatment of femoroacetabular impingement syndrome (FAIS).
Methods
A single surgeon’s operative database was retrospectively reviewed to identify patients undergoing primary hip arthroscopy for treatment of FAIS from April 2018 to October 2019. Patient-specific factors including age, sex, body mass index (BMI), and duration of symptoms were collected. Preoperative SANE, mHHS, IHOT-33, HOS-ADL, and HOS-SS scores were analyzed. Statistical analysis using Pearson correlation was performed to identify the relationship between the SANE score and the mHHS, IHOT-33, HOS-ADL, and HOS-SS, preoperatively.
Results
154 patients were included in the study. The mean mHHS was 54.4 ± 11.7; mean IHOT-33 score was 32.7 ± 15.0; mean HOS-SS 42.9 ± 23.7; and mean HOS-ADL was 63.3 ± 1. The mean SANE score was 36.7 ± 19.9. The Simple Hip Score was directly correlated with the mHHS (P < .01), the IHOT-33 (P < .01); the HOS-ADL (P < .01), and the HOS-SS (P < .01). The mean patient age was 35.9 years; 109 (70.8%) were female and 45 (29.2%) were male. Average patient BMI was 26.9. At the time of patient completion of the questionnaire, the majority of patients (65%) had been having symptoms for >1 year.
Conclusion
The SANE score was strongly correlated with mHHS, IHOT-33, HOS-ADL, and HOS-SS in the preoperative setting for patients undergoing hip arthroscopy for treatment of FAIS. Given its simplicity, SANE may be a valuable tool for rapid assessment of joint function and pain in this patient population.
Level of Evidence
IV, therapeutic case series.
Hip arthroscopy has gained wide acceptance for treatment of various nonarthritic hip disorders.1, 2, 3 Patient-reported outcome measures (PROMs) have become an integral part of measuring treatment effectiveness and have been increasingly collected and reported over recent decades.4 Their utility is evaluated based on their ability to determine validity, reliability, and detect change.5 Several hip-specific scores exist and are frequently used, such as the Modified Harris Hip Score (mHHS), Hip Outcome Score, Activities of Daily Living subscale (HOS-ADL), Hip Outcome Score, Sport-Specific subscale (HOS-SS), the International Hip Outcome Tool (IHOT-33), and the International Hip Outcome Tool (IHOT-12).6, 7, 8, 9
The Harris Hip Score (HHS) was originally designed in 1969 as a 100-point questionnaire to assess pain, function, range of motion, and deformity.10 It was then truncated to the mHHS, rendering it more applicable to patients treated with hip arthroscopy, as it includes only the pain and function components.7 The mHHS has been widely used in hip arthroscopy.6,11,12 Since its development, many other PROMs have been created, and mHHS has remained a standard for comparison for these newer assessment tools.11,13, 14, 15, 16, 17, 18
The IHOT-33 and IHOT-12 have gained popularity among hip preservation surgeons hoping to use a consistent scoring system to aid in communicating and reporting outcomes. IHOT-33 was introduced by Mohtadi et al.7 in 2012 as an evaluation tool to measure health related quality of life in active patients with hip pathology. The questionnaire has 33 questions that cover 4 domains: symptoms and functional limitations, sports and recreational activities, job-related concerns, and social/emotional/lifestyle concerns. The authors showed that this self-administered questionnaire is reliable, valid, and highly responsive to clinical change.7 Although IHOT-33 provides greater insight into the components of a patient’s hip pathology, its length is a limitation, especially when administered alongside other surveys. Thus the IHOT-12 was developed to offer a shorter, validated, and reliable version; it is thought to be useful for routine clinical practice.8
The Hip Outcome Score (HOS) was first described in 2007 by Martin et al.9 It was developed for younger patients between the ages of 13 and 66 years who had a labral tear that either underwent hip arthroscopy or did not. All questions are related to function, not symptoms, and are broken down into 2 subscales, ADL (19 questions) and sports (9 questions).6 The score was shown to have adequate internal consistency and responsiveness6 by Ramisetty et al.11 in their evaluation of this PROM.
The PROMs described above have been validated and are commonly used either in isolation or together. However, they require more time and resources from the patient, physicians, and staff,19,20 A single numeric self-rating by the patient was initially introduced in 1999 by Williams et al.21 who evaluated cadets with shoulder instability using a single question and found that it correlated with other previously used multiquestion outcome measurement tools.14 Since that time, other studies have shown similar correlations and the clinical utility of single-question scores for the knee, shoulder, and foot and ankle.19,21, 22, 23, 24 However, there are limited studies in regard to a single numeric self-rating for the hip.
The purpose of this study was to determine if the Single-Assessment Numeric Evaluation (SANE) score correlates with existing validated hip-specific PROMs including the mHHS, IHOT-33, HOS-ADL, and HOS-SS, for patients preparing to undergo hip arthroscopy for treatment of femoroacetabular impingement syndrome (FAIS).
Methods
Institutional review board approval was obtained for this study. The operative database of a single surgeon (G.D.D.) was retrospectively reviewed to identify patients who underwent hip arthroscopy from April 1, 2018, to October 30, 2019. Only patients undergoing primary surgery for treatment of FAIS were included. Specific procedures performed in this patient cohort included labral repair, labral debridement, femoroplasty, acetabuloplasty, or a combination of these procedures. Patients were required to have completed a preoperative PROM questionnaire for inclusion. The preoperative PROMs included were mHHS, IHOT-33, HOS-ADL, HOS-SS, and SANE. SANE consists of 1 question asking the patient to rate their joint function and pain on a scale from 0 to 100. Patients with missing PROM data were excluded.
A total of 168 patients were identified who underwent primary hip arthroscopy for treatment of FAIS during the study period and had completed preoperative PROMs. Fourteen patients did not have a SANE recorded and thus were excluded. Patient-specific factors including age, sex, body mass index (BMI), and duration of symptoms were also collected for analysis. The duration of symptoms at the time of questionnaire completion was recorded using using 4 different time frames: <3 months of symptoms, 3 to <6 months of symptoms, 6 months to <1 year of symptoms, and ≥1 year of symptoms. Statistical analysis using Pearson correlation was performed to determine whether SANE correlated with existing hip-specific PROMs. Pearson correlation was significant at the P < .05 level (2-tailed).
Results
A total of 154 patients were included in the study. Of those patients, 109 (70.8%) were female and 45 (29.2%) were male. The mean patient age was 35.9 years (range 15 to 69), and average patient BMI was 26.9 (range 16.6 to 42). At the time of patient completion of the questionnaire, the majority of patients (65%) had been having symptoms for >1 year. Twenty patients (13%) had been having symptoms for 6 months to <1 year. Nineteen patients (12.7%) had symptoms from 3 to <6 months, and 13 (8.7%) had symptoms for <3 months. Four patients’ duration of symptoms were not recorded.
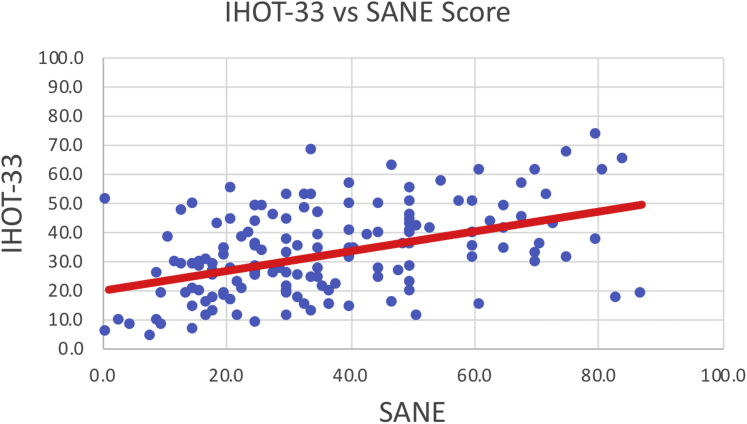
The PROMs collected were reported by patients preoperatively. The mean mHHS was 54.4 ± 11.7; mean IHOT-33, 32.7 ± 15.0; mean HOS-SS, 42.9 ± 23.7; mean HOS-ADL, 63.3 ± 18.9; and mean SANE, 36.7 ± 19.9. SANE was directly correlated with mHHS (P < .01), IHOT-33 (P < .01); HOS-ADL (P < .01), and HOS-SS (P < .01). A direct relationship was noted between each studied PROM and the SANE score. Table 1 shows Pearson correlation coefficients for each score. Figures 1 to 4 show the relationships between each PROM and the SANE score.
Fig 2.
International Hip Outcome Tool 33 (IHOT-33) versus Single-Assessment Numeric Evaluation (SANE).
Fig 3.
Hip Outcome Score, Sports Subscale (HOS-SS) versus Single-Assessment Numeric Evaluation (SANE).
Table 1.
Correlation of SANE with Existing Hip PROMs (n = 154)
| Measure | mHHS | IHOT-33 | HOS-SS | HOS-ADL |
|---|---|---|---|---|
| Pearson correlation coefficient | 0.351 | 0.445 | 0.386 | 0.43 |
| Significance (2-tailed P) | <.001 | <.001 | <.001 | <.001 |
HOS-SS, Hip Outcome Score, Sports subscale; HO-ADL, Hip Outcome Score, Activities of Daily Living subscale; IHOT, International Hip Outcome Tool; mHHS, modified Harris Hip Score; PROM, patient-reported outcome measure; SANE, Single Assessment Numeric Evaluation.
Fig 1.
Modified Harris Hip Score (mHHS) versus Single-Assessment Numeric Evaluation (SANE).
Fig 4.
Hip Outcome Score, Activities of Daily Living (HOS-ADL) versus Single-Assessment Numeric Evaluation (SANE).
Discussion
The results presented in this study support our hypothesis that preoperative SANE scores are directly correlated with commonly used hip-specific PROMs including mHHS, IHOT-33, HOS-ADL, and HOS-SS for patients undergoing hip arthroscopy.
As previously discussed, these pre-existing PROMs have been validated for use in patients undergoing hip preservation surgery. Rimesetty et al.11 compared multiple PROMs such as IHOT-33, mHHS, non-arthritic hip score (NAHS), hip disability and osteoarthritis outcome score (HOOS), Copenhagen hip and groin outcome score (HAGOS), and hip outcome score (HOS) to determine which was most useful in measuring treatment effectiveness after hip arthroscopy. The authors found that IHOT-33 scored the best of all the PROM tools based on Terwee criteria and recommended it for the future use in hip preservation surgery. Compared with the other PROMs, IHOT-33 has excellent test-retest reliability, content validity, construct validity, and responsiveness and no floor or ceiling effects.11 HOS-ADL and HOS-SS have also been validated as effective PROMs after hip arthroscopy by Rimesetty et al.11 and Martin et al.,13 showing that it has excellent test-retest reliability, construct validity, and interpretability and measurement error.7,9 However, it does lack content validity.7 mHHS demonstrates excellent construct validity but is poor in internal consistency and content validity and has ceiling effects.7 Furthermore, multiple studies have demonstrated patients’ clinically relevant improvement after hip arthroscopy based on HOS-ADL, HOS-SS, mHHS, and IHOT-12 and proposed minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient-acceptable symptomatic state (PASS) values.13, 14, 15,17,18
Although these other scoring systems are validated, are widely used, and provide a global understanding of a patient’s joint function, they include multiple items and require substantial time to complete. Although mHHS (compared with IHOT-33 and HOS) is an improvement in length and complexity, with only 8 questions and 2 subscales, time and resources are still required to collect and calculate a score, and there is possibility for incompleteness or error in comparison with a single, self-reported question such as SANE. A single question is easier for the patient, physicians, and office staff. The patients can simply report the number to the staff or physician, and this can easily be recorded in the patient’s record and easily interpreted and compared for subsequent visits.
Other joints have benefited from the adoption of single numeric scores, such as SANE, as an adjunct to more complex PROMs. Studies have found that SANE correlates with multiquestion PROMs for the knee, shoulder and the foot and ankle.19,21, 22, 23, 24 In the elbow, SANE has been compared to another short, 12-question PROM, the Oxford Elbow Score (OES). The OES has 3 domains (elbow function, pain, and social-psychological), and SANE was found to significantly correlate with all 3.20 For the shoulder, the subjective shoulder value (SSV) score is a percentage of shoulder function compared with the patient’s normal shoulder, which would be scored at 100%.21 This single numeric score has been compared to the Constant Score (CS), a 4-part, 100-point scale, and was found to be equally responsive and valid and easier to administer.25,26 The SSV has also been compared to more in-depth scores such as the Subjective Patient Outcome for Return to Sports (SPORTS), Western Ontario Shoulder Instability Index (WOSI), Rowe score, and Oxford Shoulder Instability Score (OSIS). The SSV best correlated with the SPORTS score in a study performed by Blonna et al.27 Despite its use and validity in various other joints, a single numeric score has not been validated or widely used for hip preservation procedures.
Lau et al.28 examined the use of SANE for activities of daily living and sport participation after hip arthroscopy and compared it to HOS-ADL, HOS-SS, and mHHS before and after surgery. A separate SANE score was used for activities of daily living and sport participation. That study found SANE to be an effective method of assessing outcomes after hip arthroscopy pre- and postoperatively based on Pearson correlation coefficient. Preoperatively, SANE showed a moderate correlation with the mHHS, HOS-ADL, and HOS-SS. Postoperatively, SANE showed moderate correlation with mHHS and strong correlation with HOS-ADL and HOS-SS.28 In our study, SANE was not subdivided into components for activities of daily living and sport participation, yet the single score correlated well with both HOS-SS and HOS-ADL.
Although our study did not use validity criteria such as Terwee, our Pearson correlation coefficient did show a positive correlation to previously validated PROMs. In addition, our results, although only preoperative, are similar to those found by Lau et al.28 As more of our patients reach postoperative milestones, notably 2-year postoperative status, evaluation of SANE and comparison to postoperative existing PROMs will be important, in addition to determination of MCID and PASS values for SANE.
Limitations
There are limitations to this study. Although the data were prospectively collected, they were reviewed retrospectively. The included patients also completed multiple other PROMs in the preoperative period. This may lead to response bias in which the patients included in the study had a better understanding of their symptoms after completing the more comprehensive PROMs. Survey fatigue may also have influenced patient responses on any of the PROMs, including SANE. Furthermore, our study only included evaluation of preoperative scores, which limited the extent to which we could fully assess the validity of SANE and whether the correlation remains postoperatively, and if so, for how long.
Conclusion
The SANE score was strongly correlated with mHHS, IHOT-33, HOS-ADL, and HOS-SS in the preoperative setting for patients undergoing hip arthroscopy for treatment of FAIS. Given its simplicity, SANE may be a valuable tool for rapid assessment of joint function and pain in this patient population. Future evaluation of SANE in patients undergoing various hip preservation procedures will be beneficial.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: G.D.D. reports personal fees and other, Smith & Nephew; personal fees, Conmed Linvatec, Zimmer Biomet. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Bozic K.J., Chan V., Valone F.H., 3rd, Feeley B.T., Vail T.P. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28:140–143. doi: 10.1016/j.arth.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 2.Degen R.M., Bernard J.A., Pan T.J., et al. Hip arthroscopy utilization and associated complications: A population-based analysis. J Hip Preserv Surg. 2017;4:240–249. doi: 10.1093/jhps/hnx021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly B.T., Williams R.J., 3rd, Philippon M.J. Hip arthroscopy: Current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020–1037. doi: 10.1177/03635465030310060701. [DOI] [PubMed] [Google Scholar]
- 4.Gagnier J.J. Patient reported outcomes in orthopaedics. J Orthop Res. 2017;35:2098–2108. doi: 10.1002/jor.23604. [DOI] [PubMed] [Google Scholar]
- 5.Deshpande P.R., Rajan S., Sudeepthi B.L., Abdul Nazir C.P. Patient-reported outcomes: A new era in clinical research. Perspect Clin Res. 2011;2:137–144. doi: 10.4103/2229-3485.86879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Byrd J.W., Jones K.S. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 7.Mohtadi N.G., Griffin D.R., Pedersen M.E., et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33) Arthroscopy. 2012;28:595–605. doi: 10.1016/j.arthro.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Griffin D.R., Parsons N., Mohtadi N.G., Safran M.R. Multicenter Arthroscopy of the Hip Outcomes Research Network. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy. 2012;28:611–616. doi: 10.1016/j.arthro.2012.02.027. [DOI] [PubMed] [Google Scholar]
- 9.Martin R.L., Philippon M.J. Evidence of validity for the Hip Outcome Score in hip arthroscopy. Arthroscopy. 2007;23:822–826. doi: 10.1016/j.arthro.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 11.Ramisetty N., Kwon Y., Mohtadi N. Patient-reported outcome measures for hip preservation surgery—a systematic review of the literature. J Hip Preserv Surg. 2015;2:15–27. doi: 10.1093/jhps/hnv002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byrd J.W., Jones K.S. Hip arthroscopy for labral pathology: Prospective analysis with 10-year follow-up. Arthroscopy. 2009;25:365–368. doi: 10.1016/j.arthro.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 13.Martin R.L., Kivlan B.R., Christoforetti J.J., et al. Defining variations in outcomes of hip arthroscopy for femoroacetabular impingement using the 12-Item International Hip Outcome Tool (iHOT-12) Am J Sports Med. 2020;48:1175–1180. doi: 10.1177/0363546520906408. [DOI] [PubMed] [Google Scholar]
- 14.Nwachukwu B.U., Beck E.C., Kunze K.N., Chahla J., Rasio J., Nho S.J. Defining the clinically meaningful outcomes for arthroscopic treatment of femoroacetabular impingement syndrome at minimum 5-year follow-up. Am J Sports Med. 2020;48:901–907. doi: 10.1177/0363546520902736. [DOI] [PubMed] [Google Scholar]
- 15.Robinson P.G., Maempel J.F., Rankin C.S., Gaston P., Hamilton D.F. Evaluation of the patient acceptable symptom state following hip arthroscopy using the 12 item international hip outcome tool. BMC Musculoskelet Disord. 2020;21:5. doi: 10.1186/s12891-019-3026-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ohlin A., Ahlden M., Lindman I., et al. Good 5-year outcomes after arthroscopic treatment for femoroacetabular impingement syndrome. Knee Surg Sports Traumatol Arthrosc. 2020;28:1311–1316. doi: 10.1007/s00167-019-05429-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nwachukwu B.U., Change B., Beck E.C., et al. How should we define clinically significant outcome improvement on the iHOT-12? HSS J. 2019;15:103–108. doi: 10.1007/s11420-018-9646-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kivlan B.R., Martin R.L., Christoforetti J.J., et al. The patient acceptable symptomatic state of the 12-Item International Hip Outcome Tool at 1-year follow-up of hip-preservation surgery. Arthroscopy. 2019;35:1457–1462. doi: 10.1016/j.arthro.2018.11.072. [DOI] [PubMed] [Google Scholar]
- 19.Williams G.N., Taylor D.C., Gangel T.J., Uhorchak J.M., Arciero R.A. Comparison of the single assessment numeric evaluation method and the Lysholm score. Clin Orthop Relat Res. 2000:184–192. doi: 10.1097/00003086-200004000-00022. [DOI] [PubMed] [Google Scholar]
- 20.Razaeian S., Wiese B., Zhang D., Krettek C., Meller R., Hawi N. Correlation between Oxford Elbow Score and Single Assessment Numeric Evaluation: Is one simple question enough? J Shoulder Elbow Surg. 2020;29:1223–1229. doi: 10.1016/j.jse.2020.01.067. [DOI] [PubMed] [Google Scholar]
- 21.Williams G.N., Gangel T.J., Arciero R.A., Uhorchak J.M., Taylor D.C. Comparison of the single assessment numeric evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27:214–221. doi: 10.1177/03635465990270021701. [DOI] [PubMed] [Google Scholar]
- 22.Shelbourne K.D., Barnes A.F., Gray T. Correlation of a single assessment numeric evaluation (SANE) rating with modified Cincinnati knee rating system and IKDC subjective total scores for patients after ACL reconstruction or knee arthroscopy. Am J Sports Med. 2012;40:2487–2491. doi: 10.1177/0363546512458576. [DOI] [PubMed] [Google Scholar]
- 23.Thigpen C.A., Shanley E., Momaya A.M., et al. Validity and responsiveness of the single alpha-numeric evaluation for shoulder patients. Am J Sports Med. 2018;46:3480–3485. doi: 10.1177/0363546518807924. [DOI] [PubMed] [Google Scholar]
- 24.Hunt S.A., Sherman O. Arthroscopic treatment of osteochondral lesions of the talus with correlation of outcome scoring systems. Arthroscopy. 2003;19:360–367. doi: 10.1053/jars.2003.50047. [DOI] [PubMed] [Google Scholar]
- 25.Constant C.R., Murley A.H. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987:160–164. [PubMed] [Google Scholar]
- 26.Gilbart M.K., Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg. 2007;16:717–721. doi: 10.1016/j.jse.2007.02.123. [DOI] [PubMed] [Google Scholar]
- 27.Blonna D., Bellato E., Caranzano F., et al. Validity and reliability of the SPORTS score for shoulder instability. Joints. 2014;2:59–65. doi: 10.11138/jts/2014.2.2.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lau B.C., Scribani M., Lassiter T., Wittstein J. Correlation of Single Assessment Numerical Evaluation Score for Sport and Activities of Daily Living to Modified Harris Hip Score and Hip Outcome Score in patients undergoing arthroscopic hip surgery. Am J Sports Med. 2019;47:2646–2650. doi: 10.1177/0363546519863411. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.