Abstract
COVID-19 has significantly affected the use of health care worldwide and, consequently, admissions to hospital emergency services. The aim of this study is to describe the change of the activity of a Paediatric Emergency Service (PES) of a tertiary hospital during the pandemic. A retrospective cohort study with analysis of visits to the PES from March 30 to June 30, 2020, and comparison with homologous periods in the previous 3 years (2017–2019).A total of 53,883 episodes were analysed, with a median age of 5.8 years, and 53% were boys. In 2020, there was a 60% reduction in the number of admissions (p < 0.001). There was a significant increase in referral by the public medical advice phone line of the National Health Service (NHS) (18.5% vs 5.4%) and Emergency Medical Services (EMS) (5.1% vs 4.2%). Urgent patients decreased (31.2% vs 38.3%), and non-urgent patients increased (7.5% vs 1.7%). There was a significant reduction in school (0.4% vs 7.1%) and sports accidents (0.1% vs 1.2%) and an increase in other accidents (falls, wounds, burns, and dog bites) (12.2% vs 6.3%). Hospitalisation rate was higher (5.7% vs 3.1%, p < 0.001). The infection rate for SARS-CoV-2 was 1.1%, all with mild illness or asymptomatic.
Conclusion: The pandemic brought a marked reduction in emergency admissions and a decrease in urgent situations but an increase in accidents, such as falls, wounds, burns, and dog bites. Despite the low infection rate for SARS-CoV-2, there were increased referrals by the phone line of NHS and EMS and a higher admission in the ward.
|
What is Known: • The number of admissions to emergency services significantly decreased during the COVID-19 pandemic, particularly in the paediatric population, whom has a milder disease than adults. • Diseases that justify urgent/emergent hospital admission continue to exist and the eventual delay in seeking health care might lead to a worse prognosis. | |
|
What is New: • Despite the low rate of SARS-CoV-2 infection in children, there was an increase in referrals by the phone line of the National Health Service and Emergency Medical Services. • The global admission rate to the ward increased but there were no admissions to intensive care or deaths. |
Keywords: COVID-19, Coronavirus, SARS-CoV-2, Paediatric Emergency Medicine, Child
Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first identified on January 12, 2020, after an outbreak of pneumonia in December 2019 in China [1]. The first case in Portugal was reported on March 2, 2020. On March 11, 2020, the World Health Organization (WHO) classified COVID-19 as a pandemic [2], and 8 days later, a state of national emergency was declared in Portugal, which forced compulsory lockdown for 7 weeks. After that, although part of the population remained at home, some establishments started to open and secondary schools and some kindergartens have resumed activity.
Since the beginning of the pandemic, several studies have reported a decrease in admissions to emergency service (ES), particularly in the paediatric population [3–7].
In Portugal, it was found that, since the first month of the pandemic, there has been a significant change in the pattern of health care use in the National Health Service (NHS), particularly in the use of the ES [5]. Compared to similar periods from 2017 to 2019, there was a 45% reduction in emergency episodes in Portugal [5], similar to the world overview [6, 8–11].
Over the months, there were fewer reported cases of paediatric COVID-19 than in adults, representing only about 1–2% of the total diagnoses, with the most of mild severity of disease [10, 12–14]. Unlike other viral respiratory infections, children seem to play a less important role in the transmission of the virus [12, 15], although it is not possible yet to confirm all transmission pathways.
On one hand, lockdown and social isolation can explain part of the reduction in the use of the ES, but on the other, it is known that diseases/medical conditions that justify urgent/emergent hospital admission continue to exist. The eventual delay in seeking health care in these circumstances could lead to the disease progressing to more severe stages and to a worse prognosis [5, 10].
Thus, the objective of this study is to analyse the use of a Paediatric Emergency Service (PES) during the pandemic, comparing it with the same period in the previous years, in order to understand its characteristics and the changes that occurred in the care and observation in the PES and thus optimise strategies that can be applied in future situations, whether in a pandemic context or not [5].
Methods
Study design and setting
The present work is a single-centre, retrospective cohort study, based on clinical records of children and adolescents, admitted to the ES of the Paediatric Hospital of Centro Hospitalar e Universitário de Coimbra (PH-CHUC), from March 30 to June 30, 2020, and comparison with homologous periods in the previous 3 years (2017–2019).
The PH-CHUC is one of the five reference hospitals for paediatric COVID-19 in Portugal, for consultancy and hospitalisation.
PES of the PH-CHUC is a free access paediatric polyvalent ES, where paediatricians, paediatric surgeons, and paediatric orthopaedic surgeons work, but with no paediatric emergency physicians because this medical specialty is not yet officially recognised in Portugal. Trauma falls under the expertise of paediatric surgeons and paediatric orthopaedic surgeons.
During the study period, there was a structural reorganisation of the hospital. The ES was divided into suspected and non-suspected COVID-19 areas according to the symptoms presented at admission. In line with local and national recommendations, patients with fever, respiratory symptoms (breathing difficulty, coughing), diarrhoea or vomiting, rhinorrhoea, odynophagia, loss of taste or smell, headache, myalgia, and contact with a case, were observed in the suspected COVID-19 area. The short-stay unit was reorganised as a COVID-19 ward. It was also mandatory to search for SARS-CoV-2 prior to surgery, diagnostic procedures that include an airway approach or need for sedation, such as CT scan, MRI, and endoscopy.
Participants
All admissions to the PES (under the age of 18) were included. Data were obtained through the Information Technologies and Systems Service, in an anonymised form, in accordance with the General Data Protection Regulation and with the approval of the Ethics Committee of CHUC.
Variables
Demographic and clinical characteristics were analysed. Age was categorised into age groups: newborn: 0–1 month; infant: 1–12 months; preschool: 1–5 years; school: 5–10 years; teenager: 10–18 years. The triage algorithm used was the Canadian Paediatric Triage and Acuity Scale (CPTAS), consisting of five levels: level 1, emergency; level 2, very urgent; level 3, urgent; level 4, not very urgent; level 5, not urgent. Definitive diagnoses were presented according to the International Classification of Diseases (ICD-9).
Regarding the reason for admission, patients were divided into three groups: medical causes, trauma, and psychiatric causes. Medical causes include most of the patients and are most often managed by paediatricians (example: respiratory, gastrointestinal, urinary, and other infectious diseases). Trauma includes school, sports and domestic accidents, and other accidents such as falls, wounds, burns, and dog bites. Psychiatric causes include self-injuries, aggression, and poisoning.
Study size
This is a convenience sample, so the sample size was defined by the total number of admissions in the study period.
Statistical methods
Statistical analysis was performed using the IBM Statistical Package for the Social Sciences (SPSS®), version 26. The mean, standard deviation, median, and interquartile range (IQR) were calculated for continuous variables, and the relative and absolute frequency for nominal variables. The normality of the distributions was analysed using the Kolmogorov–Smirnov test. The chi-square, Fisher, Mann–Whitney, and Kruskal–Wallis tests were used to determine the associations and significant differences between variables, respectively. The significance level (α) was set at 0.05.
Results
There were 53,883 emergency episodes between March 30 and June 30 of the years 2017 (30.1%, n = 16,216), 2018 (29.5%, n = 15,881), 2019 (29.3%, n = 15,769), and 2020 (11.1%, n = 6017). Tables 1 and 2 show the comparison of the demographic profile and the clinical characteristics associated with emergency episodes in the last 4 years. The 2020 values were compared with the average values from 2017 to 2019.
Table 1.
Comparison of the demographic and clinical characteristics associated with emergency episodes in the last 4 years
| Characteristics | 2017 (n = 16,216) |
2018 (n = 15,881) |
2019 (n = 15,769) |
2020 (n = 6017) |
p |
|---|---|---|---|---|---|
| Emergency episodes, % | 30.1 | 29.5 | 29.3 | 11.2* | <0.001 |
| Median age, years (IQR) | 6.0 (2.1–11.5) | 5.8 (2.0–11.7) | 5.7 (2.0–11.5) | 5.7 (2.0–11.9) | |
| Age groups, % (n) | <0.001 | ||||
| Newborn | 0.8 (130) | 0.9 (150) | 1.0 (159) | 2.0 (119)* | |
| Infant | 10.8 (1752) | 10.9 (1733) | 12.0 (1888) | 11.1 (668) | |
| Preschool | 32.7 (5299) | 34.3 (5446) | 33.9 (5346) | 32.9 (1980) | |
| School | 23.9 (3882) | 22.1 (3503) | 21.9 (3459) | 21.4 (1290) | |
| Teenager | 31.8 (5153) | 31.8 (5049) | 31.2 (4917) | 32.6 (1960) | |
| Gender, % (n) | 0.040 | ||||
| Male | 53.1 (8614) | 53.6 (8513) | 52.1 (8214)* | 53.5 (3218) | |
| Female | 46.9 (7602) | 46.4 (7368) | 47.9 (7555)* | 46.5 (2799) | |
| Admission source, % (n) | <0.001 | ||||
| Parents’ initiative | 79.7 (12,927) | 78.4 (12,448) | 77.8 (12,266) | 65.5 (3942)* | |
| Phone line of NHS | 4.2 (678) | 5.4 (863) | 6.5 (1029) | 18.5 (1115)* | |
| Primary health care | 7.9 (1279) | 7.6 (1203) | 7.2 (1128) | 6.4 (384)* | |
| EMS | 4.0 (648) | 4.2 (663) | 4.3 (676) | 5.1 (308)* | |
| Other NHS hospital | 3.3 (540) | 3.3 (525) | 3.3 (525) | 3.7 (222) | |
| Private hospital | 0.6 (100) | 0.7 (118) | 0.6 (98) | 0.4 (25)* | |
| Medical appointment | 0.3 (44) | 0.4 (59) | 0.3 (42) | 0.3 (17) | |
| Other | 0.0 (0) | 0.0 (2) | 0.0 (5) | 0.1 (4) | |
| Canadian triage, median (IQR) | 4 (3–4) | • 4 (3–4) | 4 (3–4) | 4 (3–4) | <0.01 |
| Canadian triage, % (n) | <0.001 | ||||
| Level 1 | 0.1 (16) | 0.1 (13) | 0.1 (23) | 0.1 (8) | |
| Level 2 | 3.6 (582) | 3.8 (598) | 4.2 (659) | 3.6 (218) | |
| Level 3 | 37.7 (6112) | 39.1 (6203) | 38.2 (6031) | 31.2 (1879)* | |
| Level 4 | 56.1 (9095) | 54.9 (8715) | 55.5 (8758) | 55.6 (3346) | |
| Level 5 | 1.9 (300) | 1.7 (276) | 1.4 (222) | 7.5 (450)*a | |
| Without triageb | 0.7 (111) | 0.5 (76) | 0.5 (76) | 1.9 (116)* |
IQR, interquartile range; NHS, National Health Service; EMS, Emergency Medical Services
*Statistically significant value
aThis value is over inflated by the internal decision to assign this priority to elective screening for SARS-CoV-2 performed in ES
bInformation technology services failure
Table 2.
Characteristics associated with emergency episodes in the last 4 years (continuation)
| Characteristics | 2017 (n = 16,216) |
2018 (n = 15,881) |
2019 (n = 15,769) |
2020 (n = 6017) |
p |
|---|---|---|---|---|---|
| Waiting times, minutes ± SD | <0.001 | ||||
| Time to triage | 16.0 ± 14.2 | 12.9 ± 8.4 | 13.1 ± 8.9 | 12.7 ± 20.1 | |
| Time to medical observation | 46.2 ± 47.7 | 44.1 ± 44.6 | 42.4 ± 48.8 | 21.6 ± 30.4 | |
| Time to discharge | 85.3 ± 145.7 | 85.8 ± 135.4 | 88.0 ± 144.5 | 98.7 ± 143.2 | |
| Cause of admission, % (n) | <0.001 | ||||
| Medical causes | 81.8 (13,272) | 82.0 (13,024) | 82.5 (13,015) | 82.1 (4938) | |
| Trauma | |||||
| Domestic accidents | 0.8 (135) | 2.6 (420) | 3.1 (493) | 4.5 (268) | |
| School accidents | 6.9 (1113) | 7.8 (1242) | 6.6 (1042) | 0.4 (24)* | |
| Road accidents | 0.4 (72) | 0.4 (62) | 0.4 (70) | 0.3 (16) | |
| Sports accidents | 1.1 (182) | 1.4 (215) | 1.2 (195) | 0.1 (6)* | |
| Others | 7.8 (1262) | 5.3 (849) | 5.7 (888) | 12.2 (732)* | |
| Psychiatric causes | 1.1 (180) | 0.4 (69) | 0.4 (66) | 1.5 (33) | |
| Specialty, % (n) | <0.001 | ||||
| General paediatricians | 71.6 (11,589) | 72.0 (11,433) | 72.6 (11,445) | 72.1 (4318) | |
| Paediatric surgery | 5.0 (815) | 5.5 (873) | 5.4 (853) | 10.0 (600)* | |
| Orthopaedics | 12.8 (2068) | 13.3 (2106) | 13.4 (2119) | 9.4 (563)* | |
| Otorhinolaryngology | 3.1 (499) | 2.9 (456) | 2.7 (429) | 2.6 (154) | |
| Ophthalmology | 2.4 (387) | 2.2 (349) | 2.0 (309) | 1.7 (100)* | |
| Neurosurgery | 1.8 (291) | 1.5 (238) | 1.4 (225) | 1.5 (92) | |
| Stomatology | 1.2 (194) | 1.1 (180) | 0.9 (144) | 1.3 (78) | |
| Child psychiatry | 1.4 (226) | 1.2 (192) | 1.1 (172) | 0.7 (43)* | |
| Neurology | 0.2 (40) | 0.1 (21) | 0.3 (40) | 0.3 (18) | |
| Paediatric cardiology | 0.2 (25) | 0.0 (7) | 0.1 (15) | 0.1 (5) | |
| Others | 0.3 (46) | 0.2 (24) | 0.1 (17) | 0.3 (17) | |
| Paediatric diagnoses, % (n) | |||||
| Fever | 6.6 (690) | 5.5 (588) | 4.8 (511) | 9.2 (376) | |
| Acute gastroenteritis | 5.8 (613) | 6.8 (733) | 9.2 (992) | 6.0 (246) | |
| Acute tonsillitis | 6.0 (632) | 5.5 (591) | 6.3 (671) | 5.3 (218) | |
| Acute nasopharyngitis | 10.2 (1074) | 10.9 (1174) | 10.5 (1128) | 4.5 (185) | |
| Abdominal pain | 3.8 (397) | 3.6 (381) | 3.5 (378) | 3.3 (134) | |
| Virus rashes | 4.5 (477) | 3.4 (360) | 2.5 (267) | 2.1 (84) | |
| Vomiting | 2.6 (269) | 2.3 (245) | 2.4 (254) | 1.8 (72) | |
| Cough | 1.4 (146) | 1.6 (167) | 1.2 (134) | 1.7 (70) | |
| Others | 59.0 (6193) | 60.3 (6486) | 59.5 (6383) | 59.4 (2429) | |
| Destination after observation, % (n) | <0.001 | ||||
| Discharge to home | 90.1 (14,614) | 91.5 (14,528) | 91.0 (14,350) | 89.3 (5373)* | |
| Hospitalisation | 3.2 (523) | 3.0 (481) | 3.2 (499) | 4.9 (293)* | |
| Elective hospitalisation | - | - | - | 0.8 (50) | |
| Discharge to medical appointment | 5.5 (887) | 4.7 (743) | 5.0 (781) | 4.7 (283) | |
| Hospital abandonment | 1.1 (175) | 0.7 (110) | 0.8 (121) | 0.2 (10)* | |
| Transfer to another hospital | 0.1 (17) | 0.1 (19) | 0.1 (17) | 0.1 (8) | |
| Deaths | 0.0 (0) | 0.0 (0) | 0.0 (1) | 0.0 (0) |
SD, standard deviation
*Statistically significant value
The median age of the total sample was 5.8 years (IQR: 2.0–11.6), with 53.1% being male.
During the pandemic period, there was 62.3% reduction in emergency episodes (p < 0.001) compared to the previous years. Despite slightly lower absolute values, the percentage of newborns admitted to the ES was significantly higher than in the previous years (2.0% vs 0.9%, p < 0.001). There was a significant increase in the cases referred by public medical advice phone line of the NHS (18.5% vs 5.4%, p < 0.001) and by the Emergency Medical Services (EMS) (5.1% vs 4.2%, p < 0.001), and a reduction in parents’ initiative to take their child to the ES (65.5% vs 78.6%, p < 0.001), referral by primary health care services (PHCS) (6.4% vs 7.6%, p < 0.001) and by private clinics (0.4% vs 0.6%, p < 0.001).
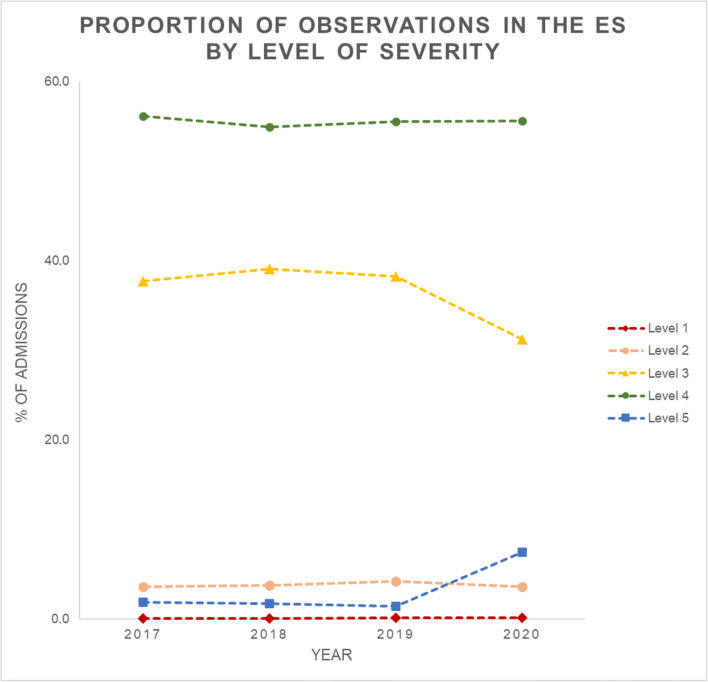
Comparing with the previous years, in 2020 there was an increase of patients screened at level 5 (not urgent) (7.5% vs 1.7%, p < 0.001) and a decrease of patients screened at level 3 (urgent) (31.1% vs 38.3%, p < 0.001) (Fig. 1).
Fig. 1.
Proportion of observations in the ES by level of severity
Patients who came to the ES to be electively tested for SARS-CoV-2 infection were included in level 5 of priority.
The pandemic also changed waiting times. Time to triage (12.7 ± 20.1 min) and time to medical observation (21.6 ± 30.4 min) were significantly shorter in 2020 (p < 0.001); the opposite occurred in the time to discharge (98.7 ± 143.1), which was higher (p < 0.001).
Regarding trauma admissions during the pandemic period, school accidents (0.4% vs 7.1%) and sports accidents (0.1% vs 1.2%) decreased significantly (p < 0.001) and other accidents, such as wounds, falls, burns, and dog bites (12,2% vs 6,3%), increased (p < 0.001).
General paediatricians observed more than 70% of all patients admitted to the ES in the 4 years. The most frequent ICD-9 diagnoses in 2020, in a decreasing order, were fever, acute gastroenteritis, acute tonsillitis, acute nasopharyngitis, abdominal pain, virus rashes, vomiting, and cough. There was a marked increase in the diagnosis of fever without other symptoms associated (9.2% vs 5.6%), and a decrease in previously more frequent diagnoses, such as acute nasopharyngitis (4.5% vs 10.5%).
In relation to the other specialties, there was an increase in the percentage of patients under the care of paediatric surgery (10.0% vs 5.3%) and a reduction in patients under the responsibility of orthopaedics (9.4% vs 13.2%), ophthalmology (1.7% vs 2.2%), and child psychiatry (0.7% vs 1.2%) (p < 0.001).
There was an increase in the global hospitalisation rate (5.7% vs 3.1%, p < 0.001). These differences were not due to COVID patients that were very rarely admitted.
During the pandemic period, there were no patients admitted to the intensive care unit or deaths recorded.
During the study period in 2020, 1610 (26.8%) patients were tested for SARS-CoV-2 by polymerase chain reaction (PCR), using throat and/or nasopharyngeal swabs, of which 17 (1.1%) tested positive. Of these, six were asymptomatic, four of whom were tested in a pre-procedure elective context and two due to contact with cases. Symptomatic cases presented with fever and cough (4), vomiting (3), diarrhoea (2), abdominal pain (2), and headache (2). Asthenia, odynophagia, myalgia, and dyspnoea were also reported. Three cases were hospitalised but received only symptomatic treatment. In patients with COVID-19, a higher proportion of patients was given a triage level 3 (35.3% vs 29.5%) and a lower proportion of patients a triage level 4 (17.6% vs 40.6%). In the other parameters, there were no differences (see Table 3).
Table 3.
Comparison of demographic and clinical characteristics between patients with and without COVID-19
| Characteristics | SARS-CoV-2 | |
|---|---|---|
| Detected (n = 17) |
Non-detected (n = 1593) |
|
| Median age, years (IQR) | 7.0 (1.1–12.4) | 4.6 (1.6–11.4) |
| Age groups, % (n) | ||
| Newborn | 0.0 (0) | 1.0 (16) |
| Infant | 23.5 (4) | 14.0 (223) |
| Preschool | 17.6 (3) | 37.0 (589) |
| School | 17.6 (3) | 17.4 (278) |
| Teenager | 41.2 (7) | 30.6 (487) |
| Gender, % (n) | ||
| Male | 47.1 (8) | 56.2 (896) |
| Female | 52.9 (9) | 43.8 (697) |
| Admission source, % (n) | ||
| Parents’ initiative | 64.7 (11) | 63.0 (1003) |
| Phone line of NHS | 17.6 (3) | 22.7 (361) |
| Primary health care | 5.9 (1) | 5.3 (84) |
| EMS | 5.9 (1) | 4.7 (76) |
| Other NHS hospital | 5.9 (1) | 3.4 (54) |
| Medical appointment | 0.0 (0) | 0.6 (10) |
| Private hospital | 0.0 (0) | 0.2 (3) |
| Others | 0.0 (0) | 0.1 (2) |
| Canadian triage, median (IQR) | 4 (3–5) | 4 (3–4) |
| Canadian triage, % (n) | ||
| Level 1 | 0.0 (0) | 0.4 (7) |
| Level 2 | 5.9 (1) | 5.1 (82) |
| Level 3 | 35.3 (6)* | 29.5 (470) |
| Level 4 | 17.6 (3)* | 40.6 (646) |
| Level 5 | 17.6 (3) | 19.6 (312) |
| Without triage | 23.5 (4)* | 4.8 (76) |
| Destination after observation, % (n) | ||
| Discharge to home | 82.4 (14) | 83.7 (1333) |
| Hospitalisation | 17.6 (3) | 15.4 (245) |
| Discharge to medical appointment | 0.0 (0) | 0.9 (14) |
| Transfer to another hospital | 0.0 (0) | 0.0 (1) |
IQR, interquartile range; NHS, National Health Service; EMS, Emergency Medical Services
*Statistically significant value
During the study period, there were no cases of COVID-19 nosocomial transmission, among children or health care professionals. Of the few cases of SARS-CoV-2 infection that occurred in health care professionals, the transmission chain has been identified and did not happen in hospital.
Discussion
The COVID-19 pandemic had significant impact on the activity and dynamics of the ES of the PH-CHUC, with a decrease of more than 60% in the number of episodes when compared to the previous 3 years.
The findings from this study are consistent with what was observed at the European and world levels [3, 4, 6, 8–10, 16]. The report by the Centers for Disease Control and Prevention (CDC), on June 3, 2020, announced a 40% decrease in emergency episodes between March 29 and April 25, compared to a similar period in the previous year, with paediatric age (<14 years) being one of the most affected subgroups [6]. In Europe, three other studies reported a reduction between 50 and 76% in hospital admissions [8–10].
The reasons for this reduction should be the result of a combination of factors in the face of the pandemic [3, 9]. Fear of SARS-CoV-2 infection [4, 8, 9, 16], a reduction in the incidence of seasonal infections [4, 8, 11] and traumatic injuries [4], such as sports and school accidents due to the lockdown and closure of schools and day-care centres, may justify part of the sharp decrease. The perception of the scarcity of available human resources [4], the moral conscience not to overload the services focused on responding to the pandemic, and the restriction in the public transport network for travelling to the hospital may also justify this change [5, 11]. Another argument may be the low level of clinical manifestation of COVID-19 found at paediatric age [3, 4, 10, 16–18].
The sample of this study is similar to other international studies that tried to understand the impact of the pandemic in PES, with respect to age and gender [10, 13, 16, 19].
Despite having a contingency plan for pandemics, several changes were made over time in order to face a rapidly evolving crisis. Furthermore, as in another study, paediatricians’ shift work was rearranged, with adjustments on shift schemes to prevent cross infection among staff [7].
The significant increase in the percentage of newborns observed in the PES, despite a small reduction in absolute numbers, may be due to pandemic-related reduction in activity and accessibility to primary health care and private hospitals. In addition, the foreseen shorter time of contact between mothers and the medical and nursing teams during the stay and even earlier discharges may have favoured this fact. These results are corroborated by the study by Cheek et al. [20] that also identified an increase in newborns’ percentage in tertiary hospitals in 2020, comparing to 2019, explained by the reduction in visits to local municipalities.
Despite the initial fear of overcrowding of the ES [5], the recommendations issued by the Ministry of Health [21] and the rules of the General-Directorate of Health (GDH) [22], suggesting initial contact via the NHS phone line, particularly in the presence of symptoms, may have discouraged direct access to the ES [22], similar to what happened in other countries. This fact justified the increase in patient referrals by phone line of the NHS and EMS and the decrease in admissions of children brought by parents’ initiative, which were in line with the recommendations of the GDH [22]. There was also a decrease in patient referrals from private clinics that were closed in this period. Despite the GDH’s recommendation to maintain child and youth health surveillance consultations, as well as compliance with the National Immunisation Programme and newborn screening in the PHCS, the decrease of these referrals might suggest some failure at this level.
We observed significant changes in waiting times. There was a greater speed up to triage because of the lower influx of patients, and a greater speed in first medical observation, justified by a different organisational strategy, in which the first medical contact with the patient was made by telephone, to obtain the clinical history. The time until discharge increased, reflecting a longer stay in the PES, which can be related to the smaller number of consultation rooms, the delay caused by the use of personal protective equipment, and cleaning of the offices, as mentioned by Molina Gutiérrez et al. [10].
Regarding triage, the decrease on level 3 can be justified by the marked decrease in conditions usually screened with a higher priority, such as exacerbated asthma. The increase in level 5 is overinflated by the internal decision to assign this priority to elective screening for SARS-CoV-2 performed in the ES to optimise human and material resources.
With the closure of schools and the suspension of sports activities, the decrease in acute infectious diseases [11, 16], particularly viral [6, 11], and school and sports accidents was to be expected [4]. In this study, the decrease in the most common diagnoses, such as acute nasopharyngitis, acute gastroenteritis, and acute otitis media, was observed, a situation similar to a multicentre study carried out in France [11]. Also in Italy, a decrease in acute gastroenteritis and abdominal pain was identified (p < 0.01) [16]. However, there was an increase in the diagnosis of fever without other symptoms associated. This may be associated with an earlier visit to the PES, similar to the results observed in other studies [10, 16]. We speculate that these could correspond to viral infections; however, this was not documented.
The reduction in school and sports accidents predicted by Lazzerini et al. [4] was confirmed in this study, explaining the reduction observed in patients under the responsibility of orthopaedics. Conversely, the increase in accidents, such as wounds, falls, burns, and dog bites related to longer stays at home [5], may partially justify the increase in the percentage of patients observed by paediatric surgery.
Although it was hypothesised that the lockdown, the break in routines, and the disease itself could represent stress factors on the population with mental illness or predisposition to such [9], we found a significant reduction in child psychiatry episodes. The same was identified in the study by Dann et al., who observed a decrease of about 28% in episodes associated with mental health [9]. This may be due to the fact that psychiatric effects of the lockdown could take some time to appear and not yet evident in the study period.
During the study period, the admission rate increased significantly. The same pattern was observed in two PES in Italy [8]. This difference can be related to some organisational aspects, like the direct admission of the patients without the usual time of observation in the short-stay units and the admission of the elective patients using the ES for SARS-CoV-2 screening.
As seen in other studies [1, 4, 10], the number of cases of COVID-19 at paediatric age represented a small proportion (1.1%) of the total number of children tested. Infected children and adolescents had mild disease, with no need for intensive care or recorded deaths. These results are in line with other studies [1].
Unlike what happened in an Italian study [14], during this period, the paediatric staff did not develop SARS-CoV-2 infection.
This study has several limitations. One derives from the fact that it is retrospective and based on non-specifically directed clinical records. Another is related to the diagnostic classification system, ICD-9, which, by allowing underdiagnosis within groups of diseases, induces a dispersion of data and makes it difficult to interpret the results. Also, our centre is a COVID-19 reference hospital and this might have introduced some bias in the number of the admissions. Finally, as a new disease, for which it is little experience and literature, particularly in paediatric age, the change in attitudes in view of the evolution of the knowledge about the disease, namely in the space management and even the approach to diagnosis, may have had implications for the results obtained and their interpretation.
Conclusion
The pandemic brought a marked reduction in emergency admissions and a decrease in urgent cases and an increase in non-urgent patients, as well as a decrease in usually common diagnoses, but an increase in accidents, such as wounds, falls, burns, and dog bites.
Despite the low infection rate for SARS-CoV-2 at paediatric age, with mild symptoms or even asymptomatic, there were increased referrals by the phone line of the NHS and EMS and a higher admission rate in the ward.
Overcrowding was a major problem of the PES before the pandemic. The recent experience makes us consider that replication of the public health measures instituted, may contribute to the reduction of acute seasonal infections in the future.
Abbreviations
- CDC
Centers for Disease Control and Prevention
- CPTAS
Canadian Paediatric Triage and Acuity Scale
- COVID-19
Coronavirus disease 2019
- ES
Emergency service
- EMS
Emergency Medical Services
- GDH
General-Directorate of Health
- ICD-9
International Classification of Diseases 9
- IQR
Interquartile range
- NHS
National Health Service
- PCR
Polymerase chain reaction
- PES
Paediatric Emergency Service
- PHCS
Primary health care service
- PH-CHUC
Paediatric Hospital of the Centro Hospitalar e Universitário de Coimbra
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- SD
Standard deviation
- SPSS
Statistical Package for the Social Sciences
- WHO
World Health Organization
Authors’ contributions
All authors conceived the study and made substantial contributions to the design of the work. Rafaela Paiva and Cátia Martins contributed toward the acquisition of data. Rafaela Paiva, Cátia Martins, and Mariana Domingues performed the analysis and interpretation of the data and drafted the manuscript. Fernanda Rodrigues and Mariana Domingues revised it critically for important intellectual content.
Materials availability
All data relevant to the study are included in the article.
Code availability
N/A.
Declarations
Ethics approval
CHUC-085-20.
Consent for publication
All authors authorise publication.
Conflict of interest
The authors declare no competing interests.
Consent to participate
N/A.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rafaela Paiva, Email: rafaelapaiva5@gmail.com.
Cátia Martins, Email: aitacmartins@gmail.com.
Fernanda Rodrigues, Email: rodriguesfmp@gmail.com.
Mariana Domingues, Email: marianadomingues@chuc.min-saude.pt.
References
- 1.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145(6). [DOI] [PubMed]
- 2.WHO. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet]. [cited 2020 Sep 1]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-11-march-2020
- 3.Isba R, Edge R, Jenner R, Broughton E, Francis N, Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child. 2020;105(7):704. doi: 10.1136/archdischild-2020-319385. [DOI] [PubMed] [Google Scholar]
- 4.Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Heal. 2020;4(5):e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Santana R, Rocha J, Sousa J, Soares P. A procura de serviços de urgência/emergência hospitalar: tendências durante o primeiro mês de resposta à COVID-19. Escola Nacional de Saúde Pública, Universidade Nova de Lisboa. 2020.
- 6.Hartnett KP, Kite-Powell A, DeVies J, A. Coletta M, K. Boehmer T, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits — United States, January 1, 2019–May 30, 2020. Vol. 69, Centers for Disease Control and Prevention. 2020. [DOI] [PMC free article] [PubMed]
- 7.Silvia B, Danilo B, Ruth F, Niccolo P, Rianne O, Luigi T, et al. Preparedness and response to pediatric COVID-19 in European emergency departments: a survey of the REPEM and PERUKI networks. Ann Emerg Med. 2020;7(May):19–21. doi: 10.1016/j.annemergmed.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scaramuzza A, Tagliaferri F, Bonetti L, Soliani M, Morotti F, Bellone S, Cavalli C, Rabbone I. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch Dis Child. 2020;105(7):704–706. doi: 10.1136/archdischild-2020-319397. [DOI] [PubMed] [Google Scholar]
- 9.Dann L, Fitzsimons J, Gorman KM, Hourihane J, Okafor I. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch Dis Child 2020;0:1–2. [DOI] [PMC free article] [PubMed]
- 10.Molina Gutiérrez M, Domínguez J, Barriocanal M, Lavisier B, López R, Martín SJ. Impacto de la pandemia COVID-19 en urgencias: primeros hallazgos en un hospital de Madrid. An Pediatr. 2020;93:313–322. doi: 10.1016/j.anpedi.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Angouvant F, Ouldali N, Dawei Yang D, Filser M, Gajdos V, Rybak A et al (2020) COVID-19 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and non-viral infections, a time series analysis. Infect Dis Soc Am [DOI] [PMC free article] [PubMed]
- 12.Posfay-Barbe KM, Wagner N, Gauthey M, Moussaoui D, Loevy N, Diana A, et al. COVID-19 in children and the dynamics of infection in families. Pediatrics. 2020;146(2). [DOI] [PubMed]
- 13.Parri N, Magistà AM, Marchetti F, Cantoni B, Arrighini A, Romanengo M, et al. Characteristic of COVID-19 infection in pediatric patients: early findings from two Italian pediatric research networks. Eur J Pediatr. 2020;179(8):1315–1323. doi: 10.1007/s00431-020-03683-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buonsenso D, Onesimo R, Valentini P, Chiaretti A, Gatto A, Attinà G, Conti G, Vento G, Cambieri A, Mercuri E, Zampino G, on behalf of the pedCOVID-team Children’s healthcare during corona virus disease 19 pandemic: the Italian experience. Pediatr Infect Dis J. 2020;39(7):E137–E140. doi: 10.1097/INF.0000000000002732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Do children catch COVID-19? [Internet]. Sant Joan de Déu, Barcelona Hospital. 2020 [cited 2020 Oct 6]. Available from: https://www.sjdhospitalbarcelona.org/en/kidscorona/do-children-catch-covid-19
- 16.Cella A, Marchetti F, Iughetti L, Di Biase AR, Graziani G, De Fanti A, et al. Italian COVID-19 epidemic: effects on paediatric emergency attendance—a survey in the Emilia Romagna region. BMJ Paediatr Open. 2020;4(1):e000742. doi: 10.1136/bmjpo-2020-000742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z et al (2020) Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics.
- 18.Bialek S, Gierke R, Hughes M, McNamara LA, Pilishvili T, Skoff T. Coronavirus disease 2019 in children: current status. J Chinese Med Assoc. 2020;83(6):527–533. doi: 10.1097/JCMA.0000000000000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rose K, Van-Zyl K, Cotton R, Wallace S, Cleugh F. Paediatric attendances and acuity in the emergency department during the COVID-19 pandemic. medRxiv. 2020;
- 20.Cheek JA, Craig SS, West A, Lewena S, Hiscock H. Emergency department utilisation by vulnerable paediatric populations during the COVID-19 pandemic. Emerg Med Australas. 2020;32:870–871. doi: 10.1111/1742-6723.13598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pata D, Gatto A, Buonsenso D, Chiaretti A. A COVID-19 outbreak’s lesson: best use of the paediatric emergency department. Acta Paediatr Int J Paediatr. 2020;109(9):1903–1904. doi: 10.1111/apa.15386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DGS Norma no 004/2020 de 23/03/2020 atualizada a 14/10/2020 - COVID-19: abordagem do doente com suspeita ou confirmação de COVID-19. 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article.
N/A.