Abstract
Parkinson’s disease (PD), an age-related progressive neurodegenerative condition, is associated with loss of dopaminergic neurons in the substantia nigra pars compacta (SNpc), which results in motor deficits characterized by the following: akinesia, rigidity, resting tremor, and postural instability, as well as nonmotor symptoms such as emotional changes, particularly depression, cognitive impairment, gastrointestinal, and autonomic dysfunction. The most common treatment for PD is focused on dopamine (DA) replacement (e.g., levodopa = L-Dopa), which unfortunately losses its efficacy over months or years and can induce severe dyskinesia. Hence, more efficacious interventions without such adverse effects are urgently needed. In this review, following a general description of PD, potential novel therapeutic interventions for this devastating disease are examined. Specifically, the focus is on nicotine and nicotinic cholinergic system, as well as butyrate, a short chain fatty acid (SCFA), and fatty acid receptors.
Keywords: Parkinsonism, Nicotine, Butyrate, Short-chain fatty acids, Depression, Comorbidity, Combination therapy
Introduction
Parkinson’s disease (PD), the second most common progressive neurodegenerative disorder, is associated with loss of dopaminergic neurons in the substantia nigra pars compacta (SNc) that leads to striatal dopamine (DA) deficiency (Blesa and Przedborski 2014; Hustad and Aasly 2020; Liu 2020; Simon et al. 2020). This loss of dopaminergic neurons results in motor deficits characterized by the following: akinesia, rigidity, resting tremor, and postural instability, as well as nonmotor symptoms that might also involve other neurotransmitter systems including the cholinergic system (Perez 2015; Mirelman et al. 2019; Quik et al. 2019; Stoker and Barker 2020). The nonmotor symptoms may include the following: emotional changes (e.g., depression, apathy and anxiety), cognitive deficits (e.g., mild to severe memory impairment), sleep perturbations (e.g., insomnia/hypersomnia), autonomic dysfunction (e.g., bladder disturbances, orthostatic hypotension, sweating), sensory symptoms (e.g., pain, visual and olfactory deficits), gastrointestinal symptoms (e.g., constipation, nausea), as well as “social symptoms” (e.g., inability to produce facial expression or recognize other’s verbal and nonverbal cues) (Perez 2015; Dinter et al. 2020; Prenger et al. 2020).
Neuronal degeneration in PD involves several cellular and molecular events including accumulation of misfolded proteins, failure of protein clearance, mitochondrial damage, oxidative stress, neuroinflammation, immune dysregulation, apoptosis, excitotoxicity, Ca++ dysregulation, as well as autophagy and dysbiosis (Hurley and Tizabi 2013; Maiti et al. 2017; Reglodi et al. 2017; Zeng et al. 2018; Genovese et al. 2020; Indrieri et al. 2020; Parra et al. 2020; Dorszewska et al. 2021; Giorgi et al. 2021; Harms et al. 2021; Rani and Mondal, 2021). In addition, mutations in a number of genes such as leucine-rich repeat kinase 2 (LRRK2), Parkin RBR E3 ubiquitin protein ligase (PARK2), Parkinson disease protein 7 (PARK7), PTEN-induced putative kinase 1 (PINK1), alpha- synuclein (SNCA), as well as polymorphism in DA receptor D2 gene (DRD2Taq1A) have been identified (Klein and Westenberger 2012; Song et al. 2019; Tran et al. 2020).
Although the etiology remains unsettled, it is believed that PD is a multifactorial disease, with both genetic and environmental factors playing a role. The biggest risk factor for PD is old age, where median age of onset is estimated to be around 60 years of age (Lees et al. 2009; Kouli et al. 2018). In addition, it is postulated that exposure to environmental toxicants such as pesticides, herbicides, and heavy metals may increase the risk of PD (Anderson et al. 2020; McKnight and Hack 2020). In the early 1980s, it was discovered that injection of underground laboratory preparations of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) could result in nigrostriatal degeneration and development of typical PD motor symptoms. MPTP is a potent analog of the opioid analgesic meperidine that gets metabolized into the neurotoxin MPP + (1-methyl-4-phenylpyridinium). MPP + is a mitochondrial complex-I inhibitor as well as substrate for DA transporter (DAT) and has been shown to selectively damage the dopaminergic cells in SNpc (Langston et al. 1983; Fujita et al. 2020). For this reason, MPTP models of PD are commonly used to investigate the mechanism of neurotoxicity and/or development of novel therapeutics (Schneider et al. 2021; Zheng et al. 2021). Similarly, rotenone, a pesticide which is also selective inhibitor of mitochondrial complex-I, is used in animal models of PD (Betarbet et al. 2000; Kouli et al. 2018). In addition, exposure to heavy metals such as manganese (Peres et al. 2016; Andrade et al. 2017; Ivleva et al. 2020) or iron (Ganz, 2018; Huang et al. 2019; Ndayisaba et al. 2019; Shi et al. 2019) have also been implicated in PD etiology. Interestingly, reduction of iron content via clioquinol was associated with a remarkable improvement of the motor and nonmotor deficits in an MPTP-induced monkey model of PD (Shi et al. 2020).
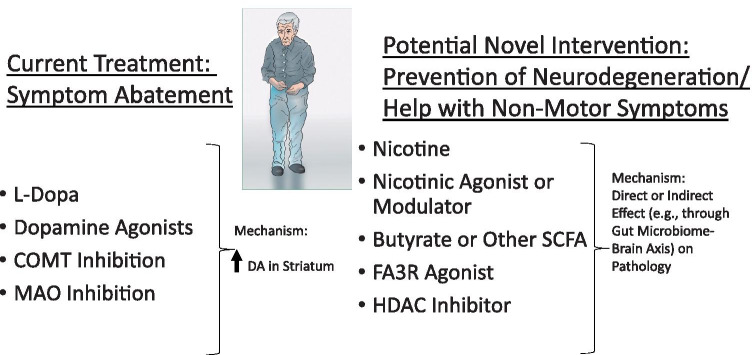
The most common treatment of PD is focused on DA replacement (e.g., levodopa = L-Dopa), which unfortunately losses its full efficacy in few years and can induce severe dyskinesia, or abnormal involuntary movements (Quik et al. 2019; Sy and Fernandez 2020; Bjørklund et al. 2020). For this reason, DA receptor agonists such as pramipexole and ropinirole may be used initially and inhibitors of DA metabolizing enzymes such as selegiline or rasagiline, both monoamine oxidase (MOA) inhibitors, or catechol-O-methyltransferase (COMT) inhibitors such as entacapone and tolcapone are often used in combination with L-Dopa (Aradi and Hauser 2020; Zheng et al. 2021). Nonpharmacologic interventions including repetitive transcranial magnetic stimulation (rTMS), and in specific circumstances neurosurgery (i.e., deep brain stimulation) may also be applied (Li et al. 2020a; Sui et al. 2021). In addition, significant efforts are devoted to development of autologous, stem cell-derived grafts, as well as viral gene therapies (Stoker et al. 2018; Osborn et al. 2020; Stoker and Barker 2020; Tao et al. 2021). Nonetheless, more efficacious interventions targeting the neurodegenerative aspect of the disease are urgently needed. Here, we discuss potential use of nicotine or nicotinic cholinergic agonists/modulators alone or together with butyrate, a short-chain fatty acid and fatty acid 3 receptor (FA3R) agonists as alternative and/or additional interventions in PD treatment (Fig. 1).
Fig. 1.
Schematic diagram depicting current pharmacotherapies for PD which result in symptomatic relief of symptoms due increase in the striatal DA (left panel). Potential novel intervention that may target the neurodegenerative aspect of the disease and may also help with nonmotor symptoms (right panel)
nAChRs
The inverse relationship between PD incidence and any form of nicotine intake such as cigarette smoking (Hernán et al. 2002; Ritz et al. 2007; Li et al. 2015), smokeless tobacco (O’Reilly et al. 2005; Liu et al. 2017b; Yang et al. 2017), exposure to environmental tobacco smoke (Searles Nielsen et al. 2012; Han et al. 2020a; Liu et al. 2020), or even from a dietary source such as peppers (Ma et al. 2020) suggests a therapeutic potential for nicotine in PD. This contention is further supported by numerous preclinical studies indicating neuroprotective effects of nicotine, especially in dopaminergic cell models as well as in vivo models of PD (discussed below). Hereby, following a brief discussion of nicotinic cholinergic system, we will focus on its therapeutic utility in PD.
Nicotine’s main targets are nicotinic receptors (nAChRs) that are widely distributed in the central nervous system (Clark and Pert 1985; Dani 2015; Wills and Kenny 2021). nAChRs belong to ionotropic class of receptors, which act by regulating directly the opening of a cation channel in the neuronal membrane (Dani 2015; Changeux 2018; Papke and Lindstrom 2020). Various subtypes of these receptors with distinct anatomical, physiological, and pharmacological characteristics have been identified (Dani 2015). Although nAChRs are present at various sites and in various organs such as neuromuscular junction, autonomic ganglia, and the central nervous system, the subunit structures of these receptors are different from each other (Kalamida et al. 2007). Considerable information on interaction between neuronal nAChRs consisting mainly of alph4-beta2 or homomeric alpha7 subunits and other neurotransmitter systems is now available (Wittenberg et al. 2020; Wills and Kenny 2021). Moreover, specific responses of these receptors to nicotine and their involvement in cognitive functions have been investigated (Valentine and Sofuoglu 2018; Azimi et al. 2020). Indeed, a potential role of nAChRs in high-order cognitive processing has been suggested (Koukouli and Changeux 2020). Therapeutic potential for selective nAChR agonists in various neuropsychiatric and neurodegenerative disorders including PD (Quik et al. 2019; Tizabi et al. 2019; Liu 2020), depression (Gandelman et al. 2018; Tizabi et al. 2019; Conti et al. 2020), mild cognitive impairment or Alzheimer’s disease (Vega et al. 2019; Azimi et al. 2020; Hahn et al. 2020; Koukouli and Changeux 2020), ischemia (Han et al. 2020b), schizophrenia (Terry and Callahan, 2020), pain (Bagdas et al. 2018), as well as energy balance (Seoane-Collazo et al. 2021) have been proposed. Given that there is a relatively high comorbid existence between depression and PD, a nicotinic intervention may have the added advantage of addressing both issues at the same time (Tizabi et al. 2019).
Role of the Nicotinic Cholinergic System in Parkinson’s Disease
Multiple studies indicate that the normal function of the basal ganglia, intimately involved in movement regulation, is dependent on the equilibrium between the midbrain dopaminergic and striatal cholinergic systems (Aosaki et al. 2010; Scarduzio et al. 2017; Assous, 2021). Thus, acetylcholine can regulate striatal DA release via an interaction at various nAChRs (Quik et al. 2019; Liu 2020). Further importance of ACh in the basal ganglia is evident from the effect of cholinergic agents in patients suffering from various neurological disorders such as Tourette syndrome, dystonia, as well as PD (Assous, 2021). In various experimental animal models of PD (e.g., 6-OHDA lesioned rodents), the impairments in DA release appear to be exacerbated by loss of nAChRs activation, suggesting that nicotinic agonists may ameliorate the dopaminergic imbalance and may thus be useful therapeutic targets for PD (Shimohama and Kawamata, 2018; Quik et al. 2019). In this regard, a number of in vitro and in vivo studies including primates and genetically modified mice have shown protective effects of nicotine against neuronal damage and/or neurotoxicity induced by 6-OHDA, MPTP, rotenone, methamphetamine, glutamate, and β-amyloid (reviewed in: Shimohama and Kawamata, 2018; Quik et al. 2019; Tizabi et al. 2019). These effects are mediated via selective nAChR subtypes containing β2 and α7 subunits (see Quik et al. 2019; Tizabi et al. 2019). We have also observed protective effects of nicotine against endogenous substances such as salsolinol (discussed later) and aminochrome that selectively damage dopaminergic cells (see Tizabi et al. 2019). More recently, protective effects of nicotine against toxicity induced by iron and manganese were also observed in cell culture (Getachew et al. 2019a). Additionally, Quik et al. (2019) have shown beneficial effects of nicotine against L-Dopa-induced dyskinesia in nonhuman primate models. Interestingly, nicotinic cholinergic system may also play a role in L-Dopa-induced dyskinesias (Bordia and Perez 2019). Hence, targeting nicotinic cholinergic receptors appears to offer a novel intervention in PD (Tizabi and Getachew, 2017, Quick, 2019; Tizabi et al. 2019, Liu 2020; Vetel et al., 2021). Nicotine’s effects are likely to involve suppression of pro-inflammatory cytokines and stimulation of neurotrophic factors as well as suppression of oxidative stress (Barreto et al. 2015; Perez 2015; Tizabi 2019; Dong et al. 2020; Vetel et al. 2021).
Several human studies have assessed the effects of nicotine gum or patch in PD, most of which have not yielded positive results (Vieregge et al. 2001; Lemay et al. 2004; see also Tizabi and Getachew 2017). The negative finding in these trials is likely due to the mode of administration of nicotine (Tizabi and Getachew 2017). Thus, it is very important to consider the route of nicotine administration, where subdermal administration via patch may not achieve the desirable nicotinic receptor stimulation obtained via pulsatile nicotine (e.g., via inhalation) (Feathersone and Siegel 2015; Tizabi and Getachew 2017). The very complex dynamic interaction of nicotine with its receptors, where initial stimulation can be followed by rapid and differential desensitization of receptor subtypes, has to be critically considered in experimental paradigms so that maximal therapeutic outcome may be obtained (Dani 2015; Tizabi and Getachew 2017; Quik et al. 2019). Thus, it may be suggested that pulsatile stimulation of specific nAChRs in selective brain regions, particularly in the nigrostriatal pathway would be critical for its therapeutic effects in PD. This could be achieved by administering nicotine via inhalation, or nasal spray. It is of relevance to note that a recent clinical study using oral administration of nicotine, reported positive effects of nicotine on falls and freezing gait in PD (Lieberman et al. 2019). Furthermore, pulsatile nicotine preparations in forms of inhalers or nasal spray are available and approved by FDA for smoking cessation and could be re-purposed for PD pending evaluation of their effectiveness in clinical trials. In addition, as alluded to earlier, potential usefulness of a pulsatile nicotine administration in improving nonmotor symptoms (e.g., depression or cognitive decline) that are commonly associated with PD (Quik et al. 2015; Tizabi and Getachew 2017; Tizabi et al. 2019), could be an added advantage of nicotinic therapy (Fig. 1).
Still, the addictive properties of nicotine (Stolerman and Jarvis, 1995; Willis and Kenny, 2021) might be of concern in its therapeutic application. In this regard, significant efforts are expanded in developing selective nicotinic receptor subtype agonists or nicotinic receptor modulators that would be of similar potency but without the addictive component (Ryan et al, 2001; Bordia et al., 2015). Nonetheless, taking into account the risk/benefit ratio of nicotine, it might still be a useful tool in PD until more suitable nonaddictive compounds are developed (Mitra et al. 2020).
It is of utmost importance, however, to emphasize that the suggested interventions are for pure nicotine available via pharmaceutical preparation and not smoking. The detrimental consequences of tobacco (chewed or smoked) or even e-cigarettes on various organs and lately in COVID-19 pandemic have been recognized (Li et al. 2020b; Ruszkiewicz et al. 2020; Tizabi et al. 2020), and hence, none of such modes should be attempted as self-medication by any PD patient. Moreover, controlled clinical trials of nicotinic preparations to establish the dose and efficacy and ultimate FDA approval are required for any nicotinic intervention in PD.
Butyrate
Butyrate is a short-chain fatty acid (SCFA) that is produced by gut microbiota and acts primarily as an energy source for colonic epithelial cells and has been shown to have anti-inflammatory, enteroendocrine and epigenetic effects that not only influences colonic and systemic health but can also affect the brain function (Cantu-Jungles et al., 2019). Recent advances in our understanding of the gut-brain axis has resulted in new insights and potential novel targets for therapeutic intervention in PD (Baizabal-Carvallo and Alonso-Juarez, 2020; Cirstea et al. 2020; Cryan et al. 2020). Indeed, it has been suggested that the initiation and progression of PD may be impeded through manipulation of the gut microbiota. Specifically, it has been suggested that misfolding of alpha-synuclein (α-Syn), a protein highly implicated in PD pathology, can be brought about via dysbiosis or altered colonic microbiota and subsequent neuroinflammation (Keshavarzian et al. 2015; Sampson et al. 2016; Meng et al. 2019; Koutzoumis et al. 2020). This contention is further supported by the observation that the composition of the gut microbiota and SCFAs might be altered in patients with PD (Unger et al. 2016; Nuzum et al. 2020; Shin et al. 2020). Thus, there is a strong indication for therapeutic use of SCFAs, particularly butyrate, the most studied SCFA, for PD treatment. In this regard, a few studies have shown beneficial effects of sodium butyrate in various animal models of PD (St Laurent et al. 2013; Liu et al. 2017a; Funakohi-Tago et al. 2018; Russo et al. 2018; Srivastav et al. 2019; Hou et al. 2021), although at higher doses, this compound might aggravate the colonic inflammation in an MPTP mouse model (Qiao et al. 2020a). In vitro and in vivo studies have consistently found protective effects of sodium butyrate against dopaminergic cell damage brought about by alpha-synuclein (Paiva et al. 2017; Qiao et al. 2020b). This protection is against both transcriptional deregulation and DNA damage (Paiva et al. 2017). The postulated mechanism for in vivo effect of sodium butyrate in degradation of α-synuclein is via Atg5-dependent and PI3K/Akt/mTOR-related autophagy pathway (Qiao et al. 2020b). Beneficial effects of butyrate in PD are further evidenced by its attenuation of neurotoxic or motor impairments induced by 6-hydroxydopamine, rotenone, and MPTP (Funakohi-Tago et al. 2018; Srivastav et al. 2019; Hou et al. 2021).
We have also observed that butyrate as well as AR 420,626 (AR), chemical name: N-(2,5-dichlorophenyl)-4-(furan-2-yl)-2-methyl-5-oxo-1,4,5,6,7,8-hexahydroquinoline-3-carboxamide), another agonist of the fatty acid-3 receptor (FA3R) can protect against salsolinol-induced toxicity in SH-SY5Y cells, which as discussed below has important implications for PD (Getachew et al. 2020). Salsolinol (SALS = 1-methyl-6,7-dihydroxy-1,2,3,4-tetrahydroisoquinoline), which has structural similarity with MPTP, is an adduct formed as a condensation product of DA and aldehydes and is considered an endogenous DA modulator with selective toxicity to dopaminergic neurons in the substantia nigra (Storch et al. 2002; Maruyama et al. 2004; Naoi et al. 2004; Mravec 2006). Dysregulation of SALS, especially its (R) enantiomer in the brain, is thought to contribute to development of PD (Antkiewicz-Michaluk 2002; Xicoy et al. 2017). The observed higher level of SALS in the cerebrospinal fluid and urine of PD patients has led to the suggestion of its measurement as a potential marker for PD (Storch et al. 2002; Maruyama et al. 2004; Naoi et al. 2004; Sharma et al. 2013; Zheng et al. 2018; Voon et al. 2020), although elevated levels of systemic derivatives of norsalsolinol may also arise from the metabolism of levodopa (Scholz et al. 2004). That SALS may actually be produced by gut microbiota, further strengthens the gut-brain axis hypothesis of PD (Villageliú et al. 2018).
SH-SY5Y cells, human neuroblastoma-derived cell line, express high levels of dopaminergic activity and are used extensively to study possible mechanism(s) of toxicity and protection in nigral dopaminergic neurons (Copeland et al. 2007; Qualls et al. 2014; Xicoy et al. 2017; Getachew et al. 2019a). As alluded to above, we observed that both butyrate and AR, a FA3 receptor agonist (Hudson et al. 2014; Bolognini et al. 2016; Kaji et al. 2018), fully blocked SALS-induced toxicity. However, the effect of butyrate was blocked partially, whereas the effect of AR was blocked totally by beta-hydroxy butyrate (BHB), a selective FA3R antagonist. This suggests that some of the effects of butyrate might be independent of FA3R activation (see below). However, since at least part of the butyrate effect is mediated through FA3R stimulation, it would not be unreasonable to suggest that agonists of this receptor might also be of therapeutic potential in PD treatment (Getachew et al. 2020) (Fig. 1).
Several mechanisms of action, including histone deacetylase (HDAC) inhibition, activation of Nrf2/HO-1 axis (activation of antioxidant defense and detoxifying genes), stimulation of glucagon like peptide-1, as well as binding to several specific G protein–coupled receptors (GPCRs) such as FA2R and FA3R (Liu et al 2017a; Funakohi-Tago et al. 2018; Cantu-Jungles et al. 2019) have been attributed to butyrate. That the effect of butyrate was partially blocked by a specific FA3R antagonist suggests that mechanism(s) other than activation of FA3R are also involved in its neuroprotective effects (Getachew et al. 2020). In this regard, protective effects of sodium butyrate against dopaminergic cell damage in vitro has been attributed mainly to HDAC inhibition (Paiva et al. 2017). Hence, targeting HDAC may also be a viable source for novel intervention in PD (Fig. 1).
It is noteworthy that butyrate not only may have neuroprotective effects but may also have beneficial application against several other diseases including graft rejection, inflammatory bowel disease, colorectal cancer, and diabetes, all of which carry an inflammatory component (Tikhonova, 2017; Alrafas et al. 2019; Baxter et al. 2019). More recently, butyrate was also advocated for treatment of obesity and sleep disorders (Baxter et al. 2019; Szentirmai et al. 2019). However, a possible drawback to butyrate’s therapeutic use may be its poor pharmacological properties including short half-life and first-pass hepatic clearance (Witt et al. 2003; Sampathkumar et al. 2006; Yoo and Jones 2006; Ghosh et al. 2012). Therefore, if AR or any other selective FA3R agonist, with a better pharmacologic profile than butyrate, show similar effects as butyrate, then their use in the myriad of diseases mentioned above can be advocated. Moreover, since some of protective effects of butyrate may be due to HDAC inhibition, it would be of importance to determine whether such compounds would also have a similar effect on HDAC (Srivastav et al. 2019). Nonetheless, it is noteworthy that several selective FA3R agonists including AR were shown to be effective in blocking NSAID-induced enteropathy (intestinal pathology) in rats (Said et al. 2017).
Similar to what was observed for nicotine, butyrate also has shown antidepressant properties. Thus, it was observed that sodium butyrate functions as an antidepressant in several animal models of depression including maternal deprivation and chronic mild stress (Gundersen and Blendy 2009; Valvassori et al. 2014). More recently, it was reported that sodium butyrate also ameliorates depressive-like behavior in lipopolysaccharide-induced depression and that this effect is mediated via inhibition of neuroinflammation and oxido-nitrosative stress (Qiu et al. 2020). These effects are likely mediated through FA3R stimulation as it was shown that histone deacetylase inhibition was not a mechanism for butyrate’s antidepressant effect (Gundersen and Blendy 2009).
As mentioned previously, there is relatively high comorbid existence between depression and PD. Hence, here also intervention by butyrate may have the added advantage of addressing both issues at the same time (Tizabi et al. 2019). In this regard, it is also noteworthy that drugs that have neuroprotective effects are likely to also show mood regulating and antidepressant properties (Tizabi 2016). On the other hand, antidepressants are also likely to show at least some neuroprotective effects (Tizabi 2016). This duality of neuroprotective/antidepressant effects are likely due to some overlap of circuitries as well as common neurobiological substrates involved in dysregulation of mood and neurodegenerative phenotypes, particularly in PD (Tizabi 2016; Tizabi et al. 2019). Moreover, recent advances also strongly connect gut microbiota not only with neurodegenerative diseases as discussed above but also with pain (Russo et al., 2018), neurodevelopmental disorders such as autism (Almeida et al. 2020; Lungba et al. 2020; O'Connor et al. 2021), neuropsychiatric disorders such as schizophrenia (Dinan and Cryan 2020; Kelly et al. 2020), and particularly depression (Caspani et al. 2019; Cruz-Pereira and Cryan, 2020). Several mechanisms including deficits in neurogenesis and synaptogenesis, reduced cortical and hippocampal expression of brain-derived neurotrophic factor (BDNF), exaggerated hypothalamic pituitary adrenal (HPA) axis response, and neuroinflammation have been implicated in dysbiosis and depressive-like characteristics (Caspani et al. 2019; Getachew et al. 2019b; Getachew and Tizabi 2019; Cruz-Pereira and Cryan 2020). Since as mentioned earlier, depression is a common manifestation with PD, agents such as butyrate or other compounds interacting with gut microbiota would be ideal candidates for further investigation in comorbid conditions.
Combination Therapy
An important consideration in disease modification is potential combination of drugs with various mechanism of action to affect the chain of events at various sites to prevent the pathology and/or the phenotype. Thus, it might prove prudent to combine the aforementioned drugs, namely nicotine and/or nicotinic agonists/modulators with butyrate and/or an FA3R agonist for maximum efficacy. Moreover, such drugs may be added to current medications used in PD to improve therapeutic outcome, particularly for comorbid conditions. In this regard, some of the current medications might actually be targeting some of the same sites discussed above, albeit to a lesser degree. For example, it was recently demonstrated that COMT inhibitors that are commonly used in PD can also affect the gut microbiota implicated in PD (Grün et al. 2020). Interestingly, recent studies also provide evidence of nicotine interaction with gut microbiota (Chi et al. 2017; Pavia and Plummer 2020). Specifically, it was demonstrated that oxidative stress response as well as DNA repair genes were particularly enriched in gut microbiome of mice treated with nicotine (Chi et al. 2017). Thus, multi-level effects of nicotine and butyrate would render their potential additive or synergistic effects in PD and perhaps more specifically in PD-depression comorbidity a very viable outcome. In support of this contention, we have recently observed a synergistic interaction between nicotine and butyrate against SALS-induced toxicity in SH-SY5Y cells (under preparation).
In summary, nicotine or nicotinic agonists or modulators alone or together with butyrate and/or FA3R agonists hold significant promise as novel therapeutic interventions in PD.
Funding
Supported by NIH/NIAAA R03AA022479 and Howard University College of Medicine Bridge Funds and Pilot Study Awards Program (BFPSAP) 2020–2021 (YT) and NIH/NIEHS R01ES10563 and R01ES07331 (MA).
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Almeida C, Oliveira R, Soares R, Barata P. Influence of gut microbiota dysbiosis on brain function:a systematic review. Porto Biomed j. 2020;5(2):1–8. doi: 10.1097/j.pbj.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alrafas HR, Busbee PB, Nagarkatti M. Nagarkatti PS Resveratrol modulates the gut microbiota to prevent murine colitis development through induction of Tregs and suppression of Th17 cells. J Leukoc Biol. 2019;106(2):467–480. doi: 10.1002/JLB.3A1218-476RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson CC, Marentette JO, Rauniyar AK, Prutton K, Khatri M, Matheson C, et al. Maneb alters central carbon metabolism and thiol redox status in a toxicant model of Parkinson’s disease. Free Radic Biol Med. 2020;S0891–5849(20):31641–31645. doi: 10.1016/j.freeradbiomed.2020.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade VM, Aschner M. Marreilha Dos Santos AP. Neurotoxicity of Metal Mixtures Adv Neurobiol. 2017;18:227–265. doi: 10.1007/978-3-319-60189-2_12. [DOI] [PubMed] [Google Scholar]
- Antkiewicz-Michaluk L. Endogenous risk factors in Parkinson’s disease: dopamine and tetrahydroisoquinolines. Pol J Pharmcol. 2002;54:567–572. [PubMed] [Google Scholar]
- Aosaki T, Miura M, Suzuki T, Nishimura K, Masuda M. Acetylcholine-dopamine balance hypothesis in the striatum: an update. Geriatr Gerontol Int. 2010;10(Suppl 1):S148–S157. doi: 10.1111/j.1447-0594.2010.00588.x. [DOI] [PubMed] [Google Scholar]
- Aradi SD, Hauser RA. Medical management and prevention of motor complications in Parkinson's disease. Neurotherapeutics. 2020;17(4):1339–1365. doi: 10.1007/s13311-020-00889-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assous M (2021) Striatal cholinergic transmission. Focus on nicotinic receptors' influence in striatal circuits. Eur J Neurosci. 53(8):2421–2442 [DOI] [PMC free article] [PubMed]
- Azimi M, Oemisch M, Womelsdorf T. Dissociation of nicotinic α7 and α4/β2 sub-receptor agonists for enhancing learning and attentional filtering in nonhuman primates. Psychopharmacology. 2020;237(4):997–1010. doi: 10.1007/s00213-019-05430-w. [DOI] [PubMed] [Google Scholar]
- Bagdas D, Gurun MS, Flood P, Papke RL, Damaj MI. New insights on neuronal nicotinic acetylcholine receptors as targets for pain and inflammation: a focus on α7 nAChRs. Curr Neuropharmacol. 2018;16:415–425. doi: 10.2174/1570159X15666170818102108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baizabal-Carvallo JF, Alonso-Juarez M. The link between gut dysbiosis and neuroinflammation in Parkinson's disease. Neuroscience. 2020;432:160–173. doi: 10.1016/j.neuroscience.2020.02.030. [DOI] [PubMed] [Google Scholar]
- Barreto GE, Iarkov A, Moran VE. Beneficial effects of nicotine, cotinine and its metabolites as potential agents for Parkinson's disease. Front Aging Neurosci. 2015;6:340. doi: 10.3389/fnagi.2014.00340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter NT, Schmidt AW, Venkataraman A, Kim KS, Waldron C, Schmidt TM (2019) Dynamics of human gut microbiota and short-chain fatty acids in response to dietary interventions with three fermentable fibers. mBio. 10(1):e02566–18 [DOI] [PMC free article] [PubMed]
- Betarbet R, Sherer TB, MacKenzie G, Garcia-Osuna M, Panov AV, Greenamyre JT. Chronic systemic pesticide exposure reproduces features of Parkinson's disease. Nat Neurosci. 2000;3(12):1301–1306. doi: 10.1038/81834. [DOI] [PubMed] [Google Scholar]
- Bjørklund G, Dadar M, Anderson G, Chirumbolo S, Maes M. Preventive Treatments to Slow Substantia Nigra Damage and Parkinson's Disease Progression: A Critical Perspective Review Pharmacol Res. 2020;161:105065. doi: 10.1016/j.phrs.2020.105065. [DOI] [PubMed] [Google Scholar]
- Blesa J, Przedborski S. Parkinson's disease: animal models and dopaminergic cell vulnerability. Front Neuroanat. 2014;8:155. doi: 10.3389/fnana.2014.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolognini D, Tobin AB, Milligan G, Moss CE. The pharmacology and function of receptors for short-chain fatty acids. Mol Pharmacol. 2016;89(3):388–398. doi: 10.1124/mol.115.102301. [DOI] [PubMed] [Google Scholar]
- Bordia T, McGregor M, Papke RL, Decker MW, McIntosh JM, Quik M. The α7 nicotinic receptor agonist ABT-107 protects against nigrostriatal damage in rats with unilateral 6-hydroxydopamine lesions. Exp Neurol. 2015;263:277–284. doi: 10.1016/j.expneurol.2014.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bordia T, Perez XA. Cholinergic control of striatal neurons to modulate L-dopa-induced dyskinesias. Eur J Neurosci. 2019;49(6):859–868. doi: 10.1111/ejn.14048. [DOI] [PubMed] [Google Scholar]
- Cantu-Jungles TM, Rasmussen HE, Hamaker BR. Potential of prebiotic butyrogenic fibers in Parkinson's disease. Front Neurol. 2019;10:663. doi: 10.3389/fneur.2019.00663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspani G, Kennedy S, Foster JA, Swann J. Gut microbial metabolites in depression: understanding the biochemical mechanisms. Microb Cell. 2019;6(10):454–481. doi: 10.15698/mic2019.10.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Changeux JP. The nicotinic acetylcholine receptor: a typical 'allosteric machine'. Philos Trans R Soc Lond B Biol Sci. 2018;373(1749):20170174. doi: 10.1098/rstb.2017.0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi L, Mahbub R, Gao B, Bian X, Tu P, Ru H, et al. Nicotine alters the gut microbiome and metabolites of gut-brain interactions in a sex-specific manner. Chem Res Toxicol. 2017;30(12):2110–2119. doi: 10.1021/acs.chemrestox.7b00162. [DOI] [PubMed] [Google Scholar]
- Cirstea MS, Yu AC, Golz E, Sundvick K, Kliger D, Radisavljevic N, et al. Microbiota composition and metabolism are associated with gut function in Parkinson's disease. Mov Disord. 2020;35(7):1208–1217. doi: 10.1002/mds.28052. [DOI] [PubMed] [Google Scholar]
- Clarke PB, Pert A. Autoradiographic evidence for nicotine receptors on nigrostriatal and mesolimbic dopaminergic neurons. Brain Res. 1985;348(2):355–358. doi: 10.1016/0006-8993(85)90456-1. [DOI] [PubMed] [Google Scholar]
- Conti AA, Tolomeo S, Steele JD, Baldacchino AM. Severity of negative mood and anxiety symptoms occurring during acute abstinence from tobacco: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2020;115:48–63. doi: 10.1016/j.neubiorev.2020.04.018. [DOI] [PubMed] [Google Scholar]
- Copeland RL, Jr, Das JR, Kanaan YM, Taylor RE, Tizabi Y. Antiapoptotic effects of nicotine in its protection against salsolinol-induced cytotoxicity. Neurotox Res. 2007;12(1):61–69. doi: 10.1007/BF03033901. [DOI] [PubMed] [Google Scholar]
- Cruz-Pereira JS, Cryan JF. In need of a quorum: from microbes to mood via the immune system. Am J Psychiatry. 2020;177(10):895–897. doi: 10.1176/appi.ajp.2020.20081182. [DOI] [PubMed] [Google Scholar]
- Cryan JF, O'Riordan KJ, Sandhu K, Peterson V, Dinan TG. The gut microbiome in neurological disorders. Lancet Neurol. 2020;19(2):179–194. doi: 10.1016/S1474-4422(19)30356-4. [DOI] [PubMed] [Google Scholar]
- Dani JA. Neuronal nicotinic acetylcholine receptor structure and function and response to nicotine. Int Rev Neurobiol. 2015;124:3–19. doi: 10.1016/bs.irn.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinan TG, Cryan JF. Gut microbiota: a missing link in psychiatry. World Psychiatry. 2020;19(1):111–112. doi: 10.1002/wps.20726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinter E, Saridaki T, Diederichs L, Reichmann H, Falkenburger BH. Parkinson’s disease and translational research. Transl Neurodegener. 2020;9(1):43. doi: 10.1186/s40035-020-00223-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y, Bi W, Zheng K, Zhu E, Wang S, Xiong Y, et al. Nicotine prevents oxidative stress-induced hippocampal neuronal injury through α7-nAChR/Erk1/2 signaling pathway. Front Mol Neurosci. 2020;13:557647. doi: 10.3389/fnmol.2020.557647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorszewska J, Kowalska M, Prendecki M, Piekut T, Kozlowska J, Kozubski W. Oxidative stress factors in Parkinson’s disease. Neural Regen Res. 2021;16(7):1383–1391. doi: 10.4103/1673-5374.300980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Featherstone RE, Siegel SJ. The Role of Nicotine in Schizophrenia. Int Rev Neurobiol. 2015;124:23–78. doi: 10.1016/bs.irn.2015.07.002. [DOI] [PubMed] [Google Scholar]
- Fujita A, Fujita Y, Pu Y, Chang L, Hashimoto K. MPTP-induced dopaminergic neurotoxicity in mouse brain is attenuated after subsequent intranasal administration of (R)-ketamine: a role of TrkB signaling. Psychopharmacology. 2020;237(1):83–92. doi: 10.1007/s00213-019-05346-5. [DOI] [PubMed] [Google Scholar]
- Funakohi-Tago M, Sakata T, Fujiwara S, Sakakura A, Sugai T, Tago K, et al. Hydroxytyrosol butyrate inhibits 6-OHDA-induced apoptosis through activation of the Nrf2/HO-1 axis in SH-SY5Y cells. Eur J Pharmacol. 2018;834:246–256. doi: 10.1016/j.ejphar.2018.07.043. [DOI] [PubMed] [Google Scholar]
- Gandelman JA, Newhouse P, Taylor WD. Nicotine and networks: potential for enhancement of mood and cognition in late-life depression. Neurosci Biobehav Rev. 2018;84:289–298. doi: 10.1016/j.neubiorev.2017.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz AB, Beker N, Hulsman M, Sikkes S, Netherlands Brain Bank Scheltens P, Smit AB et al (2018) Neuropathology and cognitive performance in self-reported cognitively healthy centenarians. Acta Neuropathol Commun 6(1):64 [DOI] [PMC free article] [PubMed]
- Genovese I, Giamogante F, Barazzuol L, Battista T, Fiorillo A, Vicario M, et al. Sorcin is an early marker of neurodegeneration, Ca2+dysregulation and endoplasmic reticulum stress associated to neurodegenerative diseases. Cell Death Dis. 2020;11(10):861. doi: 10.1038/s41419-020-03063-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getachew B, Csoka AB, Aschner M, Tizabi Y. Nicotine protects against manganese and iron-induced toxicity in SH-SY5Y cells: Implication for Parkinson's disease. Neurochem Int. 2019;124:19–24. doi: 10.1016/j.neuint.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getachew B, Reyes RE, Davies DL, Tizabi Y. Moxidectin effects on gut microbiota of Wistar-Kyoto rats: relevance to depressive-like behavior. Clin Pharmacol Transl Med. 2019;3(1):134–142. [PMC free article] [PubMed] [Google Scholar]
- Getachew B, Tizabi Y. Antidepressant effects of moxidectin, an antiparasitic drug, in a rat model of depression. Behav Brain Res. 2019;376:112220. doi: 10.1016/j.bbr.2019.112220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getachew B, Csoka AB, Bhatti A, Copeland RL, Tizabi Y. Butyrate protects against salsolinol-induced toxicity in SH-SY5Y cells: implication for Parkinson's disease. Neurotox Res. 2020;38(3):596–602. doi: 10.1007/s12640-020-00238-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh SK, Perrine SP, Williams RM, Faller DV. Histone deacetylase inhibitors are potent inducers of gene expression in latent EBV and sensitize lymphoma cells to nucleoside antiviral agents. Blood. 2012;119(4):1008–1017. doi: 10.1182/blood-2011-06-362434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giorgi C, Bouhamida E, Danese A, Previati M, Pinton P, Patergnani S. relevance of autophagy and mitophagy dynamics and markers in neurodegenerative diseases. Biomedicines. 2021;9(2):149. doi: 10.3390/biomedicines9020149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grün D, Zimmer VC, Kauffmann J, Spiegel J, Dillmann U, Schwiertz A, et al. Impact of oral COMT-inhibitors on gut microbiota and short chain fatty acids in Parkinson’s disease. Parkinsonism Relat Disord. 2020;70:20–22. doi: 10.1016/j.parkreldis.2019.11.020. [DOI] [PubMed] [Google Scholar]
- Gundersen BB, Blendy JA. Effects of the histone deacetylase inhibitor sodium butyrate in models of depression and anxiety. Neuropharmacology. 2009;57(1):67–74. doi: 10.1016/j.neuropharm.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn B, Harvey AN, Concheiro-Guisan M, Huestis MA, Ross TJ, Stein EA. Nicotinic receptor modulation of the default mode network. Psychopharmacology. 2020;238(2):589–597. doi: 10.1007/s00213-020-05711-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han C, Lu Y, Cheng H, Wang C, Chan P. The impact of long-term exposure to ambient air pollution and second-hand smoke on the onset of Parkinson disease: a review and meta-analysis. Public Health. 2020;179:100–110. doi: 10.1016/j.puhe.2019.09.020. [DOI] [PubMed] [Google Scholar]
- Han T, Wang Q, Lai R, Zhang D, Diao Y, Yin Y. Nicotine induced neurocognitive protection and anti-inflammation effect by activating α 4β 2 nicotinic acetylcholine receptors in ischemic rats. Nicotine Tob Res. 2020;22(6):919–924. doi: 10.1093/ntr/ntz126. [DOI] [PubMed] [Google Scholar]
- Harms AS, Ferreira SA, Romero-Ramos M (2021) Periphery and brain, innate and adaptive immunity in Parkinson's disease. Acta Neuropathol. Epub ahead of print [DOI] [PMC free article] [PubMed]
- Hernán MA, Takkouche B, Caamaño-Isorna F, Gestal-Otero JJ. A meta-analysis of coffee drinking, cigarette smoking, and the risk of Parkinson’s disease. Ann Neurol. 2002;52(3):276–284. doi: 10.1002/ana.10277. [DOI] [PubMed] [Google Scholar]
- Hou Y, Li X, Liu C, Zhang M, Zhang X, Ge S, Zhao L (2021) Neuroprotective effects of short-chain fatty acids in MPTP induced mice model of Parkinson's disease. Exp Gerontol 111376 [DOI] [PubMed]
- Huang C, Ma W, Luo Q, Shi L, Xia Y, Lao C, et al. Iron overload resulting from the chronic oral administration of ferric citrate induces parkinsonism phenotypes in middle-aged mice. Aging (albany NY) 2019;11(21):9846–9861. doi: 10.18632/aging.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson BD, Christiansen E, Murdoch H, Jenkins L, Hansen AH, Madsen O, et al. Complex pharmacology of novel allosteric free fatty acid 3 receptor ligands. Mol Pharmacol. 2014;86(2):200–210. doi: 10.1124/mol.114.093294. [DOI] [PubMed] [Google Scholar]
- Hurley LL, Tizabi Y. Neuroinflammation, neurodegeneration, and depression. Neurotox Res. 2013;23(2):131–144. doi: 10.1007/s12640-012-9348-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad E, Aasly JO. Clinical and imaging markers of prodromal Parkinson's disease. Front Neurol. 2020;11:395. doi: 10.3389/fneur.2020.00395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indrieri A, Pizzarelli R, Franco B, De Leonibus E. Dopamine, alpha-synuclein, and mitochondrial dysfunctions in parkinsonian eyes. Front Neurosci. 2020;14:567129. doi: 10.3389/fnins.2020.567129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivleva I, Pestereva N, Zubov A, Karpenko M. Intranasal exposure of manganese induces neuroinflammation and disrupts dopamine metabolism in the striatum and hippocampus. Neurosci Lett. 2020;738:135344. doi: 10.1016/j.neulet.2020.135344. [DOI] [PubMed] [Google Scholar]
- Kaji I, Akiba Y, Furuyama T, Adelson DW, Iwamoto K, et al. Free fatty acid receptor 3 activation suppresses neurogenic motility in rat proximal colon. Neurogastroenterol Motil. 2018;30(1):10. doi: 10.1111/nmo.13157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalamida D, Poulas K, Avramopoulou V, Fostieri E, Lagoumintzis G, Lazaridis K et al (2007) Muscle and neuronal nicotinic acetylcholine receptors. Structure, function and pathogenicity. FEBS J 274(15):3799–3845 [DOI] [PubMed]
- Kelly JR, Minuto C, Cryan JF, Clarke G, Dinan TG. The role of the gut microbiome in the development of schizophrenia. Schizophr Res. 2020;S0920–9964(20):30086–30094. doi: 10.1016/j.schres.2020.02.010. [DOI] [PubMed] [Google Scholar]
- Keshavarzian A, Green SJ, Engen PA, Voigt RM, Naqib A, Forsyth CB, et al. Colonic bacterial composition in Parkinson's disease. Mov Disord. 2015;30:1351–1360. doi: 10.1002/mds.26307. [DOI] [PubMed] [Google Scholar]
- Klein C, Westenberger A. Genetics of Parkinson’s disease. Cold Spring Harb Perspect Med. 2012;2(1):a008888. doi: 10.1101/cshperspect.a008888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koukouli F, Changeux JP. Do nicotinic receptors modulate high-order cognitive processing? Trends Neurosci. 2020;S0166–2236(20):30125–30129. doi: 10.1016/j.tins.2020.06.001. [DOI] [PubMed] [Google Scholar]
- Kouli A, Torsney K M, Kuan WL (2018) Parkinson’s disease: etiology, neuropathology, and pathogenesis. In: Stoker TB, Greenland JC, editors. Parkinson’s Disease: Pathogenesis and Clinical Aspects [Internet]. Brisbane (AU): Codon Publications, Chapter 1 [PubMed]
- Koutzoumis DN, Vergara M, Pino J, Buddendorff J, Khoshbouei H, Mandel RJ, et al. Alterations of the gut microbiota with antibiotics protects dopamine neuron loss and improve motor deficits in a pharmacological rodent model of Parkinson's disease. Exp Neurol. 2020;325:113159. doi: 10.1016/j.expneurol.2019.113159. [DOI] [PubMed] [Google Scholar]
- Langston JW, Ballard P, Tetrud JW, Irwin I. Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science. 1983;219(4587):979–980. doi: 10.1126/science.6823561. [DOI] [PubMed] [Google Scholar]
- Lees AJ, Hardy J, Revesz T. Parkinson’s disease. Lancet. 2009;373(9680):2055–2066. doi: 10.1016/S0140-6736(09)60492-X. [DOI] [PubMed] [Google Scholar]
- Lemay S, Chouinard S, Blanchet P, Masson H, Soland V, Beuter A, et al. Lack of efficacy of a nicotine transdermal treatment on motor and cognitive deficits in Parkinson’s disease. Prog Neuropsychopharm Biol Psychiatry. 2004;28:31–39. doi: 10.1016/S0278-5846(03)00172-6. [DOI] [PubMed] [Google Scholar]
- Li X, Shen L, Hua T, Liu ZJ. Structural and functional insights into cannabinoid receptors. Trends Pharmacol Sci. 2020;41(9):665–677. doi: 10.1016/j.tips.2020.06.010. [DOI] [PubMed] [Google Scholar]
- Li D, Croft DP, Ossip DJ, Xie Z. The association between statewide vaping prevalence and COVID-19. Prev Med Rep. 2020;20:101254. doi: 10.1016/j.pmedr.2020.101254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Li W, Liu G, Shen X, Tang Y. Association between cigarette smoking and Parkinson’s disease: a meta-analysis. Arch Gerontol Geriatr. 2015;61(3):510–516. doi: 10.1016/j.archger.2015.08.004. [DOI] [PubMed] [Google Scholar]
- Lieberman A, Deep A, Olson MC, Smith Hussain V, Frames CW, McCauley M, et al. Falls when standing, falls when walking: different mechanisms, different outcomes in Parkinson disease. Cureus. 2019;11(8):e5329. doi: 10.7759/cureus.5329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C. Targeting the cholinergic system in Parkinson's disease. Acta Pharmacol Sin. 2020;41(4):453–463. doi: 10.1038/s41401-020-0380-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Wang F, Liu S, Du J, Hu X, Xiong J, et al. Sodium butyrate exerts protective effect against Parkinson's disease in mice via stimulation of glucagon like peptide-1. J Neurol Sci. 2017;381:176–181. doi: 10.1016/j.jns.2017.08.3235. [DOI] [PubMed] [Google Scholar]
- Liu Z, Roosaar A, Axéll T, Ye W. Tobacco use, oral health, and risk of Parkinson's disease. Am J Epidemiol. 2017;185(7):538–545. doi: 10.1093/aje/kww146. [DOI] [PubMed] [Google Scholar]
- Liu W, Wang B, Xiao Y, Wang D, Chen W (2020) Secondhand smoking and neurological disease: a meta-analysis of cohort studies. Rev Environ Health. Epub ahead of print [DOI] [PubMed]
- Lungba RM, Khan SZA, Ajibawo-Aganbi U, Perez Bastidas MV, Veliginti S, Saleem S, et al. The role of the gut microbiota and the immune system in the development of autism. Cureus. 2020;12(10):e11226. doi: 10.7759/cureus.11226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma C, Molsberry S, Li Y, Schwarzschild M, Ascherio A, Gao X. Dietary nicotine intake and risk of Parkinson disease: a prospective study. Am J Clin Nutr. 2020;112(4):1080–1087. doi: 10.1093/ajcn/nqaa186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiti P, Manna J, Dunbar GL. Current understanding of the molecular mechanisms in Parkinson’s disease: Targets for potential treatments. Transl Neurodegener. 2017;6:28. doi: 10.1186/s40035-017-0099-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maruyama W, Yi H, Takahashi T, Shimazu S, Ohde H, Yoneda F, et al. Neuroprotective function of R-(−)-1-(benzofuran-2-yl)-2-propylaminopentane, [R-(−)-BPAP], against apoptosis induced by N-methyl(R)salsolinol, an endogenous dopaminergic neurotoxin, in human dopaminergic neuroblastoma SH-SY5Y cells. Life Sci. 2004;75:107–117. doi: 10.1016/j.lfs.2003.12.001. [DOI] [PubMed] [Google Scholar]
- McKnight S, Hack N. Toxin-induced parkinsonism. Neurol Clin. 2020;38(4):853–865. doi: 10.1016/j.ncl.2020.08.003. [DOI] [PubMed] [Google Scholar]
- Meng L, YuanX, Xuebing Cao X, Zhang Z (2019) The gut-brain axis in the pathogenesis of Parkinson’s disease. Brain Sci Adv 5(2):73–81
- Mirelman A, Bonato P, Camicioli R, Ellis TD, Giladi N, Hamilton JL, et al. Gait impairments in Parkinson's disease. Lancet Neurol. 2019;18(7):697–708. doi: 10.1016/S1474-4422(19)30044-4. [DOI] [PubMed] [Google Scholar]
- Mitra S, Khatri SN, Maulik M, Bult-Ito A, Schulte M. Allosterism of nicotinic acetylcholine receptors: therapeutic potential for neuroinflammation underlying brain trauma and degenerative disorders. Int J Mol Sci. 2020;21(14):4918. doi: 10.3390/ijms21144918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mravec B. Salsolinol, a derivate of dopamine, is a possible modulator of catecholaminergic transmission: a review of recent developments. Physiological Research / Academia Scientiarum Bohemoslovaca. 2006;55:353–364. doi: 10.33549/physiolres.930810. [DOI] [PubMed] [Google Scholar]
- Naoi M, Maruyama W, Nagy GM. Dopamine-derived salsolinol derivatives as endogenous monoamine oxidase inhibitors: occurrence, metabolism and function in human brains. Neurotoxicology. 2004;25:193–204. doi: 10.1016/S0161-813X(03)00099-8. [DOI] [PubMed] [Google Scholar]
- Ndayisaba A, Kaindlstorfer C, Wenning GK. Iron in neurodegeneration - cause or consequence? Front Neurosci. 2019;13:180. doi: 10.3389/fnins.2019.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuzum ND, Loughman A, Szymlek-Gay EA, Hendy A, Teo WP, Macpherson H. Gut microbiota differences between healthy older adults and individuals with Parkinson's disease: a systematic review. Neurosci Biobehav Rev. 2020;112:227–241. doi: 10.1016/j.neubiorev.2020.02.003. [DOI] [PubMed] [Google Scholar]
- O'Connor R, van De Wouw M, Moloney GM, Ventura-Silva AP, O'Riordan K, Golubeva AV, et al. Strain differences in behaviour and immunity in aged mice: relevance to autism. Behav Brain Res. 2021;399:113020. doi: 10.1016/j.bbr.2020.113020. [DOI] [PubMed] [Google Scholar]
- O'Reilly EJ, McCullough ML, Chao A, Henley SJ, Calle EE, Thun MJ, et al. Smokeless tobacco use and the risk of Parkinson's disease mortality. Mov Disord. 2005;20(10):1383–1384. doi: 10.1002/mds.20587. [DOI] [PubMed] [Google Scholar]
- Osborn TM, Hallett PJ, Schumacher JM, Isacson O. Advantages and recent developments of autologous cell therapy for Parkinson's disease patients. Front Cell Neurosci. 2020;14:58. doi: 10.3389/fncel.2020.00058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paiva I, Pinho R, Pavlou MA, Hennion M, Wales P, Schütz AL, et al. Sodium butyrate rescues dopaminergic cells from alpha-synuclein-induced transcriptional deregulation and DNA damage. Hum Mol Genet. 2017;26(12):2231–2246. doi: 10.1093/hmg/ddx114. [DOI] [PubMed] [Google Scholar]
- Papke RL, Lindstrom JM. Nicotinic acetylcholine receptors: conventional and unconventional ligands and signaling. Neuropharmacology. 2020;168:108021. doi: 10.1016/j.neuropharm.2020.108021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra I, Martínez I, Ramírez-García G, Tizabi Y, Mendieta L. Differential Effects of LPS and 6-OHDA on microglia's morphology in rats: implications for inflammatory model of Parkinson’s disease. Neurotox Res. 2020;37(1):1–11. doi: 10.1007/s12640-019-00104-z. [DOI] [PubMed] [Google Scholar]
- Pavia CS, Plummer MM. Clinical implications of nicotine as an antimicrobial agent and immune modulator. Biomed Pharmacother. 2020;129:110404. doi: 10.1016/j.biopha.2020.110404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peres TV, Schettinger MR, Chen P, Carvalho F, Avila DS, Bowman AB, et al. Manganese-induced neurotoxicity: a review of its behavioral consequences and neuroprotective strategies. BMC Pharmacol Toxicol. 2016;17(1):57. doi: 10.1186/s40360-016-0099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez XA. Preclinical evidence for a role of the nicotinic cholinergic system in Parkinson’s disease. Neuropsychol Rev. 2015;25(4):371–383. doi: 10.1007/s11065-015-9303-z. [DOI] [PubMed] [Google Scholar]
- Prenger MTM, Madray R, Van Hedger K, Anello M, MacDonald PA (2020) Social symptoms of Parkinson’s disease. Parkinsons Dis 8846544 [DOI] [PMC free article] [PubMed]
- Qiao CM, Sun MF, Jia XB, Li Y, Zhang BP, Zhao LP, et al. Sodium butyrate exacerbates Parkinson’s disease by aggravating neuroinflammation and colonic inflammation in MPTP-induced mice model. Neurochem Res. 2020;45(9):2128–2142. doi: 10.1007/s11064-020-03074-3. [DOI] [PubMed] [Google Scholar]
- Qiao CM, Sun MF, Jia XB, Shi Y, Zhang BP, Zhou ZL, et al. Sodium butyrate causes α-synuclein degradation by an Atg5-dependent and PI3K/Akt/mTOR-related autophagy pathway. Exp Cell Res. 2020;387(1):111772. doi: 10.1016/j.yexcr.2019.111772. [DOI] [PubMed] [Google Scholar]
- Qiu J, Liu R, Ma Y, Li Y, Chen Z, He H, et al. Lipopolysaccharide-induced depression-like behaviors is ameliorated by sodium butyrate via inhibiting neuroinflammation and oxido-nitrosative stress. Pharmacology. 2020;105(9–10):550–560. doi: 10.1159/000505132. [DOI] [PubMed] [Google Scholar]
- Qualls Z, Brown D, Ramlochansingh C, Hurley LL, Tizabi Y. Protective effects of curcumin against rotenone and salsolinol induced toxicity: implications for Parkinson’s disease. Neurotox Res. 2014;25(1):81–89. doi: 10.1007/s12640-013-9433-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quik M, Bordia T, Zhang D, Perez XA. Nicotine and nicotinic receptor drugs: potential for Parkinson’s disease and drug-induced movement disorders. Int Rev Neurobiol. 2015;124:247–271. doi: 10.1016/bs.irn.2015.07.005. [DOI] [PubMed] [Google Scholar]
- Quik M, Boyd JT, Bordia T, Perez X. Potential therapeutic application for nicotinic receptor drugs in movement disorders. Nicotine Tob Res. 2019;21(3):357–369. doi: 10.1093/ntr/nty063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rani L, Mondal AC (2021) Unravelling the role of gut microbiota in Parkinson’s disease progression: Pathogenic and therapeutic implications. Neurosci Res S0168–0102(21):00004–3. Epub ahead of print [DOI] [PubMed]
- Reglodi D, Renaud J, Tamas A, Tizabi Y, Socías SB, Del-Bel E, et al. Novel tactics for neuroprotection in Parkinson's disease: role of antibiotics, polyphenols and neuropeptides. Prog Neurobiol. 2017;155:120–148. doi: 10.1016/j.pneurobio.2015.10.004. [DOI] [PubMed] [Google Scholar]
- Ritz B, Ascherio A, Checkoway H, Marder KS, Nelson LM, Rocca WA, et al. Pooled analysis of tobacco use and risk of Parkinson disease. Arch Neurol. 2007;64(7):990–997. doi: 10.1001/archneur.64.7.990. [DOI] [PubMed] [Google Scholar]
- Russo R, Cristiano C, Avagliano C, De Caro C, La Rana G, Raso GM, et al. Gut-brain axis: role of lipids in the regulation of inflammation, pain and CNS diseases. Curr Med Chem. 2018;25(32):3930–3952. doi: 10.2174/0929867324666170216113756. [DOI] [PubMed] [Google Scholar]
- Ruszkiewicz JA, Zhang Z, Gonçalves FM, Tizabi Y, Zelikoff JT, Aschner M. Neurotoxicity of e-cigarettes. Food Chem Toxicol. 2020;38:111245. doi: 10.1016/j.fct.2020.111245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan RE, Ross SA, Drago J, Loiacono RE. Dose-related neuroprotective effects of chronic nicotine in 6-hydroxydopamine treated rats, and loss of neuroprotection in alpha4 nicotinic receptor subunit knockout mice. Br J Pharmacol. 2001;132(8):1650–1656. doi: 10.1038/sj.bjp.0703989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Said H, Akiba Y, Narimatsu K, Maruta K, Kuri A, Iwamoto KI, et al. FFA3 activation stimulates duodenal bicarbonate secretion and prevents NSAID-induced enteropathy via the GLP-2 pathway in rats. Dig Dis Sci. 2017;62(8):1944–1952. doi: 10.1007/s10620-017-4600-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampathkumar SG, Jones MB, Meledeo MA, Campbell CT, Choi SS, Hida K, et al. Targeting glycosylation pathways and the cell cycle: sugar-dependent activity of butyrate-carbohydrate cancer prodrugs. Chem Biol. 2006;13(12):1265–1275. doi: 10.1016/j.chembiol.2006.09.016. [DOI] [PubMed] [Google Scholar]
- Sampson TR, Debelius JW, Thron T, Janssen S, Shastri GG, Ilhan ZE, Challis C, et al. Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson’s disease. Cell. 2016;167(1469–80):e12. doi: 10.1016/j.cell.2016.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarduzio M, Zimmerman CN, Jaunarajs KL, Wang Q, Standaert DG, McMahon LL. Strength of cholinergic tone dictates the polarity of dopamine D2 receptor modulation of striatal cholinergic interneuron excitability in DYT1 dystonia. Exp Neurol. 2017;295:162–175. doi: 10.1016/j.expneurol.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider JS, Marshall CA, Keibel L, Snyder NW, Hill MP, Brotchie JM, et al. A novel dopamine D3R agonist SK609 with norepinephrine transporter inhibition promotes improvement in cognitive task performance in rodent and non-human primate models of Parkinson's disease. Exp Neurol. 2021;335:113514. doi: 10.1016/j.expneurol.2020.113514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholz J, Klingemann I, Moser A. Increased systemic levels of norsalsolinol derivatives are induced by levodopa treatment and do not represent biological markers of Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2004;75(4):634–636. doi: 10.1136/jnnp.2003.010769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Searles Nielsen S, Gallagher LG, Lundin JI, Longstreth WT, Jr, Smith-Weller T, Franklin GM, et al. Environmental tobacco smoke and Parkinson’s disease. Mov Disord. 2012;27(2):293–296. doi: 10.1002/mds.24012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seoane-Collazo P, Diéguez C, Nogueiras R, Rahmouni K, Fernández-Real JM, López M. Nicotine’s actions on energy balance: Friend or foe? Pharmacol Ther. 2021;219:107693. doi: 10.1016/j.pharmthera.2020.107693. [DOI] [PubMed] [Google Scholar]
- Sharma S, Moon CS, Khogali A, Haidous A, Chabenne A, Ojo C, et al. Biomarkers in Parkinson’s disease (recent update) Neurochem Int. 2013;63(3):201–229. doi: 10.1016/j.neuint.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Shi L, Huang C, Luo Q, Xia Y, Liu W, Zeng W, et al. Clioquinol improves motor and non-motor deficits in MPTP-induced monkey model of Parkinson’s disease through AKT/mTOR pathway. Aging (albany NY) 2020;12(10):9515–9533. doi: 10.18632/aging.103225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L, Huang C, Luo Q, Rogers E, Xia Y, Liu W, et al. The association of iron and the pathologies of Parkinson's diseases in MPTP/MPP+-induced neuronal degeneration in non-human primates and in cell culture. Front Aging Neurosci. 2019;11:215. doi: 10.3389/fnagi.2019.00215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimohama S, Kawamata J (2018) Roles of nicotinic acetylcholine receptors in the pathology and treatment of Alzheimer’s and Parkinson’s diseases. 2018 Apr 4 A Akaike S Shimohama Y Misu Eds Nicotinic Acetylcholine Receptor Signaling in Neuroprotection [Internet] Springer Singapore [PubMed]
- Shin C, Lim Y, Lim H, Ahn TB. Plasma short-chain fatty acids in patients with Parkinson’s disease. Mov Disord. 2020;35(6):1021–1027. doi: 10.1002/mds.28016. [DOI] [PubMed] [Google Scholar]
- Simon DK, Tanner CM, Brundin P. Parkinson disease epidemiology, pathology, genetics, and pathophysiology. Clin Geriatr Med. 2020;36(1):1–12. doi: 10.1016/j.cger.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y, Wang ZY, Jin YY, Guo J. Association between dopamine receptor D2 TaqIA polymorphism and Parkinson disease risk: a meta-analysis. Int J Clin Exp Pathol. 2019;12(9):3165–3170. [PMC free article] [PubMed] [Google Scholar]
- Srivastav S, Neupane S, Bhurtel S, Katila N, Maharjan S, Choi H, et al. Probiotics mixture increases butyrate, and subsequently rescues the nigral dopaminergic neurons from MPTP and rotenone-induced neurotoxicity. J Nutr Biochem. 2019;69:73–86. doi: 10.1016/j.jnutbio.2019.03.021. [DOI] [PubMed] [Google Scholar]
- St Laurent R, O'Brien LM, Ahmad ST (2013) Sodium butyrate improves locomotor impairment and early mortality in a rotenone-induced Drosophila model of Parkinson's disease. Neuroscience 246:382-90 Stoker TB, Barker RA (2020) Recent developments in the treatment of Parkinson’s disease. F1000Research 9:862 [DOI] [PMC free article] [PubMed]
- Stoker TB, Torsney KM, Barker RA. Emerging treatment approaches for Parkinson’s disease. Front Neurosci. 2018;12:693. doi: 10.3389/fnins.2018.00693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolerman IP, Jarvis MJ (1995) The scientific case that nicotine is addictive. Psychopharmacology (Berl). 117(1):2–10; discussion 14–20 [DOI] [PubMed]
- Storch A, Ott S, Hwang YI, Ortmann R, Hein A, Frenzel S, et al. Selective dopaminergic neurotoxicity of isoquinoline derivatives related to Parkinson’s disease: studies using heterologous expression systems of the dopamine transporter. Biochem Pharmacol. 2002;63:909–920. doi: 10.1016/s0006-2952(01)00922-4. [DOI] [PubMed] [Google Scholar]
- Sui Y, Tian Y, Ko WKD, Wang Z, Jia F, Horn A, et al. Deep brain stimulation initiative: toward innovative technology, new disease indications, and approaches to current and future clinical challenges in neuromodulation therapy. Front Neurol. 2021;11:597451. doi: 10.3389/fneur.2020.597451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sy MAC, Fernandez HH. Pharmacological treatment of early motor manifestations of Parkinson disease (PD) Neurotherapeutics. 2020;17(4):1331–1338. doi: 10.1007/s13311-020-00924-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szentirmai É, Millican NS, Massie AR, Kapás L. Butyrate, a metabolite of intestinal bacteria, enhances sleep. Sci Rep. 2019;9:7035. doi: 10.1038/s41598-019-43502-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao Y, Vermilyea SC, Zammit M, Lu J, Olsen M, Metzger JM, et al. Autologous transplant therapy alleviates motor and depressive behaviors in parkinsonian monkeys. Nat Med. 2021;27(4):632–639. doi: 10.1038/s41591-021-01257-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tikhonova IG. Application of GPCR structures for modelling of free fatty acid receptors. Handb Exp Pharmacol. 2017;236:57–77. doi: 10.1007/164_2016_52. [DOI] [PubMed] [Google Scholar]
- Terry AV Jr, Callahan PM (2020) α7 nicotinic acetylcholine receptors as therapeutic targets in schizophrenia: Update on animal and clinical studies and strategies for the future. Neuropharmacology 170:108053 [DOI] [PMC free article] [PubMed]
- Tizabi Y. Duality of antidepressants and neuroprotectants. Neurotox Res. 2016;30(1):1–13. doi: 10.1007/s12640-015-9577-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tizabi Y, Getachew B. Nicotinic receptor intervention in Parkinson’s disease: future directions. Cin Pharm Transl Med. 2017;1:1–7. [PMC free article] [PubMed] [Google Scholar]
- Tizabi Y, Getachew B, Csoka AB, Manaye KF, Copeland RL. Novel targets for parkinsonism-depression comorbidity. Prog Mol Biol Transl Sci. 2019;167:1–24. doi: 10.1016/bs.pmbts.2019.06.004. [DOI] [PubMed] [Google Scholar]
- Tizabi Y, Getachew B, Copeland RL, Aschner M. Nicotine and the nicotinic cholinergic system in COVID-19. FEBS j. 2020;287(17):3656–3663. doi: 10.1111/febs.15521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran J, Anastacio H, Bardy C (2020) Genetic predispositions of Parkinson’s disease revealed in patient-derived brain cells. npj Parkinsons Dis. 6:8 [DOI] [PMC free article] [PubMed]
- Unger MM, Spiegel J, Unger MM, Spiegel J, Dillmann KU, Grundmann D, et al. Short chain fatty acids and gut microbiota differ between patients with Parkinson's disease and age-matched controls. Parkinsonism Relat Disord. 2016;32:66–72. doi: 10.1016/j.parkreldis.2016.08.019. [DOI] [PubMed] [Google Scholar]
- Valentine G, Sofuoglu M. Cognitive effects of nicotine: recent progress. Curr Neuropharmacol. 2018;16(4):403–414. doi: 10.2174/1570159X15666171103152136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valvassori SS, Varela RB, Arent CO, Dal-Pont GC, Bobsin TS, Budni J, et al. Sodium butyrate functions as an antidepressant and improves cognition with enhanced neurotrophic expression in models of maternal deprivation and chronic mild stress. Curr Neurovasc Res. 2014;11(4):359–366. doi: 10.2174/1567202611666140829162158. [DOI] [PubMed] [Google Scholar]
- Vega JN, Albert KM, Mayer IA, Taylor WD, Newhouse PA. Nicotinic treatment of post-chemotherapy subjective cognitive impairment: a pilot study. J Cancer Surviv. 2019;13(5):673–686. doi: 10.1007/s11764-019-00786-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vetel S, Foucault-Fruchard L, Tronel C, Buron F, Vergote J, Bodard S, et al. Neuroprotective and anti-inflammatory effects of a therapy combining agonists of nicotinic α7 and σ1 receptors in a rat model of Parkinson's disease. Neural Regen Res. 2021;16:1099–1104. doi: 10.4103/1673-5374.300451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieregge A, Sieberer M, Jacobs H, Hagenah JM, Vieregge P. Transdermal nicotine in PD: a randomized, double-blind, placebo-controlled study. Neurol. 2001;57:1032–1035. doi: 10.1212/wnl.57.6.1032. [DOI] [PubMed] [Google Scholar]
- Villageliú DN, Borts DJ, Lyte M. Production of the neurotoxin salsolinol by a gut-associated bacterium and its modulation by alcohol. Front Microbiol. 2018;9:3092. doi: 10.3389/fmicb.2018.03092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voon SM, Ng KY, Chye SM, Ling APK, Voon KGL, Yap YJ, et al. The mechanism of action of salsolinol in brain: implications in Parkinson’s disease. CNS Neurol Disord Drug Targets. 2020;19(10):725–740. doi: 10.2174/1871527319666200902134129. [DOI] [PubMed] [Google Scholar]
- Wills L, Kenny PJ (2021) Addiction-related neuroadaptations following chronic nicotine exposure. J Neurochem. 10.1111/jnc.15356. Epub ahead of print. PMID: 33742685 [DOI] [PubMed]
- Witt O, Monkemeyer S, Rönndahl G, Erdlenbruch B, Reinhardt D, Kanbach K, et al. Induction of fetal hemoglobin expression by the histone deacetylase inhibitor apicidin. Blood. 2003;101(5):2001–2007. doi: 10.1182/blood-2002-08-2617. [DOI] [PubMed] [Google Scholar]
- Wittenberg RE, Wolfman SL, De Biasi M, Dani JA. Nicotinic acetylcholine receptors and nicotine addiction: A brief introduction. Neuropharmacology. 2020;177:108256. doi: 10.1016/j.neuropharm.2020.108256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xicoy H, Wieringa B, Martens GJ. The SH-SY5Y cell line in Parkinson’s disease research: a systematic review. Mol Neurodegener. 2017;12(1):10. doi: 10.1186/s13024-017-0149-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Pedersen NL, Ye W, Liu Z, Norberg M, Forsgren L, et al. Moist smokeless tobacco (Snus) use and risk of Parkinson’s disease. Int J Epidemiol. 2017;46:872–880. doi: 10.1093/ije/dyw294. [DOI] [PubMed] [Google Scholar]
- Yoo CB, Jones PA. Epigenetic therapy of cancer: past, present and future. Nat Rev Drug Discov. 2006;5(1):37–50. doi: 10.1038/nrd1930. [DOI] [PubMed] [Google Scholar]
- Zeng XS, Geng WS, Jia JJ, Chen L, Zhang PP (2018) Cellular and molecular basis of neurodegeneration in parkinson disease. Front Aging Neurosci 10:109 [DOI] [PMC free article] [PubMed]
- Zheng X, Chen X, Guo M, Ali S, Huang Y, Sun F, et al. Changes in salsolinol production and salsolinol synthase activity in Parkinson's disease model. Neurosci Lett. 2018;673:39–43. doi: 10.1016/j.neulet.2018.02.024. [DOI] [PubMed] [Google Scholar]
- Zheng M, Chen M, Liu C, Fan Y, Shi D. Alkaloids extracted from Uncaria rhynchophylla demonstrate neuroprotective effects in MPTP-induced experimental parkinsonism by regulating the PI3K/Akt/mTOR signaling pathway. J Ethnopharmacol. 2021;266:113451. doi: 10.1016/j.jep.2020.113451. [DOI] [PubMed] [Google Scholar]