Abstract
Background
Some people with multiple sclerosis (pwMS) are at increased risk of severe Coronavirus disease 19 (COVID-19) and should be rapidly vaccinated. However, vaccine supplies are limited, and there are concerns about side-effects, particularly with the ChAdOx1nCoV-19 (AstraZeneca) vaccine.
Objectives
To report our first experience of pwMS receiving the AstraZeneca vaccine.
Methods
Service evaluation. pwMS using the MS service at Barts Health NHS Trust were sent questionnaires to report symptoms following vaccination.
Results
Thirty-three responses were returned, 29/33 pwMS received a first dose of AstraZeneca vaccine, the remaining four received a first dose of BioNTech/Pfizer vaccine.
All but two patients (94%) reported any symptoms including a sore arm (70%), flu-like symptoms (64%), fever (21%), fatigue (27%), and headache (21%). In more than 2/3 patients, symptoms lasted up to 48 hours, and with the exception of two pwMS reporting symptom duration of 10 and 12 days, respectively, symptoms in the remainder resolved within seven days. No severe adverse effects occurred.
Conclusions
pwMS report transient symptoms following AstraZeneca vaccination, characteristics of which were similar to those reported in the non-MS population. Symptoms may be more pronounced in pwMS due to the temperature-dependent delay in impulse propagation (Uhthoff's phenomenon) due to demyelination.
Keywords: SARS-CoV2, COVID-19, Vaccination, Multiple sclerosis
Introduction
By the end of April 2021, coronavirus disease 19 (COVID-19) will have killed more than three million people across the Globe. People with disabilities, including those with multiple sclerosis (MS), are at increased risk of severe COVID-19 and death (Salter et al., 2021). Treatment with disease-modifying immunotherapy (DMT) may put them at yet higher risk (Baker et al., 2020).
The rapid rollout of COVID-19 vaccinations is a key element of public health strategies to reduce the severity of the disease and suppress the spread of infection (Altmann et al., 2020). However, concerns about side-effects, particularly AstraZeneca's viral vector vaccine (Greinacher et al., 2021) have led to public uncertainty and regulatory suspensions. Whilst people with MS (pwMS) appear generally not at excess risk from vaccinations (Reyes et al., 2020), the response to SARS-CoV2 immunization remains unknown, notably in those on DMT.
Our institution (Barts Health NHS Trust) has been heavily involved in the management of people with COVID-19 and research into treatments (Wilkinson, 2020) and vaccines. From January 2021, Barts Health's MS service (BartsMS) fast-tracked pwMS for early vaccination. The majority of pwMS vaccinated through BartsMS received the AstraZeneca vaccine. As part of this rapid access scheme, we asked pwMS to report on their vaccination experience.
Methods
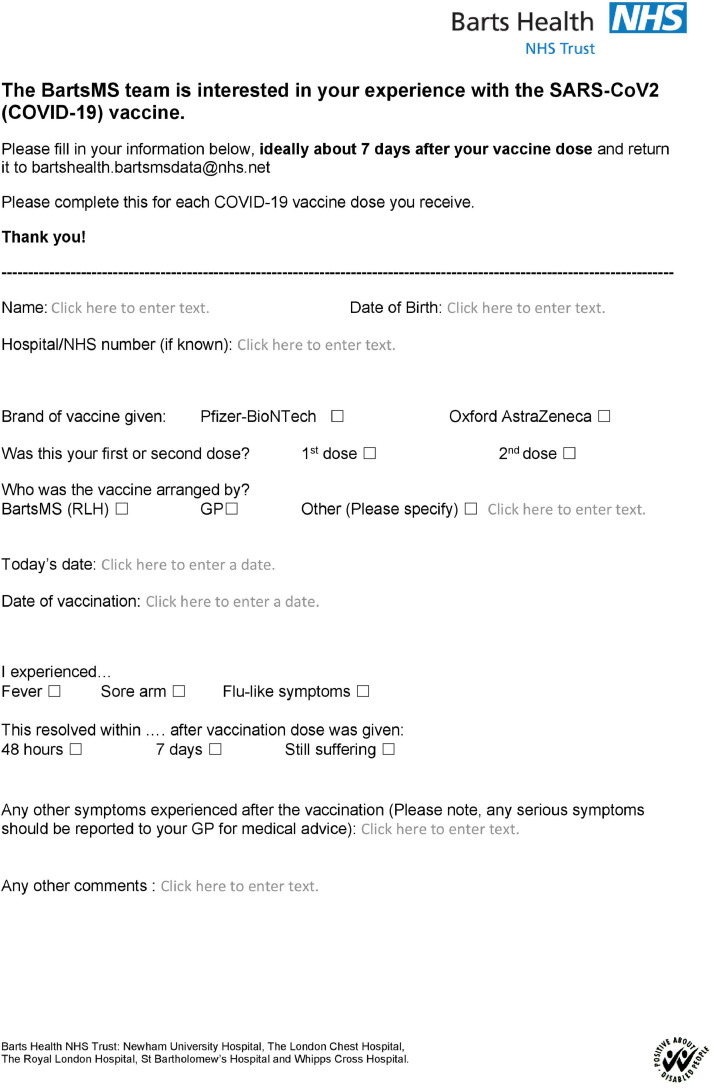
Between 25 January and 24 March 2021 BartsMS contacted their first 570 pwMS to offer vaccination slots and sent each patient a brief questionnaire (figure 1 ) they were asked to fill in approximately seven days after their first vaccine dose and then return via email. This service evaluation is registered with our Clinical Effectiveness Unit (#12011).
Fig. 1.
The questionnaire people with multiple sclerosis were asked to fill in.
Results
At the cut-off 33 pwMS had returned completed questionnaires. Twenty-nine received the AstraZeneca and four the BioNTech/Pfizer vaccine. Mean age was 50 years (range 25-76; standard deviation 13 years), 19 were female and 14 male. Mean disease duration was 15 years (range 2-38; SD 10), and median EDSS 4.0 (range 0-8.0). Nineteen patients had relapsing, five primary and nine secondary progressive MS. Fifteen pwMS were on DMT with ocrelizumab (last infusion 3-15 months ago). Eight patients had been treated with cladribine 3-23 months prior to vaccination. One patient each received natalizumab or ofatumumab one and two weeks, respectively, before vaccination. One pwMS received rituximab six months prior to vaccination. Two pwMS were on dimethyl-fumarate; five were not on DMT.
All but two patients (94%) reported any symptoms. Among symptoms we specifically inquired about, the following were reported: Sore arm (70%), flu-like symptoms (64%), fever (21%).
In a free text field, the following were described: fatigue (27%), headache (21%), fever/chills (12%), joint pain/muscle ache (9%), nausea (9%), swelling at injection site (6%). One patient each described worsening neurological symptoms, disturbed sleep, facial numbness, urinary tract infection, odd smell/lack of taste, and oral cold sore. In more than 2/3 patients, symptoms did not last longer than 48 hours, and with the exception of one sore arm lasting 10, and one swelling at the injection site lasting 12 days, symptoms in the remaining pwMS resolved within seven days.
Discussion
To the best of our knowledge, we report the first experience with the AstraZeneca vaccine in pwMS. Given the controversy surrounding this particular vaccine, our results, albeit preliminary, seem reassuring in that adverse events were consistent with those experienced in the general population. Whilst symptoms were unpleasant, affecting all but two pwMS in this small cohort, they resolved in the majority within a couple of days. By day 7, only a small proportion remained symptomatic. Symptoms themselves were commensurate with expectation from both the normal population, and from experience of pwMS with other vaccinations (Reyes et al., 2020).
Since only four pwMS in our cohort received the BNT162b2 vaccine, no dependable comparisons with the Astra Zeneca vaccine are possible. However, the frequency and characteristics of adverse events with the BNT162b1/BNT162b2 vaccines during the phase 1 trial in the United States resemble those reported in our cohort (Walsh et al., 2020). The majority of symptoms resolved within seven days of vaccine administration matching the experience in our small cohort. Recently, a significantly lower frequency of adverse events has been reported with the BNT162b2 vaccine in pwMS (Achiron et al., 2021). Whilst data in that study were collected during consultations in clinic, we relied on the return of multiple-choice questionnaires, which inevitably affects the denominator since patients having an adverse experience are more likely to voice their grievances and, thus, return their questionnaire, than people without, or only minor, side effects.
Although Uhthoff's phenomenon refers more broadly to exacerbation of symptoms due to demyelination when exposed to excess internal or external heat, it was probably first described in 1927 in the context of immunization. It is thought to result from changes in axonal membrane potentials leading to prolonged inactivation of sodium channels and impulse propagation failure in demyelinated axons (Coates et al., 2015). Particularly in pwMS with long disease duration, Uhthoff's phenomenon can lead to significant, however transient, deterioration. We did not observe any lasting neurological sequelae or MS relapse. We will continue to collect questionnaires, also covering the second vaccination dose. A larger number of pwMS will provide granularity about potential variations in in vaccine response based on the type of DMT, and serological responses to vaccination.
Notwithstanding recent reports about thrombotic thrombocytopenia following vaccination with the AstraZeneca (Greinacher et al., 2021) and other viral vector vaccine(s) against SARS-CoV2 (Muir et al., 2021), and the resulting need to observe respective regulatory restrictions and local guidelines, our preliminary experience suggests SARS-CoV2 vaccination is a relatively safe intervention that should be encouraged to protect pwMS and to bring the pandemic under control.
Declaration of Competing Interest
KAP, AS, TB and ACJ have nothing to disclose. RD has received research support from Biogen, Merck, and Celgene, and honoraria/meeting support from Biogen, Merck, Roche, Sanofi-Genzyme, and Teva. GG has received honoraria and meeting support from AbbVie Biotherapeutics, Biogen, Canbex, Ironwood, Novartis, MSD, Merck Serono, Roche, Sanofi Genzyme, Synthon, Teva and Vertex. He also serves as chief editor for Multiple Sclerosis and Related Disorders and is the academic director of the Neurology Academy. SG has received honoraria from Biogen Idec, Sanofi Genzyme, Janssen Cilag, Merck, Neurodiem, Novartis, Roche, and Teva and grant support from ECTRIMS, Genzyme, Merck, National MS Society, Takeda and UK MS Society. MM has received honoraria and travel costs from Genzyme, AbbVie, Roche and Novartis. IS was funded by an ECTRIMS clinical fellowship grant in 2019 and has received honoraria from Biogen Idec, Neurodiem and Merck. BT has received honoraria, travel grants, and been a member of advisory boards for Biogen, Merck Serono, Novartis, Sanofi Genzyme and Roche. DB has received compensation from InMuneBio, Lundbeck, Merck, Novartis, Rock and Teva. JM has received honoraria and meeting support from Arvelle, Biogen, Novartis, Merck Serono, Roche and Sanofi Genzyme. KS has received research support from Biogen, Merck KGaA, and Novartis, speaking honoraria from, and/or served in an advisory role for, Amgen, Biogen, EMD Serono, Merck KGaA, Novartis, Roche, Sanofi-Genzyme, and Teva; and remuneration for teaching activities from AcadeMe, Medscape and the Neurology Academy.
Funding
None.
References
- Salter A, Fox RJ, Newsome SD, et al. Outcomes and Risk Factors Associated With SARS-CoV-2 Infection in a North American Registry of Patients With Multiple Sclerosis. JAMA Neurol. 2021 doi: 10.1001/jamaneurol.2021.0688. Available at. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker D, Roberts CA, Pryce G, et al. COVID-19 vaccine-readiness for anti-CD20-depleting therapy in autoimmune diseases. Clinical & Experimental Immunology. 2020;202(2):149–161. doi: 10.1111/cei.13495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altmann DM, Douek DC, Boyton RJ. What policy makers need to know about COVID-19 protective immunity. Lancet. 2020;395(10236):1527–1529. doi: 10.1016/S0140-6736(20)30985-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination. N. Engl. J. Med. 2021 doi: 10.1056/NEJMoa2104840. Apr 9Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes S, Ramsay M, Ladhani S, et al. Protecting people with multiple sclerosis through vaccination. Pract. Neurol. 2020;20(6):435–445. doi: 10.1136/practneurol-2020-002527. [DOI] [PubMed] [Google Scholar]
- Wilkinson E. RECOVERY trial: the UK covid-19 study resetting expectations for clinical trials. BMJ. 2020;369:m1626. doi: 10.1136/bmj.m1626. [DOI] [PubMed] [Google Scholar]
- Walsh EE, Frenck RW, Jr., Falsey AR, et al. Safety and Immunogenicity of Two RNA-Based Covid-19 Vaccine Candidates. N. Engl. J. Med. 2020;383:2439–2450. doi: 10.1056/NEJMoa2027906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achiron A, Dolev M, Menascu S, et al. COVID-19 vaccination in patients with multiple sclerosis: What we have learnt by February 2021. Mult Scler. 2021 doi: 10.1177/13524585211003476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coates TA, Woolnough O, Masters JM, et al. Acute temperature sensitivity in optic nerve axons explained by an electrogenic membrane potential. Pflugers Arch. 2015;467(11):2337–2349. doi: 10.1007/s00424-015-1696-2. [DOI] [PubMed] [Google Scholar]
- Muir K-L, Kallam A, Koepsell SA, et al. Thrombotic Thrombocytopenia after Ad26.COV2.S Vaccination. N. Engl. J. Med. 2021 doi: 10.1056/NEJMc2105869. [DOI] [PMC free article] [PubMed] [Google Scholar]