Abstract
The effects of psychotherapies for depression have been examined in several hundreds of randomized trials, but no recent network meta‐analysis (NMA) has integrated the results of these studies. We conducted an NMA of trials comparing cognitive behavioural, interpersonal, psychodynamic, problem‐solving, behavioural activation, life‐review and “third wave” therapies and non‐directive supportive counseling with each other and with care‐as‐usual, waiting list and pill placebo control conditions. Response (50% reduction in symptoms) was the primary outcome, but we also assessed remission, standardized mean difference, and acceptability (all‐cause dropout rate). Random‐effects pairwise and network meta‐analyses were conducted on 331 randomized trials with 34,285 patients. All therapies were more efficacious than care‐as‐usual and waiting list control conditions, and all therapies – except non‐directive supportive counseling and psychodynamic therapy – were more efficacious than pill placebo. Standardized mean differences compared with care‐as‐usual ranged from –0.81 for life‐review therapy to –0.32 for non‐directive supportive counseling. Individual psychotherapies did not differ significantly from each other, with the only exception of non‐directive supportive counseling, which was less efficacious than all other therapies. The results were similar when only studies with low risk of bias were included. Most therapies still had significant effects at 12‐month follow‐up compared to care‐as‐usual, and problem‐solving therapy was found to have a somewhat higher long‐term efficacy than some other therapies. No consistent differences in acceptability were found. Our conclusion is that the most important types of psychotherapy are efficacious and acceptable in the acute treatment of adult depression, with few significant differences between them. Patient preference and availability of each treatment type may play a larger role in the choice between types of psychotherapy, although it is possible that a more detailed characterization of patients with a diagnosis of depression may lead to a more precise matching between individual patients and individual psychotherapies.
Keywords: Depression, psychotherapy, network meta‐analysis, cognitive behavioural therapy, behavioural activation therapy, problem‐solving therapy, interpersonal psychotherapy, psychodynamic therapy, life‐review therapy, “third wave” therapies
Depressive disorders are common 1 , costly2, 3, have a strong impact on quality of life of patients 4 , and are associated with considerable morbidity and mortality 5 . Next to antidepressants, psychotherapies are first‐line treatments for depression, and both treatments are effective6, 7.
Cognitive behavioural therapy (CBT) is the most examined type of psychotherapy for depression 8 , but several other types of psychotherapy have also been tested in multiple trials, including interpersonal, psychodynamic, life‐review, problem‐solving, behavioural activation and “third wave” therapies and non‐directive supportive counseling. For all these therapies, there is evidence of efficacy in comparison with care‐as‐usual and waiting list 9 .
Head‐to‐head comparisons of different types of psychotherapy indicate no significant differences between them 10 . However, these findings should be considered with caution, because more than 70% of trials in this field have considerable risk of bias 9 . Furthermore, almost all comparative outcome trials are heavily underpowered 11 .
Only one network meta‐analysis (NMA) has examined simultaneously the effects of different psychotherapies for depression 7 , confirming the comparable effects of these therapies versus control conditions. However, this previous NMA is outdated (only studies up to 2012 were included, and a considerable number of trials has been conducted since then) and did not examine acceptability of treatments. Also, the number of trials with low risk of bias was small and has substantially increased since then. Long‐term outcomes of psychotherapies have also not yet been examined in an NMA. Furthermore, the methodology of NMAs has been developed considerably in the past few years, with more sophisticated techniques.
We decided, therefore, to conduct a new NMA examining the efficacy and acceptability of the main types of psychotherapy for adult depression compared to care‐as‐usual, waiting list and pill placebo.
METHODS
Identification and selection of studies
The protocol for the current NMA has been registered at the Open Science Foundation (https://osf.io/nxvye). We used a database of studies on psychotherapies for depression 12 which is continuously updated and covered the period from 1966 to January 1, 2020. For this database, we searched four major bibliographic sources (PubMed, PsycINFO, EMBASE and Cochrane Library) by combining terms for depression and psychotherapies, with filters for randomized controlled trials (the full search string in PubMed is provided in the supplementary information). We also checked the references of earlier meta‐analyses.
All records were screened by two independent researchers, and all papers potentially meeting inclusion criteria according to one of the researchers were retrieved as full text. The decision to include or exclude a study in the database was also done by the two independent researchers, and disagreements were solved through discussion.
We included randomized trials in which one of eight major types of psychotherapy for adult depression was compared with another major type of psychotherapy or one of three types of control conditions: waiting list, care‐as‐usual, and pill placebo. The definitions of the eight major types of psychotherapy were developed by experts in the field, based on the critical reading and analysis of therapies described in comparative outcomes trials of psychotherapy for depression 10 .
The therapies that were examined were: CBT, behavioural activation therapy, problem‐solving therapy, “third wave” therapies, interpersonal psychotherapy, psychodynamic therapy, non‐directive supportive counseling, and life‐review therapy. The classification of psychotherapies was made by two independent raters. Any disagreement was resolved through discussion of the two and/or in consultation with the first author. Each of these major types of psychotherapy was examined in at least ten trials comparing the therapy with a control condition.
Depression could be established by a diagnostic interview or by a score above a cutoff on a validated self‐report measure. Studies of comorbid mental or physical disorders were included. Studies on inpatients were excluded 13 , as were maintenance treatment studies. Psychotherapies could be delivered individually, in groups, by telephone, or as guided Internet‐based treatment. Unguided interventions were excluded, because they have been found to be less effective than interventions with human contact between a patient and a therapist 14 .
Quality assessment
We evaluated the included studies using four criteria of the Risk of Bias assessment tool developed by the Cochrane Collaboration 15 : adequate generation of allocation sequence; concealment of allocation to conditions; prevention of knowledge of the allocated intervention (masking of assessors); and dealing with incomplete outcome data. Assessment of risk of bias was conducted by two independent researchers, and disagreements were solved through discussion. A study was rated as low overall risk of bias when all four items were rated as low risk of bias.
Outcome measures
Treatment response, defined as a reduction of at least 50% in depressive symptomatology, was chosen as the primary outcome. When not reported, we imputed response rates using a validated method 16 . Patients randomized but not included in the analyses of responders in the original reports were assumed to be non‐responders and included in the current analyses in order to abide the intention‐to‐treat principle.
The time point for the primary outcome was the end of the psychotherapy. When more than one depression measure was used in a study, we selected one outcome using an algorithm (see supplementary information). When a study included two or more arms of the same type of psychotherapy (e.g., individual and group CBT), the outcome data were pooled so that each study had only one outcome for one type of therapy.
We also calculated remission rates. For the selection of definitions of remission, we used the following hierarchy: a) no diagnosis of major depressive disorder; b) scoring below a specific cutoff score; c) other (e.g., significant change). In addition, we calculated the standardized mean difference (SMD) between conditions for the studies that reported means, standard deviations and number of patients at baseline and post‐test, or the change score between baseline and post‐test. Acceptability of the treatments was operationalized as all‐cause dropout rate.
Pairwise meta‐analyses
We conducted pairwise meta‐analyses for all comparisons, using a random effects model. To quantify heterogeneity, we calculated the I 2 ‐statistic with 95% confidence intervals (CIs) 17 . We tested for small study effects with Egger's test 18 .
Network meta‐analyses
The comparative effectiveness was evaluated using the NMA methodology via combining direct and indirect evidence for all relative treatment effects. First, we summarized the geometry of the network of evidence using network plots 19 . Second, the NMA for assessing the comparative efficacy or acceptability was conducted using contrast‐based methods. Comparative odds ratios (ORs) and SMDs were reported with their 95% CIs. The ranking of treatment formats was estimated according to the “surface under the cumulative ranking” (SUCRA), based on the estimated multivariate random effects models 19 .
The statistical examination of the transitivity assumption was conducted using tests of local and global inconsistency 20 . We also implemented meta‐regression analyses to evaluate the influence of small study effects involving the study‐specific variances as a covariate 21 .
Further, we evaluated the heterogeneity in the network with tau‐squared in comparison with empirically derived evidence22, 23, and conducted a multivariate meta‐regression analysis to examine possible sources of heterogeneity with core characteristics of the studies.
We performed several sensitivity analyses: a) analyses with only studies with low risk of bias; b) analyses excluding life‐review therapy (this is only used in older adults, and may violate the transitivity assumption); and c) analyses in which studies with pill placebo were excluded (because in these studies patients could also be randomized to antidepressant medication, which may violate the transitivity assumption as well).
We assessed the certainty of evidence in network estimates of the main outcome in accordance with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) framework.
The main analyses were conducted in Stata/SE 14.2 for Mac, except the meta‐regression analyses examining small sample bias, which were conducted in OpenBUGS 3.2.3. The GRADE ratings were performed in CINeMA 24 .
RESULTS
Selection and inclusion of studies
After examining 24,647 abstracts (18,217 after removal of duplicates), we retrieved 2,914 full‐text papers, of which 2,583 were excluded. The PRISMA flow chart is presented in Figure 1. A total of 331 randomized controlled trials (with 34,285 patients) met inclusion criteria.
Figure 1.
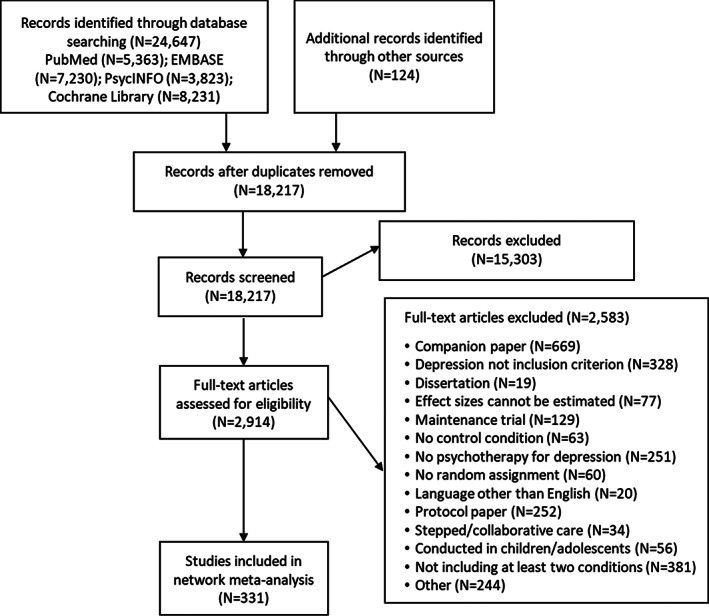
PRISMA flow chart for inclusion of studies
Characteristics and risk of bias of included studies
The aggregated characteristics of the 331 included studies are presented in Table 1. Most studies were aimed at adults in general (145; 43.8%). In 179 studies (54.1%), participants met criteria for a depressive disorder according to a diagnostic interview, while the other studies (152; 45.9%) included participants who scored above a cutoff on a self‐rating depression scale.
Table 1.
Aggregated characteristics of the included studies (N=331)
| N | % | ||
|---|---|---|---|
|
Recruitment |
Community |
148 |
44.7 |
| Clinical | 86 | 26.0 | |
| Other | 97 | 29.3 | |
|
Target group |
Adults in general |
145 |
43.8 |
| Older adults | 14 | 4.2 | |
| Students | 32 | 9.7 | |
| Perinatal depression | 30 | 9.1 | |
| General medical disorder | 67 | 20.2 | |
| Other specific group | 43 | 13.0 | |
| Diagnosis | Depressive disorder | 179 | 54.1 |
| Scoring above cutoff | 152 | 45.9 | |
| Conditions | Cognitive behavioural therapy | 211 | 63.7 |
| Behavioural activation therapy | 36 | 10.9 | |
| Problem‐solving therapy | 33 | 10.0 | |
| “Third wave” therapies | 29 | 8.8 | |
| Interpersonal psychotherapy | 35 | 10.6 | |
| Psychodynamic therapy | 21 | 6.3 | |
| Non‐directive supportive counseling | 42 | 12.7 | |
| Life‐review therapy | 13 | 3.9 | |
| Care‐as‐usual | 158 | 47.7 | |
| Waiting list | 112 | 33.8 | |
| Pill placebo | 10 | 3.0 | |
| Number of conditions per study | Two | 296 | 89.4 |
| Three | 32 | 9.7 | |
| Four | 3 | 0.9 | |
| Format | Individual | 145 | 43.8 |
| Group | 75 | 22.7 | |
| Guided self‐help | 58 | 17.5 | |
| Mixed/other | 53 | 16.0 | |
| Number of sessions | <8 | 114 | 34.4 |
| 8‐12 | 154 | 46.5 | |
| >12 | 63 | 19.0 | |
| Country | North America | 134 | 40.5 |
| Europe | 124 | 37.5 | |
| Australia | 23 | 6.9 | |
| Other | 50 | 15.1 | |
| Risk of bias | Adequate sequence generation | 184 | 55.6 |
| Concealment of allocation to conditions | 157 | 47.4 | |
| Masking of assessors | 105 | 31.7 | |
| Intention‐to‐treat analysis | 209 | 63.1 | |
| Risk of bias total score | Low (4) | 102 | 30.8 |
| Moderate (2 or 3) | 148 | 44.7 | |
| High (0 or 1) | 81 | 24.4 |
CBT was examined in the majority of studies (211 trials; 63.7%), while the other therapies were examined in 13 (3.9%; life‐review) to 42 (12.7%; non‐directive supportive counseling) studies. Care‐as‐usual control condition was used in 158 studies (47.7%), waiting list in 112 studies (33.8%), and pill placebo in 10 studies (3.0%). Most interventions had an individual treatment format (145; 43.8%), 75 used a group format (22.7%), 58 used guided self‐help (17.5%), and 53 used a mixed or another format (16.0%). Most studies were conducted in North America (134; 40.5%) and Europe (124; 37.5%).
A total of 184 studies reported adequate sequence generation (55.6%), 157 reported allocation to conditions by an independent party (47.4%), 105 reported using blinded outcome assessors (31.7%), and 195 used only self‐report outcomes (58.9%). Intent‐to‐treat analyses were conducted in 209 studies (63.1%). The risk of bias was low (total score: 4) in 102 studies (30.8%), moderate (total score: 2 or 3) in 148 studies (44.7%), and high (total score: 0 or 1) in 81 studies (24.4%).
Network plot
The network plot for response (Figure 2) indicated a well‐connected network, with no stand‐alone node. CBT was the best examined therapy and was connected to all other nodes (except life‐review therapy). Non‐directive supportive counseling was also connected to most other nodes. The other therapies were not connected well with each other. All therapies were connected to care‐as‐usual and waiting list, but not to pill placebo.
Figure 2.
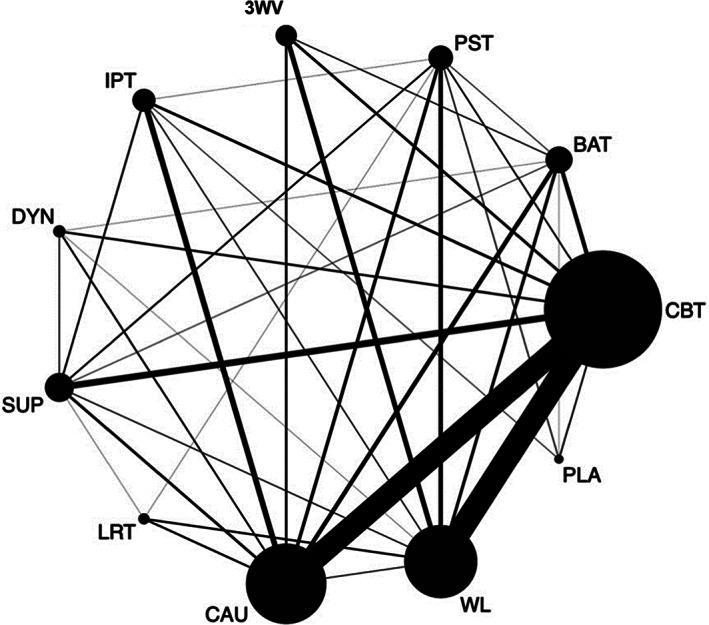
Network plot for response. 3WV – third wave therapies, BAT – behavioural activation therapy, CAU – care‐as‐usual, CBT – cognitive behavioural therapy, DYN – psychodynamic therapy, IPT – interpersonal psychotherapy, LRT – life‐review therapy, PLA – pill placebo, PST – problem‐solving therapy, SUP – non‐directive supportive counseling, WL – waiting list
Pairwise meta‐analyses
In pairwise meta‐analyses (see Table 2), all therapies were more efficacious than care‐as‐usual (except psychodynamic therapy) and waiting list (except non‐directive supportive counseling and psychodynamic therapy). There were no significant differences between therapies, except that non‐directive supportive counseling was less efficacious than CBT, problem‐solving therapy, and psychodynamic therapy.
Table 2.
Pairwise meta‐analyses: efficacy of psychotherapies compared with each other and with control conditions
| N | OR | 95% CI | I2 | ||
|---|---|---|---|---|---|
| CBT | BAT | 12 | 0.97 | 0.74‐1.26 | 0 |
| PST | 4 | 1.00 | 0.61‐1.61 | 23 | |
| 3WV | 8 | 0.96 | 0.67‐1.36 | 0 | |
| IPT | 8 | 0.98 | 0.62‐1.54 | 57 | |
| DYN | 7 | 0.92 | 0.68‐1.23 | 0 | |
| SUP | 20 | 0.74 | 0.58‐0.95 | 15 | |
| CAU | 75 | 0.47 | 0.39‐0.56 | 60 | |
| WL | 77 | 0.25 | 0.20‐0.30 | 43 | |
| PLA | 4 | 0.48 | 0.30‐0.76 | 20 | |
| BAT | PST | 2 | 0.71 | 0.18‐2.87 | 43 |
| 3WV | 3 | 0.85 | 0.43‐1.68 | 0 | |
| DYN | 1 | 0.74 | 0.25‐2.18 | ||
| SUP | 2 | 0.31 | 0.06‐1.75 | 29 | |
| CAU | 13 | 0.33 | 0.20‐0.56 | 46 | |
| WL | 9 | 0.18 | 0.11‐0.32 | 2 | |
| PLA | 1 | 0.34 | 0.15‐0.81 | ||
| PST | IPT | 1 | 0.37 | 0.13‐1.03 | |
| SUP | 5 | 0.38 | 0.25‐0.57 | 0 | |
| LRT | 1 | 0.51 | 0.18‐1.50 | ||
| CAU | 10 | 0.37 | 0.19‐0.73 | 77 | |
| WL | 13 | 0.47 | 0.29‐0.76 | 51 | |
| PLA | 3 | 0.65 | 0.36‐1.19 | 57 | |
| 3WV | CAU | 7 | 0.23 | 0.09‐0.60 | 63 |
| WL | 15 | 0.30 | 0.20‐0.45 | 39 | |
| IPT | SUP | 5 | 0.64 | 0.32‐1.29 | 20 |
| CAU | 17 | 0.42 | 0.26‐0.68 | 69 | |
| WL | 3 | 0.20 | 0.10‐0.40 | 0 | |
| PLA | 2 | 0.46 | 0.23‐0.91 | 0 | |
| DYN | SUP | 3 | 0.34 | 0.12‐0.97 | 58 |
| CAU | 5 | 0.77 | 0.52‐1.12 | 0 | |
| WL | 1 | 0.16 | 0.01‐3.85 | ||
| SUP | LRT | 1 | 3.60 | 0.34‐38.30 | |
| CAU | 8 | 0.56 | 0.41‐0.77 | 0 | |
| WL | 3 | 0.43 | 0.09‐2.12 | 0 | |
| LRT | CAU | 6 | 0.06 | 0.03‐0.13 | 0 |
| WL | 6 | 0.35 | 0.22‐0.56 | 1 | |
| CAU | WL | 3 | 0.54 | 1.09‐2.71 | 46 |
Bold prints highlight significant differences. OR – odds ratio, CBT – cognitive behavioural therapy, BAT – behavioural activation therapy, PST – problem‐solving therapy, 3WV – “third wave” therapies, IPT – interpersonal psychotherapy, DYN – psychodynamic therapy, SUP – non‐directive support counseling, LRT – life‐review therapy, CAU – care‐as‐usual, WL – waiting list, PLA – pill placebo
Although heterogeneity was low in most comparisons, several comparisons (especially involving care‐as‐usual or non‐directive supportive counseling) had an I 2 above 50%.
Network meta‐analyses
The main results of the NMA are presented in Tables 3, 4, 5, 6. The results for response indicate that all therapies are more efficacious than care‐as‐usual and waiting list, with few significant differences between therapies. Only non‐directive supportive counseling was less efficacious than all other therapies, with ORs ranging between 0.49 to 0.65. All therapies, except non‐directive supportive counseling and psychodynamic therapy, were also more efficacious than pill placebo. The results for remission and SMD are very similar to those for response. Only the results for pill placebo differ considerably, potentially related to the small number of studies.
Table 3.
Network meta‐analyses: response in psychotherapies compared with each other and with control conditions
| CBT | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
1.20 (0.90‐1.61) |
BAT | |||||||||
|
0.99 (0.75‐1.31) |
0.83 (0.57‐1.20) |
PST | ||||||||
|
1.02 (0.76‐1.38) |
0.85 (0.58‐1.25) |
1.03 (0.70‐1.51) |
3WV | |||||||
|
1.00 (0.76‐1.31) |
0.83 (0.57‐1.22) |
1.00 (0.70‐1.44) |
0.98 (0.66‐1.45) |
IPT | ||||||
|
0.89 (0.62‐1.29) |
0.74 (0.47‐1.17) |
0.90 (0.58‐1.40) |
0.88 (0.55‐1.40) |
0.90 (0.58‐1.39) |
DYN | |||||
|
0.58 (0.45‐0.75) |
0.49 (0.34‐0.70) |
0.59 (0.42‐0.82) |
0.57 (0.39‐0.84) |
0.59 (0.42‐0.83) |
0.65 (0.43‐0.99) |
SUP | ||||
|
1.47 (0.87‐2.49) |
1.23 (0.68‐2.20) |
1.48 (0.85‐2.60) |
1.45 (0.81‐2.60) |
1.48 (0.83‐2.63) |
1.65 (0.88‐3.10) |
2.52 (1.43‐4.45) |
LRT | |||
|
0.43 (0.37‐0.50) |
0.36 (0.26‐0.48) |
0.43 (0.33‐0.57) |
0.42 (0.31‐0.58) |
0.43 (0.33‐0.56) |
0.48 (0.33‐0.69) |
0.73 (0.56‐0.96) |
0.29 (0.17‐0.49) |
CAU | ||
|
0.28 (0.24‐0.34) |
0.24 (0.17‐0.32) |
0.29 (0.21‐0.38) |
0.28 (0.21‐0.38) |
0.28 (0.21‐0.39) |
0.32 (0.21‐0.47) |
0.48 (0.36‐0.65) |
0.19 (0.11‐0.32) |
0.66 (0.54‐0.81) |
WL | |
|
0.53 (0.34‐0.83) |
0.44 (0.26‐0.74) |
0.53 (0.34‐0.85) |
0.52 (0.30‐0.89) |
0.53 (0.32‐0.88) |
0.59 (0.33‐1.05) |
0.91 (0.55‐1.50) |
0.36 (0.18‐0.71) |
1.24 (0.78‐1.97) |
1.87 (1.17‐3.00) |
PLA |
Values are odds ratios (OR) with 95% confidence intervals. OR<1 means that the row‐defining intervention is less efficacious than the column‐defining intervention. Bold prints highlight significant differences. CBT – cognitive behavioural therapy, BAT – behavioural activation therapy, PST – problem‐solving therapy, 3WV – “third wave” therapies, IPT – interpersonal psychotherapy, DYN – psychodynamic therapy, SUP – non‐directive supportive counseling, LRT – life‐review therapy, CAU – care‐as‐usual, WL – waiting list, PLA – pill placebo
Table 4.
Network meta‐analyses: acceptability of psychotherapies compared with each other and with control conditions
| CBT | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
1.07 (0.78‐1.46) |
BAT | |||||||||
|
1.05 (0.79‐1.40) |
0.99 (0.66‐1.47) |
PST | ||||||||
|
0.99 (0.69‐1.42) |
0.93 (0.59‐1.46) |
0.94 (0.61‐1.46) |
3WV | |||||||
|
0.92 (0.68‐1.24) |
0.86 (0.57‐1.30) |
0.87 (0.59‐1.28) |
0.93 (0.59‐1.46) |
IPT | ||||||
|
1.38 (0.99‐1.92) |
1.29 (0.84‐1.99) |
1.31 (0.85‐2.00) |
1.39 (0.86‐2.25) |
1.50 (0.98‐2.29) |
DYN | |||||
|
1.04 (0.76‐1.42) |
0.98 (0.65‐1.47) |
0.99 (0.68‐1.44) |
1.05 (0.66‐1.67) |
1.13 (0.77‐1.68) |
0.76 (0.49‐1.17) |
SUP | ||||
|
0.82 (0.49‐1.39) |
0.77 (0.43‐1.40) |
0.78 (0.45‐1.36) |
0.83 (0.45‐1.53) |
0.90 (0.50‐1.61) |
0.60 (0.33‐1.10) |
0.79 (0.44‐1.41) |
LRT | |||
|
0.89 (0.77‐1.03) |
0.83 (0.61‐1.13) |
0.84 (0.63‐1.13) |
0.89 (0.62‐1.30) |
0.97 (0.73‐1.28) |
0.64 (0.46‐0.90) |
0.85 (0.62‐1.17) |
1.08 (0.64‐1.83) |
CAU | ||
|
0.67 (0.56‐0.80) |
0.63 (0.44‐0.88) |
0.63 (0.47‐0.85) |
0.67 (0.47‐0.96) |
0.73 (0.52‐1.02) |
0.49 (0.33‐0.70) |
0.64 (0.45‐0.90) |
0.81 (0.49‐1.35) |
0.75 (0.60‐0.94) |
WL | |
|
1.38 (0.84‐2.27) |
1.30 (0.73‐2.29) |
1.31 (0.75‐2.30) |
1.39 (0.76‐2.56) |
1.50 (0.86‐2.62) |
1.00 (0.57‐1.76) |
1.33 (0.75‐2.36) |
1.68 (0.82‐3.43) |
1.56 (0.94‐2.59) |
2.07 (1.23‐3.49) |
PLA |
Values are odds ratios (OR) with 95% confidence intervals. OR<1 means that the row‐defining intervention is more acceptable than the column‐defining intervention. Bold prints highlight significant differences. CBT – cognitive behavioural therapy, BAT – behavioural activation therapy, PST – problem‐solving therapy, 3WV – “third wave” therapies, IPT – interpersonal psychotherapy, DYN – psychodynamic therapy, SUP – non‐directive supportive counseling, LRT – life‐review therapy, CAU – care‐as‐usual, WL – waiting list, PLA – pill placebo
Table 5.
Network meta‐analyses: remission in psychotherapies compared with each other and with control conditions
| CBT | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
1.14 (0.79‐1.63) |
BAT | |||||||||
|
1.10 (0.78‐1.56) |
0.97 (0.61‐1.54) |
PST | ||||||||
|
1.03 (0.69‐1.54) |
0.90 (0.55‐1.49) |
0.93 (0.56‐1.55) |
3WV | |||||||
|
0.88 (0.63‐1.23) |
0.78 (0.49‐1.24) |
0.80 (0.51‐1.27) |
0.86 (0.52‐1.44) |
IPT | ||||||
|
0.74 (0.52‐1.06) |
0.65 (0.41‐1.05) |
0.67 (0.42‐1.08) |
0.72 (0.43‐1.22) |
0.84 (0.53‐1.33) |
DYN | |||||
|
0.59 (0.42‐0.83) |
0.52 (0.33‐0.82) |
0.54 (0.35‐0.83) |
0.58 (0.35‐0.96) |
0.67 (0.44‐1.02) |
0.80 (0.52‐1.23) |
SUP | ||||
|
0.71 (0.33‐1.52) |
0.63 (0.27‐1.43) |
0.65 (0.29‐1.42) |
0.69 (0.30‐1.59) |
0.81 (0.36‐1.82) |
0.96 (0.42‐2.19) |
1.20 (0.53‐2.73) |
LRT | |||
|
0.35 (0.29‐0.43) |
0.31 (0.21‐0.45) |
0.32 (0.22‐0.46) |
0.34 (0.22‐0.53) |
0.40 (0.29‐0.55) |
0.47 (0.33‐0.68) |
0.60 (0.42‐0.82) |
0.49 (0.23‐1.07) |
CAU | ||
|
0.25 (0.20‐0.32) |
0.22 (0.15‐0.33) |
0.23 (0.16‐0.33) |
0.25 (0.16‐0.37) |
0.29 (0.15‐0.42) |
0.34 (0.22‐0.52) |
0.43 (0.29‐0.63) |
0.36 (0.17‐0.74) |
0.72 (0.54‐0.96) |
WL | |
|
0.58 (0.33‐1.52) |
0.51 (0.27‐0.99) |
0.53 (0.30‐0.93) |
0.57 (0.28‐1.13) |
0.66 (0.35‐1.24) |
0.78 (0.42‐1.48) |
0.98 (0.52‐1.86) |
0.82 (0.32‐2.07) |
1.65 (0.92‐2.96) |
2.30 (1.26‐4.19) |
PLA |
Values are odds ratios (OR) with 95% confidence intervals. OR<1 means that the row‐defining intervention is less efficacious than the column‐defining intervention. Bold prints highlight significant differences. CBT – cognitive behavioural therapy, BAT – behavioural activation therapy, PST – problem‐solving therapy, 3WV – “third wave” therapies, IPT – interpersonal psychotherapy, DYN – psychodynamic therapy, SUP – non‐directive supportive counseling, LRT – life‐review therapy, CAU – care‐as‐usual, WL – waiting list, PLA – pill placebo
Table 6.
Network meta‐analyses: standardized mean difference for psychotherapies compared with each other and with control conditions
| CBT | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
0.06 (–0.15 to 0.28) |
BAT | |||||||||
|
–0.03 (–0.27 to 0.20) |
–0.09 (–0.39 to 0.20) |
PST | ||||||||
|
0.02 (–0.21 to 0.25) |
–0.04 (–0.33 to 0.25) |
0.05 (–0.26 to 0.37) |
3WV | |||||||
|
–0.13 (–0.36 to 0.10) |
–0.19 (–0.49 to 0.10) |
–0.10 (–0.40 to 0.21) |
–0.15 (–0.46 to 0.16) |
IPT | ||||||
|
–0.17 (–0.47 to 0.13) |
–0.23 (–0.69 to 0.13) |
–0.13 (–0.50 to 0.24) |
–0.19 (–0.56 to 0.18) |
–0.04 (–0.40 to 0.33) |
DYN | |||||
|
–0.35 (–0.55 to –0.15) |
–0.41 (–0.69 to –0.13) |
–0.32 (–0.60 to –0.03) |
–0.37 (–0.67 to –0.07) |
–0.22 (–0.49 to 0.06) |
–0.18 (–0.52 to 0.15) |
SUP | ||||
|
0.14 (–0.21 to 0.48) |
0.08 (–0.32 to 0.47) |
0.17 (–0.23 to 0.57) |
0.12 (–0.28 to 0.52) |
0.27 (–0.13 to 0.67) |
0.30 (–0.14 to 0.75) |
0.49 (0.10 to 0.87) |
LRT | |||
|
–0.67 (–0.79 to –0.56) |
–0.73 (–0.95 to –0.52) |
–0.64 (–0.88 to –0.40) |
–0.69 (–0.93 to –0.45) |
–0.54 (–0.76 to –0.32) |
–0.50 (–0.81 to –0.20) |
–0.32 (–0.53 to –0.11) |
–0.81 (–1.15 to –0.46) |
CAU | ||
|
–0.97 (–1.09 to –0.84) |
–1.03 (–1.26 to –0.80) |
–0.93 (–1.17 to –0.69) |
–0.99 (–1.22 to –0.76) |
–0.84 (–1.08 to –0.59) |
–0.80 (–1.12 to –0.48) |
–0.62 (–0.84 to –0.39) |
–1.10 (–1.45 to –0.76) |
0.29 (0.14 to 0.45) |
WL | |
|
–0.64 (–1.16 to –0.11) |
–0.70 (–1.25 to –0.15) |
–0.61 (–1.16 to –0.05) |
–0.66 (–1.23 to –0.09) |
–0.51 (–1.06 to 0.05) |
–0.47 (–1.07 to 0.13) |
–0.29 (–0.85 to 0.27) |
–0.78 (–1.40 to –0.15) |
–0.03 (–0.56 to 0.50) |
0.33 (–0.21 to 0.86) |
PLA |
Values are standardized mean differences (SMDs) with 95% confidence intervals. Negative values indicate that the row‐defining intervention is less efficacious than the column‐defining intervention. Bold prints highlight significant differences. CBT – cognitive behaviour therapy, BAT – behavioural activation therapy, PST – problem‐solving therapy, 3WV – “third wave” therapies, IPT – interpersonal therapy, DYN – psychodynamic therapy, SUP – non‐directive supportive counseling, LRT – life‐review therapy, CAU – care‐as‐usual, WL – waiting list, PLA – pill placebo
The acceptability of all therapies (except interpersonal psychotherapy and life‐review therapy) was significantly lower than waiting list, with ORs ranging between 0.49 to 0.67. Psychodynamic therapy was significantly less acceptable than care‐as‐usual (OR=0.64). No significant differences for acceptability were found between any of the therapies.
The global tau‐squared was 0.19 for response. The design‐by‐treatment interaction model indicated global inconsistency in the network (p for the null hypothesis of consistency in the network <0.01). Consistency factors were examined using the loop specific approach. Considerable inconsistency was found: out of 60 loops, four showed significant inconsistency.
Because of the global inconsistency in the network, we searched for the sources of trial‐level influential factors by a bootstrapping method 25 . Through the bootstrap‐based evaluation, 37 trials were detected as influential outliers. After excluding these outliers, global inconsistency was no longer significant (p for the null hypothesis of consistency in the network = 0.11; global tau‐squared: 0.03). The results of the NMA after excluding these outliers were similar to the main analyses (see supplementary information).
Except for some comparisons mainly involving active interventions versus waiting list (CBT, behavioural activation therapy, “third wave” therapies, interpersonal psychotherapy, psychodynamic therapy, and life‐review therapy vs. waiting list, and behavioural activation therapy vs. care‐as‐usual) which had moderate certainty, all the estimates were rated as low to very low certainty of evidence (see supplementary information).
The results of the SUCRA are shown in Table 7, separately for response, remission, SMD and acceptability. Life‐review and behavioural activation therapy ranked highest for response and SMD; behavioural activation and problem‐solving therapy ranked highest for remission; while non‐directive supportive counseling and psychodynamic therapy ranked lowest for response, remission and SMD. Psychodynamic therapy ranked lowest for acceptability, while life‐review and interpersonal psychotherapy ranked highest.
Table 7.
Ranking of psychotherapies and control conditions according to the “surface under the cumulative ranking” (SUCRA) for response, standardized mean difference (SMD), remission and acceptability
| Response | SMD | Remission | Acceptability | |
|---|---|---|---|---|
|
Cognitive behavioural therapy |
64.0 |
72.8 |
75.1 |
48.4 |
| Behavioural activation therapy | 85.2 | 82.1 | 86.3 | 39.1 |
| Problem‐solving therapy | 62.9 | 67.2 | 83.5 | 40.8 |
| “Third wave” therapies | 66.5 | 75.7 | 76.3 | 51.1 |
| Interpersonal psychotherapy | 64.6 | 52.0 | 62.3 | 62.1 |
| Psychodynamic therapy | 52.8 | 49.2 | 46.3 | 10.0 |
| Non‐directive supportive counseling | 26.6 | 30.8 | 30.5 | 42.3 |
| Life‐review therapy | 93.1 | 87.1 | 46.5 | 72.5 |
| Care‐as‐usual | 12.0 | 14.5 | 10.7 | 71.8 |
| Waiting list | 0.0 | 1.10 | 0.2 | 97.2 |
| Pill placebo | 22.3 | 17.4 | 32.2 | 14.6 |
Table 8.
Long‐term response to psychotherapies compared with each other and control conditions
| CBT | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
0.97 (0.62‐1.52) |
BAT | ||||||||
|
1.69 (1.08‐2.66) |
1.75 (0.97‐3.14) |
PST | |||||||
|
0.77 (0.46‐1.30) |
0.80 (0.43‐1.49) |
0.46 (0.23‐0.90) |
3WV | ||||||
|
1.35 (0.92‐1.99) |
1.40 (0.78‐2.49) |
0.80 (0.45‐1.41) |
1.75 (0.93‐3.31) |
IPT | |||||
|
1.02 (0.63‐1.66) |
1.05 (0.55‐2.02) |
0.60 (0.32‐1.14) |
1.32 (0.65‐2.67) |
0.75 (0.41‐1.38) |
DYN | ||||
|
0.78 (0.56‐1.09) |
0.81 (0.46‐1.40) |
0.46 (0.27‐0.79) |
1.01 (0.55‐1.86) |
0.58 (0.36‐0.94) |
0.76 (0.44‐1.33) |
SUP | |||
|
0.90 (0.19‐4.33) |
0.93 (0.18‐4.75) |
0.53 (0.10‐2.71) |
1.16 (0.22‐6.05) |
0.67 (0.13‐3.33) |
0.88 (0.17‐4.52) |
1.15 (0.24‐5.48) |
LRT | ||
|
0.59 (0.50‐0.70) |
0.61 (0.39‐0.96) |
0.35 (0.23‐0.53) |
0.76 (0.45‐1.29) |
0.43 (0.30‐0.63) |
0.58 (0.36‐0.93) |
0.75 (0.54‐1.06) |
0.65 (0.14‐3.15) |
CAU | |
|
0.49 (0.29‐0.83) |
0.51 (0.26‐1.01) |
0.29 (0.15‐0.58) |
0.63 (0.31‐1.29) |
0.36 (0.19‐0.69) |
0.48 (0.24‐0.98) |
0.63 (0.34‐1.16) |
0.55 (0.11‐2.69) |
0.84 (0.48‐1.44) |
WL |
Values are odds ratios (OR) with 95% confidence intervals. OR<1 means that the row‐defining intervention is less efficacious than the column‐defining intervention. Bold prints highlight significant differences. CBT – cognitive behavioural therapy, BAT – behavioural activation therapy, PST – problem‐solving therapy, 3WV – “third wave” therapies, IPT – interpersonal therapy, DYN – psychodynamic therapy, SUP – non‐directive supportive counseling, LRT – life‐review therapy, CAU – care‐as‐usual, WL – waiting list, PLA – pill placebo
Sensitivity and meta‐regression analyses
In the sensitivity analyses in which we only included studies with low risk of bias, we found outcomes comparable to the main analyses. Only the differences between non‐directive supportive counseling and most other therapies were no longer significant, and non‐directive supportive counseling was no longer significantly better than care‐as‐usual and waiting list. The other sensitivity analyses resulted in no materially different outcomes from the main analyses.
In meta‐regression analyses, only five predictors were found to be statistically significant (diagnosed depressive disorder for CBT vs. interpersonal psychotherapy, and CBT vs. waiting list; number of sessions for CBT vs. behavioural activation therapy; Western vs. non‐Western countries for CBT vs. care‐as‐usual; and risk of bias for CBT vs. behavioural activation therapy) (see supplementary information). Because of their correlational nature and the large number of analyses conducted, these findings should be interpreted with caution.
In the meta‐regression analysis to assess the influences of small study effects, the overall results were comparable with the main analysis.
Long‐term effects
We conducted an NMA with the 90 studies that reported outcomes for response at 12 (±6) months after randomization (see Table 7). The results indicated that CBT, behavioural activation therapy, problem‐solving therapy, interpersonal psychotherapy, and psychodynamic therapy had significant effects compared with care‐as‐usual at follow‐up. The same therapies, except behavioural activation therapy, had also significant effects compared to waiting list. Problem‐solving therapy was significantly more effective than CBT, “third wave” therapies and non‐directive supportive counseling at follow‐up. Interpersonal psychotherapy was also significantly more effective than non‐directive supportive counseling at follow‐up.
Only nine studies reported outcomes at more than 18 months after randomization. Because of the small number of studies and different periods, we did not conduct any analyses with these studies.
DISCUSSION
In this NMA, we compared the effects of the eight most common types of psychotherapy for depression with each other and with major control conditions in 331 controlled trials. We found that all therapies had significant effects compared to care‐as‐usual and waiting list control condition. The effects of the therapies did not differ significantly from each other, except for non‐directive supportive counseling, that was less effective than all the other types of therapy. These results were broadly confirmed in a series of sensitivity analyses.
These findings are in line with previous meta‐analytic research on psychotherapies for depression7, 10. However, in contrast to previous meta‐analyses, we could include a considerable number of studies with low risk of bias, which broadly confirmed the main results of this NMA.
Non‐directive supportive counseling was less effective than the other therapies, but these findings were no longer significant when we only included studies with low risk of bias. This is in line with previous meta‐analytic work 26 . However, these findings may be related to the fact that, in many studies, counseling was used as a control condition, and therapists may not have delivered optimal treatments.
Life‐review therapy was not included in previous meta‐analyses, because the number of studies was too small. This psychotherapy is mostly used in older adults, but it has also been used successfully in cancer patients27, 28, and it could very well be used in other populations without general medical disorders. Because of the small number of studies and the low quality of most of them, more research is clearly needed. However, life‐review therapy can be considered a promising intervention that is probably efficacious in depression.
Overall, the findings of this NMA suggest that all psychotherapies that were examined, except non‐directive supportive counseling, are efficacious and can be used in routine care. The fact that all psychotherapies can be efficacious means that, when choosing a therapy, patient's preferences can have a prominent role. Mental health professionals need to facilitate access to evidence‐based updated information about the effects of treatment interventions and to involve patients more in their day‐to‐day care, with a focus on carefully acknowledging the risk and outlining potential effects while managing expectations 29 . It is possible that a more detailed characterization of each patient with a diagnosis of depression may lead to a more precise matching between individual patients and individual psychotherapies 30 .
One important finding of this study is that several psychotherapies still have significant effects at one‐year follow‐up, including CBT, behavioural activation therapy, problem‐solving therapy, interpersonal psychotherapy, and psychodynamic therapy. We also found that problem‐solving therapy may be somewhat more efficacious than some other therapies at follow‐up, although this should be considered with caution, because of the relatively small number of studies and the considerable risk of bias in most studies. It is important for clinicians and patients that therapies work considerably longer than the therapy lasts.
In a recent NMA published in this journal 31 , combined psychotherapy and pharmacotherapy was more effective than either of them alone in achieving response, also in chronic and treatment‐resistant depression. Combined treatment and psychotherapy alone were also more acceptable than pharmacotherapy. Combined treatments seem therefore to be the best choice for patients with moderate to severe depression.
This study has several important strengths, but also some limitations. One strength is the large number of trials (N=331) that could be included. This is the largest NMA ever conducted in psychotherapies for depression. Although most studies were focused on CBT, care‐as‐usual and waiting list, we have sufficient studies comparing most other therapies and control conditions with each other. One important limitation is that the proportion of studies with low risk of bias was still relatively small (30.8%), although this was enough to conduct sensitivity analyses. Another important limitation is that we found some discrepancies between direct and indirect evidence, and only after excluding outliers the direct and indirect evidence pointed in the same direction. A final limitation is that only a relatively small number of trials reported longer‐term outcomes, which makes these effects uncertain.
Despite these limitations, we can conclude that the most important types of psychotherapy, including CBT, behavioural activation therapy, problem‐solving therapy, “third wave” therapies, interpersonal psychotherapy, psychodynamic therapy and life‐review therapy, can be effective and acceptable in the treatment of adult depression, with no significant differences between them.
ACKNOWLEDGEMENTS
Supplementary information on the study is available at https://osf.io/7rmgj/.
REFERENCES
- 1. Steel Z, Marnane C, Iranpour C et al. The global prevalence of common mental disorders: a systematic review and meta‐analysis 1980‐2013. Int J Epidemiol 2014;43:476‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bloom DE, Cafiero E, Jané‐Llopis E et al. The global economic burden of noncommunicable diseases. Geneva: World Economic Forum, 2011. [Google Scholar]
- 3. Hu TW. Perspectives: an international review of the national cost estimates of mental illness, 1990‐2003. J Ment Health Policy Econ 2006;9:3‐13. [PubMed] [Google Scholar]
- 4. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990‐2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1211‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cuijpers P, Vogelzangs N, Twisk J et al. Comprehensive meta‐analysis of excess mortality in depression in the general community versus patients with specific illnesses. Am J Psychiatry 2014;171:453‐62. [DOI] [PubMed] [Google Scholar]
- 6. Cipriani A, Furukawa TA, Salanti G et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta‐analysis. Lancet 2018;391:1357‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barth J, Munder T, Gerger H et al. Comparative efficacy of seven psychotherapeutic interventions for depressed patients: a network meta‐analysis. PLoS Med 2013;10:e1001454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cuijpers P, Berking M, Andersson G et al. A meta‐analysis of cognitive behavior therapy for adult depression, alone and in comparison to other treatments. Can J Psychiatry 2013;58:376‐85. [DOI] [PubMed] [Google Scholar]
- 9. Cuijpers P, Karyotaki E, de Wit L et al. The effects of fifteen evidence‐supported therapies for adult depression: a meta‐analytic review. Psychother Res 2020;30:279‐93. [DOI] [PubMed] [Google Scholar]
- 10. Cuijpers P, van Straten A, Andersson G et al. Psychotherapy for depression in adults: a meta‐analysis of comparative outcome studies. J Consult Clin Psychol 2008;76:909‐22. [DOI] [PubMed] [Google Scholar]
- 11. Cuijpers P. Are all psychotherapies equally effective in the treatment of adult depression? The lack of statistical power of comparative outcome studies. Evid Based Ment Health 2016;19:39‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cuijpers P, Karyotaki E, Ciharova M. A meta‐analytic database of randomised trials on psychotherapies for depression. www.osf.io/825c6.
- 13. Cuijpers P, Clignet F, van Meijel B et al. Psychological treatment of depression in inpatients: a systematic review and meta‐analysis. Clin Psychol Rev 2011;31:353‐60. [DOI] [PubMed] [Google Scholar]
- 14. Cuijpers P, Noma H, Karyotaki E et al. Individual, group, telephone, self‐help and internet‐based cognitive behavior therapy for adult depression; a network meta‐analysis of delivery methods. JAMA Psychiatry 2019;76:700‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Higgins JPT, Altman DG, Gøtzsche PC et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Furukawa TA, Cipriani A, Barbui C et al. Imputing response rates from means and standard deviations in meta‐analyses. Psychopharmacology 2005;20:49‐52. [DOI] [PubMed] [Google Scholar]
- 17. Orsini N, Bottai M, Higgins J et al. Heterogi: Stata module to quantify heterogeneity in a meta‐analysis. Boston: Statistical Software Components, 2006. [Google Scholar]
- 18. Egger M, Smith GD, Schneider M et al. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hutton B, Wolfe D, Moher D et al. Reporting guidance considerations from a statistical perspective: overview of tools to enhance the rigour of reporting of randomised trials and systematic reviews. Evid Based Ment Health 2017;20:46‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chaimani A, Higgins JP, Mavridis D et al. Graphical tools for network metaanalysis in STATA. PLoS One 2013;8:e76654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chaimani A, Salanti G, Leucht S et al. Common pitfalls and mistakes in the set‐up, analysis and interpretation of results in network meta‐analysis: what clinicians should look for in a published article. Evid Based Ment Health 2017;20:88‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Turner RM, Davey J, Clarke MJ et al. Predicting the extent of heterogeneity in meta‐analysis, using empirical data from the Cochrane Database of Systematic Reviews. Int J Epidemiol 2012;41:818‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rhodes KM, Turner RM, Higgins JP. Predictive distributions were developed for the extent of heterogeneity in meta‐analyses of continuous outcome data. J Clin Epidemiol 2015;68:52‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nikolakopoulou A, Higgins JPT, Papakonstantinou T et al. CINeMA: an approach for assessing confidence in the results of a network meta‐analysis. PLoS Med 2020;17:1‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Noma H, Gosho M, Ishii R et al. Outlier detection and influence diagnostics in network meta‐analysis. Res Synth Meth 2020;11:891‐902. [DOI] [PubMed] [Google Scholar]
- 26. Cuijpers P, Driessen E, Hollon SD et al. The efficacy of non‐directive supportive therapy for adult depression: a meta‐analysis. Clin Psychol Rev 2012;32:280‐91. [DOI] [PubMed] [Google Scholar]
- 27. Kleijn G, Lissenberg‐Witte BI, Bohlmeijer ET et al. The efficacy of Life Review Therapy combined with Memory Specificity Training (LRT‐MST) targeting cancer patients in palliative care: a randomized controlled trial. PLoS One 2018;13:e0197277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhang X, Xiao H, Chen Y. Effects of life review on mental health and well‐being among cancer patients: a systematic review. Int J Nurs Stud 2017;74:138‐48. [DOI] [PubMed] [Google Scholar]
- 29. Tomlinson A, Boaden K, Cipriani A. Withdrawal, dependence and adverse events of antidepressants: lessons from patients and data. Evid Based Ment Health 2019;22:137‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Maj M, Stein DJ, Parker G et al. The clinical characterization of the adult patients with depression aimed at personalization of management. World Psychiatry 2020;19:269‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cuijpers P, Noma H, Karyotaki E et al. A network meta‐analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatry 2020;19:92‐107. [DOI] [PMC free article] [PubMed] [Google Scholar]


