Abstract
Purpose
The purpose of this study is to evaluate the reliability of magnetic resonance imaging (MRI) in predicting the location of ACL tears in preoperative planning for anterior cruciate ligament (ACL) repair.
Methods
Thirty-four patients who underwent ACL repair were retrospectively analyzed to compare intraoperative arthroscopic findings with preoperative MRIs.
Results
For identifying type I tears, the sensitivity of MRI was 9.0% and the accuracy of MRI was 8.8%. There was moderate interrater agreement between MRI findings for tear location and tear degree.
Conclusion
MRI alone may not necessarily be accurate in identifying which ACL tears are amenable to repair.
Study design
Retrospective case series; Level of Evidence: IV;
Keywords: Anterior cruciate ligament tear, Magnetic resonance imaging, Anterior cruciate ligament repair
1. Introduction
Anterior cruciate ligament (ACL) tears account for approximately fifty percent of all sports-related knee injuries nationally.1 Approximately 200,000 people in the United States experience ACL tears with over $7 billion dollars in direct and indirect costs annually.2 Clinical evaluation of ACL injury aims to identify both anterior translation and anterolateral rotational instability, both of which are normally limited by the ACL.3,4 On physical exam, identification of an ACL deficient knee can be achieved through the pivot-shift and Lachman maneuvers with high specificity.5 Although these tests are useful in diagnosing the presence of a tear, the location of injury cannot be identified without advanced imaging.
Imaging evaluation of ACL tear often begins with knee magnetic resonance imaging (MRI). Studies have shown MRI to have an overall accuracy of 85.0%, a sensitivity of 82.5%, and a specificity of 92.8% for diagnosing ACL tears.6 Evaluation of ACL tears includes review of axial, sagittal, and coronal planes, with axial cuts as the most helpful for assessing the ACL at its proximal femoral attachment.7, 8, 9 However, while MRI is useful in identifying the presence of a tear, it may be limited in assessing the exact location of injury.7,10, 11, 12 Newer advanced MRI sequencing, including the use of three-dimensional fast-spin echo and apparent diffusion coefficient mapping, may provide increased ability to determine the precise location of ACL tear.8,13 However, these sequences are not routinely ordered in orthopedic practice.
ACL repair, which historically had inferior outcomes when compared to ACL reconstruction (ACLR), has recently re-emerged as a viable option in treating ACL tears, specifically in proximal ACL tears.14, 15, 16, 17, 18 Sherman et al. additionally developed a classification of ACL tear location14 which was later modified to better standardize categorization of tear location amongst radiologists and improve surgical planning of repairing ACLs, with Sherman type I ACL tears considered as repairable (Table 1).13 With the advent of arthroscopic knee surgery, early postoperative rehabilitation, a better understanding of the ACL's native anatomy, and suture augmentation (SA), ACL repair has emerged as viable, although controversial, alternative to ACLR.19, 20, 21
Table 1.
Modified Sherman Classification of ACL Tears, adapted from Daniels et al. (2018).13
| Degree of Tear | Characteristics | Tear Location |
|---|---|---|
| Type I | Proximal avulsion tear | >90% distal ligament intact |
| Type II | Proximal tear | 75–90% distal ligament intact |
| Type III | Mid-substance tear | 25–75% distal ligament intact |
| Type IV | Distal tear | 10–25% distal ligament intact |
| Type V | Distal avulsion tear | <10% distal ligament intact |
As ACL repair continues to emerge as a viable surgical option in select cases, the ability to predict ACL tear site location and tear degree becomes more important preoperatively. Preoperative imaging in which the correct location of a tear is identified is important to determine surgical candidates for repair and to guide surgeons when counseling patients about surgical options. Therefore, the purpose of this study is to evaluate the reliability of MRI in predicting the location of ACL tears in preoperative planning for ACL repair. We hypothesized there would be a high degree of variability between preoperative MRI and intraoperative arthroscopic findings.
2. Methods
Following Institutional Review Board approval, we retrospectively reviewed all patients that underwent ACL repairs by a single surgeon at our institution from June 2015 to August 2018. All patients were seen for an isolated ACL injury and were consented for both ACL reconstruction (ACLR) and repair. The final treatment decision was made intraoperatively after diagnostic arthroscopy.
Using the Sherman classification,14 an ACL repair was performed if the patient had a modified Sherman type I, which was determined intraoperatively. No midsubstance ACL tears (type II, III, IV) or distal ACL tears (type V) were repaired. Exclusion criteria included bony tibial avulsion injuries, revision ACL surgeries, and patients whose MRI imaging was unavailable in the current EMR system.
Preoperative sagittal, coronal, oblique coronal, oblique sagittal, and axial views performed in a 3T MRI were reviewed by three musculoskeletal fellowship-trained radiologists blinded to the patient's intraoperative Sherman classification. The integrity of the ligament's mid-substance, tibial, and femoral attachments were assessed to determine the tear location and then classified according to the modified Sherman classification. Additionally, tear degree was reported as no tear, partial tear, or complete/full-thickness tear.
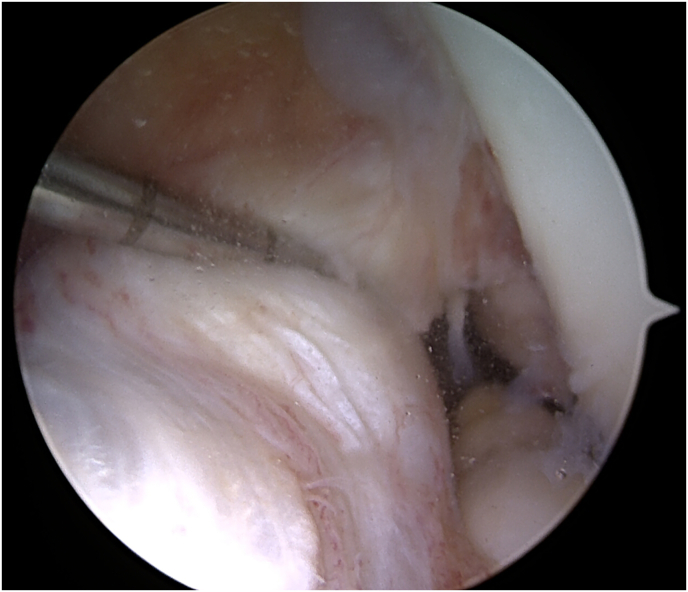
Intraoperative reports and arthroscopic images were reviewed to identify the intraoperative tear location and degree. Intraoperative tear grading was then compared with the preoperative MRI Sherman classification and tear degree to identify any discrepancies. An example of a discrepancy between MRI findings and intraoperative findings is demonstrated in Fig. 1, Fig. 2, Fig. 3. Fig. 1 demonstrates a full-thickness mid-substance tear on MRI, whereas Fig. 2, Fig. 3 demonstrate intraoperative findings of a partial-thickness tear of the anteromedial bundle of the ACL in the same patient.
Fig. 1.
Sagittal T-2 weighted magnetic resonance image of a left knee demonstrating a full thickness anterior cruciate ligament tear.
Fig. 2.
Intraoperative image of the same patient as in Fig. 1 demonstrating a partial-thickness anterior cruciate ligament tear involving anteromedial bundle.
Fig. 3.
Further probing of the anterior cruciate ligament in Fig. 2 further demonstrates a robust ligament which made the patient a suitable candidate for repair.
2.1. Statistical methods
Sensitivity and accuracy of the MRI findings in determining presence of a proximal avulsion (Sherman type I) or whether there was a complete tear were calculated with intraoperative findings set as the gold standard. Specificity, positive predictive value (PPV), and negative predictive value (NPV) were also calculated for MRI's ability to detect the presence of a complete tear. However, these values were not able to be calculated for tear location as all tears were Sherman type I intraoperatively. Additionally, to assess interrater reliability among the three radiologists, Fleiss's kappa statistic was calculated with the Altman classification assigned for the strength of the agreement.22 Cohen's kappa and percent agreement was also calculated as a measure of MRI accuracy in determining tear location and degree, compared to intraoperative findings. Agreement was defined as both when all radiologists having the same preoperative diagnosis and when that diagnosis was consistent with the intraoperative findings. Majority rules was used to compare MRI and intraoperative findings. If all 3 radiologists disagreed, the MRI was recorded as being wrong. Statistical analysis was performed using RStudio, Version 1.1.442 (RStudio Inc. Boston, MA). Values are demonstrated as mean (range), mean ± standard deviation (SD), or mean (95% confidence interval [CI]) when appropriate.
3. Results
42 consecutive ACL repairs were identified, of which 34 met inclusion criteria (81.0%). Four patients were excluded because they were bony tibial spine avulsions, 2 patients were excluded because of missing preoperative imaging studies, and 2 patients were excluded as they had repairs performed as a revision procedure of a failed anterior cruciate ligament reconstruction.23 Of the included patients, 24 were males (70.6%) and the mean ± SD of age was 31.4 ± 8.8 years (range 14–50 years). All 34 included patients had primary ACL repairs with 2–3 weeks of initial injury.
Preoperative MRI demonstrated 11 partial thickness tears (32.4%), 22 full thickness tears (64.7%), and 1 no tear (2.9%) (Table 2). With the modified Sherman classification, preoperative MRI demonstrated 3 type I tears (8.8%), 14 type II tears (41.2%), 14 type III tears (41.2%), and 0 type IV tears, and 1 type V tear (2.9%). One MRI did not identify the ACL as torn (2.9%). The most common tear types seen on MRI were type II and type III (Table 3).
Table 2.
Distribution of tear degree on preoperative magnetic resonance imaging (MRI) versus intraoperatively.
| Degree of tear | Number of tears on MRI (%) | Number of tears intraoperatively (%) |
|---|---|---|
| Partial-thickness tear | 11 (32.4%) | 20 (58.8%) |
| Full-thickness tear | 22 (64.7%) | 14 (41.2%) |
| No tear | 1 (2.9%) | 0 (0.0%) |
Table 3.
Distribution of location of tears found on preoperative magnetic resonance imaging (MRI) versus intraoperatively.
| Location of tear | Number of tears on MRI (%) | Number of tears intraoperatively (%) |
|---|---|---|
| No Tear | 1 (2.9%) | 0 |
| Type I | 3 (8.8%) | 34 (100.0%) |
| Type II | 14 (41.2%) | 0 |
| Type III | 14 (41.2%) | 0 |
| Type IV | 0 (0.0%) | 0 |
| Type V | 2 (5.9%) | 0 |
Intraoperatively, 20 partial thickness tears (58.8%) and 14 full thickness tears (41.2%) were identified. Of the partial tears, 18 were anteromedial bundle tears and 2 were posterolateral bundle tears. All intraoperative partial and full thickness tears were torn proximally at the femoral attachment and thus were classified as Sherman type I tears.
For identifying Sherman type I tears, the sensitivity of MRI was 9.0% (95% CI, 2.0%–24%) and the accuracy of MRI was 8.8%. For identifying full-thickness tears, the sensitivity of MRI was 71.0% (95% CI, 42%–92%), the specificity was 40% (95% CI, 19%–64%), the PPV was 45% (95% CI, 24%–68%), the NPV was 67% (95% CI, 35%–90%), and the accuracy was 53%. Regarding interrater variability, there was moderate agreement between MRI findings for both tear location and tear degree (Table 4). There was poor agreement between the overall MRI findings and intraoperative findings regarding both tear location and tear degree (Table 4).
Table 4.
Interrater variability and percent agreement between magnetic resonance imaging (MRI) and intraoperative findings.
| Interobserver Reliability |
MRI versus Intraoperative Findings |
||||
|---|---|---|---|---|---|
| Fleiss's Kappa | Altman Classification | Cohen's Kappa | Altman Classification | Agreement (%) | |
| Tear Location | 0.547 | Moderate | 0.0 | Poor | 2.9% |
| Tear Degree | 0.541 | Moderate | 0.080 | Poor | 35% |
4. Discussion
This study demonstrates that MRI had poor sensitivity and poor accuracy in identifying Sherman type I tears and good sensitivity and moderate accuracy for identifying full-thickness tears. Additionally, though there was moderate consistency between radiologist interpretation of the MRIs, ultimately, there was poor agreement between the overall MRI findings and intraoperative findings for both tear location (2.9% agreement) and tear degree (35% agreement). The data in this study is consistent with current literature suggesting that MRI is a relatively poor diagnostic tool in localizing and classifying ACL tears.10,11,13,24 Van Dyck et al. retrospectively reviewed 51 MRIs with surgically confirmed partial ACL tears and identified MRI accuracy for diagnosing partial ACL tears was only 25–53%.24 Moreover, they suggest that partial tears are especially difficult to differentiate between mucoid degeneration or normal ACLs.24
Recently, Van der List et al. explored the prevalence of tears based in the Sherman classification in patients with acute primary ACL tears and found mid-substance (or type III) tears to be most common (52%) followed by proximal tears (27%) and proximal avulsions (16%).25 They reported that distal tears and distal avulsions were the least common.25 This present study demonstrated similar findings, with 73.5% of patients having either a type II or type III tear on MRI, which is also consistent with other previously reported findings.7 However, Van der List et al. did not assess the accuracy of their MRI findings with intraoperative findings.25 This study demonstrates that MRI findings may significantly differ from intraoperative findings, with tears that are amenable to repair identified as unrepairable on MRI.
Consistent with previous studies, this present study demonstrates that MRI alone may not be useful in anticipating the potential for ACL repair.26,27 The discrepancy between preoperative and intraoperative findings may prevent surgeons from considering performing primary ACL repairs, as surgeons may not obtain preoperative informed consent if the tear appears to be unamenable to repair on MRI.
Currently, treatment for ACL tears includes non-operative management, reconstruction, and repair. While ACL reconstruction remains the gold standard, ACL repair has gained popularity in recent years. Theorized advantages of ACL repair include maintenance of proprioception, preservation of native insertion sites, avoidance of morbidity associated with autograft harvest, and potential faster recovery.20 Such benefits are believed to better restore normal kinematics and decrease risk of post-traumatic osteoarthritis versus standard ACLR.7,28,29 Moreover, some argue that performing an ACL repair does not “burn any bridges” if the repair needs to be revised into an ACLR.20 However, some authors have identified a significantly higher rate of ACL repair failure versus standard ACLR, especially in the adolescent athletic population.30 Van der list et al. performed a meta-analysis of recent studies regarding ACL repair and identified a failure rate between 7 and 11% and functional outcomes that were greater than 85% of maximum scores, suggesting that ACL repair may be comparable in outcomes to historical outcomes of ACLR.21
Recently, authors have compared repair of proximal ACL tears with ACL reconstruction and found favorable stability and patient reported outcomes in patients with ACL repair.25,31,32 Despite these findings, the option for ACL repair is often disregarded for a multitude of reasons given its historically poor outcomes. Moreover, misclassification of ACL tears as unamenable to repair via MRI may further discourage surgeons from considering ACL repair. Overall, this present study supports the hypothesis that there is a significant degree of variability, especially regarding tear location, between the MRI report and intraoperative arthroscopic findings of ACL tears.
4.1. Limitations
The main limitations of this study include its retrospective nature and small sample size. This study's sample size was limited by the number of ACL repairs that were performed at our institution, as at the time of retrospective review ACL repair was only being performed by one surgeon. Moreover, there were a limited number of patients amenable to repair because Sherman type I tears are not as common as type II and type III tears. This present study's sample size was further limited by a lack of preoperative imaging on file for several ACL repair cases. Due to the limited sample size, generalizability of this study's data to the larger population of ACL tears may be limited.
5. Conclusion
While ACL repair remains a controversial treatment option, this study demonstrates that MRI alone may not necessarily be accurate in identifying which ACL tears are amenable to repair. These results can guide surgeons in their preoperative discussion with their patients when discussing the possibility of repairing a torn ACL.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Henry T. Shu: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Nicholas R. Wegener: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Katherine M. Connors: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Daniel S. Yang: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Stephen D. Lockey: Supervision, Writing – original draft, Writing – review & editing. Jennifer M. Thomas: Data curation, Writing – original draft, Writing – review & editing. Evan H. Argintar: Project administration, Supervision, Writing – original draft, Writing – review & editing.
Acknowledgements
We would like to thank Dr. James Jelinek, MD and Dr. Jordan Gold, MD for their help with reviewing patient MRIs.
Footnotes
Evan Argintar is a paid consultant of Arthrex, Inc. and KCI, Inc. The rest of the authors have no relevant financial relationships to disclose.
References
- 1.Joseph A.M., Collins C.L., Henke N.M., Yard E.E., Fields S.K., Comstock R.D. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810. doi: 10.4085/1062-6050-48.6.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Musahl V., Karlsson J. Anterior cruciate ligament tear. N Engl J Med. 2019;380(24):2341. doi: 10.1056/NEJMcp1805931. [DOI] [PubMed] [Google Scholar]
- 3.Domnick C., Raschke M., Herbort M. Biomechanics of the anterior cruciate ligament: physiology, rupture and reconstruction techniques. World J Orthoped. 2016;7(2):82. doi: 10.5312/wjo.v7.i2.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dargel J., Gotter M., Mader K., Pennig D., Koebke J., Schmidt-Wiethoff R. Biomechanics of the anterior cruciate ligament and implications for surgical reconstruction. Strat Traum Limb Recon. 2007;2(1):1–12. doi: 10.1007/s11751-007-0016-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ostrowski J.A. Accuracy of 3 diagnostic tests for anterior cruciate ligament tears. J Athl Train. 2006 Jan;41(1):120–121. [PMC free article] [PubMed] [Google Scholar]
- 6.Crawford R., Walley G., Bridgman S., Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84:5. doi: 10.1093/bmb/ldm022. [DOI] [PubMed] [Google Scholar]
- 7.Gobbi A., Whyte G.P. Long-term outcomes of primary repair of the anterior cruciate ligament combined with biologic healing augmentation to treat incomplete tears. Am J Sports Med. 2018;46(14):3368. doi: 10.1177/0363546518805740. [DOI] [PubMed] [Google Scholar]
- 8.Lefevre N., Naouri J., Bohu Y., Klouche S., Herman S. Partial tears of the anterior cruciate ligament: diagnostic performance of isotropic three-dimensional fast spin echo (3D-FSE-Cube) MRI. Eur J Orthop Surg Traumatol. 2014;24(1):85–91. doi: 10.1007/s00590-012-1135-4. [DOI] [PubMed] [Google Scholar]
- 9.Roychowdhury S., Fitzgerald S., Sonin A., Peduto A., Miller F., Hoff F. Using MR imaging to diagnose partial tears of the anterior cruciate ligament: value of axial images. AJR.American journal of roentgenology. 1997;168(6):1487. doi: 10.2214/ajr.168.6.9168712. [DOI] [PubMed] [Google Scholar]
- 10.Lawrance J., Ostlere S., Dodd C. MRI diagnosis of partial tears of the anterior cruciate ligament. Injury. 1996;27(3):153–155. doi: 10.1016/0020-1383(95)00220-0. [DOI] [PubMed] [Google Scholar]
- 11.Umans H., Wimpfheimer O., Haramati N., Applbaum Y., Adler M., Bosco J. Diagnosis of partial tears of the anterior cruciate ligament of the knee: value of MR imaging. AJR.American journal of roentgenology. 1995;165(4):893. doi: 10.2214/ajr.165.4.7676988. [DOI] [PubMed] [Google Scholar]
- 12.Dyck P., Smet E., Veryser J. Partial tear of the anterior cruciate ligament of the knee: injury patterns on MR imaging. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):256–261. doi: 10.1007/s00167-011-1617-7. [DOI] [PubMed] [Google Scholar]
- 13.Daniels S., List J., Kazam J., DiFelice G. Arthroscopic primary repair of the anterior cruciate ligament: what the radiologist needs to know. Skeletal Radiol. 2018;47(5):619–629. doi: 10.1007/s00256-017-2857-5. [DOI] [PubMed] [Google Scholar]
- 14.Sherman M., Lieber L., Bonamo J., Podesta L., Reiter I. The long-term followup of primary anterior cruciate ligament repair. Am J Sports Med. 1991;19(3):243–255. doi: 10.1177/036354659101900307. [DOI] [PubMed] [Google Scholar]
- 15.Sandberg R., Balkfors B., Nilsson B., Westlin N. Operative versus non-operative treatment of recent injuries to the ligaments of the knee. A prospective randomized study. J Bone Jt Surg Am Vol. 1987;69(8):1120. [PubMed] [Google Scholar]
- 16.Odensten M., Hamberg P., Nordin M., Lysholm J., Gillquist J. Surgical or conservative treatment of the acutely torn anterior cruciate ligament. A randomized study with short-term follow-up observations. Clin Orthop. 1985;(198):87. [PubMed] [Google Scholar]
- 17.Kaplan N., Wickiewicz T., Warren R. Primary surgical treatment of anterior cruciate ligament ruptures: a long-term follow-up study. Am J Sports Med. 1990 July 1;18(4):354–358. doi: 10.1177/036354659001800404. [DOI] [PubMed] [Google Scholar]
- 18.Burton D.A., Schaefer E.J., Shu H.T., Bodendorfer B.M., Argintar E.H. Primary anterior cruciate ligament repair using internal bracing: a prospective case series of twenty-nine patients. Arthroscopy. 2021;37(4):1235–1241. doi: 10.1016/j.arthro.2020.11.034. [DOI] [PubMed] [Google Scholar]
- 19.DiFelice G.S., van der List, Jelle P. Clinical outcomes of arthroscopic primary repair of proximal anterior cruciate ligament tears are maintained at mid-term follow-up. Arthroscopy. 2018 Apr;34(4):1085–1093. doi: 10.1016/j.arthro.2017.10.028. [DOI] [PubMed] [Google Scholar]
- 20.van Der List J., Difelice G. Primary repair of the anterior cruciate ligament: a paradigm shift. Surgeon. 2017;15(3):161–168. doi: 10.1016/j.surge.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 21.van Der List J., Vermeijden H., Sierevelt I., Difelice G., van Noort A., Kerkhoffs G. Arthroscopic primary repair of proximal anterior cruciate ligament tears seems safe but higher level of evidence is needed: a systematic review and meta-analysis of recent literature. Knee Surg Sports Traumatol Arthrosc : official journal of the ESSKA. 2019 doi: 10.1007/s00167-019-05697-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altman D.G. first ed. Chapman & Hall/CRC; 1991. Practical Statistics for Medical Research. [Google Scholar]
- 23.Shu H.T., Day J., Bodendorfer B.M., Argintar E.H. Anterior cruciate ligament retensioning—a novel revision procedure using suture augmentation. JBJS Case Connector. 2020;10(2) doi: 10.2106/JBJS.CC.19.00092. [DOI] [PubMed] [Google Scholar]
- 24.Van Dyck P., De Smet E., Veryser J. Partial tear of the anterior cruciate ligament of the knee: injury patterns on MR imaging. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):256–261. doi: 10.1007/s00167-011-1617-7. [DOI] [PubMed] [Google Scholar]
- 25.van der List J., Mintz D., DiFelice G. The location of anterior cruciate ligament tears: a prevalence study using magnetic resonance imaging. Orthopaedic Journal of Sports Medicine. 2017;5(6) doi: 10.1177/2325967117709966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mcmillan S., Saini S., Alyea E., Ford E. Office-based needle arthroscopy: a standardized diagnostic approach to the knee. Arthroscopy Techniques. 2017;6(4):e1119–e1124. doi: 10.1016/j.eats.2017.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patel K., Hartigan D., Makovicka J., Dulle D., Chhabra A. Diagnostic evaluation of the knee in the office setting using small-bore needle arthroscopy. Arthroscopy Techniques. 2018;7(1):e17–21. doi: 10.1016/j.eats.2017.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heusdens C., Hopper G., Dossche L., Roelant E., Mackay G. Anterior cruciate ligament repair with Independent Suture Tape Reinforcement: a case series with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):60–67. doi: 10.1007/s00167-018-5239-1. [DOI] [PubMed] [Google Scholar]
- 29.Kiapour A., Murray M. Basic science of anterior cruciate ligament injury and repair. Bone & Joint Research. 2014;3(2) doi: 10.1302/2046-3758.32.2000241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gagliardi A.G., Carry P.M., Parikh H.B., Traver J.L., Howell D.R., Albright J.C. ACL repair with suture ligament augmentation is associated with a high failure rate among adolescent patients. Am J Sports Med. 2019 Mar;47(3):560–566. doi: 10.1177/0363546518825255. [DOI] [PubMed] [Google Scholar]
- 31.Achtnich A., Herbst E., Forkel P. Acute proximal anterior cruciate ligament tears: outcomes after arthroscopic suture anchor repair versus anatomic single-bundle reconstruction. Arthrosc J Arthrosc Relat Surg. 2016;32(12):2562–2569. doi: 10.1016/j.arthro.2016.04.031. [DOI] [PubMed] [Google Scholar]
- 32.DiFelice G.S., Villegas C., Taylor S. Anterior cruciate ligament preservation: early results of a novel arthroscopic technique for suture anchor primary anterior cruciate ligament repair. Arthroscopy. 2015;31(11):2162–2171. doi: 10.1016/j.arthro.2015.08.010. [DOI] [PubMed] [Google Scholar]