Abstract
Rationale
An important public health strategy during the COVID-19 pandemic was the protection of people at risk of severe progressions of an infection; namely, older people and people with pre-existing conditions.
Objective
To improve public health communication, it is vital to understand, which sociodemographic and psychological factors drive older people's acceptance of and compliance with public health measures.
Method
This goal was pursued in this three-wave longitudinal online study with older adults, collected between March and June during the COVID-19 pandemic in 2020 (N = 327; first and second wave during the national lockdown; third wave: after the lifting of most lockdown measures).
Results
The results show that overall acceptance of and adherence to the public health measures were high among older adults and even more so for people with pre-existing conditions (e.g., cancer, type II diabetes). However, some infringements of the measures were observed, and the longitudinal analyses suggest that increases in social trust positively influenced acceptance of measures over time, while trivialising beliefs and health fears impacted older adults’ compliance with protective measures over time.
Conclusions
This study offers insights into the behavioural responses of older adults to an ongoing threat and the associated uncertainty that is part of public communication about the pandemic and protective measures.
Keywords: SARS-CoV-2, COVID-19, Pandemic, Risk perception, Public health, Fear, Behavior change, Health psychology
1. Introduction
On March 16th, 2020, the Federal Council of Switzerland announced an exceptional press conference to address the rapidly rising numbers of patients infected with the SARS-CoV-2 virus (subsequently called COVID-19). Most of Switzerland watched in disbelief as the Federal Council announced the closing of all public schools and universities, restaurants, pubs and bars, skiing areas, and shops apart from supermarkets and pharmacies, and restricted all events with more than five people (Federal Council, 2020). Of particular importance was the protection of those at risk of severe progressions of infection, namely older people and those with pre-existing conditions (Jordan et al., 2020; Kontis et al., 2020; Zhou et al., 2020). Based on the two pillars, social distancing and hygiene, older people were advised to stay at home, refrain from meeting friends and family and adhere to strict hygiene measures when coming into contact with others or leaving the house when it is unavoidable (e.g., medical visits).
As a pandemic is driven by human behaviour, the role of the social sciences has been stressed to offer inputs for making decisions about public health measures and for improving long-term communication with the public (Betsch, 2020; van Bavel et al., 2020). The situation can evolve quickly during the onset of a pandemic (i.e., scientific knowledge about the virus increases, measures are strengthened or loosened). Based on these short-term changes, public acceptance and adherence will likely change as well. Thus, our longitudinal study aimed to examine these dynamic developments over time. For this, established theoretical models on the psychological mechanisms that drive and inhibit people's acceptance and adherence to public health measures were applied to the current situation. The goal was to improve the required understanding of the mechanisms that determine adherence to and acceptance of protective measures to provide a solid basis for interventions in a pandemic (Haushofer and Metcalf, 2020; van Bavel et al., 2020).
2. Theoretical background and research questions and hypotheses
Prior social science and health psychology research suggest several drivers and barriers of protective behaviour and acceptance of measures during a pandemic. The literature on these drivers and barriers was reviewed, and the research questions (RQ) and hypotheses (H) were derived. Established social science theories and models are presented to provide a solid scientific foundation.
2.1. Personal risk perception and risk-as-feelings as key factors for responses to health threats
Primarily, the awareness of risk and the perception of a high likelihood of infection, personal vulnerability to the infection, and severe progression in case of infection are pre-requisites to protective behaviour and higher acceptance of measures (Betsch, 2020; Bish and Michie, 2010; Brug et al., 2009; Bults et al., 2011; van Bavel et al., 2020). Protection Motivation Theory (PMT) proposes that people primarily protect themselves from harm if they perceive a threat as severe and likely to affect them (Rogers, 1975). In a similar vein, the risk-as-feelings model suggests that our responses to threats can be aggravated by our affect and fears, caused by the uncertainty of a risk (Slovic et al., 2004; Slovic and Peters, 2006). Thus, fears over potential impacts for public health and society might substantially change people's responses to pandemics, independent of their personal risk perception (Bish et al., 2011; Fitzpatrick et al., 2020; Kok et al., 2010).
COVID-19 does not affect all people equally but specifically endangers people with pre-existing health conditions or those over 75 years of age (Jordan et al., 2020; Zhou et al., 2020). This has been frequently discussed in public health campaigns and the media and was prominent in the public discourse (Federal Office of Public Health, 2020). Being part of these groups might increase risk awareness and perception substantially. Various authors (Bish and Michie, 2010; Cruwys et al., 2020) have suggested investigating perceived group membership to understand risk perceptions and protective behaviours during the pandemic.
Conversely, personal risk perception might be counteracted by a phenomenon called optimistic bias (Klein and Helweg-Larsen, 2002). Optimistic bias is the erroneous belief that negative events, such as the infection with COVID-19, are less likely to occur to oneself than to others (Cho et al., 2013; Klein and Helweg-Larsen, 2002; van Bavel et al., 2020). A recent study showed that optimism bias coincides with ignoring public health warnings of COVID-19 (Wise et al., 2020). For this reason, it first needs to be established that those individuals most at risk for a severe progression of infection with COVID-19 identified themselves as at risk at the onset of the pandemic:
Another mechanism that might counteract risk awareness and perception is trivialising beliefs regarding one's health status or the likelihood of getting infected (Cho et al., 2013; van Bavel et al., 2020). Cognitive dissonance, a phenomenon first proposed by Festinger (1957), suggests that such trivialising beliefs might counteract risk perception. Cognitive dissonance is caused by at least two pieces of conflicting information, such as the fact that a person is worried about the pandemic, while simultaneously meeting friends and family and failing to socially distance (Festinger, 1957). This state causes an uncomfortable feeling, labelled cognitive dissonance, which can be resolved by changing one's beliefs about the subject. A person might trivialise the risk of getting infected with COVID-19 by meeting friends and family to continue to do so without experiencing the discomfort of cognitive dissonance. Similarly, fears of the impact of safety measures taken (e.g., lockdown, closure of shops and restaurants) might act as a way to relieve cognitive dissonance by putting less weight on fears of the impact on public health. Thus, the following hypothesis was made:
-
•
H3: Trivialising beliefs will negatively impact people's acceptance of and adherence to protective measures.
2.2. Social trust and people's compliance with protective measures
Another key factor for the control of an ongoing pandemic is people's compliance, which involves their acceptance of the measures in place and their behaviours. People are more likely to comply if they trust the government that is issuing the measures and behavioural recommendations (Gilles et al., 2011; Liao et al., 2010; Prati et al., 2011a). In risk research, many definitions and operationalisations of trust have been suggested and recently, a discussion emerged about which type of trust is important for a particular risk (Siegrist et al., 2021; Siegrist and Zingg, 2014). For public responses to pandemics, sustained social trust in the government and other public entities has been suggested as more relevant than confidence (Prati et al., 2011a; Siegrist and Zingg, 2014). Social trust implies that people believe the information that they received is in their best interests and unbiased, which increases acceptance and compliance (Siegrist and Zingg, 2014). Thus, the following hypothesis was made:
-
•
H4: Social trust will positively impact people's acceptance of and adherence to protective measures.
2.3. The dynamic nature and the challenges of social distancing during a pandemic
As a pandemic does not represent a singular risk event but rather presents a dynamic challenge that evolves and interacts with people's behavioural responses, the importance of understanding the mechanisms and shifts in people's perceptions and responses over time has been indicated (Betsch et al., 2020; Haushofer and Metcalf, 2020; van Bavel et al., 2020). Lockdown measures are associated with negative impacts on psychological well-being (Berg-Weger and Morley, 2020; Gonzalez-Sanguino et al., 2020; Mukhtar, 2020; Noone et al., 2020; Sibley et al., 2020). Literature suggests that lockdown and continued social distancing might lead to loneliness and social isolation, particularly for people living alone (Berg-Weger and Morley, 2020; de Leo and Trabucchi, 2020; Flett & Heisel, early view; Noone et al., 2020). As a secondary aim, the article investigated the negative impacts of the lockdown and adhering to social distancing on psychological well-being, namely loneliness.
-
•
RQ2: How did older adults' perceptions and beliefs, loneliness, acceptance of measures, and adherence to protective behaviour evolve over time?
-
•
RQ3: Was a stricter adherence to social distancing measures associated with higher loneliness in older adults and does cohabitation with other people reduce the effect on loneliness?
3. Methodology
3.1. Study design and sample
This article is based on a longitudinal online study in three waves during the COVID-19 pandemic in Switzerland. The first wave (W1) ran from March 27th to April 5th, 2020 and coincided with the lockdown measures that were put in place on March 16th, 2020. In this wave, all gastronomy establishments closed, public transport restrictions were put in place, and there were urgent calls for social distancing (Federal Council, 2020). The second wave (W2) was between April 17th and 26th, 2020, and coincided with the information that the lockdown would be gradually lifted from April 27th, 2020 onwards. The third and final wave (W3) was between May 20th and 29th, 2020 and coincided with the lifting of most lockdown measures, except restaurants and bars, which were not opened until June 8th, 2020.
For the study, all German-speaking participants of the research group's panel who were aged 59 and older (N = 741) were invited to fill out an online questionnaire and a reminder was sent out on April 1st, 2020. The research group's panel was recruited by a) drawing a random sample of postal addresses from the Swiss telephone book and b) via mouth-to-mouth propaganda on our social media account and website. At W1, N = 505 older adults participated (response rate: 68%). Of the 505 participants who were invited at W2, 434 participated (retention rate: 86%) and of the 434 participants invited at W3, 373 participated (retention rate: 73%). For the final sample, only those participants who filled out the questionnaire at all three waves and that could be matched using an ID generated by the participants were considered. This resulted in a final sample of N = 327 participants (n = 226, 69% male participants; M age = 70; SD age = 7; age range: 59–90 years of age). The educational level of the sample was high, with n = 186 (57%) having a university degree. Most participants indicated living with one other person (n = 226, 69%), while n = 79 (23%) indicated living alone and n = 22 (8%) lived with more than two people. A total of 325 (99%) indicated having an outside space in their home (balcony, terrace or garden). Dropout and sensitivity analyses were conducted, which suggested that the dropout was non-systematic and the results robust (see Supplement B Dropout Analysis).
The presented data was collected as part of a larger project, but only the parts of the questionnaire that are of interest for this study's research questions were included. The relevant questionnaire sections for this article can be found in Supplement D Questionnaire. The questionnaire comprised other sections that focused on consumer behaviour during the lockdown (e.g., acceptance of hoarding food and consumer goods, perception of food security). The study was approved by the Ethics Commission of the Federal Institute of Technology (ETH Zurich).
3.2. Materials
To provide guidance, the scales and items included in the analyses are subsequently sorted into the following five categories:
-
•
Identification as risk group and personal risk perception
-
•
Perceptions and beliefs (i.e., trivialising beliefs, social trust, personal fears)
-
•
Loneliness as a measure of psychological well-being
-
•
Acceptance of measures and protective behaviour (i.e., hygiene, social distancing)
-
•
Socio-demographics (age > 75) and pre-existing conditions
Most measures presented subsequently were developed by the authors, and based on methodological recommendations for measuring public risk responses (Lermer et al., 2018), prior literature on public responses to pandemics (Cho et al., 2013; Prati et al., 2011b; Reintjes et al., 2016), the public discourse in Switzerland, and the measures in place (Federal Council, 2020; Federal Office of Public Health, 2020).
3.2.1. Identification as risk group and personal risk perception
Participants were asked to indicate whether they considered themselves in the risk group, labelled as the single-item measure subjective risk group (‘Do you consider yourself to be part of the risk group or do you see yourself as particularly vulnerable concerning the new coronavirus?’ 1: No, not at all, 2: No, rather not, 3: Yes, rather. 4: Yes, certainly. If they did not know, it was coded as missing (n = 4).
Personal risk perception was measured with three single items related to a) likelihood of infection, b) vulnerability to infection and c) severity of illness. The questions were preceded by the following introduction: ‘When answering the following three questions, please think of an average adult person in your community and compare yourself with that person).’ Likelihood of infection was measured by asking ‘Is it more or less likely that you get infected with the new coronavirus than this person?’ from 1: ‘less likely’ to 4: ‘equally likely’ to 7: ‘more likely’. Vulnerability to infection was measured by asking ‘Are you more or less susceptible to getting infected with the new coronavirus than this person?’ with 1 indicating less susceptible, 4 indicating equally susceptibly, and 7 meaning more susceptible. Severity of illness was measured by asking ‘Would an infection with the new coronavirus be more or less severe for you than for this person?’ with a scale from 1: less severe to 4: equally severe and 7: more severe.
3.2.2. Perceptions and beliefs
A scale was developed by the authors to measure trivialising beliefs regarding COVID-19 and infection with the virus. Beliefs were taken from traditional and social media (e.g., comment articles, letters to the editor, forum commentary). The items were preceded by the introduction ‘Please indicate to what extent you agree with the following statements,’ with the response scale ranging from 1 ‘do not agree at all’ to 7 ‘fully agree.’ The trivialising belief scales was unidimensional and was built by taking the mean over all six items (W1: α = 0.73, W2: α = 0.78, W3: α = 0.78; cf. Table A1 in Supplement A).
Four items were created by the authors to measure social trust in the Swiss Federal Office and the pharmaceutical industry. The items were preceded by the following introduction: ‘Please indicate to what extent you agree with the following statements.’ Participants were asked to respond on a scale from 1 ‘do not agree at all’ to 7 ‘fully agree.’ All four items were recoded so that higher values corresponded to higher levels of social trust. The final scale was unidimensional and built by taking the mean over all four items (W1: α = 0.62, W2: α = 0.72, W3: α = 0.80; cf. Table A1 in Supplement A).
A selection of personal fears was assessed in nine items with response options 1: ‘not afraid at all’ to 7: ‘very afraid’ (introduced by ‘Regarding the new coronavirus, I am afraid that … ‘). Principal Component Analysis (PCA) with varimax rotation with the data from W1 suggested a two-factor solution. The first factor (Eigenvalue: 3.0, 33.7% of variance) comprised five items and was labelled ‘health fears.’ The second factor (Eigenvalue: 2.4, 26.7% of variance) comprised four items and was labelled ‘societal fears.’ Both scales had good internal consistency (health fears: W1: α = 0.84, W2: α = 0.85, W3: α = 0.85; societal fears: W1: α = 0.75, W2: α = 0.73, W3: α = 0.77; cf. Table A2 in Supplement A).
3.2.3. Loneliness
Loneliness was measured with the ULS-8 (Hays and DiMatteo, 1987; Russel, 1996). It comprises eight items, introduced by ‘Please indicate to what extent you agree with the following statements’ with a response scale that ranges from 1: ‘Do not agree at all,’ 2: ‘Partly agree,’ 3: ‘Somewhat agree’ to 4: ‘Fully agree.’ One item of the short scale was reverse-coded (‘I can find companionship when I want it.‘) and included in the scale. The scale was unidimensional and exhibited a good internal consistency over all three waves (W1: α = 0.69, W2: α = 0.71, W3: α = 0.74). It was built by taking the mean over all eight items.
3.2.4. Acceptance of measures and protective behaviour
Participants were asked about their acceptance of the measures that were implemented by the government during the pandemic. These items changed from W1/W2 to W3 to do justice to the current situation at the point of data collection. All acceptance items were preceded by the sentence ‘I think it is right that the following measures are implemented in Switzerland.’ The response scales ranged from 1: ‘Do not agree at all’ to 7: ‘Fully agree.’ At W1 and W2, participants were asked about their acceptance of 1) closing all schools, 2) closing all restaurants and bars, 3) advising people not to leave their house, and 4) closing all shops except grocery stores and pharmacies. At W3, participants were asked about the continued and new measures that were implemented at the time, namely 1) continued closure of universities and high schools, 2) fewer tables in restaurants, 3) only a limited number of customers allowed in shops, and 4) large events (e.g., concerts, football matches) not being permitted. An overall acceptance score was calculated by taking the mean over all items with higher scores indicating high levels of overall acceptance of the measures put in place (W1: α = 0.92, W2: α = 0.88, W3: α = 0.69; cf. Table A3 in Supplement A).
Several protective behaviour items were developed based on the recommendations to increase hygiene measures and enforce social distancing (Federal Council, 2020; Federal Office of Public Health, 2020), leading to two behavioural indexes with protective measures (i.e., social distancing and hygiene behaviour). The participants were asked whether the different activities took place in the past seven days with ‘Yes,’ ‘No,’ and ‘Do not know’ (verbatim introduction: When you think of the last seven days, which of the following activities applies to you?’ verbatim items: Figure A1 and A2 in Supplement A). The two indexes were built by recoding people's responses as outlined subsequently and taking the sum of all items for each participant. For adherence to hygiene measures, all ‘Yes’ responses were coded as 1 and all responses ‘No’ and ‘Do not know’ were coded as 0. Thus, higher values on the index from 0 to 7 correspond to more cautious hygiene behaviour. For the adherence to social distancing, all ‘No’ responses were coded as 1, and all ‘Yes and ‘Do not know’ responses were coded as 0. Thus, higher values on the index from 0 to 9 correspond to more social distancing behaviour. These items measured diverse behaviours that are not necessarily correlated substantially, which is why no Cronbach's alpha is reported.
Older people were advised to remain at home during W1 (Federal Council, 2020; Federal Office of Public Health, 2020). Hence, at W1, participants were also asked whether they had left their homes in the past seven days for other reasons than to visit the doctor (verbatim question: ‘Have you left your home in the last seven days for reasons other than visiting the doctor?’ 1: Yes, 2: No, 3: Do not know) and what their reasons were for leaving the house (‘You indicated that you have left your home in the last seven days. What was the reason for leaving your home?‘).
3.2.5. Socio-demographics and aggravating conditions
At W1, participants were asked for their age, sex, and educational level. Age was recoded into two groups: 1) 59–74 years of age (n = 237) and 2) over 75 years of age (n = 87). Furthermore, the participants were asked to indicate whether they had any pre-existing health conditions (‘Do you have any of the following health conditions [please tick all that apply]?‘). They were then provided with a list of health conditions that were associated with severe progressions of infections with COVID-19 and were asked to tick each health condition that applied to them (Federal Office of Public Health, 2020). Based on their responses, participants were grouped into ‘no health condition’ (coded as 0, n = 163) and ‘at least one health condition’ (coded as 1, n = 164). Lastly, participants were asked at W1 whether they lived alone or with other people (verbatim question: ‘How many adults/children live in your household (including yourself?‘) and whether they had access to an outside space in their homes (verbatim question: ‘What possibilities do you have to go outside without leaving your home?‘).
3.3. Data analysis
All descriptive and multivariate analyses were conducted in SPSS 26.0 (IBM Corp, 2017). Before the analysis, the assumptions of each respective test were checked. Descriptive analyses produced the absolute and relative distributions, means, and standard deviations. For RQ1, Chi2-tests and independent t-tests were used to investigate the impact of aggravating conditions on identification with the risk group and risk perception. For RQ2, repeated-measures ANOVAs were conducted to check for differences between W1 and W3. For RQ3, bivariate correlations and one-way ANOVAs checked for the impact of social distancing and cohabiting with other people on loneliness. For hypothesis testing (H1–H4), linear regression analyses investigated the relationships among aggravating conditions, perceptions and beliefs, and acceptance of measures and protective behaviour. The data of W1 and W3 were used to conduct a longitudinal analysis by including the predictors from W1 and the change scores from W1 to W3 as the independent variables and the variables from W3 as dependent variables. Cut-off values for effect sizes are based on Cohen (1977) and Lakens (2013).
4. Results
4.1. RQ1: personal risk perception and identification with the risk group at the onset of the pandemic
The following analyses focusing on RQ1 are based on the data that was gathered at W1, directly after the announcement of the lockdown. Participants with pre-existing health conditions were more likely to perceive themselves as part of the risk group than participants without pre-existing health conditions (χ2(3) = 63.48, p < .001, γ = 0.66). Of the 162 participants with pre-existing health conditions, 126 participants (78%) indicated to rather or certainly being part of the risk group, whereas 36 (22%) indicated to rather not or not being part of the risk group (2 indicated that they did not know). Of the 162 participants without pre-existing health conditions, 67 participants (41%) indicated to rather or certainly being part of the risk group and 95 (59%) indicated to rather not or not being part of the risk group (1 indicated that he/she did not know). There was a statistically significant relationship between age group and the variable subjective risk group, χ2(3) = 30.30, p < .001, γ = 0.44. Participants of 75 years and older identified themselves significantly more frequently as part of the risk group than participants between 59 and 74 years of age. The Goodman-Kruskal gamma suggests strong positive associations between having a pre-existing health condition, age, and subjective risk group (Rea and Parker, 1992).
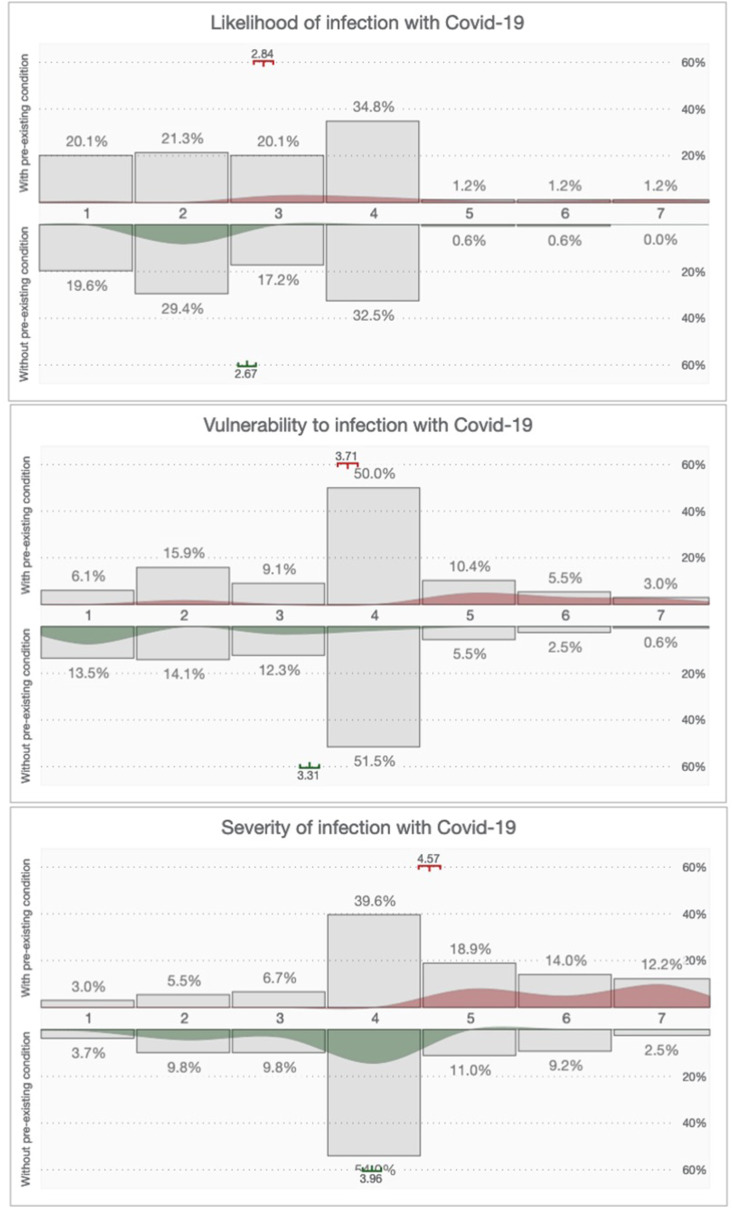
There were no significant differences between participants with and without pre-existing conditions for perceived likelihood of infection with COVID-19 (t(325) = 1.26, p = .210, d = 0.14), but there were significant differences for vulnerability (t(325) = 2.76, p = .006, d = 0.30) and severity (t(318) = 4.05, p < .001, d = 0.92). Effect sizes (Cohen's d) suggest small effects of pre-existing condition on the likelihood of infection with COVID-19, small to medium effects on vulnerability and a large effect on severity (Lakens, 2013). Participants with pre-existing conditions perceived themselves more vulnerable to an infection with COVID-19 and also perceived the severity of a potential infection as higher than participants without pre-existing conditions (see Fig. 1 ). No significant age differences were observed for likelihood of infection t(325) = 0.12, p = .903, d = 0.02, vulnerability, t(325) = 0.54, p = .536, d = 0.07, or severity, t(135) = −0.69, p = .495, d = 0.09. Effect sizes (Cohen's d) were small for all three variables.
Fig. 1.
V-Plot of likelihood of infection, vulnerability to infection and severity of illness with COVID-19, separated by pre-existing condition at W1 (Blumenschein et al., 2020). Grey bar-chart: relative distribution of responses; coloured distribution: difference distribution between participants with and without pre-existing condition; mean and standard error per group.
4.2. R2: changes in older adults’ lives over time
The most substantial increases over time according to large effect sizes (η2) were observed for trivialising beliefs (see Table 1 ). The most substantial decreases over time according to large effect sizes (η2) were observed for health fears. Furthermore, perceived likelihood of infection increased from W1 to W3 (medium effect), vulnerability to infection decreased from W1 to W3 (small effect), while severity of illness remained stable (small effect). Loneliness remained stable at W1 and W2, then decreased at W3 after the lifting of lockdown measures (small to medium effect).
Table 1.
Changes in older adults’ lives over the three waves (N = 327; W1–W3; different subscript letters indicate significant differences according to Bonferroni-corrected post hoc tests).
| W1 |
W2 |
W3 |
||||||
|---|---|---|---|---|---|---|---|---|
| W1 to W2 | W2 to W3 | M [95%CI] | M [95%CI] | M [95%CI] | F (df)1 | p | η2 | |
| Personal risk perception | ||||||||
| Likelihood of infection (1–7) | < | = | 2.76 [2.62, 2.89]a | 3.10 [2.97, 3.24]b | 3.21 [3.08, 3.34]b | 16.91 (2, 652) | <.001 | .05 |
| Vulnerability to infection (1–7) | < | = | 3.51 [3.37, 3.66]a | 3.70 [3.56, 3.85]bc | 3.61 [3.48, 3.74]ac | 3.38 (2, 631) | .035 | .01 |
| Severity of illness (1–7) | = | = | 4.27 [4.12, 4.42]a | 4.34 [4.18, 4.50]a | 4.28 [4.14, 4.43]a | 0.56 (2, 652) | .555 | .00 |
| Perceptions and beliefs | ||||||||
| Trivialising beliefs (1–7) | < | < | 2.87 [2.75, 3.00]a | 3.07 [2.93, 3.21]b | 3.48 [3.34, 3.62]c | 37.41 (2, 652) | <.001 | .17 |
| Social trust (1–7) | > | < | 6.32 [6.22, 6.41]a | 6.10 [5.99, 6.21]b | 6.27 [6.16, 6.38]a | 13.46 (2, 626) | <.001 | .04 |
| Health fears (1–7) | > | > | 3.89 [3.76, 4.02]a | 3.27 [3.15, 3.40]b | 2.93 [2.81, 3.05]c | 165.16 (2, 640) | <.001 | .34 |
| Societal fears (1–7) | > | = | 4.02 [3.88, 4.15]a | 3.82 [3.69, 3.95]b | 3.78 [3.65, 3.92]b | 8.25 (2, 652) | <.001 | .03 |
| Psychological well-being | ||||||||
| Loneliness (1–4) | = | > | 2.51 [2.46, 2.56]a | 2.51 [2.46, 2.56]a | 2.42 [2.36, 2.47]b | 11.25 (2, 652) | <.001 | .03 |
| Acceptance and adherence to protective behaviour | ||||||||
| Acceptance of measures (1–7)2 | > | 5.91 [5.74, 6.07]a | 5.67 [5.51, 5.83]b | 5.69 [5.57, 5.80] | 8.28 (1, 326) | .004 | .03 | |
| Hygiene measures (0–7) | = | < | 3.31 [3.15, 3.47]ab | 3.28 [3.12, 3.45]a | 3.50 [3.33, 3.67]b | 5.08 (2, 639) | .007 | .02 |
| Social distancing (0–9) | > | > | 7.71 [7.59, 7.83]a | 7.40 [7.26, 7.55]b | 6.04 [5.87, 6.21]c | 287.13 (2, 566) | <.001 | .47 |
Note. 1 where the assumption of sphericity had been violated (Mauchly's Test), Greenhouse-Geisser corrected tests are reported. 2 items at at W3 differed from items at W1 and W2 due to the lifting of lockdown. Thus, only values at W1 and W2 were compared.
Changes in the acceptance of measures from W1 and W2 to W3 were not investigated as the items were changed to account for the evolving situation in Switzerland and were not able to be directly compared (cf. Table A3 in Supplement A). For the measures in place during W1 and W2, comparable levels of acceptance were observed, with the highest acceptance for the closing of restaurants and bars. At W3, acceptance of the continued closure of universities and high schools was notably lower than acceptance for the other measures.
The adherence to hygiene measures increased (small effect), while the adherence to social distancing decreased over time (large effect). At W1, 80% more strictly adhered to eight out of nine social distancing measures (e.g., not receiving visits from relatives, not gathering in large groups). However, almost 60% of the older adults still went to the store and supermarket themselves at W1 and W2, despite officially being advised against this. Moreover, at W1, a total of 250 (77%) of the participants indicated having left their homes in the past seven days. When asked the reason, 54% indicated being unable to always stay inside (n = 134), 52% indicated wanting to go shopping for themselves (n = 129), 29% indicated to be healthy and thus, not being obliged to stay home (n = 72), and lastly, 10% indicated needing to be among people for their well-being (n = 24). Most notable decreases in adherence to social distancing between W1 and W3 were observed for going to the supermarket or store and for being visited by children and other people. For adherence to hygiene measures, the results were more mixed. At W1, most participants (around 70%) indicated washing their hands after receiving deliveries, using disinfectant for cleaning the hands, and washing their hands after touching the mail. Participants were more divided regarding the other measures. In particular, wearing a face mask was rather uncommon at W1, but increased to roughly 30% in W3.
4.3. R3: The impact of social distancing on loneliness
The adherence to social distancing measures was not associated with self-reported loneliness during any of the three waves (W1: r = 0.00, p = .950; W2: r = 0.02, p = .724; W3: r = −0.05, p = .377). However, living alone or with other people had a significant effect on loneliness at all three waves (W1: F(2, 324) = 7.55, p < .001, η2 = 0.05; W2: F(2, 324) = 3.62, p = .028, η2 = 0.02; W3: F(2, 324) = 3.38, p = .035, η2 = 0.02). Effect sizes ranged from small to medium (Cohen, 1977). At all three times, people that lived alone expressed the highest levels of loneliness (W1: M = 2.67, 95% CI[2.57, 2.76]; W2: M = 2.63, 95% CI[2.53, 2.73]; W3: M = 2.53, 95% CI[2.43, 2.64]) compared to those cohabiting with one (W1: M = 2.48, 95% CI[2.42, 2.54]; W2: M = 2.47, 95% CI[2.41, 2.53]; W3: M = 2.39, 95% CI[2.33, 2.45]) or more people (W1: M = 2.31, 95% CI[2.12, 2.50]; W2: M = 2.48, 95% CI[2.41, 2.53]; W3: M = 2.30, 95% CI[2.10, 2.50]).
4.4. H1 to H4: The barriers and drivers of older adults’ acceptance of and adherence to protective measures
The three risk perception measures were excluded from the regression analyses, as they were strongly correlated with health fears and trivialising beliefs (cf. Supplement C Bivariate correlations). Moreover, health fears might be a more reliable measure for risk perception than personal risk perception. This was particularly the case during the lockdown, as likelihood of getting infected depended on people's behaviour (i.e., strict social distancing reduced perceived likelihood of infection, while fear of getting infected might still be high). Table 2, Table 3, Table 4 present the results of the linear regression analyses with acceptance of and adherence to protective behaviour as dependent variables.
Table 2.
Linear regression with acceptance of the measures put in place by the Swiss government as dependent variable (cross sectional, w1-w3, N = 323).
| B (SE) | w1 β | t | B (SE) | w2 β | t | B (SE) | w3a β | t | |
|---|---|---|---|---|---|---|---|---|---|
| Constant | 4.15 (0.94) | 4.41*** | 3.38 (0.90) | 3.73*** | 3.61 (0.95) | 3.81*** | |||
| Sex (0: male, 1: female) | −0.12 (0.17) | -.04 | −0.71 | −0.05 (0.17) | -.02 | −0.32 | 0.22 (0.12) | .10 | 1.82 |
| Age group (0: 59–74 years, 1: 75–90 years) | −0.25 (0.18) | -.07 | −1.36 | −0.02 (0.18) | -.01 | −0.10 | 0.01 (0.01) | .01 | 0.20 |
| Subjective risk group (0: part of, 1: not part of) | −0.17 (0.19) | -.05 | −0.90 | −0.18 (0.18) | -.06 | −1.01 | 0.01 (0.14) | .01 | 0.06 |
| Pre-existing condition (0: present, 1: not present) | 0.15 (0.17) | .05 | 0.86 | 0.03 (0.16) | .01 | 0.16 | −0.04 (0.12) | -.02 | −0.31 |
| Trivialising beliefs | −0.29 (0.08) | -.22 | −3.59*** | −0.20 (0.08) | -.16 | −2.64** | −0.13 (0.06) | -.15 | −2.43* |
| Social trust | 0.41 (0.10) | .23 | 4.16*** | 0.43 (0.09) | .25 | 4.59*** | 0.27 (0.07) | .22 | 4.05*** |
| Health Fears | 0.20 (0.08) | .16 | 2.56* | 0.22 (0.08) | .18 | 2.85** | 0.16 (0.06) | .19 | 2.96** |
| Societal Fears | −0.03 (0.07) | -.03 | −0.44 | −0.09 (0.07) | -.07 | −1.24 | −0.08 (0.05) | -.09 | −1.48 |
Note. w1: R2 = 0.19, F(8, 315) = 9.21, p < .001. w2: R2 = 0.18, F(8, 315) = 8.60, p < .001. w3: R2 = 0.16, F(8, 315) = 7.69, p < .001.
***: p < .001, **: p < .01, *: p < .05.
Different items at w3 due to partial lifting of lockdown.
Table 3.
Linear regression with adherence to hygiene measures in the past 7 days as dependent variable (cross-sectional, W1–W3, N = 323).
| W1 |
W2 |
W3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | Β | t | B (SE) | β | t | B (SE) | β | t | |
| Constant | 3.33 (0.97) | 3.45** | 3.96 (1.00) | 3.95*** | 2.51 (1.03) | 2.09* | |||
| Sex (0: male, 1: female) | −0.16 (0.18) | -.05 | −0.91 | −0.35 (0.19) | -.11 | −1.89 | −0.07 (0.19) | -.02 | −0.38 |
| Age group (0: 59–74 years, 1: 75–90 years) | −0.15 (0.19) | -.05 | −0.81 | −0.27 (0.19) | -.08 | −1.41 | 0.12 (0.20) | .04 | 0.62 |
| Subjective risk group (0: part of, 1: not part of) | −0.15 (0.19) | -.05 | −0.75 | −0.24 (0.20) | -.08 | −1.19 | −0.12 (0.21) | -.04 | −0.57 |
| Pre-existing condition (0: present, 1: not present) | 0.27 (0.17) | .09 | 1.57 | 0.06 (0.18) | .02 | 0.34 | −0.01 (0.19) | -.01 | −0.05 |
| Trivialising beliefs | −0.13 (0.08) | -.10 | −1.58 | −0.17 (0.09) | -.13 | −2.04* | −0.12 (0.09) | -.09 | −1.42 |
| Social trust | 0.05 (0.10) | .03 | 0.52 | −0.08 (0.10) | .04 | 0.74 | 0.17 (0.11) | .09 | 1.62 |
| Health Fears | 0.19 (0.08) | .16 | 2.36* | 0.14 (0.09) | .11 | 1.67 | 0.21 (0.09) | .16 | 2.41* |
| Societal Fears | −0.07 (0.08) | -.06 | −0.87 | −0.02 (0.08) | -.02 | −0.30 | −0.02 (0.08) | -.02 | −0.30 |
Note. W1: R2 = 0.06, F(8, 315) = 2.44, p = .023. W2: R2 = 0.07, F(8, 315) = 3.06, p < .001. W3: R2 = 0.07, F(8, 315) = 2.79, p < .001.
***p < .001, **p < .01, *p < .05.
Table 4.
Linear regression with adherence to social distancing in the past 7 days as dependent variable (cross-sectional, W1–W3, N = 323).
| W1 |
W2 |
W3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | Β | t | B (SE) | β | t | B (SE) | β | t | |
| Constant | 7.87 (0.71) | 11.12*** | 7.83 (0.84) | 9.32*** | 5.50 (0.99) | 5.55*** | |||
| Sex (0: male, 1: female) | −0.22 (0.13) | -.09 | −1.63 | 0.01 (0.16) | .01 | −0.03 | −0.20 (0.18) | -.06 | −1.07 |
| Age group (0: 59–74 years, 1: 75–90 years) | 0.32 (0.14) | .12 | 2.23* | 0.30 (0.16) | .10 | 1.83 | 0.49 (0.19) | .14 | 2.55* |
| Subjective risk group (0: part of, 1: not part of) | −0.49 (0.14) | -.21 | −3.45** | −0.32 (0.17) | -.12 | −1.89 | −0.26 (0.20) | -.08 | −1.33 |
| Pre-existing condition (0: present, 1: not present) | 0.19 (0.13) | .08 | 1.48 | 0.05 (0.15) | .02 | −0.33 | −0.13 (0.18) | -.04 | −0.72 |
| Trivialising beliefs | −0.11 (0.06) | -.11 | −1.76 | −0.16 (0.07) | -.14 | −2.18* | −0.15 (0.08) | -.11 | −1.80 |
| Social trust | 0.09 (0.07) | .07 | 1.19 | −0.02 (0.09) | -.02 | −0.28 | 0.08 (0.10) | .05 | 0.80 |
| Health Fears | 0.19 (0.06) | .21 | 3.23** | 0.22 (0.07) | .20 | 3.01** | 0.24 (0.08) | .19 | 2.81** |
| Societal Fears | −0.17 (0.06) | -.18 | −3.07** | −0.15 (0.07) | -.14 | −2.27* | −0.09 (0.08) | -.08 | −1.22 |
Note. W1: R2 = 0.18, F(8, 315) = 8.35, p < .001. W2: R2 = 0.12, F(8, 315) = 5.24, p < .001. W3: R2 = 0.12, F(8, 315) = 5.28, p < .001.
***: p < .001, **: p < .01, *: p < .05.
High social trust and high health fears increased, and high trivialising beliefs decreased the acceptance of measures during all three waves. At all three waves, the highest β-values were observed for social trust. For trivialising beliefs, the β-values were largest at W1 and smaller at W2 and W3. Conversely, the β-values for health fears were largest at W3. Societal fears, age, subjective risk group, and having a pre-existing condition were not associated with higher acceptance at any of the three waves and β were near 0. Overall, more variance could be explained in social distancing behaviour compared to hygiene behaviour. Health fears exhibited a positive association (in W1 and W3) and trivialising beliefs a negative association with hygiene behaviour (in W2). All other independent variables exhibited β-values near 0. Different predictors were found for social distancing during the three waves. At W1 and W2, health fears increased, while societal fears reduced the adherence to social distancing. At W3, only health fears determined the adherence to social distancing; all other independent variables exhibited β-values near 0. At W1, members of the subjective risk group expressed more social distancing compared to participants who did not consider themselves part of the risk group. Overall, older people expressed more adherence to social distancing.
Table 5 exhibits the longitudinal relationships for acceptance of measures, adherence to hygiene measures and social distancing at W3. For all three variables prior acceptance and adherence at W1 was related to the acceptance and adherence at W3. It should be noted that the items for acceptance were different from W1 to W3. Nonetheless, they were strongly related, suggesting that participants who accepted the lockdown measures were also more likely to accept the measures taken after the lockdown. People with higher social trust and whose social trust increased over time expressed higher levels of acceptance. An increase in trivialising beliefs from W1 to W3 was associated with lower acceptance of the measures at W3. Adherence to hygiene behaviour at W3 was most strongly determined by prior behaviour. However, health fears and an increase in health fears were also associated with more hygiene behaviour. An increase in societal fears was associated with less hygiene behaviour. Adherence to social distancing was most strongly determined by prior social distancing behaviour at W1. Higher levels of and an increase in trivialising beliefs were associated with lower adherence to social distancing.
Table 5.
Linear regression with acceptance of measures, adherence to hygiene and social distancing in the past 7 days at W3 as dependent variables (longitudinal, N = 323).
| Acceptance of measures |
Hygiene measures |
Social distancing |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B (SE) | β | t | B (SE) | β | t | B (SE) | β | t | |
| Constant | 1.85 (0.89) | 2.09* | −0.29 (1.26) | −0.23 | 2.44 (1.45) | 1.68 | |||
| Acceptance of measures W1/Hygiene measures W1/Social distancing W1 | 0.13 (0.04) | .19 | 3.64*** | 0.56 (0.05) | .52 | 11.58*** | 0.48 (0.07) | .35 | 6.35*** |
| Sex (0: male, 1: female) | 0.23 (0.11) | .10 | 2.13* | 0.05 (0.15) | .02 | 0.33 | −0.06 (0.17) | -.02 | −0.36 |
| Age group (0: 59–74 years, 1: 75–90 years) | 0.01 (0.01) | .04 | 0.74 | 0.01 (0.01) | .04 | 0.90 | 0.01 (0.01) | .03 | 0.47 |
| Subjective risk group (0: part of, 1: not part of) | 0.01 (0.12) | .00 | 0.06 | −0.04 (0.17) | -.01 | −0.21 | −0.04 (0.19) | -.01 | −0.20 |
| Pre-existing condition (0: present, 1: not present) | −0.01 (0.10) | -.01 | −0.14 | −0.13 (0.15) | -.04 | −0.88 | −0.20 (0.17) | -.07 | −1.21 |
| Trivialising beliefs | −0.09 (0.06) | -.10 | −1.69 | −0.05 (0.08) | -.04 | −0.64 | −0.19 (0.09) | -.14 | −2.14* |
| Change score: Trivialising beliefs | −0.14 (0.05) | -.13 | −2.51* | −0.12 (0.08) | -.08 | −1.60 | −0.29 (0.09) | -.19 | −3.35** |
| Social trust | 0.38 (0.07) | .31 | 5.61*** | 0.15 (0.09) | .08 | 1.59 | 0.01 (0.10) | .00 | 0.07 |
| Change score: Social trust | 0.46 (0.06) | .37 | 7.32*** | 0.01 (0.09) | .01 | 0.12 | 0.03 (0.10) | .02 | 0.34 |
| Health Fears | 0.08 (0.06) | .09 | 1.36 | 0.31 (0.09) | .24 | 3.65*** | 0.15 (0.10) | .12 | 1.61 |
| Change score: Health fears | −0.01 (0.06) | -.01 | −0.22 | 0.43 (0.09) | .28 | 5.00*** | 0.10 (0.09) | .07 | 1.08 |
| Societal Fears | 0.00 (0.05) | .00 | 0.08 | −0.08 (0.08) | -.06 | −1.00 | −0.02 (0.08) | -.02 | −0.28 |
| Change score: Societal fears | 0.05 (0.05) | .06 | 1.05 | −0.17 (0.07) | -.13 | −2.41* | −0.06 (0.08) | -.04 | −0.73 |
Note. Acceptance of measures: R2 = 0.36, F(13, 310) = 13.58, p < .001. Adherence to hygiene measures: R2 = 0.41, F(13, 310) = 16.57, p < .001. Adherence to social distancing: R2 = 0.26, F(13, 310) = 8.26, p < .001.
***p < .001, **p < .01, *p < .05.
5. Discussion and implications
5.1. Summary and theoretical directions for future acceptance of public health measures
This study shows that the overall acceptance of measures and adherence to protective behaviours was rather high among older adults in our sample (see Table 1). This pattern might suggest that the public risk communication measures might have reached a large proportion of the participants. The respondents with pre-existing conditions exhibited a higher identification with the risk group and thus, perceived themselves personally at risk (see Fig. 1). Similarly, the threat of suffering a severe progression of illness was perceived as high and as personally relevant. Our results also show that the lockdown might have had temporary negative impacts on the psychological well-being of older adults, namely their loneliness. Our results provide a snapshot of the mechanisms determining people's initial reaction to a pandemic in a country that has never been affected in this way.
As the crisis is ongoing and a variety of public health measures are controversially discussed in public discourse, perceptions and attitudes will likely increase in importance for people's acceptance of and adherence to protective measures. Thus, it becomes even more important to systematically investigate people's reactions to the pandemic, as well as their reactions to short- and long-term measures taken to tackle its negative impact (i.e., lockdowns, vaccines). A theoretical frame that might be useful for this is the Secondary Risk Theory (Cummings et al., 2020), based on the Protection Motivation, which puts risk perception and the ability to cope with the risk at its core (Rogers, 1975). The Secondary Risk Theory also allows for incorporating secondary risks, meaning the investigation of people's perceptions of measures taken against the primary risk (Cummings et al., 2020). Based on our findings and other recent literature (Nivette et al., 2021; Ye and Lyu, 2020), we recommend considering social trust when applying the model as it was most strongly related to people's acceptance of the measures in place and might also guide their acceptance of the vaccine.
5.2. Influential factors for the public's adherence to public health measures
In accordance with high threat awareness, adherence to protective measures was high at the onset of the pandemic. However, some infringements compared to the official recommendations were revealed (Federal Council, 2020; Federal Office of Public Health, 2020). Older adults were asked not to leave their homes, not even for shopping, and particularly not in crowded environments. Yet, a large proportion of participants indicated having left their homes for shopping or other activities apart from going to the doctor. In our sample, no direct relationship between adherence to social distancing and loneliness was observed. However, most of our participants lived with a partner and had access to outside spaces, which might have alleviated the negative impact of social distancing on psychological well-being. Strict social distancing might still be a challenging measure, particularly for older people, as other studies have shown links to loneliness, lower physical and psychological well-being, anxiety, and psychological distress (Flett & Heisel, early view; Gonzalez-Sanguino et al., 2020; Xie et al., 2020).
In our study, living alone was associated with higher levels of loneliness. Among other reasons for leaving their homes, being independent and being able to buy groceries themselves was important to most participants. Similar issues were also discussed in other articles, for example under the theoretical framework of ‘mattering’ (i.e., the feeling of being important to others) or psychological well-being (Flett & Heisel, early view; Miller, 2020; Tang et al., 2020). The onset of the pandemic was accompanied by several altruistic and communal initiatives to buy groceries for older people or to simplify their access to online shops and delivery. Yet not all older people were able to benefit from these initiatives for a variety of reasons (e.g., living in an isolated area, being unwilling to accept help, being unaware of initiatives).
Additionally, the lack of social interactions was perceived as challenging. While younger people might be more adaptable at compensating by socialising via digital means, older people might find this more difficult and less accessible (Noone et al., 2020; Xie et al., 2020). Older people's social networks are smaller than those of younger people, which might have been aggravated by the closure of public meeting places (e.g., cafés and bars, club activities, sporting clubs) (Cornwell et al., 2008; Gonzalez-Sanguino et al., 2020; Noone et al., 2020; Wrzus et al., 2013). Future studies should investigate the role of older people's social networks, which might be smaller but also stronger than those of younger people, in light of their abilities to cope with lockdown measures. A recent study in Ireland showed the importance of staying active (e.g., walking outdoors, pursuing hobbies) for affective benefits and psychological well-being (Lades et al., 2020).
There existed some uncertainty regarding hygiene measures among the older adults in this study. Most participants adhered to the suggestion of washing and sanitising their hands after receiving goods, while others exhibited more intense hygiene measures, such as washing or disinfecting food and food packaging. Particularly, during the onset of the pandemic in Switzerland much uncertainty existed regarding the transmission pathways of COVID-19 (Eddy et al., 2020; Setti et al., 2020; Yuksel et al., 2020) and this might have led to some participants exhibiting more careful behaviour than others. A third of participants indicated that they did not disinfect their hands, and only 4% indicated that they had worn a mask to protect themselves. While this is mostly explainable by the low availability of masks and staying at home, this might also partly be an effect of the initial communication by the Federal Office of Public Health that masks did not offer protection from COVID-19 (Loser, 2020).
When interpreting the results regarding some of the hygiene measures, it is important to keep in mind that, despite some exceptions, people were mostly at home, which made it unnecessary to use disinfectant and wear a facemask. This is suggested by the changes in behaviour at W3, as in this wave, roughly a third of the respondents indicated having worn a face mask in public, which corresponded with a decrease in social distancing. Similarly, these changes in behavioural patterns explain the differences in relevant predictors over the three waves.
Some factors were found to counteract the acceptance of measures and adherence to protective behaviour (see Table 2, Table 3, Table 4, Table 5). As predicted in H4, social trust impacted people's acceptance of the measures longitudinally and their adherence to protective behaviour in most waves. Health fears (H2) were important motivators of protective behaviour, particularly hygiene behaviour longitudinally, and increased acceptance of measures. Trivialising beliefs (H3) regarding the own health status had a negative effect on the willingness to social distance in the longitudinal analysis (see Table 5). It is relevant that the adherence to social distancing at W1 and W2 was additionally negatively impacted by societal fears such as those regarding the economy.
5.3. Limitations and implications for further research
Some limitations of this study must be discussed. First, the included socio-demographic and psychological variables did not explain large amounts of variance in protective behaviour. However, particularly at the onset of the pandemic, there were only a few opportunities to infringe on social distancing rules, by, for example, receiving visits from the family, going grocery shopping, or walking in crowded environments. The theoretical foundation of this study was based on prior research of risk perception and of more localised outbreaks (e.g., Barr et al., 2008; Brug et al., 2009; Jones and Salathe, 2009; Sadique et al., 2007) and on social science theories and frameworks (Festinger, 1957; Klein and Helweg-Larsen, 2002; Prati et al., 2011b; Rogers, 1975). Future studies should build on this to expand the knowledge and incorporate relevant factors from other fields of research (see e.g., Gibson Miller et al., 2020; Lades et al., 2020; Marinthe et al., 2020; Preis et al., 2020; van Bavel et al., 2020; Yuksel et al., 2020). Moreover, experimental approaches can offer insights where communication efforts can and cannot improve people's adherence to protective measures (Felgendreff et al., 2021; Lunn et al., 2020).
Second, the sample was recruited from a pool of highly educated participants that had access to the internet from the research panel of our group. It is possible that the trivialising beliefs and the adherence to protective behaviour would have been different in a representative sample with more varied educational backgrounds or in a sample where older people were included that did not have access to the internet (in Switzerland: 79% of 60–69-year-olds and 53% of those 70 and older have internet access (Federal Statistical Office, 2020)). However, education did not impact any of the variables of interest, which suggests that the impact of educational background on our variables might be small. Nonetheless, it is important to stress that studies suggest that people with lower socio-economic status are disproportionally affected by the COVID-19 pandemic (e.g., Blundell et al., 2020; Patel et al., 2020). Thus, our study might overestimate the acceptance of and compliance with measures, as well as underestimate the negative impacts of the pandemic, particularly on older adults’ psychological well-being. Future studies should focus on recruiting a more heterogeneous sample regarding socio-economic status or specifically tackling vulnerable groups (i.e., according to education or income). Although our findings can likely be transferred to other European countries with similar measures in place, future studies should aim at conducting cross-cultural studies to look into ways to improve the public response of more individualistic societies to public health measures (e.g., wearing a mask).
Third, we did not differentiate between participants who lived at home or in a senior home facility, as this information was not gathered. Yet, it is likely that these two groups of older adults are faced with different challenges during the lockdown and ongoing pandemic. Fourth, participants may have considered their behaviour when judging the risk of infection or personal vulnerability. An older adult who strictly adheres to social distancing and hygiene measures minimises their exposure to COVID-19 and might rightfully have a low-risk perception of infection. The directionality of risk perceptions and protective behaviours, as well as the maintenance of these protective behaviours over time, should be clarified in future studies.
Fifth, the measures of acceptance were adjusted between the first two waves and the third wave to do justice to the evolving situation in Switzerland. This is an inherent challenge for this area of research. Overall measurement of people's acceptance of measures in an open format (e.g., ‘I think the measures currently implemented in Switzerland are good.‘) could potentially tackle this issue. However, overall measurement of acceptance requires that people are aware of the measures currently in place and all participants think of the same measures when responding. For this reason, we have decided that measuring people's acceptance of specific measures, rather than an overall assessment, is more valid and more reliable despite the issue of limited comparability.
Finally, the sample size was comparably small regarding the various data analyses that were conducted. The findings with small effect sizes should be interpreted with caution.
6. Conclusions
The present study makes the following contributions to the growing literature on people's reactions to the global COVID-19 pandemic. First, it suggests that the goal of raising awareness among older participants with pre-existing conditions as a specific risk group for severe progressions of infection with COVID-19 might have successfully been achieved in Switzerland. However, it also shows that it is worthwhile to tackle psychological factors as the crisis is ongoing and decreasing social trust, decreasing fear and risk awareness, and increasing trivialising beliefs might hamper the continued support of the governments' strategy and adherence to hygiene and social distancing. Second, it shows that protective behaviour is inhibited by phenomena, such as cognitive dissonance. Thus, participants who exhibited lower health fears (aka higher optimistic bias) and higher trivialising beliefs (aka relief to cognitive dissonance) reported less adherence to protective measures. Lastly, it offers some insights into the behavioural responses to an ongoing threat and the associated uncertainty that is part of public communication about the pandemic and protective measures.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.114039.
Credit author statement
Angela Bearth: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Roles/Writing - original draft, Larissa Luchsinger, Data curation, Investigation, Project administration, Writing – review & editing, Michael Siegrist: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Supervision, Writing – review & editing
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Barr M., Raphael B., Taylor M., Stevens G., Jorm L., Giffin M., et al. Pandemic influenza in Australia: using telephone surveys to measure perceptions of threat and willingness to comply. BMC Infect. Dis. 2008;8 doi: 10.1186/1471-2334-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg-Weger M., Morley J.E. Loneliness and social isolation in older adults during the covid-19 pandemic: implications for gerontological social work. J. Nutr. Health Aging. 2020;24:456–458. doi: 10.1007/s12603-020-1366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betsch C. How behavioural science data helps mitigate the COVID-19 crisis. Nature Human Behaviour. 2020;4 doi: 10.1038/s41562-020-0866-1. 438-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betsch C., Wieler L.H., Habersaat K. Monitoring behavioural insights related to COVID-19. Lancet. 2020;395:1255–1256. doi: 10.1016/S0140-6736(20)30729-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bish A., Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br. J. Health Psychol. 2010;15:797–824. doi: 10.1348/135910710X485826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bish A., Yardley L., Nicoll A., Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011;29:6472–6484. doi: 10.1016/j.vaccine.2011.06.107. [DOI] [PubMed] [Google Scholar]
- Blumenschein M., Debbeler L.J., Lages N.C., Renner B., Keim D.A., El-Assady M. v-plots: Designing Hybrid Charts for the Comparative Analysis of Data Distributions. Eurographics Conference on Visualization (EuroVis) 2020;39(3) [Google Scholar]
- Blundell R., Costa Dias M., Joyce R., Xu X. COVID-19 and inequalities*. Fisc. Stud. 2020;41:291–319. doi: 10.1111/1475-5890.12232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brug J., Aro A.R., Richardus J.H. Risk perceptions and behaviour: towards pandemic control of emerging infectious diseases international research on risk perception in the control of emerging infectious diseases. Int. J. Behav. Med. 2009;16:3–6. doi: 10.1007/s12529-008-9000-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bults M., Beaujean D., de Zwart O., Kok G., van Empelen P., van Steenbergen J.E., et al. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in The Netherlands: results of three consecutive online surveys. BMC Publ. Health. 2011;11 doi: 10.1186/1471-2458-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho H., Lee J.-S., Lee S. Optimistic bias about H1N1 flu: testing the links between risk communication, optimistic bias, and self-protection behavior. Health Commun. 2013;28:146–158. doi: 10.1080/10410236.2012.664805. [DOI] [PubMed] [Google Scholar]
- Cohen J. Academic Press; New York, NY: 1977. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Cornwell B., Laumann E.O., Schumm L.P. The social connectedness of older adults: a national profile. Am. Socio. Rev. 2008;73:185–203. doi: 10.1177/000312240807300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruwys T., Stevens M., Greenaway K.H. A social identity perspective on COVID-19: health risk is affected by shared group membership. Br. J. Soc. Psychol. 2020;59:584–593. doi: 10.1111/bjso.12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings C.L., Rosenthal S., Kong W.Y. Risk Analysis; 2020. Secondary Risk Theory: Validation of a Novel Model of Protection Motivation. (n/a) [DOI] [PubMed] [Google Scholar]
- de Leo D., Trabucchi M. COVID-19 and the fears of Italian senior citizens. Int. J. Environ. Res. Publ. Health. 2020;17 doi: 10.3390/ijerph17103572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddy C., Schuster R., Sase E. An all-hazards approach to pandemic COVID-19: clarifying pathogen transmission pathways toward the public health response. J. Environ. Health. 2020;82:28–35. [Google Scholar]
- Federal Council . Federal Council; Berne, CH: 2020. Coronavirus: Bundesrat erklärt die “ausserordentliche Lage” und verschärft die Massnahmen [Federal Council announces the ‘extraordinary situation’ and tightens measures. [Google Scholar]
- Federal Office of Public Health . 2020. Neues Coronavirus: Besonders Gefährdete Personen [New Corona Virus: Risk Factors] [Google Scholar]
- Federal Statistical Office Internetzugang der Haushalte [Internet access of households] 2020. https://www.bfs.admin.ch/bfs/de/home/statistiken/kultur-medien-informationsgesellschaft-sport/informationsgesellschaft/gesamtindikatoren/haushalte-bevoelkerung/internetzugang-haushalte.html: Federal Statistical Office
- Felgendreff L., Korn L., Sprengholz P., Eitze S., Siegers R., Betsch C. Risk information alone is not sufficient to reduce optimistic bias. Res. Soc. Adm. Pharm. : RSAP. 2021;17:1026–1027. doi: 10.1016/j.sapharm.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Festinger L. Stanford University Press; Stanford, CL: 1957. A Theory of Cognitive Dissonance. [Google Scholar]
- Fitzpatrick K.M., Drawve G., Harris C. Facing new fears during the COVID-19 pandemic: the State of America's mental health. J. Anxiety Disord. 2020;75 doi: 10.1016/j.janxdis.2020.102291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flett, G.L., & Heisel, M.J. (early view). Aging and feeling valued versus expendable during the COVID-19 pandemic and beyond: a review and commentary of why mattering is fundamental to the health and well-being of older adults. Int. J. Ment. Health Addiction, 1-27. [DOI] [PMC free article] [PubMed]
- Gibson Miller J., Hartman T.K., Levita L., Martinez A.P., Mason L., McBride O., et al. Capability, opportunity, and motivation to enact hygienic practices in the early stages of the COVID-19 outbreak in the United Kingdom. British Journal of Health Psychology, early view. 2020;25(4):856–864. doi: 10.1111/bjhp.12426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilles I., Bangerter A., Clemence A., Green E.G.T., Krings F., Staerkle C., et al. Trust in medical organizations predicts pandemic (H1N1) 2009 vaccination behavior and perceived efficacy of protection measures in the Swiss public. Eur. J. Epidemiol. 2011;26:203–210. doi: 10.1007/s10654-011-9577-2. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Sanguino C., Ausin B., Castellanos M.A., Saiz J., Lopez-Gomez A., Ugidos C., et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haushofer J., Metcalf C.J.E. Which interventions work best in a pandemic? Science. 2020;368:1063–1065. doi: 10.1126/science.abb6144. [DOI] [PubMed] [Google Scholar]
- Hays R.D., DiMatteo M.R. A short-form measure of loneliness. J. Pers. Assess. 1987;51:69–81. doi: 10.1207/s15327752jpa5101_6. [DOI] [PubMed] [Google Scholar]
- IBM Corp . IBM Corp; Armonk, NY: 2017. IBM Statistics for Macintosh, Version 26.0. [Google Scholar]
- Jones J.H., Salathe M. Early assessment of anxiety and behavioral response to novel swine-origin influenza A(H1N1) PloS One. 2009;4 doi: 10.1371/journal.pone.0008032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan R.E., Adab P., Cheng K.K. Covid-19: risk factors for severe disease and death. The BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- Klein C.T.F., Helweg-Larsen M. Perceived control and the optimistic bias: a meta-analytic review. Psychol. Health. 2002;17:437–446. [Google Scholar]
- Kok G., Jonkers R., Gelissen R., Meertens R., Schaalma H., de Zwart O. Behavioural intentions in response to an influenza pandemic. BMC Publ. Health. 2010;10 doi: 10.1186/1471-2458-10-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kontis V., Bennett J.E., Rashid T., Parks R.M., Pearson-Stuttard J., Guillot M., et al. Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nat. Med. 2020;26:1919–1928. doi: 10.1038/s41591-020-1112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lades L.K., Laffan K., Daly M., Delaney L. Daily emotional well-being during the COVID-19 pandemic. British Journal of Health Psychology, early view. 2020;25(4):902–911. doi: 10.1111/bjhp.12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front. Psychol. 2013;4 doi: 10.3389/fpsyg.2013.00863. 863-863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lermer E., Streicher B., Raue M. In: Psychological Perspectives on Risk and Risk Analysis. Raue M., Lermer E., Streicher B., editors. Springer; Cham, CH: 2018. Measuring subjective risk estimates; pp. 313–327. [Google Scholar]
- Liao Q., Cowling B., Lam W.T., Ng M.W., Fielding R. Situational awareness and health protective responses to pandemic influenza A (H1N1) in Hong Kong: a cross-sectional study. PloS One. 2010;5 doi: 10.1371/journal.pone.0013350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loser P. Tagesanzeiger; 2020. Von «Sie nützen nichts» bis zur Pflicht – der grosse Maskenknorz des Bundes [From ‘They are of no us’ to compulsory - the great difficulties of the Swiss Confederation with hygiene masks. [Google Scholar]
- Lunn P.D., Timmons S., Belton C.A., Barjaková M., Julienne H., Lavin C. Motivating social distancing during the COVID-19 pandemic: an online experiment. Soc. Sci. Med. 2020;265:113478. doi: 10.1016/j.socscimed.2020.113478. [DOI] [PubMed] [Google Scholar]
- Marinthe G., Brown G., Delouvée S., Jolley D. Looking out for myself: exploring the relationship between conspiracy mentality, perceived personal risk, and COVID-19 prevention measures. British Journal of Health Psychology, early view. 2020;25(4):957–980. doi: 10.1111/bjhp.12449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E.A. Protecting and improving the lives of older adults in the COVID-19 era. J. Aging Soc. Pol. 2020;32:297–309. doi: 10.1080/08959420.2020.1780104. [DOI] [PubMed] [Google Scholar]
- Mukhtar S. Psychological health during the coronavirus disease 2019 pandemic outbreak. Int. J. Soc. Psychiatr. 2020;66:512–516. doi: 10.1177/0020764020925835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nivette A., Ribeaud D., Murray A., Steinhoff A., Bechtiger L., Hepp U., et al. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: insights from a longitudinal cohort study. Soc. Sci. Med. 2021;268:113370. doi: 10.1016/j.socscimed.2020.113370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noone C., McSharry J., Smalle M., Burns A., Dwan K., Devane D., et al. Video calls for reducing social isolation and loneliness in older people: a rapid review. Cochrane Database Syst. Rev. 2020;(5):1–40. doi: 10.1002/14651858.CD013632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel J.A., Nielsen F.B.H., Badiani A.A., Assi S., Unadkat V.A., Patel B., et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Publ. Health. 2020;183:110–111. doi: 10.1016/j.puhe.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G., Pietrantoni L., Zani B. Compliance with recommendations for pandemic influenza H1N1 2009: the role of trust and personal beliefs. Health Educ. Res. 2011;26:761–769. doi: 10.1093/her/cyr035. [DOI] [PubMed] [Google Scholar]
- Prati G., Pietrantoni L., Zani B. A social-cognitive model of pandemic influenza H1N1 risk perception and recommended behaviors in Italy. Risk Anal. 2011;31:645–656. doi: 10.1111/j.1539-6924.2010.01529.x. [DOI] [PubMed] [Google Scholar]
- Preis H., Mahaffey B., Heiselman C., Lobel M. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc. Sci. Med. 2020;266:113348. doi: 10.1016/j.socscimed.2020.113348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rea L.M., Parker R.A. Jossey-Bass Publishers; San Francisco, CA: 1992. Designing and Conducting Survey Research: a Comprehensive Guide. [Google Scholar]
- Reintjes R., Das E., Klemm C., Richardus J.H., Kessler V., Ahmad A. Pandemic public health paradox": time series analysis of the 2009/10 influenza A/H1N1 epidemiology, media attention, risk perception and public reactions in 5 European countries. PloS One. 2016;11 doi: 10.1371/journal.pone.0151258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers R.W. A protection motivation theory of fear appeals and attitude Change1. J. Psychol. 1975;91:93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Russel D. UCLA Loneliness Scale (version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Sadique M.Z., Edmunds W.J., Smith R.D., Meerding W.J., de Zwart O., Brug J., et al. Precautionary behavior in response to perceived threat of pandemic influenza. Emerg. Infect. Dis. 2007;13:1307–1313. doi: 10.3201/eid1309.070372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M., et al. Airborne transmission route of COVID-19: why 2 meters/6 feet of inter-personal distance could not Be enough. Int. J. Environ. Res. Publ. Health. 2020;17 doi: 10.3390/ijerph17082932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley C.G., Greaves L.M., Satherley N., Wilson M.S., Overall N.C., Lee C.H.J., et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am. Psychol. 2020;75:618–630. doi: 10.1037/amp0000662. [DOI] [PubMed] [Google Scholar]
- Siegrist M., Luchsinger L., Bearth A. 2021. The Impact of Trust and Risk Perception on the Acceptance of Measures Fighting against Covid-19. Risk Analysis, Early View. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist M., Zingg A. The role of public trust during pandemics: implications for crisis communication. Eur. Psychol. 2014;19:23–32. [Google Scholar]
- Slovic P., Finucane M.L., Peters E., MacGregor D.G. Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Risk Anal. 2004;24:311–322. doi: 10.1111/j.0272-4332.2004.00433.x. [DOI] [PubMed] [Google Scholar]
- Slovic P., Peters E. Risk perception and affect. Curr. Dir. Psychol. Sci. 2006;15:322–325. [Google Scholar]
- Tang F., Liang J., Zhang H., Kelifa M.M., He Q., Wang P. COVID-19 related depression and anxiety among quarantined respondents. Psychology & Health, early view. 2020:1–15. doi: 10.1080/08870446.2020.1782410. [DOI] [PubMed] [Google Scholar]
- van Bavel J.J., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., et al. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Wise T., Zbozinek T.D., Michelini G., Hagan C.C., Mobbs D. Changes in risk perception and protective behavior during the first week of the COVID-19 pandemic in the United States. R. Soc. Open Sci. 2020;7:20742. doi: 10.1098/rsos.200742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrzus C., Hanel M., Wagner J., Neyer F.J. Social network changes and life events across the life span: a meta-analysis. Psychol. Bull. 2013;139:53–80. doi: 10.1037/a0028601. [DOI] [PubMed] [Google Scholar]
- Xie B., Charness N., Fingerman K., Kaye J., Kim M.T., Khurshid A. When going digital becomes a necessity: ensuring older adults' needs for information, services, and social inclusion during COVID-19. J. Aging Soc. Pol. 2020;32:460–470. doi: 10.1080/08959420.2020.1771237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye M., Lyu Z. Trust, risk perception, and COVID-19 infections: evidence from multilevel analyses of combined original dataset in China. Soc. Sci. Med. 2020;265:113517. doi: 10.1016/j.socscimed.2020.113517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuksel A., Karadogan D., Gurkan C.G., Akyil F.T., Toreyin Z.N., Marim F., et al. Unclear issues regarding COVID-19. Eurasian Journal of Medicine. 2020;52:191–196. doi: 10.5152/eurasianjmed.2020.20092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.