Graphical abstract
Keywords: COVID-19, Human exposure, Inhalation, Organophosphate esters, Plasticizers, SARS-COV-2
Abstract
For the first time, organophosphate ester (OPE) content was studied in different types of surgical, self-filtering (KN95, FFP2, and FFP3) and reusable face masks used for COVID-19 prevention. OPEs were detected in all mask samples, although in highly variable amounts which ranged from 0.02 to a maximum of 27.7 µg/mask, with the highest mean concentrations obtained for KN95 masks (11.6 µg/mask) and the lowest for surgical masks (0.24 µg/mask). Twelve out of 16 tested analytes were detected, with TEP, TPHP, TNBP, TEHP and TClPP being the most common OPEs as well as present at the highest concentrations. The non-carcinogenic and carcinogenic risks of OPE inhalation were calculated as being always several orders of magnitude lower than threshold levels, indicating that the use of face masks is safe with regard to OPE contamination. However, given the wide range of OPEs observed in different masks, it can be concluded that some masks (e.g. reusable) are less OPE-contaminated than others (e.g. KN95). With regard to environmental pollution, the disposal of billions of face masks is adding to the already substantial levels of microplastics and associated toxic additives worldwide, an impact that is lessened by use of reusable masks, which also have the lowest economic cost per user. However, in situations of relatively high risk of viral inhalation, such as poorly ventilated indoor public spaces, we recommend the use of FFP2 masks.
1. Introduction
The COVID-19 pandemic caused by the virus SARS-CoV-2 emerged in December 2019 and poses a huge global health threat. The pandemic progressed rapidly and the preventive measures implemented to control and mitigate its high transmissibility involved a sudden increase in demand and consumption of plastic products by the general public, and healthcare and service workers. The WHO acknowledges that “wearing a medical mask is one of the prevention measures that can limit the spread of certain respiratory viral diseases, including COVID-19” (WHO, 2020a). Currently, the use of face masks by the public both in open and closed spaces has been recommended or even enforced by health authorities.
Based on WHO estimation (WHO, 2020b), 89 million medical masks are required for the COVID-19 response each month worldwide, as well as 129 billion face masks for the general public (Prata et al., 2020). Masks will continue to be a product of necessary use in the long term and there are two aspects that must be considered: the environmental impact derived from the massive consumption of disposable masks and their effect on human health due to the prolonged and daily use of such masks.
There are very few studies evaluating the potential risks to humans from prolonged use of masks. Recently, Özdemir et al. (2020) studied the risk of carbon dioxide retention due to re-breathing in healthcare workers who use filtering facepiece (FFP)2 respirators for a long time, concluding that further studies are needed on the safety of devices used by healthcare workers and general public. However, there are no studies evaluating components in masks that may have adverse health effects.
Single use face masks are produced from polymers such as polypropylene, polyurethane, polyacrylonitrile, polystyrene, polycarbonate, polyethylene or polyester (Potluri and Needham, 2005). These polymers contain a series of chemical compounds, such as plasticizers and flame retardants, some of them characterized as toxic to human health. Commercial masks are sometimes accompanied by a certificate of chemical analysis that includes, among others, chlorinated phenols, polycyclic aromatic hydrocarbons (PAHs), and some plasticizers such as phthalates. There is no specific regulation for organic pollutants in face masks. However, some of these chemical additives are regulated in general products, being also apply to face masks. For instance, the Germany’s Product Safety Committee published a standard (AfPS GS 2019:01 PAK) on PAHs limits in products, whose level should not exceed between 0.2 and 1 mg/Kg. The EU REACH regulation (Registration, Evaluation, Authorization and Restriction of Chemical Products) restricts some phthalates to a maximum content of 0.1% by weight of the material. However, there are many other families of chemical additives that are not covered, and for which no type of control is carried out.
Organophosphate esters (OPEs) are high-production-volume chemicals widely used as plasticizers and flame retardants. This group of emerging pollutants has been raising increasing concern due to their reported toxic effects. Tri-n-butyl phosphate (TNBP) has been observed to disrupt endocrine and reproductive functions, nervous system development and is suspected carcinogen (He et al., 2020). Some epidemiological studies have reported that exposure to tris(1,3-dichloro-2-propyl) phosphate (TDClPP) is associated with decline of semen quality (He et al., 2020). OPEs are also associated with asthma and allergies (Meeker and Stapleton, 2010, Van der Veen and de Boer, 2012). Moreover, some OPEs have established oral reference doses (RfD) and oral cancer slope factors (SFO), which were recently updated by the USEPA (2019). Based on these values, the non-carcinogenic (non-CR) and carcinogenic (CR) risks of human exposure to OPEs can be evaluated.
The main objective of the present study is to evaluate the OPE occurrence in different types of masks, and to determine their human impact through prolonged and continuous use due to the current pandemic situation. In addition, we examine the likely environmental impacts resulting from the amount of mask introduced in the different environmental compartments due to incorrect disposal.
2. Materials and methods
2.1. Sampling collection
In order to obtain a broad overview, three different types of masks were selected:
-
•
Surgical masks: made of non-woven polypropylene polymers. They protect from the inside out (prevent us from emitting viruses to the outside of the mask), but only partially from the outside in.
-
•
Self-filtering masks, KN95, FFP2 and FFP3: they protect from the inside out and from the outside in (the mask prevents viruses from entering our respiratory system).
-
•
Re-usable masks: made of different types of cloth. They protect in the same way as surgical masks (with the certificate of compliance of the UNE0065 Standard, with bacterial protection efficiency greater than 90%).
In order to determine whether this selection of masks can be considered generalized at a global scale, we should have information on the use of each type of mask by the population. However, this information is very scarce. We have only found data for pedestrians in Southwest Iran (Rahimi et al., 2021), showing that the most common type was surgical mask (63.8%), followed by cloth masks (19.9%) and by filtering masks (15.4%). Similar findings were reported by Tam et al. (2020) and Gunasekaran et al. (2020). The former reported data obtained from 10,211 pedestrians in various regions of Hong Kong between 1st and 29th Feb 2020, observing that 83.7% wore surgical masks. The second presented a study among people who visited a hospital in Malaysia in April 2020. Seventy percent of people wore surgical masks.
A total of twenty samples of masks were utilised for the study (Table 1 ). In addition, two filter samples used for homemade masks which include a layer for disposable filters, were also selected. Of these twenty masks, eight were surgical masks produced by different manufacturers (all of them located in China), another eight were self-filtering masks, and the remaining four were reusable masks. With regard to the selection of self-filtering masks, these included three different types of KN95 (all manufactured in China), and two FFP2 antiCOVID-19 masks developed by researchers of IATA-CSIC and Bioinicia SL (Valencia, Spain) (commercialised by Bioinicia under the brand PROVEIL® and fabricated in Spain (PLNS) and Germany (PC)) and which contain an innovative and very thin filter made of nanofibers, typically 60 times thinner than conventional melt blown polypropylene filters, sandwiched between layers of spun bond polypropylene. Of the remaining three self-filtering mask types used in our study, one was a FFP3 manufactured in Spain by 3M, and the remaining two were FFP2 (M17) and FFP3 (M5) that both containing a valve; although such valved masks are not currently recommended for COVID-19 protection since they protect the user, but do not protect others, we included them in this study as they were used at the beginning of the COVID-19 pandemic and they are also widely used as individual protection equipment in different applications. From the wide variety of reusable masks on the market, 4 different types from 3 different companies and manufactured with different tissues (cotton, PET, polyamide) were chosen.
Table 1.
Different types of masks selected in our study.
| Code | Characteristics | Origin | Recommended use | Weight (g)* | Price (€) | Photography |
|---|---|---|---|---|---|---|
| Surgical masks | ||||||
| M1 | Non woven Polypropylene | China (Ningbo Beilai Travelling Products Co. Ltd, Gaoyou Yongye Commodity Factory, Beifa Group Co. Ltd, etc.) | 4 h | 2.429 | 0.62a |  |
| M2 | 2.604 | |||||
| M13 | 2.526 | |||||
| M14 | 2.414 | |||||
| M19 | 2.748 | |||||
| M20 | 2.442 | |||||
| M21 | 2.661 | |||||
| M22 | 2.527 | |||||
| Self-filtering masks – KN95 | ||||||
| M3 | Non woven fabric | China (Taizhou Yongli Medical Device Co. Ltd, etc.) | 8 h | 3.581 | 2.35 |  |
| M6 | 4.952 | 1.40 | ||||
| M11 | 3.501 | 2.79 | ||||
| Self-filtering masks - FFP2 | ||||||
| M16 | Spun bond polypropylene | Germany, Spain (Bioinicia-CSIC) |
2 full days | 3.260 | 2.40 |  |
| M18 | 3.293 | |||||
| M17 | not provided | not provided | 8 h | 8.298 | – | |
| Self-filtering masks - FFP3 | ||||||
| M5 | not provided | Spain (Irudek) | 8 h | 10.645 | 9.95 |  |
| M10 | Polypropylene | Spain (3 M) | 7.707 | 7.75 | ||
| Filters for homemade masks | ||||||
| F1b | Activated carbon, non woven filter cloth | not provided | 1 day | 1.527 | 1.50 |  |
| F3 | Non woven Polypropylene | not provided | 4 h Re-usable (x9) |
0.979 | 0.60 | |
| Reusable masks | ||||||
| M4 | Ecological cotton | not provided | 1 day Re-usable (x40) |
6.404 | – |  |
| M7 | PET | Spain | 8 h Re-usable (x20) |
7.238 | 15 | |
| M8 | Recycled PET | 7.321 | ||||
| M12 | Polyamide | Spain (Quretex) | 1 day Re-usable (x70) |
6.955 | 7 | |
Weight of the mask without rubber bands and nose clip, and for M5 and M17, also without valve.
Maximum price established by the Spanish government.
For an optimal filtration, the application of 2 filters was recommended for each use.
All the masks and the filters for homemade masks tested were sold in plastic packages. Some masks were individually packaged (KN95, FFP2, FFP3 and some re-usable M12), while others were in packs of 2 (some filters F1), 3 (some re-usable M7 and M8), or 10 units (surgical and some filters F3). Therefore, OPE contamination could come from both the mask material and the packaging.
2.2. Standards and reagents
A total of sixteen OPEs were analysed in the present study. Analytical standards were purchased from different companies: tris(2-chloroethyl) phosphate (TCEP), tris(2-chloroisopropyl) phosphate (TCIPP), trihexyl phosphate (THP) and tris(2-ethylhexyl) phosphate (TEHP) were purchased from Santa Cruz Biotechnology (SantaCruz, CA, USA); isodecyldiphenyl phosphate (IDPP) was purchased from AccuStandard (New Haven, CT, USA); triethyl phosphate (TEP), tripropyl phosphate (TPP), diphenylcresyl phosphate (DCP), TNBP, triphenyl phosphate (TPHP), triphenylphosphine oxide (TPPO) and TDClPP were purchased from Merck (Darmstadt, Germany); tricresyl phosphate (TCP) was purchased from Dr. Ehrenstorfer (Augsburg, Germany); tris(2-isopropylphenyl) phosphate (T2IPPP) was purchased from Chiron (Trondheim, Norway); labelled d15-TPHP were purchased from Cambridge Isotope Laboratories Inc. (Andover, MA, USA); bis(4-isopropylphenyl)phenyl phosphate (B4IPPPP), 2-isopropylphenyl diphenyl phosphate (2IPPDPP) and labelled d15-TEP, d21-TPP, d15-TDClPP, d27-TNBP and d12-TCEP were purchased from Wellington Laboratories Inc. (Guelph, ON, Canada); and labelled d15-TEHP was purchased from Toronto Research Chemicals (Toronto, ON, Canada). Labelled compounds were used as internal standards.
Methanol and water solvent for trace analysis as well as ammonium acetate and formic acid were obtained from Merck (Darmstadt, Germany). Acetone and hexane for organic trace analysis were purchased from J.T. Baker (Centre Valley, PA, USA). Glass wool was obtained from Panreac AppliChem (Barcelona, Spain).
2.3. Inhalation measurements
In order to evaluate the possibility of inhaling plasticizers via use of the different masks, an experimental campaign was carried out using two paper-mache dummy heads representing an adult human's head (size 20 cm height × 15 cm width × 20 cm depth) (Fig. 1 ). Both heads were located indoors in an office with windows and doors closed, and were fitted with the different face masks analysed. The nose of each dummy head was fitted with an anti-electrostatic inlet tube connected to a PM2.5 head to collect airborne particulate matter in 37 mm quartz microfiber filters using a Personal Environmental Monitor (PEM) with a flow rate of 10 L/min. Each mask was tested for 6 h (equivalent to the volume of air inhaled by an adult in 4 h, Maceira et al., 2019), including a field blank when the dummy head did not wear any mask. The experiment was repeated outdoors following the same protocol, to evaluate possible differences in inhalation when sunlight was affecting the mask. Details on the experimental campaign are reported in Table S1.
Fig. 1.
Inhalation experiments with paper-mache dummy heads located (a) indoors (masks M7 and M10) and (b) outdoors (masks M12 and M18).
The methodology here used for the inhalation testing has previously been applied to study the effectiveness of low cost face masks worn by cyclists to reduce the level of exposure to airborne particle matter (Pacitto et al., 2019). As stated by these authors the method has certain limitations because it does not consider the exhalation process which might compromise the fit of the mask due to the positive pressure generated, leading to possible dilution of pollutant concentration in the area between mask and face. In any case, there will also be a dilution in real conditions due to the lack of a perfect seal of the mask against a human face.
2.4. OPE analysis
Previously developed methodologies have been applied for the determination of OPEs in PM2.5 filters (Olivero-Verbel et al., 2021). Moreover, the analytical method has been also adapted for the new face mask matrix. Before masks extraction, ear loops, metal nose strips, valves or any adhesive sticks were removed. Face masks were weighed and cut into small pieces (1–2 cm2) that were placed in glass beakers. Filters were cut and transferred into 40 mL glass-centrifuge tubes. All samples were fortified with 25 ng of an internal standard mixture. After equilibration, 15 and 60 mL of hexane:acetone (1:1) were added to filters and mask samples, respectively, and ultrasound extraction took place during 15 min. Extraction was carried out twice, and both extracts were combined and filtered with glass wool. Finally, solvent was concentrated to incipient dryness and redissolved with methanol to 500 µL.
An online sample purification and analysis was performed with a Thermo Scientific TurboFlow™ system consisting of a triple quadrupole (QQQ) MS with a heated-electrospray ionisation source (H-ESI), two LC quaternary pumps and three LC columns, two for purification and one for separation. The TurboFlow™ purification columns employed were: Cyclone™-P (0.5x50mm) and C18-XL (0.5 × 50 mm). Chromatographic separation was subsequently achieved using an analytical column: Purosphere Star RP-18 (125 mm × 0.2 mm) with a particle size of 5 μm (Giulivo et al., 2016). Detailed conditions used for purification and chromatographic separation were included in Table S2. Selective reaction monitoring (SRM) mode was used for all compounds with two transitions monitored for each analyte. The most intense transition was used for quantification, while the second provided confirmation. Instrumental working parameters such as retention times, transitions, declustering potential and collision energies were summarized in Table S3.
Instrumental parameters such as recoveries, limits of detection (LODs) and limits of quantification (LOQs) are summarised in Supporting information (Table S4). Our analytical methodology provided recoveries ranging between 47 and 115% and 50–118% for masks and quartz microfiber filters, respectively. Limits of detection (LODs) ranged between 0.005 and 0.644 ng/mask, and between 0.002 and 0.114 ng/m3.
For each batch of mask and filter samples, a laboratory blank was included. Laboratory blank levels were subtracted from corresponding mask samples, whereas field blank levels were subtracted from corresponding filter samples. Results obtained for the different blanks can be found in Table S5.
3. Results
3.1. OPE levels in face masks
The OPE concentrations in face masks are summarized in Table 2 . Some mask samples were analysed in duplicate (2 masks from the same batch), obtaining similar values in both replicates, with relative standard deviation (RSD) values between 1.04 and 13.4% (Table S6). However, higher RSD values (34.5 and 38.1%) were obtained for reusable mask samples, indicating that OPE distribution in these materials may not be as uniform as in the rest of the masks.
Table 2.
OPE levels (expressed in ng/mask) in mask samples.
| TEP | TPPO | TClPP | TDClPP | TPHP | TNBP | DCP | 2IPPDPP | TCP | B4IPPPP | T2IPPP | TEHP | ΣOPEs | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgical masks | |||||||||||||
| M1 M2 M13* M14 M19 M20 M21 M22 |
2.89 65.6 15.4 26.2 30.0 nd nd nd |
nd nd nd nd nd nd nd nd |
nd nd 34.6 35.8 nd 2.90 18.8 17.4 |
3.21 10.4 nd 2.42 nd nd nd nd |
50.5 14.8 59.9 38.0 nd nd nd nd |
13.5 nd 6.23 27.3 5.14 nd 4.08 657 |
nd nd nd 0.65 nd nd nd nd |
2.39 nd 2.83 nd nd nd nd nd |
nd nd nd nd nd nd nd nd |
1.66 nd nd nd nd nd nd nd |
68.0 nd 9.30 nd nd nd nd nd |
26.5 nd 490 nd 70.9 21.8 15.5 42.4 |
169 90.7 619 130 106 24.7 38.4 717 |
| Self-filtering masks – KN95 | |||||||||||||
| M3 M6 M11* |
1.56 nd 35.6 |
nd nd 20,064 |
nd nd 37.5 |
23.5 15.4 18.1 |
154 65.2 41.1 |
44.9 nd 13.5 |
nd nd 0.96 |
nd 2.71 nd |
nd nd nd |
nd nd nd |
nd 174 nd |
98.5 13,847 216 |
323 14,104 20,427 |
| Self-filtering masks – FFP2 | |||||||||||||
| M16 M18* M17 |
36.6 50.6 764 |
nd 220 141 |
49.2 202 97.5 |
2.96 nd nd |
129 nd 45.7 |
24.0 11.4 193 |
nd nd nd |
nd nd nd |
nd nd nd |
nd nd nd |
nd nd nd |
nd nd 497 |
242 483 1737 |
| Self-filtering masks – FFP3 | |||||||||||||
| M5 M10* |
125 86.6 |
nd nd |
325 nd |
143 17.7 |
12,487 113 |
81.3 125 |
nd nd |
nd 19.6 |
nd nd |
nd nd |
nd nd |
14,574 nd |
27,735 362 |
| Filters for homemade masks | |||||||||||||
| F1* F3* |
200 10.7 |
nd nd |
nd nd |
nd nd |
4.87 nd |
1065 0.84 |
nd nd |
nd nd |
182 nd |
0.70 nd |
74.1 4.69 |
nd nd |
1527 16.3 |
| Reusable masks | |||||||||||||
| M4 M7 M8* M12* |
231 280 157 0.78 |
nd nd nd nd |
nd 42.7 144 nd |
nd 4.06 11.7 9.87 |
53.7 475 56.7 191 |
nd nd nd nd |
nd nd nd nd |
nd nd 2.42 nd |
nd nd nd nd |
nd nd nd nd |
nd nd nd nd |
nd 971 90.3 nd |
284 1773 462 202 |
nd: below limit of detection.
Mean value of two replicates.
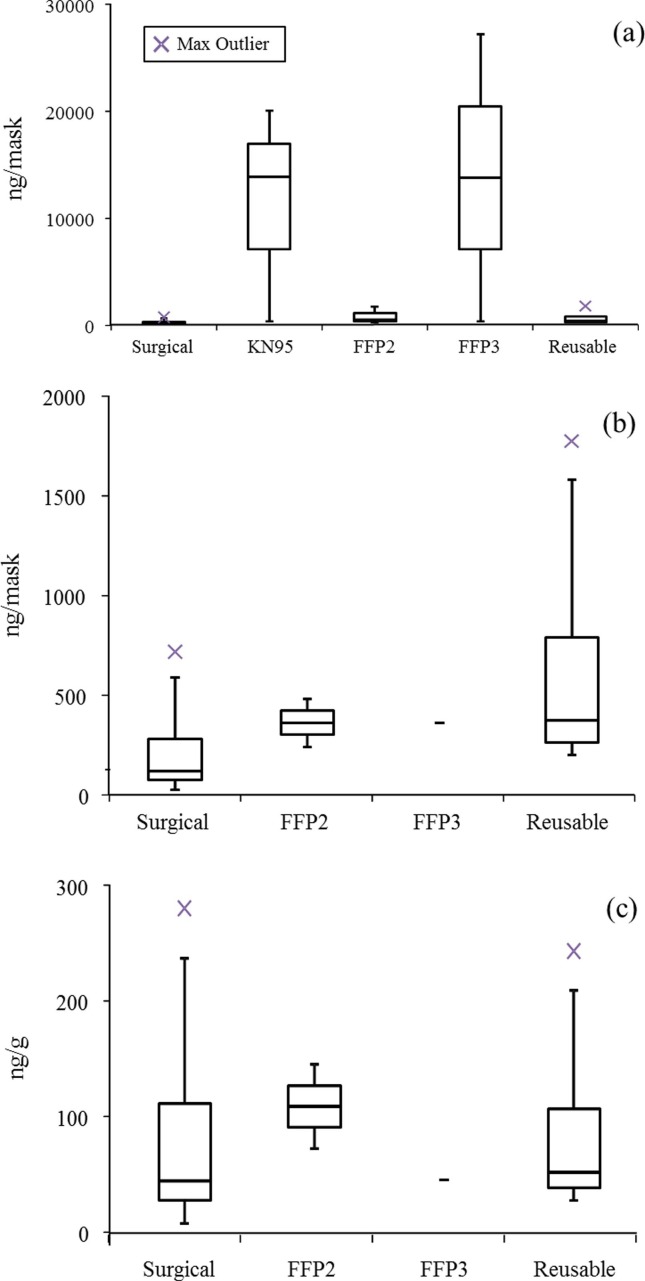
OPEs were detected in all the analysed samples (Fig. 2 ), although in concentrations that varied across a very wide range of 24.7 ng/mask to 27.7 µg/mask. The source of these OPEs could be either an intentional application in the materials used for the manufacture, or as a result of partitioning with the ambient air during the manufacture. Different studies have shown the ubiquity of OPEs in indoor air (Wong et al., 2018). Taking into account all 20 analysed samples (Fig. 2a), we observe that KN95 and FFP3 masks presented the highest OPEs values, with mean concentration levels of 11.6 and 14.1 µg/mask, respectively. If we focus exclusively on those masks that are being used for protection against COVID-19 at the moment, we have to discard the two masks that contained valves (a FFP2, M17, and a FFP3, M5) as they are not recommended for COVID-19 protection. In addition, some European countries (including Spain) have decided to ban the sale of KN95 masks from January 2021 (BOE, 2020), as they do not meet with the requirements established by the European homologation. Fig. 2b shows the comparison, excluding KN95 and masks with valves. ΣOPE levels in surgical masks seem to be lower than those of FFP2, FFP3 and reusable masks. Median values of ΣOPEs were 118, 363, 362 and 373 ng/masks for surgical, FFP2, FFP3 and reusable masks, respectively. However, the ANOVA test showed that the differences between different mask types were not significant (p = 0.46). Moreover, when levels of OPEs were expressed in ng/g (see Table S7), the previously observed differences disappear, and the contamination levels were more similar for all types of masks (Fig. 2c), with median values of ΣOPEs of 46.3, 110, 47.0 and 53.8 ng/g for surgical, FFP2, FFP3 and reusable masks, respectively. This is because surgical masks are the lightest, with a mean weight of 2.54 g, while FFP2, FFP3 and reusable masks weigh around 3.28, 7.71 and 6.98 g, respectively.
Fig. 2.
Comparison between OPE levels in the different types of masks (a) including all 20 analysed samples, and (b) and (c) excluding KN95, as well as M17 (FFP2) and M5 (FFP3) which contained a valve and they are not currently recommended for COVID-19 protection, expressed in ng/mask (b) and ng/g (c). Outliers (x) are shown.
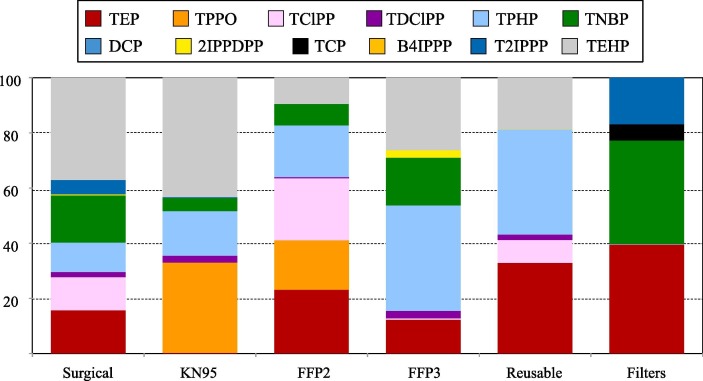
Twelve out of sixteen tested analytes were detected. Only TCEP, TPP, IDPP and THP were not detected in any sample. TEP was the most frequently detected (in 80% of masks), followed by TPHP (75%), TNBP and TEHP (65%) and TClPP and TDClPP (60%). As regards to concentration levels, Fig. 3 shows the percentage contribution of detected OPEs to the total contamination in the different masks and filters. The most contributing compounds were the same in all the mask samples: TEHP (mean contribution of 29%), TPHP (21%), TEP (18%) and TNBP and TClPP (10%). In the case of KN95 and FFP2 masks, TPPO contribution was also important, with a mean value of 33% and 18%, respectively. Finally, OPE profile in filters for homemade masks presented differences compared with those obtained for masks: TEP and TNBP were also the most contributing OPEs (40% and 37%, respectively); however, T2IPPP contribution should also be highlighted, with a mean value of 17%.
Fig. 3.
Percentage contribution of detected OPEs to the total concentration levels in masks and filters.
3.2. OPE exposure assessment
In order to evaluate the possibility of inhaling plasticizers via use of masks, different experiments at laboratory scale (indoor and outdoor) were carried out. Results obtained are presented in Table 3 .
Table 3.
OPE levels in PM2.5 filters (expressed in ng/filter) from experiments to evaluate the inhaling fraction of OPEs via use of masks (tested for 6 h, equivalent of volume inhaled by an adult in 4 h).
| TEP | TClPP | TDClPP | TPHP | TNBP | DCP | 2IPPDPP | T2IPPP | TEHP | ΣOPEs | |
|---|---|---|---|---|---|---|---|---|---|---|
| Surgical masks | ||||||||||
| M13 indoor M13 outdoor |
nd nd |
nd nd |
nd nd |
nd nd |
nd 0.82 |
nd nd |
nd nd |
nd nd |
nd nd |
nd 0.82 |
| Self-filtering masks – KN95 | ||||||||||
| M11 indoor M11 outdoor |
nd nd |
nd nd |
nd nd |
0.38 nd |
0.64 nd |
nd nd |
nd nd |
nd nd |
22.9 nd |
23.9 nd |
| Self-filtering masks – FFP2 | ||||||||||
| M16 indoor M18 indoor M18 outdoor |
nd nd nd |
4.36 11.6 nd |
nd nd nd |
nd nd nd |
1.36 1.33 nd |
nd nd nd |
nd nd nd |
nd nd nd |
nq nd nd |
5.72 13.0 nd |
| Self-filtering masks – FFP3 | ||||||||||
| M10 indoor M10 outdoor |
nd nd |
nd nd |
nd nd |
nd nd |
1.39 2.19 |
nd nd |
nd nd |
nd nd |
nd nd |
1.39 2.19 |
| Reusable masks | ||||||||||
| M7 indoor M8 indoor M12 indoor M12 outdoor |
nd nd nd nd |
nd nd nd nd |
nd nd nd nd |
nd nd nd nd |
nd nd nd nd |
nd nd nd nd |
nd nd nd nd |
nd nd nd nd |
nd nd nd nd |
nd nd nd nd |
nd: below limit of detection.
Using OPE values detected in PM2.5 filters after simulating a 4-hour use of masks, and using the initial OPE levels in masks (see Table 2), we estimated the percentage of compound that would be inhaled during the use of masks. This first approximation seems to indicate that only a small part of compounds present in masks would be inhaled in that period of time. The compounds with the highest inhalation percentages were TNBP (between 1 and 13%) and TDClPP (between 6 and 9%). On the other hand, TEP, TDClPP, DCP, 2IPPDPP and T2IPPP were not detected in any PM2.5 filter, indicating that they would not be inhaled. It should be noted that in the case of reusable masks, no OPEs were detected in any PM2.5 filter sample, suggesting that the material of these masks will retain all OPE content, avoiding their inhalation.
With respect to experiments carried out indoor and outdoor, no differences were detected. Outdoor experiments were performed to evaluate the sunlight effect and whether the temperature could cause a higher level of OPE desorption from the mask, and therefore, a higher level of inhaled compound. Such an effect was not observed, perhaps because although sunny, the temperature during the experiments was only around 19 °C. Further experiments at higher temperatures, up to 30–35 °C (most common temperature in summer, in countries such as Spain) are necessary. Moreover, the method used has the limitation of the fact that the test does not consider the humidity present between the mask and the face when inhaling, and the possibility that this can affect the emission of plasticizers from the mask. We view this as possibly leading to an underestimation of the plasticizers inhaled.
Taking into account all the aforementioned limitations on estimating the degree of inhalation, an approximation of human exposure to OPEs via inhalation during the use of masks has been carried out. Estimated daily intakes (EDIinhalation), expressed in ng/kg body weight (bw)/day, were calculated from mask concentration levels. Average body weight was assumed to be 70 kg for adults (Maceira et al., 2019). The calculation assumes that 10% of OPE content in mask was inhaled (based on our previous results in a laboratory scale and considering the less favourable scenarios) and that 100% of the inhaled chemicals were absorbed in the airways. In addition, we considered that a single mask was used per day. EDIinhalation values for ΣOPEs ranged between 0.02 and 39.6 ng/kg bw/day (Table S8), being those for KN95 masks on average the highest values. Obtained EDIinhalation values were not negligible, especially if we compare with published data on EDIinhalation values for indoor environments. Sakhi et al. (2019) reported an EDIinhalation value of 11 ng/kg bw/day in indoor air from Norwegian homes and schools. Similar values were obtained by He et al. (2018), who estimated that the daily intake corresponding to inhalation for the Australian population was 7.9 ng/kg bw/day. Therefore, considering that human exposure to OPEs via indoor air inhalation is around 10 ng/kg bw/day, the use of a KN95 mask per day would cause doubling of this exposure. On the other hand, the use of filters of activated carbon for homemade masks (F1), taking into account that for an optimal filtration the application of two filters is recommended for each use, would provide an extra OPE inhalation exposure. For the rest of the masks, their use will increase this exposure by between 3 and 10%. Thus, even though wearing a mask could prevent exposure to OPE levels present in indoor / outdoor environments, the use of face masks would be causing a higher exposure due to the inhalation of OPEs present in the mask.
Recently, USEPA (2019) updated the oral reference dose (RfD) and oral cancer slope factors (SFO) of some OPEs. We estimated the non-carcinogenic (non-CR) and carcinogenic (CR) risks of OPE exposure via the use of masks (Table S8). It must be taken into account that the non-CR and CR potency values are based on risk over a lifetime of exposure. Although we do not know how long we should use facial masks, a duration of at least 2 years has been estimated to be able to fully combat SARS-COV-2 virus. In addition, its use is likely to become common in certain environments, such as public transport, or by some groups, such as health personnel. The non-CR risk was calculated dividing the obtained EDIinhalation values by the corresponding RfD. It was reported that if the non-CR risk was higher than 1, then a potential non-CR risk to humans might occur. The CR risk was calculated multiplying the obtained EDIinhalation values by the corresponding SFO, with one cancer incidence case per million people being used as an acceptable level of risk. Hence, if the CR value was greater than 1 E-06, the EDIs exceeded the safe threshold indicating the potential adverse effects. The non-CR and CR values from exposure to OPEs were 4–7 and 1.5–5 orders of magnitude lower than the corresponding threshold level, respectively. Thus, the use of COVID-19 face mask is not considered to be dangerous for citizens regarding exposure to OPEs. However, special attention must be paid on KN95 masks. For instance, the use of mask M6 carried a CR risk value of 6.3 E-08, which is 15 times below the safe value. In this case, the risk basically comes from the high TEHP levels in this mask. Similar situation was observed for the M5 mask, a FFP3 mask containing a valve. This mask is not used for COVID-19 protection at the moment, but it was used at the beginning of the COVID-19 pandemic and is also widely used as individual protection equipment in different applications. Moreover, it is important to note that OPE exposure also occurs by other routes, such as indoor/outdoor inhalation (Wong et al., 2018), dermal absorption (He et al., 2018), dust ingestion (Kim et al., 2019) and dietary intake (Poma et al., 2017). The sum of all these exposures can bring the values closer to the established safety limits.
3.3. Environmental impact
The WHO (2020b) estimated that 129 billion face masks are required for the COVID-19 protection of general public each month worldwide (Prata et al., 2020). The use of these masks by ordinary citizens has quickly became controversial due to the lack of correct handling and disposal. According to a report by World Wide Fund for Nature (WWF, 2020), over 10 million masks can be introduced in the terrestrial and aquatic environment monthly due to incorrect disposal. Once in the environment, such facemasks will degrade, contributing to the already substantial levels of microplastics worldwide and causing environmental pollution and damage. But, in addition to the contamination by microplastics, we also have to take into account the contamination due to the chemical additives associated with these plastics, as is the case of OPEs. Considering the use and weight of each type of masks (Table 1), we have calculated the amount of waste that would be generated (Table 4 ). On the other hand, and from the OPE levels in masks obtained in our study (Table 2), we have evaluated the amount of these contaminants that would be generated and dispersed annually throughout the environment (Table 4). As can be seen, globally wastes generated by the use of face masks would be around millions (0.22–6.30) of tons of waste per year. The least impact would occur if the entire population used reusable masks, since these masks can be re-used up to 50 times. The OPE amounts dispersed throughout the environment would range between 20 and 18,000 Kg, a considerable amount taking into account the toxicity of this type of compound at very low doses. Moreover, estimated half-lives of analysed OPEs ranged between 0.49 and 575 days in air, and between 12 and 260 days in water (Sühring et al., 2020). Again, the least impact would be obtained with the use of reusable masks.
Table 4.
Globally environmental and economic impact of the use of COVID-19 face masks by the general population.
| Surgical | KN95 | FFP2 | Reusable | Filters | |
|---|---|---|---|---|---|
| Mean weight (g) | 2.544 | 4.011 | 3.277 | 6.980 | 1.253 |
| Number of applications | 1 | 1 | 2 | 50 | 1 |
| Wastes (tonnes/year) | 3.99 E6 | 6.30 E6 | 2.57 E6 | 0.22 E6 | 1.97 E6 |
| Mean OPE level (ng/mask)* | 237 | 11,618 | 363 | 680 | 771 |
| OPEs dispersed (Kg/year) | 372 | 18,234 | 285 | 21.3 | 1210 |
| Price (€/mask) | 0.62 | 2.18 | 2.40 | 11 | 1.05 |
| Economic cost (€/person and year) | 226 | 796 | 438 | 80.3 | 383 |
Mean OPE level refers to sum of all analytes detected in the mask.
However, in order to assess the whole environmental impact, it would be necessary to consider lifecycle analysis (LCA) of each type of face mask. Rizan et al. (2021) used a LCA to determine environmental impacts of personal protective equipment (PPE) distributed to health and social care in England during the first six months of the COVID-19 pandemic. They concluded that the environmental impact could be reduced through different actions, among which it was the reuse of PPE. This action would have reduced the carbon footprint by 10%. In another study, Baker et al. (2020) showed a systematic evaluation of isolation gowns, including the impacts of manufacturing, packaging, and landfill disposal of disposable gowns compared to reusable gowns. Reusables consume 28% less total energy over the product lifecycle and their use led to a 30% reduction in greenhouse gas emissions. A recent study (Boix Rodríguez et al., 2021) showed the LCA as well as the circularity of different face masks, taking into account the main phases of the mask life cycle: material and manufacturing, use and end of life. The results showed that the worst values were obtained for a FFP2 mask with valve, followed by a FFP2 mask without valve and then surgical masks. Finally, the best results were obtained for reusable masks. Taking into account the aforementioned studies, it seems that the use of reusable PPE is the most sustainable from a life cycle perspective, drastically reducing the environmental impacts.
Finally, if we evaluate the economic cost that the use of these face masks entails for each person, once again the best option would be the reusable mask, with an annual cost per person of around 80 euros. The worst results, in terms of wastes, OPE contamination and economic cost, will be for KN95 masks.
4. Conclusions
For the first time, the presence of OPEs in different types of COVID-19 face masks has been evaluated. All masks analysed presented OPE contamination, with values up to 27.7 µg/mask. The highest levels were found in KN95 masks (mean value of 11.6 µg/mask), while the lowest values were those of surgical masks (mean value of 237 ng/mask). Twelve different OPEs were detected being TEP, TPHP, TNBP, TEHP and TClPP the most frequently detected, as well as those presenting the highest concentration values. In this context, the three compounds TNBP, TEHP and TClPP have been classified as potential substances of risk to human health and, recently, USEPA has established reference doses for non-carcinogenic and carcinogenic risks for these compounds.
In order to evaluate the risk of OPE exposure via the use of COVID-19 face masks, experiments at laboratory scale were conducted. The OPE inhalation percentages during the use of masks were around 10%, although in the case of reusable masks, no inhalation of any of the compounds was observed. It is important to note that our tests do not consider the humidity present between the mask and the face when inhaling, and the higher exposure temperatures during summer time. These factors can affect the emission of plasticizers from the mask and our tests could underestimated the amount of plasticizers inhaled.
In any case, and taking in to account this 10% of inhaled compounds, estimated daily intakes via inhalation during the use of masks were calculated and used to estimate the non-CR and CR risks. Obtained values were several orders of magnitude lower than the corresponding threshold level, indicating that the use of COVID-19 face mask is safe for citizens regards OPEs inhalation. However, for some cases such as KN95 masks, CR risk value was only 15 times below the safe value. Taking into account that OPE exposure also occurs by other routes, the sum of all these exposures could bring the values closer to the established safety limits.
Finally, an environmental impact assessment was carried out showing the worst results, in terms of amount of waste generated worldwide as well as the OPE amounts dispersed throughout the environment, for KN95 masks, while the best data were obtained for reusable masks.
Thus, taking into account the results obtained in our study, as well as the doubts that have arisen in several European countries about its effectiveness in the retention of the SARS-CoV-2 virus, we suggest that KN95 masks are the least recommended to be used by the population when considering exposure to OPEs. The other masks tested had similar OPE levels, but the reusable masks seem to retain these compounds better and thus avoid their inhalation. Additional experiments will be necessary to assess their impact once these masks are washed for reuse. In addition, reusable masks also have the least environmental impact and are also the most economical option. However, in situations of relatively high risk of viral inhalation, such as indoors in public spaces with inadecuate ventilation, the best option would appear to be the use of FFP2 masks.
Finally, it is important to note that during the pandemic, a wide variety of reusable masks appeared on the market. It is necessary to also test the OPE levels in these new mask options. We are also conducting studies to evaluate the presence of other types of compounds, such as trace metals, and other plasticizers and chemical additives associated with the materials used to make facial masks.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was supported by the Spanish Ministry of Science and Innovation (Project EXPOPLAS, PID2019-110576RB-I00), the European Union (Nextgeneration EU) and the Generalitat de Catalunya (Consolidated Research Group Water and Soil Quality Unit 2017 SGR 1404 and Atmospheric Geochemistry SGR41). IDAEA-CSIC is a Centre of Excellence Severo Ochoa (Spanish Ministry of Science and Innovation, Project CEX2018-000794-S).
Handling Editor: Heather Stapleton
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envint.2021.106654.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- BOE, 2020. https://www.boe.es/boe/dias/2020/09/30/pdfs/BOE-A-2020-11423.pdf.
- Boix Rodríguez N., Formentini G., Favi C., Marconi M. Engineering design process of face masks based on circularity and Life Cycle Assessment in the constraint of the COVID-19 pandemic. Sustainability. 2021;13:4948. [Google Scholar]
- Giulivo M., Capri E., Eljarrat E., Barceló D. Analysis of organophosphorus flame retardants in environmental and biotic matrices using on-line turbulent flow chromatography-liquid chromatography-tandem mass spectrometry. J. Chromatogr. A. 2016;1474:71–78. doi: 10.1016/j.chroma.2016.10.042. [DOI] [PubMed] [Google Scholar]
- Gunasekaran G.H., Gunasekaran S.S.S., Gunasekaran S.S., Abdul Halim F.H.B. Prevalence and acceptance of face mask practice among individuals visiting hospital during COVID-19 pandemic: An observational study. Preprints. 2020;2020050152 [Google Scholar]
- He C., Wang X.Y., Thai P., Baduel C., Gallen C., Banks A., Bainton P., English K., Mueller J.F. Organophosphate and brominated flame retardants in Australian indoor environments: levels, sources, and preliminary assessment of human exposure. Environ. Pollut. 2018;235:670–679. doi: 10.1016/j.envpol.2017.12.017. [DOI] [PubMed] [Google Scholar]
- He C., Lin C.Y., Mueller J.F. Organophosphate flame retardants in the environment: Source, occurrence, and human exposure. Comprehensive Anal. Chem. 2020;88:341–365. [Google Scholar]
- Kim U.J., Wang Y., Li W., Kannan K. Occurrence of and human exposure to organophosphate flame retardants/plasticizers in indoor air and dust from various microenvironments in the United States. Environ. Int. 2019;125:342–349. doi: 10.1016/j.envint.2019.01.065. [DOI] [PubMed] [Google Scholar]
- Maceira A., Borrull F., Marcé R.M. Occurrence of plastic additives in outdoor air particulate matters from two industrial parks of Tarragona, Spain: Human inhalation intake risk assessment. J. Hazard. Mat. 2019;373:649–659. doi: 10.1016/j.jhazmat.2019.04.014. [DOI] [PubMed] [Google Scholar]
- Meeker J.D., Stapleton H.M. House dust concentrations of organophosphate flame retardants in relation to hormone levels and semen quality parameters. Environ. Health Perspect. 2010;118:318–323. doi: 10.1289/ehp.0901332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivero-Verbel R., Moreno T., Fernández-Arribas J., Reche C., Minguillón M.C., Martins V., Querol X., Johnson-Restrepo B., Eljarrat E. Organophosphate esters in air particles from subway stations. Sci. Total Environ. 2021;769 doi: 10.1016/j.scitotenv.2021.145105. [DOI] [PubMed] [Google Scholar]
- Özdemir L., Azizoğlu M., Yapıcı D. Respirators used by healthcare workers due to the COVID-19 outbreak increase end-tidal carbon dioxide and fractional inspired carbon dioxide pressure. J. Clinical Anesthesia. 2020;66 doi: 10.1016/j.jclinane.2020.109901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacitto A., Amato F., Salmatonidis A., Moreno T., Alastuey A., Reche C., Buonanno G., Benito C., Querol X. Effectiveness of commercial face masks to reduce personal PM exposure. Sci. Total Environ. 2019;650:1582–1590. doi: 10.1016/j.scitotenv.2018.09.109. [DOI] [PubMed] [Google Scholar]
- Poma G., Glynn A., Malarvannan G., Covaci A., Darnerud P.O. Dietary intake of phosphorus flame retardants (PFRs) using Swedish food market basket estimations. Food Chem. Toxicol. 2017;100:1–7. doi: 10.1016/j.fct.2016.12.011. [DOI] [PubMed] [Google Scholar]
- Potluri, P., Needham, P., 2005. Technical textiles for protection. In: Scott, R.A. (Ed.), Technical Textiles for Protection, Elsevier, Chapter 6, 151-175.
- Prata J.C., Silva A.L.P., Walker T.R., Duarte A.C., Rocha-Santos T. COVID-19 Pandemic Repercussions on the Use and Management of Plastics. Environ. Sci. Technol. 2020;2020(54):7760–7765. doi: 10.1021/acs.est.0c02178. [DOI] [PubMed] [Google Scholar]
- Rahimi Z., Shirali G.A., Araban M., Mohammadi M.J., Cheraghian B. Mask use among pedestrians during the Covid-19 pandemic in Southwest Iran: an observational study on 10,440 people. BMC Public Health. 2021;21:133. doi: 10.1186/s12889-020-10152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizan C., Reed M., Bhutta M.F. Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic. J. of the Royal Soc. of Medicine. 2021:1–14. doi: 10.1177/01410768211001583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakhi A.K., Cequier E., Becher R., Bølling A.K., Borgen A.R., Schlabach M., Schmidbauer N., Becher G., Schwarze P., Thomsen C. Concentrations of selected chemicals in indoor air from Norwegian homes and schools. Sci. Tot. Environ. 2019;674:1–8. doi: 10.1016/j.scitotenv.2019.04.086. [DOI] [PubMed] [Google Scholar]
- Sühring R., Scheringer M., Rodgers T.F.M., Jantunen L.M., Diamond M.L. Evaluation of the OECD POV and LRTP screening tool for estimating the long-range transport of organophosphate esters. Environ. Sci. Processes Impacts. 2020;22:207–216. doi: 10.1039/c9em00410f. [DOI] [PubMed] [Google Scholar]
- Tam V.C.W., Tam S.Y., Poon W.K., Law H.K.W., Lee S.W.Y. A reality check on the use of face masks during the COVID-19 outbreak in Hong Kong. EClinicalMedicine. 2020;22 doi: 10.1016/j.eclinm.2020.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USEPA, 2019. Regional Screening Levels (RSLs). https://www.epa.gov/risk/regional-screening-levels-rsls-generic-tables [Accessed on September 2020].
- Van der Veen I., de Boer J. Phosphorus flame retardants: properties, production, environmental occurrence, toxicity and analysis. Chemosphere. 2012;88:1119–1153. doi: 10.1016/j.chemosphere.2012.03.067. [DOI] [PubMed] [Google Scholar]
- WHO, 2020a. Advice on the use of masks in the context of COVID-19. https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak [Accessed on November 2020].
- WHO, 2020b. Shortage of personal protective equipment endangering health workers worldwide. https://www.who.int/news/item/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide. [Accessed on November 2020].
- Wong F., de Wit C.A., Newton S.R. Concentrations and variability of organophosphate esters, halogenated flame retardants, and polybrominated diphenyl ethers in indoor and outdoor air in Stockholm. Sweden. Environ. Pollut. 2018;240:514–522. doi: 10.1016/j.envpol.2018.04.086. [DOI] [PubMed] [Google Scholar]
- WWF, 2020. Nello smaltimento di macherine e guanti serve resposabilità. https://www.wwf.it/scuole/?53500%2FNello-smaltimento-di-mascherine-e-guantiserveresponsabilita– World Wide Fund for Nature. [Accessed on January 2021].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.