Abstract
Purpose of Review:
This review discusses the current state of racial and ethnic inequities in heart failure burden, outcomes, and management. This review also frames considerations for bridging disparities to optimize quality heart failure care across diverse communities.
Recent Findings:
Treatment options for heart failure have diversified and overall heart failure survival has improved with the advent of effective pharmacologic and non-pharmacologic therapies. With increased recognition, some racial/ethnic disparity gaps have narrowed whereas others in heart failure outcomes, utilization of therapies, and advanced therapy access persist or worsen.
Summary:
Racial and ethnic minorities have the highest incidence, prevalence, and hospitalization rates from heart failure. In spite of improved therapies and overall survival, the mortality disparity gap in African American patients has widened over time. Racial/ethnic inequities in access to cardiovascular care, utilization of efficacious guideline-directed heart failure therapies, and allocation of advanced therapies may contribute to disparate outcomes. Strategic and earnest interventions considering social and structural determinants of health are critically needed to bridge racial/ethnic disparities, increase dissemination and implementation of preventative and therapeutic measures, and collectively improve the health and longevity of patients with heart failure.
Keywords: heart failure, cardiovascular disease, outcomes, race, ethnic groups, disparities, health equity
Introduction:
Heart failure (HF) affects 6.2 million U.S. adults and remains a leading cause of death and morbidity.1 As the population ages, HF prevalence is expected to exceed 8 million, impacting 1 in every 33 U.S. adults over the next decade.1, 2 By 2030, HF total costs are anticipated to top $69.8 billion, representing a vast and pressing public health concern.1, 2 Racial and ethnic minorities are disproportionately impacted by HF burden and racial disparities in HF care and outcomes have long been enumerated in the literature. In spite of rapid pharmacologic and therapeutic advancement in HF care and notable gains in overall HF survival, racial and ethnic disparities in HF burden and outcomes persist.1
Race, Ethnicity, and Disparity
Central to the discussion of racial disparities in HF are the concepts of race and health disparities. Race is perhaps best described as a sociocultural construct that aligns groups of people by self-identified or socially perceived physical criteria. Race itself is without an inherent genetic or physiologic basis.3, 4 Genome research has determined that human beings are 99.9% similar, and the 0.1% variation bears a complexity that likely exceeds limited classifications by race.5 Furthermore, singular considerations of race underestimate the vast cultural heterogeneity within phenotypic groups. Ethnicity groups individuals based on common cultural or national traditions.
Race and ethnicity are defined and categorized by the Office of Management and Budget6 for standards in federal statistical reporting and are commonly used designations in economic and epidemiologic studies.3, 7 Disparities have been defined by the Institute of Medicine report3 as racial and ethnic differences in the quality of healthcare. This definition focuses on differences attributable to the operation of healthcare systems and recognized or unrecognized bias or discrimination.3 Healthy People 2020 further defined health disparities as differences in health attributable to economic and/or social disadvantage.8, 9 Inequity reflects differences in disease burden, allocation of resources, and outcomes. Health equity aims to achieve the highest attainable health among all people through fairness in distribution of health resources, determinants, and outcomes.8, 9
Racial Disparities in HF Prevalence, Incidence, and Risk Factors
Self-identified African-American or Black patients, and Hispanic patients have disproportionately high prevalence of HF in comparison to other racial groups.1 In individuals without baseline cardiovascular disease, as included in the Multi-Ethnic Study of Atherosclerosis (MESA), African-American participants had the highest risk of developing HF, followed by Hispanic, White, and Chinese participants (4.6, 3.5, 2.4, and 1.0 per 1000 person-years), respectively.10 Similar findings were noted over a longer follow up period in the Atherosclerosis Risk in Communities (ARIC) Community Surveillance data, in which African-American men and women had the highest burden of new-onset HF cases and the highest age-adjusted 30-day case fatality rate in comparison to White men and women.11, 12
African-American, American Indian, and Hispanic individuals have a higher burden of modifiable risk factors, such as hypertension, obesity, and diabetes that may increase HF risk.1, 2, 13–15 Structural cardiac changes, including left ventricular hypertrophy (LVH) and asymptomatic left ventricular (LV) systolic and diastolic dysfunction are more prevalent, associated with increased clinical HF and mortality risk, and underrecognized in African-American and Hispanic patients.16–18 African-American patients are also more likely to have heart failure from non-ischemic causes.19 Though HF risk increases with age, African-American and Hispanic patients are more likely than White patients to have a younger age of HF onset.12, 13 The Coronary Artery Risk Development in Young Adults (CARDIA) study described a striking 20-fold higher incidence of HF in young Black women and men before the age of 50 (cumulative incidence 1.1% and 0.9%, respectively) versus White women and men (0.08% and 0%, respectively) within this cohort.20 U.S. population projections by the year 2050 forecast increased racial/ethnic diversity with 1 of 3 individuals anticipated to be of Hispanic ethnicity or origin.2 Understanding HF risk factor burden, the earlier age of incident HF, and growing prevalence in an aging, diverse population is critical for effective interventions to attenuate HF disparities.
Racial disparities in HF Mortality
Premature deaths in young and middle-aged African-American individuals have increased and the HF mortality disparity has worsened over the last 18 years.21 A recently published assessment of the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) between 1999 and 2017 demonstrated a 2.97-fold higher and 2.60-fold higher age-adjusted HF-related cardiovascular (CVD) death rate for African-American women and men age 35 to 64, in comparison to White women and men.21, 22 Overall, age-adjusted HF-related CVD death rates increased from 1.16 to 1.43-fold in African-American men versus White men, and from 1.35 to 1.54-fold in African-American women versus White women.21 Thus, age-adjusted HF death rates were highest in African-American men (118.2 per 100,000), followed by non-Hispanic White, American Indian or Alaskan native, Hispanic, and Asian-Pacific Islander men (111.3, 95.0, 69.2, 46.2 per 100,000), respectively.1 In women, the highest age-adjusted HF death rates were observed in African-American women followed by American Indian women.1 In spite of higher risk factor profiles, Hispanic patients with HF with preserved ejection fraction (HFpEF) have lower mortality in comparison to non-Hispanic White patients, but similar mortality risk in HF with reduced EF (HFrEF).14 Comprehensive solutions addressing disparate HF mortality outcomes among racial/ethnic groups are needed.
Racial disparities in HF Hospitalizations
HF hospitalizations (HFH) reflect both acuity of illness and implications for prognosis and mortality. Two or more HF hospitalizations within a year dramatically increases 1-year mortality risk by nearly 30%.23 Trends from the National Inpatient Sample between 2002 and 2013 demonstrate an overall decrease in HF hospitalizations of 30.8%, attributed to improvements in outpatient pharmacologic and device-based management.24 Recently released analysis of the Nationwide Readmission Database, however, suggests that HF hospitalizations after 2014 are on the rise.25 In spite of improvements in overall HF management, age-standardized HF hospitalization rates among African-American men and women have not improved over the last decade and remain two and half-fold higher relative to White men and women.26 Readmission rates at 30-days27 and 1-year28 are also higher in African-American patients relative to White patients.
Trajectories of hospitalization following incident HF diagnosis observed from the Health and Retirement Study have demonstrated significantly higher all-cause hospitalizations in African-American women in comparison to Hispanic and White women.29 In contrast, the HF hospitalization disparity gap has narrowed to near similar or improved age-adjusted rates overall for Hispanic and Asian/Pacific Islander patients relative to White patients.24 In-hospital and immediate post-discharge HF mortality is higher in White patients in comparison to other racial/ethnic groups, possibly related to differences in HF severity at the time of admission.30–33 Racial/ethnic disparities also exist in acute HF triage, admission, and clinical service decisions.34 Several studies have observed less likelihood for African-American and Hispanic patients to receive cardiologists-delivered inpatient HF care, and when appropriate, palliative care during HF hospitalizations.35–38
Racial/ethnic inequity in Heart failure: GDMT, Exercise, Clinical Trials
1. GDMT
The development of efficacious guideline-directed medical therapy (GDMT) for HFrEF collectively remains one of the most impressive and important therapeutic advancements within cardiovascular medicine.39, 40 A substantial portion of the yearly 300,000 HF-related deaths could be prevented with extensive and consistent implementation of GDMT.41, 42 Underutilization of effective GDMT has been observed across racial/ethnic groups. Data from the outpatient CHAMP-HF registry (Change the Management of Patients with Heart Failure) demonstrates that one to two-thirds of eligible patients were not prescribed appropriate GDMT as stable outpatients.43 These findings are similar to underutilization reported in the IMPROVE-HF registry (The Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting) ten years prior.44 Prescribed GDMT in clinical practice is consistently below target dosing achieved in HF clinical trials.
Individuals of Hispanic ethnicity are less likely to be treated with angiotensin receptor neprilysin inhibitors (ARNI), evidenced-based beta blockers (BB), or mineralocorticoid antagonists (MRA).43 In spite of data highlighting the significant benefit of combination hydralazine and isosorbide nitrates (H/I) in African-American patients,41, 45 poor utilization of H/I persists.46 Recent registry data suggests that only 11% and 18% of eligible African-American patients are taking H/I and ARNI, respectively.46 African-American patients, however, are more likely to receive BBs and MRAs.47 Target dosing of BBs and ARNIs is more commonly achieved or approximated in African-American patients, a phenomenon likely related to higher hypertension burden within this population.43 As newer pharmacologic medications with efficacy in HF emerge, such as sodium glucose cotransporter-2 (SGLT2) inhibitors, equity in access and utilization must be a priority. Adequate prescribing and dose titration of GDMT among all demographic groups remains a systemic challenge in achieving quality HF care.
2. Cardiac Rehabilitation, Exercise, and Health Status
Exercise training and cardiac rehabilitation (CR) are safe and effective adjunctive therapies associated with improved quality of life and decreased HF mortality and hospitalizations.48–50 U.S. and European guidelines provide Class I recommendations for stable HF patients to include exercise training in standard HF management.39, 51 Though cardiac rehabilitation is generally underutilized in the overall population, racial and ethnic minorities are significantly less likely to receive cardiac rehabilitation referrals.52 In light of the mortality and functional benefits, significant attention should be focused on eliminating barriers to referral, enrollment, availability, and completion of CR.53–55
Optimization of health status with improved symptoms and quality of life is an important patient-centered focus in HF management. Clinical assessment tools and questionnaires have provided fundamental insights into living with HF. HF-specific health status differs amongst racial/ethnic groups, though reasons for this are incompletely understood. In CHAMP-HF registry data, Hispanic and African-American patients have been shown to have worse HF-specific health status in unadjusted analyses, which persisted with adjustment in Hispanic patients.56 Adjusted analysis in the Tele-HF (Telemonitoring to Improve Heart Failure Outcomes) trial however, did not demonstrate significant racial/ethnic differences in patient-reported health status at three and six months following hospital discharge.57
3. HF Clinical Trial Representation
Clinical trials are imperative to understanding the impact of pharmacotherapies and interventions across the population. Among review of 25 notable randomized clinical trials in heart failure, outcomes by race were reported for fewer than half of the trials (48%).58 In spite of increased HF incidence and hospitalization, African-American participants have been underrepresented in pivotal landmark trials that form foundational quad-therapy for HFrEF management in the modern era, often comprising less than 5.5% of the treatment group.59–62 American Indian participants are also underrepresented. Enrollment of African-American participants has decreased over time, in spite of overall population increases in clinical trial participation.63, 64 A recent review of cardiac surgical trials in ClinicalTrials.gov, including advanced HF therapy trials demonstrated that only 42.7% of these trials reported race information and even fewer (29.2%) reported ethnicity.64 Within this cohort, only 4.0% of trial participants were African-American, whereas Hispanic and Asian participants were 11.2% and 10.4%, respectively.64
Clinical trial enrollment of other racial/ethnic minorities remains modest. Local investigator decisions and independent patient perceptions may significantly impact enrollment in clinical trials.65 This enrollment deficit may contribute to an incomplete reflection of real-world patients with HF in clinical trial populations and is a missed opportunity towards understanding the complexity of therapeutic interventions in a diverse, representative population.65
Racial/ethnic inequity in HF devices, procedures, and advanced therapies
1. ICD and CRT
Implanted cardioverter defibrillators (ICD) have proven mortality benefits and are guideline-recommended in appropriately selected HF patients.39 There has historically been a wide and notable racial/ethnic disparity in ICD utilization. Eligible African-American and Hispanic patients are less likely than White patients to receive counseling for or placement of primary prevention ICDs during or following HF hospitalization.66 However, the ICD racial/ethnic disparity gap is narrowing over time.67, 68
In appropriately selected patients, cardiac resynchronization therapy (CRT) restores left ventricular (LV) synchrony, remodels the LV, improves quality of life, and reduces HF hospitalization and mortality.69–72 However, significant racial/ethnic disparities in CRT utilization persist, in spite of similar benefit across demographic groups.73, 74 Registry data has demonstrated that CRT-eligible African American and Hispanic patients are less likely to receive CRT than White patients, even with adjustment for higher HF burden.75, 76 Racial/ethnic minorities have been underrepresented and underreported in landmark CRT trials. 77
2. Percutaneous Mitral Valve Interventions
In HFrEF patients with symptomatic, severe secondary mitral regurgitation (MR) on maximally-tolerated guideline-directed medical therapy, transcatheter mitral valve repair (TMVr) reduces hospitalization and mortality risk.78 TMVr utilization has increased across the population since its introduction. However, recent evaluation of the National Inpatient Sample has demonstrated that the proportion of African-American patients receiving TMVr has not increased over time similar to White patients.79 African-American patients who did receive this therapy were younger with fewer procedure-related adverse outcomes and had better in-hospital mortality than White patients who were more likely to be older receiving this therapy.74, 79
3. Heart Transplantation and Durable Left Ventricular Assist Devices
Heart transplantation (HT) and durable left ventricular assist devices (LVAD) offer improved quality and duration of life for patients with severe symptomatic HF. Advanced heart failure therapies, however, are not equitably allocated.74 Over the last decade (2008–2018), the proportion of African-American waitlist candidates has modestly decreased (24.8%), and the transplant rate for African-American and Hispanic patients has declined (from 82.0 to 69.2 and from 90.2 to 80 per 100 waitlist-years, respectively).80 African-American patients who are bridged to transplant with an LVAD have a higher burden of pre- and post-transplant mortality, increased likelihood of delisting, and lower likelihood of transplantation in comparison to White and Hispanic patients.81, 82 African-American recipients continue to have the lowest 5-year post-transplant survival.1, 80, 83, 84 Multidisciplinary team care has been associated with more equitable post-transplant survival by race.85
Recent review of the Interagency Registry of Mechanically Assisted Circulatory Support (INTERMACS) demonstrated that destination LVAD therapy was more common in White and African-American patients than Hispanic and Asian patients.86 However, in adjusted analysis of the State Inpatient Databases, African-American and particularly Hispanic patients were less likely to receive LVADs than White patients.87 LVAD utilization increased between 2012 and 2015 in African-American patients, though utilization remains lower than expected considering HF incidence and prevalence.86 The precise reasons for the increased implantation rate in African American patients during this period have not been determined.86, 88 Medicaid expansion under the Affordable Care Act was not associated with increased LVAD implant rates by race or overall.87, 88 Among heart failure providers, Black patient race has been shown to influence decision making, resulting in less consideration for transplantation and more consideration of LVAD therapy in African-American patients represented in clinical vignettes.89 The scope of impact of the 2018 transplant allocation policy changes on equity in advanced HF therapies has not been fully elucidated, and warrants high priority investigation.
Future Directions: Innovation and Equity-focused solutions in HF care delivery
Health equity and the actionable attainment of improved health status and outcomes across populations of HF patients must be a primary focus and investment of the cardiovascular community. Integral to this pursuit is understanding the interface of social determinants of health (SDOH) and their impact on HF risk factors, progression, and outcomes. Healthy People 2030 classifies SDOH into five domains including, healthcare access and quality, economic stability, social and community context, education access and quality, and neighborhoods or built environments.90 Structural, evidenced-based interventions incorporating SDOH are necessary to achieve population-level reductions in racial/ethnic disparities and improve overall HF care and outcomes.
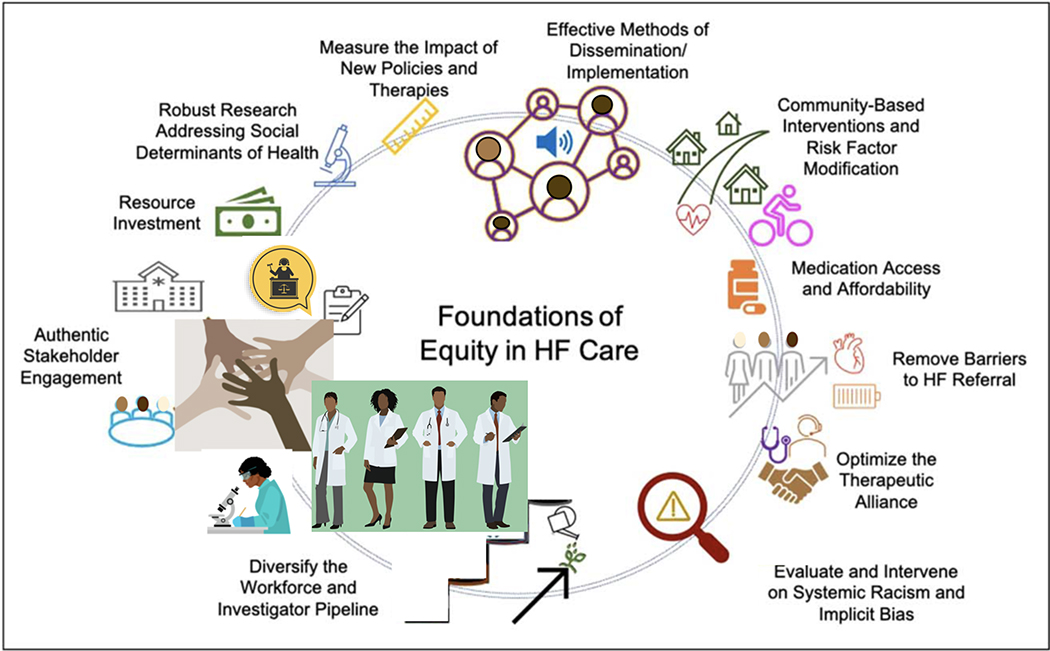
The foundation of health equity interventions (Figure 1) are based on widespread, authentic stakeholder engagement.91 Multi-disciplinary stakeholders include policy makers, health systems, clinicians, researchers, pharmacists, community advocacy groups, insurers, industry leaders, investors, and patients. Resource investment, high quality structural interventions on SDOH, and robust methods of dissemination and implementation focused on guideline-directed HF care are needed.91 Equity in HF care will be predicated on adequate and affordable insurance and prescription coverage, flexible, community-based HF screening and intervention programs, early HF risk factor modification, and improved referral, access, and utilization of HF care, including advanced HF therapies.74 Individualized therapeutic interventions and further insights regarding HF progression may also be aided by conscientious use of personalized and precision medicine tools.
Figure 1:
Foundations of Equity in HF Care
Achieving health equity will require the challenging, but necessary evaluation of and intervention on structural racism and implicit bias within health care delivery. Improved provider-patient and health system-patient relations with culturally-sensitive and language-congruent interactions are foundational to high quality care delivery. Diversification of the physician, advanced practice provider, and investigator workforce is fundamental to meeting the needs of a growing HF population and optimizing care delivery across diverse communities.
Conclusion:
Racial/ethnic inequities in HF burden, access to therapies, and outcomes persist. Notably, the HF mortality disparity in African-American patients has widened and requires urgent attention. Racial/ethnic disparities in HF incidence, hospitalization, clinical trial representation, and CRT utilization persist. Rectifying inadequate GDMT utilization and low enrollment in CR among all patients with HF remains a high-priority. Racial/ethnic disparities in ICD and LVAD utilization have narrowed, though disparities in transplantation rates and outcomes remain. Newer therapies and policies, such as new additions to GDMT, TMVr, and changes to transplant allocation, should be closely followed for impact on equitable patient utilization and access. Innovative, solutions-focused research is paramount to addressing racial/ethnic HF disparities. Evidenced-based interventions, enabled by authentic stakeholder engagement, are the mandate of the present to achieve equity in HF care.
Key Points:
Racial and ethnic disparities in heart failure incidence, hospitalization, and outcomes persist.
Over the last two decades, disparities in heart failure mortality have worsened among African-American patients and requires urgent attention.
Guideline-directed pharmacologic therapy and cardiac rehabilitation are generally underutilized, though notable racial/ethnic disparities exist.
Implantable-cardioverter defibrillators and left ventricular assist devices are increasingly utilized and racial/ethnic disparities have narrowed with these therapies. However, disparities in clinical trial representation, cardiac resynchronization therapy utilization, heart transplantation access, and post-transplant survival persist or worsen.
Structural interventions considering the social determinants of health are required to achieve health equity and optimization of HF care.
Acknowledgments:
Financial Support and Sponsorship: Dr. Breathett has research funding from National Heart, Lung, and Blood Institute (NHLBI) K01HL142848, R25HL126146 subaward 11692sc, and L30HL148881; University of Arizona Health Sciences, Strategic Priorities Faculty Initiative Grant; University of Arizona, Sarver Heart Center, Novel Research Project Award in the Area of Cardiovascular Disease and Medicine, Anthony and Mary Zoia Research Award; and Women As One Escalator Award.
Footnotes
Conflicts of Interest: None
Disclosures: The authors have no relevant financial disclosures to this work.
References:
- 1.Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. March 2020;141(9):e139–e596. doi: 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. May 2013;6(3):606–19. doi: 10.1161/HHF.0b013e318291329a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: confronting racial and ethnic disparities in healthcare. Washington (DC): National Academies Press (US); 2003. [PubMed] [Google Scholar]
- 4.Yancy CW. Race-based therapeutics. Curr Hypertens Rep. August 2008;10(4):276–85. doi: 10.1007/s11906-008-0052-8 [DOI] [PubMed] [Google Scholar]
- 5.Bonham VL, Warshauer-Baker E, Collins FS. Race and ethnicity in the genome era: the complexity of the constructs. Am Psychol. January 2005;60(1):9–15. doi: 10.1037/0003-066X.60.1.9 [DOI] [PubMed] [Google Scholar]
- 6.Office of Management and Budget. Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity. Federal Register; 1997. [Google Scholar]
- 7.Taylor AL. Racial differences and racial disparities: the distinction matters. Circulation. March 2015;131(10):848–50. doi: 10.1161/CIRCULATIONAHA.115.015358 [DOI] [PubMed] [Google Scholar]
- 8.The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I Report: Recommendations for the Framework and Format of Healthy People 2020. October 28, 2008. https://www.healthypeople.gov/sites/default/files/PhaseI_0.pdf
- 9.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. Health Disparities Data. https://www.healthypeople.gov/2020/data-search/health-disparities-data
- 10.Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med. October 2008;168(19):2138–45. doi: 10.1001/archinte.168.19.2138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loehr LR, Rosamond WD, Chang PP, Folsom AR, Chambless LE. Heart failure incidence and survival (from the Atherosclerosis Risk in Communities study). Am J Cardiol. April 2008;101(7):1016–22. doi: 10.1016/j.amjcard.2007.11.061 [DOI] [PubMed] [Google Scholar]
- 12.Carnethon MR, Pu J, Howard G, et al. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation. November 2017;136(21):e393–e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 13.Vivo RP, Krim SR, Cevik C, Witteles RM. Heart failure in Hispanics. J Am Coll Cardiol. April 2009;53(14):1167–75. doi: 10.1016/j.jacc.2008.12.037 [DOI] [PubMed] [Google Scholar]
- 14.Vivo RP, Krim SR, Krim NR, et al. Care and outcomes of Hispanic patients admitted with heart failure with preserved or reduced ejection fraction: findings from get with the guidelines-heart failure. Circ Heart Fail. March 2012;5(2):167–75. doi: 10.1161/CIRCHEARTFAILURE.111.963546 [DOI] [PubMed] [Google Scholar]
- 15.Breathett K, Sims M, Gross M, et al. Cardiovascular Health in American Indians and Alaska Natives: A Scientific Statement From the American Heart Association. Circulation. June 2020;141(25):e948–e959. doi: 10.1161/CIR.0000000000000773** This scientific statement provides important heart failure risk factor data for American Indians and Alaska Natives.
- 16.Lewis AA, Ayers CR, Selvin E, et al. Racial Differences in Malignant Left Ventricular Hypertrophy and Incidence of Heart Failure: A Multicohort Study. Circulation. March 2020;141(12):957–967. doi: 10.1161/CIRCULATIONAHA.119.043628* Malignant left ventricular hypertrophy was found to be more prevalent in Black participants in comparison to White participants in pooled data from three population cohorts. Individuals with malignant left ventricular hypertrophy had a higher risk of incident heart failure.
- 17.Yeboah J, Rodriguez CJ, Stacey B, et al. Prognosis of individuals with asymptomatic left ventricular systolic dysfunction in the multi-ethnic study of atherosclerosis (MESA). Circulation. December 2012;126(23):2713–9. doi: 10.1161/CIRCULATIONAHA.112.112201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehta H, Armstrong A, Swett K, et al. Burden of Systolic and Diastolic Left Ventricular Dysfunction Among Hispanics in the United States: Insights From the Echocardiographic Study of Latinos. Circ Heart Fail. April 2016;9(4):e002733. doi: 10.1161/CIRCHEARTFAILURE.115.002733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morris AA, Nayak A, Ko YA, et al. Racial Differences in Diuretic Efficiency, Plasma Renin, and Rehospitalization in Subjects With Acute Heart Failure. Circ Heart Fail. July 2020;13(7):e006827. doi: 10.1161/CIRCHEARTFAILURE.119.006827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bibbins-Domingo K, Pletcher MJ, Lin F, et al. Racial differences in incident heart failure among young adults. N Engl J Med. March 2009;360(12):1179–90. doi: 10.1056/NEJMoa0807265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glynn P, Lloyd-Jones DM, Feinstein MJ, Carnethon M, Khan SS. Disparities in Cardiovascular Mortality Related to Heart Failure in the United States. J Am Coll Cardiol. May 2019;73(18):2354–2355. doi: 10.1016/j.jacc.2019.02.042** This research letter highlights significantly higher heart failure related cardiovascular disease mortality among young and middle-aged Black patients, with worsening of this disparity in recent years.
- 22.Nayak A, Hicks AJ, Morris AA. Understanding the Complexity of Heart Failure Risk and Treatment in Black Patients. Circ Heart Fail. August 2020;13(8):e007264. doi: 10.1161/CIRCHEARTFAILURE.120.007264** This review provides an in-depth exploration of factors contributing to disparate HF risk and outcomes in African-American patients.
- 23.Kommuri NV, Koelling TM, Hummel SL. The impact of prior heart failure hospitalizations on long-term mortality differs by baseline risk of death. Am J Med. February 2012;125(2):209.e9–209.e15. doi: 10.1016/j.amjmed.2011.06.014 [DOI] [PubMed] [Google Scholar]
- 24.Ziaeian B, Kominski GF, Ong MK, Mays VM, Brook RH, Fonarow GC. National Differences in Trends for Heart Failure Hospitalizations by Sex and Race/Ethnicity. Circ Cardiovasc Qual Outcomes. July 2017;10(7)doi: 10.1161/CIRCOUTCOMES.116.003552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agarwal MA, Fonarow GC, Ziaeian B. National Trends in Heart Failure Hospitalizations and Readmissions From 2010 to 2017. JAMA Cardiol. February 2021;doi: 10.1001/jamacardio.2020.7472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fonarow GC, Ziaeian B. Gaps in Adherence to Guideline-Directed Medical Therapy Before Defibrillator Implantation. J Am Coll Cardiol. March 2016;67(9):1070–1073. doi: 10.1016/j.jacc.2015.12.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. February 2011;305(7):675–81. doi: 10.1001/jama.2011.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rathore SS, Foody JM, Wang Y, et al. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. JAMA. May 2003;289(19):2517–24. doi: 10.1001/jama.289.19.2517 [DOI] [PubMed] [Google Scholar]
- 29.Dupre ME, Gu D, Xu H, Willis J, Curtis LH, Peterson ED. Racial and Ethnic Differences in Trajectories of Hospitalization in US Men and Women With Heart Failure. J Am Heart Assoc. November 2017;6(11)doi: 10.1161/JAHA.117.006290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akintoye E, Briasoulis A, Egbe A, et al. National Trends in Admission and In-Hospital Mortality of Patients With Heart Failure in the United States (2001–2014). J Am Heart Assoc. November 2017;6(12)doi: 10.1161/JAHA.117.006955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gordon HS, Nowlin PR, Maynard D, Berbaum ML, Deswal A. Mortality after hospitalization for heart failure in blacks compared to whites. Am J Cardiol. March 2010;105(5):694–700. doi: 10.1016/j.amjcard.2009.10.051 [DOI] [PubMed] [Google Scholar]
- 32.Durstenfeld MS, Ogedegbe O, Katz SD, Park H, Blecker S. Racial and Ethnic Differences in Heart Failure Readmissions and Mortality in a Large Municipal Healthcare System. JACC Heart Fail. November 2016;4(11):885–893. doi: 10.1016/j.jchf.2016.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ziaeian B, Heidenreich PA, Xu H, et al. Medicare Expenditures by Race/Ethnicity After Hospitalization for Heart Failure With Preserved Ejection Fraction. JACC Heart Fail. May 2018;6(5):388–397. doi: 10.1016/j.jchf.2017.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lo AX, Donnelly JP, Durant RW, et al. A National Study of U.S. Emergency Departments: Racial Disparities in Hospitalizations for Heart Failure. Am J Prev Med. November 2018;55(5 Suppl 1):S31–S39. doi: 10.1016/j.amepre.2018.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breathett K, Liu WG, Allen LA, et al. African Americans Are Less Likely to Receive Care by a Cardiologist During an Intensive Care Unit Admission for Heart Failure. JACC Heart Fail. May 2018;6(5):413–420. doi: 10.1016/j.jchf.2018.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eberly LA, Richterman A, Beckett AG, et al. Identification of Racial Inequities in Access to Specialized Inpatient Heart Failure Care at an Academic Medical Center. Circ Heart Fail. November 2019;12(11):e006214. doi: 10.1161/CIRCHEARTFAILURE.119.006214* This observational study showed lower likelihood of admission to a cardiology service for Black and LatinX patients with heart failure. Notably, cardiology service care was associated with lower likelihood of readmission, independent of race/ethnicity.
- 37.Auerbach AD, Hamel MB, Califf RM, et al. Patient characteristics associated with care by a cardiologist among adults hospitalized with severe congestive heart failure. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Coll Cardiol. December 2000;36(7):2119–25. doi: 10.1016/s0735-1097(00)01005-6 [DOI] [PubMed] [Google Scholar]
- 38.Khan MZ, Khan MU, Munir MB. Trends and disparities in palliative care encounters in acute heart failure admissions; insight from national inpatient sample. Cardiovasc Revasc Med. August 2020;doi: 10.1016/j.carrev.2020.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. October 2013;128(16):e240–327. doi: 10.1161/CIR.0b013e31829e8776 [DOI] [PubMed] [Google Scholar]
- 40.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. August 2017;136(6):e137–e161. doi: 10.1161/CIR.0000000000000509 [DOI] [PubMed] [Google Scholar]
- 41.Fonarow GC, Hernandez AF, Solomon SD, Yancy CW. Potential Mortality Reduction With Optimal Implementation of Angiotensin Receptor Neprilysin Inhibitor Therapy in Heart Failure. JAMA Cardiol. September 2016;1(6):714–7. doi: 10.1001/jamacardio.2016.1724 [DOI] [PubMed] [Google Scholar]
- 42.Fonarow GC, Yancy CW, Hernandez AF, Peterson ED, Spertus JA, Heidenreich PA. Potential impact of optimal implementation of evidence-based heart failure therapies on mortality. Am Heart J. June 2011;161(6):1024–30.e3. doi: 10.1016/j.ahj.2011.01.027 [DOI] [PubMed] [Google Scholar]
- 43.Greene SJ, Butler J, Albert NM, et al. Medical Therapy for Heart Failure With Reduced Ejection Fraction: The CHAMP-HF Registry. J Am Coll Cardiol. July 2018;72(4):351–366. doi: 10.1016/j.jacc.2018.04.070 [DOI] [PubMed] [Google Scholar]
- 44.Fonarow GC, Albert NM, Curtis AB, et al. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF). Circulation. August 2010;122(6):585–96. doi: 10.1161/CIRCULATIONAHA.109.934471 [DOI] [PubMed] [Google Scholar]
- 45.Taylor AL, Ziesche S, Yancy C, et al. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. November 2004;351(20):2049–57. doi: 10.1056/NEJMoa042934 [DOI] [PubMed] [Google Scholar]
- 46.Giblin EM, Adams KF, Hill L, et al. Comparison of Hydralazine/Nitrate and Angiotensin Receptor Neprilysin Inhibitor Use Among Black Versus Nonblack Americans With Heart Failure and Reduced Ejection Fraction (from CHAMP-HF). Am J Cardiol. December 2019;124(12):1900–1906. doi: 10.1016/j.amjcard.2019.09.020** This study examined the Change the Management of Patients with Heart Failure Registry for frequency of hydralazine/nitrates versus sacubitril/valsartan use in Black patients. Overall, use of both medications was low.
- 47.Reynolds D, Albert NM, Curtis AB, et al. Race and improvements in the use of guideline-recommended therapies for patients with heart failure: findings from IMPROVE HF. J Natl Med Assoc. 2012 May-Jun 2012;104(5–6):287–98. doi: 10.1016/s0027-9684(15)30156-5 [DOI] [PubMed] [Google Scholar]
- 48.Flynn KE, Piña IL, Whellan DJ, et al. Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. April 2009;301(14):1451–9. doi: 10.1001/jama.2009.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Piepoli MF, Davos C, Francis DP, Coats AJ, Collaborative E. Exercise training meta-analysis of trials in patients with chronic heart failure (ExTraMATCH). BMJ. January 2004;328(7433):189. doi: 10.1136/bmj.37938.645220.EE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.O’Connor CM, Whellan DJ, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. April 2009;301(14):1439–50. doi: 10.1001/jama.2009.454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. July 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 52.Li S, Fonarow GC, Mukamal K, et al. Sex and Racial Disparities in Cardiac Rehabilitation Referral at Hospital Discharge and Gaps in Long-Term Mortality. J Am Heart Assoc. April 2018;7(8)doi: 10.1161/JAHA.117.008088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. December 2011;124(25):2951–60. doi: 10.1161/CIR.0b013e31823b21e2 [DOI] [PubMed] [Google Scholar]
- 54.Mead H, Ramos C, Grantham SC. Drivers of Racial and Ethnic Disparities in Cardiac Rehabilitation Use: Patient and Provider Perspectives. Med Care Res Rev. June 2016;73(3):251–82. doi: 10.1177/1077558715606261 [DOI] [PubMed] [Google Scholar]
- 55.Leon AS, Franklin BA, Costa F, et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation. January 2005;111(3):369–76. doi: 10.1161/01.CIR.0000151788.08740.5C [DOI] [PubMed] [Google Scholar]
- 56.Khariton Y, Nassif ME, Thomas L, et al. Health Status Disparities by Sex, Race/Ethnicity, and Socioeconomic Status in Outpatients With Heart Failure. JACC Heart Fail. June 2018;6(6):465–473. doi: 10.1016/j.jchf.2018.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Qian F, Parzynski CS, Chaudhry SI, et al. Racial Differences in Heart Failure Outcomes: Evidence From the Tele-HF Trial (Telemonitoring to Improve Heart Failure Outcomes). JACC Heart Fail. July 2015;3(7):531–538. doi: 10.1016/j.jchf.2015.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sullivan LT, Randolph T, Merrill P, et al. Representation of black patients in randomized clinical trials of heart failure with reduced ejection fraction. Am Heart J. March 2018;197:43–52. doi: 10.1016/j.ahj.2017.10.025 [DOI] [PubMed] [Google Scholar]
- 59.McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. September 2014;371(11):993–1004. doi: 10.1056/NEJMoa1409077 [DOI] [PubMed] [Google Scholar]
- 60.McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. November 2019;381(21):1995–2008. doi: 10.1056/NEJMoa1911303 [DOI] [PubMed] [Google Scholar]
- 61.Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. June 1999;353(9169):2001–7. [PubMed] [Google Scholar]
- 62.Zannad F, McMurray JJ, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. January 2011;364(1):11–21. doi: 10.1056/NEJMoa1009492 [DOI] [PubMed] [Google Scholar]
- 63.Piña IL, Apstein CS, Balady GJ, et al. Exercise and heart failure: A statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation. March 2003;107(8):1210–25. doi: 10.1161/01.cir.0000055013.92097.40 [DOI] [PubMed] [Google Scholar]
- 64.Preventza O, Critsinelis A, Simpson K, et al. Sex, Racial, and Ethnic Disparities in US Cardiovascular Trials in More Than 230,000 Patients. Ann Thorac Surg. November 2020;doi: 10.1016/j.athoracsur.2020.08.075** This study evaluated gender and racial/ethnic disparities in 178 cardiac surgery trials, including LVAD and HT trials. Less than half of these trials included race/ethnicity information. African-American participants had the lowest representation of the reported groups in the trials.
- 65.Greene SJ, DeVore AD, Sheng S, et al. Representativeness of a Heart Failure Trial by Race and Sex: Results From ASCEND-HF and GWTG-HF. JACC Heart Fail. November 2019;7(11):980–992. doi: 10.1016/j.jchf.2019.07.011 ** This analysis compared patients enrolled in the ASCEND-HF clinical trial versus a real-world HF population from GWTG-HF that met clinical trial eligibility criteria. Notably, worse clinical outcomes in the real-world population were observed, primarily driven by differences in outcomes among black patients and female patients.
- 66.Hess PL, Hernandez AF, Bhatt DL, et al. Sex and Race/Ethnicity Differences in Implantable Cardioverter-Defibrillator Counseling and Use Among Patients Hospitalized With Heart Failure: Findings from the Get With The Guidelines-Heart Failure Program. Circulation. August 2016;134(7):517–26. doi: 10.1161/CIRCULATIONAHA.115.021048 [DOI] [PubMed] [Google Scholar]
- 67.Al-Khatib SM, Hellkamp AS, Hernandez AF, et al. Trends in use of implantable cardioverter-defibrillator therapy among patients hospitalized for heart failure: have the previously observed sex and racial disparities changed over time? Circulation. March 2012;125(9):1094–101. doi: 10.1161/CIRCULATIONAHA.111.066605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Patel NJ, Edla S, Deshmukh A, et al. Gender, Racial, and Health Insurance Differences in the Trend of Implantable Cardioverter-Defibrillator (ICD) Utilization: A United States Experience Over the Last Decade. Clin Cardiol. February 2016;39(2):63–71. doi: 10.1002/clc.22496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. April 2005;352(15):1539–49. doi: 10.1056/NEJMoa050496 [DOI] [PubMed] [Google Scholar]
- 70.Cazeau S, Leclercq C, Lavergne T, et al. Effects of multisite biventricular pacing in patients with heart failure and intraventricular conduction delay. N Engl J Med. March 2001;344(12):873–80. doi: 10.1056/NEJM200103223441202 [DOI] [PubMed] [Google Scholar]
- 71.Abraham WT, Fisher WG, Smith AL, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med. June 2002;346(24):1845–53. doi: 10.1056/NEJMoa013168 [DOI] [PubMed] [Google Scholar]
- 72.Auricchio A, Stellbrink C, Sack S, et al. Long-term clinical effect of hemodynamically optimized cardiac resynchronization therapy in patients with heart failure and ventricular conduction delay. J Am Coll Cardiol. June 2002;39(12):2026–33. doi: 10.1016/s0735-1097(02)01895-8 [DOI] [PubMed] [Google Scholar]
- 73.Ziaeian B, Zhang Y, Albert NM, et al. Clinical effectiveness of CRT and ICD therapy in heart failure patients by racial/ethnic classification: insights from the IMPROVE HF registry. J Am Coll Cardiol. August 2014;64(8):797–807. doi: 10.1016/j.jacc.2014.05.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mwansa H, Lewsey S, Mazimba S, Breathett K. Racial/Ethnic and Gender Disparities in Heart Failure with Reduced Ejection Fraction Outcomes Section: Non-pharmacologic Therapy: Surgery, Ventricular Assist Devices, Biventricular Pacing, and Exercise. Current Heart Failure Reports 2021;** This review summarizes gender and racial/ethnic disparities in non-pharmacologic heart failure therapies.
- 75.Farmer SA, Kirkpatrick JN, Heidenreich PA, Curtis JP, Wang Y, Groeneveld PW. Ethnic and racial disparities in cardiac resynchronization therapy. Heart Rhythm. March 2009;6(3):325–31. doi: 10.1016/j.hrthm.2008.12.018 [DOI] [PubMed] [Google Scholar]
- 76.Sridhar AR, Yarlagadda V, Parasa S, et al. Cardiac Resynchronization Therapy: US Trends and Disparities in Utilization and Outcomes. Circ Arrhythm Electrophysiol. March 2016;9(3):e003108. doi: 10.1161/CIRCEP.115.003108 [DOI] [PubMed] [Google Scholar]
- 77.Fontaine JM, Franklin SM, Gupta A, Kang CU. Mortality in African-Americans Following Cardiac Resynchronization Therapy: A Single Center Experience. J Natl Med Assoc. February 2016;108(1):30–9. doi: 10.1016/j.jnma.2015.12.005 [DOI] [PubMed] [Google Scholar]
- 78.Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med. December 2018;379(24):2307–2318. doi: 10.1056/NEJMoa1806640 [DOI] [PubMed] [Google Scholar]
- 79.Elbadawi A, Mahmoud K, Elgendy IY, et al. Racial Disparities in the Utilization and Outcomes of Transcatheter Mitral Valve Repair: Insights From a National Database. Cardiovasc Revasc Med. November 2020;21(11):1425–1430. doi: 10.1016/j.carrev.2020.04.034* This observational study showed that TMVr use is increasing over time, though the proportion of African-American patients undergoing the procedure has not significantly changed. This study also showed that White patients undergoing TMVr were typically older with higher in-hospital mortality.
- 80.Colvin M, Smith JM, Hadley N, et al. OPTN/SRTR 2018 Annual Data Report: Heart. Am J Transplant. January 2020;20 Suppl s1:340–426. doi: 10.1111/ajt.15676 [DOI] [PubMed] [Google Scholar]
- 81.Okoh AK, Selevanny M, Singh S, et al. Racial disparities and outcomes of left ventricular assist device implantation as a bridge to heart transplantation. ESC Heart Fail. October 2020;7(5):2744–2751. doi: 10.1002/ehf2.12866* This study reviewed 10 years of data of patients with continuous flow LVADs as a bridge to transplant from the United Network of Organ Sharing (UNOS). The study team found significantly lower likelihood of transplantation and higher waitlist morbidity and mortality in African-American patients in comparison to other groups.
- 82.Lui C, Fraser CD, Zhou X, et al. Racial Disparities in Patients Bridged to Heart Transplantation With Left Ventricular Assist Devices. Ann Thorac Surg. October 2019;108(4):1122–1126. doi: 10.1016/j.athoracsur.2019.03.073* This study reviewed 13 years of UNOS data and found that African-American patients bridged with LVAD had higher risk of post-transplant graft failure and mortality at 5 years in comparison to other groups.
- 83.Kilic A, Higgins RS, Whitson BA. Racial disparities in outcomes of adult heart transplantation. Circulation. March 2015;131(10):882–9. doi: 10.1161/CIRCULATIONAHA.114.011676 [DOI] [PubMed] [Google Scholar]
- 84.Morris AA, Kransdorf EP, Coleman BL, Colvin M. Racial and ethnic disparities in outcomes after heart transplantation: A systematic review of contributing factors and future directions to close the outcomes gap. J Heart Lung Transplant. August 2016;35(8):953–61. doi: 10.1016/j.healun.2016.01.1231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pamboukian SV, Costanzo MR, Meyer P, Bartlett L, McLeod M, Heroux A. Influence of race in heart failure and cardiac transplantation: mortality differences are eliminated by specialized, comprehensive care. J Card Fail. April 2003;9(2):80–6. doi: 10.1054/jcaf.2003.11 [DOI] [PubMed] [Google Scholar]
- 86.Breathett K, Allen LA, Helmkamp L, et al. Temporal Trends in Contemporary Use of Ventricular Assist Devices by Race and Ethnicity. Circ Heart Fail. August 2018;11(8):e005008. doi: 10.1161/CIRCHEARTFAILURE.118.005008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang X, Luke AA, Vader JM, Maddox TM, Joynt Maddox KE. Disparities and Impact of Medicaid Expansion on Left Ventricular Assist Device Implantation and Outcomes. Circ Cardiovasc Qual Outcomes. June 2020;13(6):e006284. doi: 10.1161/CIRCOUTCOMES.119.006284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Breathett KK, Knapp SM, Wightman P, et al. Is the Affordable Care Act Medicaid Expansion Linked to Change in Rate of Ventricular Assist Device Implantation for Blacks and Whites? Circ Heart Fail. April 2020;13(4):e006544. doi: 10.1161/CIRCHEARTFAILURE.119.006544** This study used data from the State Inpatient Databases from multiple states and found that the Affordable Care Act Medicaid expansion did not significantly increase LVAD implantation rates by race.
- 89.Breathett K, Yee E, Pool N, et al. Does Race Influence Decision Making for Advanced Heart Failure Therapies? J Am Heart Assoc. November 2019;8(22):e013592. doi: 10.1161/JAHA.119.013592** This study examined advanced heart failure medical decision making through clinical vignettes and found that Black race influenced decision making regarding LVAD or transplantation. African-American vignette patients were less likely to be offered transplantation than White vignette patients, but were more likely to be offered LVAD therapy.
- 90.Office of Disease Prevention and Health Promotion. Social determinants of health. Healthy People 2030. U.S. Department of Health and Human Services. 2021. Available at: https://health.gov/healthypeople/objectives-and-data/social-determinants-health. [Accessed 15 January 2021] [Google Scholar]
- 91.Brown AF, Ma GX, Miranda J, et al. Structural Interventions to Reduce and Eliminate Health Disparities. Am J Public Health. January 2019;109(S1):S72–S78. doi: 10.2105/AJPH.2018.304844 [DOI] [PMC free article] [PubMed] [Google Scholar]