Abstract
Background
This review was published originally in 1999 and was updated in 2001, 2002, 2009, 2017, and 2020. Updating was deemed necessary due to the high incidence of hip fractures, the large number of official societies providing recommendations on this condition, the possibility that perioperative peripheral nerve blocks (PNBs) may improve patient outcomes, and the major role that PNBs may play in reducing preoperative and postoperative opioid use for analgesia.
Objectives
To compare PNBs used as preoperative analgesia, as postoperative analgesia, or as a supplement to general anaesthesia versus no nerve block (or sham block) for adults with hip fracture. Outcomes were pain on movement at 30 minutes after block placement, acute confusional state, myocardial infarction, chest infection, death, time to first mobilization, and costs of an analgesic regimen for single‐injection blocks.
We undertook the update to look for new studies and to update the methods to reflect Cochrane standards.
Search methods
For the updated review, we searched the following databases: the Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 11), in the Cochrane Library; MEDLINE (Ovid SP, 1966 to November 2019); Embase (Ovid SP, 1974 to November 2019); and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO, 1982 to November 2019), as well as trial registers and reference lists of relevant articles.
Selection criteria
We included randomized controlled trials (RCTs) assessing use of PNBs compared with no nerve block (or sham block) as part of the care provided for adults 16 years of age and older with hip fracture.
Data collection and analysis
Two review authors independently screened new trials for inclusion, assessed trial quality using the Cochrane Risk of Bias‐2 tool, and extracted data. When appropriate, we pooled results of outcome measures. We rated the certainty of evidence using the GRADE approach.
Main results
We included 49 trials (3061 participants; 1553 randomized to PNBs and 1508 to no nerve block (or sham block)). For this update, we added 18 new trials. Trials were published from 1981 to 2020. Trialists followed participants for periods ranging from 5 minutes to 12 months. The average age of participants ranged from 59 to 89 years. People with dementia were often excluded from the included trials. Additional analgesia was available for all participants.
Results of 11 trials with 503 participants show that PNBs reduced pain on movement within 30 minutes of block placement (standardized mean difference (SMD) ‐1.05, 95% confidence interval (CI) ‐1.25 to ‐0.86; equivalent to ‐2.5 on a scale from 0 to 10; high‐certainty evidence). Effect size was proportionate to the concentration of local anaesthetic used (P = 0.0003). Based on 13 trials with 1072 participants, PNBs reduce the risk of acute confusional state (risk ratio (RR) 0.67, 95% CI 0.50 to 0.90; number needed to treat for an additional beneficial outcome (NNTB) 12, 95% CI 7 to 47; high‐certainty evidence). For myocardial infarction, there were no events in one trial with 31 participants (RR not estimable; low‐certainty evidence). From three trials with 131 participants, PNBs probably reduce the risk for chest infection (RR 0.41, 95% CI 0.19 to 0.89; NNTB 7, 95% CI 5 to 72; moderate‐certainty evidence). Based on 11 trials with 617 participants, the effects of PNBs on mortality within six months are uncertain due to very serious imprecision (RR 0.87, 95% CI 0.47 to 1.60; low‐certainty evidence). From three trials with 208 participants, PNBs likely reduce time to first mobilization (mean difference (MD) ‐10.80 hours, 95% CI ‐12.83 to ‐8.77 hours; moderate‐certainty evidence). One trial with 75 participants indicated there may be a small reduction in the cost of analgesic drugs with a single‐injection PNB (MD ‐4.40 euros, 95% CI ‐4.84 to ‐3.96 euros; low‐certainty evidence).
We identified 29 ongoing trials, of which 15 were first posted or at least were last updated after 1 January 2018.
Authors' conclusions
PNBs reduce pain on movement within 30 minutes after block placement, risk of acute confusional state, and probably also reduce the risk of chest infection and time to first mobilization. There may be a small reduction in the cost of analgesic drugs for single‐injection PNB. We did not find a difference for myocardial infarction and mortality, but the numbers of participants included for these two outcomes were insufficient. Although randomized clinical trials may not be the best way to establish risks associated with an intervention, our review confirms low risks of permanent injury associated with PNBs, as found by others.
Some trials are ongoing, but it is unclear whether any further RCTs should be registered, given the benefits found. Good‐quality non‐randomized trials with appropriate sample size may help to clarify the potential effects of PNBs on myocardial infarction and mortality.
Plain language summary
Do local anaesthetic nerve blocks provide effective pain relief for adults with a hip fracture?
What is a peripheral nerve block?
A peripheral nerve block (PNB) is an injection of local anaesthetic close to nerves to block pain signals to the brain. PNBs can be used alone or together with other pain relief medicines. They may be given as a single injection or continuously, using a catheter (drip).
Why is this question important?
Hip fractures commonly occur in older people. Surgery is usually needed to repair the bone. Hip fractures are very painful. Opioids such as morphine, which are strong painkillers, are often used to manage hip fracture pain. Older people do not tolerate high doses of opioids well. Also, people with hip fracture may have complications such as confusion, myocardial infarction and chest infection.
By reducing the use of opioids and better treating pain, PNBs may improve the mobility of people with hip fracture and reduce risks of complications.
What did we want to find out?
We wanted to know whether using PNBs compared to no nerve block (no block at all or a placebo nerve block), in people with hip fracture could reduce:
• pain on movement;
• confusion, myocardial infarction, and chest infection;
• death from any cause within six months;
• length of time until people were mobile after surgery; and
• costs of drugs used to manage pain.
What did we do?
We searched medical databases for studies that investigated the use of PNBs versus no effective nerve block (i.e. no block at all or a placebo block) for pain in people with hip fracture. Study participants had to be over 16 years of age and had to have a hip fracture. We looked for randomized controlled trials (RCTs), where the treatment people receive is decided randomly.
What we found
We included 49 studies with 3061 participants (average age 59 to 89 years); 1553 participants received PNBs and 1508 received no nerve block. Additional pain relief, including opioids, was available for all participants when required. Studies were conducted in various countries and published between 1980 and 2020. Twenty‐six studies received non‐commercial funding, and the source of funding was not stated for the other studies.
Main results
PNBs reduced pain on movement by 2.5 on a scale of 1 to 10, compared with no nerve block (11 studies, 503 participants). PNBs reduced the risk of confusion; for every 12 people with a hip fracture, one person less will become confused with PNBs (13 studies, 1072 participants). We did not find a difference in risk of myocardial infarction (1 study, 31 participants).
PNBs probably reduce the risk of chest infection (3 studies, 131 participants) and time to first mobilization after surgery by 11 hours (3 studies, 208 participants). We did not find a difference in deaths from any cause within six months (11 studies, 617 participants). Costs of drugs used for pain management were slightly lower when a single‐injection PNB was compared to no PNB (1 study, 75 participants).
How reliable are the results?
Our confidence (certainty) in the evidence for reduced pain on movement and for reduced confusion was high; we are moderately confident in the evidence for reduced chest infection. However, we are less confident about the evidence for myocardial infarction, death, time to first mobilization, and costs of drugs used for pain management, mainly because this evidence came from small studies with few participants.
What does this mean?
We found enough good‐quality evidence to support the use of PNBs in patients with hip fracture. Larger studies are required to clarify the effects of PNBs on myocardial infarction and death.
How up‐to‐date is this review?
This is an updated review. Evidence is up‐to‐date to 16 November 2019.
Summary of findings
Summary of findings 1. Peripheral nerve blocks for hip fracture.
| Peripheral nerve blocks for hip fracture | ||||||
| Patient or population: patients with hip fracture Settings: for outcomes included in this table, studies were conducted in Argentina (N = 1), Canada (N = 1), Chile (N = 1), China (N = 4), Denmark (N = 1), France (N = 2), Germany (N = 1), Greece (N = 2), Ireland (N = 1), Japan (N = 1), Korea (N = 1), Nepal (N = 1), South Africa (N = 1), Spain (N = 2), Sweden (N = 2), Switzerland (N=1), Turkey (N = 2), United Kingdom (N = 5), and United States of America (N = 2) Intervention: peripheral nerve blocks Comparison: no block | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Systemic analgesia | Peripheral nerve blocks | |||||
| Pain on movement at 30 minutes after block placement Follow‐up: 20 to 45 minutes | Mean pain on movement at 30 minutes after block placement in the intervention groups was 1.05 standard deviations lower (1.25 to 0.86 lower) | 503 (11 studies) | ⊕⊕⊕⊕ higha,b | |||
|
Acute confusional state Follow‐up: 0 to 30 days |
Study population | RR 0.67 (0.50 to 0.90) | 1072 (13 studies) | ⊕⊕⊕⊕ higha,c | ||
| 181 per 1000 | 121 per 1000 (90 to 163) | |||||
| Low | ||||||
| 150 per 1000 | 101 per 1000 (75 to 135) | |||||
| High | ||||||
| 350 per 1000 | 235 per 1000 (175 to 315) | |||||
|
Myocardial infarction Follow‐up: 0 to 30 days |
N/A | N/A | 31 (1 study) | ⊕⊕⊝⊝ lowd | ||
|
Chest infections Follow‐up: 0 to 30 days |
Study population | RR 0.41 (0.19 to 0.89) | 131 (3 studies) | ⊕⊕⊕⊝ moderatee,f | ||
| 269 per 1000 | 110 per 1000 (51 to 239) | |||||
| Low | ||||||
| 50 per 1000 | 20 per 1000 (9 to 44) | |||||
| High | ||||||
| 200 per 1000 | 82 per 1000 (38 to 178) | |||||
| Death Follow‐up: 0 to 6 months | Study population | RR 0.87 (0.47 to 1.60) | 617 (11 studies) | ⊕⊕⊝⊝ lowd | ||
| 68 per 1000 | 59 per 1000 (32 to 109) | |||||
| Low | ||||||
| 25 per 1000 | 22 per 1000 (12 to 40) | |||||
| High | ||||||
| 150 per 1000 | 131 per 1000 (70 to 240) | |||||
|
Time to first mobilization Follow‐up: in‐hospital |
Mean time to first mobilization in intervention groups was 10.80 hours lower (12.83 to 8.77 lower) | 208 (3 studies) | ⊕⊕⊕⊝ moderatee | |||
|
Cost of analgesic regimens for single‐injection blocks Follow‐up: in‐hospital |
Mean cost of analgesic regimens for single‐injection blocks in intervention groups was 4.40 euros lower (4.84 to 3.96 lower) | 75 (1 study) | ⊕⊕⊕⊝ moderated,g | |||
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; N/A: not applicable; RR: risk ratio. | ||||||
| GRADE Working Group grades for certainty of evidence. High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aThe effect was still present even when trials at high risk of bias were withdrawn from the analysis, or when a correction for the possibility of publication bias was applied.
bThe difference was equivalent to 2.5 on a scale from 0 to 10.
cThe number needed to treat for additional beneficial outcome was 12 (95% confidence interval 7 to 47).
dDowngraded by two levels for imprecision.
eDowngraded by one level for imprecision.
fThe number needed to treat for additional beneficial outcome was 7 (95% confidence interval 5 to 72).
gMean costs in 2009 euros.
Background
Description of the condition
Among women 55 years of age and older in the USA, the Nationwide Inpatient Sample (NIS) for 2000 to 2010 reported 4.9 million hospitalizations for osteoporotic fractures (2.6 million for hip fractures) − a higher number of hospitalizations than for myocardial infarction (2.9 million), stroke (3.0 million), and breast cancer (0.7 million) (Singer 2015). Osteoporotic fractures accounted for more than 40% of hospitalizations for these four outcomes, with an age‐adjusted rate of 1124 admissions per 100,000 person‐years. The annual total population facility‐related hospital cost was highest for hospitalizations due to osteoporotic fractures (USD 5.1 billion), followed by myocardial infarction (USD 4.3 billion), stroke (USD 3.0 billion), and breast cancer (USD 0.5 billion) (Singer 2015).
The term 'hip fracture' refers to a fracture of the proximal femur down to about 5 cm below the lower border of the lesser trochanter. Costs of care for hip fractures are high and, when both acute care and the care needed for subsequent dependency were included, exceeded GBP 2 billion in 2012 for the UK as a whole. That same year, the overall rate of return home by 30 days was 44.6% in the UK (National Hip Fracture Database 2019; www.nhfd.co.uk). In the USA, from 2003 to 2005, 5.3% of patients with hip fracture returned home in 30 days, and 52.8% were discharged to a skilled nursing facility (Brauer 2009). Hip fractures are associated with reduced life expectancy when they occur in individuals over 50 years of age. Pooled data from cohort studies revealed that the relative hazard (RH) for all‐cause mortality during the first three months after hip fracture was 5.75 (95% confidence interval (CI) 4.94 to 6.67) in women and 7.95 (95% CI 6.13 to 10.30) in men (Haentjens 2010). However, improved care has resulted in encouraging figures. Indeed, data collected in UK in 2018 show a 6.1% death rate, representing a decrease of one in eight when compared with the mortality figure of 6.9% reported for 2017, implying that 564 fewer people died within a month of breaking their hip in 2018 (National Hip Fracture Database 2019).
Description of the intervention
Regional blockade refers to injection of local anaesthetics around neural structures to transiently prevent pain transmission to the brain, and may also produce motor blockade of the muscle in a specific area, depending on the type and concentration of local anaesthetic used. Local anaesthetics can be used at the spine level (neuraxial blocks = epidural or spinal) or around the nerves outside the spine (plexus blocks or peripheral nerve blocks (PNBs)). Local anaesthetic may also be infiltrated directly into wound tissues. All of these blocks can be given as a single injection or by continuous infusion through a catheter to prolong their beneficial effects. PNBs may be used as a replacement for general anaesthesia during surgery, as adjunctive treatment for preoperative and postoperative pain, or as a means of decreasing the use of intraoperative systemic drugs during general anaesthesia. Use of regional blockade as a replacement for general anaesthesia in individuals with hip fracture is covered in another review (Guay 2016). For the present review, the intervention is limited to PNBs used for analgesia (i.e. before surgery), in addition to other anaesthetic methods for surgery or for postoperative analgesia. Although neuraxial blocks may have been used in some trials included here (usually as replacement for general anaesthesia for the surgery), they will not be evaluated in the present review but, once again, are covered separately in another review (Guay 2016).
How the intervention might work
Most hip fractures occur in an elderly population; more than 30% of individuals with hip fracture are 85 years of age or older (Brauer 2009). Opioid‐related respiratory depression may result in severe brain damage or death (Lee 2015). By reducing the quantity of opioids used before, during, and after surgery (Guay 2006; Guay 2017), regional blockade may improve the mobility of persons with hip fracture (Saunders 2010), potentially facilitating their participation in rehabilitation and hence reducing complications related to prolonged immobilization such as pneumonia (Guay 2017). Hip fractures in the elderly have also been associated with a high rate of postoperative delirium. In a recent review on 8439 geriatric hip fracture patients, Arshi and colleagues reported a 30.4% rate of postoperative delirium (Arshi 2018). Patients with postoperative delirium had significantly higher risk‐adjusted 30‐day mortality (12.0% vs 4.8%; odds ratio (OR) 2.22, 95% CI 1.74 to 2.84) (Arshi 2018). Some study authors have suggested that the rate of perioperative delirium might be lower when PNBs are added to a multi‐modal regimen of perioperative analgesia (Mouzopoulos 2009).
Why it is important to do this review
Despite their advantages, PNBs still are not widely used for people with hip fracture (Haslam 2013). Many official clinical societies recommend preoperative regional anaesthesia (e.g. American Academy of Orthopaedic Surgeons 2014: "strong recommendation"; NICE 2017: "consider adding nerve blocks if paracetamol and opioids do not provide sufficient preoperative pain relief, or to limit opioid dosage") and postoperative multi‐modal analgesia including regional anaesthesia (e.g. American Academy of Orthopaedic Surgeons 2014: "strong recommendation") for patients with hip fracture. It is not the mandate of Cochrane reviewers to make any recommendations but rather to summarize the evidence, hence providing official societies, policy makers, clinicians, and patients with high‐quality systematic reviews to help them make decisions as to what intervention should or should not be used for a specific clinical condition in their specific environment.
In addition, exclusive use of opioids for perioperative pain has become a controversial clinical practice. Between 1999 and 2016, more than 630,000 people in the United States died from a drug overdose, and a record number of drug overdose deaths occurred in 2016: 63,632 − a rate of 19.8 per 100,000 persons (Centers for Disease Control and Prevention 2018). Within the first six months of 2018 alone, 2066 opioid‐related deaths were reported in Canada (11.2 deaths per 100 000 people) (Ball 2019). Up to 75% of all heroin users were first introduced to narcotics through an initial physician‐ or surgeon‐related opioid prescription (Ball 2019). Reduction in perioperative opioid consumption with the use of regional anaesthesia has already been reported (Guay 2016; Guay 2017).
Some adverse events may happen with the use of PNBs. Severe and permanent nerve injuries have occurred, at an estimated incidence of approximately 1:2500 to 1:5000 blocks (Neal 2015). Although systemic local anaesthetic toxicity has probably decreased in both incidence and severity with the use of ultrasound, seizures are still reported, with an incidence of 1.3 (95% CI 0.3 to 3.8) per 10,000 PNBs (Sites 2014). Finally, although infections are rarely seen with single PNBs, they may occur with catheter insertion (Bomberg 2017).
The topic of the present review is very important to update, considering: (1) the high prevalence of hip fractures, (2) the large number of official societies providing recommendations on this condition, (3) the possibility that perioperative PNBs may improve patient outcomes, and (4) the major role that PNBs may play in reducing preoperative and postoperative opioid use for analgesia.
Therefore, we have decided to re‐evaluate the beneficial effects of PNBs for hip fracture.
This is an update of a previously published review (Guay 2017; Parker 2002).
Objectives
To compare PNBs used as preoperative analgesia, as postoperative analgesia, or as a supplement to general anaesthesia versus no nerve block (or sham block) for adults with hip fracture. Outcomes were pain on movement at 30 minutes after block placement, acute confusional state, myocardial infarction, chest infection, death, time to first mobilization, and costs of an analgesic regimen for single‐injection blocks.
We undertook the update to look for new studies and to update the methods to reflect Cochrane standards.
Methods
Criteria for considering studies for this review
Types of studies
We included all parallel randomized controlled trials (RCTs) and cluster trials comparing PNBs inserted preoperatively, intraoperatively, or postoperatively (intervention) versus no nerve block (or sham block) (comparator).
For the purpose of this review, a sham nerve block and no nerve block were considered as equivalent. We excluded quasi‐RCTs (e.g. alternation) and cross‐over trials. These two categories of trials were also excluded from previously published versions of our review. Cross‐over trials were considered unsuitable for our review. Indeed, it would not be possible to evaluate the effects of adding PNBs on the risk of perioperative acute confusional state, pneumonia, myocardial infarction, or mortality if all participants had received a PNB at some point during their perioperative period (unless we had considered only the first part of the cross‐over trial, when results would be available as such).
Types of participants
We included adults aged 16 years of age and older with a proximal femoral fracture (hip fracture).
Types of interventions
PNBs of any type versus no nerve block (or sham block).
Types of outcome measures
Primary outcomes
Pain on movement 30 minutes after block placement (study author's scale; Thong 2018)
Acute confusional state (study author's definition), 0 to 30 days
Myocardial infarction (study author's definition), 0 to 30 days
Secondary outcomes
Chest infection (study author's definition), 0 to 30 days
Mortality (all death from any cause), 0 to 6 months
Time to first mobilization after surgery
Costs of analgesic regimens (at any time points chosen by study authors)
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 11), in the Cochrane Library; MEDLINE ALL (Ovid SP, 1966 to 16 November 2019); Embase (Ovid SP, 1974 to 16 November 2019); and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO, 1982 to 16 November 2019). We searched for studies as described in the Cochrane Handbook of Systematic Reviews of Interventions, Chapter 4 (Lefebvre 2019). We combined the MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomized trials in MEDLINE (Lefebvre 2019). For MEDLINE (Ovid SP), we designed a subject‐specific search strategy, and we used this as the basis for search strategies used in Embase, CENTRAL, and CINAHL. When appropriate, we supplemented the search strategy with search terms used to identify RCTs. All search strategies can be found in Appendix 1. We searched the bibliographic references and citations of relevant studies and systematic reviews for further potentially relevant studies. We applied no language or publication status restrictions.
Searching other resources
We also searched http://www.clinicaltrials.gov (18 January 2020) and http://apps.who.int/trialsearch/ (January 2020) to identify trials in progress. We screened the reference lists of all studies retained (during data extraction) and from other recently published systematic reviews related to the topic (December 2019). We screened conference proceedings of anaesthesiology societies for 2017, 2018, and 2019, as published in two major anaesthesiology journals: European Journal of Anaesthesiology (January 2020) and Regional Anesthesia and Pain Medicine (January 2020). In addition, we looked for abstracts on the website of the American Society of Anesthesiologists for the same years (2017 to 2019; American Society of Anesthesiologists 2020) (18 January 2020).
Data collection and analysis
Selection of studies
We independently assessed potentially eligible trials for inclusion. We resolved disagreements by discussion.
Data extraction and management
We independently extracted data for the outcomes listed above for all new trials and resolved differences through discussion. When we were unable to extract relevant data or information, we contacted the study authors for whom we could find an email address (N = 38; Albrecht 2014; Altermatt 2013; Antonopoulou 2006; Bang 2016; Brownbridge 2018; Cuvillon 2007; De La Tabla 2010; Diakomi 2014; Domac 2015; Fletcher 2003; Foss 2005a; Gille 2006; Godoy Monzon 2010; Graham 2008; Gürtan Bölükbasi 2013; Jadon 2014; Jang 2018; Kullenberg 2004; Landsting 2008; Liebmann 2012; Luger 2012; Ma 2018a; Madabushi 2016; Morrison 2008; Mosaffa 2005; Mouzopoulos 2009; Murgue 2006; Nie 2015; Ranjit 2016; Segado Jimenez 2009; Szucs 2010; Thompson 2019; Tuncer 2003; Unneby 2017; Uysal 2018; Wang 2015; Yamamoto 2016; Yun 2009).
Assessment of risk of bias in included studies
We evaluated the quality of all included studies using the new Cochrane Risk of Bias‐2 tool for each outcome (Table 1) (last accessed July 2020; Sterne 2019).
Pain on movement at 30 minutes after block placement.
Acute confusional state (0 to 30 days).
Myocardial infarction (0 to 30 days).
Pneumonia (0 to 30 days).
Death (0 to 6 months).
Time to first mobilization (in‐hospital).
Cost of analgesic regimens for single‐injection PNBs (in‐hospital).
Risks of bias for all outcomes were independently assessed by two review authors with respect to the effect of assignment to the intervention at baseline. We first read the detailed guidance document (available at drive.google.com/file/d/19R9savfPdCHC8XLz2iiMvL_71lPJERWK/view). We completed a Word document template (available at drive.google.com/file/d/18Zks7k4kxhbUUlbZ51Ya5xYa3p3ECQV0/view) for each included trial and for each outcome to allow agreement between the two review authors. We settled any disagreement by discussion. Then, one review author (JG) entered data into the Excel tool (available at drive.google.com/file/d/1KSFASeBJP8FjBMpEbNlDiYxp4CKuOZgM/view). The Word document was converted into a PDF document and stored online in an open repository (Figshare) (Guay 2020).
Briefly, we considered bias arising from the following domains: bias in the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in measurement of outcomes, and bias in selection of the reported result. For each signalling question, we answered yes, probably yes, probably no, no, or no information, based on information retrieved from the reports or from the study authors. We inserted brief direct quotations into the text box to support those answers.
Subsequently, each outcome result was given an overall judgement for risk of bias.
Low risk of bias overall, if all domains for this result were assessed as ‘low’ risk.
Some concerns overall, if at least one domain for this result was assessed as ‘some concerns’ but none were assessed as ‘high’ risk.
High risk of bias overall, if at least one domain was assessed as ‘high’ risk, or if we had ‘some concerns’ about several domains that, when considered together, could indicate ‘high’ risk of bias.
Additional details can be found in Appendix 2.
We planned to evaluate risks of bias of cluster trials using the cluster trial extension for Risk of Bias‐2 (Eldridge 2016).
When possible, we mentioned the direction of the bias.
Measures of treatment effect
We presented results as risk ratios (RRs) or risk differences (RDs), along with the 95% confidence intervals (95% CIs) for dichotomous data, and as mean differences (MDs) and 95% CIs for continuous data. Although hazard ratio would have been optimal for time to event data (time to first mobilization; Deeks 2019), data were unfortunately not available in this format. If some of the continuous data were reported using different scales, or when results were not provided as mean and standard deviation (SD) (therefore extracted as P values), we produced the results as standardized mean differences (SMDs) and 95% CIs. For SMDs, we considered 0.2 to be a small effect, 0.5 to be a moderate effect, and 0.8 to be a large effect (Pace 2011). A clinical equivalence was calculated for results produced as SMD. When results for dichotomous data showed an effect, we calculated the number needed to treat for an additional beneficial outcome (NNTB) or the number needed to treat for an additional harmful outcome (NNTH), using the odds ratio. We provided results for dichotomous data as RRs as often as was feasible, as the odds ratio (OR) is not easily understood by clinicians (Deeks 2002; McColl 1998). We used the OR for calculation of NNTB and NNTH (http://www.nntonline.net/visualrx/), as this value is less likely to be affected by the side (benefit or harm) on which data are entered (Cates 2002; Deeks 2002). When we noted no effect, we calculated the optimal information size to make sure that enough participants were included in the retained studies to justify a conclusion on the absence of effect (Pogue 1998; http://www.stat.ubc.ca/~rollin/stats/ssize/b2.html). We arbitrarily defined a difference of 25% (increase or decrease) as the minimal clinically relevant difference (Schünemann 2019).
Unit of analysis issues
If a trial included more than two groups, we fused two groups (by using the appropriate formula for adding standard deviations, when required) when we thought that they were equivalent according to the criteria chosen a priori for exploration of heterogeneity; we separated them and split the control group in half if we thought that they were different (Higgins 2019). For cluster trials, we planned to simply extract odds ratios and their confidence intervals when an appropriate analysis was used by study authors. If not, we planned to correct the sample sizes or inflate the standard errors, as recommended by Cochrane (Higgins 2019).
Dealing with missing data
We contacted study authors to ask for apparently missing data. We did not consider medians as equivalent to means. Instead, we used the P value and the number of participants included in each group to calculate the effect size. We did not use imputed results. We entered data as intention‐to‐treat (ITT) as much as was feasible in accordance with our choice for risk of bias assessment (i.e. "assignment to the intervention at baseline"). If this was not possible, we entered the data on a per‐protocol basis and took this into account in our risk of bias assessment.
Assessment of heterogeneity
We considered clinical heterogeneity before pooling results, and we examined statistical heterogeneity. We visually examined all forest plots. We quantified statistical heterogeneity by using the I² statistic with data entered in the way (benefit or harm) that yielded the lowest amount. We qualified the amount as follows: might not be important (0% to 40%), may represent moderate heterogeneity (30% to 60%), may represent substantial heterogeneity (50% to 90%), or considerable heterogeneity (75% to 100%), depending on the value obtained for the I2 statistic (Deeks 2019).
Assessment of reporting biases
We examined publication bias by using a funnel plot, then performed Duval and Tweedie’s trim and fill technique for each outcome. When publication bias is present, this technique yields an adjusted point of estimate that takes into account the number of theoretically missing studies.
Data synthesis
We analysed the data using RevMan 5.3 and Comprehensive Meta‐Analysis Version 2.2.044 (www.Meta-Analysis.com; visual inspection of forest plots with data placed in a specific order, Egger's regression intercept, Duval and Tweedie's trim and fill analysis, and meta‐regression) with fixed‐effect models. We avoided random‐effects models due to a large number of small studies. Random‐effects models give greater weight to small studies. We presented study characteristics in relevant tables (Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies). We presented risk of bias assessments in graphs and results for each comparison as forests plots or narratively (in the case of comparisons with fewer than two available trials or for results with a high level of heterogeneity unexplained by heterogeneity exploration).
Subgroup analysis and investigation of heterogeneity
For exploration of heterogeneity, we focused specifically on comparisons with more than a small amount of heterogeneity (I2 > 40%) (Deeks 2019). We used Egger’s regression intercept to assess the possibility of a small‐study effect (Rucker 2011; Sterne 2001). We visually inspected forest plots with trials placed in order according to a specific moderator. If forest plots suggested a specific moderator to be relevant, we used subgroup analysis or meta‐regression with Comprehensive Meta‐Analysis Version 2.2.044 (www.Meta-Analysis.com).
We explored heterogeneity by conducting subgroup analysis based on the following categories.
Type of nerve block (e.g. psoas compartment, fascia iliaca, femoral nerve (we considered three‐in‐one and triple nerve blocks as femoral nerve blocks), lateral femoral cutaneous, obturator).
Single‐injection PNB versus continuous infusion.
Technique of localization (landmark, nerve stimulator, or ultrasound).
American Society of Anesthesiologists (ASA) physical status of participants.
We used meta‐regression for ages of participants included, year the study was published, and local anaesthetic concentration in lidocaine equivalent (used for single‐injection PNBs only and calculated as follows: lidocaine = 1, bupivacaine = 4, chloroprocaine = 1.5, dibucaine = 4, etidocaine = 4, levobupivacaine = 3.9, mepivacaine = 0.8, prilocaine = 0.9, procaine = 0.5, ropivacaine = 3, and tetracaine = 4) (Berde 2009)).
Sensitivity analysis
We performed a sensitivity analysis based on risk of bias of the study, or if a study was a clear outlier, as long as a reason differentiating this study from the other studies (difference in study design, population, intervention, comparator, or outcome measurement) could be identified. For risk of bias, for each outcome, we reported the results obtained while excluding trials at high risk of bias based on overall risk of bias judgements.
Summary of findings and assessment of the certainty of the evidence
We used the principles of the GRADE approach to assess the certainty of evidence associated with all outcomes (pain on movement 30 minutes after block placement, acute confusional state, myocardial infarction, pneumonia, death, time to first mobilization, and cost of analgesic regimen for single PNBs) (Schünemann 2019), and we constructed Table 1 using GRADEPro.
For uncertainty resulting from risk of bias, we judged the certainty of evidence as presenting low risk of bias when exclusion of trials at high risk of bias did not change the conclusion. We downgraded quality by one or two levels when excluding trials at high risk of bias changed the conclusion, or when evidence was based mainly on trials with multiple domains with some concerns.
For uncertainty resulting from inconsistency, we downgraded the certainty of evidence by one level when the I2 statistic was 50% or higher without satisfactory explanation, and by two levels when the I2 statistic was 75% or higher without an explanation. We also considered clinical heterogeneity as a potential contributor to inconsistency.
For uncertainty resulting from indirectness and applicability, we planned to downgrade the certainty of evidence if outcomes were not measured on the population of interest, involved differences in intervention (different setting or related interventions), involved differences in outcomes measures (surrogate markers) or were based on indirect comparisons (Schünemann 2013).
For uncertainty resulting from imprecision (Zhang 2019), we downgraded the certainty of evidence by one or two levels when the CI around the effect size was large or overlapped with absence of effect and failed to exclude an important benefit or harm, or when the number of participants was smaller than the optimal information size. The outcome itself was also taken into account.
For uncertainty resulting from publication bias, we downgraded the certainty of evidence by one level when correcting for the possibility of publication bias as assessed by Duval and Tweedie’s fill and trim analysis changed the conclusion.
Results
Description of studies
Characteristics of included studies, excluded studies, and ongoing trials can be found in Characteristics of included studies, Characteristics of excluded studies, and Characteristics of ongoing studies tables, respectively.
Results of the search
Details of the search for this update can be found in Figure 1. We found 477 titles from the Cochrane Central Register of Controlled Trials (CENTRAL), 211 from the Cumulative Index to Nursing and Allied Health Literature (CINHAL), 410 from Embase, and 418 from MEDLINE. Upon adding articles from the latest previously published version, titles from references lists of articles retained and from relevant reviews, conference proceedings, and ongoing trials, we retrieved 158 articles. We excluded 46 trials due to ineligible study design, 20 because they studied a different population, 40 because they studied a different intervention, and five because they were withdrawn or were terminated by study authors. Twenty‐nine trials were ongoing.
1.

Flow diagram for the 2020 update.
CENTRAL: The Cochrane Central Register of Controlled Trials; CINHAL: Cumulative Index to Nursing and Allied Health Literature.
Included studies
We included 49 trials with 3061 participants; 1553 participants were randomized to PNBs and 1508 to no nerve block (or sham block). Forty‐three trials with 2750 participants could be included in the analysis: 1368 participants randomized to PNBs and 1382 randomized to no nerve block (or sham block).
Trials were published between 1980 and 2020 and were funded by a charitable organization (N = 5; Cuvillon 2007; Foss 2005a; Liebmann 2012; Ma 2018a; Unneby 2017), by a governmental organization (N = 5; Altermatt 2013; Jang 2018; Landsting 2008; Morrison 2008; Nie 2015), or by departmental/institutional resources (N = 16; Albrecht 2014; Bang 2016; Brownbridge 2018; Domac 2015; Gille 2006; Henderson 2008; Godoy Monzon 2010; Jadon 2014; Luger 2012; Madabushi 2016; Szucs 2010; Thompson 2019; Uysal 2018; Wang 2015; Yamamoto 2016; Yun 2009). Remaining trials did not specify the source of funding.
Some trials were registered at an official trial registry outside the institution (N = 13; Albrecht 2014; Altermatt 2013; Bang 2016; Brownbridge 2018; Diakomi 2014; Foss 2005a; Hogg 2009; Jang 2018; Landsting 2008; Liebmann 2012; Morrison 2008; Wang 2015; Yamamoto 2016).
Trials were performed in Argentina (N = 1; Godoy Monzon 2010), Austria (N = 1; Luger 2012), Canada (N = 1; Brownbridge 2018), Chile (N = 1; Altermatt 2013), China (N = 5; Graham 2008; Nie 2015; Ma 2018a; Wang 2015; Yang 2016), Denmark (N = 2; Foss 2005a; Spansberg 1996), France (N = 2; Cuvillon 2007; Murgue 2006), Greece (N = 3; Antonopoulou 2006; Diakomi 2014; Mouzopoulos 2009), Germany (N = 1; Gille 2006), India (N = 2; Jadon 2014; Madabushi 2016), Iran (N = 1; Mosaffa 2005), Ireland (N = 1; Szucs 2010), Israel (N = 1; Chudinov 1999), Japan (N = 1; Yamamoto 2016), Korea (N = 3; Bang 2016; Jang 2018; Yun 2009), Nepal (N = 1; Ranjit 2016), South Africa (N = 1; White 1980), Spain (N = 2; De La Tabla 2010; Segado Jimenez 2009), Sweden (N = 3; Kullenberg 2004; Landsting 2008; Unneby 2017), Switzerland (N =1; Albrecht 2014), Turkey (N = 5; Deniz 2014; Domac 2015; Gürtan Bölükbasi 2013; Tuncer 2003; Uysal 2018), United Kingdom (N = 6; Coad 1991; Fletcher 2003; Haddad 1995; Hogg 2009; Hood 1991; Jones 1985), and United States of America (N = 4; Henderson 2008; Liebmann 2012; Morrison 2008; Thompson 2019).
The average age of participants ranged from 59 to 89 years. Participants included had an American Society of Anesthesiologists (ASA) physical status between I and IV. The proportion of included females varied between 33% and 95%. The proportion of arthroplasty varied between 0 and 100%.
Details of the PNBs, anaesthetic techniques, comparators, and rescue analgesics used are included in Table 2.
1. Anaesthetic techniques.
| Study | Purpose of blockade | Time of block placement | Surgical anaesthesia | Block technique | Comparison | Supplemental analgesia for both groups |
| Albrecht 2014 | Preoperative analgesia | In the emergency department | No information | Fascia iliaca compartment block Landmarks Single injection Bupivacaine 0.5% with epinephrine 1:200,000 30 mL Operator: trained emergency physicians |
Sham block with normal saline | Acetaminophen Morphine |
| Altermatt 2013 | Preoperative, intraoperative, and postoperative analgesia | Preoperatively, probably in the emergency department | Spinal anaesthesia | Psoas compartment block Nerve stimulator (quadriceps contraction at 0.5 mA, 1 Hz, 0.1 millisecond) Continuous infusion Bupivacaine 0.1% 20 mL followed by patient‐controlled analgesia: basal rate 8 mL/hour, bolus 5 mL, lock‐out time 30 minutes for 72 hours Operator: no information |
No nerve block IV PCA with Morphine |
Acetaminophen Ketorolac |
| Antonopoulou 2006 | Postoperative analgesia | After recovery of anaesthesia | Spinal anaesthesia | Femoral nerve block Nerve stimulator Continuous infusion Levobupivacaine 0.25% 18 mL followed by levobupivacaine 0.125% at 3 to 4 mL/hour for 24 hours after surgery Operator: no information |
No nerve block | Acetaminophen Pethidine |
| Bang 2016 | Postoperative analgesia | After surgery and after confirmation of patient’s mental status to be alert, able to communicate, and obey commands | Spinal anaesthesia | Fascia iliaca compartment block Ultrasound‐guided Single injection Ropivacaine 0.2% 40 mL Operator: no information |
No nerve block | Ketorolac Celecoxib IV PCA with Fentanyl Tramadol |
| Brownbridge 2018 | Preoperative, intraoperative, and postoperative analgesia | Preoperatively, after patients had been assigned to a bed on the ward | Spinal (53% for intervention group and 40% for comparator group) or general anaesthesia | Fascia iliaca compartment block Landmarks Continuous infusion Ropivacaine 0.125% 40 mL followed by ropivacaine 0.2% 10 mL/hour until surgery. In the operating room, catheters were re‐bolused with 40 mL 0.125% ropivacaine, then removed Operator: anaesthesiology department |
No nerve block | Acetaminophen NSAIDs Opioids |
| Chudinov 1999 | Preoperative, intraoperative, and postoperative analgesia Surgery for some participants |
Preoperatively, within 6 hours after admission to the orthopaedic ward | Intervention: psoas block alone (3/20) with sciatic block (5/20), spinal (11/20) or general anaesthesia (1/20) Comparator: neuraxial block (19/20) or general anaesthesia (1/20) |
Psoas compartment block Landmarks and loss of resistance to air, lateral decubitus with operated side up (1 epidural spread) Continuous infusion: started preoperatively (16 to 48 hours) and kept for 72 hours after surgery Test dose with 3 mL of 0.5% bupivacaine with epinephrine 5 mcg/mL followed by bupivacaine 0.25% with epinephrine 5 mcg/mL 0.8 mL/kg over 8 minutes plus 1 to 2 mg/kg routinely every 8 hours and before surgery (unless already received < 3 hours) Operator: anaesthesiologists |
No nerve block IM Meperidine Diclofenac |
IM Meperidine |
| Coad 1991 | Postoperative analgesia | At completion of surgery before awakening from general anaesthesia | General anaesthesia | 1) Lateral femoral cutaneous nerve block
2) 3‐in‐1 femoral nerve block Landmarks Single injection 1) Bupivacaine 0.5% with epinephrine 5 mcg/mL 15 mL 2) Bupivacaine 0.5% with epinephrine 5 mcg/mL 15 mL Operator: anesthesiology department |
No nerve block | Pethidine |
| Cuvillon 2007 | Postoperative analgesia | After ending of effects of spinal blockade | Spinal anaesthesia | Femoral nerve block Nerve stimulator (quadriceps for patella ascension with 0.3 to 0.5 mA at 0.1 ms and catheter 10 to 15 cm passed over the needle tip) Continuous infusion Lidocaine 1.5% plus epinephrine 30 mL of lidocaine 1.5% followed by ropivacaine 0.2% at 10 mL/hour for 48 hours Operator: anesthesiology department |
No nerve block IV Paracetamol for half of participants in the comparator group |
1 dose of paracetamol in the emergency department Morphine |
| De La Tabla 2010 | Preoperative, intraoperative, and postoperative analgesia | Upon hospital arrival | No information | Femoral nerve block Dual technique: ultrasound‐guided plus nerve stimulator Continuous infusion Ropivacaine 0.2% 15 mL followed by ropivacaine 0.2% at 5 mL/hour basal rate plus boluses of 10 mL every 30 minutes Operator: no information |
No nerve block IV Metamizole |
IV Tramadol |
| Deniz 2014 | Intraoperative and postoperative analgesia | In the operating room, before induction of general anaesthesia | General anaesthesia | 1) Fascia iliaca compartment block
2) 3‐in‐1 femoral nerve block 1) Ultrasound‐guided 2) Dual technique: ultrasound‐guided plus nerve stimulator (quadriceps contraction at 0.5 mA) Single injection 1) Bupivacaine 0.25% 30 mL 2) Bupivacaine 0.25% 30 mL Operator: anesthesiology department |
No nerve block | Tenoxicam IV PCA with Tramadol |
| Diakomi 2014 | Spinal positioning, intraoperative and postoperative analgesia | Before positioning for spinal anaesthesia | Spinal anaesthesia | Fascia iliaca compartment block Landmarks Single injection Ropivacaine 0.5% 40 mL Operator: anesthesiology department |
No nerve block IV Fentanyl for positioning for spinal block |
IV PCA with Morphine |
| Domac 2015 | Spinal positioning, intraoperative and postoperative analgesia | In the regional anaesthetic technique room, before spinal anaesthesia | Spinal anaesthesia | Fascia iliaca compartment block Landmarks Single injection Bupivacaine 0.5% 15 mL and lidocaine 2% 15 mL Operator: anesthesiology department |
No nerve block | IV PCA with Morphine Tramadol |
| Fletcher 2003 | Preoperative analgesia | In the emergency department, after radiographic confirmation | No information | 3‐in‐1 femoral nerve block Paraesthesia Single injection Bupivacaine 0.5% 20 mL Operator: trained emergency physicians |
No nerve block | IV Morphine |
| Foss 2005a | Preoperative analgesia | Upon arrival in the emergency department | No information | Fascia iliaca compartment block Landmarks Single injection Mepivacaine 1% with epinephrine 5 mcg/mL 40 mL Operator: junior anaesthesiologists with less than 2 years of training |
Sham block with 0.9% saline plus IM Morphine |
IV Morphine Epidural analgesia after 3‐hour study period |
| Gille 2006 | Preoperative, intraoperative. and postoperative analgesia | Upon arrival in the emergency department | Intervention: spinal anaesthesia for 37/50 and general anaesthesia for 13/50 Comparator: spinal anaesthesia for 38/50 and general anaesthesia for 12/50 |
Femoral nerve block Nerve stimulator (0.5 mA and 0.1 millisecond) Continuous infusion (non‐stimulating catheters advanced about 10 cm past the needle tip) Prilocaine 1% 40 mL followed 2 hours later by ropivacaine 0.2% 30 mL, repeated every 6 hours (up to 40 mL; N = 5) and at intervals (up to every 4 hours; N = 8) or both (N = 6), adjusted on pain scores Operator: anaesthesiology department |
No nerve block IV Metamizole Oral Tilidine and Naloxone |
Ibuprofen Tilidine |
| Godoy Monzon 2010 | Preoperative analgesia | In the emergency department, after confirmation of diagnosis | No information | Fascia iliaca compartment block Landmarks Single injection Bupivacaine 0.25% 0.3 mL/kg Operator: physicians (first study author is an orthopaedic surgeon) |
Sham block with saline and IV NSAIDs | NSAIDs Opioids |
| Graham 2008 | Preoperative analgesia | In the emergency department | No information | Femoral (3‐in‐1) nerve block Single injection Nerve stimulator Bupivacaine 0.5% 30 mL (not exceeding 3 mg/kg) Operator: specialist emergency physician or higher trainee resident, post intermediate examination level |
No nerve block IV Morphine |
IV Morphine Dihydrocodeine Diclofenac Paracetamol |
| Gürtan Bölükbasi 2013 | Spinal positioning, intraoperative and postoperative analgesia | Before spinal anaesthesia | No information | Fascia iliaca compartment block Single injection Ultrasound‐guided Levobupivacaine 0.375% 30 mL Operator: anesthesiology department |
No nerve block IV Remifentanil |
Additional analgesia |
| Haddad 1995 | Preoperative analgesia | In the emergency department | No information | Femoral nerve block Single injection Bupivacaine 0.25%.0.3 mL/kg Paraesthesia technique with a short bevel needle Operator: 1 orthopaedic registrar |
No nerve block | Co‐dydramol Voltarol Pethidine |
| Henderson 2008 | Preoperative analgesia | In the emergency department | No information | Femoral nerve block Nerve stimulator Single injection Bupivacaine 0.5% Operator: trained emergency physicians |
No nerve block | Opioids |
| Hogg 2009 | Spinal positioning, intraoperative and postoperative analgesia | Before spinal anaesthesia | Spinal anaesthesia | Fascia iliaca compartment block No information on localizing technique Single injection Lidocaine 1% 2 mg/kg Operator: anaesthesiology department |
No nerve block IV Ketamine 0.2 mg/kg IV Midazolam 0.025 mg/kg |
Ketamine |
| Hood 1991 | Intraoperative and postoperative analgesia | Before induction of general anaesthesia | General anaesthesia | 1) Femoral "3‐in‐1" nerve block
2) Infiltration above the iliac crest 1) Nerve stimulator (quadriceps contraction with < 1 mA) 2) Landmarks Single injection 1) Prilocaine 0.75% 35 mL 2) Prilocaine 0.75% 8 mL Operator: anaesthesiology department |
No nerve block | Papaveratum |
| Jadon 2014 | Spinal positioning, intraoperative and postoperative analgesia | Before spinal anaesthesia | Spinal anaesthesia | Femoral nerve block Nerve stimulator (quadriceps contraction with 0.3 to 0.5 mA) Single injection Lidocaine 1.5% (2% diluted with distilled water) with epinephrine 5 mcg/mL 20 mL Operator: anaesthesiology department |
No nerve block IV Fentanyl |
IV Fentanyl |
| Jang 2018 | Preoperative analgesia | In the emergency department, 48 hours before surgery | No information | Femoral nerve block Single injection Ultrasound‐guided (in‐plane) Bupivacaine 0.5% 0.3 mL/kg (maximum 20 mL) Operator: 1 physician experienced in administering ultrasound‐guided femoral nerve blocks |
Sham block with saline | IV Tramadol |
| Jones 1985 | Postoperative analgesia | At completion of surgery, while still under general anaesthesia | General anaesthesia | Lateral femoral cutaneous nerve block Single injection Landmarks Bupivacaine 0.5% with epinephrine 5 mcg/mL 15 mL Operator: anaesthesiology department |
No nerve block | IM Pethidine |
| Kullenberg 2004 | Preoperative analgesia | As soon as the diagnosis of hip fracture was radiologically confirmed | No information | Femoral nerve block Nerve stimulator Single injection Ropivacaine 0.75% 30 mL. Operator: 1 orthopaedic surgeon |
No nerve block | Paracetamol Tramadol Ketobemidon |
| Landsting 2008 | Preoperative analgesia | Within 1 hour of hospital admission | No information | Fascia iliaca compartment block Landmarks Single injection Ropivacaine 0.2% 30 mL Operator: orthopaedic surgeons |
Sham block with saline | IV Morphine Paracetamol |
| Liebmann 2012 | Preoperative analgesia | In the emergency department | No information | 3‐in‐1 femoral nerve block Ultrasound‐guided (in‐plane) Single injection Bupivacaine 0.5% 25 mL Operator: emergency physicians experienced with the technique |
Sham block with saline | Morphine |
| Luger 2012 | Preoperative, intraoperative, and postoperative analgesia | In the emergency department | Spinal anaesthesia | Femoral "3‐in‐1" nerve block Ultrasound‐guided Continuous infusion (catheters inserted ≥ 12 to 15 cm past the needle tip) Bupivacaine 0.25% 30 mL (additional 10 mL if required for adequate sensory blockade) followed by bupivacaine 0.125% at 6 mL/hour Operator: anesthesiology department |
No nerve block | Piritramide Paracetamol |
| Ma 2018a | Preoperative analgesia | After hospital admission | No information | Fascia iliaca compartment block Ultrasound‐guided (in‐plane) Continuous infusion (catheters 5 to 10 cm beyond the tip of the needle) Ropivacaine 0.4% 30 mL followed by ropivacaine 0.2% at 5 mL/hour plus 5 mL for breakthrough pain until surgery (mean 3.5 days). Catheters removed on the morning of surgery Operator: 1 anaesthesiologist experienced in ultrasound‐guided nerve block |
No nerve block | Tramadol Acetaminophen Pethidine |
| Madabushi 2016 | Spinal positioning, intraoperative and postoperative analgesia | Before spinal anaesthesia | Spinal anaesthesia | Fascia iliaca compartment block Landmarks Single injection Ropivacaine 0.375% 30 mL Operator: anaesthesiologists |
No nerve block IV Fentanyl |
Paracetamol Tramadol Diclofenac |
| Morrison 2008 | Preoperative analgesia, intraoperative and postoperative analgesia | In the emergency department for femoral nerve block and within 24 hours of femoral block for continuous fascia iliaca block | Regional anaesthesia for 62.1% | 1) Femoral nerve block
2) Fascia iliaca compartment block (within 24 hours of #1) Ultrasound‐guided (out‐of‐plane for insertion, but advancement visualized) 1) Single injection Bupivacaine 0.5% 20 mL 2) Continuous infusion Ropivacaine 0.2% 15 mL followed by 5 mL/hour for 72 hours after surgery Operators: 1) Trained emergency physicians 2) Anaesthesiologists (mobile peripheral nerve block service) |
No nerve block | Opioids Acetaminophen |
| Mosaffa 2005 | Spinal positioning, intraoperative and postoperative analgesia | Before spinal anaesthesia | Spinal anaesthesia | Fascia iliaca block with 20 mL of 1.5% lidocaine No information for localizing technique Single injection Lidocaine 1.5% 20 mL Operator: anaesthesiology department |
No nerve block IV Fentanyl |
No information |
| Mouzopoulos 2009 | Preoperative and postoperative analgesia | Started upon admission to the orthopaedic ward | Epidural anaesthesia | Fascia iliaca compartment blocks daily (from admission until surgery, restarted at 24 hours after surgery until discharge, stopped earlier (before or after surgery) if delirium occurred) Landmarks Bupivacaine 0.3 mL/kg (0.25%?) Operator: orthopaedic surgeons |
Sham blocks with water | IV Paracetamol Pethidine |
| Murgue 2006 | Preoperative analgesia | In the emergency department | No information | Femoral nerve block Nerve stimulator (quadriceps contraction with patellar ascension) Single injection Mepivacaine 20 mL Operator: unclear, published by emergency physicians |
No nerve block IV Morphine or IV Paracetamol and Ketoprofen |
Nitrous oxide |
| Nie 2015 | Postoperative analgesia | After closure of the surgical wound | General anaesthesia | Fascia iliaca block Landmarks Continuous infusion (catheter inserted ≥ 10 cm cranially) Ropivacaine 0.5% according to body weight (20 mL if weight < 50 kg, 25 mL if weight 50 kg to 70 kg, 30 mL if weight > 70 kg) followed by ropivacaine 0.25% at 0.1 mL/kg/hour for 48 hours Operator: no information, probably anaesthesiology department |
No nerve block IV PCA with Fentanyl |
Acetaminophen Dihydrocodeine Morphine |
| Ranjit 2016 | Spinal positioning, intraoperative and postoperative analgesia | Before spinal anaesthesia | Spinal anaesthesia | Femoral nerve block Dual technique: nerve stimulator plus in‐plane ultrasound guidance Single injection Lidocaine 2% 20 mL Operator: anaesthesiology department |
No nerve block IV Fentanyl |
IV Fentanyl |
| Segado Jimenez 2009 | Postoperative analgesia | In post‐anaesthesia care unit after full recuperation of motor blockade from the spinal block | Spinal anaesthesia | 1) Lateral femoral cutaneous nerve block
2) Obturator nerve block Landmarks Single injections 1) Bupivacaine 0.5% with vasoconstrictor 5 mL 2) Bupivacaine 0.5% with vasoconstrictor 15 mL Operator: anaesthesiology department |
No nerve block | IV Metamizole Dexketoprofen trometamol Tramadol Morphine |
| Spansberg 1996 | Postoperative analgesia | Catheters inserted before spinal anaesthesia Administration of local anaesthetics started after surgery |
Spinal anaesthesia | Femoral nerve block Nerve stimulator Continuous infusion (non‐stimulating catheter advanced 8 to 15 cm past needle tip) Bupivacaine 0.5% 0.4 mL/kg followed by bupivacaine 0.25% at 0.14 mL/kg/hour for 16 hours after surgery Operator: anaesthesiology department |
Sham block with saline | Morphine Acetylsalicylic acid |
| Szucs 2010 | Preoperative, intraoperative, and postoperative analgesia | Catheters inserted in the emergency department Administration of local anaesthetics started during catheter installation |
Spinal anaesthesia | Femoral nerve block Nerve stimulator (quadriceps contraction resulting in patellar movement with 0.4 mA and 0.1 millisecond) Continuous infusion (non‐stimulating catheter, space dilated with 10 mL of lidocaine 2%, catheter advanced cephalad 3 cm past the needle tip) Bupivacaine 0.5% 10 mL followed by 0.25% bupivacaine at 4 mL/hour for 72 hours Bolus of 2% lidocaine 10 mL 15 minutes before positioning for spinal anaesthesia Operator: anaesthesiology department |
No nerve block | Paracetamol Morphine |
| Thompson 2019 | Intraoperative and postoperative analgesia | Immediately before induction of anaesthesia | General or spinal anaesthesia (38%) | Fascia iliaca compartment block Ultrasound‐guided Single injection Ropivacaine 0.25% 30 mL Operator: a board‐certified anaesthesiologist |
No nerve block | Acetaminophen Tramadol Opioids |
| Tuncer 2003 | Postoperative analgesia | After surgery and reversal of neuromuscular blockade | General anaesthesia | Femoral (3‐in‐1) nerve block Nerve stimulator (quadriceps contraction with patellar ascension with < 1 mA) Continuous infusion (non‐stimulating catheter advanced 4 to 5 cm past the needle tip) Lidocaine 2% with epinephrine 5 mcg/mL 30 mL followed by bupivacaine 0.125% patient‐controlled analgesia: basal rate 4 mL/hour, boluses 3 mL, lockout time 20 minutes Operator: probably anaesthesiology department |
No nerve block IV PCA with Morphine |
Tenoxicam |
| Unneby 2017 | Preoperative analgesia | Before surgery, as soon as possible after admission to the orthopaedic ward | No information | Femoral nerve block Nerve stimulator (quadriceps contraction) Single injection Levobupivacaine 0.25% 20 to 40 mL In case of delayed surgery or if otherwise necessary, participants could receive 1 additional block Operator: 36 anaesthesiologists with various training |
No nerve block | Opioids |
| Uysal 2018 | Preoperative analgesia | In the emergency department | Spinal anaesthesia | Femoral nerve block Dual technique: ultrasound‐guided (in‐plane) and nerve stimulator (quadriceps contraction) Repeated doses every 8 hours through a catheter Bupivacaine 0.25% 10 mL | No nerve block IV Paracetamol |
IV Tramadol Epidural analgesia after surgery |
| Wang 2015 | Preoperative, intraoperative, and postoperative analgesia | Upon admission, after radiographic confirmation of the diagnosis | Combined spinal‐epidural anaesthesia | Fascia iliaca compartment block Ultrasound‐guided (out‐of‐plane for needle insertion and in‐plane for solution diffusion, injected cephalad) Continuous infusion (catheter inserted 5 to 10 cm past the needle tip) Ropivacaine 0.4% 50 mL followed by ropivacaine 0.2% at 5 mL/hour (plus 5 mL top‐up doses) Operator: anaesthesiologist with experience in ultrasound‑guided nerve block |
Sham block with saline Paracetamol Tramadol |
IVPCA with Sufentanil after surgery |
| White 1980 | Intraoperative and postoperative analgesia | After induction of anaesthesia, before surgery | General anaesthesia | Psoas compartment block Landmarks Single injection Mepivacaine 2% 30 mL Operator: anaesthesiology department |
No nerve block | Usual surgical care |
| Yamamoto 2016 | Spinal positioning, intraoperative and postoperative analgesia | Before spinal anaesthesia | Spinal anaesthesia | Fascia iliaca compartment block Ultrasound‐guided Single injection Levobupivacaine 0.25% 40 mL Operator: an orthopaedic surgeon with extensive experience in this block procedure |
No nerve block IV Acetaminophen |
Diclofenac Rescue analgesics |
| Yang 2016 | Intraoperative and postoperative analgesia | Catheter insertion and local anaesthetic administration started before induction of anaesthesia | General anaesthesia | Fascia iliaca compartment block Ultrasound‐guided Continuous infusion Ropivacaine 0.33% 30 mL followed by 0.15% ropivacaine at 2 mL/hour plus a bolus of 30 mL 0.15% ropivacaine every 24 hours for 72 hours after surgery Operator: anaesthesiology department |
No nerve block IV PCA with Sufentanil |
Rescue analgesics |
| Yun 2009 | Spinal positioning, intraoperative and postoperative analgesia | Before spinal anaesthesia | Spinal anaesthesia | Fascia iliaca compartment block Landmarks Single injection Ropivacaine 0.375% 30 mL Operator: 1 experienced anaesthesiologist |
No nerve block IV Alfentanil |
IV Alfentanil for spinal block Pethidine before spinal block and after surgery |
G: gram.
h: hour.
IM: intramuscular.
IV: inteavenous.
mA: milliAmpere.
mcg/mL: microgram/millilitre.
mg/kg: milligram/kilogram.
MHz: megahertz.
mL: millilitre.
msec: millisecond.
n: number.
NSAIDs: non‐steroidal anti‐inflammatory drugs.
PCA: patient‐controlled analgesia.
SC: subcutaneous.
PNBs performed included a femoral nerve block (femoral or three‐in‐one block or triple nerve block) (N = 22; Antonopoulou 2006; Coad 1991; Cuvillon 2007; De La Tabla 2010; Deniz 2014; Fletcher 2003; Gille 2006; Graham 2008; Haddad 1995; Henderson 2008; Jadon 2014; Jang 2018; Kullenberg 2004; Liebmann 2012; Luger 2012; Murgue 2006; Ranjit 2016; Spansberg 1996; Szucs 2010; Tuncer 2003; Unneby 2017; Uysal 2018), a femoral nerve block plus an infiltration above the iliac crest (N = 1; Hood 1991), a femoral nerve block followed by a fascia iliaca block (N =1; Morrison 2008), a fascia iliaca compartment block (N = 21; Albrecht 2014; Bang 2016; Brownbridge 2018; Deniz 2014; Diakomi 2014; Domac 2015; Foss 2005a; Godoy Monzon 2010; Gürtan Bölükbasi 2013; Hogg 2009; Landsting 2008; Ma 2018a; Madabushi 2016; Mosaffa 2005; Mouzopoulos 2009; Nie 2015; Thompson 2019; Wang 2015; Yamamoto 2016; Yang 2016; Yun 2009), a lateral femoral cutaneous nerve block (N = 2; Coad 1991; Jones 1985), a lateral femoral cutaneous nerve block plus an obturator nerve block (N = 1; Segado Jimenez 2009), an obturator nerve block (N = 1; Segado Jimenez 2009), or a psoas compartment block (N = 3; Altermatt 2013; Chudinov 1999; White 1980).
Techniques of localization used for PNBs included loss of resistance to air (N = 1; Chudinov 1999), use of nerve stimulator (N = 14; Altermatt 2013; Antonopoulou 2006; Cuvillon 2007; Gille 2006; Graham 2008; Henderson 2008; Hood 1991; Jadon 2014; Kullenberg 2004; Murgue 2006; Spansberg 1996; Szucs 2010; Tuncer 2003; Unneby 2017), paraesthesia (N = 2; Fletcher 2003; Haddad 1995), ultrasound with or without a nerve stimulator (N = 15; Bang 2016; De La Tabla 2010; Deniz 2014; Gürtan Bölükbasi 2013 ; Jang 2018; Liebmann 2012; Luger 2012; Ma 2018a; Morrison 2008; Ranjit 2016; Thompson 2019; Uysal 2018; Wang 2015; Yamamoto 2016; Yang 2016), or landmarks (N = 15; Albrecht 2014; Brownbridge 2018; Coad 1991; Diakomi 2014; Domac 2015; Foss 2005a; Godoy Monzon 2010; Jones 1985; Landsting 2008; Madabushi 2016; Mouzopoulos 2009; Nie 2015; Segado Jimenez 2009; White 1980; Yun 2009). Hogg 2009 and Mosaffa 2005 provided no information on the localizing technique.
PNBs were single‐injection PNBs or continuous PNBs (infusion or repeated doses) (N = 17; Altermatt 2013; Antonopoulou 2006; Brownbridge 2018; Chudinov 1999; Cuvillon 2007; De La Tabla 2010; Gille 2006; Luger 2012; Ma 2018a; Morrison 2008; Mouzopoulos 2009; Nie 2015; Spansberg 1996; Szucs 2010; Tuncer 2003; Wang 2015; Yang 2016) given for a duration ranging from 15 to 72 hours.
Investigators performed PNBs for preoperative analgesia (N = 14; Albrecht 2014; Fletcher 2003; Foss 2005a; Godoy Monzon 2010; Graham 2008; Haddad 1995; Henderson 2008; Jang 2018; Kullenberg 2004; Landsting 2008; Liebmann 2012; Ma 2018a; Murgue 2006; Uysal 2018); for preoperative, intraoperative, and postoperative analgesia (N = 10; Altermatt 2013; Brownbridge 2018; Chudinov 1999; De La Tabla 2010; Gille 2006; Luger 2012; Morrison 2008; Szucs 2010; Unneby 2017; Wang 2015); for spinal positioning and intraoperative and postoperative analgesia (N = 10; Diakomi 2014; Domac 2015; Gürtan Bölükbasi 2013; Hogg 2009; Jadon 2014; Madabushi 2016; Mosaffa 2005; Ranjit 2016; Yamamoto 2016; Yun 2009); for preoperative and postoperative analgesia (N = 1; Mouzopoulos 2009); for intraoperative and postoperative analgesia (N = 5; Deniz 2014; Hood 1991; Thompson 2019; White 1980; Yang 2016); or for postoperative analgesia (N = 9; Antonopoulou 2006; Bang 2016; Coad 1991; Cuvillon 2007; Jones 1985; Nie 2015; Segado Jimenez 2009; Spansberg 1996; Tuncer 2003). Exact time of block placement can be found in Table 2.
Excluded studies
We excluded 46 studies based on study design (Akhtar 2015; Arsoy 2017; Arsoy 2017a; Barnes 2019; Beaudoin 2010; Bendtsen 2015b; Callear 2016; Candal‐Couto 2005; Castillon 2017; Chang 2011; Christos 2010; Dulaney‐Cripe 2012; Elkhodair 2011; Evans 2019; Finlayson 1988; Foss 2009; Fujihara 2013; Godoy Monzon 2007; Gosavi 2001; Gozlan 2005; Grigg 2009; Groot 2015; Haines 2012; Hauritz 2009; Helsø 2016; Hogh 2008; Irwin 2012; Isalgue 2014; Ishioka 2018; Kassam 2018; Klukowski 2017; Kumar 2016; Kumie 2015; Leeper 2012; Levente 2017; Lopez 2003; McGlone 1987; Perrier 2010; Randall 2008; Rapchuk 2013; Rojas Rivera 2002; Tao 2016; Thakur 2018; Vats 2016; Wang 2019; Williams 2016); 20 trials because they studied a different population (Anaraki 2012; Bhadani 2017; Bulger 2015; Carlisle 2004; Durrani 2013; Iamaroon 2010; Kacha 2018; Levine 2003; Li 2013; Masoumi 2014; McRae 2015; Memary 2015; Mostafa 2015; Mutty 2007; Pakhare 2016; Reddy 2016; Segado Jimenez 2010; Shi 2018; Sia 2004; Singh 2016); and 40 trials because they studied a different intervention (Amini 2012; Amiri 2012; Aprato 2018; Bech 2011; Bendtsen 2015a; Bhattacharya 2019; Bouhours 2010; Dodd 2019; Foss 2005; Gasanova 2019; George 2016; Ghimire 2015; Gorodetskyi 2007; Hao 2018; Hoffmann 2015; Hussain 2014; Inan 2009; Kang 2013; Kristek 2019; Lee 2015; Lee 2016; Li 2013; Mannion 2005; Manohara 2015; Marhofer 1998; Matot 2003; Nielsen 2015; Parras 2016; Piangatelli 2004; Rashwan 2013; Reavley 2015; Sahota 2011; Scheinin 2000; Sonawane 2019; Swart 2017; Turker 2003; Van Leeuwen 2000; Wei 2018; Zadeh 2015; Zheng 2017). Five trials were either terminated or withdrawn by study authors (Bendtsen 2014; Bendtsen 2015; Hallberg 2012; Siguira 2014; WHO Int 2007). Details on reasons for exclusion can be found in Characteristics of excluded studies tables.
Studies awaiting classification
We have no studies awaiting classification.
Ongoing studies
We found 29 ongoing trials (Capelleri 2017; Carvalho 2015; Chinachoti 2010; Chiu 2016; ClinicalTrials.gov 2019; Compere 2012; Cong 2016; Dhimar 2017; Diakomi 2015; El Sharkawy 2016; Kulkarni 2018; Levins 2006; Li 2018; Luo 2019; Mathijssen 2015; Nguyen 2018; Park 2009; Postma 2017; Qiu 2018; Ridderikhof 2015; Saga 2019; Sahiti 2019; Shah 2016; Tsui 2015; Winso 2009; Xi 2014; Xuesheng 2019; Yuan 2017; Yun 2018). Details on ongoing trials can be found under Characteristics of ongoing studies. Fifteen trials were first posted (N = 10; ClinicalTrials.gov 2019; Kulkarni 2018; Li 2018; Luo 2019; Nguyen 2018; Qiu 2018; Saga 2019; Sahiti 2019; Xuesheng 2019; Yun 2018), or they were at least last updated (N = 5; Capelleri 2017; Dhimar 2017; Diakomi 2015; Postma 2017; Ridderikhof 2015), after 1 January 2018.
Risk of bias in included studies
A summary of the risks of bias of studies included in each analysis can be found in forest plots of each outcome (Analysis 1.1; Analysis 1.2; Analysis 1.3; Analysis 1.4; Analysis 1.5; Analysis 1.6; Analysis 1.7). Risk of bias assessments for each outcome, including all domain judgements and support for judgement, is located in the Risk of bias section (located after the Characteristics of included studies). Additional details on how the Risk of Bias‐2 tool was applied for each trial for each outcome can be found in the supplemental data file available in Figshare (Guay 2020).
1.1. Analysis.

Comparison 1: Peripheral nerve blocks (PNBs) versus no nerve block (or sham block), Outcome 1: Pain on movement within 30 minutes of block placement
1.2. Analysis.

Comparison 1: Peripheral nerve blocks (PNBs) versus no nerve block (or sham block), Outcome 2: Acute confusional state
1.3. Analysis.

Comparison 1: Peripheral nerve blocks (PNBs) versus no nerve block (or sham block), Outcome 3: Myocardial infarction
1.4. Analysis.

Comparison 1: Peripheral nerve blocks (PNBs) versus no nerve block (or sham block), Outcome 4: Chest infections
1.5. Analysis.

Comparison 1: Peripheral nerve blocks (PNBs) versus no nerve block (or sham block), Outcome 5: Mortality
1.6. Analysis.

Comparison 1: Peripheral nerve blocks (PNBs) versus no nerve block (or sham block), Outcome 6: Time to first mobilization
1.7. Analysis.

Comparison 1: Peripheral nerve blocks (PNBs) versus no nerve block (or sham block), Outcome 7: Costs of analgesic drugs
Briefly, the number of results at high risk of bias was low. Reasons to judge risk of bias as high were: possible problems with randomization (one trial), missing data and inability to determine whether or not missingness was related to the outcome (one trial for pain on movement at 30 minutes after block placement and one trial for acute confusional state), deviation from pre‐planned analysis (one trial for pain on movement at 30 minutes after block placement), and possible unplanned outcome at the specific time point measured (one trial for mortality). Details on the implications of assessments of risk of bias for each specific result are reported in the Effects of interventions section.
Effects of interventions
See: Table 1
Primary outcomes
1. Pain
1.1 Pain on movement and at rest within 30 minutes after block placement
Pain on movement at 30 minutes after block placement
We did not retain data from three studies for this analysis due to inappropriate timing of outcome measurement. Jadon 2014 evaluated pain scores during positioning for spinal anaesthesia five minutes after a femoral nerve block performed with a nerve stimulator and 20 mL of a solution containing 15 mL of lidocaine 2% and 5 mL of distilled water. Parkinson 1989 reported that at five minutes after a femoral nerve block with lidocaine‐HCl and a nerve stimulator, only 6 and 11 participants out of 20 would have a complete or partial femoral nerve block, and 15 minutes would be required for a complete or partial femoral nerve block in all participants. Mosaffa 2005 evaluated pain scores during positioning for spinal anaesthesia five minutes after a fascia iliaca block with 20 mL of lidocaine 1.5%. Although some effects on pain scores can be seen at 10 minutes after a fascia iliaca block with lidocaine, maximal effects are more likely to occur at 30 minutes or later (Dochez 2014; Gozlan 2005). For Brownbridge 2018, the exact time point was unclear.
We retained 11 trials that included 503 participants and evaluated pain on movement within 30 minutes after block placement (Albrecht 2014; Diakomi 2014; Domac 2015; Foss 2005a; Gille 2006; Hogg 2009; Landsting 2008; Murgue 2006; Ranjit 2016; Szucs 2010; Yun 2009). The specific intervention was a femoral nerve block ‐ Gille 2006; Murgue 2006; Ranjit 2016; Szucs 2010 ‐ or a fascia iliaca block ‐ Albrecht 2014; Diakomi 2014; Domac 2015; Foss 2005a; Hogg 2009; Landsting 2008; Yun 2009. Pain scores were lower with PNBs (standardized mean difference (SMD) ‐1.05, 95% CI ‐1.25 to ‐0.86; I2 = 83%; Analysis 1.1; Figure 2). There was no statistical difference between a femoral nerve block versus a fascia iliaca block (P value for difference between subgroups 0.16). On the basis of a typical standard deviation in the control group of one study (2.4 (Diakomi 2014)), this was equivalent to ‐2.5 on a scale from 0 to 10.
2.

We identified possible significant risk of bias for two trials for this outcome (Figure 2). Landsting 2008 was judged as at high risk of bias for bias due to missing outcome data, as results for this outcome were available for 33 out of 66 participants randomized to the intervention group and for 38 out of 61 participants randomized to the comparator group. No information was provided on possible differences between participants with and without missing values. We had no information to help us determine whether or not missingness in the outcome could depend on its true value. Albrecht 2014 was judged as at high risk of bias in selection of the reported result due to the fact that study authors elected to deviate from the original planned analysis when they realized that the two groups had different mean baseline scores.
When the two trials at high risk of bias for this outcome were excluded (Albrecht 2014; Landsting 2008), SMD was ‐1.12 (95% CI ‐1.34 to ‐0.90). Egger's regression intercept showed the possibility of a small‐study effect as a source of heterogeneity (P = 0.03; 2‐tailed). Duval and Tweedie's trim and fill analysis showed the possibility of publication bias. Correcting for the possibility of publication bias would give an SMD of ‐0.88 (95% CI ‐1.07 to ‐0.70; Figure 3). Excluding trials at high risk of bias and one study that did not provide the exact concentration of local anaesthetic injected ‐ Murgue 2006 ‐ led to an effect size that was correlated with the concentration of local anaesthetic used in lidocaine equivalent (P = 0.0003; Figure 4). We calculated equivalences as mentioned in the methods section (i.e. lidocaine = 1, bupivacaine = 4, chloroprocaine = 1.5, dibucaine = 4, etidocaine = 4, levobupivacaine = 3.9, mepivacaine = 0.8, prilocaine = 0.9, procaine = 0.5, ropivacaine = 3, and tetracaine = 4) (Berde 2009). Therefore, for Diakomi 2014, the concentration in lidocaine equivalent was calculated as 15 mg/mL (ropivacaine 0.5% or ropivacaine 5 mg/mL multiplied by 3 = 15 mg/mL). For Domac 2015, the concentration in lidocaine equivalent was calculated as 20 mg/mL (mixture of 15 mL bupivacaine 0.5% or bupivacaine 5 mg/mL multiplied by 4 = 20 mg/mL and 2% lidocaine or lidocaine 20 mg/mL). For Foss 2005a, the equivalence was calculated as 8 mg/mL (mepivacaine 1% or mepivacaine 10 mg/mL multiplied 0.8 = 8 mg/mL). For Gille 2006, the lidocaine equivalent was calculated as 9 mg/mL (1% prilocaine or prilocaine 10 mg/mL multiplied by 0.9 = 9 mg/mL). For Hogg 2009, the solution injected was lidocaine 1% (or 10 mg/mL). For Ranjit 2016, the solution injected was lidocaine 2% (or 20 mg/mL). For Szucs 2010, the equivalence was calculated as 20 mg/mL (10 mL of 2% lidocaine or lidocaine 20 mg/mL and 10 mL of 0.5% bupivacaine or bupivacaine 5 mg/mL multiplied by 4 = 20 mg/mL). For Yun 2009, the equivalence was calculated as 11.25 mg/mL (ropivacaine 0.375% or ropivacaine 3.75 mg/mL multiplied by 3 = 11.25 mg/mL). Results from Diakomi 2014 (mean and SD of the control group 7.5 and 2.4) show that 182 participants (91 per group) would be required in a simple trial to eliminate a difference of 1 on a 0 to 10 scale (alpha 0.05; beta 0.2; two‐sided test) (http://stat.ubc.ca/~rollin/stats/ssize/n2a.html).
3.
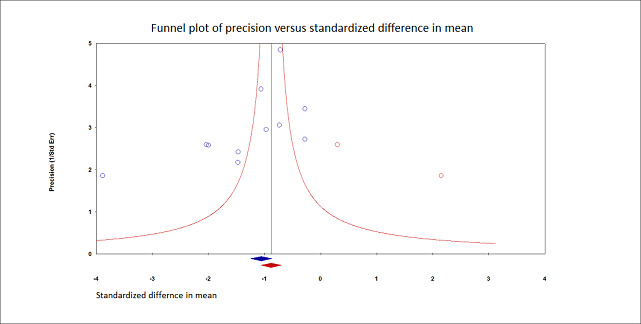
Pain on movement at 30 minutes after block placement.
Duval and Tweedie's trim and fill analysis: blue circles indicate studies found, and red circles are imputed studies. Correcting for the possibility of publication bias would give an estimated standardized mean difference of ‐0.88 (95% confidence interval ‐1.07 to ‐070).
4.
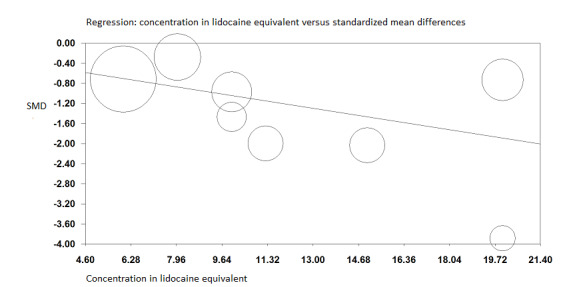
Pain on movement at 30 minutes after block placement.
A meta‐regression indicates that the effect size was proportional to the concentration of local anaesthetic injected in lidocaine equivalents; P = 0.0003.
Level of certainty for pain on movement at 30 minutes after block placement
We did not downgrade for risk of bias because the effect was still present when trials at high risk of bias were excluded from the analysis. We did not downgrade the level of certainty on the basis of inconsistency because we found a reasonable explanation for heterogeneity. We used direct comparisons only with studies performed on the population of interest, and this is not a surrogate marker. The optimal information size was achieved. We did not downgrade for publication bias because the effect was still present after correction for this possibility. We rated the level of certainty as high.
2. Acute confusional state
We have provided in Appendix 3 definitions for acute confusional state used by study authors. Based on 13 trials with 1072 participants (Brownbridge 2018; Cuvillon 2007; Godoy Monzon 2010; Graham 2008; Kullenberg 2004; Liebmann 2012; Morrison 2008; Mouzopoulos 2009; Nie 2015; Uysal 2018; White 1980 ; Yamamoto 2016; Yang 2016), the risk of acute confusional state was reduced by the use of PNBs (RR 0.67, 95% CI 0.50 to 0.90; I2 = 16%; Analysis 1.2; Figure 5). There was no statistical difference according to the type of localizing technique used (landmark versus nerve stimulation versus ultrasound guidance; P value for difference between subgroups 0.75).
5.

Forest plot of comparison: 1 Nerve block versus other modes of analgesia, outcome: 1.11 Acute confusional state.
Godoy Monzon 2010 was judged as at high risk of bias for this outcome due to a large quantity of missing data in the comparator group yielding two very unequal groups (i.e. 92 for the intervention group and 62 for the comparator group). We had no information to help us determine whether or not missingness in the outcome could depend on its true value. Excluding Godoy Monzon 2010, the estimate would be RR 0.70 (95% CI 0.52 to 0.95; I2 = 9%).
Egger's regression intercept showed no evidence of small‐study effect. Duval and Tweedie's trim and fill analysis calculated that two trials might be missing to right of mean for an adjusted point of estimate of RR 0.70 (95% CI 0.51 to 0.94; Figure 6). Given a rate of 30% (Arshi 2018), the number of participants required in a large trial to eliminate a 25% decrease would be 850 (425 per group) (alpha 0.05; beta 0.2; one‐sided test). The NNTB was 12 (95% CI 7 to 47).
6.

Acute confusional state.
Duval and Tweedie's trim and fill analysis: blue circles indicate studies found, and red circles are imputed studies. Correcting for the possibility of publication bias would give an estimated risk ratio 0.70 (95% CI 0.51 to 0.94).
Level of certainty for acute confusional state
We did not downgrade the level of certainty for risk of bias because the effect was still present when we excluded the trial at high risk of bias. We did not downgrade for heterogeneity (I2 < 25%). We included only direct comparisons performed on the population of interest, and this is not a surrogate marker. We did not downgrade for imprecision because the optimal information size was achieved. We did not downgrade the level of certainty on the basis of the possibility of publication bias because applying a correction for the possibility of one would not modify the conclusion. We rated the level of certainty of evidence as high.
3. Myocardial infarction
Only one small trial with 31 participants reported data suitable for extraction for myocardial infarction (Altermatt 2013). There were no events (Analysis 1.3). The definition used can be found in Appendix 4.
Altermatt 2013 was judged as at low risk of bias for this outcome.
Level of certainty for myocardial infarction
The trial was not at high risk of bias. We downgraded the level by two for imprecision and rated the level of certainty as low.
Secondary outcomes
1. Chest infection
Results of three trials with 131 participants show that PNBs reduced the risk of chest infection (RR 0.41, 95% CI 0.19 to 0.89; I2 = 3%; Analysis 1.4; Figure 7) (Fletcher 2003; Haddad 1995; White 1980). Definitions used by study authors are provided in Appendix 5.
7.

The three trials were judged as at low risk of bias for this outcome. Egger's regression intercept showed no significant evidence of a small‐study effect. Duval and Tweedie's trim and fill analysis revealed no evidence of publication bias. Given a basal rate of 27%, the NNTB would be 7 (95% CI 5 to 72) and the number of participants required to eliminate a 25% decrease in a large trial would be 978 (489 per group) (alpha 0.05; beta 0.2; one‐sided test).
Level of certainty for chest infection
We did not downgrade for risk of bias because no trial was judged as at high risk of bias. Statistical heterogeneity was less than 25% (I2 = 3%). We used direct comparisons only with studies performed on the population of interest, and this is not a surrogate marker. The optimal information size was not achieved, so we downgraded by one level for imprecision. We found no evidence of publication bias. We rated the level of certainty as moderate.
2. Mortality
Based on 11 trials including 617 participants (Albrecht 2014; Brownbridge 2018; Cuvillon 2007; De La Tabla 2010; Fletcher 2003; Haddad 1995; Hood 1991; Jones 1985; Morrison 2008; Wang 2015; White 1980), we did not find a difference in short‐term (within six months) mortality (RR 0.87, 95% CI 0.47 to 1.60; I2 = 0%; Analysis 1.5; Figure 8). There was no statistical difference according to the type of block (i.e. single injection versus continuous infusion) (P value for the difference between subgroups 0.67).
8.

Two trials were judged at high risk of bias for this result (Albrecht 2014; De La Tabla 2010). The study Albrecht 2014 was judged as at high risk for selection of the reported result due to the fact that mortality was not an outcome for this trial, and that no other outcome had this specific time point for measurement when the trial was registered. The study De La Tabla 2010 was judged at high risk for randomization process due to the fact that groups were of very unequal sizes (i.e. 11 participants allocated to the intervention group and 38 participants allocated to the comparator group).
With exclusion of the two trials at high risk of bias (Albrecht 2014; De La Tabla 2010), the estimate would be RR 0.81 (95% CI 0.42 to 1.59).
Egger's regression intercept showed no significant evidence of a small‐study effect. Correcting for the possibility of publication bias with Duval and Tweedie's trim and fill analysis would yield an estimate of RR 0.78 (95% CI 0.41 to 1.51). Given an incidence of 9.8%, 3228 participants (1614 per group) would have been required to eliminate a 25% reduction (alpha 0.05; beta 0.2; one‐sided test).
Level of certainty for mortality within six months
We did not downgrade for risk of bias because excluding the two trials judged as at high risk of bias would not change the conclusion. We noted no heterogeneity. We used direct comparisons only with studies performed on the population of interest, and this is not a surrogate marker. Correcting for the possibility of publication bias would not change the conclusion. We downgraded the level of evidence by two for imprecision because the confidence interval included both absence of effect and important benefit. We rated the level of certainty as low.
3. Time to first mobilization
Findings of three trials with 208 participants show that PNBs reduced time to first mobilization (MD ‐10.80, 95% CI ‐12.83 to ‐8.77 hours; I2 = 41%; Analysis 1.6) (Kullenberg 2004; Segado Jimenez 2009; Yamamoto 2016).
All three trials were judged as at low risk of bias for this outcome.
Egger's regression intercept showed no evidence of a small‐study effect. Correcting for the possibility of publication bias would yield an estimate of MD ‐11.17 hours (95% CI ‐13.07 to ‐9.26).
Level of certainty for time to first mobilization
We did not downgrade the level of certainty for risk of bias because no trial was judged at high risk of bias. We downgraded certainty by one level for a moderate amount of heterogeneity. We used direct comparisons only with studies performed on the population of interest, and this is not a surrogate marker. We did not downgrade evidence for imprecision. The effect was still present with correction for the possibility of publication bias. We rated the level of certainty as moderate.
4. Costs of analgesic regimens
One trial with 75 participants reported that costs related to analgesia were reduced when PNBs were given as a single‐injection PNB (MD ‐4.40 euros (2009 value), 95% CI ‐4.84 to ‐3.96; Analysis 1.7) compared to no nerve block (Segado Jimenez 2009). Segado Jimenez 2009 was judged as at low risk of bias for this outcome.
Level of certainty for costs of analgesic regimens
The trial was not at high risk of bias. The comparison was a direct one. We downgraded the evidence by two levels for the small number of trials included. We could not assess publication bias. We rated the level of certainty as low.
Complications
Complications of analgesic techniques can be found in Table 3.
2. Complications of blocks and/or analgesic techniques.
| Study | Complications related to regional anaesthesia | Complications related to analgesic technique |
| Albrecht 2014 | Not reported | Not reported |
| Altermatt 2013 | Not reported | Not reported |
| Antonopoulou 2006 | No complications such as motor block. local haematoma or infection, inadvertent arterial puncture, direct nerve damage, and cardiovascular or neurological toxicity were observed Five participants had accidental removal of the catheter: 4 during the procedure or while the catheter was secured, and 1 while in the ward |
Not reported |
| Bang 2016 | No patient developed any residual sensory‐motor deficit during the postoperative period | Patients in the non‐block group had nausea (N=2) and pruritus (N=1), and 1 patient in the block group had nausea within the first 2 postoperative days |
| Brownbridge 2018 | Not reported | Respiratory complications in 5 out of 15 participants for each group Opioid side effects after enrolment: 3/15 in the block group; 7/15 in the non‐block group |
| Chudinov 1999 | No major complications in group regional blockade were described. Three participants developed local erythema at the catheter insertion site at the end of the study period No signs of local anaesthetic toxicity were documented One participant developed bilateral blockade (L1‐L3 on the opposite side) |
Not reported |
| Coad 1991 | No complications related to nerve blocks and no case of prolonged motor blockade | Not reported |
| Cuvillon 2007 | Four catheters were prematurely removed: 1 by a confused participant, 2 by nurses (unexplained fever), and 1 by a surgeon (unconfirmed suspicion of local anaesthetic toxicity) (ropivacaine blood level < 2 ng/mL)) | More constipation (47% vs 19% for regional blockade) |
| De La Tabla 2010 | Not reported | Not reported |
| Deniz 2014 | Hypotension occurred in 1 participant in the fascia iliaca compartment block group (1/20) and in 1 participant in the femoral nerve block group (1/20) There was no complication that might be relevant to fascia iliaca compartment block in our study In 1 case, prolonged (4 months) temporary motor and sensory neurological deficits occurred due to 3‐in‐1 block |
Hypotension occurred in 2 patients with IV patient‐controlled analgesia (2/20), requiring stopping of IV patient‐controlled analgesia |
| Diakomi 2014 | Complications such as local anaesthetic toxicity recorded as well (none reported in results section) Nor did complication rates vary between groups |
Complications such as hypoventilation (breathing rate < 8 breaths/min) were recorded as well Moreover, the 2 groups did not differ in these parameters at any time point until study completion at 24 hours after surgery. Nor did complication rates vary between groups |
| Domac 2015 | Not reported | Not reported |
| Fletcher 2003 | Among study participants, none experienced adverse effects as a result of nerve block administration | No clinically important differences between groups with respect to pulse rate, oxygen saturation, or respiratory rate at any time interval. Oxygen saturation 94.87% |
| Foss 2005a | No side effects attributable to femoral nerve block were noted in any participants during their hospital stay | More participants (P = 0.05) in the morphine group were sedated at 180 minutes after block placement No difference in nausea and vomiting was noted between groups, with 3 participants in each group having these side effects Tendency towards lower saturation was noted in the opioid group at 60 and 180 minutes after the block despite oxygen supplementation (P = 0.08) |
| Gille 2006 | One inadvertent arterial puncture and blood aspiration positive for 3 participants Two transient paraesthesias No catheter site infection Ten catheters accidentally removed No severe complications related to analgesia |
No respiratory depression from systemic analgesia and no allergic reactions All complications were reversible |
| Godoy Monzon 2010 | The only complications were local bruises at the site of injection | Two participants with nausea and 2 with nausea and vomiting |
| Graham 2008 | No immediate complications occurred in either group defined as inadvertent vascular puncture, anaphylaxis or collapse, severe pain, or inability to tolerate the procedure | No immediate complications were noted in either group |
| Haddad 1995 | No local or systemic complications of femoral nerve blocks were noted | Not reported |
| Henderson 2008 | No complications associated with femoral nerve block were noted | Not reported |
| Hogg 2009 | One patient was withdrawn from the fascia iliaca compartment block group due to new‐onset arrhythmia | Not reported |
| Hood 1991 | No untoward sequelae were associated with nerve blocks All plasma prilocaine concentrations (maximum 3 pg/mL) were below the suggested threshold for toxicity for prilocaine of 6 pg/mL |
Not reported |
| Jadon 2014 | Not reported | In participants of fentanyl group, drowsiness was observed that required the presence of more persons holding the participant during positioning SpO2 was significantly lower in the fentanyl group (P = 0.001). However, no participant in either group had SpO2 < 90% during the procedure Mean arterial blood pressure was significantly lower in the fentanyl group (P = 0.0019) |
| Jang 2018 | All femoral nerve block procedures required a single attempt and no complications were observed | Nausea and vomiting 4 vs 6, hypotension 2 vs 4, pruritus 0 vs 1, and desaturation 3 vs 2 for intervention and comparator, respectively |
| Jones 1985 | No untoward sequelae associated with the nerve block were seen | Not reported |
| Kullenberg 2004 | No complications related to the nerve blockade were noted in this study | Not reported |
| Landsting 2008 | No serious adverse events due to the fascia iliaca compartment block were reported in this study | Not reported |
| Liebmann 2012 | No other adverse events were noted during the study period, and no other adverse events were reported to study investigators | Four‐hour oxygen saturation (%) 96 (93 to 99) vs (%) 98 (95 to 99) for regional blockade Adverse events: Hypotension, number (%) 3 (17) vs number (%) 0 (0) for regional blockade Respiratory depression, number (%) 9 (50) vs number (%) 4 (22) for regional blockade Nausea/vomiting, number (%) 5 (28) vs number (%) 5 (28) for regional blockade One participant had an episode of rapid atrial fibrillation requiring diltiazem, but the participant had a history of chronic atrial fibrillation |
| Luger 2012 | Not reported | Not reported |
| Ma 2018a | Two patients’ catheters kinked. This problem was solved after the catheter was adjusted No other complications (local anaesthetic toxicity, puncture site infection, haematoma, catheter dislodgment) occurred |
The occurrence of nausea and vomiting in group fascia iliaca compartment block were lower than those in group control. No patients experienced respiratory depression and over‐sedation in 2 groups during the waiting period |
| Madabushi 2016 | No complications were noted in either group | No complications were noted in either group |
| Morrison 2008 | There were no episodes of bleeding, falls, or catheter‐related infections in the intervention group | Intervention participants were significantly less likely to report opioid side effects |
| Mosaffa 2005 | Not reported | Not reported |
| Mouzopoulos 2009 | No complications of femoral nerve block administration occurred, except 3 local haematomas developed at the injection site, which resolved spontaneously | Not reported |
| Murgue 2006 | Not reported | Not reported |
| Nie 2015 | No adverse effects such as pain at the insertion site or paraesthesia were observed No positive cultures were observed with the fascia iliaca block catheter tip, nor were any signs of infection noted in the current study |
Not reported |
| Ranjit 2016 | There was no inadvertent vascular puncture nor adverse effect of systemic local anaesthetic toxicity in the study group | SpO₂ was significantly lower in the IV fentanyl group during positioning (95 vs 97; P < 0.001) and 5 minutes after (95 vs 98; P < 0.001). However, none of the patients in either group had their oxygen saturation below 90% |
| Segado Jimenez 2009 | We did not observe any complications in the realization of regional anaesthetic techniques during or subsequent to these techniques | The incidence of side effects (sleepiness, hypotension, constipation, pruritus) was greater in the group with no block than in groups with blocks (P < 0.01) |
| Spansberg 1996 | No haematomas at the site of femoral catheters | Two participants in each group experienced nausea and vomiting |
| Szucs 2010 | For 1 participant, the elastomeric pump failed, resulting in local anaesthetic administered over less than 54 hours instead of 72 hours, and another participant, suffering from acute confusional state, disconnected his pump after 12 hours | The incidence of nausea/vomiting, pruritus, or excessive sedation was similar in the 2 groups |
| Thompson 2019 | Of the 23 patients in group fascia iliaca compartment block, there were no intervention‐related complications or adverse events. None of the patients receiving a block reported residual injection site pain, sensory or motor deficits, intravascular injections, cardiopulmonary events, or other adverse events | Not reported |
| Tuncer 2003 | Not reported | Side effects (vomiting and pruritus) were observed significantly more frequently with intravenous analgesia |
| Unneby 2017 | No adverse events related to the femoral nerve block were noted | Not reported |
| Uysal 2018 | Not reported | Not reported |
| Wang 2015 | The study group did not develop complications (local anaesthetic toxicity, puncture site infection, hematoma in preoperative waiting period) | All patients in the present study did not demonstrate symptoms of respiratory depression and excessive sedation in the preoperative waiting period Nausea 7 vs 12 and vomiting 5 vs 5 for intervention and comparator, respectively |
| White 1980 | No participants showed any evidence of local anaesthetic toxicity | Not reported |
| Yamamoto 2016 | Patients were also evaluated for potential drug‐ or block‐related complications during the course of the trial No complications |
Patients were also evaluated for potential drug‐ or block‐related complications during the course of the trial No complications |
| Yang 2016 | Not reported | Fewer side effects for fascia iliaca compartment block group Nausea and vomiting 0 vs 3, respiratory depression 0 vs 1 for intervention and comparator, respectively |
| Yun 2009 | No adverse systemic toxicity of ropivacaine was noted, and neither vascular puncture nor paraesthesia was elicited No complications such as haematoma or persistent paraesthesia were observed in participants with a femoral nerve block within 24 hours after the operation |
Hypoventilation (ventilatory rate 6 to 8/min) or pulse oximetric desaturation (oxygen saturation 88% or 89%) was encountered in 4 participants (20%) in the intravenous analgesia group. This was reverted with assisted manual mask ventilation All participants in the intravenous group experienced mild dizziness, and mild drowsiness was present in 12/20 of them |
Brief summary: For peripheral nerve block, there was no case of systemic local anaesthetic toxicity and no infection. One case of prolonged (4 months) temporary motor and sensory neurological deficit occurred due to a 3‐in‐1 block (Deniz 2014). One new‐onset arrhythmia was reported (Hogg 2009). Four cases of respiratory depression requiring face mask ventilation were reported with intravenous analgesia (Yun 2009). Other opioid side effects such as drowsiness, hypoventilation, desaturation, hypotension, nausea and vomiting, pruritus, and constipation were reported in both groups. No allergic reaction was reported.
%: percentage.
L: litre.
mg: milligram.
min: minute.
ng/mL: nanogram/millilitre.
pg/mL: picogram/millilitre.
Discussion
Summary of main results
We found some advantages of peripheral nerve block (PNB) versus systemic analgesia alone for pain treatment in people with hip fracture. Compared with systemic analgesia, pain on movement within 30 minutes after block placement will be less by approximately 2.5 out of 10 (Analysis 1.1; Table 1). This represents a clear and undeniable advantage over systemic analgesia, especially in this era of opioid crisis.
Acute confusional state is common after hip fracture and may delay rehabilitation, may increase hospital length of stay, and may impede nursing home placement and even increase risk for mortality (Pompei 1994). PNBs reduce the risk of acute confusional state (risk ratio (RR) 0.67, 95% confidence interval (CI) 0.50 to 0.90; Analysis 1.2; Table 1). The pathophysiology of acute confusional state in these patients may be multifactorial and may include side effects of medications used, hypoxaemia, immobilization, infection, and systemic inflammation (Mouzopoulos 2009). PNBs (or local anaesthetics) may have an influence on any of these factors. Also, PNBs are associated with a reduction in opioid consumption (Guay 2017).
We could not demonstrate a reduction in the incidence of myocardial infarction (Table 1). We found it odd that only one trial reported on the risk of myocardial infarction with PNBs (Altermatt 2013). Although the number of participants included in this trial was relatively small, study authors monitored ST segments continuously up to three days after surgery. They reported no difference in ischaemic episodes with a continuous psoas compartment block. This contrasts with results reported by Schenin and colleagues (i.e. a reduction in myocardial ischaemic episodes with an epidural infusion of bupivacaine and fentanyl) (Scheinin 2000). Epidural analgesia has been reported to reduce myocardial infarction in high‐risk patients undergoing high‐risk surgery (Guay 2016a).
Chest infections were reduced with PNBs (Analysis 1.4; Table 1). This could be due to reduced time to first mobilization (Analysis 1.6).
We did not find a reduction in short‐term (up to six months) mortality rate (Analysis 1.5; Table 1), but participants were too few to allow definitive conclusions on this.
Compared with systemic analgesia alone, adding a single‐injection PNB will make little or no difference in the cost of analgesic drugs (equivalent to ‐4 euros per patient in 2009).
Only one trial (Deniz 2014) reported one major complication: a sensory/motor deficit lasting four months with a femoral nerve block (Table 3). This is consistent with information derived from large prospective studies indicating that the incidence of nerve injury lasting longer than six months associated with femoral nerve block would be relatively low, at 0 to 1.2 per 1000 procedures (Auroy 2002; Brull 2007; Sites 2012).
Overall completeness and applicability of evidence
We are confident that our results reflect the actual available literature. More data may be required to evaluate the effects of PNBs on myocardial infarction and death. Indeed the number of participants included for these two outcomes was still below the optimal information size. The population included in these trials reflects quite well the overall adult population with hip fracture, with the exception of patients with dementia, who were often excluded from randomized controlled trials. Furthermore, the low incidence of major complications related to PNBs in this review has probably been made possible by adherence of study authors to recommendations of major societies on the topic. Some recommendations on the prevention of infectious and bleeding complications for each type of regional anaesthetic technique are available at www.asra.com/advisory-guidelines.
Quality of the evidence
We have summarized the certainty of evidence in Table 1. We quantified the level of certainty as high for reduced pain on movement and for acute confusional state, and as moderate for reduced chest infection. Although some studies might not have been perfect, excluding studies at high risk of bias did not change any of our conclusions. The quality of evidence was most often reduced by insufficient numbers of included participants (myocardial infarction, chest infection, death, time to first mobilization, and cost of analgesia).
Potential biases in the review process
Our search was extensive. We chose factors for exploration of heterogeneity a priori. Trials reporting on outcomes included in our summary of findings were evaluated with the Cochrane Risk of Bias‐2 tool. Certainty was evaluated according to the GRADE system.
Cochrane is introducing a new tool for quality evaluation of randomized controlled trials: Risk of Bias‐2. Compared with the previous tool, all trials are now assessed for each domain specifically for each outcome. Indeed evaluation of the quality of a trial may vary according to the outcome for which it is evaluated. Domains are also reorganized differently, and the process of evaluation is much more detailed and extensive (see details under Characteristics of included studies). Using this new tool, very few results had trials at high risk of bias.
Regional blockade is a topic for which adequate blinding of participants and personnel taking care of participants is rarely feasible. A simple evaluation of block effectiveness is incompatible with preserved blinding. Blinding of outcome assessors and at least of the researcher analysing data should, however, often be feasible. Therefore, clarity on how allocation is concealed until the time the participant has been included in the trial and formally attributed to his/her treatment group and to blinding of outcome assessors, as well as of the researcher analysing data, represents domains on which study authors could try to improve the quality of future trials.
Agreements and disagreements with other studies or reviews
Even at rest, the level of pain after hip fracture is relatively high, particularly among those with subtrochanteric fracture (median 5 out of 10) (Foss 2005a). Movement by these individuals immediately after injury is unavoidable: transport from the scene of injury to the hospital, unclothing for medical examination, transport for X‐ray diagnostic confirmation, transfer to the operating room table, positioning for spinal anaesthesia, etc. Movement‐associated median pain ranges from 8 to 10 out of 10, depending on the type of fracture (intracapsular = 8; trochanteric = 9; subtrochanteric = 10) (Foss 2005a).
In our latest previous version of this review (Other published versions of this review), we included 31 trials with 1760 participants. We found that PNBs reduce pain and chest infection. Based on the evidence available at the time, we did not find a difference between PNBs and other modes of analgesia in terms of acute confusional state, but the number of participants included in the 2017 version was insufficient to eliminate a difference in the risk of acute confusional state. In the present version, we included 49 trials with 3061 participants. We confirmed that PNBs reduced pain on movement within 30 minutes after block placement and chest infection. We also found a reduction in acute confusional state.
In Appendix 6, we have summarized the main findings of recent reviews on this topic published in the English language (Amin 2017; Dizdarevic 2019; Fadhlillah 2019; Freeman 2016; Hards 2018; Hartmann 2017; Hong 2019; Hsu 2018; Hsu 2019; Parker 2016; Rashiq 2013; Scurrah 2018; Skjold 2019; Soffin 2019; Steenberg 2018). These reviews included between 2 and 25 trials. Most reviews focused on effects of PNBs on acute pain and confirmed our findings for this outcome. Many reviews evaluated only one specific block compared to systemic analgesia alone (i.e. either a fascia iliaca compartment block or a femoral nerve block). Therefore it is not surprising that none of these reviews included sufficient participants for evaluation of effects of PNBs on major morbidity or mortality. Indeed, chest infection and acute confusional state were not included as outcomes in most of these reviews.
Our review did not include enough participants with adequate follow‐up to evaluate the effects of adding PNBs on mortality in this population with a high level of certainty. A retrospective chart review on 535 patients evaluated the effects of a comprehensive programme, including a switch from systemic opiates to a local anaesthetic femoral nerve catheter block, an earlier assessment by the anaesthesiologist, and a more systematic approach to nutrition, fluid, oxygen therapy, and urinary retention (Pedersen 2008). Investigators reported that overall 12‐month mortality was 29% in the control group and 23% in the intervention group (P = 0.2).
Authors' conclusions
Implications for practice.
The present review shows that peripheral nerve blocks (PNBs) reduce pain on movement at 30 minutes after block placement, as well as the risk of an acute confusional state and probably also the risk of chest infection, compared with systemic analgesia alone. Whether or not these benefits justify the use of PNBs in clinical practice probably has to be judged on a case‐by‐case basis. Although randomized clinical trials may not be the best way to establish risks associated with an intervention, our review confirms the low risk of permanent injury associated with PNBs, as found by others (Neal 2015).
Included trials often excluded patients with dementia (Characteristics of included studies). These patients may be uncooperative and less suitable for awake regional anaesthetic techniques. The American Society of Regional Anesthesia suggests that regional anaesthetic techniques should not be performed routinely in adult patients whose sensorium is compromised by general anaesthesia or deep sedation (Neal 2015). However, adult patients with specific conditions (e.g. developmental delay) may be appropriate exceptions to this recommendation after risk versus benefit is considered (Neal 2015).
The purpose of our review was not to evaluate the relative efficacy of various nerve blocks. However, when looking at our results on pain scores, we found no compelling evidence to favour a femoral nerve block over a fascia iliaca block (Analysis 1.1). This observation, which was based on a single subgroup analysis (indirect evidence), should be interpreted very cautiously. Having said this, and given a femoral nerve block requiring a needle position closer to the nerve and, hence, perhaps increasing the risk of inadvertent intraneural injection, we are inclined to favour the use of fascia iliaca compartment blocks for this population. Risks of inadvertent intravascular injection with systemic local anaesthetic toxicity are present with both techniques but may be decreased with the use of ultrasound guidance (Sites 2014). Use of an intravascular marker (Guay 2006a), repeated aspirations, and slow injection of fractionated doses have also been suggested to decrease the risks of inadvertent intravascular injection of large amounts of local anaesthetics. Finally, adapting doses to a patient's clinical condition and capacity to metabolize and excrete the drug and its metabolites is also part of good clinical practice (Pere 2011; Shammas 1998).
Implications for research.
Given that high‐certainty evidence shows that PNBs reduce pain and acute confusional state and moderate‐certainty evidence indicates that PNBs probably also reduce chest infection compared with systemic analgesia alone, we are reluctant to encourage further randomized controlled trials comparing PNBs with systemic analgesia alone. If patients accept PNBs and have no contraindication to their use, and if the expertise and resources needed to perform them safely are available, we no longer consider it appropriate for patients with a hip fracture to be administered a placebo or sham intervention. We think that evidence is sufficient to support the use of PNBs in patients with hip fracture. However, the ideal technique of PNB (injection site, type of local anaesthetic, dose, the addition of an infusion or not, etc.) may warrant further exploration. Also, good‐quality non‐randomized trials with appropriate sample sizes may help to clarify the potential effects of PNBs on myocardial infarction and mortality (Analysis 1.5).
What's new
| Date | Event | Description |
|---|---|---|
| 1 April 2021 | Amended | Amendment: Risk of Bias (RobB‐2) tables changed to interactive format. |
History
Protocol first published: Issue 3, 1998 Review first published: Issue 2, 1999
| Date | Event | Description |
|---|---|---|
| 27 January 2021 | Amended | Correction to the format of the Risk of Bias figures. |
| 19 February 2020 | New citation required and conclusions have changed | In this update, the conclusions and the certainty of evidence have changed for one outcome. There is now high certainty evidence for a reduction in acute confusional state with the use of peripheral nerve blocks. Previously (2017 update), there was very low certainty evidence of no difference in this outcome. |
| 16 November 2019 | New search has been performed | The search was updated on 16 November 2019. Since the last version of this review (published in 2017), 18 new relevant randomized controlled trials including 1301 participants were published and have been included in this update. This review differs from the 2017 version by assessing the risk of bias of included trials with the risk of bias 2 tool. Two of the authors involved in the 2017 update withdrew from this update. |
| 1 December 2018 | Amended | We reran the search 1 December 2018 |
| 16 August 2016 | New citation required and conclusions have changed | Two new authors joined the review We updated the search in June 2015 We updated the review and brought the methods up‐to‐date We found 55 new studies: 20 included, 13 excluded and 22 ongoing. We left no studies awaiting classification |
| 16 August 2016 | New search has been performed | We reran the search in August 2016 |
| 6 May 2015 | New search has been performed | This review has been transferred to the Anaesthesia, Critical and Emergency Care Group by the Bone, Joint and Muscle Group |
| 17 February 2009 | New search has been performed | For the second substantive update (Issue 2, 2009), we made the following changes. 1. We included the following newly identified studies: Cuvillon 2007, Fletcher 2003, Foss 2005, Foss 2007, Gille 2006, Kullenberg 2004, Matot 2003, Murgue 2006 and Tuncer 2003. 2. We excluded the following studies: Gorodetskyi 2007, Mannion 2005, Marhofer 1998, Mutty 2007, Schiferer 2007, Turker 2003 and Piangatelli 2004. We made no changes to the conclusions of the review |
| 6 November 2008 | Amended | We converted the review to new review format |
| 21 November 2001 | New citation required and conclusions have changed | In this substantive update (Issue 1, 2002), we included one newly identified study (Scheinin 2000). We made no changes to the conclusions of the review For details on all updates, please see 'Notes' |
Notes
For the first update (Issue 1, 2001), we made the following changes.
Included study of Chudinov 1999 on psoas compartment blocks.
Changed methods score to include item 8.
Changed statistical analysis to relative risks.
Added a synopsis.
In the second update (Parker 2002), we excluded one newly identified study (Van Leeuwen 2000), and we included another (Scheinin 2000a). We have not made changes to the conclusions of the review.
We also updated this review in 2009. At that time, Cochrane updates did not earn a new citation unless they included new review authors or made a change to review conclusions.
For the 2016 update, we made the following changes.
Transferred this review to the Anaesthesia, Critical and Emergency Care Group from the Bone, Joint and Muscle Group.
Included two new review authors.
Updated the search in August 2016.
Updated the review and brought the methods up‐to‐date.
Excluded from the review studies evaluating neuraxial blocks (epidural/spinal) and wound infiltration as techniques of regional blockade.
For the 2020 update, we made the following changes.
Updated the search in November 2019.
Updated the review and brought the methods up‐to‐date.
Risk of bias
Risk of bias for analysis 1.1 Pain on movement within 30 minutes of block placement.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 1.1.1 Fascia iliaca compartment block | ||||||||||||
| Albrecht 2014 | Low risk of bias | Randomly allocated according to a computer‐generated list of random numbers and allocation concealed in sealed opaque envelopes. Intervention group had lower pain score at baseline. This difference was judged as compatible with what could be expected from chance alone in a study with a sample size. | Low risk of bias | No deviations from intended interventions identified | Low risk of bias | 100% of included participants were analyzed | Low risk of bias | Pain scores collected by a nurse blinded to the intervention group | High risk of bias | Study authors elected to deviate from the planned statistical analysis after knowing the results. | High risk of bias | This trial was judged as at high risk of bias for this outcome due to the fact that study authors elected to deviate from the planned statistical analysis after knowing the results. |
| Diakomi 2014 | Low risk of bias | Patients were randomly assigned, using a sealed envelope method and there was no baseline differences between intervention groups. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 98% of included participants were analysed | Low risk of bias | Pain scores collected by an anaesthesiologist blinded to the intervention group. | Low risk of bias | No deviation to the planned statistical analysis reported. Only one result provided for the time point selected by review authors. |
Low risk of bias | No risk of bias identified |
| Domac 2015 | Low risk of bias | Patients included in the study were divided into two equal groups for this prospective double‐blind study. No difference between intervention groups at baseline identified. | Low risk of bias | No deviations from intended interventions identified | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Pain scores probably collected by an assessor blinded to the intervention group. | Low risk of bias | No deviation to the statistical analysis reported. Only one result provided for the time point selected by review authors. | Low risk of bias | No risk of bias identified |
| Foss 2005a | Low risk of bias | The randomization was done via a computer‐generated list. Pain at rest before intervention was higher in the intervention group (P = 0.04). The imbalance can be compatible with the one expected due to chance alone in a study with a small sample size. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | One patient did not have a fracture but only a severe contusion and was excluded after x‐ray; an extra patient was therefore included on a new number. 98% of included participants were analyzed |
Low risk of bias | Pain scores collected by an assessor blinded to the intervention group. | Low risk of bias | No deviation from the plan analysis identified. Only one result provided for the time point selected by review authors. | Low risk of bias | No risk of bias identified |
| Hogg 2009 | Low risk of bias | Prospective, randomised controlled trial and no baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 98% of included participants were analysed. | Low risk of bias | Pain scores. Although this is a subjective score, the fact that a correlation between the effect size and the local anaesthetic drug concentration was found in the review (meta‐regression P value = 0.0003) seems to indicate that scores were valid indicators of pain on movement. | Low risk of bias | No deviation to the statistical analysis reported. Only one result provided for the time point selected by review authors. | Low risk of bias | No risk of bias identified |
| Landsting 2008 | Low risk of bias | Randomization was carried out using a computer, and information about the study intervention was sealed in envelopes. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | High risk of bias | Only 56% of included participants had data available for the time point selected by review authors. We were unable to determine if missingness was related to the outcome or not. We therefore deemed it prudent to judge this trial at high risk of bias for this domain for this outcome. | Low risk of bias | Pain scores derived from a combination of self‐rating scales collected by a blinded assessor. | Low risk of bias | No deviation to the statistical analysis reported. Only one result provided for the time point selected by review authors. | High risk of bias | Judged as at high risk of bias for this outcome due to high number of missing data at the time point selected by review authors and uncertainty as to whether or not missingness could be related to this outcome. |
| Yun 2009 | Low risk of bias | Randomly assigned using an allocation sequence generated by a computer, and allocation sequence concealed in envelopes until group was assigned. No baseline differences between intervention groups identified. | Low risk of bias | No deviations form intended interventions identified. | Low risk of bias | 100% of included participants analyzed. | Low risk of bias | Pain scores collected by an assessor probably blinded to te intervention group. | Low risk of bias | No deviations from the planned statistical analysis identified and only one result provided for the time point selected by the review authors. | Low risk of bias | No risk of bias identified |
| Subgroup 1.1.2 Femoral nerve block | ||||||||||||
| Gille 2006 | Low risk of bias | Randomization in two groups by the anaesthesiologist. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Pain scores. This is a subjective score but the fact that a correlation between the effect size and the local anaesthetic drug concentration was found by the review authors (meta‐regression P value = 0.0003) seems to indicate that scores were valid indicators of pain on movement. | Low risk of bias | No deviation to the planned statistical analysis reported, only one results provided for the time point selected by review authors. | Low risk of bias | No risk of bias identified |
| Murgue 2006 | Low risk of bias | Randomized by “tirage au sort (translated as "hat drawing) ” and no baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 94% of included participants were analyzed. | Low risk of bias | Pain scores. This is a subjective score but the fact that a correlation between the effect size and the local anaesthetic drug concentration was found by the review authors (meta‐regression P value = 0.0003) seems to indicate that scores were valid indicators of pain on movement. | Low risk of bias | No deviation to the planned statistical analysis reported. Only one result provided for the time point selected by review authors. | Low risk of bias | No risk of bias identified |
| Ranjit 2016 | Low risk of bias | Selected patients were randomized by sealed envelope technique and no baseline differences between intervention groups were identified. | Low risk of bias | No deviations from the intended interventions were identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Pain scores. This is a subjective score but the fact that a correlation between the effect size and the local anaesthetic drug concentration was found by the review authors (meta‐regression P value = 0.0003) seems to indicate that scores were valid indicators of pain on movement. | Low risk of bias | No deviation to the planned statistical analysis reported. Only one result provided for the time point selected by review authors. | Low risk of bias | No risk of bias identified |
| Szucs 2010 | Low risk of bias | Randomized using a random number sequence and sealed envelopes. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 89% of included participants were analyzed. | Low risk of bias | Pain scores. This is a subjective score but the fact that a correlation between the effect size and the local anaesthetic drug concentration was found by the review authors (meta‐regression P value = 0.0003) seems to indicate that scores were valid indicators of pain on movement. | Low risk of bias | No deviations from the planned statistical analysis identified and only one result provided for the time point selected by the review authors. | Low risk of bias | No risk of bias identified |
Risk of bias for analysis 1.2 Acute confusional state.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 1.2.1 Peripheral nerve block based on landmarks | ||||||||||||
| Godoy Monzon 2010 | Low risk of bias | Randomized using numbers generated by a computer. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | High risk of bias | 88% of included participants analyzed: 92 for the intervention group and 62 for the comparator group. We were uncertain if missingness was related to the outcome or not. Therefore, we deemed it prudent to judge this trial at high risk of bias for this domain for this outcome. | Low risk of bias | Delirium. To be qualified as delirious, a patient has to show clear symptoms of disorientation. It seems to us that knowledge of the intervention group was not likely to influence the fact that a patient was diagnosed as delirious or not. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | High risk of bias | Judged as at high risk of bias for this outcome due to high number of missing data and inability to determine whether or not missingness was related to this outcome |
| Mouzopoulos 2009 | Low risk of bias | Computer‐generated randomization code. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 95% of included participants were analyzed. | Low risk of bias | Diagnosis of the syndrome was defined using the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM‐IV) and Confusion Assessment Method (CAM) criteria [1, 21]. The method chosen to evaluate the outcome makes it unlikely to be influenced by possible knowledge of assignment. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Nie 2015 | Low risk of bias | Randomly assigned according to a computer‐generated random number table. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 98% of included participants were analyzed. | Low risk of bias | The Confusion Assessment Method was used to diagnose delirium pre‐ and postsurgery. The method chosen to evaluate the outcome makes it unlikely to be influenced by possible knowledge of assignment. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| White 1980 | Low risk of bias | Patients were randomly allocated. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | Participants with failed block were excluded: 4/20 no other exclusion. So, 90 % of included participants analyzed. | Low risk of bias | Confusion. To be qualified as confused, a patient has to show clear symptoms of disorientation. It seems to us that knowledge of the intervention group was not likely to influence the fact that a patient was diagnosed as confused or not. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Subgroup 1.2.2 Peripheral nerve block based on nerve stimulator | ||||||||||||
| Cuvillon 2007 | Low risk of bias | Randomized using sealed numbered envelopes. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Results are given for sedation and/or confusion. To be qualified as confused, a patient has to show clear symptoms of disorientation. It seems to us that knowledge of the intervention group was not likely to influence the fact that a patient was diagnosed as confused or not. Participants in comparator groups received less morphine than the block group, we therefore have no reason to believe that the highest number of participants with sedation and or confusion in the comparator group were assessed as positive for this outcome because they were excessively sedated from morphine. Also, results of this trial are consistent with results of the other trials included in the analysis. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Graham 2008 | Low risk of bias | Randomized by numbered, sequential, sealed opaque envelopes. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 85% of included participants were analyzed. | Low risk of bias | Confusion. To be qualified as confused, a patient has to show clear symptoms of confusion. It seems to us that knowledge of the intervention group was not likely to influence the fact that a patient was diagnosed as confused or not. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Kullenberg 2004 | Low risk of bias | Randomized using the envelope method. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | An experienced nurse evaluated patients' mental status with the Short Portable Mental Status Questionnaire, Pfeiffer‐test, graded according to a 4‐degree scale. The method chosen to evaluate the outcome makes it unlikely to be influenced by possible knowledge of assignment. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Subgroup 1.2.3 Peripheral nerve blocks inserted on ultrasound guidance | ||||||||||||
| Brownbridge 2018 | Low risk of bias | Patients were randomized. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | CAM‐ICU scoring system will be used daily to measure delirium. The method chosen to evaluate the outcome makes it unlikely to be influenced by possible knowledge of assignment. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Liebmann 2012 | Low risk of bias | Randomization occurred using an Internet‐based program. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 95% of included participants were analyzed. | Low risk of bias | Confusion. To be qualified as confused, a patient has to show clear symptoms of disorientation. It seems to us that knowledge of the intervention group was not likely to influence the fact that a patient was diagnosed as confused or not. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Morrison 2008 | Low risk of bias | Randomized using a computer‐generated, stratified, blocked randomization list, with stratification according to site and allocation concealed in sealed envelopes. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 95% of included participants were analyzed. | Low risk of bias | Confusion Assessment Method supplemented by chart review evaluated by an assessor blinded to the treatment group. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Uysal 2018 | Low risk of bias | A randomized controlled trial. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 83% of included participants were analyzed. | Low risk of bias | The delirium status of patients was assessed using “Delirium Rating Scale‐R‐98 (DRS‐R‐98)” in the postoperative period for three days. The method chosen to evaluate the outcome makes it unlikely to be influenced by possible knowledge of assignment. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Yamamoto 2016 | Low risk of bias | Randomisation was performed with a random number list generated by a computer software. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Delirium occurring within 24 h after surgery was diagnosed by the confusion assessment method. The method chosen to evaluate the outcome makes it unlikely to be influenced by possible knowledge of assignment. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Yang 2016 | Low risk of bias | Randomized. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Delirium. To be qualified as delirious, a patient has to show clear symptoms of disorientation. It seems to us that knowledge of the intervention group was not likely to influence the fact that a patient was diagnosed as delirious or not. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
Risk of bias for analysis 1.3 Myocardial infarction.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Altermatt 2013 | Low risk of bias | Randomized using a computer generated random number table. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Serial EKGs and troponin concentration measurements were performed daily until postoperative day 3 or more frequently if an ischemic episode was suspected. Analysis of ST segments were evaluated a posteriori by a cardiologist blinded the allocated group. | Low risk of bias | No deviation to the statistical analysis reported. No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
Risk of bias for analysis 1.4 Chest infections.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Fletcher 2003 | Low risk of bias | The randomization sequence was derived from a random number generator, and allocation concealment was achieved by means of the sealed opaque envelope method. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Lower respiratory tract infections determined by a blinded assessor. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Haddad 1995 | Low risk of bias | Randomized by sealed envelope. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 90% of included participants were analyzed. | Low risk of bias | Chest infections which required antibiotics. We judged it as unlikely to have been influenced by knowledge of the treatment group. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| White 1980 | Low risk of bias | Patients were randomly allocated. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 80% of included participants were analyzed. | Low risk of bias | Pneumonia. We judged it as unlikely to have been influenced by knowledge of the treatment group. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
Risk of bias for analysis 1.5 Mortality.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 1.5.1 Single‐injection block | ||||||||||||
| Albrecht 2014 | Low risk of bias | Randomly allocated according to a computer‐generated list of random numbers and allocation concealed in sealed opaque envelopes. Intervention group had lower pain score at baseline. This difference was judged as compatible with what could be expected from chance alone in a study with a sample size. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Death from all causes | High risk of bias | This outcome was not part of the outcomes when the trial was registered. There was no other planned measurement at 3 months. | High risk of bias | Judged as at high risk of bias for this outcome due to possibility that this outcome was not pre‐determined for the specific time point at which it was measured |
| Fletcher 2003 | Low risk of bias | The randomization sequence was derived from a random number generator, and allocation concealment was achieved by means of the sealed opaque envelope method. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Haddad 1995 | Low risk of bias | Randomized by sealed envelope. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Hood 1991 | Low risk of bias | Randomly allocated by choosing an unmarked envelope. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Jones 1985 | Low risk of bias | Prospective controlled randomised trial, an envelope was opened after surgery completion. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| White 1980 | Low risk of bias | Patients were randomly allocated. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | Participants with failed block were excluded: 4/20 no other exclusion. So, 90 % of included participants analyzed. | Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Subgroup 1.5.2 Continuous infusion | ||||||||||||
| Brownbridge 2018 | Low risk of bias | Patients were randomized. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Cuvillon 2007 | Low risk of bias | Randomized using sealed numbered envelopes. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| De La Tabla 2010 | High risk of bias | Prospective, randomized study. 49 patients were included: 38 in group 1 (77,6%) and 11 in group 2 (22,4%). | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed | Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | High risk of bias | Judged as at high risk of bias due to a possible problem with randomization leading to two very unequal number of participants per group. |
| Morrison 2008 | Low risk of bias | Randomized using a computer‐generated, stratified, blocked randomization list, with stratification according to site and allocation concealed in sealed envelopes. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 95% of included participants were analyzed. Missingness not related to outcome. |
Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Wang 2015 | Low risk of bias | Randomly assigned using a computer‑generated random number table method with randomized group information sealed in an opaque envelope. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Deaths from all causes. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
Risk of bias for analysis 1.6 Time to first mobilization.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Kullenberg 2004 | Low risk of bias | Randomized using the envelope method. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Time to first support of body weight next to the bed in hours after surgery. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Segado Jimenez 2009 | Low risk of bias | Patients were randomized. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Time to sit down for the first time. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
| Yamamoto 2016 | Low risk of bias | Randomisation was performed with a random number list generated by a computer software. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Time to first standing. | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
Risk of bias for analysis 1.7 Costs of analgesic drugs.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Segado Jimenez 2009 | Low risk of bias | Patients were randomized. No baseline differences between intervention groups identified. | Low risk of bias | No deviations from intended interventions identified. | Low risk of bias | 100% of included participants were analyzed. | Low risk of bias | Drugs expenses (not including indirect costs or stay). | Low risk of bias | No deviation to the planned statistical analysis identified. Only one result provided. | Low risk of bias | No risk of bias identified. |
Acknowledgements
The review authors thank Janne Vendt, who designed the search strategy for this update, as well as University of Sherbrooke, University Laval, and University of Quebec in Abitibi‐Temiscamingue, for granting access to electronic databases and to medical journals.
We would like to thank Lars Lundstrøm (Content Editor), Jing Xie (Statistical Editor), Pekka Tarkkila and Fernanda Fukushima (Peer Reviewers), Gabriel Kwok (Consumer Reviewer), Liz Bickerdike (Network Associate Editor), Janne Vendt (Information Specialist), Teo Quay (Managing Editor), and Andrew Smith (Co‐ordinating Editor) for their help and editorial advice during the preparation of this systematic review. We would also like to thank the Cochrane Editorial and Methods Department's 'Methods Support Unit' for their advice and support related to implementation of Risk of bias‐2 as part of the pilot programme.
We thank Eric Albrecht (Albrecht 2014), Fernando Altermatt (Altermatt 2013), Raquel Ortiz de la Tabla González (De La Tabla 2010), Jochen Gille (Gille 2006), Nicolai B Foss (Foss 2005a), K. Sanem Cakar Turhan (Gürtan Bölükbasi 2013), Daniel Godoy Monzon (Godoy Monzon 2010), Ashok Jadon (Jadon 2014), Francesca L Beaudoin (Liebmann 2012), Pär Wennberg (Landsting 2008), Hongling Nie (Nie 2015), Harry Scheinin (Scheinin 2000), Szilard Szucs (Szucs 2010), and M Yung (Yun 2009), who provided additional information for the 2017 and 2020 updates; Karl Sales for translation of two articles (Segado Jimenez 2009; Segado Jimenez 2010); Gideon Heinert for translation of Gille 2006; and Jia Jiang for translation of Ma 2018a.
We also thank Martyn Parker and Richard Griffiths, co‐authors of previous versions, who read this version during the revision process.
Appendices
Appendix 1. Search strategies
MEDLINE ALL (Ovid) 1946 to 15 November 2019
1 exp Femoral Fractures/
2 exp Hip Fractures/
3 ((hip* or fem?r* or trochant* or pertrochant* or intertrochant* or subtrochant* or intracapsular* or extracapsular*) adj5 fracture*).mp.
4 1 or 2 or 3
5 exp Anesthesia/
6 exp nerve block/
7 ((an?est* or analg*) adj5 (regional* or local* or block* or nerv*)).mp.
8 (((nerv* or plexus or femoral or femur* or psoas or compartment or regional) adj3 block*) or lumbar plexus or fascia iliac*).mp.
9 5 or 6 or 7 or 8
10 ((randomized controlled trial or controlled clinical trial).pt. or random*.ab. or placebo.ab. or drug therapy.fs. or trial.ab. or groups.ab.) not (animals not (humans and animals)).sh.
11 Meta‐analysis.pt. or exp Meta‐analysis/ or exp Meta‐analysis as topic/ or (meta analy* or metaanaly*).tw. or ((review* or search*) adj10 (literature* or medical database* or medline or pubmed or embase or cochrane or cinahl or biosis or current content* or systemat*)).tw.
12 10 or 11
13 4 and 9 and 12
Embase (Ovid) 1974 to 2019 November 13
1 exp femur fracture/
2 exp hip fracture/
3 ((hip* or fem?r* or trochant* or pertrochant* or intertrochant* or subtrochant* or intracapsular* or extracapsular*) adj5 fracture*).mp.
4 1 or 2 or 3
5 exp regional anesthesia/
6 exp nerve block/
7 ((an?est* or analg*) adj5 (regional* or local* or block* or nerv*)).mp.
8 (((nerv* or plexus or femoral or femur* or psoas or compartment or regional) adj3 block*) or lumbar plexus or fascia iliac*).mp.
9 5 or 6 or 7 or 8
10 (randomized controlled trial/ or crossover procedure/ or double blind procedure/ or single blind procedure/ or controlled clinical trial/ or ((single or double or triple or treble or doubly or singly) adj2 (blind* or mask*)).ti,ab. or (controlled adj5 (study or design or trial)).ti,ab. or (parallel group* or open label).ti,ab. or (allocat* or assign* or crossover* or cross over* or multicenter* or multi center* or placebo* or random* or factorial or volunteer* or (trial or groups)).tw.) not ((exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti,ab.))
11 4 and 9 and 10
CENTRAL (Cochrane Library)
#1 MeSH descriptor: [Hip Fractures] explode all trees #2 MeSH descriptor: [Femoral Fractures] explode all trees #3 (hip* or femor* or femur* or trochant* or pertrochant* or intertrochant* or subtrochant* or intracapsular* or extracapsular*) NEAR fracture* #4 #1 OR #2 OR #3 #5 MeSH descriptor: [Anesthesia] explode all trees #6 MeSH descriptor: [Nerve Block] explode all trees #7 ((anesth* or anaesth* or analg*) NEAR (regional* or local* or block* or nerv*)) #8 ((nerv* or plexus or femoral or femur* or psoas or compartment or regional) NEAR block*) or lumbar plexus or fascia iliac* #9 #5 or #6 or #7 or #8 #10 #4 and #9 #11 #10 in Trials
CINAHL (Ebsco)
| S1 | (MH "Femoral Fractures+") | |
| S2 | (MH "Hip Fractures+") | |
| S3 | TX ((hip* or femur* or femoral* or trochant* or pertrochant* or intertrochant* or subtrochant* or intracapsular* or extracapsular*) N5 fracture*) | |
| S4 | S1 OR S2 OR S3 | |
| S5 | (MH "Anesthesia+") | |
| S6 | (MH "Nerve Block+") | |
| S7 | TX ((anesth* or anaesth* or analg*) N5 (regional* or local* or block* or nerv*)) | |
| S8 | TX (((nerv* or plexus or femoral or femur* or psoas or compartment or regional) N3 block*) or lumbar plexus or fascia iliac*) | |
| S9 | S5 OR S6 OR S7 OR S8 | |
| S10 | S4 AND S9 | |
| S11 | ((MH "Randomized Controlled Trials") OR (MH "Clinical Trials+") OR (MH "Random Assignment") OR (MH "Prospective Studies+") OR (MH "Clinical Trial Registry") OR (MH "Double‐Blind Studies") OR (MH "Single‐Blind Studies") OR (MH "Triple‐Blind Studies") OR (MH "Multicenter Studies") OR (MH "Placebos") OR (PT Clinical trial) OR (MH "Quantitative Studies")) OR TX (random* or placebo* or trial* OR cross over OR crossover) OR TX ((singl* OR doubl* OR trebl* OR tripl*) N3 (blind* OR mask*)) OR TX (clinic* N1 trial*) | |
| S12 | S10 AND S11 |
Appendix 2. Risk of bias assessment
Supplement toMethods.
For bias due to the randomization process, we evaluated allocation sequence generation, allocation sequence concealment, and baseline imbalances suggesting a problem in the randomization process.
For bias due to deviations from intended interventions, we evaluated the effect of assignment to intervention. To assess the effect of assignment to intervention, we evaluated if participants were aware of their assigned intervention during the trial, if carers and people delivering the interventions were aware of participants' assigned intervention during the trial, if there were deviations from the intended intervention that arose because of the trial context, if these deviations were likely to have affected the outcome, if these deviations from the intended intervention were balanced between groups, if an appropriate analysis was used to estimate the effect of assignment to the intervention, and if there was potential for a substantial impact (on the result) of the failure to analyse participants in the groups to which they were randomized.
For bias due to missing outcome data, we evaluated if data for this outcome were available for all, or nearly all, participants randomized, if there was evidence that the result was not biased by missing outcome data, if missingness in the outcome could depend on its true value, and if it was likely that missingness in the outcome depended on its true value.
For bias due to measurement of the outcome, we evaluated if the method of measuring the outcome was inappropriate, if measurement or ascertainment of the outcome could have differed between intervention groups, if outcome assessors were aware of the intervention received by study participants, if assessment of the outcome could have been influenced by knowledge of intervention received, and if it was likely that assessment of the outcome was influenced by knowledge of intervention received.
For bias due to selection of the reported result, we evaluated if the data that produced this result were analysed in accordance with a pre‐specified analysis plan that was finalized before unblinded outcome data were available for analysis, and if the numerical result being assessed was likely to have been selected from multiple eligible outcome measurements or multiple eligible analyses of the data.
Appendix 3. Diagnostic criteria for acute confusional state
| Study ID | Diagnostic criteria |
| Brownbridge 2018 | CAM‐ICU scoring system will be used daily to measure delirium (time frame: during hospital stay up to 1 month) |
| Cuvillon 2007 | Clinical evaluation "somnolence‐confusion" and Mini Mental Test |
| Godoy Monzon 2010 | "episodes of delirium" |
| Graham 2008 | "acute confusional state" |
| Kullenberg 2004 | Pfeiffer test, graded according to a 4‐degree scale (0 to 3: no, light, moderate, and pronounced confusion) |
| Liebmann 2012 | "agitation or confusion" |
| Morrison 2008 | Confusion Assessment Method daily supplemented by chart review |
| Mouzopoulos 2009 | Perioperative delirium: syndrome defined using the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM‐IV), and Confusion Assessment Method (CAM) criteria "Daily patient assessments using the MMSE, DRS‐R‐ 98, and Digit Span test [assessment of attention, range 0 (no attention) to 42 (good attention)] were used to enable the DSM‐IV and CAM diagnoses and assess delirium severity"; "CAM and DRS‐R‐98 assessments were continued once delirium was diagnosed" |
| Nie 2015 | "The Confusion Assessment Method was used to diagnose delirium pre‐ and postsurgery" |
| Uysal 2018 | "Delirium Rating Scale‐R‐98 (DRS‐R‐98)" |
| White 1980 | "confusion" |
| Yamamoto 2016 | "Delirium occurring within 24 hour after surgery was diagnosed by the Confusion Assessment Method" |
| Yang 2016 | "delirium" |
Appendix 4. Diagnostic criteria for myocardial infarction
| Study ID | Diagnostic criteria |
| Altermatt 2013 | Serial electrocardiograms and troponin concentration measurements were performed daily until postoperative day 3, or more frequently if an ischaemic episode was suspected |
Appendix 5. Diagnostic criteria for chest infection
| Study ID | Diagnostic criteria |
| Fletcher 2003 | "lower respiratory tract infections" |
| Haddad 1995 | “chest infections which required antibiotics” |
| White 1980 | "pneumonia" |
Appendix 6. Results from other recent reviews on the topic published in English
| Review | Pain | Acute confusional state | Myocardial infarction | Chest infections | Death | Time to first mobilization | Cost of analgesic regimen | Remarks |
| Amin 2017 | FICB is safe and effective in controlling perioperative pain | N/A | N/A | N/A | N/A | N/A | N/A | NR 25 trials |
| Dizdarevic 2019 | Utilize various strategies to reduce pain including RA | N/A | N/A | N/A | N/A | N/A | N/A | NR |
| Fadhlillah 2019 | FICB reduces acute pain on movement Variable results for pain at rest |
N/A | N/A | N/A | N/A | N/A | N/A | MA 8 RCTs |
| Freeman 2016 | FICB is part of recommended practices | Use multi‐modal analgesia to reduce the incidence of delirium | N/A | N/A | N/A | N/A | N/A | NR |
| Hards 2018 | FICB is suitable for pre‐hospital use and has few adverse effects Comparisons with systemic opioids are required |
N/A | N/A | N/A | N/A | N/A | N/A | SR
7 studies:
|
| Hartmann 2017 | FNB seemed to be more effective than IV fentanyl | N/A | N/A | N/A | N/A | N/A | N/A | SR 2 RCTs |
| Hong 2019 | FICB reduced pain at 1 to 8, 12, 24, and 48 hours No difference at 72 hours |
N/A | N/A | N/A | N/A | N/A | N/A | MA 11 RCTs |
| Hsu 2018 | Limited evidence for reduced pain on movement at 30 minutes and at 6 hours after surgery with FICB No significant complications |
N/A | N/A | N/A | N/A | N/A | N/A | MA 3 RCTs |
| Hsu 2019 | FNB achieved lower pain scores on movement at 30 minutes than IV analgesia | N/A | N/A | N/A | N/A | N/A | N/A | MA
10 studies
|
| Parker 2016 | N/A | N/A | N/A | N/A | Nerve blocks may reduce mortality or morbidity Continuing research is required |
N/A | N/A | NR |
| Rashiq 2013 | ONB plus LFCNB had the highest probability of being effective against acute postoperative pain More trials comparing multiple nerve blocks in hip fractures are required |
FICB had the highest probability of being the most effective | N/A | N/A | N/A | N/A | N/A | SR 21 RCTs |
| Scurrah 2018 | Consistent evidence that PNBs reduce pain and are more effective than standard systemic analgesia alone | Moderate evidence for a reduction | N/A | N/A | Limited evidence for a reduction | N/A | N/A | NR |
| Skjold 2019 | Limited quantity of evidence for decreased pain scores leading to very low certainty of evidence supporting preoperative single‐injection FNBs | N/A | N/A | N/A | N/A | N/A | N/A | SR with MA 5 RCTs |
| Soffin 2019 | PNBs and non‐opioid multi‐modal analgesic agents are suggested preoperatively | N/A | N/A | N/A | N/A | N/A | N/A | ER |
| Steenberg 2018 |
FICB superior to opioids during movement Very few adverse effects |
Insufficient evidence | N/A | N/A | Insufficient evidence | N/A | N/A | SR
11 studies
|
| CR: Case report; ER: evidence review; FICB: fascia iliaca compartment block; FNB: femoral nerve block; LFCNB: lateral femoral cutaneous nerve block; IV: intravenous; N/A: not a purpose of the review; MA: meta‐analysis; NR: narrative review; ONB: obturator nerve block; P: prospective non‐randomized trial; PNB: peripheral nerve block: qRCT: quasi‐randomized controlled trial; RA: regional anaesthesia; RCT: randomized controlled trial; R: retrospective trial; SR: systematic review. | ||||||||
Data and analyses
Comparison 1. Peripheral nerve blocks (PNBs) versus no nerve block (or sham block).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Pain on movement within 30 minutes of block placement | 11 | 503 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.05 [‐1.25, ‐0.86] |
| 1.1.1 Fascia iliaca compartment block | 7 | 309 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.17 [‐1.42, ‐0.92] |
| 1.1.2 Femoral nerve block | 4 | 194 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.89 [‐1.19, ‐0.60] |
| 1.2 Acute confusional state | 13 | 1072 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.50, 0.90] |
| 1.2.1 Peripheral nerve block based on landmarks | 4 | 501 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.44, 1.13] |
| 1.2.2 Peripheral nerve block based on nerve stimulator | 3 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.31, 0.97] |
| 1.2.3 Peripheral nerve blocks inserted on ultrasound guidance | 6 | 389 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.44, 1.20] |
| 1.3 Myocardial infarction | 1 | 31 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.4 Chest infections | 3 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.19, 0.89] |
| 1.5 Mortality | 11 | 617 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.47, 1.60] |
| 1.5.1 Single‐injection block | 6 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.44, 2.24] |
| 1.5.2 Continuous infusion | 5 | 382 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.30, 1.89] |
| 1.6 Time to first mobilization | 3 | 208 | Mean Difference (IV, Fixed, 95% CI) | ‐10.80 [‐12.83, ‐8.77] |
| 1.7 Costs of analgesic drugs | 1 | 75 | Mean Difference (IV, Fixed, 95% CI) | ‐4.40 [‐4.84, ‐3.96] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Albrecht 2014.
| Study characteristics | ||
| Methods | Parallel RCT
Approved by the ethics committee and informed consents obtained
Site: Lausanne University Hospital, Switzerland Data collection: between 7 November 2014 and 2 June 2016 Funding: departmental/institutional Registration: NCT02433548 |
|
| Participants | 30 participants with a hip fracture Excluded: patients with bleeding disorder or presence of anticoagulation, periprosthetic fracture, a known polyneuropathy, body weight < 40 kg, chronic pain condition, patients undergoing chemotherapy, infection at the site of injection, allergy to local anaesthetics, cognitive disorder Type of fracture: hip fracture Anaesthetic technique for surgery: not mentioned Surgical technique: not mentioned Mean age: 80.5 years (range 73 to 90) Percentage female: 70% Length of follow‐up: 3 months |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 15) Comparator: sham block (N = 15) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no conflicts of interest from any study authors related to this work DOI: 10.1186/s12877‐019‐1193‐0 Email sent on 5 January 2020: additional information received from study authors Sources obtained for risk of bias assessment.
|
|
Altermatt 2013.
| Study characteristics | ||
| Methods | RCT Approved by the ethics committee and informed consents obtained Site: Pontificia Universidade Católica de Chile Data collection: 2 years; exact dates unspecified Funding: governmental Registration: retrospectively registered; NCT01961895 |
|
| Participants | 31 ASA II to III participants older than 60 years, with risk factors for known coronary artery disease (≥ 2 risk factors for coronary heart disease as defined by Wallace 1987) and hip fracture, admitted within 48 hours of fracture Excluded: patients with ≥ 2 independent predictors of perioperative cardiac adverse events (age ≥ 68, body mass index ≥ 30 kg/m2, active congestive heart failure, previous cardiac intervention, cerebrovascular disease or hypertension); receiving orthopaedic treatment; with evidence of abnormal cognitive function, dementia, or delirium; with non‐sinusal heart rhythm or conduction abnormalities (complete left or right bundle branch blocks, or atrioventricular block); no electrocardiogram at admission; patients with a pacemaker, coagulopathy, contraindication to anaesthesia or regional analgesia, severe liver or renal failure (creatinine > 2.0 mg.dL‐1), or known allergy to a drug used in the study Type of fracture: hip fracture Anaesthetic technique for surgery: spinal block Surgical technique: not mentioned Mean age: 81 years (range not mentioned) Percentage female: 77% Length of follow‐up: in‐hospital (mean 7.6 days and 8.2 days) |
|
| Interventions |
Intervention: continuous psoas compartment block (N = 17) Comparator: no nerve block (N = 14) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
Ischaemic events per participant (extracted as P value): continuous EKG monitoring and serial cardiac enzymes |
|
| Notes | Conflict of interest: "authors declare having no conflict of interest" DOI: 10.1016/j.bjan.2018.03.003 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Antonopoulou 2006.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained: not mentioned Site: General Hospital of Xanthi, Greece Data collection: no information Funding: no information Registration: no information |
|
| Participants | 84 participants with hip fracture (48 intracapsular fractures, 36 extracapsular fractures) Excluded: no information Type of fracture: 48 patients had an intracapsular fracture; 36 patients had an extracapsular fracture Anaesthetic technique for surgery: spinal block Surgical technique: not mentioned Mean age: 76 years (range 68 to 95) Percentage female: 75% Lost to follow‐up: no information Length of follow‐up: in‐hospital |
|
| Interventions |
Intervention: continuous femoral nerve block (N = 49) Comparator: no nerve block (N = 35) Spinal anaesthesia and paracetamol after surgery for all participants |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: no information Conference abstract Email sent on 25 May 2015: no reply |
|
Bang 2016.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: The Catholic University of Korea, Seoul, Korea Data collection: 2015 to 2016 Funding: departmental/institutional Registration: KCT0001450 |
|
| Participants | 22 participants aged 70 to 90 years who underwent bipolar hemiarthroplasty for femoral neck fracture Excluded: clinically significant coagulopathy, infection at the injection site, allergy to local anaesthetics, severe cardiopulmonary disease (≥ ASA IV), body mass index > 35 kg/m2, diabetic or other neuropathies, receiving opioids for long‐term analgesic therapy, contraindication to spinal anaesthesia, inability to comprehend verbal/visual analogue pain scale, patient‐controlled analgesia device Type of fracture: femoral neck fracture Anaesthetic technique for surgery: spinal block Surgical technique: bipolar hemiarthroplasty Mean age: 81.8 years (range not mentioned) Percentage female: 67% Length of follow‐up: 1 week |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 11) Comparator: no nerve block (N = 11) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: none DOI: 10.1097/MD.0000000000005018 Email sent on 5 January 2020 |
|
Brownbridge 2018.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: University Hospital, Saskatoon, Canada Data collection: May 2018 to March 2019 Funding: departmental/institutional Registration: NCT03588689 |
|
| Participants | 30 participants ≥ 65 years of age admitted for hip fracture Excluded: ASA score ≥ 4, open fracture; concomitant injury that might interfere with positioning; local anaesthetic allergy; delirium or cognitive impairment preventing consent; infection or previous surgery at the femoral triangle; using warfarin, anti‐Xa inhibitors, or long‐term opioids Type of fracture: hip fracture Anaesthetic technique for surgery: spinal block or general anaesthesia Surgical technique: not mentioned Mean age: not mentioned (range ≥ 65 years old) Percentage female: no information Length of follow‐up: 1 month |
|
| Interventions |
Intervention: continuous fascia iliaca block (N = 15) Comparator: no nerve block (N = 15) |
|
| Outcomes | Relevant to this review.
Not relevant to this review:
|
|
| Notes | Conflict of interest: "none declared" DOI: 10.1007/s12630‐019‐01428‐2 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Chudinov 1999.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee Site: Sheba Medical Center, Ramat Gan, Israel Data collection: not mentioned Funding: no information Registration: no information |
|
| Participants | 40 participants (30 female and 10 male) with hip fracture undergoing surgery Excluded: severe cardiac, pulmonary, renal, or liver dysfunction; systemic infection; decubitus ulcer; dementia; aspirin or anticoagulant treatment; allergy to local anaesthetics Type of fracture: hip fracture Anaesthetic technique for surgery: according to assessment, a sciatic nerve block (N = 5), general anaesthesia (N = 1), or spinal anaesthesia (N = 11) was added for participants in the intervention group; neuraxial block (spinal or epidural, N = 19) or general anaesthesia (N = 1) was used for participants in the comparator group Surgical technique: not mentioned Mean age: 80 years (range 67 to 96) Percentage female: 75% Length of follow‐up: 72 hours |
|
| Interventions |
Intervention: continuous psoas compartment block (N = 20) Comparator: no nerve block (N = 20) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: not stated DOI: n/a No email address |
|
Coad 1991.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and consents obtained Site: Derbyshire Royal Infirmary, Nottingham, UK Data collection: not mentioned Funding: no information Registration: no information |
|
| Participants | 50 participants with a hip fracture undergoing surgery with a pin and plate or a sliding hip screw Excluded: receiving analgesic drugs, diagnosis of dementia, regional anaesthesia considered indicated for surgery Type of fracture: hip fracture Anaesthetic technique for surgery: general anaesthesia Surgical technique: pin and plate or compression/screw fixation Mean age: 77 years (range 64 to 89) Percentage female: 84% Length of follow‐up: 24 hours |
|
| Interventions |
Intervention 1: lateral femoral cutaneous nerve block (N = 17) Intervention 2: femoral (3‐in‐1) nerve block (N = 17) Comparator: no nerve block (N = 16) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a No email address |
|
Cuvillon 2007.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and written informed consents obtained Site: Centre Hospitalier Universitaire de Nîmes, France Data collection: September 1999 to June 2002 Funding: charity Registration: no information |
|
| Participants | 62 ASA physical status I to IV, ≥ 70 years of age, with proximal end femur fracture undergoing surgery Excluded: more than 72 hours between fracture and surgery, weight < 40 kg, ASA physical status > IV, neurological disease (alcoholic or diabetic), allergy or contraindication to regional anaesthesia, severe hepatic or renal dysfunction, Mini Mental score < 15/30 Type of fracture: proximal end femur fracture Anaesthetic technique for surgery: spinal block Surgical technique: plate and screw (58%) or intermediate prosthesis (42%) Mean age: 82 years (range not stated) Percentage female: 86%. Length of follow‐up: in‐hospital |
|
| Interventions |
Intervention: continuous femoral nerve block (N = 21) Comparator: no nerve block (N = 41) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: not mentioned DOI: 10.1016/j.annfar.2006.06.025 Study authors contacted 22 May 2015; no reply Sources obtained for risk of bias assessment.
|
|
De La Tabla 2010.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Valme Hospital, Seville, Spain Data collection: no information Funding: no information Registration: no information |
|
| Participants | 49 participants older than 65 years with a neck fracture scheduled for surgical treatment Excluded: not stated Type of fracture: neck fracture Anaesthetic technique for surgery: not stated Surgical technique: not stated Mean age: 81.9 years (range not stated) Percentage female: % not stated Length of follow‐up: 1 month |
|
| Interventions |
Intervention: continuous femoral nerve block (N = 11) Comparator: no nerve block (N = 38) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a Conference abstract Additional information on pain scores received from study authors for the 2017 version Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Deniz 2014.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: military university hospital, Anakara, Turkey Data collection: between June 2009 and May 2010 Funding: departmental/institutional Registration: no information |
|
| Participants | 70 participants who underwent hip prosthesis for hip fracture under general anaesthesia Excluded: spinal or epidural anaesthesia, ASA physical status ≥ IV, weight < 40 kg or > 125 kg, inguinal or femoral hernia, allergy to local anaesthetics, peripheral neuropathy, neurological deficit or abnormal coagulation profile, mental retardation, dementia, insufficient understanding of pain scoring systems, use of patient‐controlled analgesia device Type of fracture: hip fracture Anaesthetic technique for surgery: general anaesthesia Surgical technique: hip prosthesis Mean age: 63 years (range 20 to 80 years) Percentage female: 55% Length of follow‐up: 4 months |
|
| Interventions |
Intervention 1: fascia iliaca compartment block (N = 24) Intervention 2: 3‐in‐1 femoral nerve block (N = 24) Comparator: no nerve block (N = 22) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "none declared" DOI: 10.5505/agri.2014.76993 No email address |
|
Diakomi 2014.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: University of Athens School of Medicine, Greece Data collection: 4‐month period; exact dates not specified Funding: no information Registration: NCT02037633 |
|
| Participants | 41 ASA I to III participants scheduled for hip fracture repair Excluded: contraindications for central nervous blockade, impaired cognition or dementia, multiple fractures, any previous analgesic administration in last 12 hours before surgery Type of fracture: intertrochanteric (60%) or neck (40%) fracture Anaesthetic technique for surgery: spinal block Surgical technique: not stated Mean age: 78 years (range 38 to 94) Percentage female: 78.6% Length of follow‐up: 48 hours |
|
| Interventions |
Intervention: fascia iliaca block (N = 21) Comparator: no nerve block (N = 20) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: 10.1097/AAP.0000000000000133 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Domac 2015.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Samsun, Turkey Data collection: no information Funding: departmental Registration: no information |
|
| Participants | 40 ASA I to III participants undergoing hip fracture repair under spinal anaesthesia Excluded: < 65 years of age or > 80 years of age, peripheral neurological disease, mental disorder, allergy to amide local anaesthetics, coagulation/haemostasis disease, moderate or severe liver or kidney failure, contraindication to or refusing fascia iliaca block Type of fracture: hip fracture Anaesthetic technique for surgery: spinal block Surgical technique: not mentioned Mean age: 70.5 years (range 65 to 80) Percentage female: 62.5% Length of follow‐up: 48 hours |
|
| Interventions |
Intevention: fascia iliaca block (N = 20) Comparator: no nerve block (N = 20) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "authors do not report any conflict of interest" DOI: n/a SDs of 0.00 entered as 0.001 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Fletcher 2003.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Rotherham General Hospital, UK Data collection: 6‐month period from February until August; exact years unspecified Funding: no information Registration: no information |
|
| Participants | 50 participants with a neck of femur fracture Excluded: confused (and therefore unable to give informed consent), bleeding diathesis or taking warfarin, local or systemic infection, previous hypersensitivity to local anaesthetics Type of fracture: intertrochanteric (60%) and subcapital‐transcervical (40%) Anaesthetic technique for surgery: not mentioned Surgical technique: not mentioned Mean age: 78 years (range not stated) Percentage female: 70% Length of follow‐up: 6 months |
|
| Interventions |
Intervention: femoral (3‐in‐1) nerve block (N = 24) Comparator: no nerve block (N = 26) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: 10.1067/mem.2003.51 Extra information supplied by trialists to confirm secure randomization and that no participants were lost to follow‐up Study authors re‐contacted 22 May 2015: no reply Sources obtained for risk of bias assessment.
|
|
Foss 2005a.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and written informed consents obtained Site: Hvidovre University Hospital, Denmark Data collection: May 2003 to January 2006 Funding: charity Registration: NCT00162630 |
|
| Participants | 48 participants with hip fracture Excluded: refusal to participate in the study, previous surgery in the affected hip, regular prefracture opioid or glucocorticoid therapy, alcohol or substance abuse, infection at the injection site, morphine intolerance, any previous opioid administration for acute pain, non‐confirmation of hip fracture suspicion on X‐ray Type of fracture: intracapsular (37.5%), subtrochanteric (48%), trochanteric (14.5%) Anaesthetic technique for surgery: not mentioned Surgical technique: not mentioned Mean age: 80 years (range 69 to 88) Percentage female: 73% Length of follow‐up: in‐hospital |
|
| Interventions |
Intervention: fascia iliaca compartment blockade (N = 24) Comparator: sham block with saline (N = 24) After 3 hours, all participants received epidural analgesia |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a Email sent on 5 January 2020; study authors think that their published report should contain the information that we need; study authors available to answer additional questions Sources obtained for risk of bias assessment.
|
|
Gille 2006.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: St.Georg, Leipzig, Germany Data collection: no information Funding: corresponding study author had no relationship with any mentioned product nor competitors classified as departmental resources Registration: no information |
|
| Participants | 100 participants with an isolated hip fracture Excluded: < 18 years old, uncooperative, with contraindications to regional anaesthesia or drugs used in the protocol, long‐term use of opioids and/or opioid dependence, history of ulcers, multiple trauma, absence of consent, anaesthetists inexperienced (fewer than 5) with the technique Type of fracture: intracapsular (43%), extracapsular (57%) Anaesthetic technique for surgery: spinal (75%) or general anaesthesia (25%) Surgical technique: prosthesis (41%), osteosynthesis (59%) Mean age: 80 years (range 35 to 103) Percentage female: 77% Length of follow‐up: 72 hours |
|
| Interventions |
Intervention: continuous femoral nerve block (N = 50) Comparator: no nerve block (N = 50) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "there is no conflict of interest" DOI: 10.1007/s00101‐005‐0949‐4 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Godoy Monzon 2010.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and signed informed consents obtained Site: Hospital Italiano de Buenos Aires‐Centro Agustín Rocca, San Justo‐La Matanza, Argentina (university hospital) Data collection: June 2006 to January 2008 Funding: departmental/institutional Registration: not registered |
|
| Participants | 175 adult participants > 65 years old who presented to the emergency department because of a previously undiagnosed and untreated hip fracture Excluded: anatomical abnormalities in the inguinal area different from fracture, known coagulation disorder, history of allergy to any of the active ingredients used during the study, refusal to participate Type of fracture: hip fracture Anaesthetic technique for surgery: not mentioned Surgical technique: not mentioned Median age: 75.9 years (range not mentioned) Percentage female: 62.3% Length of follow‐up: 8 hours |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 92) Comparator: sham block with saline (N = 62) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "none" DOI: 10.1007/s12245‐010‐0234‐4 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Graham 2008.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed written consents obtained Site: The Chinese University of Hong Kong, Trauma & Emergency Centre, Prince of Wales Hospital, Shatin, N.T., Hong Kong, China Data collection: April 2000 to October 2001 Funding: no information Registration: no information |
|
| Participants | 40 adult participants (> 16 years of age) with adequate abbreviated mental tests and hip fracture confirmed by X‐ray Excluded: known allergy or contraindication to morphine or bupivacaine, abbreviated mental test score < 9 Type of fracture: hip fracture Anaesthetic technique for surgery: no information Surgical technique: no information Mean age: 79.2 years (range: not stated) Percentage female: 93.5% Length of follow‐up: 24 hours |
|
| Interventions |
Intervention: femoral (3‐in‐1) nerve block (N = 18) Comparator: no nerve block (N = 22) |
|
| Outcomes | Relevant to this review.
Not relevant to this review:
|
|
| Notes | Conflict of interest: no information DOI: n/a Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Gürtan Bölükbasi 2013.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Ankara University Medical School, Turkey Data collection: no information Funding: no information Registration: no information |
|
| Participants | 31 ASA I to III participants undergoing hip fracture surgery under spinal anaesthesia Excluded: no information Type of fracture: hip fracture Anaesthetic technique for surgery: spinal block Surgical technique: surgery for hip fracture Mean age: no information (range 60 to 90) Percentage female: no information Length of follow‐up: no information |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 15) Comparator: no nerve block (N = 16) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a Study authors contacted on 25 May 2015. Confirmed that they were the authors of the abstracts but did not provide requested information |
|
Haddad 1995.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Stevenage, UK Data collection: no information Funding: no information Registration: no information |
|
| Participants | 50 participants with an extracapsular hip fracture Excluded: dementia, inability to rate pain Type of fracture: extracapsular fracture of the femoral neck Anaesthetic technique for surgery: not stated Surgical technique: internal fixation of fracture with a dynamic hip screw Mean age: 77 years (range 68 to 89) Percentage female: 70% Length of follow‐up: in‐hospital |
|
| Interventions |
Intervention: femoral nerve block (N = 25) Comparator: no nerve block (N = 25) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a No email address Sources obtained for risk of bias assessment.
|
|
Henderson 2008.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee Site: Beth Israel Medical Center, New York, NY, USA Data collection: no information Funding: departmental/institutional Registration: no information |
|
| Participants | 14 participants older than 55 years of age presenting with acute hip fracture Excluded: no information Type of fracture: hip fracture Anaesthetic technique for surgery: not mentioned Surgical technique: no information Median age: 78 years (range not stated) Percentage female: 64% Length of follow‐up: 24 hours or until surgery |
|
| Interventions |
Intervention: femoral nerve block (N = 6) Comparator: no nerve block (N = 8) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a Conference abstract; reported as preliminary results of a larger trial No email address Sources obtained for risk of bias assessment.
|
|
Hogg 2009.
| Study characteristics | ||
| Methods | Parallel RCT Ethics committee approval and participant consents: not stated Site: Belfast, UK Data collection: no information Funding: no information Registration: ISRCTN07083722 |
|
| Participants | 39 participants undergoing surgery for femoral neck fracture Excluded: no information Type of fracture: femoral neck fracture Anaesthetic technique for surgery: spinal block Surgical technique: no information Mean age: 78 years (range not mentioned) Percentage female: no information Length of follow‐up: 15 minutes |
|
| Interventions |
Intervention: fascia iliaca block (N = 19) Comparator: no nerve block (N = 20) All participants had a block at the end of surgery (part 2 of the study); therefore, for the present review, we retained only part 1 of the study (i.e. pain scores during positioning for spinal block) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a Conference abstract No email address Sources obtained for risk of bias assessment.
|
|
Hood 1991.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and written informed consents obtained Site: Sheffield, UK Data collection: no information Funding: no information Registration: no information |
|
| Participants | 50 participants > 60 years of age with hip fracture surgically treated with a pin and plate or a compression screw Excluded: absolute contraindication to a regional technique, allergy to local anaesthetic agents, systemic disease that indicated an alternative method of anaesthesia Type of fracture: intertrochanteric fracture of the neck of the femur Anaesthetic technique for surgery: general anaesthesia Surgical technique: compression screw or pin and plate device Mean age: 81 years (range 62 to 94) Percentage female: 88% Length of follow‐up: 24 hours |
|
| Interventions | Intervention: femoral (triple nerve block) nerve block and infiltration above the iliac crest (N = 25) Comparator: no nerve block (N = 25) | |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a No email address Sources obtained for risk of bias assessment.
|
|
Jadon 2014.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Tata Motors Hospital, Jamshedpur, Jharkhand, India Data collection: no information Funding: departmental/institutional Registration: no information |
|
| Participants | 60 ASA I to II participants of both sexes, weight > 50 kg, scheduled for fracture femur operation under central neuraxial block but unable to sit because of pain Excluded: could sit comfortably; any contraindication to spinal anaesthesia, FNB, or local anaesthetic Type of fracture: neck femur fracture (N = 16), intertrochanteric femur fracture (N = 29), shaft femur fracture (N = 15) Anaesthetic technique for surgery: spinal block Surgical technique: not stated Mean age: 64.3 years (range 18 to 70 years) Percentage female: 33% Length of follow‐up: 5 minutes |
|
| Interventions |
Intervention: femoral nerve block (N = 23 for proximal end femur fracture) Comparator: no nerve block (N = 21 for proximal end femur fracture) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "none declared" DOI: 10.4103/0019‐5049.147146 Study also includes participants with shaft fracture. We obtained results for pain scores on movement for participants with proximal fracture only from the study authors. However, we did not keep results in the analysis (see Effects of interventions) owing to the short delay between the block and the evaluation Email sent on 5 January 2020 for additional information Sources obtained for risk of bias assessment.
|
|
Jang 2018.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Hallym University, Chuncheon Sacred Heart Hospital, Department of Anesthesiology, Chuncheon, Korea Data collection: no information Funding: governmental Registration: KCT0001702 |
|
| Participants | 32 participants 60 years of age or older, radiographically proven and isolated femoral neck fracture, normal distal neurovascular status, moderate to severe (≥ 5) verbal/visual analogue scale pain score Excluded: refused to participate or with known history of study drug allergy, previous femoral vascular surgery on same side of the fracture, inability to understand the study protocol Type of fracture: femoral neck fracture Anaesthetic technique for surgery: not mentioned Surgical technique: not mentioned Mean age: 75.6 years (range 61 to 90) Percentage female: 70% Length of follow‐up: 48 hours |
|
| Interventions |
Intervention: femoral nerve block (N = 16) Comparator: sham block with saline (N = 16) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: none DOI: 10.1016/j.bjan.2018.03.004 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Jones 1985.
| Study characteristics | ||
| Methods | Parallel RCT Informed consents obtained Site: Royal Free Hospital, Pond Street, Hampstead, London, UK Data collection: not mentioned Funding: no information Registration: no information |
|
| Participants | 19 participants with an extracapsular hip fracture treated with a pin and plate or a sliding hip screw Excluded: other painful lesions, signs of moderate or severe dementia, < 65 years of age, systemic disease indicating an alternative method of anaesthesia (e.g. spinal) Type of fracture: extracapsular hip fracture Anaesthetic technique for surgery: general anaesthesia Surgical technique: pin and plate or a sliding hip screw Mean age: 82 years (range 67 to 93) Percentage female: 95% Length of follow‐up: 24 hours |
|
| Interventions | Intervention: lateral femoral cutaneous nerve block (N = 10) Comparator: no nerve block (N = 9) | |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a No email address Sources obtained for risk of bias assessment.
|
|
Kullenberg 2004.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Ortopedkliniken, Blekingesjukhuset, Karlshamn, Sweden Data collection: no information Funding: no information Registration: no information |
|
| Participants | 80 participants with hip fracture confirmed by X‐ray Excluded: inability to rate pain Type of fracture: femoral neck (66%) or trochanteric (44%) fracture Anaesthetic technique for surgery: not stated Surgical technique: nail‐osteosynthesis (Garden 1 to 2 fractures) or hemi‐endoprosthesis (Garden 3 to 4 fractures) Mean age: 82 years (range not stated) Percentage female: 64% Length of follow‐up: in‐hospital (mean 11 days) |
|
| Interventions |
Intervention: femoral nerve block (N = 40) Comparator: no nerve block (N = 40) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "no conflict of interest declared" DOI: n/a Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Landsting 2008.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained. "Patients who were unable to give their consent were included following presumed consent; they were assessed as not having the capacity for consent at the time of inclusion. This assessment was made by the including physician, together with the nurse responsible for the patient. The Short Portable Mental Status Questionnaire was used to support the decision of inclusion on presumed consent. Presumed consent was given with the support of the Regional Ethics Board in Uppsala, as directed by Swedish law". Site: University Hospital, Örebro University, Sweden Data collection: October 2010 to February 2012 Funding: governmental (external monitoring) Registration: EudraCT number 2008‐004303‐59 |
|
| Participants | 127 participants > 64 years of age with radiographically confirmed hip fracture and fascia iliaca compartment block administered within 1 hour of admission to hospital Excluded: refusal to participate, more than 1 fracture, trauma longer than 12 hours before inclusion, hypersensitivity to local anaesthetics, infection in the injection area, neurovascular problems in the affected leg, unable to receive fascia iliaca compartment block within the inclusion time frame, assessed as at risk for complications from fascia iliaca compartment block due to health status Type of fracture: neck (48.8%), trochanteric (45.7%), subtrochanteric (5.5%) Anaesthetic technique for surgery: not stated Surgical technique: no information Mean age: 84.7 years (range 65 to 99) Percentage female: 69.3% Length of follow‐up: in‐hospital (mean 11 days) |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 66) Comparator: sham block with saline (N = 61) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "the authors declare that they have no competing interests" DOI: 10.1016/j.ijotn.2018.11.003 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Liebmann 2012.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and written informed consents obtained Site: University Hospital, Rhode Island Hospital, USA Data collection: January 2009 through June 2010 Funding: charity Registration: NCT01701414 |
|
| Participants | 36 participants: ≥ 55 years of age, with radiographically proven femoral neck or intertrochanteric fracture, normal lower extremity neurovascular examination, ability to consent and actively participate in the study, moderate to severe pain (numerical pain rating score 5) at time of enrolment Excluded: patients with known international normalized ratio > 3.0, prior femoral artery vascular surgery on the same side as the fracture, other significant trauma, hypoxia (pulse oximetry < 92%), hypotension (systolic blood pressure < 100 mmHg), known hypersensitivity to local anaesthetics or morphine Type of fracture: femoral neck or intertrochanteric fracture Anaesthetic technique for surgery: not mentioned Surgical technique: not mentioned Mean age: 82 years (range 64 to 98) Percentage female: 67% Length of follow‐up: time in the emergency department (median durations 480 and 510 minutes) |
|
| Interventions |
Intervention: femoral nerve block (N = 18) Comparator: sham block (N = 18) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no conflict of interest DOI: 10.1111/acem.12154 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Luger 2012.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and written informed consents obtained Site: Innsbruck Medical University, Innsbruck, Austria Data collection: no information Funding: "the manuscript was solely supported by institutional and private resources" Registration: no information |
|
| Participants | 34 ASA I to III very elderly participants (> 80 years) with hip fracture (of whom 3 with dementia had to be excluded) scheduled for surgery under spinal anaesthesia Excluded: patients with score < 18 on the Mini‐Mental State Examination, whose surgery did not take place within 36 hours, with known intolerance or allergies to drugs, planned or required general anaesthesia, refusal of consent, participation in a different study, administration of midazolam as premedication, chronic pain, contraindications and spinal anaesthesia failure, incomplete data records Type of fracture: pertrochanteric femur fracture (45%) or medial femur neck fracture (55%) Anaesthetic technique for surgery: spinal block Surgical technique: hemi‐arthroplasty (35%), total hip replacement (10%), dynamic hip screw (30%), cannulated screws (5%) or proximal femoral nail (20%) Mean age: 89 years (range not mentioned) Percentage female: 95% Length of follow‐up: in hospital |
|
| Interventions |
Intervention: continuous femoral (3‐in‐1) nerve block (N = 10) Comparator: no nerve block (N = 10) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "the author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article" DOI: 10.1177/2151458512470953 Study also includes a group with epidural analgesia (N = 14) ‐ not retained in this review Email sent on 5 January 2020 |
|
Ma 2018a.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Xuanwu Hospital of Capital Medical University, Beijing, China Data collection: December 2015 to December 2016 Funding: governmental Registration: no information |
|
| Participants | 116 ASA II to IV participants with hip fracture (femoral neck or intertrochanteric fracture) diagnosed by X‐ray Excluded: patients with multiple fractures; allergy to amide local anaesthetic, paracetamol, tramadol, and pethidine; infection at the puncture site of the fascia iliaca compartment; peripheral neuropathy; renal insufficiency; dementia; waiting time before surgery longer than 5 days; patient refusal to join in the study Type of fracture: femoral neck (30%) or intertrochanteric fractures (70%) Anaesthetic technique for surgery: not mentioned Surgical technique: not mentioned Mean age: 80.5 years (range 65 to 95) Percentage female: 65.5% Length of follow‐up: AD surgery |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 58) Comparator: no nerve block (N = 58) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: 10.3760/cma.j.issn.0376‐2491.2018.10.002 Email sent on 5 January 2020 |
|
Madabushi 2016.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: MS Ramaiah Medical College and Hospitals, Bangalore, India Data collection: no information Funding: departmental/institutional Registration: no information |
|
| Participants | 60 ASA status I to III participants undergoing surgery for all types of femoral neck fractures Excluded: patients with bleeding diathesis and neuropsychiatric complaints, those on previous opioid therapy or with polytrauma Type of fracture: intertrochanteric or neck fracture Anaesthetic technique for surgery: spinal block Surgical technique: not mentioned Mean age: 59.6 years (range 25 to 75) Percentage female: 47% Length of follow‐up: 24 hours |
|
| Interventions |
Intervention: fascia iliaca block (N = 30) Comparator: no nerve block (N = 30) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: none DOI: 10.1016/j.jclinane.2016.09.014 Email sent on 5 January 2020 |
|
Morrison 2008.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: 3 university hospitals: Beth Israel, Icahn School of Medicine at Mount Sinai, and Maimonides Medical Center, New York, NY, USA Data collection: April 2009 to March 2013 Funding: governmental Registration: NCT00749489 |
|
| Participants | 164 adult patients 60 years of age and over, presenting from 08H00 to 20H00 with a radiographically confirmed hip fracture (femoral neck, intertrochanteric, or pericapsular) Excluded: history of advanced dementia, presence of multiple trauma, pathological fractures, bilateral hip fractures, previous fracture or surgery at the currently fractured site, transferred from another hospital, with cirrhosis or liver failure, had a delay between fracture and admission > 48 hours, were delirious according to the Confusion Assessment Type of fracture: femoral neck (40.5%) or femoral intertrochanteric fracture Anaesthetic technique for surgery: regional (62.1%) or general anaesthesia Surgical technique: hemi‐arthroplasty (29%) or internal fixation Mean age: 82.5 years (range 60 to 98) Percentage female: 72.6% Length of follow‐up: 6 weeks |
|
| Interventions |
Intervention: femoral nerve block followed by a continuous fascia iliaca block (N = 72) Comparator: no nerve block (N = 81) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "the editor‐in‐chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper. Dr. Silverstein died before the study’s completion. At the time of his death, he reported no conflicts of interest" DOI: 10.1111/jgs.14386 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Mosaffa 2005.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Akhtar Hospital, Iran Data collection: not stated Funding: not stated Registration: not stated |
|
| Participants | 40 participants with femoral neck fracture Excluded: not stated Type of fracture: femoral neck fracture Anaesthetic technique for surgery: spinal block Surgical technique: not stated Mean age: not stated (no information on range) Percentage female: not stated Length of follow‐up: not stated |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 20) Comparator: no nerve block (N = 20) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a Conference abstracts Email sent on 26 May 2015; no reply |
|
Mouzopoulos 2009.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and signed informed consents obtained Site: University of Athens, Athens, Greece Data collection: July 2004 until March 2008 Funding: not stated Registration: not stated |
|
| Participants | 207 participants aged ≥ 70 years at intermediate or high risk of delirium scheduled for hip fracture repair Risk classification was based on the presence of 4 predictive risk factors (severity of illness, measured by acute physiology, age, and long‐term health examination; cognitive impairment, measured by the mini‐mental state examination score; index of dehydration, measured by the ratio of blood urea nitrogen to creatinine; and visual impairment, measured by the standardized Snellen test) as described by Inouye. Intermediate risk for postoperative delirium was defined as the presence of 1 or 2 risk factors; high risk was defined as the presence of ≥ 3 risk factors Excluded: delirium at admission, metastatic hip cancer, history of bupivacaine allergy, use of cholinesterase inhibitors, severe coagulopathy, parkinsonism, epilepsy, levodopa treatment, surgery delayed longer than 72 hours after admission, inability to participate in interviews (profound dementia, respiratory isolation, intubation, aphasia, coma, or terminal illness) Type of fracture: intertrochanteric (71.5%) or subcapital fracture Anaesthetic technique for surgery: epidural anaesthesia Surgical technique: subcapital and trochanteric hip fractures were treated with hemi‐arthroplasty (29.5%) and intramedullary nailing, respectively Mean age: 72.7 years (range not stated) Percentage female: 74.4% Length of follow‐up: in‐hospital |
|
| Interventions |
Intervention: repeated fascia iliaca compartment block (N = 108) Comparator: sham block (N = 111) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "the authors declare that they have no conflict of interest related to the publication of this manuscript" DOI: 10.1007/s10195‐009‐0062‐6 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Murgue 2006.
| Study characteristics | ||
| Methods | Parallel RCT Informed consents obtained Site: Feurs, France Data collection: 1 January 2003 to 1 January 2004 Funding: no information Registration: no information |
|
| Participants | 45 participants with hip fracture Excluded: inability to rate their pain (evaluated with a Mini Mental score), contraindication to nitrous oxide, regional anaesthesia, allergy to study drugs, severe respiratory disease, thoracic trauma, renal dysfunction, pre‐fracture opioid treatment Type of fracture: neck femoral fracture Anaesthetic technique for surgery: no information Surgical technique: no information Mean age: 86 years (range 70 to 96) Percentage female: 82% Length of follow‐up: AD skin traction placement before surgery |
|
| Interventions |
Intervention: femoral nerve block (N = 16) Comparator: no nerve block (N = 29); IV morphine (N = 14), or IV paracetamol and ketoprofen (N = 15) We retained only the IV morphine group as the comparator |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a Invalid email address Sources obtained for risk of bias assessment.
|
|
Nie 2015.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and written informed obtained Site: The 4th People’s Hospital of Guiyang, Guiyang, China Data collection: December 2012 to December 2013 Funding: governmental Registration: "the trial was not registered with a trial registry" |
|
| Participants | 104 participants scheduled for open reduction of hip fracture Excluded: neuropathy involving lower extremities, bladder dysfunction, coagulopathies, known allergy to amide local anaesthetic drugs or opioids, inability to co‐operate, psychological disorder, linguistic difficulty that could interfere with pain assessment Type of fracture: proximal femoral fracture Anaesthetic technique for surgery: general anaesthesia Surgical technique: open reduction and internal fixation using the anti‐rotation proximal femoral nail technique Mean age: 70.8 years (range not stated) Percentage female: no information Length of follow‐up: in‐hospital (mean 22 days) |
|
| Interventions |
Intervention: continuous fascia iliaca compartment block (N = 51) Comparator: no nerve block (N = 53) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "the authors have no conflicts of interest to declare" DOI: n/a Additional information received from study authors Email sent on 5 January 2020 for additional information Sources obtained for risk of bias assessment.
|
|
Ranjit 2016.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Dhulikhel Hospital, Kathmandu University Hospital Dhulikhel, Kavre, Nepal Data collection: January 2015 to December 2015 Funding: no information Registration: no information |
|
| Participants | 40 ASA I or II participants undergoing surgery for proximal femur fracture Excluded: bleeding diathesis, known adverse reaction to amide local anaesthetics, polytrauma, inability to assign pain score for any reason, use of analgesics 6 hours before surgery Type of fracture: proximal femur fracture Anaesthetic technique for surgery: spinal block Surgical technique: closed reduction fixation for proximal femur fracture Mean age: 61.7 years (range 18 to 75) Percentage female: 37.5% Length of follow‐up: intraoperative |
|
| Interventions |
Intervention: femoral nerve block (N = 20) Comparator: no nerve block and intravenous fentanyl (N = 20) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Segado Jimenez 2009.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Complexo Hospitalario de Ourense, Spain Data collection: May to December 2008 Funding: no information Registration: no information |
|
| Participants | 75 participants undergoing hip fracture repair under spinal anaesthesia Excluded: general anaesthesia or intravenous administration of analgesics intraoperatively; pretreatment for chronic pain or for ischaemic heart rhythm disorder; neurodegenerative or psychiatric disease; lack of collaboration and/or understanding of the participant; allergy to local anaesthetics; contraindications for regional anaesthesia Type of fracture: hip fracture Anaesthetic technique for surgery: spinal block Surgical technique: total (50.7%) or partial (26.7%) arthroplasty or femur osteosynthesis (gamma nail insertion (14.7%) or clove Richards insertion (8%)) Mean age: 72 years (range 47 to 96) Percentage female: 56% Length of follow‐up: in‐hospital |
|
| Interventions |
Intervention 1: lateral femoral cutaneous nerve block and obturator nerve block (N = 25) Intervention 2: obturator nerve block only (N = 25) Comparator: no nerve block (N = 25) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Spansberg 1996.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: University Hospital of Aarhus, Denmark Data collection: not stated Funding: no information Registration: no information |
|
| Participants | 20 participants with hip fracture surgically treated Excluded: no information Type of fracture: femoral neck fracture Anaesthetic technique for surgery: spinal block Surgical technique: no information Mean age: 81 years (range 58 to 91) Percentage female: unclear Length of follow‐up: in‐hospital |
|
| Interventions |
Intervention: continuous femoral nerve block (N = 10) Comparator: sham block (N = 10) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a No email address Sources obtained for risk of bias assessment.
|
|
Szucs 2010.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and written informed consents obtained Site: University Hospital, Wilton, Cork, Ireland Data collection: no information Funding: departmental/institutional Registration: not registered |
|
| Participants | 24 ASA I to III participants aged > 50 years presenting with fractured neck of femur Excluded: patients who refused or had more than 1 fracture; Mini‐Mental Score < 22; coagulation disorder; head injury; loss of consciousness; 10 mg or more morphine administered pre‐hospital; acute intercurrent heart disease; allergy to bupivacaine, morphine, or paracetamol; skin lesion/infection at block site; renal dysfunction; evidence of systemic infection (clinically defined or elevated C‐reactive protein levels, leucocytosis, or body temperature > 37.8 °C) Type of fracture: neck of femur fracture Anaesthetic technique for surgery: spinal block Surgical technique: no information Mean age: 78.1 years (range not stated) Percentage female: 67% Length of follow‐up: 72 hours after surgery |
|
| Interventions |
Intervention: continuous femoral nerve block (N = 12) Comparator: no nerve block (N = 12) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "the authors declare that they have no competing interests" DOI: 10.1186/2047‐0525‐1‐4 Email sent on 5 January 2020: additional information received from study authors Sources obtained for risk of bias assessment.
|
|
Thompson 2019.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: University Hospital, East Meadow, NY, USA Data collection: February 2017 to February 2019 Funding: departmental/institutional Registration: no information |
|
| Participants | 47 participants ≥ 60 years of age diagnosed with acute fracture of the femoral neck, intertrochanteric or subtrochanteric region of the femur Excluded: dementia, periprosthetic or pathological hip fracture, incarcerated patient, history of complex regional pain syndrome, history of opioid abuse, current opioid use, chronic pain Type of fracture: femoral neck (25.5%), intertrochanteric (66%), or subtrochanteric (8.5%) Anaesthetic technique for surgery: spinal block or general anaesthesia Surgical technique: cephalomedullary nail (≅ 70%), closed reduction percutaneous pinning (≅ 2%), dynamic hip screw (≅ 6%), hemi‐arthroplasty (≅ 19%), or total hip arthroplasty (≅ 2%) Mean age: not stated (range not stated) Percentage female: 70% Length of follow‐up: 72 hours after surgery |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 23) Comparator: no nerve block (N = 24) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "the authors report no conflicts of interest related to this work" DOI: 10.1097/BOT.0000000000001634 Invalid email address |
|
Tuncer 2003.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Konya, Turkey Funding: no information Registration: no information |
|
| Participants | 40 ASA I to II participants with hip fracture, undergoing surgery for trochanteric hip fracture Excluded: coagulation abnormality, age < 18 or > 80 years, weight < 50 or > 100 kg, known allergy to bupivacaine or opioids, previous analgesic treatment with opioids, inability to understand pain scales or use a patient‐controlled analgesia device Type of fracture: trochanteric femur fracture Anaesthetic technique for surgery: general anaesthesia Surgical technique: trochanteric fracture repair Mean age: 59 years (range not stated) Percentage female: not stated Length of follow‐up: in‐hospital |
|
| Interventions |
Intervention: continuous femoral (3‐in‐1) nerve block (N = 20) Comparator: no nerve block (N = 20) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
Participant satisfaction (rated as excellent, good, moderate, or poor; we assigned scores from 1 to 4 to compare data) |
|
| Notes | Conflict of interest: no information DOI: 10.1016/S1366‐0071(03)00004‐4 Email sent to study authors on 24 May 2015, to ask for additional information; no reply |
|
Unneby 2017.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Umeå University, Umeå, Sweden Data collection: between April 2009 and September 2011 Funding: charity Registration: no information |
|
| Participants | 266 participants aged ≥ 70 years with hip fracture (trochanteric and cervical), including those with dementia (N = 120) Excluded: infection or previous vascular surgery in the inguinal area Type of fracture: trochanteric (48.1%) or neck (51.9%) femur fracture Anaesthetic technique for surgery: no information Surgical technique: no information Mean age: 84.1 years (range not stated) Percentage female: 64% Length of follow‐up: 18 hours |
|
| Interventions |
Intervention: femoral nerve block (N = 129) Comparator: no nerve block (N = 137) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: none DOI: 10.1016/j.injury.2017.04.043 Email sent on 5 January 2020 |
|
Uysal 2018.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: Mugla Sitki Koçman University Training and Research Hospital, Isparta, Turkey Data collection: 15 April 2018 to 18 May 2018 Funding: departmental/institutional Registration: ACTRN12618000546257 | |
| Participants | 110 ASA II to IV participants > 65 years of age with hip fracture Excluded: preexisting delirium at admission to emergency service, femur fracture due to metastatic carcinoma, bupivacaine allergy, cholinesterase inhibitor or levodopa medication, parkinsonism or epilepsy, contraindication for nerve blockage. Patients operated longer than 48 hours after admission were excluded from the trial Type of fracture: trochanteric femur fracture Anaesthetic technique for surgery: combined spinal/epidural; both groups had postoperative epidural analgesia Surgical technique: no information Mean age: 81.7 years (range not stated) Percentage female: 44% Length of follow‐up: 3 days |
|
| Interventions | Intervention: continuous femoral nerve block (N = 46) Comparator: no nerve block and IV paracetamol (N = 45) | |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "none declared"
DOI: 10.14744/tjtes.2019.78002 Email sent to authors 23 January 2020 Sources obtained for risk of bias assessment.
|
|
Wang 2015.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: University Hospital, Beijing, China Data collection: October 2015 to December 2016 Funding: departmental/institutional and governmental Registration: ChiCTR‑IPR‑15007283 |
|
| Participants | 88 ASA classification III or IV, very elderly (age ≥ 80 years) participants with hip fracture, complicated by at least 1 cardiovascular, neurological, or pulmonary disease Excluded: more than 1 fracture; allergy to amide local anaesthetics, paracetamol, or tramadol; infection at the puncture site; peripheral neuropathy; contraindication to spinal block; renal insufficiency; dementia; preoperative waiting time ≥ 5 days Type of fracture: femoral neck or intertrochanteric femur fracture Anaesthetic technique for surgery: combined spinal/epidural Surgical technique: proximal femoral nail anti‐rotation (76.1%), hemi‐arthroplasty (17.1%), cannulated screws (3.4%), or total hip replacement (3.4%) Mean age: 83.9 years (range ≥ 80 years) Percentage female: 65% Length of follow‐up: in‐hospital (mean 10 and 14 days) |
|
| Interventions |
Intervention: continuous fascia iliaca block (N = 44) Comparator: sham block with saline (N = 44) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: none DOI: 10.3892/etm.2018.6417 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
White 1980.
| Study characteristics | ||
| Methods | Parallel RCT Consents obtained Site: Groote Schuur Hospital, Observatory, Cape Town, South Africa Data collection: not mentioned Funding: no information Registration: no information |
|
| Participants | 60 participants with hip fracture undergoing surgery Excluded: fracture sustained longer than 8 days before admission; < 60 years old; absolute contraindication to a regional technique, such as localized sepsis, suspicion of bacteraemic process, or anticoagulant therapy; overt or suspected endocrine disorder other than diabetes mellitus Type of fracture: neck of femur fracture Anaesthetic technique for surgery: general anaesthesia Surgical technique: Austin Moore prosthesis or a Zimmer sliding screw Mean age: 79 years (range not stated) Percentage female: 81% Length of follow‐up: 4 weeks |
|
| Interventions |
Intervention: psoas compartment block (N = 20) Comparator 1: no nerve block (N = 20) Comparator 2: spinal (N = 20), not retained for this review |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: no information DOI: n/a No email address Sources obtained for risk of bias assessment.
|
|
Yamamoto 2016.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: Shimane University Faculty of Medicine, Shimane, Japan Data collection: October 2016 to January 2018 Funding: departmental/institutional Registration: JPRN‐UMIN0 0 0 024147 |
|
| Participants | 53 ASA I or II participants over 50 years of age with acute proximal hip fracture Excluded: poorly controlled diabetes mellitus, defined as haemoglobin A1c level > 7.0%; neurological disease; history of allergy to study drugs; serious systemic comorbidity; bleeding disorder; previous surgery in affected hip; regular opioid therapy; infection at injection site; open fracture; multiple injuries requiring pain medications or other surgeries; impaired cognition or dementia; delirium at admission Type of fracture: femoral neck (39.6%) or pertrochanteric (60.4%) femur fracture Anaesthetic technique for surgery: spinal block Surgical technique: internal fixation (84.9%) or bipolar hemi‐arthroplasty (15.1%) Mean age: 84.6 (range not stated) Percentage female: 84.9% Length of follow‐up: 7 days |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 25) Comparator: no nerve block (N = 28) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "there are no conflicts of interest to declare" DOI: 10.1016/j.injury.2019.03.008 Email sent on 5 January 2020 Sources obtained for risk of bias assessment.
|
|
Yang 2016.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: West China Hospital, Sichuan University, Sichuan, China Data collection: not mentioned Funding: no information Registration: no information |
|
| Participants | 32 ASA II to III participants scheduled for hip fracture surgery Excluded: no information Type of fracture: hip fracture Anaesthetic technique for surgery: general anaesthesia Surgical technique: hip fracture surgery Mean age: not mentioned (range 66 to 90) Percentage female: no information Length of follow‐up: 3 days |
|
| Interventions |
Intervention: continuous fascia iliaca compartment block (N not clearly mentioned, taken as 16) Comparator: no nerve block and intravenous patient‐controlled analgesia with sufentanil (N not clearly mentioned, taken as 16) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "none declared" DOI: 10.1213/01.ane.0000492738.72065.76 Conference abstract No email address Sources obtained for risk of bias assessment.
|
|
Yun 2009.
| Study characteristics | ||
| Methods | Parallel RCT Approved by the ethics committee and written informed consents obtained Site: University Hospital, College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea Data collection: July 2007 to December 2007 Funding: departmental/institutional Registration: no information |
|
| Participants | 40 ASA physical status I to III participants with isolated femoral neck fracture Mean age: not mentioned (range 62 to 88) Excluded: known allergy to amide local anaesthetics, haemorrhagic diathesis, peripheral neuropathy, mental disorder Type of fracture: Garden’s classification III or IV femoral neck fracture Anaesthetic technique for surgery: spinal block Surgical technique: bipolar hemi‐arthroplasty (82.5%), closed reduction and internal fixation with compression hip screw (12.5%), or total hip replacement arthroplasty (5%) Mean age: 75 years (range 62 to 88) Percentage female: 65% Length of follow‐up: 24 hours |
|
| Interventions |
Intervention: fascia iliaca compartment block (N = 20) Comparator: no nerve block (N = 20) |
|
| Outcomes | Relevant to this review.
Not relevant to this review.
|
|
| Notes | Conflict of interest: "no conflict of interest" DOI: 10.1111/j.1399‐6576.2009.02052.x Email sent on 5 January 2020; additional information received from study authors Sources obtained for risk of bias assessment.
|
|
ASA: American Society of Anesthesiologists physical status.
CSF: cerebrospinal fluid.
DSM: Diagnostic and Statistical Manual of Mental Disorders.
ECG or EKG: electrocardiogram.
ED: emergency department.
FNB: femoral nerve block.
G: gram.
h: hour.
IM: intramuscular.
IQR: interquartile range.
IV: intravenous.
mcg: microgram.
mg: milligram.
mL: millilitre.
N: number
n/a: not available.
PCA: patient‐controlled analgesia.
RCT: randomized controlled trial.
SC: subcutaneous.
SD: standard deviation.
VAS or VRS: visual or verbal analogue/response scale.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Akhtar 2015 | Not an RCT: the word 'random' is not mentioned anywhere. The methods section does not suggest any form of randomization: "55 patients with a NOF fracture admitted between August 2014 and January 2015 were recruited. 21 patients were given FIBi and 34 (control) had regular analgesia as per trust guidelines" |
| Amini 2012 | Different intervention: addition or not of dexamethasone to nerve block |
| Amiri 2012 | Different intervention: comparison of combined spinal plus femoral nerve block vs lumbar plexus block |
| Anaraki 2012 | Different population: "the primary aim of our study was to investigate the effects of gabapentin and fascia iliaca block on pain score and morphine consumption after femoral shaft surgery" |
| Aprato 2018 | Different intervention: a comparison of fascia‐iliaca compartment block vs intra‐articular hip injection for preoperative pain management in intracapsular hip fracture |
| Arsoy 2017 | Not an RCT: "we retrospectively reviewed all geriatric hip fracture patients who were treated surgically from January 11, 2012 to December 31, 2015" |
| Arsoy 2017a | Not an RCT: "we retrospectively identified 265 consecutive geriatric hip fracture patients who underwent surgical treatment" |
| Barnes 2019 | Not an RCT: "we conducted a prospective case‐control study" |
| Beaudoin 2010 | Not an RCT: "this prospective observational study" |
| Bech 2011 | Different intervention: local anaesthetic infiltration |
| Bendtsen 2014 | "Terminated (less inclusions than expected with the given criteria)" Last update posted: 14 September 2015 |
| Bendtsen 2015 | "Withdrawn (the study was completely redesigned)" Last update posted: 14 September 2015 |
| Bendtsen 2015a | Different intervention: additional nerve blocks if "verbal pain score (0‐10) > 3 at rest or > 5 with passive leg raise 30 minutes after femoral nerve block" |
| Bendtsen 2015b | Not an RCT: validation of a new block technique that could apply to hip fracture |
| Bhadani 2017 | Different population: "in patients with femoral shaft fracture" |
| Bhattacharya 2019 | Different intervention: comparison between 2 different block techniques (i.e. pericapsular nerve group block and fascia iliaca) |
| Bouhours 2010 | Different intervention: "this study compared the reduction in morphine consumption and related side effects of a continuous femoral block with a single shot block in hip‐fracture patients" |
| Bulger 2015 | Different population: 8 participants had no X‐ray‐proven fracture, 3 had a shaft fracture, and 3 had a fracture of acetabulum, pelvis, or pubic ramus. We were unable to obtain data separately for hip fracture only from study authors |
| Callear 2016 | Not an RCT: "the aim of this project was to evaluate the proportion of patients receiving a fascia‐iliac block prior to operative intervention" |
| Candal‐Couto 2005 | Not an RCT: "we studied 30 consecutive patients, regardless of their mental state. One hour following the block, there was a significant improvement in the sitting scores as well as the passive hip flexion (mean increase 44 degrees). Visual analogue scores also improved significantly from 7.2 to 4.6 (S.D. 2.4) in the 18 patients without cognitive impairment. We conclude that fascia iliaca blocks can provide significant benefit in the pre‐operative period and allow patients to sit up more comfortably while they await surgery" |
| Carlisle 2004 | Different population: this was a randomized trial of 62 participants with femoral trauma who were randomized to receive at the site of the accident a femoral nerve block or intravenous metamizole for pain. Study provided a variety of causes for femoral trauma, including 20 cases of hip fracture. The nerve block was shown to reduce the degree of pain as assessed by the visual analogue scale and to reduce anxiety and heart rate. We excluded the study, as it included participants with other conditions. Trialists were unable to provide separate results for hip fracture participants |
| Castillon 2017 | Not an RCT: "a cohort of 216 patients, from January to December 2016, was studied prospectively" |
| Chang 2011 | Not an RCT: observational trial of patients who were never operated |
| Christos 2010 | Not an RCT: educational article on ultrasound‐guided femoral nerve block for hip fracture |
| Dodd 2019 | Different intervention: "objectives: to prove superiority of repeated bolus fascia iliaca catheters compared to single bolus delivered by emergency physicians in emergency hip fractures up to time of surgery" |
| Dulaney‐Cripe 2012 | Not an RCT: "all patients who presented to our institution with a hip fracture were given the option of having a continuous fascia iliaca compartment block for pain control versus usual pain management (non‐opioids, opioids, and ice therapy)" |
| Durrani 2013 | Different population: 47 proximal fractures, 28 shaft fractures, 9 distal fractures. Mean age 42 years Email sent 17 March 2016, to request separate data for participants with a proximal fracture; no reply |
| Elkhodair 2011 | Not an RCT: "a prospective cohort study was carried out on 137 patients" |
| Evans 2019 | Not an RCT: conference abstract trying to identify patient‐prioritized outcomes when evaluating blocks performed by paramedics |
| Finlayson 1988 | Not an RCT: "thirty‐six patients with femoral neck fractures attending the accident department over a three month period received femoral blocks from one of the two authors" |
| Foss 2005 | Different intervention: epidural analgesia |
| Foss 2009 | Not an RCT: "one hundred and seventeen hip fracture patients were included in a descriptive prospective study" |
| Fujihara 2013 | Not an RCT: "the included patients were assigned to one of two groups in alternating order" |
| Gasanova 2019 | Different intervention: comparison between different peripheral nerve blocks |
| George 2016 | Different intervention: trial comparing femoral nerve block vs fascia iliaca compartment block |
| Ghimire 2015 | Different intervention: comparison between fascia iliaca block and femoral nerve block for positioning for spinal anaesthesia |
| Godoy Monzon 2007 | Not an RCT: "after informed consent, a physician administered one FICB to 63 sequential adult ED patients (43 women, 20 men; ages 37‐96 years, mean 73.5 years) with radiographically diagnosed hip fractures" |
| Gorodetskyi 2007 | Different intervention: this was a randomized study of 60 participants with a trochanteric hip fracture fixed with a sliding hip screw or a trochanteric external fixator. After surgery, participants were randomized to an active non‐invasive interactive neurostimulation device or to a sham device. The active device generated biphasic electrical impulses. Participants allocated to the active group had a reduced level of pain, a reduced analgesic requirement, and a greater range of flexion of the injured limb. We excluded the study, as it was not a study of nerve blocks |
| Gosavi 2001 | Not an RCT: all participants had a femoral nerve block |
| Gozlan 2005 | Not an RCT: "étude prospective et descriptive" = prospective and descriptive study |
| Grigg 2009 | Not an RCT: observational report on feasibility of nurses administering a nerve block |
| Groot 2015 | Not an RCT: "between September 2012 and July 2013, we performed a prospective pilot study" |
| Haines 2012 | Not an RCT: "in this prospective, observational, feasibility study", based on published article The trial registry "ClinicalTrial.gov" includes registration NCT01904071 done by one of the study authors (First posted: 22 July 2013; Results first posted: 24 April 2014; Last update posted: 6 June 2018). In the trial registry, one can find results for 3 groups of participants: (1) ultrasound‐guided femoral nerve block, (2) ultrasound‐guided fascia iliaca block, and (3) no block. Characteristics of participants and results of group ultrasound‐guided fascia iliaca published on the website of the trial registry are identical to those published in the observational study, namely, N = 20; age = 82 (SD 7.7) years; female/male = 11/9; and pain score before the procedure = 5.50 (3.99). Furthermore, the trial registry (accessed 27 December 2019) cites the published article summarizing the "observational study" as "Publications of results". For this reason, the study at the trial registry was considered not randomized and was linked to this publication of an observational study The only results available in the trial registry that would have been included in the review are pain at rest 30 minutes after block placement: "1.94 (2.43); 2.05 (2.61); 5.13 (2.70) for ultrasound‐guided femoral nerve block, ultrasound‐guided fascia iliaca block, and no block, respectively, and absence of serious adverse events" |
| Hallberg 2012 | Terminated |
| Hao 2018 | Different intervention: comparison of ultrasound‐guided vs landmark fascia iliaca block; all participants had epidural analgesia for postoperative pain |
| Hauritz 2009 | Not an RCT: all participants had a fascia iliaca block |
| Helsø 2016 | Not an RCT: retrospective trial: "patients were identified from the local database on all hip fracture patients admitted" |
| Hoffmann 2015 | Different intervention: comparison of ultrasound‐guided femoral nerve block vs femoral nerve block with no ultrasound for guidance |
| Hogh 2008 | Not an RCT: "the FIB technique has routinely been used pre‐operatively in the emergency department since 1 January 2004 for all patients with hip fractures. Over an 8‐month period, 187 patients were treated.....Effect of FIB was prospectively assessed on 70 patients" |
| Hussain 2014 | Different intervention: amount of local anaesthetic used (bupivacaine 12.5 mg/kg of body weight) exceeds recommendations |
| Iamaroon 2010 | Different population: although the vast majority of participants had a proximal fracture, 10 participants had a shaft fracture (6 participants for femoral nerve block, 1 for control, or 3 for distal (participants in the control group)). An email was sent on 17 March 2016, to obtain data separately for participants with a proximal fracture; no reply was received |
| Inan 2009 | Different intervention: all participants had a 3‐in‐1 femoral nerve block with or without the addition of oral dexketoprofen |
| Irwin 2012 | Not an RCT: retrospective study |
| Isalgue 2014 | Not an RCT: although the same number of participants was included in the 2 groups, the word 'random' is not mentioned anywhere in the abstract nor in the text |
| Ishioka 2018 | Not an RCT: "basic design: single arm; randomization: non‐randomized" |
| Kacha 2018 | Different population: include patients with acetabular fracture; we were unable to obtain data separately for femur fracture only |
| Kang 2013 | Different intervention: local anaesthetic infiltration |
| Kassam 2018 | Not an RCT: "the first 20 patients (Group A) were treated with traditional analgesia regimen... the second consecutive 20 patients, all underwent a landmark based FIB" |
| Klukowski 2017 | Not an RCT: "a retrospective analysis of perioperative medical records of 78 patients undergoing surgical treatment of proximal femur fractures was performed" |
| Kristek 2019 | Different intervention: "to investigate the possible effect of postoperatively applied analgesics ‐ epidurally applied levobupivacaine or intravenously applied morphine..." |
| Kumar 2016 | Not an RCT: "all 50 patients received an ultrasound guided Fascia Iliaca Compartment Block (FICB)" |
| Kumie 2015 | Not an RCT: single‐institution case control study |
| Lee 2015 | Different intervention: in Abstract, "we conducted a prospective cluster trial, randomized by emergency physicians". The trial, published as a conference abstract, reported that peripheral nerve block use was higher for trained emergency physicians compared with (17/21) those without specific training (1/52) |
| Lee 2016 | Different intervention: randomized by emergency physicians: "all participating emergency physicians (EPs) will be randomly assigned to the order they receive training in a stepped wedge design"; "which block that will be used will be randomly determined at the individual patient level" |
| Leeper 2012 | Not an RCT: "analgesia requirements for all patients admitted with fractured neck of femur to one unit over a 9‐month period were gathered prospectively" |
| Levente 2017 | Not an RCT: prospective observational trial |
| Levine 2003 | Different population: "patients with traumatic mid and distal femur fractures" |
| Li 2013 | Different intervention: all participants had the same blocks; they were randomized by type of general anaesthesia |
| Lopez 2003 | Not an RCT: "a fascia iliaca compartment block was performed on all of them" |
| Mannion 2005 | Different intervention: this was a randomized trial of 36 participants who were having hip fracture surgery. All participants had a psoas block and general anaesthesia. Participants were randomized to 3 groups. A control group received a psoas block and IV saline, another group received psoas block and IV clonidine 1 mg/kg, and a third group received a psoas block and perineural clonidine. The interval from time of completion of block to first supplementary analgesic administration was longer in the IV clonidine group. Results show no significant differences among groups regarding postoperative adverse effects. We excluded the study, as investigators included no 'control' group that received no block |
| Manohara 2015 | Different intervention: comparison between ultrasound‐guided supra‐inguinal fascia iliaca block and femoral nerve block |
| Marhofer 1998 | Different intervention: this was a randomized trial of 60 participants. 20 received a 3‐in‐1 block with ultrasound guidance with 20 mL 0.5% bupivacaine, 20 received 20 mL of 0.5% bupivacaine, and 20 received 30 mL of 0.5% bupivacaine, with nerve stimulator guidance. We excluded the study, as investigators included no comparison with a group without nerve block |
| Masoumi 2014 | Different population: type of fracture: femoral intertrochanteric (N = 30), femoral neck (N = 17), or femoral shaft fracture (N = 13). No email address to obtain results from proximal end fractures separately |
| Matot 2003 | Different intervention: epidural analgesia |
| McGlone 1987 | Not an RCT: "all received a femoral nerve block" |
| McRae 2015 | Different population: 6 participants with shaft fracture. Letter sent 17 March 2016, to request separate data for participants with a proximal fracture; no reply |
| Memary 2015 | Different population: "elective femoral shaft fracture" |
| Mostafa 2015 | Different population: "femur fracture". We were unable to confirm the exact site of femur fracture from study author |
| Mutty 2007 | Different population: this was a randomized trial comparing femoral nerve block vs no block for 54 participants with a femoral shaft or distal femoral fracture. We excluded the study, as it included no proximal femoral fractures |
| Nielsen 2015 | Different intervention: "the aim of this trial is to test the analgesic effect of a femoral nerve block in combination with an obturator nerve block compared to femoral nerve block alone" |
| Pakhare 2016 | Different population: "objective: to compare the analgesic efficacy of femoral nerve block and IV fentanyl in femur shaft fracture patients for positioning them for neuraxial block" |
| Parras 2016 | Different intervention: comparison of quadratus lumborum block type vs femoral nerve block |
| Perrier 2010 | Not an RCT: "prospective, observational study" |
| Piangatelli 2004 | Different intervention: this was a randomized study of 80 participants undergoing lower extremity surgery that compared 4 different methods. A lumbar plexus block with 30 mL 0.5% levobupivacaine or a lumbar plexus block with 30 mL 0.75% ropivacaine or a sciatic nerve block with 10 mL 0.75% ropivacaine or a sciatic nerve block with 10 mL 0.5% levobupivacaine. We excluded the study from this review, as investigators included no 'control' group without nerve block |
| Randall 2008 | Not an RCT: audit on nurse administering peripheral nerve blocks |
| Rapchuk 2013 | Not an RCT: case series of 4 patients |
| Rashwan 2013 | Different intervention: comparison of fascia iliaca vs epidural analgesia |
| Reavley 2015 | Different intervention: comparison between fascia iliaca block and femoral (3‐in‐1) block for preoperative analgesia in the emergency department |
| Reddy 2016 | Different population: 8 participants with shaft fracture and 12 participants with distal femur fracture. We were unable to obtain data for proximal femur fractures separately |
| Rojas Rivera 2002 | Not an RCT: prospective observational study |
| Sahota 2011 | Different intervention: both groups could have a single‐injection block, but the catheter for a continuous infusion was allowed only for the intervention group: "common practice at our institution is to place a femoral nerve block either to facilitate patient positioning for a spinal anaesthetic or as postoperative analgesia in patients having general anaesthesia. This will be permitted in patients in the control group, however catheter insertion is not" |
| Scheinin 2000 | Different intervention: epidural analgesia |
| Segado Jimenez 2010 | Different population: study authors informed us that the trial included participants with hip fracture and participants without hip fracture undergoing elective hip arthroplasty. They could not give us data separately for participants with and without hip fracture: "I did not register which patients were hip fractures, just the type of surgery" |
| Shi 2018 | Different population: hip replacement; the word "fracture" is not mentioned anywhere in the report |
| Sia 2004 | Different population: femoral shaft fractures |
| Siguira 2014 | Terminated on 1 June 2015 |
| Singh 2016 | Different population: intertrochanteric femur fracture (70%), L/C (not defined) femur fracture (1.7%), femoral neck fracture (16.7%), mid‐shaft femur fracture (6.7%), or S/T (not defined) femur fracture (5%). We were unable to obtain data for proximal femur fracture separately |
| Sonawane 2019 | Different intervention: comparison between different peripheral nerve blocks |
| Swart 2017 | Different intervention: "subcutaneous injection at conclusion of surgical fixation of hip fracture" |
| Tao 2016 | Not an RCT: cross‐sectional study to be used for planning an RCT |
| Thakur 2018 | Not an RCT: "observational" |
| Turker 2003 | Different intervention: this was a randomized study of 30 participants who underwent partial hip replacement surgery. 15 received general anaesthesia plus epidural block with 15 mL of 0.5% bupivacaine, and 15 received general anaesthesia plus psoas compartment block with 30 mL of 0.5% bupivacaine. Both groups had similar pain scores, but the epidural group showed greater drops in mean arterial blood pressure from baseline and more complications. We excluded the study from this review because it did not include a control group that did not receive nerve block |
| Van Leeuwen 2000 | Different intervention: this was a randomized study of 3 different combinations of doses of local anaesthetics given to produce a 'three in one' femoral nerve block. We excluded this study from the review because it did not include a 'control' group that did not receive nerve block |
| Vats 2016 | Not an RCT: "in this observational study" |
| Wang 2019 | Not an RCT: "study type: observational study" |
| Wei 2018 | Different intervention: all participants will have a peripheral nerve block |
| WHO Int 2007 | Study terminated in 2010 |
| Williams 2016 | Not an RCT: probably retrospective: "in patients with femoral neck fracture, 69 patients who received standard preoperative analgesia (regular paracetamol 1 g 4 times a day, codeine 60 mg 4 times a day, and opioid 10 mg 2 hourly as required) were compared with 50 patients who received standard preoperative analgesia plus FICB" |
| Zadeh 2015 | Different intervention: comparison of femoral nerve block vs fascia iliaca block |
| Zheng 2017 | Different intervention: comparison of injection below vs at the level of inguinal ligament for fascia iliaca block |
FICB (FIB): fascia iliaca compartment block (fascia iliaca block).
RCT: randomized controlled trial.
Characteristics of ongoing studies [ordered by study ID]
Capelleri 2017.
| Study name | Early femoral block in elderly with hip fracture |
| Methods | Parallel RCT, triple (participant, investigator, outcomes assessor) Approved by the ethics committee and informed consents obtained Site: Italy Data collection: to be determined Funding: to be determined Registration: NCT03092466 |
| Participants | 600 elderly participants > 70 years of age with hip fracture and admission to emergency department from Monday to Friday (from 8H00 AM to 20H00 PM) Excluded: ASA physical status > III, contraindications to regional anaesthesia, allergic to 1 or more drugs used in the study, unable or refuse to provide informed consent, show cognitive impairment or signs of confusion or delirium already on arrival to emergency department, postoperative intensive care unit admission, haemoglobin value < 8 g/dL at admission Type of fracture: femoral neck fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: %: to be determined Length of follow‐up: 12 months |
| Interventions |
Intervention: continuous femoral nerve block Comparator: sham block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 28 March 2017 Study start date: 26 February 2017 Study completion date: 23 October 2020 Last update posted: 31 July 2019 |
| Contact information | Gianluca Cappelleri |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Carvalho 2015.
| Study name | Contribution of anaesthesia technique for post‐operative mortality reduction after proximal femur fractures surgical treatment ‐ a randomized clinical trial |
| Methods | Parallel RCT, double‐blind (investigator, outcome assessor) Approved by the ethics committee and informed consent obtained: to be determined Site: Centro Hospitalar do Porto, Portugal Data collection: to be determined Funding: to be determined Registration: NCT02406300 |
| Participants | 260 adults (≥ 60 years of age) admitted with a diagnosis of proximal femur fracture (ICD‐9 codes 820.0 to 820.9) and submitted to surgical internal fixation of femur or hip prosthesis (ICD‐9 codes 7935, 8151, and 8152) Exclusion criteria: multiple fractures, polytrauma, active malignancy, ASA physical status V, antiplatelet drugs (other than aspirin) in previous 5 days, known allergies to local anaesthetics, contraindication to general or regional anaesthesia Type of fracture: proximal femur fracture Anaesthetic technique for surgery: general anaesthesia in the intervention group and spinal block in the comparator group Surgical technique: to be determined Mean age: (range ) to be determined Percentage female: % to be determined Length of follow‐up: 1 year |
| Interventions |
Intervention: femoral, lateral femoral cutaneous nerve of the thigh and anterior obturator nerve blocks Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 2 April 2015 Study start date: April 2015 Study completion date: January 2017 Last update posted: 2 April 2015 |
| Contact information | Raul Carvalho, MD |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Chinachoti 2010.
| Study name | Intrathecal morphine, femoral nerve block, periarticular bupivacaine infiltration for pain after intramedullary hip screw |
| Methods | Parallel RCT, single masking (outcomes assessor) Approved by the ethics committee and informed consent obtained: to be determined Site: Mahidol University, Taiwan Data collection: to be determined Funding: to be determined Registration: NCT01219088 |
| Participants | 80 ASA I to III participants with femoral neck fracture from 18 to 90 years of age Excluded: contraindication to spinal anaesthesia, inability to use patient‐controlled analgesia, body weight < 30 kg, body mass index > 35 kg/m2, history of research drug allergy, previous history of hip surgery on the same side, pathological fracture (severe infection, bone cancer) Type of fracture: femur fracture Anaesthetic technique for surgery: spinal anaesthesia Surgical technique: intramedullary hip screw Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 48 hours Excluded: patients with contraindication to spinal anaesthesia, inability to use patient‐controlled analgesia, body weight < 30 kg, body mass index > 35 kg/m2, history of research drug allergy, previous history of hip surgery on the same side, pathological fracture (severe infection, bone cancer) |
| Interventions |
Intervention: femoral nerve block Comparator 1: no block Comparator 2: intrathecal morphine Comparator 3: periarticular infiltration |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 13 October 2010 Study start date: September 2010 Study completion date: September 2012 Last update posted: 4 August 2011 |
| Contact information | Thitima Chinachoti, MD |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Chiu 2016.
| Study name | Evaluating the addition of regional analgesia to reduce postoperative delirium in patients having hip fracture surgery (RASAPOD) |
| Methods | Parallel RCT, triple masking (participant, care provider, outcomes assessor) Approved by the ethics committee and informed consents obtained Site: Auckland City Hospital, New Zealand Data collection: to be determined Funding: to be determined Registration: NCT02689388 |
| Participants | 50 participants ≥ 65 years of age with hip fracture requiring surgery Excluded: contraindication to peripheral nerve block or local anaesthetics; unable to do delirium or cognitive testing due to language, vision, or hearing impairment; unable to communicate with research staff due to language barrier; history of long‐term opioid use (longer than 1 month); contraindication to general anaesthesia Type of fracture: hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 90 days |
| Interventions |
Intervention: femoral nerve block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 24 February 2016 Study start date: 28 August 2016 Study completion date: 31 December 2017 Last update posted: 18 July 2017 |
| Contact information | Davina J McAllister |
| Notes | Conflict of interest: to be determined DOI: to be determined |
ClinicalTrials.gov 2019.
| Study name | Fascia iliaca compartment blocks for pain control in hip fractures |
| Methods | Parallel RCT, open label Approved by the ethics committee and informed consent obtained Site: Medical University of South Carolina, Charleston, SC, USA Data collection: to be determined Funding: to be determined Registration: NCT04086914 |
| Participants | 32 participants ≥ 50 years with low‐energy hip fracture Excluded: anticoagulants, hardware present near injection site, preexisting nerve injury Type of fracture: low‐energy acute hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 8 hours |
| Interventions |
Intervention: fascia iliaca compartment block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 12 September 2019 Study start date: 1 November 2019 Study completion date: 1 December 2020 Last update posted: 12 September 2019 |
| Contact information | Medical University of South Carolina, Charleston, SC, USA |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Compere 2012.
| Study name | Hip fracture and perineural catheter |
| Methods | Parallel RCT, open label Approved by the ethics committee and informed consent obtained Site: University Hospital, Rouen, France Data collection: to be determined Funding: to be determined Registration: NCT01638845 |
| Participants | 314 ASA I to III participants aged ≥ 60 years undergoing surgery for hip fracture occurring less than 24 hours after fracture Excluded: contraindication to regional anaesthesia (constitutional or acquired disorder of coagulation), sepsis, local infection of the puncture area, history of vascular femoral prosthetic surgery, prosthetic neuropathy, allergy to local anaesthetics, weight < 40 kg, respiratory failure, severe liver failure, brain injury associated with intracranial hypertension, uncontrolled epilepsy, simultaneous treatment with monoamine oxidase inhibitor, persons not affiliated with a health insurance plan Type of fracture: hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 12 months |
| Interventions |
Intervention: continuous femoral nerve block (N = 157) Comparator: no block (N = 157) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 12 July 2012 Study start date: July 2012 Study completion date: July 2016 Last update posted: 17 August 2016 |
| Contact information | Vincent Compere |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Cong 2016.
| Study name | Nerve block anesthesia and general anesthesia: influence on postoperative cognitive dysfunction after hip arthroplasty of aged patients with femoral neck fracture (a randomized controlled trial) |
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Shanghai 10th Hospital, Shanghai, China Data collection: 1 June 2017 to 1 October 2019 Funding: departmental/institutional Registration: ChiCTR‐INR‐16009481 |
| Participants | 100 participants between 60 and 80 years of age with normal mental status and unilateral hip fracture undergoing hip arthroplasty Excluded: severe respiratory disease, preoperative cognitive dysfunction Type of fracture: femoral neck fracture Anaesthetic technique for surgery: to be determined Surgical technique: hip arthroplasty Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 3 months |
| Interventions |
Intervention 1: nerve block plus enhanced recovery protocol (N = 25) Intervention 2: nerve block without enhanced recovery protocol (N = 25) Comparator 1: no block plus general anaesthesia (N = 25) Comparator 2: no block and no general anaesthesia (N = 25) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 18 October 2016 Study start date: to be determined Study completion date: to be determined Last update posted: 18 April 2017 |
| Contact information | Ruijun Cong |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Dhimar 2017.
| Study name | Analgesic effect provided by femoral nerve block versus intravenous fentanyl prior to positioning for subarachnoid block in patients with fracture femur |
| Methods | Parallel RCT, open label Approved by the ethics committee and informed consent obtained Site: Medical College and SSG Hospital, Vadodara, India Data collection: to be determined Funding: to be determined Registration: retrospectively registered 4 October 2017 |
| Participants | 60 ASA I to III participants posted for fracture surgery under subarachnoid block; the exact site of fracture is not specified Excluded: contraindications to subarachnoid block; allergy to amide local anaesthetics or fentanyl; history of drug or alcohol abuse; morbid obesity (body mass index > 29 kg/m2); comorbid condition such as diabetes, hypertension, bronchial asthma, chronic pulmonary obstructive disease; neurological or musculoskeletal disease; multiple fractures; refusal or inability to understand visual analogue pain scale score; use of analgesics 8 hours before performance of subarachnoid block Type of fracture: femur fracture Anaesthetic technique for surgery: spinal anaesthesia Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 90 minutes |
| Interventions |
Intervention: femoral nerve block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 5 November 2019 Study start date: 12 May 2015 Study completion date: to be determined Last update posted: 5 November 2019 |
| Contact information | Dr Aditi A Dhimar |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Diakomi 2015.
| Study name | Fascia iliaca compartment block in acute and chronic pain management in hip fracture patients |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: Asklepieion General Hospital Athens, Voula, Greece Data collection: June 2015 to March 2018 Funding: to be determined Registration: NCT02479828 |
| Participants | 198 ASA I to III participants from 18 to 90 years old with intertrochanteric femur or femoral neck fracture Excluded: existing pain in hip joint to be operated, cognitive or mental disorder, administration of analgesic drugs before surgery, contraindications of spinal anaesthesia, refusal to participate in the study Type of fracture: to be determined Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 6 months |
| Interventions |
Intervention: fascia iliaca compartment block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 24 June 2015 Study start date: June 2015 Study completion date: January 2018 Last update posted: 12 March 2019 |
| Contact information | Maria Diakomi |
| Notes | Conflict of interest: to be determined DOI: to be determined |
El Sharkawy 2016.
| Study name | Fascia iliaca compartment block for proximal‐end femur fractures |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: Mansoura University, Mansoura City, Egypt Data collection: to be determined Funding: to be determined Registration: retrospectively registered NCT02696915 |
| Participants | 60 ASA physical status I to III participants scheduled for fixation of proximal end femur fracture Excluded: patients who refused, morbid obesity (body mass index > 40 kg/m²), bleeding diathesis, previous femoral bypass surgery, inguinal hernia, inflammation/infection over injection site, peripheral neuropathy, allergy to local anaesthetic agents, severely altered consciousness level, psychiatric disorder, polytrauma Type of fracture: proximal end femur fracture Anaesthetic technique for surgery: spinal anaesthesia Surgical technique: to be determined Mean age: (range ) to be determined Percentage female: % to be determined Length of follow‐up: 24 hours |
| Interventions |
Intervention: iliaca compartment block Comparator: sham block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 2 March 2016 Study start date: January 2015 Study completion date: August 2015 Last update posted: 8 March 2016 |
| Contact information | Reem A El Sharkawy |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Kulkarni 2018.
| Study name | USG guided fascia iliaca compartment block for post operative analgesia in proximal femur fracture |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: MGM Medical College and Hospital, Navi Mumbai, India Data collection: to be determined Funding: to be determined Registration: CTRI/2018/12/016679 |
| Participants | 128 ASA I to III participants between 50 and 80 years of age undergoing proximal femur fracture surgery requiring spinal anaesthesia Excluded: patients who refused, bleeding diathesis, inguinal hernia, inflammation/infection over injection site, allergy to local anaesthetic agents used, altered consciousness level, psychiatric disorder, polytrauma, morbid obesity Type of fracture: proximal femur fracture Anaesthetic technique for surgery: spinal anaesthesia Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 24 hours |
| Interventions |
Intervention: fascia iliaca compartment block (N = 64) Comparator: no block (N = 64) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 14 December 2018 Study start date: 20 December 2018 Study completion date: to be determined Last update posted: 5 November 2019 |
| Contact information | Dr Sanhita Jiten Kulkarni |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Levins 2006.
| Study name | Intra‐ and post‐operative analgesia for patients undergoing surgery for hip fracture ‐ role of fascia iliaca compartment block |
| Methods | Parallel RCT, double‐blind (participants and caregivers) Approved by the ethics committee and informed consent obtained Site: Selly Oak Hospital, Birmingham, UK Data collection: to be determined Funding: governmental Registration: retrospectively registered ISRCTN75659782 |
| Participants | 40 adult participants of ASA I to III admitted to Selly Oak Hospital with hip fracture and scheduled for fixation will be recruited after consent is obtained Exclusion criteria: dementia/confusion, preoperative chest infection and/or poor respiratory function, temperature ≥ 38° C, white cell count > 11,000/mm3, respiratory rate > 25/min, auscultation and/or chest X‐ray evidence, SpO2 < 90% on air, congestive cardiac failure, bed‐bound or use of ≥ 2 aids for mobilization pre‐fracture, malignancy, coagulopathy, known or suspected allergy to ropivacaine and/or morphine, local infection at site where the block is to be performed, refusal of permission to approach general practitioner Type of fracture: hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 24 hours |
| Interventions |
Intervention: fascia iliaca compartment block (N = 20) Comparator: morphine (N = 20) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 28 September 2007 Study start date: 4 April 2006 Study completion date: 4 April 2007 Last update posted: 12 October 2017 |
| Contact information | FA Levins, UK |
| Notes | Conflict of interest: to be determined DOI 10.1186 |
Li 2018.
| Study name | Effect of continuous lumbar plexus block combined with dexmedetomidine on postoperative delirium in elderly patients with hip fractures: a prospective, randomized controlled trial |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: Shanghai General Hospital, China Data collection: to be determined Funding: departmental/institutional Registration: ChiCTR1900021549 |
| Participants | 280 ASA I to III participants ≥ 65 years of age with hip fracture undergoing surgery Excluded: compound injury (multiple fractures, combined with trauma of the head, chest, abdomen, pelvis, and parts other than the hip), contraindications for lumbar plexus block (puncture site infection, peripheral neuropathy, local anaesthetic allergy, etc.), coexisting neurological disease (Alzheimer's disease, vascular dementia, and other diseases that affect cognitive function), allergy to the test drug, participated in other clinical trials Type of fracture: hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age (range ): to be determined Percentage female: % to be determined Length of follow‐up: 7 days |
| Interventions |
Intervention 1: continuous posterior lumbar plexus block and dexmedetomidine (N = 70) Intervention 2: continuous posterior lumbar plexus block and no dexmedetomidine (N = 70) Comparator 1: no block and dexmedetomidine (N = 70) Comparator 2: no block and no dexmedetomidine(N = 70) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 27 February 2019 Study start date: 15 March 2019 Study completion date: 15 March 2021 Last update posted: 27 February 2019 |
| Contact information | Jin Bao LI, Jian Hai Zhang |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Luo 2019.
| Study name | Effects of ultrasound‐guided continuous modified fascia iliaca compartment block for postoperative recovery in elderly patients with femoral fracture |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: The First Affiliated Hospital of Nanchang University, Jiangxi, China Data collection: 1 May 2010 to 1 December 2019 Funding: to be determined Registration: ChiCTR1900022595 |
| Participants | 60 ASA I to III participants between 60 and 85 years of age undergoing elective surgery for unilateral femoral fracture under spinal anaesthesia Excluded: fractures in other sites, pulmonary infection or lower extremity venous thrombosis before surgery, severe puncture site infection or damage, psychiatric or neurological disorder, history of coagulation dysfunction or haemorrhagic disease, severe liver dysfunction (≥ Child‐Pugh level 3), severe renal dysfunction (serum creatinine ≥ 177μmol/L) Type of fracture: femoral fracture Anaesthetic technique for surgery: spinal anaesthesia Surgical technique: to be determined Mean age: to be determined Percentage female: to be determined Length of follow‐up: 48 hours |
| Interventions | Intervention: continuous modified fascia iliaca compartment block (N = 30) Comparator: no block (N = 30) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 18 April 2019 Study start date: 1 May 2019 Study completion date: 1 December 2019 Last update posted: 18 April 2019 |
| Contact information | Foquan Luo |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Mathijssen 2015.
| Study name | Femoral nerve blockage in proximal femoral fractures in patients 65 years of age or older, a randomised controlled trial |
| Methods | Parallel RCT, double‐blind Approved by the ethics committee and informed consent obtained Site: Reinier de Graaf Hospital, Delft, The Netherlands Data collection: to be determined Funding: to be determined Registration: EudraCT Number: 2015‐004119‐19 |
| Participants | 84 participants with proximal femoral fracture, normal lower extremity anatomy and neurovascular examination, pain score ≥ 4 at admission, 65 years of age or older Excluded: cognitive impairment, previously diagnosed with dementia or Mini Mental score ≤ 22, delirium at inclusion, no good understanding of the Dutch language, known hypersensitivity to local anaesthetics or morphine, multiple trauma, pre‐injury use of opioids, pre‐injury bedridden or wheelchair‐bound Type of fracture: proximal femoral fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: in hospital |
| Interventions |
Intervention: repeated doses femoral nerve block Comparator: sham block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 22 February 2016 Study start date: 25 April 2016 Study completion date: to be determined Last update posted: 9 May 2016 |
| Contact information | Nina Mathijssen, The Netherlands |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Nguyen 2018.
| Study name | Impact of fascia iliaca block in hip fracture patients |
| Methods | Parallel RCT, open label Approved by the ethics committee and informed consent obtained Site: Texas Tech University Health Sciences Center, El Paso, TX, USA Data collection: Febuary 2018 to May 2019 Funding: to be determined Registration: NCT03525977 |
| Participants | 97 participants from 18 to 99 years of age with femoral neck and intertrochanteric hip fractures requiring surgery Excluded: polytrauma; pathological fracture; required revision procedure; long‐term opioid use; clinical status that precludes verbal pain assessment such as dementia; head injury; unwillingness to participate Type of fracture: femoral neck and intertrochanteric hip fractures Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 2 days |
| Interventions |
Intervention: fascia compartment iliaca block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 16 May 2018 Study start date: 20 February 2018 Study completion date: 1 May 2019 Last update posted: 27 May 2019 |
| Contact information | Mai P Nguyen, USA |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Park 2009.
| Study name | Ultrasound guided femoral nerve block using 1% ropivacaine as a method of pain control in patients who present to emergency with a fractured hip |
| Methods | Parallel RCT, open label Approved by the ethics committee and informed consent obtained Site: St Vincent's Hospital, New South Wales, Australia Data collection: to be determined Funding: institutional/departmental Registration: retrospectively registered; ACTRN12609000526279 |
| Participants | 46 participants 18 years of age and older with radiologically proven fractured neck of femur Excluded: pregnant or lactating; allergy to ropivacaine, paracetamol, or morphine; anticogulated patients; those with significant coagulation abnormalities; localized injection site infection; neurological deficits in distribution of the femoral nerve; severe hepatic disease; unable to give consent themselves; history of heart block; on amiodarone; acute cardiac event in the last 3 months Type of fracture: femoral neck fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: to be determined Percentage female: to be determined Length of follow‐up: 24 hours |
| Interventions | Intervention: femoral nerve block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 10 June 2009 Study start date: 4 April 2009 Study completion date: to be determined Last update posted: 6 July 2012 |
| Contact information | Dr Edmond Park |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Postma 2017.
| Study name | Morphine use in the fascia iliaca compartment block with ultrasound guidance (MORFICUS) |
| Methods | Parallel RCT, with quadruple masking (participant, care provider, investigator, outcomes assessor) Approved by the ethics committee and informed consents obtained Site: Zuyderland Medisch Centrum, Heerlen, The Netherlands Data collection: 28 January 2019 to 1 February 2020 Funding: departmental/institutional plus industry Registration: EUCTR2016‐004698‐42‐NL 2016 |
| Participants | 120 participants ≥ 18 years of age diagnosed with a proximal femoral fracture (femoral neck, trochanteric and subtrochanteric femoral fracture) upon arrival at the emergency department Excluded: no informed consent, skin infection at injection site(s), morphine allergy, levobupivacaïne allergy, operation within an hour after admission, inability to understand and quantify pain on an NRS scale, history of dementia, neurological deficit of fractured leg upon arrival at the emergency department, trauma with multiple fractures (more than 1), risk of compartment syndrome of ipsilateral lower leg, proximal femoral fracture with other definitive treatment than operation, transfer to another hospital, actual morphine use, distracting pain in other location than hip, pregnancy, no physician/nurse available for procedure, body mass index > 40, saturation < 90%, previously unreported hypotension (systolic blood pressure < 100 mmHg) or ASA IV or higher Type of fracture: femoral neck, trochanteric or subtrochanteric femoral fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 30 days |
| Interventions |
Intervention: fascia iliaca compartment block Comparator: sham block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 4 January 2017 Study start date: 29 May 2017 Study completion date: 1 February 2020 Last update posted: 26 February 2019 |
| Contact information | Rory O'Connor, Sanne Postma Sponsor's protocol code number 10102016 |
| Notes | Conflict of interest: sponsored by industry DOI: to be determined |
Qiu 2018.
| Study name | A randomized controlled trial for the efficacy of early analgesia by continuous fascia block under ultrasound guidance for elderly patients with hip fracture |
| Methods | Parallel RCT Approved by the ethics committee and informed consents obtained Site: Fujian Provincial Hospital, Fujan, China Data collection: 1 October 2018 to 30 June 2019 Funding: departmental/institutional Registration: ChiCTR1800018604 |
| Participants | 40 ASA I to III participants ≥ 65 years of age with X‐ray‐confirmed unilateral femoral neck fracture or intertrochanteric fracture; body mass index 18.5 to 30 kilograms per square meter Excluded: history of abnormal surgical anaesthesia recovery with serious injuries combined with other important organs, history of acute inflammation of the respiratory tract within 2 weeks, neuromuscular disease and mental illness, suspected abuse of narcotic analgesics or sedatives, known to be allergic to local anaesthetics or opioids, do not cooperate and cannot communicate Type of fracture: femoral neck fracture or intertrochanteric fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: in hospital |
| Interventions |
Intervention: fascia iliaca compartment block (N = 20) Comparator: no block (N = 20) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 30 September 2018 Study start date: 1 October 2018 Study completion date: to be determined Last update posted: 30 September 2018 |
| Contact information | Chun‐Hua Qiu |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Ridderikhof 2015.
| Study name | A multicenter randomized controlled trial in elderly patients with hip fractures comparing continuous fascia iliaca compartment block to systemic opioids and its effect on delirium occurrence |
| Methods | Parallel RCT, open label Approved by the ethics committee and informed consent obtained Site: Academisch Medisch Centrum ‐ Universiteit van Amsterdam, The Netherlands Data collection: May 2016 to December 2021 Funding: governmental Registration: NCT02689024 |
| Participants | 340 participants ≥ 55 years of age with radiographically confirmed hip fracture Excluded: multiple injuries (polytrauma patients), previous adverse reaction or known allergy to local anaesthetics or opioids or paracetamol, skin infection in proximity of injection site, delirious state at presentation in the emergency department Type of fracture: hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 3 months |
| Interventions |
Intervention: compartment fascia iliaca block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 23 February 2016 Study start date: May 2016 Study completion date: April 2022 Last update posted: 27 March 2019 |
| Contact information | Milan Ridderikhof, The Netherlands |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Saga 2019.
| Study name | Nurse led ultrasound guided femoral nerve block in the emergency department (URGENT) |
| Methods | Parallel RCT (open label) Approved by the ethics committee and informed consent obtained Site: University College of Southeast Norway Data collection: 15 December 2019 to 31 December 2022 Funding: departmental/institutional Registration: NCT04145752 |
| Participants | 50 ASA I to IV participants 18 to 110 years of age with radiologically confirmed hip fracture Excluded: dementia, known allergy to local anaesthetic used in femoral nerve block, anticoagulated or using platelet inhibitors (acetylsalicylic acid and dipyridamole are allowed), recent (last 2 hours) international normalized ratio > 1.5, pregnant women, < 18 years of age, severe head injury that leads to significant loss of consciousness (Glasgow coma score < 12), > 10 mg morphine administered pre‐hospital, skin lesion/infection at block site, admitted with other suspected or verified fracture except small fractures in hands and feet Type of fracture: hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: in hospital |
| Interventions | Intervention: femoral nerve block (N = 25) Comparator: no block (N =25) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 31 October 2019 Study start date: 15 December 2019 Study completion date: 31 December 2022 Last update posted: 31 October 2019 |
| Contact information | Espen Lindholm, Tomm Bernklev |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Sahiti 2019.
| Study name | A randomized control study to evaluate the efficacy of ultrasound guided pre‐emptive fascia iliaca compartment block for postoperative analgesia in femur and hip fracture surgeries |
| Methods | Parallel RCT, outcome assessor blinded Approved by the ethics committee and informed consent obtained Site: SRM Medical College Hospital and Research Centre, Tamil Nadu, India Data collection: to be determined Funding: to be determined Registration: CTRI/2019/04/018488 |
| Participants | 60 ASA I to III participants 18 to 75 years of age with body mass index between 18.5 and 25 kg/m2 admitted for elective femur and hip fracture surgeries under spinal anaesthesia Excluded: ASA IV and above, allergy to local anaesthetics, coagulation abnormalities Type of fracture: hip fracture Anaesthetic technique for surgery: spinal anaesthesia Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 24 hours |
| Interventions |
Intervention: fascia iliaca compartment block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 8 April 2019 Study start date: 01 May 2019 Study completion date: to be determined Last update posted: 5 November 2019 |
| Contact information | Tomurthy Sahithi |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Shah 2016.
| Study name | Analgesia for positioning patient with femur fracture for spinal anaesthesia |
| Methods | Parallel RCT, single‐blinded Approved by the ethics committee and informed consent obtained Site: Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia Data collection: October 2015 to December 2016 Funding: to be determined Registration: retrospectively registered; NCT02983344 |
| Participants | 24 ASA I or II participants between 60 and 85 years of age undergoing elective surgery for repair of unilateral, single femoral fracture under spinal anaesthesia Excluded: contraindication to spinal anaesthesia, known hypersensitivity or contraindication to medication used in this study, morbid obesity (body mass index > 35 kg/m2), infection at the intended site of administration of fascia iliaca compartment block, impaired cognitive function Type of fracture: femoral neck or femoral shaft fracture Anaesthetic technique for surgery: spinal anaesthesia Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 24 hours |
| Interventions |
Intervention: fascia iliaca compartment block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 6 December 2016 Study start date: October 2015 Study completion date: December 2016 Last update posted: 6 September 2017 |
| Contact information | Dr Aida Mastura Mohd Shah |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Tsui 2015.
| Study name | Use of pre‐operative nerve blocks in older patients with hip fracture: a pilot study |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: University of Alberta, Canada Data collection: June 2015 to December 2016 Funding: to be determined Registration: NCT02450045 |
| Participants | 75 participants ≥ 65 years or age, ambulatory pre‐fracture, who sustained a low‐energy hip fracture (i.e. fall from standing), have a Mini Mental Status Examination score ≥ 13 (moderate dementia), and received consent to participate in the study Excluded: admitted to hospital more than 30 hours from injury, regular use of opiate medications, Confusion Assessment Method (CAM) test not performed within 6 hours of ward admission, known allergy to local anaesthetic Type of fracture: low‐energy hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 5 days |
| Interventions |
Intervention: femoral nerve block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 21 May 2015 Study start date: June 2015 Study completion date: December 2016 Last update posted: 26 October 2016 |
| Contact information | Ban Tsui |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Winso 2009.
| Study name | Femoral nerve blockade in hip fracture patients: a randomised controlled trial |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: Umea University, Umea, Sweden Data collection: 30 March 2009 to 31 December 2010 Funding: governmental Registration: retrospectively registered; ISRCTN46653818 |
| Participants | 250 participants ≥ 70 years of age with hip fracture Excluded: local infection, allergic to local anaesthesia, dying, pathological hip fracture Type of fracture: hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: 5 days |
| Interventions |
Intervention: femoral nerve block Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 5 May 2009 Study start date: 30 March 2009 Study completion date: 31 December 2010 Last update posted: 13 January 2015 |
| Contact information | Professor Ola Winso |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Xi 2014.
| Study name | A research of postoperative cognitive dysfunction of elderly patients after general anesthesia combined with nerve block or not for femoral fracture surgery |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: Shanghai Ninth People's Hospital, China Data collection: to be determined Funding: departmental/institutional Registration: ChiCTR‐IPR‐14005641 |
| Participants | 70 participants ≥ 70 years of age undergoing femoral fracture surgery Excluded: anaesthesia within past 180 days, baseline Mini Mental State Examination score < 17, Barthel Index of Activities of Daily Living < 70, preexisting neuropsychiatric disease, nable to speak Chinese Type of fracture: to be determined Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age (range 70 to 95): to be determined Percentage female: % to be determined Length of follow‐up: no information |
| Interventions |
Intervention: nerve block (N = 35) Comparator: no nerve block (N = 35) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 10 December 2014 Study start date: 1 January 1990 (date of ethics committee approval 26 August 2013) Study completion date: to be determined Last update posted: 18 April 2017 |
| Contact information | Siwei Xi |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Xuesheng 2019.
| Study name | Comparison of combined lumbar and sacral plexus block with low general anesthesia versus spinal anaesthesia on postoperative outcomes in elderly patients undergoing hip fracture surgery |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: The First Affiliated Hospital of Anhui Medical University, China Data collection: 12 August 2019 to May 2020 Funding: institutional/departmental Registration: ChiCTR1900025113 |
| Participants | 120 ASA I to IV participants 65 years of age or older scheduled for elective hip fracture surgery Excluded: dementia or severe cognitive dysfunction, unstable mental state or mental disease, psychotropic drugs, opioid abuse, delirium, history of delirium, anaesthesia and surgery within 6 months, visual or auditory language barrier affecting cognitive assessment, bilateral hip or other fracture surgery at the same time, cerebrovascular accident within the last 3 months, scheduled to receive prosthesis surgery Type of fracture: hip fracture Anaesthetic technique for surgery: general anaesthesia for the intervention group; spinal anaesthesia for the comparator group Surgical technique: fixation Mean age: to be determined Percentage female: to be determined Length of follow‐up: 30 days |
| Interventions | Intervention: lumbosacral plexus block (N = 60) Comparator: no peripheral nerve block (N = 60) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 12 August 2019 Study start date: 12 August 2019 Study completion date: May 2020 Last update posted: 12 August 2019 |
| Contact information | Liu Xuesheng, Fang Panpan |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Yuan 2017.
| Study name | Efficacy of perioperative advanced protocol enhance recovery of elderly patients suffering limb fracture: a clinical study |
| Methods | Parallel RCT Approved by the ethics committee and informed consent obtained Site: Shanghai Changzheng Hospital, China Data collection: to be determined Funding: to be determined Registration: ChiCTR‐IOR‐17012042 |
| Participants | 120 ASA II to III participants 60 to 90 years of age with simple hip fracture and undergoing surgery Excluded: long‐term endocrine system disease; severe diabetic complications (diabetic ketoacidosis, hyperosmolar coma, diabetic nephropathy, macrovascular disease); severe gastrointestinal ulcer; blood system disease; severe liver and kidney disease (such as ALT, AST, bilirubin, and so on, more than twice the upper limit of normal; creatinine clearance rate < 30 mL/min); non‐steroidal anti‐inflammatory drug allergy history; aspirin allergy history; cerebrovascular accident within recent 3 months such as stroke, transient ischaemic attack, etc.; serious psychological problem; long psychiatric history or psychiatric drug history; drug addiction; allergy to any of the analgesic drugs Type of fracture: hip fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: (range ): to be determined Percentage female: % to be determined Length of follow‐up: no information |
| Interventions |
Intervention: femoral nerve block before surgery and fascia iliaca block after surgery Comparator: no block |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 10 July 2017 Study start date: 1 January 2017 (approved by ethics committee 26 August 2013) Study completion date: 30 December 2019 Last update posted: 24 July 2017 |
| Contact information | Hongbin Yuan, Weiwei Li |
| Notes | Conflict of interest: to be determined DOI: to be determined |
Yun 2018.
| Study name | Clinical study on analgesia of Top‐Tql lumbar quadratus muscle block induced by ultrasound‐guided after PFNA surgery for senile femoral trochanteric fracture |
| Methods | Parallel RCT
Approved by the ethics committee and informed consent obtained
Site: Xiamen 5th Hospital, Fujian, China
Data collection: 1 October 2018 to 1 December 2020 Funding: institutional/departmental Registration: ChiCTR1800016421 |
| Participants | 90 participants over 65 years old with confirmed femoral trochanteric fracture scheduled for internal fixation Excluded: local anaesthesia allergy, puncture site infection, severe cardiovascular disease or cerebrovascular complications, severe cognitive dysfunction Type of fracture: trochanteric fracture Anaesthetic technique for surgery: to be determined Surgical technique: to be determined Mean age: to be determined Percentage female: to be determined Length of follow‐up: 72 hours |
| Interventions | Intervention: quadratus lumborum plexus block (N = 45) Comparator: no block (N = 45) |
| Outcomes | Relevant to this review.
Not relevant to this review.
|
| Starting date | First posted: 1 June 2018 Study start date: 1 January 2018 (approved by ethics committee on 26 August 2013) Study completion date: 1 December 2020 Last update posted: 1 June 2018 |
| Contact information | Wang Yun |
| Notes | Conflict of interest: to be determined DOI: to be determined |
AMTS: Abbreviated 10‐point Mental Test Score.
ASA: American Society of Anaesthesiologists physical status.
C: Celsius.
CAM Questionnaire: Confusion Assessment Method.
EQ‐5D or EUROQOL: score for measurement of health‐related quality of life.
G: gram.
ICD‐9: list of codes for International Statistical Classification of Diseases and Related Health Problems.
IV: intravenous.
kg: kilogram.
kg/m2: kilogram per square metre.
mm: millimetre.
mmHg: millimetre of mercury.
MSMC ED: Maimonides Medical Center emergency department.
n: number.
NHS: Nottingham University Hospitals.
NRS: numerical rating scale.
OMC: orientation‐memory‐concentration.
RCT: randomized controlled trial.
RfPB: Research for Patient Benefit.
Differences between protocol and review
For this update, we made the following changes from the 2017 version.
Instead of using the 'Risk of bias' tool, as we did in the 2017 version, we are now using the 'Risk of bias‐2' (RoB 2) tool.
For this update, we kept only the outcomes included in the summary of findings table of the previous version.
Contributions of authors
Joanne Guay: screened abstracts, searched websites, checked reference lists for new articles, selected new articles, retrieved relevant articles, graded articles for risk of bias, extracted data, analysed data, interpreted results, rated certainty of evidence, and drafted the update.
Sandra Kopp: screened abstracts, selected new articles, graded articles for risk of bias, extracted data, interpreted results, rated certainty of evidence, and drafted the update.
The contributions listed above refer to the 2020 version only. Please see previously published versions of this review for contributions of authors of earlier versions of this review.
Sources of support
Internal sources
-
University of Sherbrooke, Canada
University of Sherbrooke granted access to electronic databases and medical journals.
-
University of Quebec in Abitibi‐Temiscamingue, Canada
Universiuty of Quebec in Abitibi‐Temiscamingue granted access to electronic databases and medical journals.
-
Laval University, Quebec City, Quebec, Canada, Canada
Laval University granted access to electronic databases and medical journals.
External sources
No sources of support supplied
Declarations of interest
Joanne Guay: no conflict of interest.
Sandra Kopp: no conflict of interest.
Edited (no change to conclusions)
References
References to studies included in this review
Albrecht 2014 {published and unpublished data}
- Albrecht E. Information on our trial [personal communication]. Email to: J Guay 3 December 2018.
- Albrecht E. Fascia iliaca block in the emergency department for analgesia after femoral neck fracture. Available at https://clinicaltrials.gov/ct2/show/NCT02433548 2014:Accessed December 2019. [CENTRAL: CN-01506191] [PMID: 10.1002/central/CN-01506191/full] [DOI]
- Albrecht E. Information on our trial [personal communication]. Email to: J Guay 6 January 2020.
- Pasquier M, Taffe P, Hugli O, Borens O, Kirkham K R, Albrecht E. Fascia iliaca block in the emergency department for hip fracture: a randomized, controlled, double-blind trial. BMC Geriatrics 2019;19(1):180. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Altermatt 2013 {published and unpublished data}
- Altermatt FR, Echevarria GC, la Fuente RF, Baeza R, Ferrada M, la Cuadra JC, et al. Perioperative lumbar plexus block and cardiac ischemia in patients with hip fracture: randomized clinical trial [Bloqueio perioperatorio do plexo lombar e isquemia cardiaca em pacientes com fratura de quadril: ensaio clinico randomizado]. Revista Brasileira de Anestesiologia 2018;68(5):484-91. [CENTRAL: CN-01617336] [DOI: 10.1016/j.bjan.2018.03.003] [EMBASE: 2000949539] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altermatt FR. Additional information for our trial [personal communication]. Email to J Guay 26 May 2015.
- Altermatt RF, De la Fuente RF, Echevarría GC, Baeza R, Ferrada M, De la Fuente N, et al. Evaluation of the effect of perioperative continuous lumbar plexus block upon the incidence of Ischaemic cardiovascular events in elderly patients with hip fracture. Regional Anesthesia and Pain Medicine 2013;38(5 Suppl 1):E182. [Google Scholar]
- Clinical Trialgov. Lumbar plexus block upon the incidence of ischemic cardiovascular events in elderly patients with hip fracture [2013]. Available at https://clinicaltrials.gov/ct2/results?cond=&term=NCT01961895&cntry=&state=&city=&dist=:Accessed December 2019.
Antonopoulou 2006 {published data only}
- Antonopoulo E, Papaloannou K, Konstantinou G, Papadopoulos D, Karamoulas B, Molas TH. Continous femoral block in elderly patients with hip fractures. Regional Anesthesia and Pain Medicine 2006;31(5 Suppl 1):92. [Google Scholar]
Bang 2016 {published data only}
- Bang S, Chung J, Jeong J, Bak H, Kim D. Efficacy of ultrasound-guided fascia iliaca compartment block after hip hemiarthroplasty: a prospective, randomized trial. Medicine (Baltimore) 2016;95(39):e5018. [CENTRAL: CN-01263276] [DOI: 10.1097/MD.0000000000005018 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brownbridge 2018 {published data only}
- Brownbridge B, Yang C. Continuous fascia iliaca block for acute hip fractures. Available at https://clinicaltrials.gov/show/NCT03588689 2018. [CENTRAL: CN-01661154] [DOI: 10.1002/central/CN-01661154/full]] [DOI] [PubMed]
- Loessin V, ElZahabi A J, Brownbridge B, Bajwa J S. Continuous fascia iliaca block for acute hip fractures: a randomized-controlled pilot study. Canadian Journal of Anaesthesia 2019;66(10):1265-7. [CENTRAL: CN-01959471] [DOI: 10.1007/s12630-019-01428-2] [EMBASE: 628355678] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chudinov 1999 {published data only}
- Chudinov A, Berkenstadt H, Salai M, Cahana A, Perel A. Continuous psoas compartment block for anaesthesia and perioperative analgesia in patients with hip fractures. Regional Anesthesia and Pain Medicine 1999;24(6):563-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Chudinov A, Berkenstadt H, Salai M, Cahana A, Perel A. Continuous psoas compartment block for anesthesia and perioperative analgesia in patients with hip fractures. British Journal or Anaesthesia 1999;82(Suppl 1):111. [DOI] [PubMed] [Google Scholar]
Coad 1991 {published data only}
- Coad NR. Post-operative analgesia following femoral-neck surgery - a comparison between 3 in 1 femoral nerve block and lateral cutaneous nerve block. European Journal of Anaesthesiology 1991;8(4):287-90. [PMID: ] [PubMed] [Google Scholar]
Cuvillon 2007 {published data only}
- Cuvillon P, Ripart J, Debureaux S , Boisson C, Veyrat E, Mahamat A, et al. Analgesia after hip fracture repair in elderly patients: the effect of a continuous femoral nerve block: a prospective and randomised study [Analgésie postopératoire par cathéter femoral après fracture du col du fémur chez la personne agée: étude prospective randomisée]. Annales Françaises d' Anesthésie et de Réanimation 2007;26(1):2-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
De La Tabla 2010 {published and unpublished data}
- De La Tabla Gonzalez SRO, Angel Martinez ND, Mercedes Echevarra MS. Influence of perioperative pain treatment in postoperative morbidity in femur fractured patients over sixty-five years old: a randomised study. Regional Anesthesia and Pain Medicine 2010;35(5):469. [Google Scholar]
- Ortiz de la Tabla González R. Additional information for our trial [personal communication]. Email to J Guay 5 July 2015.
Deniz 2014 {published data only}
- Deniz S, Atim A, Kurklu M, Cayci T, Kurt E. Comparison of the postoperative analgesic efficacy of an ultrasound-guided fascia iliaca compartment block versus 3 in 1 block in hip prosthesis surgery. Agri 2014;26(4):151-7. [CENTRAL: CN-01201069] [PMID: ] [DOI] [PubMed] [Google Scholar]
Diakomi 2014 {published data only}
- Diakomi M, Gkliatis E, Papaioannou M, Polymenopoulou E, Papadopoulos P, Makris A. Fascia iliaca compartment block for positioning hip fracture patients for spinal anaesthesia: a randomised trial. Regional Anesthesia and Pain Medicine 2014;39(5 Suppl):ESRA1-0229. [DOI] [PubMed] [Google Scholar]
- Diakomi M, Papaioannou M, Mela A, Kouskouni E, Makris A. Preoperative fascia iliaca compartment block for positioning patients with hip fractures for central nervous blockade: a randomized trial. Regional Anesthesia and Pain Medicine 2014;39(5):394-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Diakomi M. Analgesia for positioning hip fracture patients for spinal anesthesia. Available at http://clinicaltrials.gov/ct2/show/NCT02037633?cond=NCT02037633&draw=2&rank=1 2014:Accessed December 2019.
Domac 2015 {published data only}
- Domac A, Kelsaka, Sarihasan B. The effect of preoperative fascia iliaca compartment block on postoperative analgesic use in patients with femoral fracture [Femur kiriti olan hastalarda preoperatif uygulanan fasia iliaka kompartman blotunun postoperatif analjezik tuketimine etkisi]. Anestezi Dergisi 2015;23(3):144-51. [CENTRAL: CN-01471885] [EMBASE: 2015379598] [Google Scholar]
Fletcher 2003 {published data only}
- Fletcher AK, Rigby AS, Heyes FL. Three-in-one femoral nerve block as analgesia for fractured neck of femur in the emergency department: a randomized, controlled trial. Annals of Emergency Medicine 2003;41(2):227-33. [PMID: ] [DOI] [PubMed] [Google Scholar]
Foss 2005a {published data only}
- Foss N. Fascia iliaca compartment blockade as analgesia for hip fractures in the acute phase. Available at https://clinicaltrials.gov/ct2/show/NCT00162630 2005:Accessed December 2019.
- Foss NB, Kristensen BB, Bundgaard M, Bak M, Heiring C, Virkelyst C, et al. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology 2007;106(4):773-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Foss NB. Information on our trial [personal communication]. Email to: J Guay 14 January 2020.
Gille 2006 {published and unpublished data}
- Gille J, Gille M, Gahr R, Wiedemann B. Acute pain management in proximal femoral fractures. Femoral nerve block (catheter technique) vs. systemic pain therapy using a clinic internal organisation model [Akutschmerztherapie bei patienten mit huftgelenknahen frakturen. N.-femoralis-katheter-analgesie vs. systemische schmerztherapie unter anwendung eines klinikinternen organisationsmodells]. Der Anaesthesist 2006;55(4):414-22. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gille J. Additional information for our trial [personal communication]. Email to M Parker 2006.
Godoy Monzon 2010 {published data only}
- Godoy Monzon D, Vazquez J, Jauregui JR, Iserson KV. Pain treatment in post-traumatic hip fracture in the elderly: regional block vs. systemic non-steroidal analgesics. International Journal of Emergency Medicine 2010;3(4):321-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godoy Monzon D. Information on our trial [personal communication]. Email to: J Guay 30 January 2020.
Graham 2008 {published data only}
- Graham CA, Baird K, McGuffie AC. A pilot randomised clinical trial of 3-in-1 femoral nerve block and intravenous morphine as primary analgesia for patients presenting to the emergency department with fractured hip. Hong Kong Journal of Emergency Medicine 2008;15(4):205-11. [EMBASE: 2008542025] [Google Scholar]
Gürtan Bölükbasi 2013 {published and unpublished data}
- Bolukbasi GE, Turhan CK, Can SO, Ozcelik M, Okten F. Comparison of the effects of ultrasound-guided fascia iliaca compartment block and remifentanil infusion on positional pain in patients undergoing hip fracture surgery under spinal anaesthesia. Regional Anesthesia and Pain Medicine 2013;38(5 Suppl 1):E182. [CENTRAL: 01061852] [Google Scholar]
- Turhan CK. Additional information for our trial [personal communication]. Email to J Guay 25 May 2015.
Haddad 1995 {published data only}
- Haddad FS, Williams RL. Femoral nerve block in extracapsular femoral neck fractures. Journal of Bone and Joint Surgery - British Volume 1995;77(6):922-3. [PMID: ] [PubMed] [Google Scholar]
Henderson 2008 {published data only}
- Henderson K, Akhtar S, Sandoval M, Siddiqui S, Todd K, Wirtner A. Femoral nerve block for pain management of hip fractures in the emergency department: preliminary results of a randomised,controlled trial. Annals of Emergency Medicine 2008;52(4):S164. [CRSREF: 3338724] [Google Scholar]
Hogg 2009 {published data only}ISRCTN07083722
- Hogg R. Comparison of fascia iliac compartment block with conventional sedation to facilitate the positioning of patients with fractured neck of femur for spinal anaesthesia and the effect of nerve blockade on post-operative pain and mobility: a randomised double-blind controlled study. http://isrctn.com/ISRCTN07083722 2009:Accessed December 2019.
- Hogg RMG, Lappin EL, StevensonM, Shields MO, Mirakhur RK. Comparison of fascia iliaca compartment block with conventional sedation to facilitate the positioning of patients with fractured neck of femur for spinal anaesthesia. European Journal of Anaesthesilogy 2010;27(Suppl 47):138-9. [CENTRAL: CN-01889719] [Google Scholar]
Hood 1991 {published data only}
- Hood G, Edbrooke DL, Gerrish SP. Postoperative analgesia after triple nerve block for fractured neck of femur. Anaesthesia 1991;46(2):138-40. [PMID: ] [DOI] [PubMed] [Google Scholar]
Jadon 2014 {published and unpublished data}
- Jadon A, Kedia SK, Dixit S, Chakraborty S. Comparative evaluation of femoral nerve block and intravenous fentanyl for positioning during spinal anaesthesia in surgery of femur fracture. Indian Journal of Anaesthesia 2014;58(6):705-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadon A. Additional information for our trial [personal communication]. Email to J Guay 22 March 2016.
Jang 2018 {published data only}
- Jang JS, Lee YH, Kandahar HK, Shrestha SK, Lee JS, Lee JK, et al. [Changes in the tumor necrosis factor-alpha level after an ultrasound-guided femoral nerve block in elderly patients with a hip fracture] [Alteracoes no nivel de TNF-alpha apos bloqueio do nervo femoral guiado por ultrassom em idosos com fratura de quadril.]. Revista Brasileira de Anestesiologia 2018;68(6):558-63. [CENTRAL: CN-01944091] [DOI: 10.1016/j.bjan.2018.03.004] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 1985 {published data only}
- Jones SF, White A. Analgesia following femoral neck surgery. Lateral cutaneous nerve block as an alternative to narcotics in the elderly. Anaesthesia 1985;40(7):682-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kullenberg 2004 {published data only}
- Kullenberg B, Ysberg B, Heilman M, Resch S. Femoral nerve block as pain relief in hip fracture. A good alternative in perioperative treatment proved by a prospective study [Femoralnervsblockad som smärtlindring vid höftfraktur. Bra alternativ i perioperativ behandlingsarsenal visar prospektiv studie. [Swedish]]. Lakartidningen 2004;101(24):2104-7. [PMID: ] [PubMed] [Google Scholar]
Landsting 2008 {published data only}2008‐004303‐59
- Landsting OL. Blocking the femoral nerve on patients with suspected hip fracture - does it work in clinically? [Blockad av femoralnerven till patienter med misstänkt höftfraktur – fungerar den i klinisk praxis?]. https://www.clinicaltrialsregister.eu/ctr-search/trial/2008-004303-59/SE 2008:Accessed December 2019. [CENTRAL: CN-01822205]
- Wennberg P, Moller M, Herlitz J, Kenne Sarenmalm E. Fascia iliaca compartment block as a preoperative analgesic in elderly patients with hip fractures - effects on cognition. BMC Geriatrics 2019;19(1):252. [CENTRAL: CN-01990793] [DOI: 10.1186/s12877-019-1266-0] [EMBASE: 629303148] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg P, Norlin R, Herlitz J, Sarenmalm E K, Moller M. Pre-operative pain management with nerve block in patients with hip fractures: a randomized, controlled trial. Journal of Orthopaedic and Trauma Nursing 2019;33:35-43. [CENTRAL: CN-01956019] [EMBASE: 627859303] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Wennberg P. Information on our trial [personal communication]. Email to: J Guay 5 January 2020.
Liebmann 2012 {published data only}
- Beaudoin F. Information on our trial [personal communication]. Email to: J Guay 5 January 2019.
- Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. Academic Emergency Medicine 2013;20(6):584-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Liebmann O, Beaudoin F. Ultrasound-guided femoral nerve blocks in elderly patients with hip fractures (FNB). Available at https://clinicaltrials.gov/ct2/show/NCT01701414?term=NCT01701414&draw=2&rank=1 2012:Accessed December 2019. [DOI] [PubMed]
Luger 2012 {published data only}
- Luger TJ, Kammerlander C, Benz M, Luger MF, Garoscio I. Peridural anesthesia or ultrasound-guided continuous 3-in-1 block: which is indicated for analgesia in very elderly patients with hip fracture in the emergency department? Geriatric Orthopaedic Surgery & Rehabilitation 2012;3(3):121-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ma 2018a {published data only}
- Ma Y H, Wu J, Jia B, Xue J X, Wang TL. Continuous fascia iliaca compartment block combined with oral analgesics for pre-operative pain control in elderly hip fracture patients. Zhonghua Yi Xue Za Zhi 2018;98(10):723-7. [CENTRAL: CN-01628679] [DOI: 10.3760/cma.j.issn.0376-2491.2018.10.002.] [PMID: ] [DOI] [PubMed] [Google Scholar]
Madabushi 2016 {published data only}
- Madabushi R, Rajappa GC, Thammanna PP, Lyer SS. Fascia iliaca block vs intravenous fentanyl as an analgesic technique before positioning for spinal anesthesia in patients undergoing surgery for femur fractures-a randomized trial. Journal of Clinical Anesthesia 2016;35:398-403. [DOI: 10.1016/j.jclinane.2016.09.014] [PMID: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Morrison 2008 {published data only}
- Dickman E, Pushkar I, Likourezos A, Todd K, Hwang U, Akhter S, et al. Erratum to "Ultrasound-guided nerve blocks for intracapsular and extracapsular hip fractures". The American Journal of Emergency Medicine 2016;34(9):1921. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Dickman E, Pushkar I, Likourezos A, Todd K, Hwang U, Akhter S, et al. Ultrasound-guided nerve blocks for intracapsular and extracapsular hip fractures. Academic Emergency Medicine 2015;22(5 Suppl 1):S133. [CENTRAL: CN-01080180] [EMBASE: 71878940] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickman E, Pushkar I, Likourezos A, Todd K, Hwang U, Akhter S, et al. Ultrasound-guided nerve blocks for intracapsular and extracapsular hip fractures. The American Journal of Emergency Medicine 2016;34(3):586-9. [CENTRAL: CN-01140859] [EMBASE: 608135846] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang U, Todd K, Dickman E, Akhtar S, Morrison S. Emergency department femoral nerve blocks for acute hip fracture pain: a randomized controlled trial. Journal of the American Geriatrics Society 2015;63(Suppl 1):S103. [EMBASE: 71856034] [Google Scholar]
- Morrison RS, Dickman E, Hwang U, Akhtar S, Ferguson T, Huang J, et al. Regional nerve blocks improve pain and functional outcomes in hip fracture: a randomized controlled trial. Journal of the American Geriatrics Society 2016;64(12):2433-9. [CENTRAL: CN-01382226] [EMBASE: 613487879] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison RS, Todd K. Improving pain and function in hip fracture. Available at https://clinicaltrials.gov/ct2/show/NCT00749489 2008:Accessed December 2019. [PMID: ]
- Todd K, Dickman E, Hwang U, Akhtar S, Morrison R. Emergency department femoral nerve blocks for acute hip fracture pain: a randomized controlled trial. The Journal of Pain 2015;16(4 Suppl 1):S68. [EMBASE: 71856817] [Google Scholar]
Mosaffa 2005 {published data only}
- Mosaffa F, Esmaelijah A, Khoshnevis H. Analgesia before performing a spinal block in the lateral decubitus position in patients with a femoral neck fracture: a comparison between fascia iliaca block and IV fentanyl. In: Regional Anesthesia and Pain Medicine. Vol. 30. Available at: https://rapm-bmj-com.ezproxy.usherbrooke.ca/content/30/Suppl_1/61.2: BMJ Journals, 2005:61 (A153). [CENTRAL: CN-01929454]
- Mosaffa F, Razavi S. A comparison between fascia iliaca block and IV fentanyl for analgesia before spinal block in the lateral decubitus position in femoral neck fracture. In: 5th World Congress—World Institute of Pain , editors(s). Pain Practice. Vol. 9. Available at: https://onlinelibrary-wiley-com.ezproxy.usherbrooke.ca/doi/pdfdirect/10.1111/j.1533-2500.2009.00267.x: Wiley, March 2009:PB200, Page 148.
Mouzopoulos 2009 {published data only}
- Mouzopoulos G, Vasiliadis G, Lasanianos N, Nikolaras G, Morakis E, Kaminaris M. Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study. Journal of Orthopaedics and Traumatology 2009;10(3):127-33. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murgue 2006 {published data only}
- Murgue D, Ehret B, Massacrier-Imbert S, Durand O, Gibaud F, Maakel A, et al. Equimolar nitrous oxide/oxygen combined with femoral nerve block for emergency analgesia of femoral neck fractures [Utilisation du mélange équimolaire de protoxyde d'azote/oxygène et du bloc fémoral pour la prise en charge antalgique des fractures du col du fémur dans un service d'urgences]. Journal Europeen Des Urgences (Jeur) 2006;19(1):9-14. [EMBASE: 2006161776] [Google Scholar]
Nie 2015 {published data only}
- Nie H, Yang YX, Wang Y, Liu Y, Zhao B, Luan B. Effects of continuous fascia iliaca compartment blocks for postoperative analgesia in hip fracture patients. Pain Research & Management 2015;20(4):210-2. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie H. Information on our trial [personal communication]. Email to: J Guay 5 September 2016.
Ranjit 2016 {published data only}
- Raghuraman MS, Ranjit S. Regarding "Ultrasound guided femoral nerve block to provide analgesia for positioning patients with femur fracture before subarachnoid block: comparison with intravenous fentanyl" in Kathmandu University Medical Journal 2016;54(2):125-9. Kathmandu University Medical Journal 2017;15(57):89-90. [PMID: ] [PubMed] [Google Scholar]
- Ranjit S, Pradhan BB. Ultrasound guided femoral nerve block to provide analgesia for positioning patients with femur fracture before subarachnoid block: comparison with intravenous fentanyl. Kathmandu University Medical Journal 2016;14(54):125-9. [CENTRAL: 01332705] [EMBASE: 614127239] [PMID: ] [PubMed] [Google Scholar]
Segado Jimenez 2009 {published data only}
- Segado Jimenez MI, Bayon Gago M, Arias Delgado J, Casas Garcia ML, Dominguez Hervella F, Lopez Perez A, et al. Efficacy of obturator and femoral cutaneous nerve blocks for postoperative analgesia in hip surgery [Eficacia del bloqueo de los nervios obturador y femorocutaneo para analgesia postoperatoria en cirugia de cadera]. Revista Espanola de Anestesiologia y Reanimacion 2009;56(10):590-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Spansberg 1996 {published data only}
- Spansberg NL, Anker-Moller E, Dahl JB, Schultz P, Christensen EF. The value of continuous blockade of the lumbar plexus as an adjunct to acetylsalicyclic acid for pain relief after surgery for femoral neck fractures. European Journal of Anaesthesiology 1996;13(4):410-2. [PMID: ] [DOI] [PubMed] [Google Scholar]
Szucs 2010 {published data only}
- Szucs S, Iohom G, O'Donnell B, Sajgalik P, Ahmad I, Salah N, et al. Analgesic efficacy of continuous femoral nerve block commenced prior to operative fixation of fractured neck of femur. Perioperative Medicine (London, England) 2012;1:4. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szucs S, Iohom G. Functional recovery following operative fixation of fractured neck of femur in the elderly. Regional Anesthesia and Pain Medicine 2010;35(5):Abstract 534. [Google Scholar]
- Szucs S, Sajgalik P, O’Donnell, Ahmad I, Iohom G. Analgesic efficacy of continuous femoral nerve block prior to operative fixation of fracture neck of femur. Anesthesia and Analgesia 2010;110(Suppl 1):S484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szucs S. Information on our trial [personal communication]. Email to: J Guay 14 January 2020.
Thompson 2019 {published data only}
- Thompson J, Long M, Rogers E, Pesso R, Galos D, Dengenis R C, et al. Fascia iliaca block decreases hip fracture postoperative opioid consumption: a prospective randomized controlled trial. Journal of Orthopaedic Trauma 2020;34(1):49-54. [DOI: 10.1097/BOT.0000000000001634] [EMBASE: 629204478] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tuncer 2003 {published data only}
- Tuncer S, Sert OA, Yosunkaya A, Mutlu M, Celik J, Okesli S. Patient-controlled femoral nerve analgesia versus patient-controlled intravenous analgesia for postoperative analgesia after trochanteric fracture repair. Acute Pain 2003;4(3-4):105-8. [CENTRAL: CN-00473759] [EMBASE: 2003155122] [Google Scholar]
Unneby 2017 {published data only}
- Unneby A, Svensson O, Gustafson Y, Olofsson B. Femoral nerve block in a representative sample of elderly people with hip fracture: A randomised controlled trial. Injury 2017;48(7):1542-9. [DOI: 10.1016/j.injury.2017.04.043] [PMID: ] [DOI] [PubMed] [Google Scholar]
Uysal 2018 {published data only}ACTRN12618000546257U1111‐1193‐6260
- Comparison of the effect of preoperative continue femoral nerve block and paracetamol administration on preoperative pain management and postoperative delirium incidence of geriatric patients scheduled for trochanteric femur fracture. https://anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12618000546257 2018:Accessed January 2020.
- Uysal AI, Altıparmak B, Yaşar E, Turan M, Canbek U, et al. The effects of early femoral nerve block intervention on preoperative pain management and incidence of postoperative delirium geriatric patients undergoing trochanteric femur fracture surgery: a randomized controlled trial. Ulus Travma Acil Cerrahi Derg 2020;26(1):109-14. [DOI: 10.14744/tjtes.2019.78002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wang 2015 {published data only}
- Ma Y, Wu J, Xue J, Lan F, Wang T. Ultrasound-guided continuous fascia iliaca compartment block for pre-operative pain control in very elderly patients with hip fracture: A randomized controlled trial. Experimental and Therapeutic Medicine 2018;16(3):1944-1952. [CENTRAL: CN-01629193] [DOI: 10.3892/etm.2018.6417] [EMBASE: 623399950] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang T-I, Ma Y-H. Effect of continuous fascia iliaca compartment block on preoperative cardiac and pulmonary events in elderly patients with hip fracture. http://www.chictr.org.cn/showproj.aspx?proj=12161 2015:Accessed December 2019.
White 1980 {published data only}
- White IWC, Chappell WA. Anaesthesia for surgical correction of fractured femoral neck. A comparison of three techniques. Anaesthesia 1980;35(11):1107-10. [PMID: ] [DOI] [PubMed] [Google Scholar]
Yamamoto 2016 {published data only}
- Yamamoto N, Danura T. Comparison of the postoperative analgesic efficacy of intravenous acetaminophen versus ultrasound-guided fascia iliaca compartment block for patients with proximal femoral fracture: a randomized controlled trial. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000024147 2016:Accessed December 2019. [CENTRAL: CN-01828954] [DOI: 10.1002/central/CN-01828954/full] [DOI]
- Yamamoto N, Sakura S, Noda T, Nishiyama A, Danura T, Matsui Y, et al. Comparison of the postoperative analgesic efficacies of intravenous acetaminophen and fascia iliaca compartment block in hip fracture surgery: a randomised controlled trial. Injury 2019;50(10):1689-1693. [CENTRAL: CN-01918126] [DOI: DOI: 10.1016/j.injury.2019.03.008] [EMBASE: 2001708250] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yang 2016 {published data only}
- Yang J. Ultrasound guided continuous fascia iliaca block for pain management in elder patients with hip fractures. Anesthesia and Analgesia 2016;123(3 Supplement 2):440-441. [CENTRAL: CN-01768433] [DOI: 10.1002/central/CN-01768433/full] [EMBASE: 612648909] [DOI] [Google Scholar]
Yun 2009 {published and unpublished data}
- Yun M, Han M, Park S, Kim S. Analgesia prior to spinal block in the lateral position in elderly patients with a femoral neck fracture: a comparison of fascia iliaca compartment block and intravenous alfentanil. European Journal of Anaesthesiology 2009;26(Suppl 45):8AP3-3. [Google Scholar]
- Yun M. Information on our trial [personal communication]. Email to: J Guay 14 January 2020.
- Yun MJ, Kim YH, Han MK, Kim JH, Hwang JW, Do SH. Analgesia before a spinal block for femoral neck fracture: fascia iliaca compartment block. Acta Anaesthesiologica Scandinavica 2009;53(10):1282-7. [CENTRAL: CN-00734383] [EMBASE: 355385327] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Yun MJ, Kim YH, Han MK, Kim JH, Hwang JW, Do SH. Analgesia before a spinal block for femoral neck fracture: fascia iliaca compartment block. Bone, Joint and Muscle Trauma 2009;53(10). [CENTRAL: 10.1002/central/CN-00847713/full] [DOI: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Akhtar 2015 {published data only}
- Akhtar Z, Allen C, Langton B, Watters H, Barker H, Raymond M, et al. The use of fascia iliaca block infusions in patients presenting with neck of femur fractures. European Geriatric Medicine 2015;6(S1):S146-S146. [EMBASE: 72037580] [Google Scholar]
Amini 2012 {published data only}IRCT201201158728N1
- Amini A, Khaledi AR. The effect of 3-in-1 block with bupivacaine 0.25% versus bupivacaine 0.25% plus 8 milligram dexamethaasone in acute pain control of patientsundergone hip nailing surgery. http: apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT201201158728N1 2012:Accessed January 2020.
Amiri 2012 {published data only}
- Amiri H R, Safari S, Makarem J, Rahimi M, Jahanshahi B. Comparison of combined femoral nerve block and spinal anesthesia with lumbar plexus block for postoperative analgesia in intertrochanteric fracture surgery. Anesthesiology and Pain Medicine 2012;2(1):32-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anaraki 2012 {published data only}
- Anaraki A, Mirzaei K. The effect of fascia iliaca compartment block versus gabapentin on postoperative pain and morphine consumption in femoral surgery, a prospective, randomized, double-blind study. Indian Journal of Pain 2014;28(2):111-6. [CENTRAL: CN-01870728] [DOI: 10.4103/0970-5333.132852] [DOI] [Google Scholar]
- Anaraki AN. The comparison between the effect of preemptive gabapentin and fascia iliaca block in reduction of postoperative pain of femoral shaft surgery. http://en.irct.ir/trial/1514:Accessed December 2019.
Aprato 2018 {published data only}
- Aprato A, Audisio A, Santoro A, Grosso E, Devivo S, Berardino M, et al. Fascia-iliaca compartment block vs intra-articular hip injection for preoperative pain management in intracapsular hip fractures: A blind, randomized, controlled trial. Injury 2018;49(12):2203-8. [CENTRAL: CN-01652210] [EMBASE: 2001141345] [PMID: ] [DOI] [PubMed] [Google Scholar]
Arsoy 2017 {published data only}
- Arsoy D, Huddleston JI 3rd, Amanatullah DF, Giori NJ, Maloney WJ, Goodman SB. Femoral nerve catheters improve home disposition and pain in hip fracture patients treated with total hip arthroplasty. The Journal of Arthroplasty 2017;32(11):3434-7. [DOI: 10.1016/j.arth.2017.05.047] [PMID: 28641968] [DOI] [PubMed] [Google Scholar]
Arsoy 2017a {published data only}
- Arsoy D, Gardner MJ, Amanatullah DF, Huddleston JI 3rd, Goodman SB, Maloney WJ, et al. Continuous femoral nerve catheters decrease opioid-related side effects and increase home disposition rates among geriatric hip fracture patients. Journal of Orthopaedic Trauma 2017;31(6):e186-9. [DOI: 10.1097/BOT.0000000000000854] [PMID: ] [DOI] [PubMed] [Google Scholar]
Barnes 2019 {published data only}
- Barnes M, Haber B, Flannigan M J. Efficacy of ultrasound-guided fascia iliaca compartment block for elderly hip fracture patients. Academic Emergency Medicine 2019;26(Suppl 1):S234. [Google Scholar]
Beaudoin 2010 {published data only}
- Beaudoin FL, Nagdev A, Merchant RC, Becker BM. Ultrasound-guided femoral nerve blocks in elderly patients with hip fractures. American Journal of Emergency Medicine 2010;28(1):76-81. [DOI: 10.1016/j.ajem.2008.09.015] [PMID: 20006206 ] [DOI] [PubMed] [Google Scholar]
Bech 2011 {published data only}
- Bech RD, Lauritsen J, Ovesen O, Emmeluth C, Lindholm P, Overgaard S. Local anaesthetic wound infiltration after internal fixation of femoral neck fractures: a randomized, double-blind clinical trial in 33 patients. Hip International 2011;21(2):251-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bendtsen 2014 {published data only}
- Bendtsen T F. Femoral nerve block with bupivacaine and adjuvant dexamethasone in patients with hip fracture. Available at https://clinicaltrials.gov/show/NCT02248870 2014:Accessed December 2019. [CENTRAL: CN-01548932]
Bendtsen 2015 {published data only}
- Bendtsen TF. Obturator nerve block for hip fracture. Available at https://clinicaltrials.gov/ct2/show/NCT02408419:Accessed December 2019. [CENTRAL: CN-01505505]
Bendtsen 2015a {published data only}
- Bendtsen TF. Analgesic effect of a supplemental nerve block in patients with hip fracture. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2015-000078-36-DK 2015:Accessed December 2019. [CENTRAL: CN-01548932] [DOI: ]
Bendtsen 2015b {published data only}
- Bendtsen T F. Gluteus medius fascia plane block - Validating a new nerve block technique. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2015-003726-14-DK:Accessed December 2019.
Bhadani 2017 {published data only}
- Bhadani U K. Comparison between femoral nerve block and intravenous fentanyl for analgesia before performing a spinal block in the sitting position in patients with femoral shaft fracture. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2017/09/009665:Accessed December 2019. [CENTRAL: CN-01892890] [DOI: 10.1002/central/CN-01892890/full] [DOI] [PubMed]
Bhattacharya 2019 {published data only}
- Bhattacharya A, Bhatti T, Haldar M. Pericapsular nerve group block- Is it better than the rest for pain relief in fracture neck femur. Regional Anesthesia and Pain Medicine 2019;44(10 Suppl 1):A116. [Google Scholar]
Bouhours 2010 {published data only}
- Bouhours G. Perioperative analgesia by femoral perineural catheter for femoral neck fracture - study KTcol. Available at https://clinicaltrials.gov/show/NCT01052974 2010:Accessed December 2019. [CENTRAL: CN-01527741]
- Chaudet A, Bouhours G, Rineau E, Hamel J F, Leblanc D, Steiger V, et al. Impact of preoperative continuous femoral blockades on morphine consumption and morphine side effects in hip-fracture patients: a randomized, placebo-controlled study. Anaesthesia, Critical Care and Pain Medicine 2016;35(1):37-43. [CENTRAL: CN-01259379] [DOI: 10.1016/j.accpm.2015.07.004] [EMBASE: 614025563] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bulger 2015 {published data only}
- Bulger J, Brown A, Evans B, Fegan G, Ford S, Guy K, et al. Rapid analgesia for prehospital hip disruption: a feasibility study. International Journal of Technology Assessment in Health Care 2017;33(Suppl 1):140-1. [Google Scholar]
- Bulger J, Brown A, Evans B A, Fegan G, Ford S, Guy K, et al. Rapid analgesia for prehospital hip disruption (rapid). British Medical Journal Open 2018;8(Suppl 1):A3. [CENTRAL: CN-01613074] [DOI: 10.1002/central/CN-01613074/full] [EMBASE: 622675029] [DOI] [Google Scholar]
- Bulger J. Rapid analgesia for prehospital hip disruption (RAPID): a feasibility study for a randomised controlled trial. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN60065373 2015:Accessed December 2019. [CENTRAL: CN-01847947]
- Bulger J K, Brown A, Evans B A, Fegan G, Ford S, Guy K, et a l. Rapid analgesia for prehospital hip disruption (RAPID): protocol for feasibility study of randomised controlled trial. Pilot and Feasibility Studies 2017;3:8. [DOI: 10.1186/s40814-016-0115-6] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans B, Brown A, Bulger J, Fegan G, Ford S, Guy K, et al. Paramedic's experiences of administering fascia iliaca compartment block to patients with suspected hip fracture. British Medical Journal Open 2018;8(Suppl 1):A28. [Google Scholar]
- Evans B A, Brown A, Bulger J, Fegan G, Ford S, Guy K, et al. Paramedics' experiences of administering fascia iliaca compartment block to patients in South Wales with suspected hip fracture at the scene of injury: results of focus groups. British Medical Journal Open 2019;9(2):e026073-e026073. [CENTRAL: CN-01792310] [DOI: 10.1136/bmjopen-2018-026073] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JK, Evans BA, Fegan G, Ford S, Guy K, Jones S, et al. Rapid Analgesia for Prehospital hip Disruption (RAPID): findings from a randomised feasibility study. Pilot and Feasibility Studies 2019;5:77. [DOI: 10.1186/s40814-019-0454-1] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keen L, Bulger JK, Rees N, Snooks H, Fegan G, Ford S, et al. Use of scratch cards for allocation concealment in a prehospital randomised controlled trial. Emergency Medicine Journal 2018;35:708-10. [DOI: 10.1136/emermed-2018-207881] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Callear 2016 {published data only}
- Callear J, Shah K. Analgesia in hip fractures. Do fascia-iliac blocks make any difference? British Medical Journal Quality Improvment Reports 2016;5(1):u210130.w4147. [DOI: 10.1136/bmjquality.u210130.w4147] [PMID: ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Candal‐Couto 2005 {published data only}
- Candal-Couto JJ, McVie JL, Haslam N, Innes AR, Rushmer J. Pre-operative analgesia for patients with femoral neck fractures using a modified fascia iliaca block technique. Injury 2005;36(4):505-10. [DOI: 10.1016/j.injury.2004.10.015 ] [PMID: 15755432 ] [DOI] [PubMed] [Google Scholar]
Carlisle 2004 {published data only}ISRCTN48754612
- Carlisle J. Randomised controlled trial of femoral nerve blockade for fractured femurs. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN48754612 2004:Accessed December 2019. [CENTRAL: CN-01831183]
- Schiferer A, Gore C, Gorove L, Lang T, Steinlechner B, Zimpfer M, et al. A randomized controlled trial of femoral nerve blockade administered preclinically for pain relief in femoral trauma. Anesthesia and Analgesia 2007;105(6):1852-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Castillon 2017 {published data only}
- Castillon P, Veloso M, Gomez O, Salvador J, Bartra A, Angles F. Fascia iliaca block for pain control in hip fracture patients. Revista Espanola de Cirugia Ortopedica y Traumatologia 2017;61(6):383-9. [DOI] [PubMed] [Google Scholar]
Chang 2011 {published data only}
- Chang G, Rajamoney G N, Chua N H. Preliminary experience in acute pain control for non operated hip fracture. The Journal of Trauma 2011;71(1):269. [PMID: ] [DOI] [PubMed] [Google Scholar]
Christos 2010 {published data only}
- Christos SC, Chiampas G, Offman R, Rifenburg R. Ultrasound-guided three-in-one nerve block for femur fractures. Western Journal of Emergency Medicine 2010;11(4):310-3. [PMID: 21079698] [PMC free article] [PubMed] [Google Scholar]
Dodd 2019 {published data only}
- Dodd O, Polischuk M, Gangathimmaiah V, Jan S, Hooper K, Furyk J. Fascia iliaca catheters in emergency hip fractures: repeated boluses versus single bolus. A pilot study and double blind RCT protocol. Emergency Medicine Australasia 2019;31(Suppl 1):59. [CENTRAL: CN-01937925] [DOI: 10.1111/1742-6723.13240] [EMBASE: 627392159] [DOI] [Google Scholar]
Dulaney‐Cripe 2012 {published data only}
- Dulaney-Cripe E, Hadaway S, Bauman R, Trame C, Smith C, Sillaman B, et al. A continuous infusion fascia iliaca compartment block in hip fracture patients: a pilot study. Journal of clinical medicine research 2012;4(1):45-8. [DOI: 10.4021/jocmr724w ] [PMID: 22383926 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Durrani 2013 {published data only}
- Durrani HD, Butt KJ, Khosa AH, Umer A, Pervaiz M. Pain relief during positioning for spinal anaesthesia in patients with femoral fracture: a comparison between femoral nerve block and intravenous nalbuphine. Pakistan Journal of Medical and Health Sciences 2013;7(4):928-32. [CENTRAL: CN-00977951] [Google Scholar]
Elkhodair 2011 {published data only}
- Elkhodair S, Mortazavi J, Chester A, Pereira M. Single fascia iliaca compartment block for pain relief in patients with fractured neck of femur in the emergency department: a pilot study. European Journal of Emergency Medicine 2011;18(6):340-3. [DOI: 10.1097/MEJ.0b013e32834533dd ] [PMID: 21422933 ] [DOI] [PubMed] [Google Scholar]
Evans 2019 {published data only}
- Evans B, Bulger J, Ford S, Foster T, Goodacre S, Jones S, et al. Public patient involvement in prehospital care research development - Designing the RAPID 2 Trial. British Medical Journal Open 2019;9(Suppl 2):A8-9. [Google Scholar]
Finlayson 1988 {published data only}
- Finlayson BJ, Underhill TJ. Femoral nerve block for analgesia in fractures of the femoral neck. Archives of Emergency Medicine 1988;5(3):173-6. [PMID: 3178977 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Foss 2005 {published data only}
- Foss NB, Kristensen MT, Kristensen BB, Jensen PS, Kehlet H. Effect of postoperative epidural analgesia on rehabilitation and pain after hip fracture surgery: a randomized, double-blind, placebo-controlled trial. Anesthesiology 2005;102(6):1197-204. [PMID: ] [DOI] [PubMed] [Google Scholar]
Foss 2009 {published data only}
- Foss NB, Kristensen MT, Palm H, Kehlet H. Postoperative pain after hip fracture is procedure specific. British Journal of Anaesthesia 2009;102(1):111-6. [DOI: 10.1093/bja/aen345] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fujihara 2013 {published data only}
- Fujihara Y, Fukunishi S, Nishio S, Miura J, Koyanagi S, Yoshiya S. Fascia iliaca compartment block: its efficacy in pain control for patients with proximal femoral fracture. Journal of Orthopaedic Science 2013;18(5):793-7. [CENTRAL: CN-00862811] [DOI: 10.1007/s00776-013-0417-y] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gasanova 2019 {published data only}
- Gasanova I, Alexander J C, Estrera K, Wells J, Sunna M, Minhajuddin A, et al. Response to the letter to the editor by Vermeylen and Leunen concerning "Ultrasound-guided suprainguinal fascia iliaca compartment block versus periarticular infiltration for pain management after total hip arthroplasty: a randomized controlled trial". Regional Anesthesia and Pain Medicine 2019 April 16;N/A:[Epub ahead of print]. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gasanova I, Alexander J C, Estrera K, Wells J, Sunna M, Minhajuddin A, Joshi G P. Ultrasound-guided suprainguinal fascia iliaca compartment block versus periarticular infiltration for pain management after total hip arthroplasty: a randomized controlled trial. Regional Anesthesia and Pain Medicine 2019;44(2):206-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Vermeylen K, Leunen I. Ultrasound-guided suprainguinal fascia iliaca compartment block versus periarticular infiltration for pain management after total hip arthroplasty: a randomized controlled trial. Regional Anesthesia and Pain Medicine 2019 Apr 16;NA(NA):[Epub ahead of print]. [DOI: 10.1136/rapm-2019-100519] [PMID: ] [DOI] [PubMed] [Google Scholar]
George 2016 {published data only}CTRI/2016/09/007316
- George B. Comparative evaluation of ultrasound guided femoral nerve block versus fascia iliaca block for positioning during central neuraxial anesthesia in patients with proximal femoral fractures - FNBFIB. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2016/09/007316 2016:Accessed December 2019. [CENTRAL: CN-01868477] [DOI: 10.1002/central/CN-01868477/full] [DOI]
Ghimire 2015 {published data only}
- Ghimire A, Bhattarai B, Koirala S, Subedi A. Analgesia before performing subarachnoid block in the sitting position in patients with proximal femoral fracture: a comparison between fascia iliaca block and femoral nerve block. Kathmandu University Medical Journal (KUMJ) 2015;13(50):152-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Godoy Monzon 2007 {published data only}
- Godoy Monzon D, Iserson KV, Vazquez JA. Single fascia iliaca compartment block for post-hip fracture pain relief. Journal of Emergency Medicine 2007;32(3):257-62. [DOI: 10.1016/j.jemermed.2006.08.011 ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gorodetskyi 2007 {published data only}
- Gorodetskyi IG, Gorodnichenko AI, Tursin PS, Reshetnyak VK, Uskov ON. Non-invasive interactive neurostimulation in the post-operative recovery of patients with a trochanteric fracture of the femur. a randomised, controlled trial. Journal of Bone and Joint Surgery - British Volume 2007;89(11):1488-94. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gosavi 2001 {published data only}
- Gosavi CP, Chaudhari LS, Poddar R. Use of femoral nerve block to help positioning during conduct of regional anesthesia. http://www.bhj.org.in/journal/2001_4304_oct/org_531.htm 2001:Accessed December 2019.
Gozlan 2005 {published data only}
- Gozlan C, Minville V, Asehnoune K, Raynal P, Zetlaoui P, Benhanou D. Fascia iliaca block for femoral bone fractures in prehospital medicine [Bloc iliofascial en médecine préhospitalière pour les fractures du fémur]. Annales Françaises d'Anesthésie et de Réanimation 2005;24(6):617-20. [DOI: 10.1016/j.annfar.2005.03.030] [PMID: ] [DOI] [PubMed] [Google Scholar]
Grigg 2009 {published data only}
- Grigg L, Randall A. Pain management in the pre-operative period for patients with a fractured neck of femur. Orthopaedic Nursing 2009;13(4):215. [DOI: 10.1016/j.joon.2009.08.019] [DOI] [Google Scholar]
Groot 2015 {published data only}
- Groot L, Dijksman LM, Simons MP, Zwartsenburg MM, Rebel JR. Single fascia iliaca compartment block is safe and effective for emergency pain relief in hip-fracture patients. Western Journal of Emergency Medicine 2015;16(7):1188-93. [DOI: 10.5811/westjem.2015.10.28270] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Haines 2012 {published data only}
- Haines L, Dickman E, Ayvazyan S, Pearl M, Wu S, Rosenblum D, et al. Ultrasound-guided fascia iliaca compartment block for hip fractures in the emergency department. The Journal of Emergency Medicine 2012;43(4):692-97. [DOI: 10.1016/j.jemermed.2012.01.050] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Likourezos A. Ultrasound guided pain control versus standard treatment in emergency department hip fracture patients. Available at https://clinicaltrials.gov/ct2/show/results/NCT01904071?term=NCT01904071&rank=1&view=results 2013:Accessed December 2019.
Hallberg 2012 {published data only}
- Hallberg A. Is regional anesthesia of the hip preferable over traditional analgesia in the acute stage of the management of patients with a fracture of the hip. Available at https://clinicaltrials.gov/show/NCT01593319 2012:Accessed December 2019. [CENTRAL: CN-01503294] [DOI: 10.1002/central/CN-01503294/full] [DOI]
Hao 2018 {published data only}
- Hao J, Dong B, Zhang J, Luo Z. Pre-emptive analgesia with continuous fascia iliaca compartment block reduces postoperative delirium in elderly patients with hip fracture. A randomized controlled trial. Saudi Medical Journal 2019;40(9):901-6. [CENTRAL: CN-01987094] [DOI: 10.15537/smj.2019.9.24483] [EMBASE: 629332755] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao J. Early continuous fascia iliaca compartment block reduces postoperative delirium in elderly patients undergoing hip fracture surgery. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR1800014917:Accessed December 2019. [CENTRAL: CN-01899457] [DOI: 10.1002/central/CN-01899457/full]]
Hauritz 2009 {published data only}
- Hauritz RW, Gerlif C, Rønholm E. Fascia iliaca block performed by emergency department physician trainees in hip fractures. Ugeskrift for Laeger 2009;9(7):515-8. [PMID: 19210934 ] [PubMed] [Google Scholar]
Helsø 2016 {published data only}
- Helsø I, Jantzen C, Lauritzen JB, Jørgensen HL. Opioid usage during admission in hip fracture patients-The effect of the continuous femoral nerve block. Geriatric Orthopaedic Surgery and Rehabilitation 2016;7(4):197-201. [DOI: 10.1177/2151458516672284 ] [PMID: 27847679 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoffmann 2015 {published data only}
- Hoffmann B, Rosseto E. Comparison of ultrasound guided femoral nerve blockade and standard parenteral opioid pain management alone in patients with hip fracture in the emergency department. https://clinicaltrials.gov/ct2/show/NCT02381717?term=NCT02381717&draw=2&rank=1 2015:Accessed December 2019.
- Hoffmann B, Rosseto E. Ultrasound guided femoral nerve block. Available at https://clinicaltrials.gov/ct2/show/NCT02381717 2015. [CENTRAL: CN-01504812] [DOI: 10.1002/central/CN-01504812/full] [DOI]
Hogh 2008 {published data only}
- Høgh A, Dremstrup L, Jensen SS, Lindholt J. Fascia iliaca compartment block performed by junior registrars as a supplement to pre-operative analgesia for patients with hip fracture. Strategies in Trauma Limb Reconstruction 2008;3(2):65-70. [DOI: 10.1007/s11751-008-0037-9 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hussain 2014 {published data only}
- Hussain R, Nazeer T, Asim A. Unilateral fascia iliaca block (FIB) for post-operative analgesia in fracture neck of femur surgery; comparison with standard post-operative analgesia. Pakistan Journal of Medical and Health Sciences 2014;8(4):818-20. [Google Scholar]
Iamaroon 2010 {published data only}
- Iamaroon A, Raksakietisak M, Halilamien P, Hongsawad J, Boonsararuxsapong K. Femoral nerve block versus fentanyl: analgesia for positioning patients with fractured femur. Local and Regional Anesthesia 2010;3:21-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Inan 2009 {published data only}
- Inan N, Akin Takmaz S, Iltar S, Yazici I, Başar H. The effects of two different multimodal analgesic regimens in total hip replacement surgery [Total kalça protezi operasyonlarında iki multimodal analjezi yönteminin etkinliği]. Agri 2009;21(2):69-74. [PMID: 19562535 ] [PubMed] [Google Scholar]
Irwin 2012 {published data only}
- Irwin M, Mahalingam S, Mills G, Krahe L. Acute pain management for neck of femur fractures: a comparison of the fascia iliaca block versus traditional opiates. British Journal of Anaesthesia 2012;108(Suppl 2):ii422. [EMBASE: 70719658] [Google Scholar]
Isalgue 2014 {published data only}
- Isalgue SA, González Castilla R, Luzardo Silveira EM. Blocking of the iliac fascia compared to metamizol for preoperative analgesiain patients with hip fracture [Bloqueo de la fascia iliaca frente al metamizol para analgesia preoperatoriaen pacientes con fractura de cadera]. Medisan 2014;18(8):1127-33. [Google Scholar]
Ishioka 2018 {published data only}UMIN000034343
- Ishioka Y. The analgesic efficacy and the effect on postoperative outcome of preoperative fascia iliaca block for hip fracture. https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000039149:Accessed January 2020.
Kacha 2018 {published data only}
- Kacha NJ, Jadeja CA, Patel PJ, Chaudhari HB, Jivani JR, Pithadia VS. Comparative study for evaluating efficacy of fascia iliaca compartment block for alleviating pain of positioning for spinal anesthesia in patients with hip and proximal femur fractures. Indian Journal of Orthopaedics 2018;52(2):147-53. [DOI: 10.4103/ortho.IJOrtho_298_16] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kang 2013 {published data only}
- Kang H, Ha YC, Kim JY, Woo YC, Lee JS, Jang EC. Effectiveness of multimodal pain management after bipolar hemiarthroplasty for hip fracture: a randomized, controlled study. The Journal of Bone and Joint Surgery - American Volume 2013;95(4):291-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kassam 2018 {published data only}
- Kassam A M, Gough A T, Davies J, Yarlagadda R. Can we reduce morphine use in elderly, proximal femoral fracture patients using a fascia iliac block? Geriatric Nursing 2018;39(1):84-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Klukowski 2017 {published data only}
- Klukowski M, Kowalczyk R, Górniewski G, Łęgosz P, Janiak M, Trzebicki J. Iliac fascia compartment block and analgesic consumption in patients operated on for hip fracture. Ortopedia Traumatologia Rehabiltacjia 2017;19(5):451-9. [DOI: 10.5604/01.3001.0010.5825] [PMID: 29154229] [DOI] [PubMed] [Google Scholar]
Kristek 2019 {published data only}
- Kristek G, Rados I, Kristek D, Kapural L, Neskovic N, Skiljic S, et al. Influence of postoperative analgesia on systemic inflammatory response and postoperative cognitive dysfunction after femoral fractures surgery: a randomized controlled trial. Regional Anesthesia and Pain Medicine 2019;44(1):59-68. [CENTRAL: CN-01789399] [DOI: 10.1136/rapm-2018-000023] [EMBASE: 625942994] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Regional Anesthesia and Pain Medicine. Erratum: Influence of postoperative analgesia on systemic inflammatory response and postoperative cognitive dysfunction after femoral fractures surgery: a randomized controlled trial. Regional Anesthesia and Pain Medicine 2019;44(10):e2. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kumar 2016 {published data only}
- Kumar D, Hooda S, Kiran S, Devi J. Analgesic efficacy of ultrasound guided FICB in patients with hip fracture. Journal of Clinicial Diagnostic Research 2016;10(7):UC13-6. [DOI: 10.7860/JCDR/2016/17802.8123] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumie 2015 {published data only}
- Kumie FT, Gebremedhn EG, Tawuye HY. Efficacy of fascia iliaca compartment nerve block as part of multimodal analgesia after surgery for femoral bone fracture. World Journal of Emergency Medicine 2015;6(2):142-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2015 {published data only}
- Lee J S, Bhandari T, Emond M, Perry J J, Woo M, Chenkin J. Ultrasound guided regional anesthesia in older hip fractures patients: uptake of regional anesthesia in randomly selected emergency physicians. Canadian Journal of Emergency Medicine 2015;17:S47-8. [CENTRAL: CN-01375699] [EMBASE: 616389794] [Google Scholar]
Lee 2016 {published data only}
- Lee JS. ED Ultrasonographic regional anesthesia to prevent incident delirium in hip fracture patients (EDU-RAPID). Available at https://clinicaltrials.gov/ct2/show/NCT02892968 2016. [CENTRAL: CN-01448965] [DOI: 10.1002/central/CN-01448965/full] [DOI]
Leeper 2012 {published data only}
- Leeper A D, Brandon P T, Morgan A V, Cutts S, Cohen A M. Fascia iliaca compartment block reduces morphine requirement pre-operatively for patients with fractured neck of femur. European Journal of Trauma and Emergency Surgery 2012;38(6):673-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Levente 2017 {published data only}
- Levente B Z, Filip M N, Romaniuc N, Gheorghe S. Efficacy and duration of ultrasound guided fascia iliaca block for hip fracture performed in the emergency departments. Romanian Journal of Anaesthesia and Intensive Care 2017;24(2):167-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Levine 2003 {published data only}
- Levine J, Triner W R, Lai SY. A randomized controlled trial comparing femoral nerve block to intravenous morphine in isolated femur fractures. Academic Emergency Medicine 2003;10(5):469. [CENTRAL: CN-00453244] [Google Scholar]
- Triner W, Levine J, Lai SY, McErlean M. Femoral nerve block for femur fractures. Annals of Emergency Medicine 2005;45(6):679. [CENTRAL: CN-00600793] [PMID: ] [DOI] [PubMed] [Google Scholar]
Li 2013 {published data only}
- Chen WQ, Guo N, Wang SS, Wang R, Huang F, Li SR. General laryngeal mask airway anesthesia with lumbar plexus and sciatic block provides better outcomes than general anesthesia and endotracheal intubation in elderly patients undergoing hip surgery. Archives of Gerontology and Geriatrics 2018;78:227-32. [CENTRAL: CN-01930236] [DOI: 10.1016/j.archger.2018.07.005] [EMBASE: 2000946813] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Li S, Chen W. The laryngeal mask anesthesia compound nerve block in the applications of the elderly orthopaedic surgery clinical research. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR-TRC-13003405 2013:Accessed December 2019.
Lopez 2003 {published data only}
- Lopez S, Gros T, Bernard N, Plasse C, Capdevila X. Fascia iliaca compartment block for femoral bone fractures in prehospital care. Regional Anesthesia and Pain Medicine 2003;28(3):203-7. [DOI: 10.1053/rapm.2003.50134 ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mannion 2005 {published data only}
- Mannion S, Hayes I, Loughnane F, Murphy DB, Shorten GD. Intravenous but not perineural clonidine prolongs postoperative analgesia after psoas compartment block with 0.5% levobupivacaine for hip fracture surgery. Anesthesia and Analgesia 2005;100(3):873-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Manohara 2015 {published data only}
- Manohara S, Lim YC. A randomized, controlled trial comparing analgesic effects of ultrasound-guided supra-inguinal fascia iliaca block with femoral nerve block for surgical fixation of hip fractures. Regional Anesthesia and Pain Medicine 2015;40(5 Suppl 1):e93-4. [EMBASE: 72027148] [Google Scholar]
Marhofer 1998 {published data only}
- Marhofer P, Schrogendorfer K, Wallner T, Koinig H, Mayer N, Kapral S. Ultrasonographic guidance reduces the amount of local anesthetic for 3-in-1 blocks. Regional Anesthesia and Pain Medicine 1998;23(6):584-8. [PMID: 9840855 ] [DOI] [PubMed] [Google Scholar]
Masoumi 2014 {published data only}IRCT2014041717316N1
- Forouzan A, Masoumi K, Yadegar N, Rahim F, FeliM, Darian AA. Comparison of femoral nerve block with intravenous morphine sulfate for pain relief of femoral fracture. Asian Journal of Scientific Research 2015;8(3):429-35. [DOI: 10.3923/ajsr.2015.429.435] [DOI] [Google Scholar]
- Masoumi K. Pain in femoral fractures. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2014041717316N1 2014:Accessed December 2019. [CENTRAL: CN-01870541] [DOI: 10.1002/central/CN-01870541/full] [DOI]
Matot 2003 {published data only}
- Matot I, Oppenheim-Eden A, Ratrot R, Baranova J, Davidson E, Eylon S, et al. Preoperative cardiac events in elderly patients with hip fracture randomized to epidural or conventional analgesia. Anesthesiology 2003;98(1):156-63. [PMID: ] [DOI] [PubMed] [Google Scholar]
McGlone 1987 {published data only}
- McGlone R, Sadhra K, Hamer DW, Pritty PE. Femoral nerve block in the initial management of femoral shaft fractures. Archives of Emergency Medicine 1987;4(3):163-8. [DOI: 10.1136/emj.4.3.163 ] [PMID: 3689541 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
McRae 2015 {published data only}
- McRae P, Bendall JC, Madigan V, Middleton P. Paramedic performed fascia iliaca compartment block (FICB) for femoral fractures: a randomised controlled trial. Australasian Journal of Prehospital Care 2013;10(3):14-5. [Google Scholar]
- McRae PJ, Bendall JC, Madigan V, Middleton PM. Paramedic-performed fascia iliaca compartment block for femoral fractures: a controlled trial. The Journal of Emergency Medicine 2015;48(5):581-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Memary 2015 {published data only}IRCT201204309593N1
- Memary E. The effect of perineural administration of dexmedetomidine on propofol and narcotic consumption and pain intensity in the patients undergoing femoral shaft fracture surgery. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT201204309593N1 2015:Accessed December 2019. [CENTRAL: CN-01822701] [DOI: 10.1002/central/CN-01822701/full] [DOI] [PMC free article] [PubMed]
Mostafa 2015 {published data only}
- Mostafa S F, Eid G M, Elkalla R S. Patient-controlled fascia iliaca compartment block versus fentanyl patient controlled intravenous analgesia in patients undergoing femur fractures surgery. Egyptian Journal of Anaesthesia 2018;34:9-13. [CENTRAL: CN-01452659] [DOI: 10.1016/j.egja.2017.12.002] [EMBASE: 620031634] [DOI] [Google Scholar]
- Mostafa S F. Fascia iliaca compartment block. http://www.who.int/trialsearch/Trial2.aspx?TrialID=PACTR201512001376158 2015 2015:Accessed December 2019. [CENTRAL: CN-01828502] [DOI: 10.1002/central/CN-01828502/full] [DOI]
Mutty 2007 {published data only}
- Mutty CE, Jensen EJ, Manka MA Jr, Anders MJ, Bone LB. Femoral nerve block for diaphyseal and distal femoral fractures in the emergency department. Journal of Bone and Joint Surgery - American Volume 2007;89(12):2599-603. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nielsen 2015 {published data only}
- Nielsen TD, Brendtsen TF. Obturator and femoral nerve block in patients with hip fracture. Available at https://clinicaltrials.gov/show/NCT02540837 2015:Accessed December 2019. [CENTRAL: CN-01491994]
Pakhare 2016 {published data only}
- Pakhare PV, Pendyala P. A randomized prospective study of comparison of IV fentanyl vs. femoral nerve block to facilitate administration of subarachnoid block in sitting position for femur fracture surgeries. Indian Journal of Clinical Anaesthesia 2016;3(4):507-11. [DOI: 10.18231/2394-4994.2016.0004] [DOI] [Google Scholar]
Parras 2016 {published data only}
- Parras T, Blanco R. Randomised trial comparing the transversus abdominis plane block posterior approach or quadratus lumborum block type I with femoral block for postoperative analgesia in femoral neck fracture, both ultrasound-guided. Revista Espanola de Anestesiologia y Reanimacion 2016;63(3):141-8. [CENTRAL: CN-01411593] [PMID: ] [DOI] [PubMed] [Google Scholar]
Perrier 2010 {published data only}
- Perrier V, Julliac B, Lelias A, Morel N, Dabadie P, Sztark F. Influence of the fascia iliaca compartment block on postoperative cognitive status in the elderly. Annales Françaises d'Anesthésie et de Réanimation 2010;29(4):283-8. [DOI: 10.1016/j.annfar.2009.12.021] [PMID: ] [DOI] [PubMed] [Google Scholar]
Piangatelli 2004 {published data only}
- Piangatelli C, De Angelis C, Pecora L, Recanatini F, Testasecca D. Levobupivacaine versus ropivacaine in psoas compartment block and sciatic nerve block in orthopedic surgery of the lower extremity. Minerva Anestesiologica 2004;70(12):801-7. [PMID: ] [PubMed] [Google Scholar]
Randall 2008 {published data only}
- Obideyi A, Srikantharajah I, Grigg L, Randall A. Nurse administered fascia iliaca compartment block for pre-operative pain relief in adult fractured neck of femur. Acute Pain 2008;10(3-4):145-9. [DOI: 10.1016/j.acpain.2008.05.014] [DOI] [Google Scholar]
- Randall A, Grigg L, Obideyi A, Srikantharajah I. Fascia iliaca compartment block: a nurse-led initiative for preoperative pain management in patients with a fractured neck of femur. Journal of Orthopaedic Nursing 2008;12(2):69-74. [DOI: 10.1016/j.joon.2008.07.007] [DOI] [Google Scholar]
Rapchuk 2013 {published data only}
- Rapchuk IL, Glover P. Combined use of fascia iliaca block, subarachnoid block and dexmedetomidine sedation for patients having fractured femur surgery. Journal of Anesthesia 2013;27(1):149-50. [DOI: 10.1007/s00540-012-1481-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rashwan 2013 {published data only}
- Rashwan D. Levobupivacaine patient controlled analgesia: epidural versus blind fascia iliaca compartment analgesia – a comparative study. Egyptian Journal of Anaesthesia 2013;29(2):155-9. [DOI: 10.1016/j.egja.2012.10.002] [DOI] [Google Scholar]
Reavley 2015 {published data only}
- Reavley P, Montgomery AA, Smith JE, Binks S, Edwards J, Elder G, et al. Randomised trial of the fascia iliaca block versus the '3-in-1' block for femoral neck fractures in the emergency department. Emergency Medicine Journal 2015;32(9):685-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Reddy 2016 {published data only}
- Reddy ED, Rao BD. Comparative study of efficacy of femoral nerve block and IV fentanyl for positioning during femur fracture surgery. International Surgery Journal 2016;3(1):321-4. [DOI: 10.18203/2349-2902.isj20160252] [DOI] [Google Scholar]
Rojas Rivera 2002 {published data only}
- Rojas Rivera W, Abed-R M. Three-in-one femoral block for transtoncanteric hip fracture surgery: safety and analgesia [Bloqueo femoral tres en uno para cirugía de fractura transtoncantérica de cadera: seguridad y analgesia]. Acta Medica Costarricense 2002;44(2):62-7. [Google Scholar]
Sahota 2011 {published data only}2010‐023871‐25ISRCTN92946117
- Nottingham University Hospitals NHS Trust. The FINOF(femoral nerve-block intervention in neck of femur fracture) study - FINOF. http://www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2010-023871-25-GB 2011:Accessed December 2019. [CENTRAL: CN-01843196] [DOI: 10.1002/central/CN-01843196/full] [DOI]
- Rowlands M, Walt G V, Bradley J, Mannings A, Armstrong S, Bedforth N, et al. Femoral nerve block intervention in neck of femur fracture (FINOF): a randomised controlled trial. British Medical Journal Open 2018;8(4):e019650-e019650. [CENTRAL: CN-01708268] [DOI: 10.1136/bmjopen-2017-019650] [EMBASE: 625044103] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahota O, Rowlands M, Bradley J, Van de Walt G, Bedforth N, Armstrong S, et al. Femoral nerve block Intervention in neck of femur fracture (FINOF): study protocol for a randomized controlled trial. Trials 2014;15(May 24):189. [DOI: 10.1186/1745-6215-15-189] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahota O. The FINOF - femoral nerve-block Intervention in neck of femur fracture study. https://apps.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN92946117 2012:Accessed December 2019.
Scheinin 2000 {published and unpublished data}
- Scheinin 2015. Additional information for our trial [personal communication]. Email to: J Guay 25 May 2015.
- Scheinin H, Virtanen T, Kentala E, Uotila P, Laitio T, Hartiala J, et al. Epidural infusion of bupivacaine and fentanyl reduces perioperative myocardial ischaemia in elderly patients with hip fracture - a randomized controlled trial. Acta Anaesthesiologica Scandinavica 2000;44(9):1061-70. [PMID: ] [DOI] [PubMed] [Google Scholar]
Segado Jimenez 2010 {published data only}
- Segado Jimenez I. Information on our trial [personal communication]. Email to: J Guay 24 April 2016.
- Segado Jimenez MI, Arias Delgado J, Casas Garcıa ML, Domınguez Hervella F, Lopez Perez A, Bayon Gago M, et al. Post-surgical analgesia in hip surgery: a comparison of three techniques [Abordaje de la analgesia postoperatoria en cirugıa de cadera: comparativa de 3 tecnicas]. Revista Sociedad Espanola del Dolor 2010;17(6):259-67. [Google Scholar]
Shi 2018 {published data only}
- Shi Z Y, Jiang C N, Shao G. Application of lower limb nerve block combined with slow induction of light general anesthesia and tracheal induction in elderly hip surgery. Medicine 2018;97(40):e12581. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sia 2004 {published data only}
- Sia S, Pelusio F, Barbagli R, Rivituso C. Analgesia before performing a spinal block in the sitting position in patients with femoral shaft fracture: a comparison between femoral nerve block and intravenous fentanyl. Anesthesia and Analgesia 2004;99(4):1221-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Siguira 2014 {published data only}JPRN‐UMIN000016015
- Sugiura T. Articular branches of the femoral nerve block; it`s analgesic efficacy on patients with proximal femoral fracture. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000016015 2014:Accessed December 2019. [CENTRAL: CN-01879824]
Singh 2016 {published data only}
- Singh A P, Kohli V, Bajwa S J. Intravenous analgesia with opioids versus femoral nerve block with 0.2% ropivacaine as preemptive analgesic for fracture femur: A randomized comparative study. Anesthesia, Essays and Researches 2016;10(2):338-42. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sonawane 2019 {published data only}
- Sonawane K. Analgesic efficacy of on-arrival ultrasound guided pericapsular nerve group (PENG) block vs femoral nerve block vs femoral articular branch block in patients with unilateral hip fracture. http://www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2019/04/018651 2019:Accessed December 2019. [CENTRAL: CN-01974563]
- Sonawane K. Analgesic efficacy of Pre-Emptive USG guided pericapsular nerve group (PENG) block vs femoral nerve block vs articular branch block while positioning the patient during neuraxial anaesthesia for unilateral hip fracture surgery. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2019/04/018654:Accessed December 2019.
Swart 2017 {published data only}
- Swart E, Matuszewski P. Randomized controlled trial for exparel hip fracture. Available at https://clinicaltrials.gov/ct2/show/NCT03289858 2017:Accessed December 2019. [CENTRAL: CN-01564275] [DOI: 10.1002/central/CN-01564275/full] [DOI]
Tao 2016 {published data only}ChiCTR‐INC‐16009960
- Tao K. Nerve block anesthesia and general anesthesia influnce postoperative on cognitive dysfunction after hip athroplasty of aged fracture of neck of femur patients: randomized controlled trial. http://www.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR-INC-16009960 2016:Accessed December 2019. [CENTRAL: CN-01805484]
Thakur 2018 {published data only}CTRI/2018/01/011435
- Takhur DP. Efficacy of fascia iliaca compartment block versus intravenous fentanyl onpositioning for regional anaesthesia in patients with fracture femur. http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=15672 2018:Accessed January 2020.
Turker 2003 {published data only}
- Turker G, Uckunkaya N, Yavascaoglu B, Yilmazlar A, Ozcelik S. Comparison of the catheter-technique psoas compartment block and the epidural block for analgesia in partial hip replacement surgery. Acta Anaesthesiologica Scandinavica 2003;47(1):30-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Leeuwen 2000 {published data only}
- Van Leeuwen FL, Bronselaer K, Gilles M, Sabbe MB, Delooz HH. The 'three in one' block as locoregional analgesia in an emergency department. European Journal of Emergency Medicine 2000;7(1):35-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Vats 2016 {published data only}
- Vats A, Gandhi M, Jain P, Arora KK. Comparative evaluation of femoral nerve block and intravenous fentanyl for positioning during spinal anaesthesia in surgeries of femur fracture. International Journal of Contemporary Medical Research 2016;3(8):2298-301. [Google Scholar]
Wang 2019 {published data only}ChiCTR1900021118
- Wang QH. Application of continuous nerve block guided by ultrasound in perioperative analgesia of hip fracture patients. http://www.chictr.org.cn/showprojen.aspx?proj=33224 2019:Accessed January 2020.
Wei 2018 {published data only}ChiCTR1800018503
- Wei D. Application of iliofascial gap block combined with lumbar epidural anesthesia in total hip replacement. http://www.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR1800018503 2018:Accessed December 2019. [CENTRAL: CN-01908354] [DOI: 10.1002/central/CN-01908354/full] [DOI]
WHO Int 2007 {published data only}EUCTR2006‐004001‐26‐GB
- WHO Int. A randomised controlled trial of fascia iliaca compartment block vs. morphine for pain in fractured neck of femur in the emergency department: a pilot study - fascia iliaca compartment block vs parenteral morphine sulphate. http://www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2006-004001-26-GB 2007:Accessed December 2019. [CENTRAL: CN-01838104] [DOI: 10.1002/central/CN-01838104/full] [DOI]
Williams 2016 {published data only}
- Williams H, Paringe V, Shenoy S, Michaels P, Ramesh B. Standard preoperative analgesia with or without fascia iliaca compartment block for femoral neck fractures. Journal of Orthopedic Surgery (Hong Kong) 2016;24(1):31-5. [DOI: 10.1177/230949901602400109 ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Zadeh 2015 {published data only}IRCT2015102712642N19
- Zadeh P R. The effect of nerve block anesthesia on patients with femur fractures. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2015102712642N19 2015:Accessed December 2019. [CENTRAL: CN-01873707]
Zheng 2017 {published data only}
- Zheng X, You M. Application of modified fascial iliaca block approach in enhanced recovery after surgery of femoral fracture in elderly patients. http://www.chictr.org.cn/showprojen.aspx?proj=21433 2017:Accessed January 2020.
References to ongoing studies
Capelleri 2017 {published data only}
- Capelleri G. Early femoral block in elderly with hip fracture. Available at https://clinicaltrials.gov/show/NCT03092466:Accessed December 2019. [CENTRAL: CN-01562908] [DOI: 10.1002/central/CN-01562908/full] [DOI]
Carvalho 2015 {published data only}
- Carvalho R. Anesthesia and post-operative mortality after proximal femur fractures. Available at https://clinicaltrials.gov/ct2/show/NCT02406300?cond=NCT02406300&draw=2&rank=1 2015:Accessed December 2019.
Chinachoti 2010 {published data only}
- Chinachoti T, Chairatthanawanit S. Intrathecal morphine, femoral nerve block, periarticular bupivacaine infiltration for pain after intramedullary hip screw. Available at https://clinicaltrials.gov/ct2/show/NCT01219088?cond=NCT01219088&draw=2&rank=1 2010:Accessed December 2019.
- Chinachoti T, Chairatthanawanit S. Post operative pain control among intrathecal 0.1 mg morphine, femoral nerve block, or periarticular infiltration of 20 mL of 0.25% bupivacaine in patients post intramedullary hip screw. CENTRAL 2010. [CENTRAL: CN-01501321] [DOI: 10.1002/central/CN-01501321/full] [DOI]
Chiu 2016 {published data only}
- Chiu TL, McAllister D, Ali M, Short T. Evaluating the addition of regional analgesia to reduce postoperative delirium in patients having hip fracture surgery. Available at https://clinicaltrials.gov/show/NCT02689388 2016:Accessed December 2019. [CENTRAL: CN-01448955] [DOI: 10.1002/central/CN-01448955/full] [DOI]
ClinicalTrials.gov 2019 {published data only}
- Medical University of South Carolina. Fascia iliaca compartment blocks for pain control in hip fractures. Available at https://clinicaltrials.gov/ct2/show/NCT04086914 2019:Accessed December 2019.
Compere 2012 {published data only}
- Compere V. Hip fracture and perineural catheter. Available at https://clinicaltrials.gov/show/NCT01638845 2012:Accessed December 2019.
Cong 2016 {published data only}ChiCTR‐INR‐16009481
- Cong R. Nerve block anesthesia and general anesthesia influence postoperative on cognitive dysfunction after hip athroplasty of aged fracture of neck of femur patients: randomized controlled trial. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR-INR-16009481 2016:Accessed December 2019. [CENTRAL: CN-01849088]
- Cong R. Nerve block anesthesia and general anesthesia influence postoperative on cognitive dysfunction after hip athroplasty of aged fracture of neck of femur patients: randomized controlled trial. http://www.chictr.org.cn/showproj.aspx?proj=15781 2016:Accessed December 2019.
Dhimar 2017 {published data only}CTRI/2017/10/009995
- Dhimar A A. Analgesic effect provided by femoral nerve block versus intravenous fentanyl prior to positioning for sub arachnoid block in patients with fracture femur. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2017/10/009995 2017:Accessed December 2019. [CENTRAL: CN-01894746] [DOI: 10.1002/central/CN-01894746/full] [DOI]
Diakomi 2015 {published data only}
- Diakomi M. Fascia iliaca compartment block in acute and chronic pain management in hip fracture patients. Available at https://clinicaltrials.gov/ct2/results?cond=&term=NCT02479828&cntry=&state=&city=&dist= Accessed 18 January 2020.
El Sharkawy 2016 {published data only}
- El Sharkawy RA. Fascia iliaca compartment block for proximal-end femur fractures. Available at https://clinicaltrials.gov/ct2/show/NCT02696915 2016:Accessed December 2019. [CENTRAL: CN-01556201] [DOI: 10.1002/central/CN-01556201/full] [DOI]
Kulkarni 2018 {published data only}CTRI/2018/12/016679
- Kulkarni SJ, Sahasrabuddhe S. USG guided fascia iliaca compartment block for post operative analgesia In proximal femur fracture. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2018/12/016679 2018:Accessed December 2019. [CENTRAL: CN-01948470] [DOI: 10.1002/central/CN-01948470/full] [DOI]
Levins 2006 {published data only}ISRCTN75659782
- Levins FA. Intra- and post-operative analgesia for patients undergoing surgery for hip fracture - role of fascia iliaca compartment block. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN75659782 2017:Accessed December 2019. [CENTRAL: CN-01862137] [DOI: 10.1002/central/CN-01862137/full]]
Li 2018 {published data only}ChiCTR1900021549
- Li JB, Zhang JH. Effect of lumbar plexus block combined with dexmedetomidine on postoperative delirium in elderly patients with hip fractures: a prospective, randomized controlled trial. http://www.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR1900021549 2018:Accessed December 2019. [CENTRAL: CN-01949555] [DOI: 10.1002/central/CN-01949555/full] [DOI]
Luo 2019 {published data only}ChiCTR1900022595
- Luo F, Zhao W. Effects of ultrasound-guided continuous modified fascia iliaca compartment block for postoperative recovery in elderly patients with femoral fracture. http://www.chictr.org.cn/showprojen.aspx?proj=33236:Accessed January 2020.
Mathijssen 2015 {published data only}EUCTR2015‐004119‐19‐N
- Mathijssen N. Nerve blockage in patients with a hip fracture. http://www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2015-004119-19-NL 2016:Accessed December 2019.
Nguyen 2018 {published data only}
- Nguyen MP. Impact of fascia iliaca block in hip fracture patients. Available at https://clinicaltrials.gov/show/NCT03525977 2018:Accessed December 2019. [CENTRAL: CN-01659565] [DOI: 10.1002/central/CN-01659565/full] [DOI]
Park 2009 {published data only}ACTRN12609000526279
- Park E. Ultrasound guided femoral nerve block using 1% ropivacaine as a method of pain control in patients whopresent to emergency with a fractured hip.. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ACTRN12609000526279 2009:Accessed January 2020.
Postma 2017 {published data only}16T215NL60104.096.16
- EU Clinical Trials Register. Morphine use in the fascia iliaca compartment block with ultrasound guidance. https://www.clinicaltrialsregister.eu/ctr-search/trial/2016-004698-42/NL 2017:Accessed December 2019.
- O'Connor R, Postma S. Morphine use in the fascia iliaca compartment block with ultrasound(MORFICUS). https://clinicaltrials.gov/ct2/results?cond=&term=NCT03846102&cntry=&state=&city=&dist= Accessed 18 January 2020.
- WHO Int. Morphine use after blocking the nerve of the leg with medication. Available at http://www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2016-004698-42-NL 2017:Accessed December 2019. [CENTRAL: CN-01886419] [DOI: 10.1002/central/CN-01886419/full] [DOI]
Qiu 2018 {published data only}ChiCTR1800018604
- Qiu CH. A randomized controlled trial for the efficacy of early analgesia by continuous fascia block under ultrasound guidance for elderly patients with hip fracture. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR1800018604 2018:Accessed December 2019. [CENTRAL: CN-01908328] [DOI: 10.1002/central/CN-01908328/full] [DOI]
Ridderikhof 2015 {published data only}EUCTR2015‐003650‐40‐NL
- Ridderikhof M, Kolk D, Ziekenhuis T, Post J, Pouw M, Hollmann M. Delirium in elderly patients with trauma of the hip (DEPTHip). https://clinicaltrials.gov/ct2/show/NCT02689024?term=NCT02689024&draw=2&rank=1 2016:Accessed December 2019.
- Ridderikhof M. Acute confusional state in elderly patients with a broken hip. Available at http://www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2015-003650-40-NL 2015:Accessed December 2019. [CENTRAL: CN-01857976] [DOI: 10.1002/central/CN-01857976/full] [DOI]
- Ridderikhof M L. A multicenter randomized controlled trial in elderly patients with hip fractures comparing continuous fascia iliaca compartment block to systemic opioids and Its effect on delirium occurrence. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=NTR5747 2016:Accessed December 2019. [CENTRAL: CN-01881250]
Saga 2019 {published data only}
- Saga E, Lindholm E, Bernklev T. Nurse led ultrasound guided femoral nerve block in the emergency department (URGENT). Available at https://clinicaltrials.gov/ct2/show/NCT04145752?term=Nerve+Block+OR+compartment+block&type=Intr&cond=Hip+Fracture+OR+femur+fracture+OR%E2%80%A6 Accessed 18 January 2020.
Sahiti 2019 {published data only}CTRI/2019/04/018488
- Sahiti T, Venkatraman. A randomized control study to evaluate the efficacy of ultrasound guided pre- emptive fasicia iliaca compartment block for post operative analgesia in femur and hip fracture surgeries. http://www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2019/04/018488 2019:Accessed December 2019. [CENTRAL: CN-01974714] [DOI: 10.1002/central/CN-01974714/full] [DOI]
Shah 2016 {published data only}
- Shah AMM, Rahman RA, Azidin AM. Analgesia for positioning patient with femur fracture for spinal. Available at https://clinicaltrials.gov/show/NCT02983344 2016:Accessed December 2019. [CENTRAL: CN-01560412] [DOI: 10.1002/central/CN-01560412/full] [DOI]
Tsui 2015 {published data only}
- Tsui B, Beaupre L, Menon M, Green J. Pre-op femoral nerve block for hip fracture. Available at https://clinicaltrials.gov/show/NCT02450045 2015:Accessed December 2019.
Winso 2009 {published data only}ISRCTN46653818
- Winso O. Femoral nerve blockade in hip fracture patients: a randomised controlled trial. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN46653818 2009:Accessed December 2019.
- Winso O. Femoral nerve blockade in hip fracture patients. http://www.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN46653818 2009:Accessed December 2019. [CENTRAL: CN-01842337] [DOI: 10.1002/central/CN-01842337/full] [DOI]
Xi 2014 {published data only}ChiCTR‐IPR‐14005641
- Xi S. A research of postoperative cognitive dysfunction of elderly patients after general anesthesia combined with nerve block or not for femoral fracture surgery. http://www.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR-IPR-14005641 2014:Accessed December 2019. [CENTRAL: CN-01841112]
Xuesheng 2019 {published data only}ChiCTR1900025113
- Xuesheng L, Panpan F. Comparison of combined lumbar and sacral plexus block with low general anesthesia versus spinal anaesthesia on postoperative outcomes in elderly patients undergoing hip fracture surgery. http://www.chictr.org.cn/showprojen.aspx?proj=41891 2019:Accessed January 2020.
Yuan 2017 {published data only}ChiCTR‐IOR‐17012042
- Yuan H, Li W. Efficacy of perioperative advanced protocol enhance recovery of elderly patients suffering limb fracture: A clinical study. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR-IOR-17012042 2017:Accessed December 2019. [CENTRAL: CN-01887074] [DOI: 10.1002/central/CN-01887074/full] [DOI]
Yun 2018 {published data only}ChiCTR1800016421
- Yun W. Clinical study on analgesia of Top-Tql lumbar quadratus muscle block induced by ultrasound-guided after PFNA surgery for senile femoral trochanteric fracture. http://www.chictr.org.cn/showprojen.aspx?proj=27849:Accessed January 2020.
Additional references
American Academy of Orthopaedic Surgeons 2014
- American Academy of Orthopedic Surgeons. Management of hip fractures in the elderly: guidelines. Available at https://www.aaos.org/CustomTemplates/Content.aspx?id=6395&ssopc=1 2014 (accessed 11 January 2020).
American Society of Anesthesiologists 2020
- American Society of Anesthesiologists. The Anesthesiology Annual Meeting. http://www.asaabstracts.com/strands/asaabstracts/search.htm 2020 (accessed January 2020).
Amin 2017
- Amin NH, West JA, Farmer T, Basmajian HG. Nerve blocks in the geriatric patient with hip fracture: a review of the current literature and relevant neuroanatomy. Geriatric Orthopaedic Surgery & Rehabilitation 2017;8(4):268-75. [DOI: 10.1177/2151458517734046] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Arshi 2018
- Arshi A, Lai WC, Chen JB, Bukata SV, Stavrakis AI, Zeegen EN. Predictors and sequelae of postoperative delirium in geriatric hip fracture patients. Geriatric Orthopaedic Surgery and Rehabilitation 2018;9:1-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Auroy 2002
- Auroy Y, Benhamou D, Bargues L, Ecoffey C, Falissard B, Mercier FJ, et al. Major complications of regional anesthesia in France: the SOS Regional Anesthesia Hotline Service. Anesthesiology 2002;97(5):1274-80. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ball 2019
- Ball CG. Surgeons as advocates for opioid control. Canadian Journal of Surgery 2019;62(4):220-1. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Berde 2009
- Berde CB, Strichartz GR. Local anesthetics (Chapter 30). In: Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL, editors(s). Miller's Anesthesia. 7th edition. London, UK: Churchill Livingstone, 2009:913-39. [Google Scholar]
Bomberg 2017
- Bomberg H, Huth A, Wagenpfeil S, Kessler P, Wulf H, Standl T, et al. Psoas versus femoral blocks: a registry analysis of risks and benefits. Regional Anesthesia and Pain Medicine 2017;42(6):719-24. [PMID: ] [DOI] [PubMed] [Google Scholar]
Brauer 2009
- Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA 2009;302(14):1573-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brull 2007
- Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesthesia and Analgesia 2007;104(4):965-74. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cates 2002
- Cates CJ. Simpson's paradox and calculation of number needed to treat from meta-analysis. BMC Medical Research Methodology 2002;2:1. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Centers for Disease Control and Prevention 2018
- National Center for Injury Prevention and Control (NCIPC), Centers for Disease Control and Prevention (CDC), US Department of Health and Human Services, Atlanta, Georgia. Annual surveillance report of drug-related risks and outcomes | United States. Available at https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillance-report.pdf (accessed 23 March 2020).
Deeks 2002
- Deeks JJ. Issues in the selection of a summary statistic for meta-analysis of clinical trials with binary outcomes. Statistics in Medicine 2002;21(11):1575-600. [PMID: ] [DOI] [PubMed] [Google Scholar]
Deeks 2019
- Deeks JJ, Higgins JPT, Altman DG. Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. Version 6.0 edition. Available at https://training.cochrane.org/handbook: Cochrane, 2019:Chapter 10. [Google Scholar]
Dizdarevic 2019
- Dizdarevic A, Farah F, Ding J, Shah S, Bryan A, Kahn M, et al. A comprehensive review of analgesia and pain modalities in hip fracture pathogenesis. Current Pain and Headache Reports 2019;23(10):72. [DOI: 10.1007/s11916-019-0814-9] [DOI] [PubMed] [Google Scholar]
Dochez 2014
- Dochez E, Geffen GJ, Bruhn J, Hoogerwerf N, de Pas H, Scheffer G. Prehospital administered fascia iliaca compartment block by emergency medical service nurses, a feasibility study. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2014;22:38. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eldridge 2016
- Eldridge S, Campbell M, Campbell M, Dahota A, Giraudeau B, Higgins JPT, et al. Revised Cochrane risk of bias tool for randomized trials (RoB 2.0): additional considerations for cluster‐randomized trials. https://www.riskofbias.info/welcome/rob-2-0-tool/archive-rob-2-0-cluster-randomized-trials-2016 (accessed 20 January 2020).
Fadhlillah 2019
- Fadhlillah F, Chan D, Pelosi P, Rubulotta F. Systematic review and meta-analysis of single injection fascia iliaca blocks in the peri- operative management of patients with hip fractures. Minerva Anestesiologica 2019;85(11):1211-8. [DOI: 10.23736/S0375-9393.19.13535-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Freeman 2016
- Freeman N, Clarke J. Perioperative pain management for hip fracture patients. Orthopaedics and Trauma 2016;30(2):145-52. [Google Scholar]
Gozlan 2005
- Gozlan C, Minville V, Asehnoune K, Raynal P, Zetlaoui P, Benhamou D. Fascia iliaca block for femoral bone fractures in prehospital medicine [Bloc iliofascial en médecine préhospitalière pour les fractures du fémur]. Annales Françaises d'Anesthésie et de Réanimation 2005;24(6):617-20. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guay 2006
- Guay J. The benefits of adding epidural analgesia to general anaesthesia: a meta-analysis. Journal of Anaesthesia 2006;20(4):335-40. [PMID: ] [DOI] [PubMed] [Google Scholar]
Guay 2006a
- Guay J. The epidural test dose: a review. Anesthesia and Analgesia 2016;102(3):921-9. [DOI: 10.1213/01.ane.0000196687.88590.6b] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guay 2016
- Guay J, Parker MJ, Gajendragadkar PR, Kopp S. Anaesthesia for hip fracture surgery in adults. The Cochrane Database of Systematic Reviews 2016;2:CD000521. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guay 2016a
- Guay J, Kopp S. Epidural pain relief versus systemic opioid-based pain relief for abdominal aortic surgery. Cochrane Database of Systematic Reviews 2016, Issue 1. Art. No: CD005059. [DOI: 10.1002/14651858.CD005059.pub4] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guay 2020
- Guay J, Kopp SL. PNBs for hip fractures in adults RoB2. Available at: https://figshare.com/articles/dataset/Guay_J_and_Kopp_SL_PNBs_for_Hip_Fractures_in_Adults_RoB2_20_May_2020_pdf/12338585 (accessed 6 November 2020). [DOI: 10.1002/14651858.CD001159.pub3] [DOI]
Haentjens 2010
- Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Annals of Internal Medicine 2010;152(6):380-90. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hards 2018
- Hards M, Brewer A, Bessant G, Lahiri S. Efficacy of prehospital analgesia with fascia iliaca compartment block for femoral bone fractures: a systematic review. Prehospital and Disaster Medicine 2018;33(3):299-307. [DOI: 10.1017/S1049023X18000365] [DOI] [PubMed] [Google Scholar]
Hartmann 2017
- Hartmann FV, Novaes MR, Carvalho MR. Femoral nerve block versus intravenous fentanyl in adult patients with hip fractures - a systematic review. Brazilian Journal of Anesthesiology 2017;67(1):67-71. [DOI: 10.1016/j.bjane.2015.08.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Haslam 2013
- Haslam L, Lansdown A, Lee J, Vyver M. Survey of current practices: peripheral nerve block utilization by ED physicians for treatment of pain in the hip fracture patient population. Canadian Geriatrics Journal 2013;16(1):16-21. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2019
- Higgins JPT, Eldridge S, Li T. Including variants on randomized trials. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. Vol. Version 6.0. Available from www.training.cochrane.org/handbook: Cochrane, 2019:Chapter 23. [Google Scholar]
Hong 2019
- Hong HK, Ma Y. The efficacy of fascia iliaca compartment block for pain control after hip fracture: a meta-analysis. Medicine 2019;98(28):e16157. [DOI: 10.1097/MD.0000000000016157] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hsu 2018
- Hsu YP, Hsu CW, Bai CH, Cheng SW, Chen C. Fascia iliaca compartment block versus intravenous analgesic for positioning of femur fracture patients before a spinal block: a PRISMA-compliant meta-analysis. Medicine 2018;97(49):e13502. [DOI: 10.1097/MD.0000000000013502] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hsu 2019
- Hsu YP, Hsu CW, Chu KCW, Huang WC, Bai CH, Huang CJ, et al. Efficacy and safety of femoral nerve block for the positioning of femur fracture patients before a spinal block: a systematic review and meta-analysis. PloS One 2019;14(5):e0216337. [DOI: 10.1371/journal. pone.0216337] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2015
- Lee LA, Caplan RA, Stephens LS, Posner KL, Terman GW, Voepel-Lewis T, et al. Postoperative opioid-induced respiratory depression: a closed claims analysis. Anesthesiology 2015;122(3):659-65. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. Version 6.0 edition. Available at www.training.cochrane.org/handbook: Cochrane, 2019:Chapter 4. [Google Scholar]
McColl 1998
- McColl A, Smith H, White P, Field J. General practitioner's perceptions of the route to evidence based medicine: a questionnaire survey. BMJ (Clinical research ed.) 1998;316(7128):361-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
National Hip Fracture Database 2019
- National Hip Fracture Database. Annual report 2019. Available at https://www.nhfd.co.uk 2019:Accessed 11 January 2020.
Neal 2015
- Neal JM, Barrington MJ, Brull R, Hadzic A, Hebl JR, Horlocker TT, et al. The Second ASRA Practice Advisory on Neurologic Complications Associated With Regional Anesthesia and Pain Medicine: Executive Summary 2015. Regional Anesthesia and Pain Medicine 2015;40(5):401-30. [PMID: ] [DOI] [PubMed] [Google Scholar]
NICE 2017
- National Institute for Health and Care. Hip fracture management. Available at https://www.nice.org.uk/Guidance/CG124 2017:Accessed 11 January 2020.
Pace 2011
- Pace NL. Research methods for meta-analyses. Best Practice & Research. Clinical Anaesthesiology 2011;25(4):523-33. [PMID: ] [DOI] [PubMed] [Google Scholar]
Parker 2016
- Parker MJ. Reducing morbidity and mortality in the hip fracture patient group. Orthopaedics and Trauma 2016;30(2):153-8. [Google Scholar]
Parkinson 1989
- Parkinson SK, Mueller JB, Little WL, Bailey SL. Extent of blockade with various approaches to the lumbar plexus. Anesthesia and Analgesia 1989;68(3):243-8. [PMID: ] [PubMed] [Google Scholar]
Pedersen 2008
- Pedersen SJ, Borgbjerg FM, Schousboe B, Pedersen BD, Jørgensen HL, Duus BR, et al. A comprehensive hip fracture program reduces complication rates and mortality. Journal of the America Geriatric Society 2008;56(10):1831-8. [DOI: 10.1111/j.1532-5415.2008.01945.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pere 2011
- Pere PJ, Ekstrand A, Salonen M, Honkanen E, Sjovall J, Henriksson J, et al. Pharmacokinetics of ropivacaine in patients with chronic renal failure. British Journal of Anaesthesia 2011;106(4):512-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pogue 1998
- Pogue J, Yusuf S. Overcoming the limitations of current meta-analysis of randomised controlled trials. Lancet 1998;351(9095):47-52. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pompei 1994
- Pompei P, Foreman M, Rudberg MA, Inouye SK, Braund V, Cassel CK. Delirium in hospitalized older persons: outcomes and predictors. Journal of the American Geriatric Society 1994;42(8):809-15. [PMID: 8046190 ] [DOI] [PubMed] [Google Scholar]
Rashiq 2013
- Rashiq S, Vandermeer B, Abou-Setta AM, Beaupre LA, Jones CA, Dryden DM. Efficacy of supplemental peripheral nerve blockade for hip fracture surgery: multiple treatment comparison. Canadian Journal of Anaesthesia 2013;60(3):230-43. [CENTRAL: CN-00906278] [DOI: 10.1007/s12630-012-9880-8] [EMBASE: 52403619] [PMID: ] [DOI] [PubMed] [Google Scholar]
RevMan 5.3 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rucker 2011
- Rucker G, Schwarzer G, Carpenter JR, Binder H, Schumacher M. Treatment-effect estimates adjusted for small-study effects via a limit meta-analysis. Biostatistics (Oxford, England) 2011;12(1):122-42. [PMID: ] [DOI] [PubMed] [Google Scholar]
Saunders 2010
- Saunders KW, Dunn KM, Merrill JO, Sullivan M, Weisner C, Braden JB, et al. Relationship of opioid use and dosage levels to fractures in older chronic pain patients. Journal of General Internal Medicine 2010;25(4):310-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G and Oxman A. GRADE Handbook. The GRADE Working Group, 2013. [Google Scholar]
Schünemann 2019
- Schünemann HJ, Vist GE, Higgins JPT, Santesso N, Deeks JJ, Glasziou P et al. Interpreting results and drawing conclusions. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. Version 6.0 edition. Available from www.training.cochrane.org/handbook: Cochrane, 2019:Chapter 15. [Google Scholar]
Scurrah 2018
- Scurrah A, Shiner CT, Stevens JA, Faux SG. Regional nerve blockade for early analgesic management of elderly patients with hip fracture - a narrative review. Anaesthesia 2018;73(6):769-83. [DOI: 10.1111/anae.14178] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shammas 1998
- Shammas FV, Dickstein K. Clinical pharmacokinetics in heart failure. An updated review. Clinical Pharmacokinetics 1988;15(2):94-113. [DOI: 10.2165/00003088-198815020-00002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Singer 2015
- Singer A, Exuzides A, Spangler L, O'Malley C, Colby C, Johnston K, et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clinic Proceedings 2015;90(1):53-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sites 2012
- Sites BD, Taenzer AH, Herrick MD, Gilloon C, Antonakakis J, Richins J, et al. Incidence of local anesthetic systemic toxicity and postoperative neurologic symptoms associated with 12,668 ultrasound-guided nerve blocks: an analysis from a prospective clinical registry. Regional Anesthesia and Pain Medicine 2012;37(5):478-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sites 2014
- Sites BD, Barrington MJ, Davis M. Using an international clinical registry of regional anesthesia to identify targets for quality improvement. Regional Anesthesia and Pain Medicine 2014;39(6):487-95. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Skjold 2019
- Skjold C, Moller AM, Wildgaard K. Pre‐operative femoral nerve block for hip fracture - A systematic review with meta‐analysis. Acta Anaesthesiologica Scandinavica 2020;64(1):23-33. [DOI: 10.1111/aas.13491] [PMID: ] [DOI] [PubMed] [Google Scholar]
Soffin 2019
- Soffin EM, Gibbons MM, Wick EC, Kates SL, Cannesson M, Scott MJ, et al. Evidence review conducted for the Agency for Healthcare Research and Quality Safety Program for Improving Surgical Care and Recovery: focus on anesthesiology for hip fracture surgery. Anesthesia and Analgesia 2019;128(6):1107-17. [DOI: 10.1213/ANE.0000000000003925] [PMID: ] [DOI] [PubMed] [Google Scholar]
Steenberg 2018
- Steenberg J, Moller AM. Systematic review of the effects of fascia iliaca compartment block on hip fracture patients before operation. British Journal of Anaesthesia 2018;120(6):1368-80. [DOI: 10.1016/j.bja.2017.12.042] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sterne 2001
- Sterne JAC, Egger M, Smith GD. Systematic reviews in health careInvestigating and dealing with publication and other biases in metaanalysis. British Medical Journal 2001;323(7304):101-5. [DOI: 10.1136/bmj.323.7304.101] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2019
- Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. British Medical Journal 2019;366:l4898. [DOI: 10.1136/bmj.l4898] [PMID: ] [DOI] [PubMed] [Google Scholar]
Thong 2018
- Thong ISK, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scandinavian Journal of Pain 2018;18(1):99-107. [DOI: 10.1515/sjpain-2018-0012] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wallace 1987
- Wallace RB, Anderson RA. Blood lipids, lipid-related measures, and the risk of atherosclerotic cardiovascular disease. Epidemiologic Reviews 1987;9:95-119. [PMID: ] [DOI] [PubMed] [Google Scholar]
Zhang 2019
- Zhang Y, Coello PA, Guyatt GH, Yepes-Nuñez JJ, Akl EA, Hazlewood G et al. GRADE guidelines: 20. Assessing the certainty of evidence in the importance of outcomes or values and preferences-inconsistency, imprecision, and other domains. Journal of Clinical Epidemiology 2019;111(July):83-93. [DOI: 10.1016/j.jclinepi.2018.05.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Guay 2017
- Guay J, Parker MJ, Griffiths R, Kopp S. Peripheral nerve blocks for hip fractures. Cochrane Database of Systematic Reviews 2017, Issue 5. Art. No: CD001159. [DOI: 10.1002/14651858.CD001159.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guay 2018
- Guay J, Parker MJ, Griffiths R, Kopp SL. Peripheral nerve blocks for hip fractures: a Cochrane review. Anesthesia and Analgesia 2018;126(5):1695-704. [PMID: ] [DOI] [PubMed] [Google Scholar]
Parker 2002
- Parker MJ, Griffiths R, Appadu BN. Nerve blocks (subcostal, lateral cutaneous, femoral, triple, psoas) for hip fractures. Cochrane Database of Systematic Reviews 2002, Issue 2. Art. No: CD001159. [DOI: 10.1002/14651858.CD001159] [DOI] [PubMed] [Google Scholar]


