Abstract
Objectives
Socioeconomic factors such as elevated incidence of chronic disease, overcrowding, and increased occupational exposure result in higher risk of infectious disease. The COVID-19 pandemic has appeared to disproportionately affect communities affected by deprivation and discrimination, who also appear to be at greater risk of severe disease. Our aim was to investigate the evolution of the socioeconomic groups affected by COVID-19 over the course of the first wave of the pandemic by examining patients presenting to an acute NHS trust.
Study design
and methods: A retrospective study using the postcodes of patients presenting to the Brighton and Sussex University Hospitals NHS Trust who tested PCR-positive for COVID-19 were used to determine average house price and index of multiple deprivation. These were used as markers of affluence to examine the trend in the socioeconomic status of affected patients from February to May 2020.
Results
384 cases were included. The postcodes of those individuals who were initially infected had higher average house prices and index of multiple deprivation, both of which followed downward trends as the outbreak progressed.
Conclusion
Our data shows that the outbreak spread from higher to lower affluence groups through the course of the pandemic. We hypothesise that this was due to wealthier individuals initially transmitting the virus from abroad. Therefore, an earlier and more effective quarantine could have reduced spread to members of the community at greater risk of infection and harm. We suggest that hospitals systematically record the socioeconomic status of affected individuals in order to monitor trends, identify those who may be at risk of severe disease, and to push for more equitable public health policy.
Keywords: COVID-19, Social determinants of health, Epidemiology, Socioeconomic status
Historically, pandemics such as the Spanish Flu of 1918 and the H1N1 outbreak in 2009 have highlighted the health inequalities inherent in our societies, with higher mortality and morbidity rates in lower socio-economic groups [1]. Similarly, COVID-19 is likely to underscore existing health inequalities. It has already been noted that people of colour are disproportionately affected [2]. A recent study in Chicago showed that COVID-19 has had an outsized impact on African-American communities whose health was already harmed by high levels of poverty and discrimination [3]. The differential impact of COVID-19 can be attributed to existing social determinants of health, notably, the increased incidence of chronic diseases in socioeconomically deprived groups and the increased occupational exposure [4].
In order to contribute to this urgent conversation, we investigated the evolution of the socioeconomic groups affected by the COVID-19 outbreak in Brighton via the changes in average house price and Index of Multiple Deprivation associated with the affected patients' postcodes using Zoopla [5] and the Ministry of Housing, Communities and Local Government's 2019 deprivation data [6]. We used these measures of affluence as a surrogate marker for socioeconomic status. Clinical setting and audit data collection methods have been described previously [7]. The patients included were only those who were swab-positive for SARS-CoV-2; those patients diagnosed radiologically were not included. The postcode data was extracted anonymously from the patient electronic records (Medway, System C, Maidstone, UK) accessed using their hospital ID number. Three affected patients were excluded from the analysis. One patient's postcode was listed as unknown, one was listed as France, and the final patient's postcode did not exist and was, therefore, presumed incorrect.
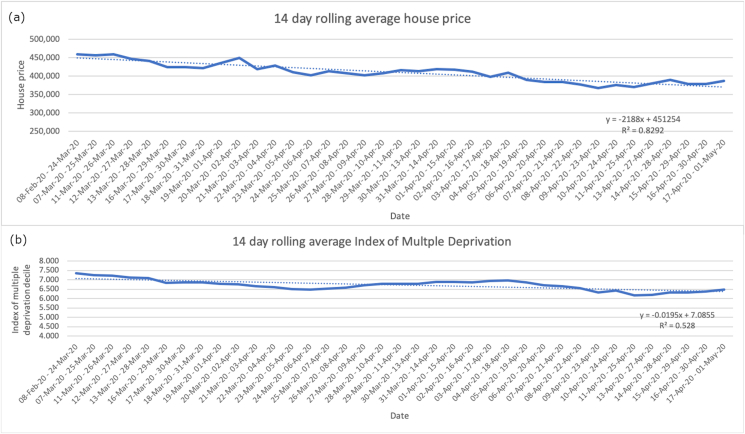
Data were collated into 14-day rolling averages of the available data points. These were plotted on a line graph against date, and line of best fit, R2 value and equation of the trendline calculated. As there were few cases initially during February and early March, all sporadic, the early rolling average incorporates a larger time period. However, the data was presented in this way to limit loss of early cases and their contribution to the trend.
384 cases were included between February 2, 2020 and May 1, 2020. The majority (281/384, 73.1%) of patients presenting to Brighton's acute hospitals had a BN postcode, denoting the Brighton area. Over the course of the COVID-19 outbreak, the house prices of the postcodes associated with the patients presenting to Brighton hospitals had a downwards trend (Fig. 1a). The equation of the line of best fit was y = -2188x + 451254, with R2 = 0.8292. The highest 14-day average house price was £459,866 between 11th and March 26, 2020. The lowest 14-day average house price was £367,756 between 9th and April 23, 2020. The 14-day rolling average of the index of multiple deprivation decile of patients testing positive also had a negative trendline (Fig. 1b). The equation of the line of best fit is y = -0.0195x + 7.0855 and R2 = 0.528. The highest average index of multiple deprivation decile was 7.351 in patients testing positive between February 8, 2020 and March 24, 2020. The lowest average decile was 6.157 in patients testing positive between 11th and April 25, 2020.
Fig. 1.
(a) The change in 14-day rolling house price of the postcodes associated with patients testing positive for COVID-19 in Brighton and Sussex. (b) The change in 14-day rolling average of index of multiple deprivation decile of the postcodes of patients testing positive for COVID-19 in Brighton and Sussex.
Our data suggest that the COVID-19 outbreak between February and May 2020 spread from affluent areas to less affluent areas based on average house price and the Index of Multiple Deprivation according to the addresses of patients diagnosed with the disease. Brighton was affected relatively early in the course of pandemic in the UK, and was home to one of the first cases in the country [8]. We suggest that the initial outbreak was triggered by those from wealthier socioeconomic groups returning to Brighton after being exposed to the virus abroad. They then returned to the UK and interacted with other individuals as normal, unaware that they were transmitting the virus. If this assertion is correct, then spread of COVID-19 could have been mitigated by instituting a 14-day quarantine for returning travellers from all countries earlier. While such measures are costly for those subject to them, wealthier individuals are more likely to have the material resources to cope with this situation. Such a quarantine at the time of the first case in Brighton was only instituted for those who were unwell following recent travel to China, Thailand, Japan, Republic of Korea, Taiwan, Singapore, Malaysia, Hong Kong and Macau [8]. Given that 21 of 35 of early cases of COVID-19 in Europe were infected in Europe itself [9], rather than any of the above countries, a more evidence-based approach for quarantining at the outset of the pandemic might have reduced early transmission.
Socioeconomic factors are associated with higher risk of serious disease from COVID-19 [4]. This is a specific case of a more general trend. Multiple compounding social determinants of health which put certain groups at higher risk of infectious diseases are already widely noted, such as overcrowding, malnutrition, higher occupational exposure, all of which contribute to higher rates of chronic disease and worse health outcomes [4]. While the trend of infection appears to have been from higher earners to lower earners, it is likely that lower earners were more likely to be infected once the outbreak was well established due to decreased ability to protect themselves. As a rule, higher earners are more likely to be able to work from home, while many lower-earners working in the service and care sectors did not have this option [10], leaving them at greater risk of occupational exposure. We also hypothesise that a range of material factors, such as the ability to work from home, purchase personal protective equipment, and switch to safer services including online shopping, would have conferred a protective advantage on those with greater financial means.
In order to improve the quality of care during the on-going COVID-19 pandemic, currently progressing through a second wave in the UK, and indeed any future pandemic outbreaks, social determinants of health must be at the centre of our preparation and response. We suggest that earlier interventions to prevent spread from overseas returning travellers could have reduced spread to more vulnerable groups and prevented excess morbidity and mortality. In addition, hospitals should be advised to collect data on the socioeconomic status of patients who are admitted with COVID-19, and other future pandemic infectious diseases, in order to accurately study the dynamic trends of the outbreak. Finally, we advise that clear and concise health information relating to the pandemic should be given to all patients attending hospitals, GP practices and pharmacy services, to aid the public in understanding their risk, and that personal protective equipment should be distributed to all who need it.
One of the limitations of our study is that house prices and index of multiple deprivation are only a few of ways of measuring socio-economic status of our affected patients. For example, for a more holistic picture, we could have collected information about occupation or salary from our patients. In addition, while the average house price for each postcode was clearly not representative of each individual's socioeconomic status, it did provide a useful surrogate measure of the average affluence of patients over time that could be used to track dynamic changes in the pandemic. Finally, we acknowledge that our data only incorporates patients affected in the first wave of the COVID-19 pandemic and that the distribution of socioeconomic status may be different for patients with COVID-19 in the second wave.
Our data shows that the COVID-19 outbreak in Brighton originated in more affluent groups and spread to lower affluence individuals. We believe that a plausible explanation for this is wealthier individuals returning to Brighton following exposure to the virus abroad and then unwittingly bringing it back and facilitating its transmission. Given existing health inequalities in socioeconomically deprived groups, we contend that the government should have taken stronger action to protect those most vulnerable from disease by instituting earlier and more universal quarantine. In addition, every healthcare setting can improve the quality of its care by ensuring it collects socioeconomic data on affected patients and by providing clear health information and protective resources to assist individuals in minimising their personal risk.
Author statement
TC formulated the research question and supervised the project. TC and EC collected and collated the data. BS analysed the data and drafted the manuscript. TC and AS contributed to the data analysis and edited the manuscript.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
No acknowledgements. Patient data was collected as part of a quality improvement project and all patient data was anonymised. This research received no financial support. No conflicts of interests are declared.
Contributor Information
B.R.H. Sturrock, Email: beattie.sturrock@yahoo.co.uk.
T.J.T. Chevassut, Email: t.chevassut@bsms.ac.uk.
References
- 1.Bambra C., Riordan R., Ford J., Matthews F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health. 2020 Jun 13 doi: 10.1136/jech-2020-214401. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7298201/ [Internet] [cited 2020 Jun 27];jech-2020-214401. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dorn A van, Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020 Apr;395(10232):1243–1244. doi: 10.1016/S0140-6736(20)30893-X. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7162639/ [cited 2020 Jul 12] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim S.J., Bostwick W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ. Behav. 2020 Aug 21;47(4):509–513. doi: 10.1177/1090198120929677. http://www.ncbi.nlm.nih.gov/pubmed/32436405 [cited 2020 Jul 12] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel J.A., Nielsen F.B.H., Badiani A.A., Assi S., Unadkat V.A., Patel B., et al. vol. 183. Public Health. Elsevier B.V.; 2020. pp. 110–111.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7221360/ (Poverty, Inequality and COVID-19: the Forgotten Vulnerable [Internet]). [cited 2020 Jul 12] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zoopla . 2020. House prices and values.https://www.zoopla.co.uk/house-prices/ [Internet]. [cited 2020 Jun 27]. Available from: [Google Scholar]
- 6.Ministry of Housing Communities & Local Government . 2020. English indices of deprivation 2019: postcode Lookup.http://imd-by-postcode.opendatacommunities.org/imd/2019 [Internet]. [cited 2020 Jun 27]. Available from: [Google Scholar]
- 7.Stoneham S.M., Milne K.M., Nuttal E., Frew G.H., Sturrock B.R., Sivaloganathan H., et al. Thrombotic risk in COVID-19: a case series and case–control study. Clin. Med. (Northfield Il) 2020 May 18 doi: 10.7861/clinmed.2020-0228. https://pubmed.ncbi.nlm.nih.gov/32423903/ [Internet] [cited 2020 Jun 27];clinmed.2020-0228. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.BBC News Coronavirus: third UK patient “caught coronavirus in Singapore”. BBC news. 2020 https://www.bbc.co.uk/news/uk-51398039 [Internet] [cited 2020 Jul 13]. Available from: [Google Scholar]
- 9.Spiteri G., Fielding J., Diercke M., Campese C., Enouf V., Gaymard A., et al. vol. 25. Eurosurveillance. European Centre for Disease Prevention and Control (ECDC); 2020. p. 1.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7068164/ (First Cases of Coronavirus Disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020 [Internet]). [cited 2020 Jul 13] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mobility Commission S. 2019. The adult skills gap: is falling investment in UK adults stalling social mobility?https://feweek.co.uk/wp-content/uploads/2019/01/Social-Mobility-Commission-adult-skills-report.pdf [Internet] [cited 2020 Aug 15]. Available from: [Google Scholar]