Abstract
Background
Studies show patients may have gender or racial preferences for physicians.
Objective
To determine the degree to which physicians’ gender and name characteristics influenced physician clinical load in medical practice, including patient panel size and percent of slots filled.
Design
Observational cohort study of a continuity clinic site in Rochester, MN, from July 1, 2015 to June 30, 2017 (“historical” period) and July 1, 2018 to January 30, 2020 (“contemporary” period).
Participants
Internal medicine resident physicians.
Main Measures
Resident gender, name, and race came from residency management system data. Panel size, percent of appointment slots filled (“slot fill”), panel percent female, and panel percent non-White came from the electronic health record. Multivariable linear regression models calculated beta estimates with 95% confidence intervals and R2 for the impact of physician gender, surname origin, name character length, and name consonant-to-vowel ratio on each outcome, adjusting for race and year of residency.
Key Results
Of the 307 internal medicine residents, 122 (40%) were female and 197 (64%) were White. Their patient panels were 51% female (SD 16) and 74% White (SD 6). Female gender was associated with a 5.3 (95% CI 2.7–7.9) patient increase in panel size and a 1.5% (95% CI −0.6 to 3.7) increase in slot fill. European, non-Hispanic surname was associated with a 5.3 (95% CI 2.6–7.9) patient increase in panel size and a 4.3 percent (95% CI 2.1–6.4) increase in slot fill. Race and other name characteristics were not associated with physician clinical load. From the historical to contemporary period, the influence of name characteristics decreased from 9 to 4% for panel size and from 15 to 5% for slot fill.
Conclusions
Female gender and European, non-Hispanic surname origin are associated with increased physician clinical load—even more than race. While these disparities may have serious consequences, they are also addressable.
Electronic supplementary material
The online version of this article (10.1007/s11606-020-06296-x) contains supplementary material, which is available to authorized users.
KEY WORDS: gender, surname, race, physician, patient
INTRODUCTION
Recent tragic events in the USA, including the deaths of George Floyd and Rayshard Brooks, have sparked national riots and civil unrest, but they are also inspiring society to face and address systematic racism and racial bias that exist throughout our country’s infrastructure. And healthcare is not immune. There is a unifying call for us to not be mere bystanders but rather a part of the solution by evaluating for the ways bias is affecting those we work with and serve.
Studies have shown that patients may select their physicians based on not only their capabilities, such as experience and knowledge,1 but also their demographics, such as gender and race. For example, many studies show that patients have gender preferences for their physicians,1–6 and physicians may see more visits for patients of the same gender.7,8 One study also showed participants rated the performance quality of hypothetical physicians differently based on not only the gender but also the race of the names, with a preference for White, male names.9 Outside of the medical field, easy-to-pronounce names10 and names more similar to oneself11 are judged more positively, while non-White names are perceived more negatively.12 Together, these differential preferences based on gender, race, and name are important, as they may translate into disparities in clinical load and training experience for resident physicians based on their name, race, or gender.
Anecdotal evidence in our internal medicine (IM) resident continuity clinic suggested a discrepancy in patient panel size and composition by physician gender. On further review, we also noticed a difference by physician surname origin and/or complexity. To our knowledge, no study to date has evaluated the degree to which specific name characteristics influence physician clinical load or panel composition in a medical practice setting.
To explore this further, we aimed to determine the degree to which physicians’ gender and name influenced their clinical load, as measured by panel size and slot fill. Second, we aimed to investigate whether physicians’ names influenced the composition of their patient panel, as measured by percent of patients who were female or non-White.
METHODS
Study Design and Participants
This observational cohort study included all IM resident physicians who worked in the Mayo Clinic Department of IM Primary Care Clinic in Rochester, MN, between July 1, 2015 and January 30, 2020. This clinic serves patients who reside in southern Minnesota and western Wisconsin, of whom approximately 53% are female, 88% are White, 3% Black, 2% Asian, 3% Other or mixed, and 4% unknown.13,14 Patients are empaneled and scheduled to see residents based on first availability, though when multiple residents are available, the patients and/or staff in charge of empanelment and scheduling can decide. We obtained data in two time periods, termed the “historical” period (July 1, 2015 to June 30, 2017) and “contemporary” period (July 1, 2018 to January 30, 2020) due to an electronic health record (EHR) transition that occurred May 2018.
In addition to reporting all data together, we also reported it separately for the historical and contemporary periods. We did this because on July 1, 2018, IM residents merged from two separate continuity clinics on campus to one, integrated continuity clinic (of note, this explains the drop in mean panel size, as existing continuity clinic patients were divided among a larger number of residents). In addition, in response to testimonials from schedulers that they offered appointments more readily for physicians whose names they felt confident in pronouncing, clinic leadership provided phonetic pronunciation information to the offices responsible for assigning patients to panels and clinic slots in March of 2019. Previously, the empanelment process also largely assigned intact panels to incoming residents, and assigned new patients to open panels based on patient preferences, without consideration of panel size. Clinic leadership therefore made a concerted effort to balance panel size for the residents starting July 1, 2019. The historical period thus served as a “control” comparator before the effects of these interventions occurred.
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies,15 received approval from the Mayo Clinic Institutional Review Board (19-006746) on August 13, 2019, and complied with the Declaration of Helsinki.
Measures
Primary outcome data for this study, including panel size and percent of appointment slots filled (“slot fill”), came from EHR reporting tools. To allow more time for external influence on panel size to accrue, we calculated panel size and composition by averaging the resident’s most recent four quarters of data. We calculated slot fill percent in the historical period by dividing the total number of filled slots by the total number of available slots for the entire time period. Slot fill in the contemporary period came directly from a reporting tool in the EHR. Secondary outcomes of interest including panel percent female and percent non-White were available only for the historical period.
Demographic variables, including physician gender and name, came from the residency management system data that each resident provided when they matched to the IM residency program. As of April 18, 2019, a complete literature search of the PsycINFO, Cochrane, MEDLINE, and Embase databases on the topic of provider or patient characteristics, preferences, or biases showed no prior studies examining the impact of provider name on clinical load. Therefore, we created our own variables for other potentially influential name characteristics. We manually abstracted surname origin using an online ancestry website.16 Surnames originating from Western European countries including Austria, Belgium, Denmark, England, Finland, France, Germany, Ireland, Netherlands, Norway, Sweden, and Switzerland were categorized as “European, non-Hispanic.”17 We also manually calculated first and last name character length and first and last name consonant-to-vowel ratio. Covariates including physician race and year of residency came from residency management system data as well.
Statistical Analyses
We used means, standard deviations, and t tests for normal, continuous variables; medians, interquartile ranges, and Mann-Whitney tests for non-normal, continuous variables; and proportions and chi-square tests for categorical variables. For our first aim, we performed multivariable linear regression models with physician gender, surname country of origin, first and last name character length, and first and last name consonant-to-vowel ratio as the exposures of interest and panel size or slot fill percent as the outcome, adjusting for race (dichotomized as White, non-Hispanic versus other due to small numbers of other races) and year of residency. For our second aim, we ran the same models with panel percent female or panel percent non-White as the outcome. Beta coefficients and their 95% confidence intervals (CI) from these models indicated the degree to which each exposure influenced the outcome of physician clinical load. We used the models’ coefficient of determination (R2) to measure how much of the observed clinical load could be attributed to name-related factors.
For sensitivity analyses, we performed subgroup analyses for different races (White non-Hispanic, Asian, Indian [Asia], and Other) and tested multiplicative interactions between surname character length, origin, and consonant-to-vowel ratio. Because of moderate collinearity between surname origin and race (0.5 to 0.7), we ran separate models for race and surname origin. None of the residents was missing any data. All analyses were pre-specified in a protocol and performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
RESULTS
Demographics
Of the 307 IM residents included in this study, 122 (40%) were female, 197 (64%) were White, non-Hispanic race, and 203 (66%) had European, non-Hispanic surname origin (Table 1). Importantly, 47 (15%) were discordant for White race versus surname. In comparison, their patient panels were 51% female (SD 16) and 74% White (SD 6) (Table 1).
Table 1.
Baseline Characteristics of All 307 Resident Physicians and Their Primary Care Clinic Panels
| Characteristic | Full cohort (N = 307)b | Historical cohort (N = 131) | Contemporary cohort (N = 205) |
|---|---|---|---|
| Female gender, N (%) | 122 (40) | 56 (43) | 83 (40) |
| Race, N (%) | |||
| White, non-Hispanic | 197 (64) | 88 (68) | 128 (62) |
| Asian | 44 (14) | 20 (15) | 28 (14) |
| Indian (Asia) | 23 (7) | 10 (7) | 14 (7) |
| Other | 42 (14) | 13 (10) | 35 (17) |
| Most recent year of residency (%) | |||
| First | 56 (18) | 33 (25) | 52 (25) |
| Second | 86 (28) | 22 (25) | 53 (26) |
| Third | 165 (54) | 65 (50) | 100 (49) |
| Surname origin European non-Hispanic, N (%) | 203 (66) | 86 (65) | 134 (65) |
| Character length first name, median (IQR) | 6 (5, 7) | 6 (5, 7) | 6 (5, 7) |
| Character length surname, median (IQR) | 6 (5, 8) | 6 (5, 8) | 6 (5, 7) |
| Consonant/vowel ratio first name, median (IQR) | 1.2 (1.0, 2.0) | 1.3 (1.0, 1.7) | 1.3 (1.0, 1.7) |
| Consonant/vowel ratio surname, median (IQR) | 2.0 (1.0, 2.5) | 2.0 (1.2, 3.0) | 2.0 (1.3, 2.5) |
| Panel size, mean (SD)ͣ | 88 (13) | 95 (7) | 84 (14) |
| Panel percent female, mean (SD)ͣ | 51 (16) | 51 (16) | N/A |
| Panel percent non-White, mean (SD)ͣ | 26 (6) | 26 (6) | N/A |
| Slot fill percent, mean (SD) | 77 (11) | 84 (5) | 74 (12) |
IQR, interquartile range; N/A, not applicable; SD, standard deviation
aBased on average of the most recent four quarters
b29 residents worked in both time periods
Panel Size
After adjusting for resident year, gender, and other name characteristics, female gender was associated with a 5-person increase in panel size compared to male gender (Table 2). Having a European, non-Hispanic surname origin was also associated with a 5-person increase in panel size (Table 2). Given the mean panel size of 88, being a female physician with a European, non-Hispanic name was therefore associated with a 12% increase in panel size compared to male peers with non-European or Hispanic surnames.
Table 2.
Adjusted Relationship Between Physician Name Characteristics and Continuity Clinic Panel Size
| Characteristic | Beta estimate (95% Cl)ͣ | ||
|---|---|---|---|
| Full cohort (N = 307) | Historical cohort (N = 131) | Contemporary cohort (N = 205) | |
| Female gender | 5.3 (2.7, 7.9) | 1.5 (− 0.9, 4.0) | 7.3 (4.0, 10.6) |
| Race White, non-Hispanic | 0.6 (− 2.9, 4.1) | 1.7 (− 1.1, 5.5) | − 0.31 (− 4.7, 4.1) |
| Surname origin European, non-Hispanic | 5.3 (2.6, 7.9) | 3.9 (1.4, 6.4) | 6.8 (3.4, 10.2) |
| Character length first name | 0.3 (− 0.4, 1.0) | 0.3 (− 0.3, 0.9) | 0.0 (− 1.0, 1.0) |
| Character length surname | 0.3 (− 0.2, 0.9) | − 0.2 (− 0.7, 0.3) | 0.1 (− 0.6, 0.8) |
| Consonant/vowel ratio first name | 0.9 (− 0.9, 2.7) | 1.2 (− 0.8, 3.3) | 1.2 (− 1.0, 3.3) |
| Consonant/vowel ratio surname | 0.1 (− 1.2, 1.4) | 0.2 (− 1.2, 1.5) | 0.0 (− 1.6, 1.6) |
CI, confidence interval
aAdjusting for resident year, gender, surname origin, first and last name character length, and first and last name consonant/vowel ratio. Italic values are statistically significant
While White, non-Hispanic race was associated with increased panel size when not adjusting for surname origin (3.8, 95% CI 1.0–6.5), after including adjusting for surname origin, it was not associated with panel size (Table 2). In a sensitivity analysis examining racial subgroups, Indian race was associated with smaller panel size (− 5.4, 95% CI − 11 to − 0.1), whereas Asian and Other race were not (1.2, 95% CI − 3.7 to 6.1 and 0.3, 95% CI − 3.6 to 4.3, respectively). The percent of panel size attributable to name characteristics (as reflected by the model’s R2 value) was 8.9% in the historical period, and decreased to 4.2% in the contemporary period.
Panel Size over Time
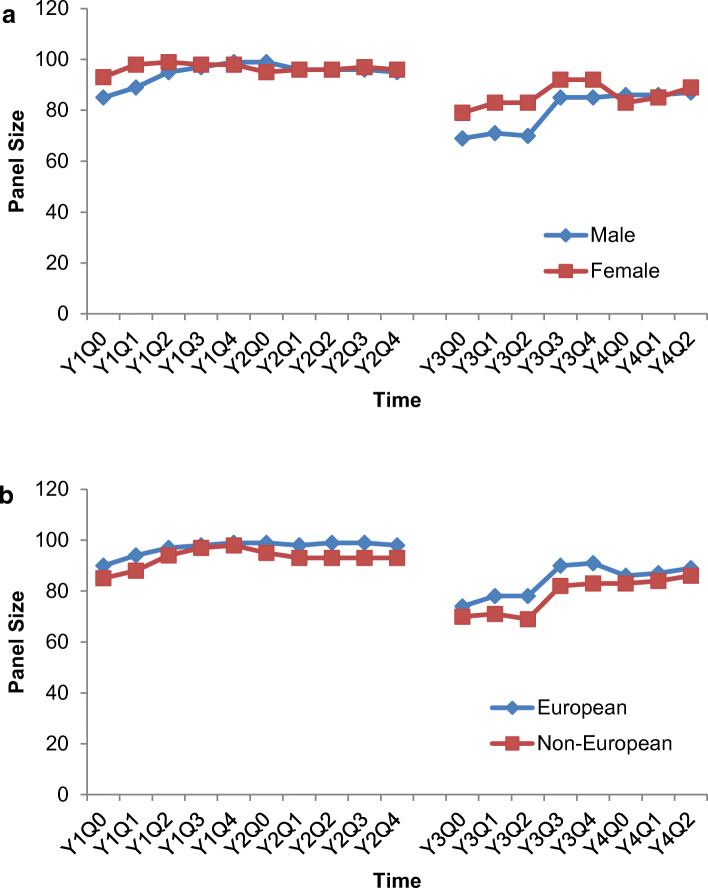
Panel size stratified by gender and surname origin showed evidence of fluctuation over time (Fig. 1). In particular, the gender gap within the contemporary period narrowed in April 2019 (Y3Q3) and then completely reversed at the start of the 2019–2020 academic year (Y4Q0) (Fig. 1a). However, the gap began to widen again in the following two quarters (Fig. 1a).
Fig. 1.
Continuity clinic panel size over time, stratified by physician gender (a) and surname origin (b). “Y” signifies the academic year, where Y1 was the 2015–2016 academic year, Y2 2016–2017, Y3 2018–2019, and Y4 2019–2020. “Q” denotes the quarter, where July 8 was Q0, October 1 was Q1, January 1 was Q2, April 1 was Q3, and June 1 was Q4.
Similarly, the surname origin gap narrowed in April 2019 (Y3Q3) and then nearly equalized at the start of the 2019–2020 academic year (Y4Q0) (Fig. 1b). In contrast, the surname origin gap widened in the second academic year of the historical period (Fig. 1b).
Slot Fill
After adjusting for resident year and name characteristics, European, non-Hispanic surname was associated with approximately 4% increase in slot fill (Table 3). Female gender was not associated with slot fill in the full cohort, though was associated with a 1.6% increase in slot fill compared to males in the historical period (Table 3). White, non-Hispanic race was not associated with increased slot fill (Table 3), even when not adjusting for surname origin (0.2, 95% CI − 2.6 to 3.0). A sensitivity analysis of the racial subgroups showed that none of the races was associated with a difference in appointment slot fill (Asian 0.8, 95% CI − 3.2 to 4.8; Indian − 0.7, 95% CI − 5.0 to 3.7; Other − 0.5, 95% CI − 3.8 to 2.8). The percent of slot fill percent attributable to name characteristics was 15% in the historical period and decreased to 5.3% in the contemporary period.
Table 3.
Adjusted Relationship Between Physician Name Characteristics and Continuity Clinic Slot Fill Percent
| Characteristic | Beta estimate (95% Cl)ͣ | ||
|---|---|---|---|
| Full cohort (N = 307) | Historical cohort (N = 131) | Contemporary cohort (N = 205) | |
| Female gender | 1.5 (− 0.6, 3.7) | 1.6 (0.04, 3.2) | 0.0 (− 2.0 (2.1) |
| Race White, non-Hispanic | 1.4 (− 2.6, 3.0) | 0.91 (− 1.2, 3.0) | − 0.4 (− 3.1, 2.4) |
| Surname origin European, non-Hispanic | 4.3 (2.1, 6.4) | 2.8 (1.2, 4.3) | 3.2 (1.0, 5.3) |
| Character length first name | 0.3 (− 0.2, 0.9) | 0.3 (− 0.1, 0.7) | 0.4 (− 0.2, 1.0) |
| Character length surname | 0.1 (− 0.4, 0.5) | − 0.2 (− 0.5, 0.1) | − 0.1 (− 0.5, 0.4) |
| Consonant/vowel ratio first name | − 0.4 (− 1.9, 1.0) | − 0.1 (− 1.4, 1.2) | 0.1 (− 1.2, 1.5) |
| Consonant/vowel ratio surname | − 0.3 (− 1.4, 0.8) | 0.6 (− 0.2, 1.4) | − 0.1 (− 1.1, 0.9) |
CI, confidence interval
ͣAdjusting for resident year, gender, surname origin, first and last name character length, and first and last name consonant/vowel ratio. Italic values are statistically significant
Panel Composition
Like panel size and slot fill, panel composition varied by physician name characteristics. After adjustment, female gender was associated with a 28% increase in the percent of panel that was female (Table 4). Given the mean panel size of 95, this corresponded to 27 more female patients. In contrast, both female gender and European, non-Hispanic physician names were associated with a slight (2 to 3 person) decrease in patients with non-White race (Table 4). Character length and consonant-to-vowel ratio of the physician name was not associated with any of the outcomes in this study. In addition, no interactions were significant (p < 0.05) and were thus not included in the models.
Table 4.
Adjusted Relationship Between Physician Name Characteristics and Continuity Clinic Panel Gender and Racial Composition for the 131 Resident Physicians in the Historical (2017–2017) Cohort
| Characteristic | Beta estimate (95% Cl)* | |
|---|---|---|
| Panel percent female | Panel percent non-White | |
| Female gender | 28 (24, 32) | − 2.8 (− 4.9, − 0.7) |
| Race White, non-Hispanic | 0.22 (− 3.2, 4.8) | − 2.0 (− 4.8, 0.85) |
| Surname origin European, non-Hispanic | 1.9 (− 1.8, 5.5) | − 2.3 (− 4.5, − 0.2) |
| Character length first name | 0.30 (− 0.60, 1.2) | 0.0 (− 0.53, 0.53) |
| Character length surname | 0.58 (− 0.12, 1.3) | − 0.24 (− 0.65, 0.17) |
| Consonant/vowel ratio first name | 0.16 (− 2.8, 3.1) | − 0.50 (− 2.2, 1.2) |
| Consonant/vowel ratio surname | − 0.66 (− 2.57, 1.24) | − 0.35 (− 1.4, 0.80) |
CI, confidence interval
*Adjusting for resident year, gender, surname origin, first and last name character length, and first and last name consonant/vowel ratio. Italic values are statistically significant
DISCUSSION
In this observational cohort study of one IM resident continuity clinic, physicians with female gender and European, non-Hispanic surname origin had evidence of higher clinical load, as measured by patient panel size and slots filled. In fact, surname origin was a stronger predictor of clinical load than race, suggesting that future studies of physician selection should incorporate this factor. Importantly, certain interventions may correct these disparities.
Several reasons might explain why female gender and European, non-Hispanic surname were associated with higher panel size and slot fill. First, it may reflect an underlying perception among patients or schedulers that such providers are superior in some way. Several studies show that female physicians provide more counseling,18–20 empathy,18,20 and preventive services19,20 than their male counterparts, resulting in higher patient satisfaction21 and lower mortality and readmission,22 while another study showed that adults rate hypothetical White providers superiorly to African American or Middle Eastern providers of the same quality.9 It might also reflect a preference for similarity, with surname origin being a proxy for a provider’s race.11 Such requests for similarity in gender or race (via surname origin) would disproportionately increase female and European, non-Hispanic surname residents’ panel sizes simply because there were fewer of them to absorb such requests compared to the patient population served. Therefore, establishing a distribution of resident physicians that matches the distribution of patients they serve may be important. Such balance would also align with the growing movement to increase workforce diversity, given increasing recognition of racial and ethnic disparities in medicine.23–25
The observed differences in panel composition might produce substantial disparity in training experience, workload, and potentially well-being for residents. Similar to our findings, residents in a family medicine training program also saw more health visits for patients of the same sex.7 The decrease in non-White patients among female residents with European, non-Hispanic names also reflects a reduction in racial diversity exposure. Because female and male patients each require unique health maintenance testing and procedures, and because of increased recognition of the phenomenon of “institutional racism” in healthcare,24 the imbalanced panel composition among residents may have serious implications for training programs, which strive to train competent physicians of all genders. Perhaps as a result of having more female patients and patients with complex psychosocial issues,7,8,26 female physicians have longer visit duration, especially with female patients.8,18 On top of that, we observed that female residents with European, non-Hispanic surnames had a 12% increase in panel size compared to their peers. A recent study showed that physicians spend 85 min managing their inbox per work day (or 32 h per month),27 meaning this difference could translate to an additional 4 h of work per month. These differences may further impact well-being, as female physicians are known to have a higher rate of burnout than their male colleagues.26,28
The observed name selection preference may even have societal impacts. In competitive healthcare environments where physician supply exceeds demand, such an impact of patient bias could have financial or patient satisfaction consequences. To illustrate, in the contemporary period, the clinic had 4993 open slots per year, with 5.3% of slot fill attributable to name characteristics, and a cost per visit that was typically several hundred dollars.29 Multiplying these together, name characteristics could be associated with hundreds of thousands of dollars in lost earnings per year if patients elected to pursue care elsewhere. Furthermore, a study of immigrant women showed that patients may experience psychological distress and delay or avoid care if openings are not available for a female physician.5 In other words, if patients choose to switch or delay care when preferred physicians are not available, even a small amount of name bias could result in significant revenue and health loss.
Fortunately, these disparities may be addressed through three types of interventions. First, clinics can manually reverse the disparities in empanelment. Such efforts can be effective, as shown by the decrease in physician clinical load attributable to name characteristics from historical to contemporary time period as well as the improvement of panel size by gender and surname in March 2019 and July 2019, coinciding with the clinic-wide pronunciation and panel size interventions. However, the gradual re-separation of panel size by gender after these interventions suggests that constant vigilance may be required to maintain equalization. Second, clinics can synchronize physician characteristics with patient characteristics by recruiting a workforce that reflects the population they will be serving. However, this synchronization may not always be possible or appropriate. Third, and perhaps most effectively, clinics can provide patients and/or schedulers with information about physicians other than just their names. Several studies have shown that the degree of patients’ gender and racial preferences decreases when they receive more information about physician characteristics,1,2,6 and their satisfaction may increase.30 Even just a few descriptors decreased patients’ same-gender preference from 80 to 60%.1,2 Future studies should investigate whether providing even a small amount of information about the physician can offset physician clinical load disparities.
This study has several important limitations. First, these results may not generalize to practices in other locations with different compositions and ratios of physicians and patients. For example, the patient population in this study had a higher percentage female and White race than the physicians, which might explain why female physicians with European, non-Hispanic surnames had higher clinical load. However, even if the compositions and therefore disparities are flipped in other practices, awareness and attempts to address them are still important. Second, because of the EHR transition that occurred on May 2018, data on slot fill for the contemporary period may not have been fully accurate at the start of the contemporary period. Similarly, the continuity clinic integration on July 1, 2018, reduced overall panel size and might have also influenced physician clinical load in other, artificial ways. Finally, residual confounding is possible, such as bias by those empaneling and scheduling patients, proactivity of residents in recruiting patients to their panels and scheduling return visits, and day of the week (for slot fill). Future work should seek to understand the reason for patients’ demographic preferences and determine whether the primary driver of these disparities is truly patient preference, racial and gender bias, or other system factors.
In conclusion, ensuring resident physicians, regardless of their name, gender, or race, are given equitable training experiences warrants ongoing considerations and study. This study showed that gender and surname origin may affect physician clinical load, and that surname origin may be more influential than race. While these disparities can have serious consequences in both resident and general practices, they may be addressable through concerted and continued interventions.
Electronic supplementary material
(DOCX 16 kb)
(DOCX 40 kb)
Acknowledgments
The authors wish to thank the Mayo Clinic Internal Medicine Research in Education Group (IMREG) for their support and insights for this project.
Compliance with Ethical Standards
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational studies,15 received approval from the Mayo Clinic Institutional Review Board (19-006746) on August 13, 2019, and complied with the Declaration of Helsinki.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guile MW, Schnatz PF, O’Sullivan DM. Relative importance of gender in patients’ selection of an obstetrics and gynecology provider. Conn Med. 2007;71(6):325–332. [PubMed] [Google Scholar]
- 2.Schnatz PF, Murphy JL, O’Sullivan DM, Sorosky JI. Patient choice: comparing criteria for selecting an obstetrician-gynecologist based on image, gender, and professional attributes. Am J Obstet Gynecol. 2007;197(5):548.e541–547. doi: 10.1016/j.ajog.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 3.Al-Omar BA, Saeed KS. Factors influencing patients’ utilization of primary health care providers in saudi arabia. J Family Community Med. 1998;5(2):23–30. [PMC free article] [PubMed] [Google Scholar]
- 4.Odunukan OW, Abdulai RM, Hagi Salaad MF, Lahr BD, Flynn PM, Wieland ML. Provider and interpreter preferences among Somali women in a primary care setting. J Prim Care Community Health. 2015;6(2):105–110. doi: 10.1177/2150131914552846. [DOI] [PubMed] [Google Scholar]
- 5.Aubrey C, Chari R, Mitchell BFP, Mumtaz Z. Gender of Provider-Barrier to Immigrant Women’s Obstetrical Care: A Narrative Review. J Obstet Gynaecol Can. 2017;39(7):567–577. doi: 10.1016/j.jogc.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 6.Amir H, Beri A, Yechiely R, Amir Levy Y, Shimonov M, Groutz A. Do Urology Male Patients Prefer Same-Gender Urologist? Am J Mens Health. 2018;12(5):1379–1383. doi: 10.1177/1557988316650886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garrison GM, Gentile N, Lai B, Angstman KB, Bonacci R. Differential Experience With Men’s and Women’s Health Care Visits Between Male and Female Family Medicine Residents. Fam Med. 2016;48(7):546–550. [PubMed] [Google Scholar]
- 8.Franks P, Bertakis KD. Physician gender, patient gender, and primary care. J Womens Health (Larchmt). 2003;12(1):73–80. doi: 10.1089/154099903321154167. [DOI] [PubMed] [Google Scholar]
- 9.Greene J, Hibbard JH, Sacks RM. Does the Race/Ethnicity or Gender of a Physician’s Name Impact Patient Selection of the Physician? J Natl Med Assoc. 110(3):206-211. [DOI] [PubMed]
- 10.Nakayama M, Saito S. Please do not judge me by my name: Effects of within-item phonological similarity and phonotactic frequencies on judgement of name impression. Cognitive Studies: Bulletin of the Japanese Cognitive Science Society. 2015;22(3):456–462. [Google Scholar]
- 11.Garner R. What’s in a Name? Persuasion Perhaps. J Consum Psychol. 2005;15(2):108–116. doi: 10.1207/s15327663jcp1502_3. [DOI] [Google Scholar]
- 12.Anderson-Clark TN, Green RJ, Henley TB. The relationship between first names and teacher expectations for achievement motivation. J Lang Soc Psychol. 2008;27(1):94–99. doi: 10.1177/0261927X07309514. [DOI] [Google Scholar]
- 13.St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41(6):1614–1624. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rocca WA, Grossardt BR, Brue SM, et al. Data Resource Profile: Expansion of the Rochester Epidemiology Project medical records-linkage system (E-REP) Int J Epidemiol. 2018;47(2):368–368j. doi: 10.1093/ije/dyx268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 16.MyHeritage. MyHeritage Ltd. www.myheritage.com. Published 2020. Accessed 15 April 2020.
- 17.ADL Global 100 List of Countries: Western Europe. Anti-Defamation League. https://www.adl.org/sites/default/files/documents/assets/pdf/press-center/Global-A-S-Survey-Countries.pdf. Published 2014. Accessed 4 March, 2020.
- 18.Roter DL, Hall JA. Physician gender and patient-centered communication: a critical review of empirical research. Annu Rev Public Health. 2004;25:497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- 19.Flocke SA, Gilchrist V. Physician and patient gender concordance and the delivery of comprehensive clinical preventive services. Med Care. 2005;43(5):486–492. doi: 10.1097/01.mlr.0000160418.72625.1c. [DOI] [PubMed] [Google Scholar]
- 20.Linzer M, Harwood E. Gendered Expectations: Do They Contribute to High Burnout Among Female Physicians? J Gen Intern Med. 2018;33(6):963–965. doi: 10.1007/s11606-018-4330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmid C, Tjan TD, Welp H, Klotz S, Scheld HH. Implantation of a right heart assist device without a heart-lung machine in a patient with an acontractile right ventricle and HIT Type II. Thorac Cardiovasc Surg. 2007;55(6):398–399. doi: 10.1055/s-2006-955944. [DOI] [PubMed] [Google Scholar]
- 22.Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of Hospital Mortality and Readmission Rates for Medicare Patients Treated by Male vs Female Physicians. JAMA Intern Med. 2017;177(2):206–213. doi: 10.1001/jamainternmed.2016.7875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richardson LD, Babcock Irvin C, Tamayo-Sarver JH. Racial and ethnic disparities in the clinical practice of emergency medicine. Acad Emerg Med. 2003;10(11):1184–1188. doi: 10.1197/S1069-6563(03)00487-1. [DOI] [PubMed] [Google Scholar]
- 24.Morse M, Loscalzo J. Creating real change at academic medical centers - how social movements can be timely catalysts. N Engl J Med. 2020. [DOI] [PubMed]
- 25.Hardeman RR, Medina EM, Boyd RW. Stolen breaths. N Engl J Med. 2020. [DOI] [PubMed]
- 26.McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K. The work lives of women physicians results from the physician work life study. The SGIM Career Satisfaction Study Group. J Gen Intern Med. 2000;15(6):372–380. doi: 10.1111/j.1525-1497.2000.im9908009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR Event log data and time-motion observations. Ann Fam Med. 2017;15(5):419–426. doi: 10.1370/afm.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Puffer JC, Knight HC, O’Neill TR, et al. Prevalence of burnout in board certified family physicians. J Am Board Fam Med. 2017;30(2):125–126. doi: 10.3122/jabfm.2017.02.160295. [DOI] [PubMed] [Google Scholar]
- 29.What would you like to get a cost estimate for? Rally Health, Inc. https://costestimator.mayoclinic.org/. Published 2020. Accessed 17 April 2020.
- 30.Krupat E, Stein T, Selby JV, Yeager CM, Schmittdiel J. Choice of a primary care physician and its relationship to adherence among patients with diabetes. Am J Manag Care. 2002;8(9):777–784. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 16 kb)
(DOCX 40 kb)