INTRODUCTION
Podcasts are downloadable, digitally recorded audio files. Residents report using podcasts as educational tools because they are convenient, entertaining, and easily personalized, and foster a sense of intellectual community.1 These characteristics make podcasts an intriguing solution to a ubiquitous problem in resident education: poor attendance at residency conferences. We created a podcast specific to our internal medicine (IM) residency program to disseminate learning points from our teaching conferences. We then evaluated its impact on residents’ self-reported practice and learning habits.
METHODS
All residents in the Vanderbilt University IM training program between June 2016 and June 2018 were included in this study. The Institutional Review Board deemed this study exempt. At our institution, IM residents are expected to attend noon conferences 4 days per week and a morning report three times per week during inpatient rotations.
Podcast content included high-yield learning points from noon conferences and morning reports. Beginning July 2016 (year 1), episodes were distributed approximately twice monthly. The podcast was recorded by two chief residents. In year 2, the format changed to a single chief resident and an IM resident as hosts. Both years, Audacity® open source software, version 2.1.2 was used for editing. Podcast production required 2 to 3h per episode.
We evaluated the impact of the podcast with a pre-implementation survey followed by annual post-implementation surveys, hereafter referred to as end-of-year 1 and 2 surveys. Study data were collected using REDCap electronic data capture tools.2 The pre-intervention survey occurred in June 2016 and the end-of-year 1 and 2 surveys in July 2017 and April 2018.
RESULTS AND DISCUSSION
As seen in Table 1, survey response rates were 58% (87 of 151), 44% (73 of 165), and 43% (71 or 165) in the pre-implementation, end-of-year 1, and end-of-year 2 surveys. Of the survey respondents, the number of residents who reported listening to at least one podcast episode was 38/73 (52%) at the end-of-year 1 and 56/71 (79%) at the end-of-year 2. Of those who listened to at least one episode, 12/38 (32%) and 20/56 (36%) reported listening to at least half of the episodes in the end-of-year 1 and 2 surveys.
Table 1.
Demographics and Response Rates per Year: There Was a Similar Distribution of Training Level of Respondents to the Survey (p Value 0.60) and Percentage of Podcasts Listened to (p Value 0.33)
| Year 0 | Year 1 | Year 2 | |
|---|---|---|---|
| Total residents | 151 | 165 | 165 |
| Total respondents | 87 | 73 | 71 |
| Training level | |||
| PGY-1 | 33 | 26 | 26 |
| PGY-2 | 28 | 28 | 34 |
| PGY-3 | 24 | 16 | 10 |
| PGY-4 | 2 | 3 | 1 |
| % podcasts listened | |||
| 0% | n/a | 9 | 15 |
| 1–25% | n/a | 11 | 26 |
| 26–50% | n/a | 15 | 10 |
| 51–75% | n/a | 2 | 11 |
| 76–99% | n/a | 4 | 3 |
| 100% | n/a | 6 | 6 |
| No-response | 26* | 0 | |
PGY, post graduate year
*All “No-response” were from PGY-1 who did not have access to the prior year’s podcasts
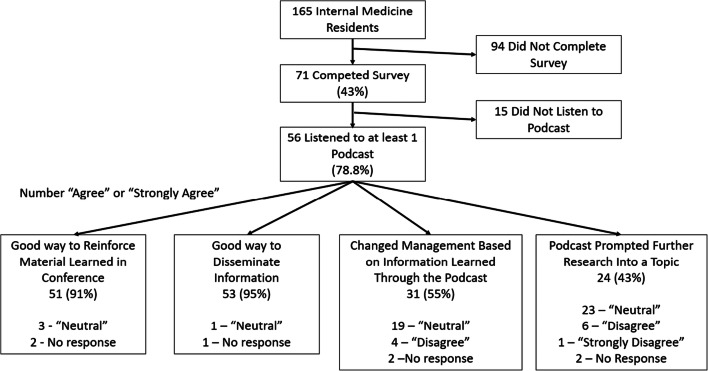
Podcast impact was evaluated by the 56 residents on the end-of-year 2 survey who reported listening to least one podcast episode. As demonstrated in Figure 1, 51 of 56 residents (91%) reported the podcast was useful for disseminating information from conferences and 53 of 56 (95%) reported it was useful for reinforcing conference information. Furthermore, 31 of 56 (55%) listeners reported changing their practice habits from information gained from the podcast and 24 of 56 (43%) reported further researching the topics presented in the podcast.
Figure 1.
Flowchart of results from the end-of-year 2 survey—43% of residents completed the survey at the end-of-year 2 where 78.8% of those residents listened to at least one podcast. For the respondents who listened the podcast was overwhelmingly well received and caused self-reported practice and learning changes.
There are few reports of residency program-specific podcasts in the literature. One IM program created a weekly podcast reviewing teaching points from morning report and found a podcast utilization rate of 70% with 23% listening to half the episodes.3 The higher rates measured in our study might reflect our podcast’s involvement of residents in the creation of the podcast or the general increase in popularity of the podcasting medium.
Regarding study limitations, no validated survey tools were available so we created our own instruments. Our results could be influenced by response bias, in that trainees who listened to the podcast may have been more likely to respond to our surveys. However, a manual count of podcast downloads from the private storage website roughly matched the utilization rates reported in the surveys, suggesting minimal response bias.
Other programs could easily adapt our intervention to meet local educational needs. Recording equipment can be as simple as a laptop with a microphone. Educational material can be curated from existing educational conferences or new material can be developed. If unable to edit audio, there are free web-based services that assist with audio leveling and noise reduction. Podcasts can then be hosted by a distribution service or distributed by email.
In summary, residents reported that our podcast was a useful tool for disseminating and reinforcing information from conferences, and many residents reported changing their clinical practice and pursuing independent inquiry on the topics covered. Our podcast is available on many podcast services including Spotify, Pocket Casts, and Apple Podcasts by searching “Vanderbilt Internal Medicine Residency Podcast.”
Compliance with Ethical Standards
The Institutional Review Board deemed this study exempt.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Riddell J, Robins L, Brown A, Sherbino J, Lin M, Ilgen J. 2019. Independent and Interwoven: A Qualitative Exploration of Resident’ Experiences with Educational Podcasts. [published online ahead of print January 9, 2010]. Acad Med. doi: 10.1097/ACM.0000000000002984. [DOI] [PubMed]
- 2.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Childers RE, Dattalo M, Christmas C. Podcast pearls in residency training. Ann Intern Med. 2014;160(1):70. doi: 10.7326/L14-5000-2. [DOI] [PubMed] [Google Scholar]