INTRODUCTION
Burnout is a syndrome driven by the work environment that has a negative impact on physician well-being, patient care, and the health care system.1–3 The Maslach Burnout Inventory (MBI) is the most widely used measure of burnout and consists of a 22-item survey of emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA).2 Health care organizations have called upon leaders to address burnout and take positive steps on a systems-level to promote physician well-being.2, 3 In addition to contributions from the clinical learning environment on residents and faculty well-being, the environment itself is also affected by resident and faculty burnout, suggesting residents need skills for coping and resilience as they enter their careers, and faculty physicians can build and teach these same skills.1, 4, 5
Well-being is defined by the Center for Disease Control as the state of being comfortable, happy, or healthy.1, 6 The key components of well-being are positive emotions and psychological resources (e.g., positive affect, autonomy, mastery); and it is thought to encompass physical, mental, and social domains.1, 6 Professional well-being is defined by the experience of positive perceptions and the presence of conditions at work and beyond that enables workers to thrive and achieve their full potential.1, 6 Markers of professional well-being are thought to be finding meaning, feeling engaged at work, having a high-quality working life, and finding professional fulfillment in one’s work.1, 6 These constructs are not fully represented in the MBI.6
The PERMA model may offer a new approach to measuring well-being, although not yet widely studied in physicians (Table 1). The PERMA model has five domains: positive emotion (P), engagement (E), positive relationships (R), meaning (M), and accomplishment (A).7 Each domain was selected based on three criteria: (1) contribution to well-being, (2) pursuit by many people for its own sake, not merely to achieve another element, and (3) exclusivity, in that each element is defined and measured independently of the others.7, 8 The combination of these elements contributes to one’s ability to flourish, or be well.7, 8
Table 1.
PERMA Components and Application to Medicine. Details of the Five Independent Core Components that Contribute to One’s Well-being: Positive Emotions, Engagement, Relationships, Meaning, and Accomplishment.7 The PERMA-Profiler, Developed by Butler and Kern in 2016, Integrates these 5 Components into a 23-Item Questionnaire that Has Been Validated to Assess an Individual’s State of Wellness in its 15-Item and 23-Item Format6
| Positive Emotions | Engagement | Relationships | Meaning | Accomplishment | |
|---|---|---|---|---|---|
| Method of measurement | Subjective | Subjective | Objective | Subjective and objective | Objective |
| Definition | Happiness and satisfaction | Absorption in the moment | Interpersonal interactions | Serving a greater purpose | Achievement and mastery |
| Application to medical field* | Reduce workplace stressors | Reduce non-valued work | Include mentorship and small group learning | Encourage reflection and support humanities | Promote innovation and recognize humanism |
| Items on 15-item PERMA scale |
I feel joyful. I feel positive. I feel content. |
I become absorbed in what I am doing. I feel particularly excited or interested in things. I lose track of time while doing something I enjoy. |
I receive help and support from others when I need it. I feel loved. I am satisfied with my personal relationships. |
My life is purposeful and meaningful. My life is valuable and worthwhile. I feel I have a sense of direction in my life. |
I feel I am making progress toward accomplishing my goals. I am achieving the important goals I have set for myself. I am able to handle my responsibilities. |
Butler and Kern created the PERMA-Profiler in 2016, a 23-item validated instrument to assess and monitor well-being across all five PERMA domains. To convergently and divergently validate this instrument as a reliable and valid measure of well-being, three studies were performed in which each domain of PERMA was positively linked to physical health, flourishing, and life satisfaction and negatively linked to depression, fatigue, anxiety, perceived stress, loneliness, and negative emotion.9 The original 23 items were reduced to three items per domain, for a total of 15 items. The PERMA-profiler has been used in its reduced 15-item format in the USA, Japan, and China in both student and professional populations, but not with other physician or physician trainee studies, nor in comparison with the MBI .7, 8
We sought to (1) measure well-being using the 15-item PERMA scale in resident and faculty physicians and to compare results between the two and (2) to compare the PERMA scale with the standardized MBI model using an individual internal control. We hypothesized that resident well-being would be lower compared with faculty scores and that the PERMA and MBI models would correlate inversely given the focus on measuring positive versus negative aspects of well-being.
SETTING AND PARTICIPANTS
The source of data for this analysis is self-reported surveys conducted in the baseline year of a multisite, multiyear investigation. We administered the 15-item PERMA scale and the MBI to 272 interns and 244 faculty at four internal medicine residency programs in the Northeast and Southeast of the USA as part of the baseline data collection for a positive psychology coaching intervention in the 2016–2017 academic year.4, 5 Surveys were sent using REDCap to all participants and reminders were sent every 2 weeks for 4 weeks. Participants received a $10 gift card to an online retailer for completing the survey.
PROGRAM DESCRIPTION
The 15-item PERMA scale was scored such that the highest score possible for each of the 5 components was 15, with a maximum total score of 75. Individual items are assessed on a 0–5 scale with 0 correlating with “never” and 5 with “always”.7, 9 We assessed the mean PERMA score, and the individual domain scores (P, E, R, M, and A) across residents and faculty at pre-survey completion. The MBI was scored using a 7-level scale ranging from “never” (0) to “every day”6 for the 3 components: emotional exhaustion (9 items), depersonalization (5 items), and personal accomplishment (8 items).10 The EE and DP subscales were analyzed separately as continuous variables. We compared intern and faculty MBI scores for the 3 subscales. We performed a t test to compare the difference between faculty and interns. We also assessed whether a correlation exists between interns’ and faculty members’ individual PERMA and MBI scores using Pearson’s correlation.
PROGRAM EVALUATION
One hundred twenty-three interns and 154 faculty members completed the pre-survey and were included in this study. No participants who completed the survey in its entirety were excluded from the study.
There were slight differences between the sites in MBI and PERMA scores, but differences across sites were not significant; there were no differences in demographics between respondents and non-respondents. Faculty physicians’ overall mean PERMA score was 60.4 with meaning (M) being the highest domain at 13.2 and positive emotion (P) being the lowest domain at 11.3. The mean PERMA score of residents was 59.1 which was not statistically different from the mean faculty score (p = 0.13). By domain scores, interns also scored the highest in meaning with a score of 12.7 and lowest in positive emotion with a score of 11.1.
Faculty had statistically significantly higher scores than residents in the meaning component (p=0.042). All other component scores and the overall PERMA scores showed no significant differences between the groups. Items in the meaning component included making progress toward accomplishing goals, achieving important goals set, and ability to handle responsibilities.
EE and DP components of the MBI showed statistically significant differences between the interns and faculty, with residents scoring higher on EE and DP than faculty (EE—23.3 vs 20.4, p=0.029; DP—9.5 vs 6.4, p<0.001).
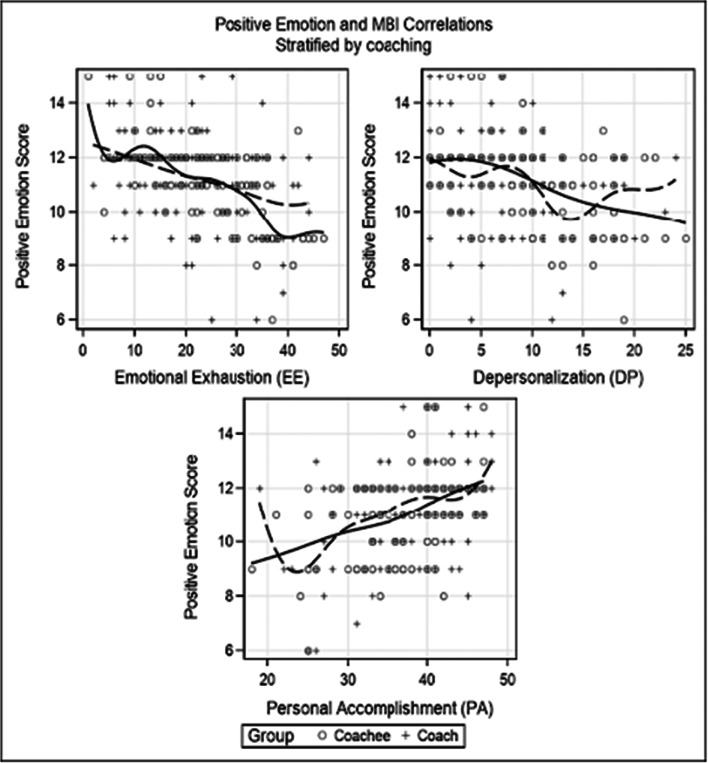
Figure 1 displays the correlation analysis. There was not a statistically significant strong correlation between the total scores of the two assessment tools (r = - 0.48). The largest degree of correlation was among residents with a negative association between PERMA’s positive emotion score and EE (r = - 0.63). A moderately strong correlation was also seen between the total PERMA score and the personal accomplishment component of MBI among residents (r = 0.51).
Figure 1.
Correlation of PERMA positive emotion (P) and MBI (EE, DP, PA) scores. PERMA Positive emotion score (range 0–15) plotted against MBI (EE, DP, PA components). The largest degree of correlation was among residents with a negative association between PERMA’s positive emotion score and EE (r = - 0.63)). The smoothing splines depict the correlations for coachees and coaches, respectively.
DISCUSSION
To our knowledge, this is the first study using a PERMA scale in physicians to assess well-being, and to compare it with the MBI as an outcome of an intervention. These baseline data indicate that there were no significant differences between intern and faculty overall PERMA scores, and only one of five domains (M) showed a difference. Meaning was the highest in both groups and suggests that this particular domain may be central to the overall assessment of physician well-being, fitting with prior models and definition of professional well-being.1, 2, 6
Comparisons of resident and faculty well-being have previously been reported. Residents, when compared with faculty, were found to have lower overall well-being as measured by less fulfillment in their work, lower personal accomplishment, and lower career satisfaction.11, 12 One study assessing well-being using the MBI and personal and career satisfaction questions of over 7000 physicians found that early career physicians had the lowest satisfaction with overall career choice and also had the highest rates of emotional exhaustion and burnout.11 In our study, residents and faculty were assessed to have similar levels of well-being using the PERMA construct. When that same group of individuals was assessed by the MBI, however, levels of burnout within the two populations were consistent with prior findings in the literature: residents scored higher in levels of burnout compared with faculty. This suggests that well-being is not the absence of burnout, but instead a more complex relationship rather than a continuum.
To define this relationship more concretely, we sought to find a correlation between the MBI and PERMA models in assessing physician well-being. Overall, no correlation between the two models was found; however, in the subgroup analyses of residents only, a statistically significant inverse relationship was found between the positive emotion (P) of PERMA and the emotional exhaustion (EE) of MBI. Because each individual served as his or her own internal control at the same point in time, the lack of correlation is especially noteworthy. Given the absence of a correlation when measured across all physicians, as well as the lack of correlation between the MBI and PERMA scores in totality, we conclude that PERMA and MBI measure different aspects of a physician’s well-being. We hypothesize that the inverse correlation of positive emotion with emotional exhaustion may represent an early sign of measurable burnout, though this will need to be explored in future studies. These assessments could be used synergistically to assess a physician’s overall well-being and allow identification of both modifiable and non-modifiable factors affecting one’s well-being in a multifactorial complex. As was noted by Steptoe in an article on happiness in the geriatric population, “happiness is not the same as the absence of depression and distress.”.13
The implications of using the PERMA scale in physicians are yet to be determined. Interestingly, when the PERMA scale was distributed among elite musicians, this group was also found to have meaning scores that rank the highest compared with the remaining PERMA domains.8 Because both studies were in actively practicing, highly-skilled professionals, this may suggest that commitment to extensive training in a particular field, regardless of the specific area of focus, suggests greater meaning in one’s work. Meaning may be a defining factor in a professional choosing to continue to pursue career goals. Other PERMA domains, such as positive emotion or accomplishment, may require a greater degree of introspection and reflection and therefore may be more limited in currently practicing individuals. Engagement may be anticipated to be greater in those early in their career, given the focus on career building and finding one’s niche in early career stages, but this finding was not identified in this study. Relationship likely manifests differently throughout one’s career—early career residents may be eager to connect and find their niche, while faculty have presumably build relationships over time. Further delineation of participants in the study by years in training may provide greater insights into differences between PERMA domains.
We note limitations within our study. The study population was limited to only 4 internal medicine residency programs that were assessed as part of a baseline measurement for a coaching program. The relatively small study size is also a limitation when applying findings across a much larger population; however, it is one of the largest studies to date using PERMA as a construct for well-being. Furthermore, the inherent self-selection as a result of a voluntary program and survey may impact our results given those experiencing the greatest burnout may be less likely to have the motivation to complete the survey. Additionally, our smaller sample size precludes our ability to expound upon the work in this study with the comparison of late versus early career faculty physicians. A potential challenge to these findings might be the perceived impact that a 0.5-point difference in the meaning scale has in a physician’s experience of meaning in their life. Responses from both faculty and interns were clustered in the highest quartile of the meaning subscale, which may explain why a 0.5-point difference was significant when comparing faculty and interns. From a review of the existing literature, subtle changes in PERMA denote a meaningful difference in well-being between scores.7–9 The ability to detect subtle changes in well-being suggests how this measure may be promising in future studies.
Further studies may focus on the comparison of physicians with other professional fields to evaluate well-being compared to other intensive fields of training. Additionally, a comparison of changes in PERMA and MBI scores over the course of an academic year or following a specific well-being intervention would be interesting to assess for incremental relationships between degrees of change across both assessment tools.
There is a clear need for ongoing interventions to improve resident well-being and reliably measure the impact of these interventions.1, 2 The PERMA scale lack of correlation with the MBI model suggests that both may be useful in synergistic ways to measure the complex construct of physician well-being.
Acknowledgements
The authors wish to thank the faculty coaches and resident participants who engaged in the program, as well as the Departments of Medicine at each institution for their support in developing and onboarding this program. The authors wish to express gratitude to the Arthur Vining Davis Foundation and the Physicians Foundation, for the financial support for our program evaluation. The authors wish to acknowledge the Institute of Coaching and Carol Kauffman, PhD, for their expertise in designing and implementing this program. The authors wish to acknowledge Dr. Peggy Kern for her assistance in analyzing the PERMA results.
Funding
The Arthur Vining Davis Foundation and The Physicians Foundation each provided $100,000 of funding to support the investigation and dissemination of this program.
Declarations
Ethical Approval
This program and its evaluation were exempt by the Institutional Review Board with exemption #45 CFR 46.101(b)1 Research conducted in established or commonly accepted educational settings, involving normal educational practices.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Prior Presentations
While the tools and implementation process used in the coaching program have been shared in numerous workshops at national conferences (Society of General Internal Medicine, Association of Program Directors in Internal Medicine, American College of Physicians) and invited grand rounds and faculty development workshops, the data included in this paper has not been previously presented.
This manuscript has not been previously published and is not under consideration in the same or substantially similar form in any other journal.
All those listed as authors are qualified for authorship and all qualified to be authors are listed as authors on the byline.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Academies of Sciences, Engineering, and Medicine . Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington, DC: The National Academies Press; 2019. [PubMed] [Google Scholar]
- 2.National Academy of Medicine. Valid and Reliable Survey Instruments to Measure Burnout, Well-Being, and Other Work-Related Dimensions. Updated 2020. Accessed 22 June 2020. https://nam.edu/valid-reliable-survey-instruments-measure-burnout-well-work-related-dimensions/.
- 3.Sinsky CA, Daugherty Biddison L, Mallick A, Legreid Dopp A, Perlo J, Lynn L, Smith CD. Organizational Evidence-Based and Promising Practices for Improving Clinician Well-Being. NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palamara K, Kauffman C, Chang Y, et al. Professional Development Coaching for Residents: Results of a 3-Year Positive Psychology Coaching Intervention. J Gen Intern Med. 2018;33(11):1842–1844. doi: 10.1007/s11606-018-4589-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palamara K, Kauffman C, Stone VE, Bazari H, Donelan K. Promoting Success: A Professional Development Coaching Program for Interns in Medicine. J Grad Med Educ. 2015;7(4):630–637. doi: 10.4300/JGME-D-14-00791.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Well-Being Concepts. Updated Oct 2018. Accessed Jan 2020. www.cdc.gov.
- 7.Butler J, Kern ML. The PERMA-Profiler: A brief multidimensional measure of flourishing. Int J Wellbeing. 2016;6(3):1–48. doi: 10.5502/ijw.v6i3.526. [DOI] [Google Scholar]
- 8.Ascenso S, Perkins R, Williamon A. Resounding Meaning: A PERMA Wellbeing Profile of Classical Musicians. Front Psychol. 2018;9:1895. doi: 10.3389/fpsyg.2018.01895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Umucu E, Wu J, Sanchez J, Brooks JM, Chiu C, Tu W, Chan F. Psychometric validation of the PERMA-profiler as a well-being measure for student veterans. J Am Coll Heal. 2020;68(3):271–277. doi: 10.1080/07448481.2018.1546182. [DOI] [PubMed] [Google Scholar]
- 10.Maslach C, Schaufeli W, Leiter M. Job burnout. Annu Rev Psychol. 2001;52(1):397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 11.Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367. doi: 10.1016/j.mayocp.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Sargent MC, Sotile W, Sotile MO, Rubash H, Barrack RL. Stress and coping among orthopaedic surgery residents and faculty. J Bone Joint Surg. 2004;86A:1579–1586. doi: 10.2106/00004623-200407000-00032. [DOI] [PubMed] [Google Scholar]
- 13.Steptoe A. Investing in Happiness: The Gerontological Perspective. Gerontology. 2019;65(6):634–639. doi: 10.1159/000501124. [DOI] [PMC free article] [PubMed] [Google Scholar]