Abstract
Abstract
Background
While health-related social needs (HRSN) are known to compromise health, work to date has not clearly demonstrated the relationship between clinically acknowledged social needs, via ICD-10 Z-codes, and readmission.
Objective
Assess the rate of 30-, 60-, and 90-day readmission by the level of ICD-10-identified social need. In addition, we examined the associations between demographics, social need, hospital characteristics, and comorbidities on 30-day readmission.
Design
Retrospective study using the 2017 Nationwide Readmission Database
Participants
We identified 5 domains of HRSN from ICD-10 diagnosis codes including employment, family, housing, psychosocial, and socioeconomic status (SES) and identified how many and which an individual was coded with during the year.
Main Measures
The proportion of patients with 30-, 60-, and 90-day readmission stratified by the number of HRSN domains with a multivariable logistic regression to examine the relationship between the number/type of and readmission adjusting for sex, age, payer, hospital characteristics, functional limitations, and comorbidities.
Key Results
From 13,217,506 patients, only 2.4% had at least one HRSN diagnosis. Among patients without HRSN, 11.5% had a 30-day readmission, compared to 27.0% of those with 1 domain, increasing to 63.5% for patients with codes in 5 domains. Similar trends were observed for 60- and 90-day readmission; 78.7% of patients with documented HRSN in all 5 domains were hospitalized again within 90 days. The adjusted odds ratio for readmission for individuals with all 5 domains was 12.55 (95% CI: 9.04, 17.43). Housing and employment emerged as two of the most commonly documented HRSN, as well as having the largest adjusted odds ratio.
Conclusions
There is a dose-response relationship between the number of HRSN diagnoses and hospital readmission. This work calls attention to the need to develop interventions to reduce readmissions for those at social risk and demonstrates the significance of ICD-10 Z-codes in health outcomes studies.
Key Words: social determinants of health, health-related social needs, health equity, health disparities, readmission, utilization
INTRODUCTION
The relationship between health-related social needs (HRSN) and health outcomes is widely recognized, and in recent years, we have seen this relationship become more explicit and quantified.1–11 As a result of this deepening understanding of how HRSN such as food insecurity, social isolation, and housing instability impact health, most hospitals report screening patients for social factors and interventions are being developed.12–17 In addition to limited training for providers on HRSN, including screening and documentation, interventions are presently not reimbursable. Thus, positive screens are rarely coded using specific, existing ICD-10 diagnostic codes developed to capture patient social factor data. Indeed, a recent study by CMS found that among 33.7 million Medicare fee-for-service beneficiaries, these codes, which begin with the letter Z (hence, referred to as Z-codes), were present in just 1.4% of claims filed in 2017.18–22
Recently, there has been a growing focus on expanding the use and utility of Z-codes.23–25 This focus is largely driven by research demonstrating that data on patients’ HRSN can improve population health management efforts and may eventually be used to adjust publicly reported quality measures to better isolate true differences and avoid unfairly penalizing safety net providers caring for clinically and socially complex patients.
If one thing threatens to stymie these quality adjustment efforts, however, it is the lack of available, valid, standardized, and systematically collected data on individual-level HRSN, a gap that Z-codes seem well poised to fill.23,25,26 Most recently, leading healthcare organizations including the American Medical Association (AMA) and United Healthcare have partnered to advocate for the expansion of Z-codes to capture HRSN while concurrently encouraging research to better refine and develop interventions.27,28
Unplanned hospital readmission (hereafter referred to as “readmission”) is a quality metric for which HRSN data might be particularly salient. Both HRSN (e.g., whether a patient has social support, whether the patient has access to stable housing) and the social determinants in the community to which that patient is discharged (e.g., air quality, reliable public transportation) could result in readmission regardless of the quality of care received during the initial inpatient stay. Indeed, a number of studies have demonstrated the relationship between social determinants of health (SDOH) and health-related social needs and hospital readmission.29–33 Specifically, this body of work has frequently examined area-level measures of social determinants of health (e.g., area deprivation index, census tract, ZIP code, and county-level factors), and the specific subset of studies that do examine the effect of social needs at the individual level often rely on data extracted from notes rather than from formal diagnostic codes.29,31–41 To more precisely estimate the effect of SDOH or HRSN, the statistical models used in this body of work often control for a common set of covariates including sex, race, age, marital status, comorbidities, social determinants of health or social risk, and hospital or site characteristics.29,30,34–37,42,43 The effect of SDOH or HRSN has varied, but studies have identified that 34% of patients with two HRSN and 24.5% of patients with housing instability have hospital readmission, and for those who live in areas of high deprivation, the odds ratio of readmission was 1.7.29,32,36 Together, these studies have demonstrated the importance of SDOH and HRSN and their association with readmission.
In this manuscript, we quantify the relationship between HRSN and readmission within a large national sample using ICD-10 Z-codes as the means for identifying HRSN, while adjusting for the aforementioned common covariates, as well as functional limitations which have been documented as a key driver of readmission.44
METHODS
From the nationally representative 2017 Nationwide Readmission Database, part of the Healthcare Cost and Utilization Project (HCUP) family of databases, we identified 5 domains of health-related social needs (HRSN) from ICD-10 Z-codes: employment, family, housing, psychosocial (e.g., problems related to primary support group), and socioeconomic status (SES). The diagnostic Z-codes for each domain were identified and grouped following a framework established by Reidhead (2018) and can also be found in Supplemental Table 1.19 We then calculated the total number of the domains that an individual had been coded with within the year, while also identifying whether or not an individual ever had another hospitalization within 30, 60, and 90 days. For example, if an individual were to have 3 hospitalizations in the year and have one domain of HRSN coded on just one discharge record, they would be considered to have “1 domain.” Extending this, if an individual had 3 hospitalizations, and 2 of the discharge records each had an HRSN diagnosis, but they were different domains, this person would be considered to have “2 domains.” If two of these hospitalizations were within 30 days, this person would be said to have had a 30-day readmission. For the readmission analysis, individuals whose only hospitalization for the year had a known disposition as death were excluded. Additionally, the 30-day readmission excluded anyone whose first discharge was in December, as they did not have full 30 days of follow-up. For 60 days, we excluded those in November and December and for 90 days excluded those in October, November, and December.
We conducted multivariable logistic regression to examine the relationship between the number of HRSN domains and ever having a 30-day readmission after adjusting for select covariates. Following previous work, we identified covariates that are potential confounders of the relationship between social needs and readmission, including sex (reference: female), payer (reference: privately insured), hospital control (reference: private, investor-owned), hospital teaching status (reference: metropolitan, teaching), and the validated Elixhauser comorbidities. Race and ethnicity were not available in these data. The Elixhauser comorbidities are commonly used in analyses of administrative data and are associated with death in hospital, increased length of stay, and increased charges.45 We used all available hospitalizations and all available diagnosis code slots (40 on each discharge) to identify comorbidities. Each comorbidity was coded as present or absent and entered into the model as its own covariate. In an effort to account for functional limitations, another important predictor of readmission, we utilized another subset of ICD-10 codes beginning with the prefix Z that refer to aspects of limitations in activities and care provider dependency including “Z736X” and “Z74XX,” where X represents all sub-codes. For the primary payer covariate, “no charge” and “other” were combined to a single variable, “other.” Age was taken as age in years, as a continuous variable, at first hospitalization in the dataset. Finally, hospital control and teaching status, as two separate variables, were taken from the first hospitalization. The number of HRSN was included as a single, multi-categorical variable where 0 HRSN was the reference level.
To examine the impact of specific HRSN on readmission, we repeated the above-described multivariable logistic regression, including each of the domains (employment, family, housing, psychosocial, and SES) as their own variables, each coded as yes or no. This model was further stratified into those with only 1 recorded HRSN (model 2a) and those with 2 or more HRSN (model 2b). In both models, 2a and 2b, the reference population consisted of individuals without a documented HRSN.
The analysis was conducted in SAS Version 9 and visualized using R version 3.6.0. This work was deemed as exempt by the Institutional Review Board (IRB # EM-14-30).
RESULTS
In 2017, there were 17,978,754 total hospitalizations of 13,217,506 unique patients in the Nationwide Readmission Database (NRD). From these, 2.4% (314,151) of patients had at least one HRSN recorded including, at the patient level: housing 1.2% (152,567); socioeconomic status (SES) 0.5% (70,242); family situations 0.5% (69,639); employment 0.4% (54,440); and psychosocial factors 0.2% (27,969) (Table 1). Among those with HRSN, 48.6% had housing-related needs; 22.4% SES; 22.2% family; 17.3% employment; 8.9% psychosocial. Two of the most common HRSN, and nearly all of individuals within the housing and employment domains respectively, were documented to experience homelessness (149,983, 98.3%) and unemployment (48,868, 89.8%). The complete list and description of codes included in the domains, as well as the number of patients with the specific codes can be found in Supplemental Table 1. For individuals with documented HRSN compared to those without HRSN, there was a higher proportion of males (56.7 vs. 40.6%), a higher proportion insured via Medicaid (44.1% vs 20.9%), and a higher proportion were seen at government, nonfederal hospitals (18.1% vs 11.7%).
Table 1.
Characteristics of Individuals With and Without Health-Related Social Needs (HRSN)
| Percent of all patients, N = 13,217,506 | Percent of patients with HRSN, N = 314,151 | |
|---|---|---|
| HRSN Z-code domain* | ||
| Employment, n = 54,440 | 0.4 | 17.3 |
| Family, n = 69,639 | 0.5 | 22.2 |
| Housing, n = 152,567 | 1.2 | 48.6 |
| Psychosocial, n = 27,969 | 0.2 | 8.9 |
| SES, n = 70,242 | 0.5 | 22.4 |
| Number of HRSN domains, ever | ||
| 0 Domains, n = 12,903,355 | 97.6 | ---- |
| 1 Domain, n = 265,997 | 2.0 | 84.7 |
| 2 Domains, n = 37,644 | 0.3 | 12.0 |
| 3 Domains, n = 8,624 | 0.1 | 2.7 |
| 4 Domains, n = 1670 | 0.01 | 0.5 |
| 5 Domains, n = 196 | 0.001 | 0.1 |
| Patients with no HRSN, N = 12,903,355; n (%) | Patients with any HRSN, N = 314,151; n (%) | |
| Male | 5,241,776 (40.6) | 178,078 (56.7) |
| Age: median [IQR] | 57 (32–72) | 45 (30–57) |
| Payer | ||
| Private Insurance | 4,025,713 (31.2) | 49,270 (15.7) |
| Medicaid | 2,691,808 (20.9) | 138,665 (44.1) |
| Medicare | 5,299,326 (41.1) | 79,170 (25.2) |
| Other | 451,999 (3.5) | 18,996 (6) |
| Self-pay | 434,509 (3.4) | 28,050 (8.9) |
| Site of first hospitalization | ||
| Government, nonfederal | 1,510,993 (11.7) | 56,833 (18.1) |
| Private, not-profit | 9,628,471 (74.6) | 212,336 (67.6) |
| Private, investor-owned | 1,763,891 (13.7) | 44,982 (14.3) |
| Metropolitan, teaching | 8,783,784 (68.1) | 227,410 (72.4) |
| Metropolitan, non-teaching | 3,084,018 (23.9) | 66,419 (21.1) |
| Nonmetropolitan | 1,035,553 (8.0) | 20,322 (6.5) |
| Functional limitations | ||
| Functional limitations | 101,476 (0.8) | 2357 (0.8) |
| Comorbidities | ||
| Congestive heart failure | 1,187,134 (9.2) | 23,432 (7.5) |
| Valvular disease | 541,826 (4.2) | 9653 (3.1) |
| Pulmonary circulation disorders | 104,372 (0.8) | 3009 (1.0) |
| Peripheral vascular disorders | 749,141 (5.8) | 13,263 (4.2) |
| Paralysis | 418,590 (3.2) | 9070 (2.9) |
| Other neurological disorders | 108,3811 (8.4) | 42,775 (13.6) |
| Chronic pulmonary disease | 2,310,672 (17.9) | 75,930 (24.2) |
| Diabetes | 1,400,558 (10.9) | 31,111 (9.9) |
| Diabetes with complications | 1,623,837 (12.6) | 33,205 (10.6) |
| Hypothyroidism | 1,487,931 (11.5) | 24,598 (7.8) |
| Renal failure | 1,566,759 (12.1) | 23,945 (7.6) |
| Liver disease | 523,129 (4.1) | 30,549 (9.7) |
| Peptic ulcer disease | 120,141 (0.9) | 3872 (1.2) |
| HIV/AIDS | 23,392 (0.2) | 3042 (1.0) |
| Lymphoma | 87,651 (0.7) | 1072 (0.3) |
| Metastatic cancer | 289,136 (2.2) | 3235 (1.0) |
| Solid tumor w/o metastasis | 295,355 (2.3) | 4533 (1.4) |
| Rheumatoid arthritis | 358,236 (2.8) | 6083 (1.9) |
| Coagulation deficiency | 821,177 (6.4) | 23,053 (7.3) |
| Obesity | 2,075,910 (16.1) | 45,821 (14.6) |
| Weight loss | 790,775 (6.1) | 27,912 (8.9) |
| Fluid and electrolyte disorders | 3,436,551 (26.6) | 100,637 (32) |
| Blood loss anemia | 449,948 (3.5) | 5,982 (1.9) |
| Deficiency anemias | 2,195,739 (17) | 61,662 (19.6) |
| Alcohol abuse | 531,463 (4.1) | 72,788 (23.2) |
| Drug abuse | 521,323 (4.0) | 101,578 (32.3) |
| Psychoses | 429,068 (3.3) | 50,731 (16.1) |
| Depression | 1,581,814 (12.3) | 81,207 (25.8) |
*The “percent of patients with HRSN” will total to more than 100%, given patients with multiple domains of HRSN; p values are not displayed, due to the overwhelming sample size. In this analysis, all p values, using chi-squared tests for all comparisons except age, which was compared using a Kruskal-Wallis test, were significant (< 0.001, except functional limitations < 0.05), but that is largely due to sample size and provides little information on the meaningfulness of these differences
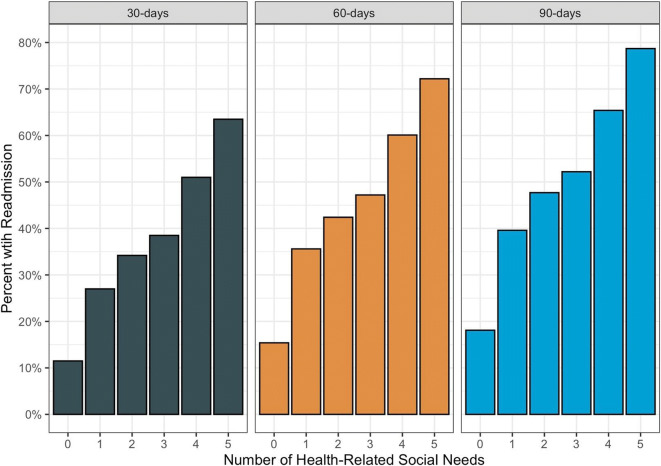
There was a dose-response relationship between the number of domains ever coded and the percent of those patients readmitted within 30, 60, or 90 days. While the overall 30-day readmission rate was just 11.9%, for those with 1 domain it rose substantially to 27.0%, then steadily increased to 34.2%, 38.5%, 51.0%, and 63.5% for patients with 2 through 5 domains, respectively (Table 2, Fig. 1). This trend was observed with both 60- and 90-day rates with 78.7% of those patients with 5 domains being readmitted within 90 days, compared to only 18.1% of patients without documented HRSN (Table 2, Fig. 1).
Table 2.
Percent of Patients with a Readmission by the Number of Health-Related Social Needs (HRSN)
| Patients readmitted within: | ||||||
|---|---|---|---|---|---|---|
| Number of HRSN domains, ever | 30 days | 60 days | 90 days | |||
| Eligible | % | Eligible | % | Eligible | % | |
| 0 | 11,734,148 | 11.5 | 10,817,395 | 15.4 | 9,858,005 | 18.1 |
| 1 | 249,843 | 27.0 | 234,336 | 35.6 | 217,016 | 39.6 |
| 2 | 35,879 | 34.2 | 33,973 | 42.4 | 31,760 | 47.7 |
| 3 | 8276 | 38.5 | 7881 | 47.2 | 7419 | 52.2 |
| 4 | 1626 | 51.0 | 1568 | 60.1 | 1510 | 65.4 |
| 5 | 192 | 63.5 | 187 | 72.2 | 178 | 78.7 |
| Overall | 12,029,964 | 11.9 | 11,095,340 | 16.0 | 10,115,888 | 18.7 |
The eligible columns represent the number of individuals eligible for a readmission for that time frame, while the % columns represent the percent with a readmission
Figure 1.
The relationship between the number of clinically acknowledged health-related social needs, via ICD-10 Z-codes, and percent of patients with a readmission
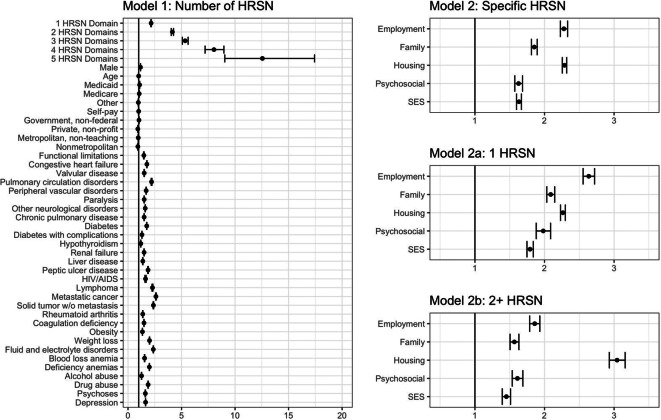
The first multivariable logistic regression (model 1) revealed that being male and on Medicaid and all Elixhauser comorbidities were positively associated with having at least one readmission within 30 days (Table 3, Fig. 2). Among the comorbidities, cancer, solid tumors, and lymphoma had the largest effect size. After adjusting for sex, payer, comorbidities, functional limitations, and hospital characteristics, the number of domains remained positively associated with readmission with adjusted odds ratios ranging from 2.16 (95% CI: 2.13, 2.18) for those individuals with 1 domain to 12.55 (95% CI: 9.04, 17.43) for those with all 5 domains (Table 3, Fig. 2). These results were consistent in a sensitivity analysis where we used a multilevel logistic regression model with random effects at the facility level.
Table 3.
Model 1 Unadjusted Odds Ratios, Adjusted Odds Ratios, and 95% Confidence Intervals for Ever Having a 30-day Readmission
| Model 1: number of HRSN | ||
|---|---|---|
| Term | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
| Health-related social need domain counts | ||
| 0 HRSN domains (reference) | ----- | ----- |
| 1 HRSN domain | 2.84 (2.81, 2.87) | 2.16 (2.13, 2.18) |
| 2 HRSN domains | 4.00 (3.91, 4.09) | 4.14 (4.04, 4.25) |
| 3 HRSN domains | 4.82 (4.61, 5.04) | 5.34 (5.08, 5.62) |
| 4 HRSN domains | 8.00 (7.26, 8.82) | 8.03 (7.20, 8.96) |
| 5 HRSN domains | 13.26 (9.89, 17.78) | 12.55 (9.04, 17.43) |
| Demographics | ||
| Male | ----- | 1.17 (1.16, 1.17) |
| Age | ----- | 1.00 (1.00, 1.00) |
| Private insurance (reference) | ----- | ----- |
| Medicaid | ----- | 1.09 (1.08, 1.09) |
| Medicare | ----- | 1.05 (1.04, 1.05) |
| Other | ----- | 0.96 (0.95, 0.98) |
| Self-pay | ----- | 1.00 (0.98, 1.01) |
| Hospital characteristics | ||
| Private, investor-owned (reference) | ----- | ----- |
| Government, nonfederal | ----- | 1.03 (1.02, 1.03) |
| Private, not-profit | ----- | 0.92 (0.91, 0.92) |
| Metropolitan, teaching (reference) | ----- | ----- |
| Metropolitan, non-teaching | ----- | 0.95 (0.95, 0.96) |
| Nonmetropolitan | ----- | 0.92 (0.91, 0.93) |
| Functional limitations | ||
| Functional limitations | ----- | 1.48 (1.46, 1.50) |
| Comorbidities | ||
| Congestive heart failure | ----- | 1.76 (1.75, 1.77) |
| Valvular disease | ----- | 1.51 (1.50, 1.53) |
| Pulmonary circulation disorders | ----- | 2.20 (2.16, 2.23) |
| Peripheral vascular disorders | ----- | 1.70 (1.68, 1.71) |
| Paralysis | ----- | 1.51 (1.50, 1.52) |
| Other neurological disorders | ----- | 1.61 (1.60, 1.62) |
| Chronic pulmonary disease | ----- | 1.51 (1.50, 1.51) |
| Diabetes | ----- | 1.75 (1.74, 1.76) |
| Diabetes with complications | ----- | 1.30 (1.30, 1.31) |
| Hypothyroidism | ----- | 1.20 (1.19, 1.20) |
| Renal failure | ----- | 1.50 (1.49, 1.51) |
| Liver disease | ----- | 1.38 (1.37, 1.40) |
| Peptic ulcer disease | ----- | 1.87 (1.84, 1.90) |
| HIV/AIDS | ----- | 1.64 (1.59, 1.69) |
| Lymphoma | ----- | 2.28 (2.25, 2.32) |
| Metastatic cancer | ----- | 2.61 (2.58, 2.63) |
| Solid tumor w/o metastasis | ----- | 2.37 (2.35, 2.40) |
| Rheumatoid arthritis | ----- | 1.38 (1.37, 1.39) |
| Coagulation deficiency | ----- | 1.49 (1.48, 1.50) |
| Obesity | ----- | 1.35 (1.34, 1.35) |
| Weight loss | ----- | 2.01 (2.00, 2.02) |
| Fluid and electrolyte disorders | ----- | 2.36 (2.35, 2.37) |
| Blood loss anemia | ----- | 1.55 (1.53, 1.57) |
| Deficiency anemias | ----- | 2.00 (1.99, 2.00) |
| Alcohol abuse | ----- | 1.26 (1.25, 1.27) |
| Drug abuse | ----- | 1.88 (1.86, 1.89) |
| Psychoses | ----- | 1.62 (1.61, 1.63) |
| Depression | ----- | 1.64 (1.63, 1.65) |
Model 1 evaluated the total number of health-related social needs (HRSN). Functional limitations and comorbidities were each included as their own variable, with the reference level being not having limitations or the respective comorbidity
Figure 2.
Odds ratios and 95% confidence intervals for logistic regression models, with an outcome of ever having a 30-day readmission adjusted for sex, age, payer, hospital characteristics, functional limitations, Elixhauser comorbidities, and the number of HRSN domains (model 1) and the specific HRSN domains (model 2). Model 2 was adjusted with the same covariates, which are not displayed due to nearly identical estimates and odds ratios (Supplemental Table 2). Model 2 was further stratified to those with only 1 HRSN (model 2a) and those with 2 or more HRSN (model 2b). Across models, reference levels include female, private insurance, private investor-owned, metropolitan teaching, and 0 documented HRSN (model 1 only)
The second multivariable logistic regression, model 2, revealed that housing and employment HRSN had the highest adjusted odds ratios of 2.29 (95% CI: 2.26, 2.32) and 2.28 (95% CI: 2.23, 2.33) respectively (Table 4, Fig. 2). When this model was stratified to those with just 1 HRSN (model 2a) and those with 2 or more (model 2b), we saw a decrease in individual adjusted odds ratios for HRSN in model 2b compared to model 2a, except for housing, which rose to 3.04 (95% CI: 2.93, 3.16) (Table 4, Fig. 2).
Table 4.
Model 2, 2a, and 2b Unadjusted Odds Ratios, Adjusted Odds Ratios, and 95% Confidence Intervals for Ever Having a 30-day Readmission
| Health-related social needs components1 | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Model 2: specific HRSN | ||
| Employment | 3.42 (3.36, 3.49) | 2.28 (2.23, 2.33) |
| Family | 2.05 (2.02, 2.09) | 1.85 (1.81, 1.90) |
| Housing | 4.07 (4.03, 4.12) | 2.29 (2.26, 2.32) |
| Psychosocial | 2.54 (2.47, 2.61) | 1.63 (1.57, 1.68) |
| SES | 2.76 (2.71, 2.81) | 1.63 (1.60, 1.67) |
| Model 2a: 1 HRSN | ||
| Employment | ----- | 2.64 (2.56, 2.72) |
| Family | ----- | 2.09 (2.03, 2.15) |
| Housing | ----- | 2.26 (2.23, 2.30) |
| Psychosocial | ----- | 1.98 (1.88, 2.09) |
| SES | ----- | 1.79 (1.75, 1.84) |
| Model 2b: 2+ HRSN | ||
| Employment | ----- | 1.86 (1.79, 1.93) |
| Family | ----- | 1.57 (1.51, 1.63) |
| Housing | ----- | 3.04 (2.93, 3.16) |
| Psychosocial | ----- | 1.61 (1.54, 1.69) |
| SES | ----- | 1.45 (1.39, 1.51) |
1The HRSN component variables were each their own yes/no, and therefore, the unadjusted results come from 5 different unadjusted logistic regression models. Model 2 evaluated specific health-related social needs (HRSN). We display here only the variables of interest, as the covariate-adjusted odds ratios were nearly identical to model 1. They can be found in Supplemental Table 2
DISCUSSION
To our knowledge, this study is one of the first, and the first using all-payer national data, to demonstrate a dose-response relationship between HSRN and readmission; specifically, as the magnitude of social need increases, so does the readmission rate (Fig. 1). Previous work has identified a relationship between high, compared to low, social need and readmission, while another found no dose-response relationship with mortality.38,41 Our findings on this dose-response relationship further stand apart as the first paper of which we know where social need was captured and recorded in a clinical setting, at the individual level, using ICD-10 Z-codes. The observed relationship highlights that those with documented social needs are at an increased risk for hospital readmission, at much greater rates than those without documented needs (Fig. 1 and Table 2). This relationship is still present even after adjusting for sex, payer, comorbidities, functional limitations, and hospital characteristics with those individuals with HRSN in all 5 domains having 12.5 times the odds of having a 30-day readmission than those without any HRSN (Fig. 2 and Table 3). This work provides evidence of the utility of ICD-10 Z-codes to document HRSN for intervention and research, by presenting estimates of readmission that are largely consistent with previous literature.29
When evaluating the role of specific HRSN, rather than the number of documented HRSN, we observed lower adjusted odds ratios than was found when considering the number of domains in model 1 (Table 4, Fig. 2). When this analysis was further stratified to those with 1 HRSN and those with 2 or more HRSN, we saw that for most HRSN, the adjusted odds ratio was even lower. The exception to this was for housing, which was higher. The increased odds ratios for model 2a underscore that while these individuals are documented to have only 1 HRSN, they likely have more than just 1. Specifically, in model 2a, there is likely confounding by other HRSN, which were not documented. This confounding is partially eliminated in model 2b, as it excludes individuals with just 1 documented HRSN. These findings further demonstrate the impact of having multiple, co-occurring HRSN and that when controlling for other HRSN domains, the effect size of a single HRSN is reduced. The direction of change for housing, while in the opposite direction as the others, confirms its critical role as a HRSN and its impact on readmission. This analysis also reaffirms that future work should continue to expand our understanding of the combinations of HRSN and the total effect on health and health outcomes.
Our findings also support the need to direct resources and interventions to this population and their communities in order to improve their health and wellbeing and reduce readmissions.26,46 As two of the most common HRSN were homelessness and unemployment, and those two domains had the highest adjusted odds ratios in our models, interventions that focus on these two areas, such as permanent supportive housing and employment assistance, should be particularly emphasized.47 However, the dose-response relationship in this study would also support the previously recognized need for programs that are prepared and equipped to address multiple domains of health-related social needs.10 Hospitals should continue to expand efforts to connect patients with social needs to these programs and community partners.
From a healthcare administration and policy perspective, the expanded use of Z-codes would allow for the documentation of patients with complex social needs and ensure that hospitals are not unfairly penalized for care delivered when structural or social factors contribute to readmission. Recently, the Department of Health and Human Services recommended that outcome measures not be adjusted for social risk, citing a myriad of factors including lack of data collection and interoperability, and instead suggest “additional payments or bonuses” to safety net providers.26 The expanded use of Z-codes could not only address the data collection and interoperability issue, as they are collected and stored in a standard format, but would also allow for a more clear and comparable analysis of the specific social needs patients at a given hospital, practice, or provider. Our work reaffirms the important relationship between social risk and outcomes.
This study is limited by the nature of administrative data, including lack of clinical depth and delay in data availability as well as limited demographic data available, notably race. However, this omission is consistent with recommendations to not use race in risk adjustment as a proxy for social risk as race is a socially constructed (and not biological) concept and therefore not a risk factor.23,48 Unfortunately, the data used for this study capture only inpatient hospitalizations during a single year, and lack information regarding other care utilization (such as emergency department visits that do not result in hospitalization), prescription drug utilization, and other health histories. While the Elixhauser comorbidities are the gold standard in health services research and cover a broad range of conditions, they may not provide a complete picture of the specific comorbidities and health needs of those with documented HRSN. Future work should continue to examine the role of comorbidity and multimorbidity (the co-occurrence of chronic conditions, functional limitations, and/or geriatric syndromes49), as well as its association with outcomes, for this population. This may include expanding these often-used comorbidities to include conditions that are particularly important for this population.
A further limitation, and important to this analysis, is the underreporting of Z-codes, as they are not presently billable and not well known to providers. Reimbursement policies relevant to HRSN will likely lead to more complete documentation of Z-codes, and therefore, a better assessment of the health care needs in subgroups of the population with complex social needs. As mentioned above, there are almost certainly individuals who do not have any HRSN clinically documented but do in fact have these needs. This potential bias does not just exist at the individual level, but it is quite plausible that certain facilities or providers will be more likely to document HRSN with Z-codes than others or that certain facilities see a higher volume of patients with social needs and thus are more acutely aware of their coding. For this reason, these estimates of readmission may, in fact, be conservative, not representative of all patients with social needs, and the true dose-response relationship stronger than presently observed. On the other hand, the possibility exists that patients who have frequent admissions and frequent contact with care providers may be more likely to be assigned an HRSN code than patients who have fewer admissions and contacts. This reverse causality may partially inflate the observed relationship. Additionally, it is possible that social factors may be indirectly captured in other diagnosis codes, particularly related to a cause of injury and violence; however, this study sought to examine the use of codes dedicated for HRSN. While the use of Z-codes is still rare, this limitation provides an area for future research. First, to understand potential motivating factors of documenting HRSN using Z-codes, as well as approaches that could estimate the current under-coding, including work to harness previous approaches (e.g., chart review, area-level measures) in combination with Z-codes as we continue to see their expanded use. In addition, care providers should continue to be made aware and trained in the use of Z-codes and the opportunity for documenting HRSN using standard ICD-10 codes.
In conclusion, the relationship between the number of documented HRSN domains and readmission remains even after adjusting for sex, age, payer, functional limitations, comorbidities, and hospital characteristics. This work should motivate the use of ICD-10 Z-codes to better identify and intervene for those who have social needs and promote utilizing these Z-codes to expand the body of knowledge on the impact of social needs and their associated community-level social determinants of health. Finally, this work should encourage change in reimbursement policies and quality improvement initiatives to continue addressing health-related social needs.
Declarations
Conflict of Interest
The authors report no conflicts related to this work. Dr. Koroukian is supported by grants from the National Cancer Institute, Case Comprehensive Cancer Center (P30 CA043703); Ohio Medicaid Technical Assistance and Policy Program (MEDTAPP); National Institutes of Health (R15 NR017792, and UH3-DE025487); The American Cancer Society ( 132678-RSGI-19-213-01-CPHPS and RWIA-20-111-02 RWIA); and by contracts from Cleveland Clinic Foundation, including a subcontract from Celgene Corporation.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014;129(Suppl 2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galea S, Tracy M, Hoggatt KJ, Dimaggio C, Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101(8):1456–1465. doi: 10.2105/AJPH.2010.300086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(Suppl):S28–40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- 4.Adler NE, Stewart J. Preface to the biology of disadvantage: socioeconomic status and health. Ann N Y Acad Sci. 2010;1186:1–4. doi: 10.1111/j.1749-6632.2009.05385.x. [DOI] [PubMed] [Google Scholar]
- 5.Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 6.Ofice of Disease Prevention and Health Promotion. Social Determinants of Health. Department of Health and Human Services. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health#five. Accessed.
- 7.Artiga S, Hinton E. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. Washington, DC: Henry J. Kaiser Family Foundation; 2018. [Google Scholar]
- 8.Lax Y, Martinez M, Brown NM. Social Determinants of Health and Hospital Readmission. Pediatrics. 2017;140(5). [DOI] [PubMed]
- 9.Kangovi S, Grande D. Hospital readmissions--not just a measure of quality. JAMA. 2011;306(16):1796–1797. doi: 10.1001/jama.2011.1562. [DOI] [PubMed] [Google Scholar]
- 10.National Academies of Sciences E, Medicine. Investing in Interventions That Address Non-Medical, Health-Related Social Needs: Proceedings of a Workshop. Washington, DC: The National Academies Press; 2019. [PubMed]
- 11.Castrucci B, Auerbach J. Meeting Individual Social Needs Falls Short Of Addressing Social Determinants Of Health. Health Affairs Blog. 2019.
- 12.Lee J, Korba C.Social determinants of health: How are hospitals and health systems investing in and addressing social needs? : Deloitte;2017.
- 13.Finkelstein A, Zhou A, Taubman S, Doyle J. Health Care Hotspotting - A Randomized, Controlled Trial. N Engl J Med. 2020;382(2):152–162. doi: 10.1056/NEJMsa1906848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a Housing and Case Management Program on Emergency Department Visits and Hospitalizations Among Chronically Ill Homeless Adults A Randomized Trial. Jama-J Am Med Assoc. 2009;301(17):1771–1778. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 15.Kangovi S, Mitra N, Norton L, et al. Effect of Community Health Worker Support on Clinical Outcomes of Low-Income Patients Across Primary Care Facilities: A Randomized Clinical Trial. JAMA Intern Med. 2018;178(12):1635–1643. doi: 10.1001/jamainternmed.2018.4630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bielaszka-DuVernay C. The 'GRACE' model: in-home assessments lead to better care for dual eligibles. Health Aff (Millwood). 2011;30(3):431–434. doi: 10.1377/hlthaff.2011.0043. [DOI] [PubMed] [Google Scholar]
- 17.McClintock HF, Bogner HR. Incorporating Patients' Social Determinants of Health into Hypertension and Depression Care: A Pilot Randomized Controlled Trial. Community Ment Health J. 2017;53(6):703–710. doi: 10.1007/s10597-017-0131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reidhead M, Moyer L, Gerimann A.Z Codes for Social Determinants of Health: Which hospitals are most likely to use them and for which patients? : Missouri Hospital Association;2020.
- 19.Reidhead M.Decoding Social Determinants of Health. Missiouri Hospital Association; 09/2018 2018.
- 20.Freiedman NL. Toward Addressing Social Determinants of Health: A Health Care System Strategy. The Permanente Journal. 2018.
- 21.Weeks WB, Cao SY, Lester CM, Weinstein JN, Morden NE. Use of Z-Codes to Record Social Determinants of Health Among Fee-for-service Medicare Beneficiaries in 2017. J Gen Intern Med. 2019. [DOI] [PMC free article] [PubMed]
- 22.Mathew J, Hodge C, Hjau M. Z Codes Utilization among Medicare Fee-for-Service (FFS) Beneficiaries in 2017. Baltimore, MD: CMS Office of Minority Health; 2020. [Google Scholar]
- 23.National Quality Forum. Risk Adjustment for Socioeconomic Status or Other Sociodemographic Factors. Washington, DC 2014.
- 24.Ash AS, Mick EO, Ellis RP, Kiefe CI, Allison JJ, Clark MA. Social Determinants of Health in Managed Care Payment Formulas. JAMA Intern Med. 2017;177(10):1424–1430. doi: 10.1001/jamainternmed.2017.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Quality Forum. Evaluation of the NQF Trial Period for Risk Adjustment for Social Risk Factors. Washington, DC 2017.
- 26.Office of the Assistant Secretary for Planning and Evaluation. Second Report to Congress on Social Risk Factors and Performance in Medicare’s Value-Based Purchasing Program. Washington, DC: U.S. Department of Health & Human Services; 2020.
- 27.UnitedHealthcare and the AMA Collaborate to Understand and Address Social Barriers Preventing People’s Access to Better Health [press release]. Minnetonka, Minnesota and Chicago: BusinessWire, 04/02/2019 2019.
- 28.Gottlieb L, Tobey R, Cantor J, Hessler D, Adler NE. Integrating Social And Medical Data To Improve Population Health: Opportunities And Barriers. Health Aff (Millwood). 2016;35(11):2116–2123. doi: 10.1377/hlthaff.2016.0723. [DOI] [PubMed] [Google Scholar]
- 29.Carter J, Ward C, Thorndike A, Donelan K, Wexler DJ. Social Factors and Patient Perceptions Associated With Preventable Hospital Readmissions. J Patient Exp. 2020;7(1):19–26. doi: 10.1177/2374373518825143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Joynt Maddox KE, Reidhead M, Hu J, et al. Adjusting for social risk factors impacts performance and penalties in the hospital readmissions reduction program. Health Serv Res. 2019;54(2):327–336. doi: 10.1111/1475-6773.13133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meddings J, Reichert H, Smith SN, et al. The Impact of Disability and Social Determinants of Health on Condition-Specific Readmissions beyond Medicare Risk Adjustments: A Cohort Study. J Gen Intern Med. 2017;32(1):71–80. doi: 10.1007/s11606-016-3869-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Navathe AS, Zhong F, Lei VJ, et al. Hospital Readmission and Social Risk Factors Identified from Physician Notes. Health Serv Res. 2018;53(2):1110–1136. doi: 10.1111/1475-6773.12670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang Y, Zhang Y, Sholle E, et al. Assessing the impact of social determinants of health on predictive models for potentially avoidable 30-day readmission or death. PLoS One. 2020;15(6):e0235064. doi: 10.1371/journal.pone.0235064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765–774. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hu J, Gonsahn MD, Nerenz DR. Socioeconomic status and readmissions: evidence from an urban teaching hospital. Health Aff (Millwood). 2014;33(5):778–785. doi: 10.1377/hlthaff.2013.0816. [DOI] [PubMed] [Google Scholar]
- 36.Hu J, Kind AJH, Nerenz D. Area Deprivation Index Predicts Readmission Risk at an Urban Teaching Hospital. Am J Med Qual. 2018;33(5):493–501. doi: 10.1177/1062860617753063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Joynt Maddox KE, Chen LM, Zuckerman R, Epstein AM. Association Between Race, Neighborhood, and Medicaid Enrollment and Outcomes in Medicare Home Health Care. J Am Geriatr Soc. 2018;66(2):239–246. doi: 10.1111/jgs.15082. [DOI] [PubMed] [Google Scholar]
- 38.Demianczyk AC, Behere SP, Thacker D, et al. Social Risk Factors Impact Hospital Readmission and Outpatient Appointment Adherence for Children with Congenital Heart Disease. J Pediatr. 2019;205:35–40. doi: 10.1016/j.jpeds.2018.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hatef E, Searle KM, Predmore Z, et al. The Impact of Social Determinants of Health on Hospitalization in the Veterans Health Administration. Am J Prev Med. 2019;56(6):811–818. doi: 10.1016/j.amepre.2018.12.012. [DOI] [PubMed] [Google Scholar]
- 40.Schootman M, Lian M, Pruitt SL, et al. Hospital and geographic variability in thirty-day all-cause mortality following colorectal cancer surgery. Health Serv Res. 2014;49(4):1145–1164. doi: 10.1111/1475-6773.12171a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sterling MR, Ringel JB, Pinheiro LC, et al. Social Determinants of Health and 90-Day Mortality After Hospitalization for Heart Failure in the REGARDS Study. J Am Heart Assoc. 2020;9(9):e014836. doi: 10.1161/JAHA.119.014836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Joynt KE, Jha AK. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ Cardiovasc Qual Outcomes. 2011;4(1):53–59. doi: 10.1161/CIRCOUTCOMES.110.950964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tsai TC, Orav EJ, Joynt KE. Disparities in surgical 30-day readmission rates for Medicare beneficiaries by race and site of care. Ann Surg. 2014;259(6):1086–1090. doi: 10.1097/SLA.0000000000000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schiltz NK, Dolansky MA, Warner DF, Stange KC, Gravenstein S, Koroukian SM. Impact of Instrumental Activities of Daily Living Limitations on Hospital Readmission: an Observational Study Using Machine Learning. J Gen Intern Med. 2020. [DOI] [PMC free article] [PubMed]
- 45.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 46.American Academy of Family Physicians. The EveryONE Project: Neighborhood Navigator. https://www.aafp.org/family-physician/patient-care/the-everyone-project/neighborhood-navigator.html. Published 2021. Accessed 2021.
- 47.Rog DJ, Marshall T, Dougherty RH, et al. Permanent supportive housing: assessing the evidence. Psychiatr Serv. 2014;65(3):287–294. doi: 10.1176/appi.ps.201300261. [DOI] [PubMed] [Google Scholar]
- 48.Boyd RW, Lindo EG, Weeks LD, R MM. On Racism: A New Standard For Publishing On Racial Health Inequities. Health Affairs Blog. 2020.
- 49.Warner DF, Schiltz NK, Stange KC, et al. Complex multimorbidity and health outcomes in older adult cancer survivors. Fam Med Community Health. 2017;5(2):129–138. doi: 10.15212/FMCH.2017.0127. [DOI] [PMC free article] [PubMed] [Google Scholar]