Objective
This study aimed to establish whether there was a decrease in the rate of prematurity in France after the beginning of lockdown (March 17, 2020) and whether there was an increase in the rate of stillbirths compared with 2017 to 2019.
Study Design
We included all births from January to September of each year from 2017 to 2020 from the national Programme de Médicalisation des Systèmes d’Information database: 496,171 newborns from women with singleton pregnancies and 15,441 newborns from women with multiple pregnancies were included for 2020. Concerning the 2017 to 2019 period, we included a mean of 518,798 newborns from women with singleton pregnancies and 16,441 newborns from women with multiple pregnancies per year. Prematurity was defined according to the World Health Organization classification as a birth that occurred before 37 weeks’ gestation (WG).1 We also studied extremely preterm births (before 28 WG), moderate preterm births (between 28 and 31 WG), and late preterm births (between 32 and 36 WG). Prematurity rates were compared by month between the 2 periods (January to September months of 2017, 2018, and 2019 vs January to September 2020) using chi-squared test, and the variations (relative risk difference) were calculated. We also identified hospital stays for COVID-19 in 2020 in relation to the date of admission during pregnancy by International Classification of Diseases, Tenth Revision, codes U0710, U0711, U0712, U0714, or U0715. This algorithm has been used in previous studies.2 , 3 This study was approved by institutional review boards.
Results
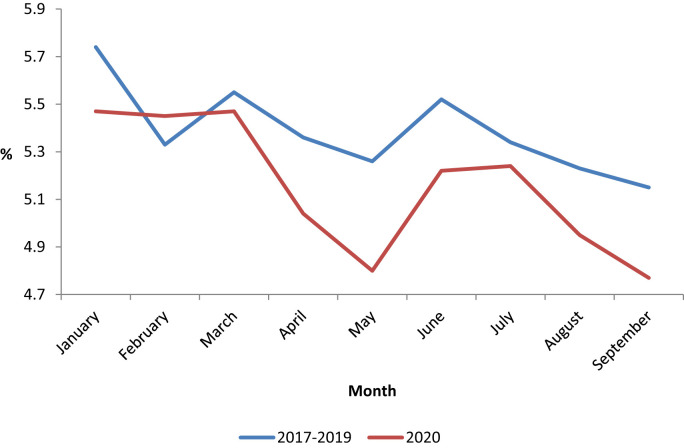
Between April to May 2017 to 2019 and April to May 2020, there was a decrease of −7.53% in the rate of prematurity (from 5.31% to 4.91%; P<.01) for singleton pregnancies (Figure ). Between these 2 periods, the rate of change was −12.90% between 22 and 27 WG (P=.03), +1.96% between 28 and 31 WG (P=.69), and −8.24% between 32 and 36 WG (P<.01). The decrease in the rate of prematurity was still observed after the end of lockdown (from June to September 2020). For multiple births, there was no decrease in prematurity between January to September 2017 to 2019 and January to September 2020: 50.14% vs 50.36% (P=.63), respectively, for twins and 95.51% vs 94.9% (P=.62), respectively, for high-order multiple pregnancies. In January to September, there were 363 stillbirths among singleton pregnancies in 2017 to 2019 and 114 in 2020 (0.00% change rate). Among the 1752 women with a diagnosis of SARS-CoV-2 infection with singleton pregnancies, the rate of prematurity was higher in 2020 than in 2017 to 2019 (9.93% vs 5.32%; P<.01), regardless of the severity of prematurity (P<.05 for all). On the contrary, the rate of prematurity was lower among women who were uninfected or untested in 2020 than among women who delivered in 2017 to 2019 (4.67% vs 5.32%; P<.01), regardless of the severity of prematurity (P<.05 for all).
Figure.
Rate of prematurity among singleton births
By month for 2017 to 2019 and 2020.
Simon. Impact of the COVID-19 pandemic on preterm birth and stillbirth. Am J Obstet Gynecol 2021.
Conclusion
Large-scale socioenvironmental modifications like the lockdown in spring 2020 may be associated with beneficial effects on perinatal morbidity. We did not find an increase in the rate of stillbirth since the beginning of the pandemic. At this stage, the practical consequences are not obvious, but our results encourage further reflection regarding behaviors that could modify the risk of prematurity outside of the context of an epidemic.
Acknowledgments
The authors thank Suzanne Rankin for reviewing the English and Gwenaëlle Periard for her help with the layout and management of this article.
Footnotes
The authors E.S. and J.C. contributed equally to the article.
The project was funded by the French National Research Agency.
The authors report no conflict of interest.
References
- 1.Blencowe H., Cousens S., Oestergaard M.Z., et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 2.Piroth L., Cottenet J., Mariet A.S., et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respir Med. 2021;9:251–259. doi: 10.1016/S2213-2600(20)30527-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mariet A.S., Giroud M., Benzenine E., et al. Hospitalizations for stroke in France during the COVID-19 pandemic before, during, and after the national lockdown. Stroke. 2021;52:1362–1369. doi: 10.1161/STROKEAHA.120.032312. [DOI] [PubMed] [Google Scholar]