Abstract
Purpose
To evaluate outcomes for a combined osteoligamentous reconstruction technique for Neer Type IIB clavicle fractures.
Methods
Patients with Neer Type IIB clavicle fractures treated with combined clavicular locking plate and coracoclavicular ligament suture reconstruction were identified. Demographics, clinical outcomes, and radiographic outcomes were collected.
Results
Twenty-four patients with mean 13 months of follow-up were included. Bony union and normal radiographic coracoclavicular relationship were achieved in 23 (96%) patients. The mean UCLA Shoulder score was 33.3. Three (13%) complications occurred.
Discussion
The combined osteoligamentous reconstruction approach as described is a successful option for treating Neer Type IIB clavicle fractures.
Keywords: Distal clavicle, Fracture, Neer type II, Coracoclavicular ligament, Locking plate, Surgical technique
1. Introduction
Fractures of the distal third of the clavicle were first classified by Neer based on the position of the fracture line relative to the coracoclavicular (CC) ligament.1 Although these fractures only account for 10–30% of clavicle fractures, they account for 30–45% of all clavicle fracture nonunions.2, 3, 4, 5 Within the Neer classification, Type II fractures are characterized by significant displacement and can be further subdivided into Type IIA and Type IIB fractures.1,2 Type IIA fractures occur medial to the CC ligaments without any ligament disruption. Conversely, Type IIB fractures occur either between the conoid and trapezoid ligament of the CC ligament complex with rupture of the conoid ligament or lateral to the CC ligaments with rupture of both ligaments. Disruption of the ligaments makes these fractures unstable due to the superior displacement of the medial fragment and much more likely to require surgery versus nonoperative treatment, which has higher nonunion rates.1,6
Treating these fractures is challenging due to the small distal fragment that makes obtaining adequate fixation and maintaining reduction difficult. Various techniques have been described including hook plates, tension band constructs, and joint-spanning locking plates.7, 8, 9, 10, 11, 12, 13, 14 Many early, more established fixation methods are associated with high reoperation rates due to symptomatic hardware or planned removal of hardware. More recently, newer techniques involving flexible constructs using fiber tapes or tendon allograft to recreate the disrupted CC ligament have emerged in place of rigid osteosynthesis.15, 16, 17, 18, 19 Despite the many options available, there is not yet a consensus on surgical technique for treatment of Neer IIB distal clavicles fractures.
At our institution, Type IIB fractures are treated using a technique involving a clavicular locking plate and CC ligament reconstruction with suture tape. We hypothesize the suture tape reduces stress on the locking plate and subsequently results in less fixation failure than rigid osteosynthesis alone. The purpose of this study is to assess the clinical and radiographic outcomes of a standardized surgical technique for fixing unstable Neer type IIB distal clavicle fractures that uses a combined osteoligamentous reconstruction with a distal clavicular specific locking plate and CC ligament reconstruction.
2. Materials and methods
This is an IRB approved, retrospective study. Between January 1, 2013 and March 31, 2020 thirty consecutive patients with displaced distal clavicle fractures with CC ligament rupture (Neer type IIb, Fig. 1a) treated by one of five orthopedic surgeons underwent open reduction internal fixation with a locking plate and concurrent CC ligament reconstruction (Fig. 1b). Three fellowship trained orthopedic trauma surgeons reviewed all injury radiographs to confirm Neer type IIB classification prior to each patient being included in the cohort. Patients without at least 6 months of follow-up were excluded from the final cohort. Patient's charts were reviewed for demographic, injury, surgery and outcome data such as age, sex, type of fracture, mechanism of injury, time to surgery, surgery duration, length of follow-up, complications, pain, reoperations, and range of motion at the latest follow-up visit. Mechanism of injury for each patient was categorized into low energy, high energy, and motor vehicle accidents (MVA). The low energy group included ground level falls or an equivalent, while the high energy group included bicycling, skateboarding, skiing, and horseback riding accidents. Clinical outcomes at the latest follow-up visit were assessed using the University of California, Los Angeles (UCLA) Shoulder rating scale.20 Shoulder range of motion was measured by the treating surgeon and included forward elevation, external rotation and internal rotation with the hand behind the back. Postoperative radiographs were assessed for radiographic healing. Coracoclavicular distance was measured on injury and postoperative radiographs using the “ruler” tool on the PACS (Siemens, Ehrlanger, Germany). Means with standard deviation were calculated for numerical variables, while incidence was calculated for categorical variables.
Fig. 1a.
Neer Type IIB distal clavicle fracture with CC ligament disruption.
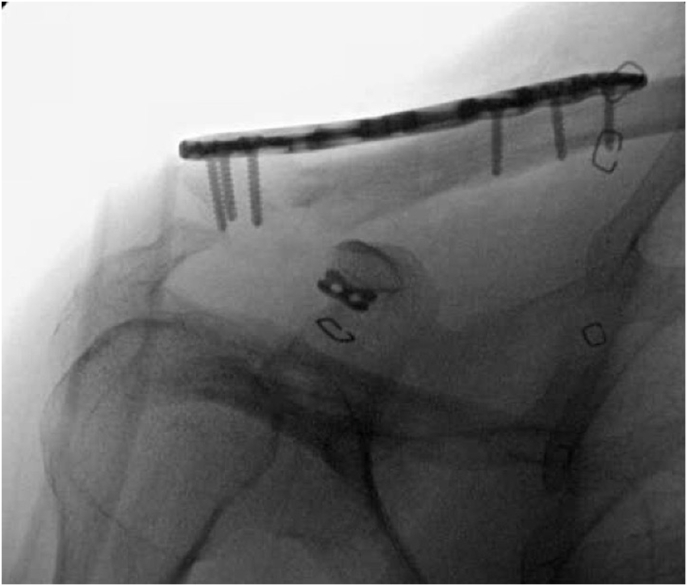
Fig. 1b.
Surgical repair with locking plate and CC ligament reconstruction.
2.1. Surgical technique
A sabre incision was made from the AC joint to the coracoid. The deltopectoral interval was developed distally and the coracoid directly visualized. With the coracoid protected, a cannulated drill was passed through the coracoid base and a suture passer fed through the cannulation. Next the #5 suture tape with a button on it was passed through the coracoid. Next, a drill hole was created in the medial clavicular fragment medial enough to the fracture line to prevent fracture propagation and the suture tape again passed proximally. Following fracture site reduction, a distal clavicular locking plate is applied superiorly. The suture tape ends are passed through two separate holes in the plate or a self-locking suture button. The tapes are tensioned prior to plate fixation. The plate is fixed with several mini-fragment bicortical locking screws into the lateral fragment and at least two bicortical 3.5 mm locking screws medially. Following bony fixation, the suture tape is tied down over the plate or through a suture button on top of the plate to reconstruct the CC ligaments. Intraoperative image films are obtained to confirm reduction of the fracture and CC distance (Fig. 1b). Closure is performed in layers with a monofilament for the skin.
3. Results
Of the 30 patients identified, one patient died of unrelated causes and 5 were lost to follow up, leaving 24 patients (80%) with a minimum 6 months of follow up (Table 1). The cohort had a mean age of 43 years (range: 18 to 84). There were 18 males and 6 females. Mechanism of injury was low energy fall in 5 patients (21%), high energy fall in 18 patients (75%) and MVA in 1 patient (4%). All of the fractures were initially closed. One elderly patient in the cohort initially refused surgery and was treated non operatively until the medial fragment ulcerated through the skin and the fracture site became exposed. Average time to surgery was 10.5 days (range: 2–32 days), and average surgery duration was 97.5 min (range: 72–137 min).
Table 1.
Demographic, injury, and surgery information for cohort. All patients initially presented with closed fractures.
| Patient No. | Age at Surgery (Years) | Sex | Injury | Mechanism of Injury | Time to Surgery (Days) | Surgery Duration (Minutes) |
|---|---|---|---|---|---|---|
| 1 | 68 | M | Neer IIB Closed Fracture | high energy | 16 | 91 |
| 2 | 18 | F | Neer IIB Closed Fracture | low energy | 4 | 91 |
| 3 | 47 | M | Neer IIB Closed Fracture | high energy | 8 | 84 |
| 4 | 34 | F | Neer IIB Closed Fracture | high energy | 6 | 72 |
| 5 | 25 | M | Neer IIB Closed Fracture | high energy | 16 | 72 |
| 6 | 24 | M | Neer IIB Closed Fracture | high energy | 5 | 102 |
| 7 | 25 | F | Neer IIB Closed Fracture | high energy | 7 | 91 |
| 8 | 57 | M | Neer IIB Closed Fracture | motor vehicle accident | 2 | 96 |
| 9 | 27 | M | Neer IIB Closed Fracture | high energy | 16 | 108 |
| 10 | 23 | F | Neer IIB Closed Fracture | high energy | 2 | 79 |
| 11 | 57 | F | Neer IIB Closed Fracture | high energy | 10 | 101 |
| 12 | 44 | M | Neer IIB Closed Fracture | high energy | 7 | 101 |
| 13 | 48 | M | Neer IIB Closed Fracture | high energy | 6 | 84 |
| 14 | 22 | M | Neer IIB Closed Fracture | high energy | 27 | 111 |
| 15 | 62 | M | Neer IIB Closed Fracture | low energy | 9 | 113 |
| 16 | 59 | F | Neer IIB Closed Fracture | high energy | 18 | 112 |
| 17 | 27 | M | Neer IIB Closed Fracture | high energy | 9 | 90 |
| 18 | 31 | M | Neer IIB Closed Fracture | high energy | 7 | 84 |
| 19 | 84 | M | Neer IIB Open Fracture | low energy | 32 | 92 |
| 20 | 54 | M | Neer IIB Closed Fracture | low energy | 3 | 137 |
| 21 | 30 | M | Neer IIB Closed Fracture | high energy | 10 | 87 |
| 22 | 75 | M | Neer IIB Closed Fracture | high energy | 16 | 93 |
| 23 | 63 | M | Neer IIB Closed Fracture | high energy | 10 | 119 |
| 24 | 28 | M | Neer IIB Closed Fracture | low energy | 6 | 87 |
| Mean: 43 ± 19 | Total: 18 males 6 females |
Total: 23 closed 1 open |
Total: 5 low energy 18 high energy 1 motor vehicle accident |
Mean: 10.5 ± 7.5 | Mean: 95.7 ± 15.3 |
Mean follow up was 13 months (range: 6–28 months) (Table 2). Shoulder range of motion as measured by the treating surgeon at latest follow up was mean forward elevation of 168° (range: 120–180°), mean external rotation of 57° (range: 20–90°) and mean internal rotation to the T7 vertebral level (range: L4 to T3 level). The mean UCLA Shoulder score was 33.3 out of 35 (range: 29 to 35). Twenty-three patients (96%) went on to bony union and ligamentous stability (Table 3). Mean preoperative CC distance was 22.3 mm (range: 17–29 mm). Postoperative CC distance and CC distance at final follow up were 11.8 mm (range: 8–15 mm) and 12.5 mm (range: 8–18 mm), respectively.
Table 2.
Clinical outcomes for cohort. Average follow-up period was 13 months.
| Patient No. | Follow up (months) | Complication (Y/N) | Description | Pain (Y/N) | Reoperation (Y/N) | Description | Forward Elevation (Degrees) | External Rotation (Degrees) | Internal Rotation (Degrees) | UCLA Shoulder Score | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 28 | N | Y | Y | removal of hardware | 160 | 30 | T8 | 33 | ||
| 2 | 24 | N | Y | Y | removal of hardware | 180 | 60 | T3 | 33 | ||
| 3 | 23 | N | N | N | 160 | 30 | T8 | 31 | |||
| 4 | 21 | N | Y | Y | removal of hardware | 180 | 80 | T4 | 29 | ||
| 5 | 19 | N | N | N | 170 | 90 | T5 | 35 | |||
| 6 | 18 | N | N | N | 180 | 90 | T4 | 33 | |||
| 7 | 18 | N | N | N | 165 | 50 | T10 | 35 | |||
| 8 | 16 | N | N | N | 180 | 45 | T4 | 31 | |||
| 9 | 16 | Y | Nonunion with infection | Y | Y | Removal of hardware with iliac crest bone graft | 160 | 50 | T4 | 33 | |
| 10 | 12 | N | N | N | 180 | 90 | T4 | 35 | |||
| 11 | 12 | N | N | N | 170 | 45 | T12 | 35 | |||
| 12 | 12 | N | N | N | 180 | 90 | T4 | 35 | |||
| 13 | 12 | Y | Pulmonary Embolism | N | N | 160 | 30 | T8 | 33 | ||
| 14 | 11 | N | N | N | 170 | 50 | T4 | 35 | |||
| 15 | 10 | N | Y | Y | removal of hardware | 120 | 20 | L4 | 30 | ||
| 16 | 10 | N | N | N | 180 | 60 | T10 | 35 | |||
| 17 | 8 | N | N | N | 180 | 90 | T5 | 35 | |||
| 18 | 7 | N | Y | N | 160 | 30 | T8 | 33 | |||
| 19 | 6 | Y | Nonunion, Hardware Failure | N | N | 170 | 70 | T4 | 35 | ||
| 20 | 6 | N | N | N | 150 | 30 | L3 | 31 | |||
| 21 | 6 | N | N | N | 180 | 90 | T4 | 31 | |||
| 22 | 6 | N | N | N | 170 | 90 | T4 | 35 | |||
| 23 | 6 | N | N | N | 160 | 30 | T8 | 35 | |||
| 24 | 6 | N | N | N | 160 | 30 | T8 | 33 | |||
| Mean: 13.1 ± 6.6 | Total: 3 (13%) | Total: 6 (25%) | Total: 5 (21%) | Mean: 167.7 ± 13.8 | Mean: 57.1 ± 25.7 | Mean: T7 ± 4 levels | Mean 33.3 ± 1.9 | ||||
Table 3.
Radiographic outcomes for cohort. 23 out of 24 patients achieved radiographic healing.
| Patient No. | Radiographic Healing (Y/N) | Preoperative CC Distance (mm) | Postoperative CC Distance (mm) | Final Follow Up CC Distance (mm) |
|---|---|---|---|---|
| 1 | Y | 22 | 11 | 11 |
| 2 | Y | 20 | 11 | 12 |
| 3 | Y | Unavailable | 13 | 14 |
| 4 | Y | Unavailable | 8 | 8 |
| 5 | Y | 26 | 14 | 14 |
| 6 | Y | Unavailable | 15 | 15 |
| 7 | Y | Unavailable | 11 | 11 |
| 8 | Y | Unavailable | 12 | 12 |
| 9 | Y | 19 | 14 | 14 |
| 10 | Y | 26 | 10 | 11 |
| 11 | Y | 23 | 14 | 15 |
| 12 | Y | Unavailable | 9 | 10 |
| 13 | Y | 29 | 12 | 13 |
| 14 | Y | 17 | 15 | 15 |
| 15 | Y | 25 | 15 | 15 |
| 16 | Y | 17 | 9 | 10 |
| 17 | Y | 24 | 11 | 11 |
| 18 | Y | 22 | 10 | 11 |
| 19 | N | 19 | 12 | 18 |
| 20 | Y | Unavailable | 13 | 13 |
| 21 | Y | 17 | 10 | 10 |
| 22 | Y | 26 | 9 | 10 |
| 23 | Y | 25 | 15 | 15 |
| 24 | Y | Unavailable | 11 | 11 |
| Total: 23 (96%) | Mean: 22.3 ± 3.8 | Mean: 11.8 ± 2.2 | Mean: 12.5 ± 2.4 |
Note: Preoperative imaging was unavailable for 8 patients who initially presented to an outside hospital.
Three patients (13%) sustained complications. One patient had an uncomplicated pulmonary embolism on post-op day 6 and was treated successfully with Warfarin on an outpatient basis. Of note, he had a history of two prior pulmonary embolisms. The second complication was in an elderly male who had an early fixation failure with fragment re-displacement following development of a delayed open wound. He had initially refused operative intervention and at 4 weeks the medial fragment eroded though his skin. His soft tissue envelope remained closed following surgery and he declined further intervention. The third patient experienced a bony nonunion with maintenance of the CC relationship and underwent reoperation 15 months after his initial repair (Fig. 2a). His second operation consisted of removal of hardware (ROH) and nonunion repair with iliac crest bone graft (ICBG). Cultures from the nonunion site were positive for Cultibacterium acnes, so he was given a course of antibiotic as an outpatient. At his most recent follow up 3 months after the procedure, x-rays demonstrated interval healing at the nonunion site (Fig. 2b). Four other patients underwent elective removal of hardware after healing for discomfort with specific movements or with sleeping. All four resulted in resolution of symptoms.
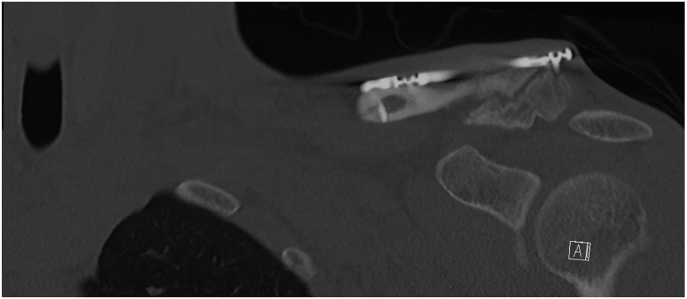
Fig. 2a.
Distal fracture gap under locking plate at 15 months post op.
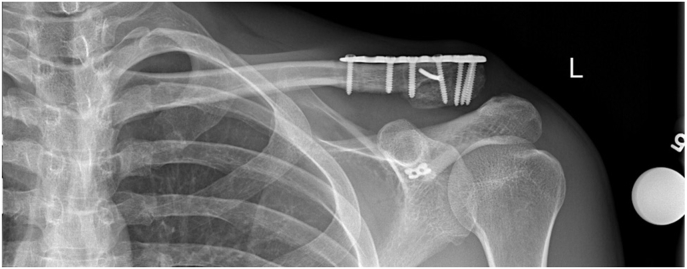
Fig. 2b.
Interval healing at 2 months post op ROH and ICBG placement.
4. Discussion
In this study, we have demonstrated that our surgical technique using a locking plate with CC ligament reconstruction for treating Type IIB distal clavicle fractures resulted in successful clinical and radiographic healing with a relatively low complication rate in a cohort of 24 patients. The large majority of patients in our cohort recovered to their baseline functional status without any pain, while a small subset reported mild pain with specific daily activities. The pain reported in this small subset resolved following removal of hardware. While our sample size was relatively small, we ultimately achieved bony union and maintained CC relationship in 23 out of 24 patients, which is consistent with other fixation techniques reported in the literature.21
Neer Type II fractures are characterized by the significant displacement due to the proximal segment separating from the CC ligaments.1,2 Type II fractures can be further subdivided into Type IIA and Type IIB fractures. In Type IIA fractures, the fracture occurs medially to the CC ligaments and the ligaments remain intact, while in Type IIB fractures the fracture occurs either between or lateral to the CC ligaments and either one or both of the CC ligaments are disrupted. Type II fractures are considered unstable and have a high rate of nonunion with nonoperative management, so they are often treated surgically.1,2,6 In one retrospective study comparing operative management to nonoperative management for Type II fractures, the authors found that operative management resulted in a lower rate of nonunions, but the two groups did not differ in functional outcomes.6
Treating Type II fractures surgically has proven challenging for surgeons over the years due to difficulty in obtaining adequate fixation. Since the distal fragment can be very small, there is often only a limited area remaining distally for screw purchase, leaving the construct susceptible to failure.22 When the fixation fails with plate and screws, the reduction between the medial and distal fragments is lost. This challenge led to innovation with other techniques such as a CC ligament fixation. Theoretically, it was thought that CC ligament fixation would take some of the fixation tension off of the plate alone, and thus lead to less failure. Currently, there are several techniques proposed in the literature designed to restore normal anatomy and function for type IIB fractures, but a gold standard has yet to be declared for management of these fractures. Proposed techniques include different variations of hook plating, clavicular locking plates, CC fixation, and tension banding.7, 8, 9, 10, 11, 12, 13, 14
Hook plating is the most well studied of these techniques and has been associated with several complications including impingement, acromioclavicular joint arthrosis, acromial osteolysis, and need for removal.7,8,23 In one prospective study of 36 patients who underwent surgery with a hook plate, 92% of the patients underwent reoperation to remove the hook plate to prophylactically mitigate the risk of impingement.8 Despite the high reoperation rate, 95% went on to bony union. In another study which retrospectively reviewed 44 patients treated with hook plates, 68% of patients required removal of the hook plate due to discomfort associated with the implant.7 Additionally, this study reported 10 complications (23%) including implant dislocation, pseudoarthrosis, superficial wound infections, hypertrophic scar tissue, and acromial osteolysis. The technique described in our study uses a clavicular locking plate instead of a hook plate. In our study, we observed a similar union rate (96%) with a considerably lower complication (13%) and reoperation (20%) rates compared to hook plating. While most who undergo removal of hardware end up having good outcomes, it is still always optimal to minimize the need for reoperation to avoid the risks of surgery such as infection or anesthesia complications. Additional retrospective studies directly comparing hook plates to locking plates types have also demonstrated lower complication and reoperation rates with locking plates, further supporting its use over hook plates for fixation of Neer Type II fractures.10,11
There have also been studies evaluating techniques focused on stabilizing the CC ligament without the use of plating. Cho et al.15 proposed a technique which uses a suture button for stabilization of the CC ligament. Of the 18 cases reported by the authors, 94% of patients achieved bony union and 22% experienced complications. In a different study evaluating the use of tension banding combined with a suture anchor or flip button for CC augmentation, all thirteen patients successfully reached bony union and returned to their normal daily activities within 5 months.9 Both of these techniques demonstrated similar union and complication rates to the technique used in our study. It is clear that a major advantage of these techniques is avoiding the need for removal of the implant commonly seen with plate fixation techniques. However, since both of these studies were relatively small, questions still remain about whether CC ligament fixation alone is a strong enough construct to maintain reduction between the medial and distal fragments. Furthermore, it's unclear if these techniques result in similar outcomes for both patterns of Type IIB fractures. Given the very small distal fragment with Type IIB fractures lateral to the CC ligament complex, CC ligament reconstruction alone may be more suitable for this fracture pattern.
The literature on plate fixation combined with CC reconstruction is sparse. We are only aware of a few small studies that assessed an osteoligamentous repair similar to the technique described in this paper. Han et al.12 retrospectively evaluated twelve patients with Neer Type IIB treated with a locking plate and coracoclavicular augmentation with a suture anchor. Bony union was reached within 3 months in all patients. The cohort did not experience any complications and had good clinical outcomes measured by validated shoulder scoring tools. In another study, Hohmann et al.13 assessed outcomes in 31 patients with Neer Type II fractures repaired with a superiorly placed distal radius locking plate and coracoclavicular augmentation with a suture fixation system using two suture buttons. After 12 months of follow up, the cohort had positive clinical outcomes as measured by validated scoring tools, and all but one patient went on to bony union. The one nonunion required re-plating and bone grafting. The only other complication was a superficial wound infection.
The techniques described in these two studies differed from ours in a few ways. First, Hohmann et al. used a distal radius plate instead of a clavicular plate. Furthermore, both the Hohmann et al. and Han et al. techniques involve fixating the plate prior to reconstructing the CC ligament. In our technique, the CC ligament is first reconstructed and reduced before the plate is fixed with screws. Lastly, these two techniques reconstructed the CC ligament using a suture anchor or a suture fixation system with two suture buttons, while we used a suture tape secured over the plate or through a suture button. It should also be noted our technique secures the suture tape to the coracoid through a drillhole rather than a loop around the bone in order to avoid osteolysis described as a complication of certain suspensory looping techniques.24 Both of these studies reported lower complication and reoperation rates, but similar bony union rates when compared to our cohort. Additionally, with an average UCLA Shoulder score of 33.3 out of 35, our technique also resulted in positive clinical and functional outcomes for patients as measured by a validated shoulder scoring tool. Despite the slight difference in outcomes between the techniques described in the above studies, it is difficult to determine if one approach is superior without conducting a comparative study. Nevertheless, we feel the Han et al. and Hohmann et al. studies provide additional evidence that an osteoligamentous repair is a reasonable approach with good clinical and radiographic outcomes for the treatment Neer Type II fractures.
In this paper we describe a technique that uses a combined osteoligamentous reconstruction with a locking plate and concurrent CC ligament reconstruction to treat Neer Type IIB fractures. The relatively low complication rate and positive clinical and radiographic outcomes seen in our cohort support the notion that our technique is a feasible way to treat Neer Type IIB fractures and is worth further investigating. One of the nonunions in our cohort occurred in an elderly gentleman with an open fracture. The other nonunion, thought to be secondary to infection, healed after ROH and ICBG. Both patients reported good functional outcomes at their latest follow up visits.
The major limitation of our study is its retrospective and non-comparative study design. Furthermore, the cohort included a relatively small sample size with variable follow-up periods, which limits any conclusions that can be drawn. Additionally, its generalizability is limited since all procedures were performed at a single academic medical center in a major city. Lastly, an element of observer bias could have existed in our study as range of motion values were measured by five different surgeons.
5. Conclusions
The technique described in this paper appears to be an effective option for treating Neer Type IIb distal clavicle fractures based on the overall positive results seen in our cohort. While our findings are encouraging, future prospective studies will need to be done comparing our technique to other techniques reported in the literature before any major conclusions can be drawn. However, at this time we do still feel our technique is an improvement on plating alone for distal clavicular fractures and one for surgeons to consider using when treating Neer Type IIb distal clavicle fractures.
Declaration of competing interest
None.
References
- 1.Neer C.S., II Fractures of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma. 1963;99–110 doi: 10.1097/00005373-196303000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Neer C.S., II Fractures of the distal third of the clavicle. Clin Orthop. 1968;58:43–50. [PubMed] [Google Scholar]
- 3.Nordqvist A., Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–132. [PubMed] [Google Scholar]
- 4.Banerjee R., Waterman B., Padalecki J., Robertson W. Management of distal clavicle fractures. J Am Acad Orthop Surg. 2011;19(7):392–401. doi: 10.5435/00124635-201107000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Kim D.W., Kim D.H., Kim B.S., Cho C.H. Current concepts for classification and treatment of distal clavicle fractures. Clin Orthop Surg. 2020;12(2):135–144. doi: 10.4055/cios20010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rokito A.S., Zuckerman J.D., Shaari J.M., Eisenberg D.P., Cuomo F., Gallagher M.A. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis. 2002;61(1-2):32–39. [PubMed] [Google Scholar]
- 7.Renger R.J., Roukema G.R., Reurings J.C., Raams P.M., Font J., Verleisdonk E.J. The clavicle hook plate for Neer type II lateral clavicle fractures. J Orthop Trauma. 2009;23(8):570–574. doi: 10.1097/BOT.0b013e318193d878. [DOI] [PubMed] [Google Scholar]
- 8.Good D.W., Lui D.F., Leonard M., Morris S., McElwain J.P. Clavicle hook plate fixation for displaced lateral-third clavicle fractures (Neer type II): a functional outcome study. J Shoulder Elbow Surg. 2012;21(8):1045–1048. doi: 10.1016/j.jse.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 9.Choi S., Kim S.R., Kang H., Kim D., Park Y.G. Modified tension band fixation and coracoclavicular stabilisation for unstable distal clavicle fracture. Injury. 2015;46(2):259–264. doi: 10.1016/j.injury.2014.09.025. [DOI] [PubMed] [Google Scholar]
- 10.Erdle B., Izadpanah K., Jaeger M. Comparative analysis of locking plate versus hook plate osteosynthesis of Neer type IIB lateral clavicle fractures. Arch Orthop Trauma Surg. 2017;137(5):651–662. doi: 10.1007/s00402-017-2645-7. [DOI] [PubMed] [Google Scholar]
- 11.Ochen Y., Frima H., Houwert R.M. Surgical treatment of Neer type II and type V lateral clavicular fractures: comparison of hook plate versus superior plate with lateral extension: a retrospective cohort study. Eur J Orthop Surg Traumatol. 2019;29(5):989–997. doi: 10.1007/s00590-019-02411-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han L., Hu Y., Quan R., Fang W., Jin B., Huang L. Treatment of neer IIb distal clavicle fractures using anatomical locked plate fixation with coracoclavicular ligament augmentation. J Hand Surg Am. 2017;42(12) doi: 10.1016/j.jhsa.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Hohmann E., Hansen T., Tetsworth K. Treatment of Neer type II fractures of the lateral clavicle using distal radius locking plates combined with TightRope augmentation of the coraco-clavicular ligaments. Arch Orthop Trauma Surg. 2012;132(10):1415–1421. doi: 10.1007/s00402-012-1570-z. [DOI] [PubMed] [Google Scholar]
- 14.Kao F.C., Chao E.K., Chen C.H., Yu S.W., Chen C.Y., Yen C.Y. Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma. 2001;51(3):522–525. doi: 10.1097/00005373-200109000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Cho C.H., Jung J.H., Kim B.S. Coracoclavicular stabilization using a suture button device for Neer type IIB lateral clavicle fractures. J Shoulder Elbow Surg. 2017;26(5):804–808. doi: 10.1016/j.jse.2016.09.048. [DOI] [PubMed] [Google Scholar]
- 16.Hsu K.H., Tzeng Y.H., Chang M.C., Chiang C.C. Comparing the coracoclavicular loop technique with a hook plate for the treatment of distal clavicle fractures. J Shoulder Elbow Surg. 2018;27(2):224–230. doi: 10.1016/j.jse.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 17.Kraus N., Stein V., Gerhardt C., Scheibel M. Arthroscopically assisted stabilization of displaced lateral clavicle fractures with coracoclavicular instability. Arch Orthop Trauma Surg. 2015;135(9):1283–1290. doi: 10.1007/s00402-015-2271-1. [DOI] [PubMed] [Google Scholar]
- 18.Struhl S., Wolfson T.S. Closed-loop double endobutton technique for repair of unstable distal clavicle fractures. Orthop J Sports Med. 2016;4(7) doi: 10.1177/2325967116657810. Published 2016 Jul 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yagnik G.P., Jordan C.J., Narvel R.R., Hassan R.J., Porter D.A. Distal clavicle fracture repair: clinical outcomes of a surgical technique utilizing a combination of cortical button fixation and coracoclavicular ligament reconstruction. Orthop J Sports Med. 2019;7(9) doi: 10.1177/2325967119867920. Published 2019 Sep. 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amstutz H.C., Sew Hoy A.L., Clarke I.C. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981;155:7–20. [PubMed] [Google Scholar]
- 21.Singh A., Schultzel M., Fleming J.F., Navarro R.A. Complications after surgical treatment of distal clavicle fractures. Orthop Traumatol Surg Res. 2019;105(5):853–859. doi: 10.1016/j.otsr.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 22.Egol K.A., Koval K.J., Zuckerman J.D. Wolters Kluwer/Lippincott Williams & Wilkins Health; Philadelphia, PA: 2010. Handbook of Fractures. [Google Scholar]
- 23.Lopiz Y., Checa P., García-Fernández C., Valle J., Vega M.L., Marco F. Complications with the clavicle hook plate after fixation of Neer type II clavicle fractures. Int Orthop. 2019;43(7):1701–1708. doi: 10.1007/s00264-018-4108-3. [DOI] [PubMed] [Google Scholar]
- 24.Huang Y.C., Yang S.W., Chen C.Y., Lin K.C., Renn J.H. Single coracoclavicular suture fixation with Mersilene tape versus hook plate in the treatment of acute type V acromioclavicular dislocation: a retrospective analysis. J Orthop Surg Res. 2018;13(1):110. doi: 10.1186/s13018-018-0831-0. Published 2018 May 16. [DOI] [PMC free article] [PubMed] [Google Scholar]