Dear Editor,
Scoring systems are invaluable tools for research, quality assurance, and performance comparison in intensive care medicine. They allow for adjustment for underlying risk of unwanted outcomes, primarily mortality, and make comparisons between interventions, units, and systems possible. The Simplified Acute Physiology Score 3 (SAPS 3) is a well-validated scoring system used worldwide for the prediction of hospital mortality based on variables of acute physiologic derangements, current conditions and interventions, and previous health status [1, 2].
Coronavirus disease 2019 (COVID-19) put pressure on intensive care units (ICU), health care systems, nations, and societies worldwide. Measurement of health care performance is therefore more important than ever. Previous studies put the validity of other well-established intensive care scoring systems in COVID-19 cases in question [3], while others claimed good predictive capabilities [4]. Several outcome prognostication models for patient groups affected by COVID-19 have also been proposed. For these, a living systematic review and critical appraisal of the available literature finds C-index estimates for the prognostication of mortality to range from 0.68 to 0.98 [5]. In this study, we seek to evaluate the performance of SAPS 3 in the prediction of hospital mortality in COVID-19 patients admitted to ICUs.
Anonymous data from the Austrian Centre for Statistics and Documentation in Intensive Care (ASDI) database on patients with documented SARS-CoV-2 infection admitted to participating ICUs from January 1st, 2020, to January 31st, 2021, were retrieved and used for retrospective analyses. The anonymous fashion of the dataset precluded the need for ethical approval.
Discriminative performance of SAPS 3 for hospital mortality was evaluated by calculation of the area under the receiver operating curve (AUC) and 95% confidence intervals (95% CI) based on the DeLong approach [6]. Hosmer–Lemeshow test in deciles of observed-to-expected ratios (O/E ratios) and the calibration belt method [7] were used to assess goodness of fit of the formula to calculate predicted hospital mortality. Recalibration was conducted using the structure of the formula for regional customisations in ref. [2]; parameters were estimated by maximum likelihood method. Weights of individual SAPS 3 items remained unchanged. Analyses were conducted using R version 4.0.0 with packages pROC and givitiR.
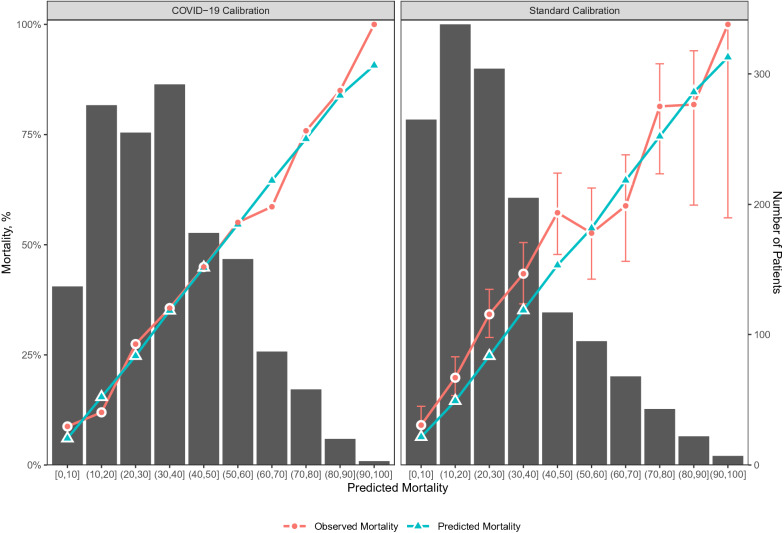
1464 patients with COVID-19 admitted to 90 participating ICUs were identified (electronic supplement Table 1). Of these, 501 (34%) died during their hospital stay. AUC for discrimination of hospital mortality was 0.745 (95% CI 0.719–0.770). Standard calibration [2] led to under-estimation of hospital mortality [O/E ratio (95% CI) 1.20 (1.12–1.27), Ĥ = 41.10 (p < 0.001), Ĉ = 40.92 (p < 0.001)], especially in lower risk groups (Fig. 1, electronic supplement Fig. 2). Dedicated calibration for COVID-19 using the formula Probability of death = elogit/(1 + elogit), where logit = − 14.451 + 3.666 * ln(SAPS3 + − 12.092) led to improved goodness of fit [Ĥ = 7.15 (p = 0.71), Ĉ = 5.01 (p = 0.89)]] (Fig. 1, electronic supplement Fig. 3).
Fig. 1.
Binned plots of hospital mortality predicted by SAPS 3 in deciles (x-axis), observed mortality (primary y-axis) for COVID-19 calibration (left) and standard calibration (right) [dot-and-line graphs, unadjusted confidence intervals], number of patients (secondary y-axis) [bar graphs]
We find the SAPS 3 to be of satisfactory performance in the prognostication of hospital mortality in patients with COVID-19 admitted to intensive care units. Use of a general prediction model such as the SAPS 3 allows for the evaluation of outcomes in patient cohort, units, and systems irrespective of the underlying disease and is, therefore, preferable. Recalibration of the SAPS 3 can be used to allow for more precise performance evaluation in COVID-19 cohorts.
Supplementary Information
Below is the link to the electronic supplementary material.
Declarations
Conflicts of interest
MP reports institutional grants from the Austrian Center for Documentation and Quality Assurance in Intensive Care Medicine. TF reports his employment at the Center for Medical Statistics, Informatics, and Intelligent Systems to be funded by the Austrian Center for Documentation and Quality Assurance in Intensive Care Medicine.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Metnitz PG, Moreno RP, Almeida E, Jordan B, Bauer P, Campos RA, Iapichino G, Edbrooke D, Capuzzo M, Le Gall JR, SAPS 3 Investigators SAPS 3–from evaluation of the patient to evaluation of the intensive care unit. Part 1: objectives, methods and cohort description. Intensive Care Med. 2005;31(10):1336–1344. doi: 10.1007/s00134-005-2762-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moreno RP, Metnitz PG, Almeida E, Jordan B, Bauer P, Campos RA, Iapichino G, Edbrooke D, Capuzzo M, Le Gall JR, SAPS 3 Investigators SAPS 3–from evaluation of the patient to evaluation of the intensive care unit. Part 2: development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med. 2005;31(10):1345–1355. doi: 10.1007/s00134-005-2763-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stephens JR, Stümpfle R, Patel P, Brett S, Broomhead R, Baharlo B, Soni S (2021) Analysis of Critical Care Severity of Illness Scoring Systems in Patients With Coronavirus Disease 2019: A Retrospective Analysis of Three U.K. ICUs. Crit Care Med 49(1): e105–e107. 10.1097/CCM.0000000000004674 [DOI] [PMC free article] [PubMed]
- 4.Zou X, Li S, Fang M, Hu M, Bian Y, Ling J, Yu S, Jing L, Li D, Huang J. Acute physiology and chronic health evaluation II score as a predictor of hospital mortality in patients of coronavirus disease 2019. Crit Care Med. 2020;48(8):e657–e665. doi: 10.1097/CCM.0000000000004411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wynants L, Van Calster B, Collins GS, Riley RD, Heinze G, et al. Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal. BMJ. 2020;369:m1328. doi: 10.1136/bmj.m1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. doi: 10.2307/2531595. [DOI] [PubMed] [Google Scholar]
- 7.Finazzi S, Poole D, Luciani D, Cogo PE, Bertolini G. Calibration belt for quality-of-care assessment based on dichotomous outcomes. PLoS ONE. 2011;6(2):e16110. doi: 10.1371/journal.pone.0016110. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.