Abstract
The malfeasant role of the hypoxic tumour microenvironment (TME) in cancer progression was recognized decades ago but the exact mechanisms that augment the hallmarks of cancer and promote treatment resistance continue to be elucidated. Gastroesophageal cancers (GOCs) represent a major burden of worldwide disease, responsible for the deaths of over 1 million people annually. Disentangling the impact of hypoxia in GOCs enables a better overall understanding of the disease pathogenesis while shining a light on novel therapeutic strategies and facilitating precision treatment approaches with the ultimate goal of improving outcomes for patients with these diseases. This review discusses the underlying principles and processes of the hypoxic response and the effect of hypoxia in promoting the hallmarks of cancer in the context of GOCs. We focus on its bidirectional influence on inflammation and how it drives angiogenesis, innate and adaptive immune evasion, metastasis, and the reprogramming of cellular bioenergetics. The contribution of the hypoxic GOC TME to treatment resistance is examined and a brief overview of the pharmacodynamics of hypoxia-targeted therapeutics is given. The principal methods that are used in measuring hypoxia and how they may enhance prognostication or provide rationale for individually tailored management in the case of tumours with significant hypoxic regions are also discussed.
Keywords: Esophageal cancer, Gastric cancer, Tumor hypoxia, Tumour microenvironment, Gastroesophageal cancer
Core Tip: Improved methods in measuring the oxygen status in the tumour microenvironment have allowed for a better understanding of the role of hypoxia and how it contributes to tumour progression and treatment resistance. These methods include non-invasive imaging techniques as well as validated hypoxic molecular signatures. Specific hypoxia-targeted therapies have not matched their expectations but may have potential application in combination with traditional treatment approaches in gastroesophageal cancer.
INTRODUCTION
One of the major turning points in the study of solid tumours arose with the realization that a critical regulatory influence in the process of angiogenesis was an environmental feature; hypoxia[1,2]. Many studies have since demonstrated the oncogenic transforming power of hypoxia in the microenvironment of different tumour types and the observation that tumour oxygenation status could disrupt the anti-tumour effects of radiation therapy was published over 60 years ago[3-8]. This review will discuss the role of hypoxia in the tumour microenvironment (TME) of gastroesophageal cancers (GOCs) including gastric cancer (GC) and oesophageal cancer (OC), how it augments disease, and additionally its relevance in the setting of prognostication and therapeutic targeting.
GOC is a substantial cause of morbidity and mortality, responsible for 1.2 million deaths per year globally[9-12]. An improved understanding of the risk factors for GC has seen a steady decline in both the incidence and mortality which is in sharp contrast to the rising incidence of OC, particularly oesophageal adenocarcinoma (OAC) globally[13,14]. GOCs develop insidiously and consequently, are commonly diagnosed at an advanced stage where chemotherapy with or without radiation remains the treatment of choice in the neoadjuvant setting[15]. Treatment at this stage is rarely curative and several mechanisms account for this resistance to treatment including tumour cell-intrinsic and extrinsic mechanisms. Hypoxia is a characteristic feature of the TME and a key mediator in conferring and enhancing treatment resistance[16-18]. The TME being the complex reciprocity between both the cellular (resident and infiltrating) and non-cellular components that surround, envelop, and make up the tumour mass, the components of which are summarized in Figure 1[19-21]. The exact mechanisms underlying resistance continue to be elucidated and as such, interest in the role of hypoxia in translational oncology research has garnered increasing interest recently as shown in Figure 2.
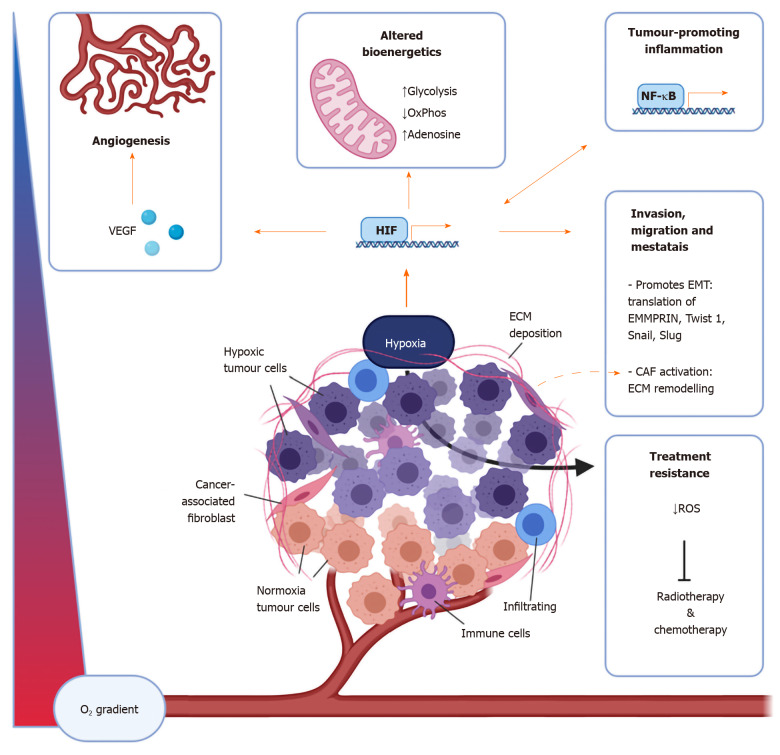
Figure 1.
The components of the tumour microenvironment are affected by hypoxia in numerous ways. Important cellular components of the tumour microenvironment include immune cells including macrophages, dendritic cells, myeloid-derived suppressor cells, T cells, natural killer cells, as well as cancer-associated fibroblasts. Non-cellular aspects include the extracellular matrix and signalling molecules such as vascular endothelial growth factor, adenosine, and cytokines and chemokines including interleukin-6, interferon-γ, CXCL1, CXCL3, CCL28[12-14,40]. CAF: Cancer associated fibroblasts; OxPhos: Oxidative phosphorylation; ROS: Reactive oxygen species; VEGF: Vascular endothelial growth factor; NFκB: Nuclear factor-kappa light chain enhancer of activated B cells; HIF: Hypoxia inducible factor; ECM: Extracellular matrix; EMT: Epithelial-mesenchymal transition.
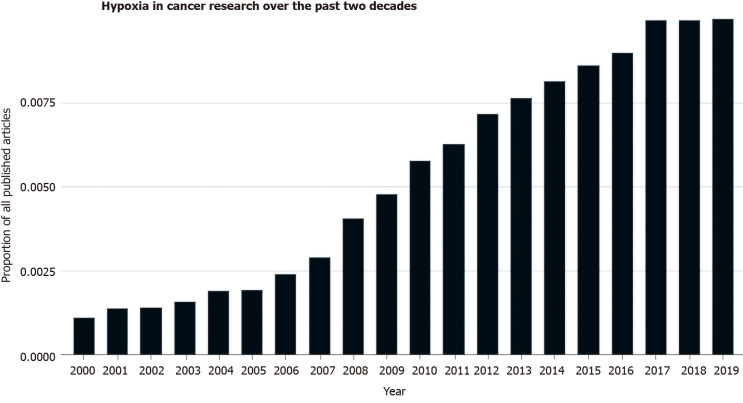
Figure 2.
The amount of research investigating the role of hypoxia in cancer has increased over the past 20 yr as seen as a proportion of PubMed listed articles[177].
Hypoxia mediates aggressive, metastatic, and treatment-resistant disease by augmenting the hallmarks of cancer through various cellular and physiological events including; enhanced tumour cell proliferation, survival, immune evasion, inflammation, induction of angiogenesis, and activation of invasion[16,17,22]. In large part these events are influenced or orchestrated by the relationship between oxygen availability and the genes encoding hypoxia-inducible factors (HIF) and von Hippel Lindau protein (pVHL)[23,24]. HIFs are a family of heterodimeric transcription factors consisting of a labile α subunit and a stable β subunit. There are several HIF isotypes but the most well-studied is HIF1. HIF1-α contains domains amenable to post-translational modifications thereby mediating interactions with the molecular machinery responsible for cellular degradation[25,26]. When induced, HIF1-α associates with the constitutively expressed HIF1-β subunit and together act to bring about the transcription of a multitude of genes involved in complex signalling pathways with a diverse degree of roles. There exists a whole host of HIF target genes that are transcribed in response to hypoxia that have been implicated in driving tumour progression. The roles of these target genes range from receptors to enzymes to further transcription factors and more (Table 1), which are involved in the enhancement of inflammation, angiogenesis, immune evasion, and the other remaining hallmarks of cancer.
Table 1.
Hypoxia induces the transcription of a range of genes that mediate diverse roles in promoting the hallmarks of cancer[178-180]
|
Function
|
Gene
|
| Enzymes | MMP1, MMP3, LOX, ADAMST1, ACE |
| Transcription factors | Twist1, Snail, Slug, β-Catenin, c-Myc, Oct4, NF-κB |
| Receptors | CXCR4, c-Met, TLR4, Notch |
| Growth factors | VEGF, TGFα |
| Transporters | Glut-1, MDR1 |
| Intracellular signalling | Cdc42, Rac1, RhoE |
| Bioenergetics | LDHA, PGK1, PKM2, GAPDH, GPI, ALDOC |
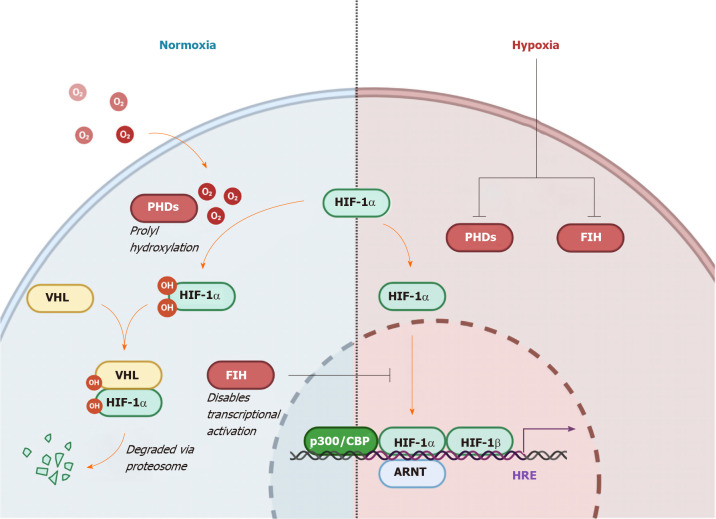
In the setting of normoxia, HIF1-α is regulated by two principal mechanisms; oxygen-dependent pVHL-dependent degradation, and oxygen-dependent non-pVHL-dependent inactivation (Figure 3)[25,27,28]. Hydroxylation by oxygen-dependent prolyl hydroxylase domain enzymes trigger recognition by the E3 ubiquitin ligase, pVHL, ensuring proteasomal degradation. In the non-pVHL dependent pathway, induction of factor inhibiting HIF leads to hydroxylation of an asparagine residue preventing HIF1-α from localizing with the co-activators p300 and CBP, hence disabling transcriptional activation[29].
Figure 3.
Regulation of hypoxia-inducible factor 1-α by oxygen levels and von Hippel Lindau protein. Hydroxylation by oxygen-dependent prolyl hydroxylase domain enzymes triggers recognition by the E3 ubiquitin ligase von Hippel Lindau, ensuring proteasomal degradation. In the non-von Hippel Lindau protein dependent pathway, induction of Factor Inhibiting hypoxia-inducible factor (HIF) leads to hydroxylation of an asparagine residue preventing HIF1-α from localizing with the co-activators p300 and CBP, hence disabling transcriptional activation[30]. The HIF pathway functions to conduct and orchestrate the cellular response to low oxygen availability[24,25]. HRE: Hypoxia response element; ARNT: Aryl hydrocarbon receptor nuclear translocator; PHD: Prolyl hydroxylase domain enzymes; VHL: Von Hippel Lindau; HIF1-α: Hypoxia-inducible factor 1-α; FIH: Factor inhibiting hypoxia-inducible factor.
The contribution of hypoxia to disease progression makes it an attractive therapeutic target and potential prognostic aide. However, in the setting of GOC, there are currently no agents specifically targeting hypoxia, nor are there any biomarkers that assess the extent of tumour hypoxia, to guide treatment choice or to indicate the likelihood of treatment response. In this era of precision medicine, a validated biomarker would improve the standard of care for this group of patients.
HYPOXIA PROMOTES THE HALLMARKS OF CANCER WITHIN THE TME
Inflammation
Cancer has long been described as a “wound that never heals”, in part due to inflammation, one of the enabling characteristics of cancer originally described by Hanahan and Weinberg[30-31]. Hypoxia and inflammation are intricately intertwined as illustrated through the fact that hypoxia has been shown to directly induce signalling via the inflammatory master transcription factor nuclear factor-kappa light chain enhancer of activated B cells (NF-κB), and likewise NF-κB induces HIFs[32-37]. In the context of malignancy, there exists a multitude of cancer implicated genes that are regulated by both HIFs and NF-κB, such as cyclooxygenase 2 and interleukin-6 (IL-6)[38]. This illustrates the complex crosstalk between signalling pathways and the difficulty involved in unravelling the net influence of certain factors in the network. In the setting of GOC, OAC has been described as “a model of inflammatory driven upper gastrointestinal cancer”[39,40]. The paramount importance of inflammation in the aetiology of OC is further validated by the risk reduction conferred by administration of the non-steroidal anti-inflammatory drugs such as aspirin, as demonstrated in a meta-analysis of 9 observational studies by Corley et al[41] and Farrow et al[42]. In a retrospective study of 53 patients with OAC and the metaplastic precursor lesion, Barrett’s oesophagus (BO), immunohistochemical staining of specimens revealed a significant increase in the expression of HIF1-α in OAC and BO compared to normal tissue but no further elevation between BO and OAC[43]. Furthermore, histological assessment of specimens’ inflammatory status, based on recruitment of neutrophils (reflecting acute inflammation) and monocytes (reflecting chronic inflammation) (known as the Sydney System), demonstrated a significant correlation with HIF1-α expression from normal tissue to metaplastic tissue but no association between other stages or between inflammatory status[43].
Angiogenesis
As previously mentioned, one of the defining discoveries involved in the study of the TME was the effect of hypoxia on angiogenesis[44-46]. This was originally demonstrated in HIF1-β deficient hepatoma cells having markedly reduced vascular endothelial growth factor (VEGF) mRNA levels when cultured under hypoxic conditions[24,47]. In the setting of GOC, a study of 92 oesophageal biopsy samples found a significant increase in the expression of HIF1-α in OAC vs dysplastic and metaplastic tissues but not between normal and metaplastic tissues[48]. These findings also reflected an increase in VEGF and HIF2-α expression in OAC vs dysplastic tissue. Several studies have revealed how hypoxia appears to drive tumour cell plasticity and hence vasculogenic mimicry, a process that allows malignant cells to impersonate endothelial cells and form a network of vessels, and in a sense bypass true angiogenic activity[49-54]. In an in vitro analysis of oral squamous cell carcinoma (OSCC) cells, transfection with siRNA targeting HIF1-α was shown to inhibit both vasculogenic mimicry (through three-dimensional culture) and proliferation (as measured by MTT assay)[55]. Validation of these results in a xenograft implant model was then performed; the HIF-1α knockout mice showed a longer time to tumour formation and had smaller tumours. In an experiment conducted by Chai et al[56] of 160 OSCC tumour tissues, both HIF1-α and the degree of vasculogenic mimicry correlated negatively with overall survival (OS). In a separate study, OSCC cell lines cultured under conditions of severe hypoxia (0.5% oxygen) for 5 d secreted exosomes which through tube formation assays, were shown to increase the angiogenic capacity of human umbilical vein endothelial cells when cultured together[57]. Vessel formation was significantly increased compared to umbilical vein endothelial cells cultured with exosomes obtained from OSCC cells exposed to normoxic conditions. When assessed in an in vivo implant model, findings reflected those found in the in vitro assay. As a consequence of these described phenomena, the blood vessels formed in tumours do not resemble those found in non-malignant tissues. The resulting network is disorganized and highly permeable and this limits the supply of blood and hence oxygen, nutrients, and anti-cancer drugs, further contributing to tumour hypoxia.
Immune evasion
The cancer-immune set point refers to the equilibrium between factors that promote or suppress the anti-cancer immune response[58]. This is of great interest in GOC given the yet unrealized efficacy that was predicted of immune checkpoint inhibitor drugs in treating these cancer types, which are generally characterized as having high tumour mutational burden and evident immune cell infiltration[59]. A hypoxic TME promotes an immunosuppressive phenotype through actions on the diverse array of cellular and non-cellular entities across innate and adaptive immune arms and thus constitutes a vital host factor that may be contributing to a high cancer-immune set point and treatment failure. For example, in the context of cancer, the recruitment of myeloid-derived suppressor cells (MDSCs) is associated with less favourable patient outcomes which are likely mediated by their potent dampening of the anti-tumour immune response[60-62].
MDSCs are defined as “a heterogenous population of cells of myeloid origin that consist of myeloid progenitors, immature macrophages, immature granulocytes, and immature dendritic cells” (DCs)[63,64]. In a murine model of OSCC, intratumoural MDSC percentages were shown to correlate with the tumour progression sequence[65]. The role of IL-6 was then explored in the context of MDSCs and tumour progression. In patients with OSCC compared to healthy controls, serum IL-6 was significantly increased. Also, the percentage of intratumoural MDSCs correlated with general serum IL-6 levels. Delving further into this, the murine model of OSCC was utilized with 3 cohorts; IL-6 knockout, IL-6 stimulation (via 100 ng intraperitoneal injection twice weekly for 6 wk), and normal wild type. The cohort receiving IL-6 had a significant 3-fold increase in the percentage of MDSCs compared to the IL-6 deficient cohort (15% to 5% respectively). These findings were analogous when examining tumour invasiveness. As mentioned previously, HIF has been shown to upregulate the transcription of inflammatory factors including IL-6, and overall, the results demonstrate the importance of hypoxia in driving the pro-tumour immunosuppressive functions of MDSCs[38,66]. Others have shown the hypoxic TME to drive MDSC differentiation to tumour associated macrophages (TAMs), again in a manner that is orchestrated by HIF1-α[67].
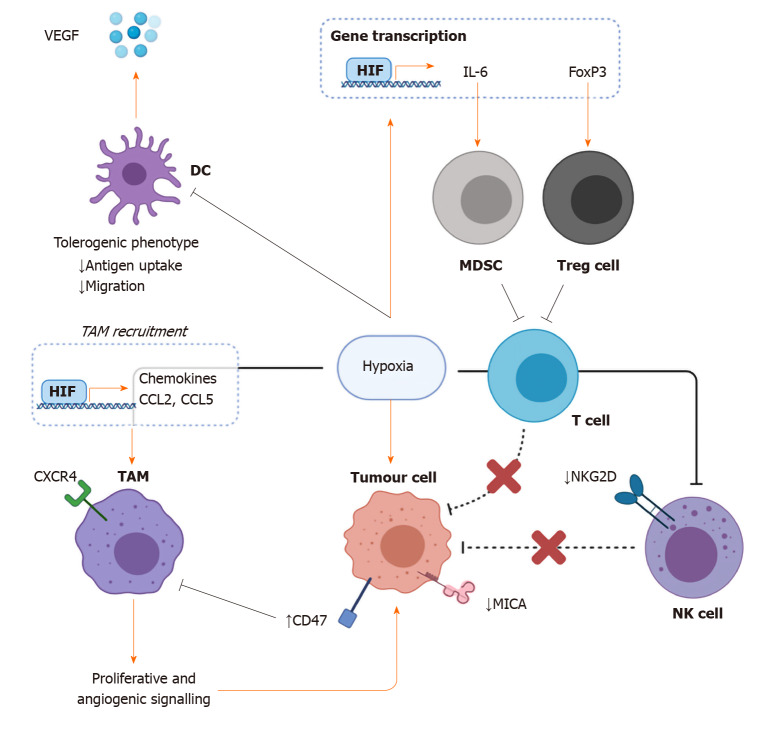
TAMs comprise a large part of the cellular TME and as such are gaining further infamy for their role in driving tumour progression[68,69]. Studies have demonstrated how TAM recruitment and infiltration into the TME is in part mediated by the hypoxic response and HIF-driven regulation of chemoattractant including CCL2, CCL5, and receptors such as CXCR4[70-73] (Figure 4). There is strong evidence that macrophage infiltration and density are associated with worse patient outcomes in the setting of malignancy[74-76]. A meta-analysis of 16 OC cancer studies (n = 2292), found that M2-polarised pro-tumour macrophage density to be predictive of worse OS and disease stage[77,78]. In addition, in vitro evidence suggests that TAM density is significantly associated with an increase in programmed death-ligand 1 expression on OSCC cells[78]. Once infiltrated into the TME, low oxygen tension enhances the oncogenic role of TAMs via the promotion of proliferative and angiogenic growth signalling pathways[79,80]. Notably, while two studies have characterized the correlation between HIF1-α expression, TAM infiltration, and patient survival in the setting of gastric malignancy, the impact of hypoxia on the biology of TAMs could be further expanded in the context of GOC[81,82].
Figure 4.
The effects of hypoxia on immune evasion. Hypoxia has been shown to impair antigen uptake and migration in dendritic cells while at the same time increasing vascular endothelial growth factor production thus impairing the bridge between the innate anticancer immune response and the adaptive response while also enhancing angiogenic signalling. Hypoxia-inducible factor-mediated transcription of the cytokine interleukin-6 and FoxP3 results in the subsequent recruitment of immunosuppressive myeloid derived suppressor cells and in increased proportion of protumourigenic Tregs respectively. Low oxygen status is also linked with decreased tumour expression of the natural killer (NK) cell receptor ligand MHC class I chain-related molecule A, as well as its receptor NKG2D on NK cells. Hypoxia-dependent transcription of chemokines such as CCL2 and CCL5 enhance the recruitment of tumour associated macrophages through receptors such as CXCR4. DC: Dendritic cell; MDSC: Myeloid derived suppressor cell; NK cell: Natural killer cell; TAM: Tumour associated macrophage; Treg cell: T regulatory cell; VEGF: Vascular endothelial growth factor; HIF: Hypoxia inducible factor; IL: Interleukin; MICA: MHC class I chain-related molecule A.
Signifying the potential of innate immune research in cancer, Gilead recently invested $4.8 billion for ownership of magrolimab[83], a monoclonal antibody that works through the disruption of CD47 which is expressed on cancer cells and acts to downregulate the anti-tumour phagocytic capability of macrophages. Targeting hypoxia-mediated CD47 function may also extend to cancers of the alimentary tract. Immunohistochemical staining and reverse transcription quantitative real-time polymerase chain reaction (RT-qPCR) of OSSC specimens taken from 14 patients demonstrated a significant increase in expression of CD47 while another preclinical study revealed an augmented response to immune checkpoint inhibition in combination with CD47 antagonism[84,85]. CD47 expression has also been shown to predict prognosis in OSCC[86].
Natural killer (NK) cells are a type of innate lymphoid cell that are capable of recognizing tumour cells through two principal mechanisms; altered expression of self or missing-self[87,88]. For example, in the absence of cellular stress, MHC class I chain-related molecules (MICA and MICB) are not normally expressed on cells. In one study of prostate cancer cells, culture under hypoxic conditions is shown to result in the shedding of MICA hence characterizing an immune evasive phenotype[89]. Hypoxia also affects both resting and activated NK cells directly by curtailing the expression of costimulatory NKG2D and other NK cell receptors (NKp46, NKp30) which enable NK cell function[90]. Furthermore, a low oxygen environment has revealed impaired NK cell differentiation in one in vitro study[91]. The density of infiltrating NK cells has been shown to be prognostic in OSCC[92]. In a study of OSCC xenografts implanted in nude mice, NK cell depletion was shown to restore tumour growth following treatment with an anti-PD-1 (programmed death-1) agent illustrating the important anti-tumour role of NK cells which is tightly regulated by the PD-1 pathway[93]. In human OC, NK cells that demonstrate high expression of a novel inhibitory regulator protein, T cell immunoglobulin domain and mucin domain 3 (Tim-3) are predisposed to apoptosis and hence fail to combat tumour progression[94]. Increased expression of Tim-3 in this context occurs through NF-κB signalling thus linking hypoxia to NK cell-mediated anti-tumour dysfunction. NK cells are also an important entity in GC. Tumour infiltrating NK cells expressing high levels of Tim-3 have been correlated with adverse prognosis in a study of 62 patients with the disease[95].
DCs present antigens to T cells including CD4+ T helper cells, resulting in the initiation of the adaptive anti-tumour immune response[96]. In cancer, impaired DC function is associated with defective anti-tumour immune responses and hence cancer progression[97-99]. While there are contrasting studies, the net effect of the hypoxic TME may be skewed towards a tolerogenic DC phenotype[100,101]. An in vitro study of peripheral blood mononuclear cells isolated from a healthy human cohort and cultured under hypoxic conditions (1% oxygen) showed that hypoxia impairs DC uptake of antigens and causes modulation of their cytokine expression patterns in both resting and activated states[100]. Hypoxia increased VEGF production and CXCR4 expression and lead to a reduction in DC production of tumor necrosis factor-α thereby revealing the pro-angiogenic and immunosuppressive effect of reduced oxygen tension on DCs. Lysosomal-associated membrane protein (LAMP3) is a marker of mature DCs and it has been shown to be induced by hypoxia in breast cancer both in vitro and in vivo[102]. It is thought to be implicated in metastasis[103]. RT-qPCR analysis of 157 OSCC tissues as well as immunohistochemical staining of 46 specimens reveal its expression to be correlated with poor patient outcomes, further emphasizing the tolerogenic capacity of DCs[104]. Again, in the context of OAC, co-culture with DCs has been shown to induce Treg (T regulatory) differentiation supporting the tolerogenic DC phenotype in these malignancies[105]. Given that successful activation of adaptive T cell responses is dependent on DC migration to peripheral lymphoid organs, further research and investigation of the effect of hypoxia in the TME on DCs is required to fully dissect the potential clinical impact regarding patient outcomes and treatment resistance[106].
Hypoxia-induced HIF1-α expression is also associated with the upregulation of the transcription factor Forkhead Box Protein P3 (FoxP3), highlighting the role of hypoxia in regulating the abundance and function of Treg cells, further illustrating the potential immunosuppressive effect of a hypoxic TME on anti-tumour immunity[107,108]. In a study of GC, the frequency of Treg cells was significantly higher in the tumour compared with peripheral circulation wherein, intratumoural levels of FoxP3 correlated with TNM stage[109]. In a complementary study, elevated Treg/CD8+ cell ratio was shown to be an independent predictor for worse OS in a study of 133 patients with GC. Tregs are also crucially important in OC; one study found an increased percentage of peripheral Treg cells in OC patients vs healthy controls and they further demonstrated that a higher proportion of Tregs was inversely correlated to survival[110]. The administration of an agent that disrupts Treg recruitment to a hypoxic TME may represent a potential therapeutic target capable of improving outcomes[111].
Invasion, migration, and metastasis
The activation of cancer-associated fibroblasts (CAFs) in hypoxic TMEs has been implicated in the altered deposition, remodelling and degradation of the extracellular matrix (ECM) and hence invasion, migration, and metastasis[112-114]. In a study of 183 patients with OAC, characteristic expression of CAF marker α-SMA was found to be correlated with worse OS[115]. It was initially hypothesized that increased collagen production and fibrosis would present an obstacle to tumour cell invasion and metastasis, but evidence suggests that this is a lot more complex. In one study of pancreatic carcinoma cells, collagen has been shown to increase expression of the key epithelial to mesenchymal transition (EMT) transcription factor Snail in a transforming growth factor-β-mediated manner[116]. Thus, this series of events is thought to be involved in the activation of CAFs thereby, ensuring enhanced migratory capacity, invasiveness, survival, and ECM deposition in a positive feedback loop[117,118]. In the area of GOC, an in vitro assay revealed extracellular matrix metalloproteinase inducer (EMMPRIN) promoted EMT and hence invasion and migration of an OC cell line[119]. The authors followed up this study by showing, through HIF1-α interference and culture under hypoxic (1% oxygen) conditions, that EMMPRIN was regulated by HIF1-α. Further research probing the relationship between traditionally neglected components of the TME like CAFs and hypoxia in upper gastrointestinal cancers is required.
Altered energetics
Cells deprived of oxygen promote tumour proliferation and survival through reprogramming of energy metabolism[30]. The observation that neoplastic cells shift their metabolism from aerobic to anaerobic respiration was first observed nearly 100 years ago by Otto Warburg[120,121]. This shift is orchestrated by the hypoxia master regulator HIF which upregulates enzymes involved in glycolysis such as pyruvate dehydrogenase kinase 1, and ultimately the production of lactate from pyruvate[122,123]. Immunoblot analysis of both gastric and OSCC specimens has demonstrated reductions in the expression of the β catalytic subunit of a key protein involved in oxidative phosphorylation, ATP synthase, further implicating the role of metabolic reprogramming in upper gastrointestinal malignancies[124]. It is also probable that an altered bioenergetic phenotype contributes to treatment resistance in a hypoxia-driven manner. In one study, the expression of 4 proteins involved in metabolic respiration in the setting of OAC (n = 23), were assessed prior to chemoradiation[125]. Increased levels of the oxidative phosphorylation protein ATP5B were significantly increased in those with poor response to chemoradiation as defined per tumour regression grade. This suggests that tumours that retain some sense of metabolic plasticity may predict treatment-refractory disease.
Lactate dehydrogenase is responsible for converting pyruvate to lactate under hypoxic conditions[126]. In a study of 152 patients with GC, immunohistochemical staining for lactate dehydrogenase (LDH) isoenzyme 5 demonstrated significant associations between immunoreactivity and a number of different tumour features such as tumour size, venous and lymphatic invasion, and tumour stage[127]. Inoculation of mice with LDH knock-out pancreatic cancer cells has been shown to result in reduced tumour size[128]. Furthermore, the quantity of MDSCs isolated from the LDH knock-out cancer mice both in tumour and spleen was significantly less in controls, and they demonstrated lower suppressive activity.
The effects of these processes are not restricted to neoplastic cells, as the evidence implicates hypoxia-driven metabolic shifts in other cellular components of the TME, particularly immune cells. Tissue hypoxia in cancerous or non-cancerous cells results in the build-up of the purine adenosine, extracellularly which augments a plethora of the hallmarks of cancer[129-134]. Evidence suggests this is conferred predominantly through the release and metabolism of ATP by the surface membrane nucleotidases CD39 and CD73[133,135,136]. In one in vitro experiment, an epithelial cell line demonstrated increased CD73 expression when exposed to hypoxic conditions, and examination of the CD73 gene has identified a binding site for HIF1[137]. Subsequent binding to purinergic receptors and adenosinergic signalling is known to mediate an anti-tumour immunosuppressive phenotype through effects on Tregs, MDSCs, TAMs, and B lymphocytes across various solid tumours types including OC[135,138-141]. In the context of GOC, a gene expression study of several radiotherapy resistant OC cell lines, CD73 expression was shown to be increased in TE-2, TE-13, and KYSE170 when compared to parent cell lines[142]. Once again, given the hypoxia-driven mechanism, this highlights the pro-inflammatory, tumour-promoting effect of the adenosine axis, thereby signifying another potential method of clinically targeting hypoxia pathways in the treatment of GOC.
Also, hypoxia (oxygen of 1.5%) driven reprogramming of energetic metabolism is linked to PD-1 immune checkpoint blockade resistance[143]. In vivo treatment with metformin, decreases OCR in tumour cells, while increasing consumption in T cells resulting in reduced hypoxia. The authors further examined the effect of anti-PD-1 agents in concert with metformin administration in vivo in a melanoma tumour type that traditionally fails to respond to immune checkpoint blockade. The synergistic effect demonstrated substantially increased tumour elimination[143]. These intricately woven hypoxia-mediated effects exist in concert with one another to contribute to an aggressive phenotype characterized by treatment resistance and poor prognosis.
MEASURING HYPOXIA
Measuring tissue and tumour hypoxia is challenging. There are four principal methods for measuring oxygen levels in vivo; the Eppendorf oxygen electrode, exogenous markers, endogenous markers, and imaging techniques. The Eppendorf electrode quickly became the gold standard for measuring oxygen tension when it was introduced at the beginning of the millennium after studies confirmed that low tumour oxygenation status was associated with worse outcomes in cervical as well as head and neck cancer[144,145]. However, it fell out of favour just as quickly for a variety of reasons. It was notably limited to tumours that were accessible and it was steadfastly invasive. It was additionally prone to sampling error[146]. Although hypoxia can be arbitrarily classified as acute/perfusion limited or chronic/diffusion-limited, there remains significant spatiotemporal variation in tumour oxygen tension and hence multiple sampling observations must be taken[147]. The literature on the use of endogenous hypoxia markers in GOC is extensive and is discussed in the context of prognosis and treatment and resistance[148-152]. Exogenous markers such as pimonidazole are administered to a patient and undergo chemical modification in hypoxic cells and are then amenable to visualization in specimens. A summary of the major methods used to measure tumour hypoxia and their associated advantages and disadvantages can be found in Table 2.
Table 2.
Techniques used in the measurement of tissue oxygenation and their associated advantages and disadvantages[10,181-183]
|
Technique
|
Advantages
|
Disadvantages
|
| Needle Electrodes | Instrumental in establishing the link between hypoxia and treatment failure | Prone to sampling error due to poor spatial resolution |
| Real time direct measurement | Invasive and requires direct access to tumours | |
| Exogenous Markers | More sensitive than electrodes at lower oxygen levels | Requires biopsy and immunohistochemistry |
| Reproducible | ||
| Precise spatial resolution | ||
| Endogenous Markers | Precise spatial resolution | Requires biopsy and immunohistochemistry |
| Can be serological such as Osteopontin | ||
| Can be tissue based such as HIFs or carbonic anhydrase IX | ||
| Radiological | Non-invasive | Expensive |
| Reproducible | Radiation exposure | |
| Precise spatial resolution | Relatively less well established |
HIF: Hypoxia inducible factor.
In the last decade, several studies have characterized gene expression signatures corresponding to oxygenation status[153-155]. Using a 15 gene expression panel derived from these studies, Ye et al[156] classified 24 cancer types from The Cancer Genome Atlas into a hypoxia score of high, low, and intermediate after adjusting for confounding factors such as sex and ethnicity. They were further able to validate this categorization with independent proteomic data where hypoxic status was known. 135/193 (70%) of GC samples had high hypoxic status while only 34/124 (27%) of OC samples fell into this category. There may be differences between OSCC and OAC but they were grouped together in this study. They further built on these findings by comparing molecular characteristics such as miRNA expression, highly mutated genes, and significant copy number alterations between the hypoxia score high and low tumours. In both OC and GC samples that had molecular signatures of high hypoxic status, a number of miRNAs that target the tumour suppressor gene tumour protein p53 inducible nuclear protein 1 (TP53INP1), were significantly downregulated[156].
TREATMENT RESISTANCE AND PROGNOSIS
Ionizing radiation generates free radicals from molecules of oxygen which then induce double-stranded DNA breaks resulting in mitotic catastrophe. This is one of the key mechanisms for radiation-induced tumour cell death and it is reliant on the presence of oxygen within the TME[144,157]. GC and OC cells cultured in vitro under hypoxic conditions (1% oxygen) were more resistant to radiation-induced cell death compared to GC and OC cells cultured under normoxic conditions, as assessed by colony formation assay[158]. The contribution of hypoxia to radiotherapy treatment resistance is relatively well established but its role in conventional chemotherapy and molecularly targeted therapy is less clear cut, particularly in GOC. Functional inactivation of HIF1-α in GC cell lines demonstrated increased susceptibility to 5-fluorouracil and cisplatin as determined by proliferation and apoptosis assays which lends support to the use of HIF1-α in predicting response to therapy[159]. Analysis of cell cycle distribution patterns following treatment with 5-fluorouracil revealed a greater proportion of senescent HIF1-α deficient cells compared with controls. Likewise, the apoptotic cell fraction as determined by caspase 3 cleavage of HIF1-α deficient cells was greatly increased. The mechanism for this is thought to be mediated by HIF1-α dependent suppression of P53 induction in response to 5-fluorouacil[159,160]. Another potential mechanism is suggested by a different study, using RT-PCR and Western blot to demonstrate the HIF1-α dependent upregulation of p-glycoprotein in GC cells incubated at 1% oxygen levels[161]. P-glycoprotein is a transporter protein that augments the efflux of drugs from cells and hence is associated with chemoresistance in GOC[162,163].
There are a large number of studies that have investigated the prognostic value of hypoxia in OC. A systematic review carried out by Peerlings et al[152] evaluated 22 studies assessing various hypoxia-related markers and established that increased expression of HIF1-α in early-stage OSCC was associated with increased resistance to chemoradiotherapy treatment. They also conclude that radiologically, the positron emission tomography (PET) marker 18F-FETNIM was significantly predictive for response to combined chemoradiation in the setting of OSCC[164]. In brief, these tracers work by diffusing into cells non-specifically. In the absence of oxygen, they undergo a chemical reaction and their resultant physicochemical properties do not allow diffusion out of the cell[165]. PET with 18F-FAZA (18F-fluoroazomycin arabinoside) has been shown to predict radiotherapy response in OAC murine xenografts[166]. Validation of the tracer 18F-HX4 has been performed in OC but is yet to be studied as a potential prognostic factor[167]. Overall, imaging of hypoxia continues to be an attractive approach for studying the TME and subsequent patient outcomes.
The markers assessed in the systematic review by Peerlings et al[152] included HIF1-α, VEGF, carbonic anhydrase IX, GLUT1, Beclin-2, HIF2-α, as well as PET. The most common method used to assess these markers was immunohistochemical staining of surgical or biopsied specimens i.e. an invasive technique. The authors indicate that HIF1-α overexpression was associated with worse outcomes for OS and disease-free survival in OSCC but the evidence for its association in OAC was inconclusive, mainly due to the absence of data. VEGF expression correlated with patient outcomes in OSCC but not OAC[152]. In contrast, carbonic anhydrase IX appears to be an independent predictor of survival in OAC. Carbonic anhydrase IX is a glycoprotein expressed on the cell surface and its primary function is the catalytic conversion of carbon dioxide to bicarbonate and protons[150,168]. Under the transcriptional control of HIF1-α, the metalloenzyme is thought to contribute to tumour growth and proliferation through the regulation of pH, ECM degradation, and EMT[168,169]. In the majority of studies assessing endogenous markers, the determination of what constituted “hypoxic” was based on relatively arbitrary thresholds of immunohistochemical expression, with very little in the way of standardized protocols across studies. For example, Munipalle et al[151] defined “high” HIF-1α expression as greater than 10% of OSCC cells showing positive staining. Birner et al[170] devised a score based on intensity and percentage of cells showing positive expression in a cohort of 333 OCs. Anything above the median was then considered a "high" expression while those below were considered a "low" expression.
In a more recent systematic review and meta-analysis, Luo et al[148] examined the clinical predictive value of HIF2-α. It included 40 studies with 4345 cancer cases but only 2 of these studies assessed upper gastrointestinal cancers. Of these 2 studies, 1 was solely GC (n = 127), while the other was both GC and OC (n = 177)[149,171]. Based on the Newcastle Ottawa score, the authors determined that both of these papers were of high quality. Both of these studies demonstrated a statistically significant association between HIF2-α and OS on univariate analysis but not multivariate. In the pooled analysis, the authors conclude that high HIF2-α expression was associated with a lower OS.
While there is a non-insignificant aggregate of clinical evidence denoting a statistically significant association between endogenous markers of tumour oxygenation and clinical outcomes, the heterogeneity in study methods and contrasting results ultimately indicates a need for more prospective research with greater adherence to the standardization of reporting. The REMARK recommendations for tumour marker prognostic studies published by the Equator Network lay out a checklist for researchers to improve both quality and transparency in research[172]. The wealth of data as discussed above, demonstrating the correlation between outcomes or treatment resistance and tumour hypoxia further illustrates the importance of the development and clinical implementation of new techniques in measuring tumour hypoxia such as non-invasive imaging[148,149,151,170,171].
HYPOXIA-TARGETED THERAPIES
Hypoxic areas of the TME inherently suffer from poor perfusion and disorganized vasculature and this has been one of the primary limitations to systemically administered therapeutics[173]. Nevertheless, a number of agents have been tested in clinical studies. Hypoxia-targeted therapies mainly consist of bioreductive prodrugs (hypoxia-activated prodrugs) but molecularly targeted agents that inhibit effectors in hypoxia-responsive pathways such as HIF1-α target genes or receptor tyrosine kinases like the VEGF receptor could be grouped here as well[173].
Bioreductive agents such as tirapazamine work in a similar manner to exogenous markers of hypoxia; they undergo chemical modification in hypoxic cells resulting in hypoxia-selective cytotoxicity. The bioreductive alkylating agent apaziquone demonstrated efficacy as a first-line agent in early clinical studies of bladder cancer but in a phase II study in 20 patients with GC, there was no clinical benefit[174,175]. In a preclinical murine model of OSCC and OAC, administration of the bioreductive prodrug evofosfamide was shown to delay tumour growth in combination with radiotherapy vs radiotherapy alone[176]. This came with the added benefit of no additional toxicity. As of the time of writing, there have been no clinical trials investigating the potential use of evofosfamide or other bioreductive prodrugs in OC and although the efficacy of these agents has largely been disappointing as first-line treatment in other cancer types, they may potentially improve sensitivity when used in combination with conventional chemoradiation.
CONCLUSION
The myriad of components that comprise the TME and the effects imposed on them by oxygen deprivation ensures that researchers have yet to scratch the surface in disentangling the key processes amenable to overcoming treatment-refractory disease and prognostication. Hypoxia plays a role in promoting immunosuppressive cells and subverting anti-tumour immune responses within the TME. Hypoxia also promotes the additional hallmarks of cancer including inflammation, angiogenesis, and reprogramming of metabolism. The intricate nature of these hypoxia-mediated effects is very complex and further research is required to elucidate the mechanisms as they pertain to GOC. Standardization of methodology in hypoxia focused basic research and clinical reporting would be conducive to driving this area forward. This deeper understanding will hopefully reveal novel therapeutic targets to control disease progression in GOC but currently, this remains out of reach. However, hypoxia as a clinical marker to stratify patients into certain treatment pathways or aid prognosis is something that is firmly within our grasp.
Footnotes
Conflict-of-interest statement: The authors report no known conflict of interests.
Manuscript source: Invited manuscript
Peer-review started: December 27, 2020
First decision: February 14, 2021
Article in press: April 14, 2021
Specialty type: Oncology
Country/Territory of origin: Ireland
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang ZK S-Editor: Gao CC L-Editor: A P-Editor: Ma YJ
Contributor Information
Ross King, Department of Surgery, St. James’s Hospital Campus, Trinity Translational Medicine Institute, Dublin D8, Ireland.
Conall Hayes, Department of Surgery, St. James’s Hospital Campus, Trinity Translational Medicine Institute, Dublin D8, Ireland.
Claire L Donohoe, Department of Surgery, St. James’s Hospital Campus, Trinity Translational Medicine Institute, Dublin D8, Ireland.
Margaret R Dunne, Department of Surgery, St. James’s Hospital Campus, Trinity Translational Medicine Institute, Dublin D8, Ireland.
Maria Davern, Department of Surgery, St. James’s Hospital Campus, Trinity Translational Medicine Institute, Dublin D8, Ireland.
Noel E Donlon, Department of Surgery, St. James’s Hospital Campus, Trinity Translational Medicine Institute, Dublin D8, Ireland. donlonn@tcd.ie.
References
- 1.Shweiki D, Itin A, Soffer D, Keshet E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature. 1992;359:843–845. doi: 10.1038/359843a0. [DOI] [PubMed] [Google Scholar]
- 2.Mazure NM, Chen EY, Yeh P, Laderoute KR, Giaccia AJ. Oncogenic transformation and hypoxia synergistically act to modulate vascular endothelial growth factor expression. Cancer Res. 1996;56:3436–3440. [PubMed] [Google Scholar]
- 3.Rofstad EK, Rasmussen H, Galappathi K, Mathiesen B, Nilsen K, Graff BA. Hypoxia promotes lymph node metastasis in human melanoma xenografts by up-regulating the urokinase-type plasminogen activator receptor. Cancer Res. 2002;62:1847–1853. [PubMed] [Google Scholar]
- 4.Bedogni B, Welford SM, Cassarino DS, Nickoloff BJ, Giaccia AJ, Powell MB. The hypoxic microenvironment of the skin contributes to Akt-mediated melanocyte transformation. Cancer Cell. 2005;8:443–454. doi: 10.1016/j.ccr.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Semenza GL. HIF-1 mediates metabolic responses to intratumoral hypoxia and oncogenic mutations. J Clin Invest. 2013;123:3664–3671. doi: 10.1172/JCI67230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomlinson RH, Gray LH. The histological structure of some human lung cancers and the possible implications for radiotherapy. Br J Cancer. 1955;9:539–549. doi: 10.1038/bjc.1955.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gray LH, Conger AD, Ebert M, Hornsey S, Scott OC. The concentration of oxygen dissolved in tissues at the time of irradiation as a factor in radiotherapy. Br J Radiol. 1953;26:638–648. doi: 10.1259/0007-1285-26-312-638. [DOI] [PubMed] [Google Scholar]
- 8.Kolstad P. Intercapillary distance, oxygen tension and local recurrence in cervix cancer. Scand J Clin Lab Invest Suppl. 1968;106:145–157. [PubMed] [Google Scholar]
- 9.Rubenstein JH, Shaheen NJ. Epidemiology, Diagnosis, and Management of Esophageal Adenocarcinoma. Gastroenterology 2015; 149: 302-17. :e1. doi: 10.1053/j.gastro.2015.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut. 2015;64:381–387. doi: 10.1136/gutjnl-2014-308124. [DOI] [PubMed] [Google Scholar]
- 11.Torre LA, Siegel RL, Ward EM, Jemal A. Global Cancer Incidence and Mortality Rates and Trends--An Update. Cancer Epidemiol Biomarkers Prev. 2016;25:16–27. doi: 10.1158/1055-9965.EPI-15-0578. [DOI] [PubMed] [Google Scholar]
- 12.Sitarz R, Skierucha M, Mielko J, Offerhaus GJA, Maciejewski R, Polkowski WP. Gastric cancer: epidemiology, prevention, classification, and treatment. Cancer Manag Res. 2018;10:239–248. doi: 10.2147/CMAR.S149619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bosetti C, Bertuccio P, Malvezzi M, Levi F, Chatenoud L, Negri E, La Vecchia C. Cancer mortality in Europe, 2005-2009, and an overview of trends since 1980. Ann Oncol. 2013;24:2657–2671. doi: 10.1093/annonc/mdt301. [DOI] [PubMed] [Google Scholar]
- 14.Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomarkers Prev. 2014;23:700–713. doi: 10.1158/1055-9965.EPI-13-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rice TW, Blackstone EH, Rusch VW. 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol. 2010;17:1721–1724. doi: 10.1245/s10434-010-1024-1. [DOI] [PubMed] [Google Scholar]
- 16.Ruan K, Song G, Ouyang G. Role of hypoxia in the hallmarks of human cancer. J Cell Biochem. 2009;107:1053–1062. doi: 10.1002/jcb.22214. [DOI] [PubMed] [Google Scholar]
- 17.Muz B, de la Puente P, Azab F, Azab AK. The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Hypoxia (Auckl) 2015;3:83–92. doi: 10.2147/HP.S93413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vaupel P, Mayer A. Hypoxia in cancer: significance and impact on clinical outcome. Cancer Metastasis Rev. 2007;26:225–239. doi: 10.1007/s10555-007-9055-1. [DOI] [PubMed] [Google Scholar]
- 19.Wang M, Zhao J, Zhang L, Wei F, Lian Y, Wu Y, Gong Z, Zhang S, Zhou J, Cao K, Li X, Xiong W, Li G, Zeng Z, Guo C. Role of tumor microenvironment in tumorigenesis. J Cancer. 2017;8:761–773. doi: 10.7150/jca.17648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen F, Zhuang X, Lin L, Yu P, Wang Y, Shi Y, Hu G, Sun Y. New horizons in tumor microenvironment biology: challenges and opportunities. BMC Med. 2015;13:45. doi: 10.1186/s12916-015-0278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Belli C, Trapani D, Viale G, D'Amico P, Duso BA, Della Vigna P, Orsi F, Curigliano G. Targeting the microenvironment in solid tumors. Cancer Treat Rev. 2018;65:22–32. doi: 10.1016/j.ctrv.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Gillies RJ, Gatenby RA. Hypoxia and adaptive landscapes in the evolution of carcinogenesis. Cancer Metastasis Rev. 2007;26:311–317. doi: 10.1007/s10555-007-9065-z. [DOI] [PubMed] [Google Scholar]
- 23.Wang GL, Jiang BH, Rue EA, Semenza GL. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci USA. 1995;92:5510–5514. doi: 10.1073/pnas.92.12.5510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Forsythe JA, Jiang BH, Iyer NV, Agani F, Leung SW, Koos RD, Semenza GL. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol Cell Biol. 1996;16:4604–4613. doi: 10.1128/mcb.16.9.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Semenza GL. HIF-1: upstream and downstream of cancer metabolism. Curr Opin Genet Dev. 2010;20:51–56. doi: 10.1016/j.gde.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaelin WG Jr, Ratcliffe PJ. Oxygen sensing by metazoans: the central role of the HIF hydroxylase pathway. Mol Cell. 2008;30:393–402. doi: 10.1016/j.molcel.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 27.Jaakkola P, Mole DR, Tian YM, Wilson MI, Gielbert J, Gaskell SJ, von Kriegsheim A, Hebestreit HF, Mukherji M, Schofield CJ, Maxwell PH, Pugh CW, Ratcliffe PJ. Targeting of HIF-alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001;292:468–472. doi: 10.1126/science.1059796. [DOI] [PubMed] [Google Scholar]
- 28.Majmundar AJ, Wong WJ, Simon MC. Hypoxia-inducible factors and the response to hypoxic stress. Mol Cell. 2010;40:294–309. doi: 10.1016/j.molcel.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Masoud GN, Li W. HIF-1α pathway: role, regulation and intervention for cancer therapy. Acta Pharm Sin B. 2015;5:378–389. doi: 10.1016/j.apsb.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 31.Dvorak HF. Tumors: wounds that do not heal-redux. Cancer Immunol Res. 2015;3:1–11. doi: 10.1158/2326-6066.CIR-14-0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koong AC, Chen EY, Giaccia AJ. Hypoxia causes the activation of nuclear factor kappa B through the phosphorylation of I kappa B alpha on tyrosine residues. Cancer Res. 1994;54:1425–1430. [PubMed] [Google Scholar]
- 33.Culver C, Sundqvist A, Mudie S, Melvin A, Xirodimas D, Rocha S. Mechanism of hypoxia-induced NF-kappaB. Mol Cell Biol. 2010;30:4901–4921. doi: 10.1128/MCB.00409-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Uden P, Kenneth NS, Rocha S. Regulation of hypoxia-inducible factor-1alpha by NF-kappaB. Biochem J. 2008;412:477–484. doi: 10.1042/BJ20080476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Uden P, Kenneth NS, Webster R, Müller HA, Mudie S, Rocha S. Evolutionary conserved regulation of HIF-1β by NF-κB. PLoS Genet. 2011;7:e1001285. doi: 10.1371/journal.pgen.1001285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eltzschig HK, Carmeliet P. Hypoxia and inflammation. N Engl J Med. 2011;364:656–665. doi: 10.1056/NEJMra0910283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bartels K, Grenz A, Eltzschig HK. Hypoxia and inflammation are two sides of the same coin. Proc Natl Acad Sci USA. 2013;110:18351–18352. doi: 10.1073/pnas.1318345110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Balamurugan K. HIF-1 at the crossroads of hypoxia, inflammation, and cancer. Int J Cancer. 2016;138:1058–1066. doi: 10.1002/ijc.29519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Picardo SL, Maher SG, O'Sullivan JN, Reynolds JV. Barrett's to oesophageal cancer sequence: a model of inflammatory-driven upper gastrointestinal cancer. Dig Surg. 2012;29:251–260. doi: 10.1159/000341498. [DOI] [PubMed] [Google Scholar]
- 40.O'Sullivan KE, Phelan JJ, O'Hanlon C, Lysaght J, O'Sullivan JN, Reynolds JV. The role of inflammation in cancer of the esophagus. Expert Rev Gastroenterol Hepatol. 2014;8:749–760. doi: 10.1586/17474124.2014.913478. [DOI] [PubMed] [Google Scholar]
- 41.Corley DA, Kerlikowske K, Verma R, Buffler P. Protective association of aspirin/NSAIDs and esophageal cancer: a systematic review and meta-analysis. Gastroenterology. 2003;124:47–56. doi: 10.1053/gast.2003.50008. [DOI] [PubMed] [Google Scholar]
- 42.Farrow DC, Vaughan TL, Hansten PD, Stanford JL, Risch HA, Gammon MD, Chow WH, Dubrow R, Ahsan H, Mayne ST, Schoenberg JB, West AB, Rotterdam H, Fraumeni JF Jr, Blot WJ. Use of aspirin and other nonsteroidal anti-inflammatory drugs and risk of esophageal and gastric cancer. Cancer Epidemiol Biomarkers Prev. 1998;7:97–102. [PubMed] [Google Scholar]
- 43.Ling FC, Khochfar J, Baldus SE, Brabender J, Drebber U, Bollschweiler E, Hoelscher AH, Schneider PM. HIF-1alpha protein expression is associated with the environmental inflammatory reaction in Barrett's metaplasia. Dis Esophagus. 2009;22:694–699. doi: 10.1111/j.1442-2050.2009.00957.x. [DOI] [PubMed] [Google Scholar]
- 44.Witz IP. The tumor microenvironment: the making of a paradigm. Cancer Microenviron. 2009;2 Suppl 1:9–17. doi: 10.1007/s12307-009-0025-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Otrock ZK, Hatoum HA, Awada AH, Ishak RS, Shamseddine AI. Hypoxia-inducible factor in cancer angiogenesis: structure, regulation and clinical perspectives. Crit Rev Oncol Hematol. 2009;70:93–102. doi: 10.1016/j.critrevonc.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 46.Liao D, Johnson RS. Hypoxia: a key regulator of angiogenesis in cancer. Cancer Metastasis Rev. 2007;26:281–290. doi: 10.1007/s10555-007-9066-y. [DOI] [PubMed] [Google Scholar]
- 47.Wood SM, Gleadle JM, Pugh CW, Hankinson O, Ratcliffe PJ. The role of the aryl hydrocarbon receptor nuclear translocator (ARNT) in hypoxic induction of gene expression. Studies in ARNT-deficient cells. J Biol Chem. 1996;271:15117–15123. doi: 10.1074/jbc.271.25.15117. [DOI] [PubMed] [Google Scholar]
- 48.Griffiths EA, Pritchard SA, McGrath SM, Valentine HR, Price PM, Welch IM, West CM. Increasing expression of hypoxia-inducible proteins in the Barrett's metaplasia-dysplasia-adenocarcinoma sequence. Br J Cancer. 2007;96:1377–1383. doi: 10.1038/sj.bjc.6603744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang S, Li M, Zhang D, Xu S, Wang X, Liu Z, Zhao X, Sun B. Hypoxia influences linearly patterned programmed cell necrosis and tumor blood supply patterns formation in melanoma. Lab Invest. 2009;89:575–586. doi: 10.1038/labinvest.2009.20. [DOI] [PubMed] [Google Scholar]
- 50.van der Schaft DW, Hillen F, Pauwels P, Kirschmann DA, Castermans K, Egbrink MG, Tran MG, Sciot R, Hauben E, Hogendoorn PC, Delattre O, Maxwell PH, Hendrix MJ, Griffioen AW. Tumor cell plasticity in Ewing sarcoma, an alternative circulatory system stimulated by hypoxia. Cancer Res. 2005;65:11520–11528. doi: 10.1158/0008-5472.CAN-05-2468. [DOI] [PubMed] [Google Scholar]
- 51.Ma JL, Han SX, Zhu Q, Zhao J, Zhang D, Wang L, Lv Y. Role of Twist in vasculogenic mimicry formation in hypoxic hepatocellular carcinoma cells in vitro. Biochem Biophys Res Commun. 2011;408:686–691. doi: 10.1016/j.bbrc.2011.04.089. [DOI] [PubMed] [Google Scholar]
- 52.Sun B, Zhang D, Zhang S, Zhang W, Guo H, Zhao X. Hypoxia influences vasculogenic mimicry channel formation and tumor invasion-related protein expression in melanoma. Cancer Lett. 2007;249:188–197. doi: 10.1016/j.canlet.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 53.Hillen F, Griffioen AW. Tumour vascularization: sprouting angiogenesis and beyond. Cancer Metastasis Rev. 2007;26:489–502. doi: 10.1007/s10555-007-9094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kirschmann DA, Seftor EA, Hardy KM, Seftor RE, Hendrix MJ. Molecular pathways: vasculogenic mimicry in tumor cells: diagnostic and therapeutic implications. Clin Cancer Res. 2012;18:2726–2732. doi: 10.1158/1078-0432.CCR-11-3237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tang NN, Zhu H, Zhang HJ, Zhang WF, Jin HL, Wang L, Wang P, He GJ, Hao B, Shi RH. HIF-1α induces VE-cadherin expression and modulates vasculogenic mimicry in esophageal carcinoma cells. World J Gastroenterol. 2014;20:17894–17904. doi: 10.3748/wjg.v20.i47.17894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chai DM, Bao ZQ, Hu JG, Ma L, Feng ZZ, Tao YS. Vasculogenic mimicry and aberrant expression of HIF-lα/E-cad are associated with worse prognosis of esophageal squamous cell carcinoma. J Huazhong Univ Sci Technolog Med Sci. 2013;33:385–391. doi: 10.1007/s11596-013-1129-4. [DOI] [PubMed] [Google Scholar]
- 57.Mao Y, Wang Y, Dong L, Zhang Y, Wang C, Zhang Q, Yang S, Cao L, Zhang X, Li X, Fu Z. Hypoxic exosomes facilitate angiogenesis and metastasis in esophageal squamous cell carcinoma through altering the phenotype and transcriptome of endothelial cells. J Exp Clin Cancer Res. 2019;38:389. doi: 10.1186/s13046-019-1384-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen DS, Mellman I. Elements of cancer immunity and the cancer-immune set point. Nature. 2017;541:321–330. doi: 10.1038/nature21349. [DOI] [PubMed] [Google Scholar]
- 59.Power R, Lowery MA, Reynolds JV, Dunne MR. The Cancer-Immune Set Point in Oesophageal Cancer. Front Oncol. 2020;10:891. doi: 10.3389/fonc.2020.00891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Diaz-Montero CM, Salem ML, Nishimura MI, Garrett-Mayer E, Cole DJ, Montero AJ. Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage, metastatic tumor burden, and doxorubicin-cyclophosphamide chemotherapy. Cancer Immunol Immunother. 2009;58:49–59. doi: 10.1007/s00262-008-0523-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Condamine T, Ramachandran I, Youn JI, Gabrilovich DI. Regulation of tumor metastasis by myeloid-derived suppressor cells. Annu Rev Med. 2015;66:97–110. doi: 10.1146/annurev-med-051013-052304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gabitass RF, Annels NE, Stocken DD, Pandha HA, Middleton GW. Elevated myeloid-derived suppressor cells in pancreatic, esophageal and gastric cancer are an independent prognostic factor and are associated with significant elevation of the Th2 cytokine interleukin-13. Cancer Immunol Immunother. 2011;60:1419–1430. doi: 10.1007/s00262-011-1028-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Talmadge JE, Gabrilovich DI. History of myeloid-derived suppressor cells. Nat Rev Cancer. 2013;13:739–752. doi: 10.1038/nrc3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen MF, Kuan FC, Yen TC, Lu MS, Lin PY, Chung YH, Chen WC, Lee KD. IL-6-stimulated CD11b+ CD14+ HLA-DR- myeloid-derived suppressor cells, are associated with progression and poor prognosis in squamous cell carcinoma of the esophagus. Oncotarget. 2014;5:8716–8728. doi: 10.18632/oncotarget.2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ambler DR, Fletcher NM, Diamond MP, Saed GM. Effects of hypoxia on the expression of inflammatory markers IL-6 and TNF-a in human normal peritoneal and adhesion fibroblasts. Syst Biol Reprod Med. 2012;58:324–329. doi: 10.3109/19396368.2012.713439. [DOI] [PubMed] [Google Scholar]
- 67.Corzo CA, Condamine T, Lu L, Cotter MJ, Youn JI, Cheng P, Cho HI, Celis E, Quiceno DG, Padhya T, McCaffrey TV, McCaffrey JC, Gabrilovich DI. HIF-1α regulates function and differentiation of myeloid-derived suppressor cells in the tumor microenvironment. J Exp Med. 2010;207:2439–2453. doi: 10.1084/jem.20100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Poh AR, Ernst M. Targeting Macrophages in Cancer: From Bench to Bedside. Front Oncol. 2018;8:49. doi: 10.3389/fonc.2018.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ostuni R, Kratochvill F, Murray PJ, Natoli G. Macrophages and cancer: from mechanisms to therapeutic implications. Trends Immunol. 2015;36:229–239. doi: 10.1016/j.it.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 70.Henze AT, Mazzone M. The impact of hypoxia on tumor-associated macrophages. J Clin Invest. 2016;126:3672–3679. doi: 10.1172/JCI84427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Murdoch C, Giannoudis A, Lewis CE. Mechanisms regulating the recruitment of macrophages into hypoxic areas of tumors and other ischemic tissues. Blood. 2004;104:2224–2234. doi: 10.1182/blood-2004-03-1109. [DOI] [PubMed] [Google Scholar]
- 72.Murdoch C, Lewis CE. Macrophage migration and gene expression in response to tumor hypoxia. Int J Cancer. 2005;117:701–708. doi: 10.1002/ijc.21422. [DOI] [PubMed] [Google Scholar]
- 73.Schioppa T, Uranchimeg B, Saccani A, Biswas SK, Doni A, Rapisarda A, Bernasconi S, Saccani S, Nebuloni M, Vago L, Mantovani A, Melillo G, Sica A. Regulation of the chemokine receptor CXCR4 by hypoxia. J Exp Med. 2003;198:1391–1402. doi: 10.1084/jem.20030267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bingle L, Brown NJ, Lewis CE. The role of tumour-associated macrophages in tumour progression: implications for new anticancer therapies. J Pathol. 2002;196:254–265. doi: 10.1002/path.1027. [DOI] [PubMed] [Google Scholar]
- 75.Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Steidl C, Lee T, Shah SP, Farinha P, Han G, Nayar T, Delaney A, Jones SJ, Iqbal J, Weisenburger DD, Bast MA, Rosenwald A, Muller-Hermelink HK, Rimsza LM, Campo E, Delabie J, Braziel RM, Cook JR, Tubbs RR, Jaffe ES, Lenz G, Connors JM, Staudt LM, Chan WC, Gascoyne RD. Tumor-associated macrophages and survival in classic Hodgkin's lymphoma. N Engl J Med. 2010;362:875–885. doi: 10.1056/NEJMoa0905680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Li J, Xie Y, Wang X, Li F, Li S, Li M, Peng H, Yang L, Liu C, Pang L, Zou H, Zhao J, Qi Y, Cao Y, Hu J. Prognostic impact of tumor-associated macrophage infiltration in esophageal cancer: a meta-analysis. Future Oncol. 2019;15:2303–2317. doi: 10.2217/fon-2018-0669. [DOI] [PubMed] [Google Scholar]
- 78.Yagi T, Baba Y, Okadome K, Kiyozumi Y, Hiyoshi Y, Ishimoto T, Iwatsuki M, Miyamoto Y, Yoshida N, Watanabe M, Komohara Y, Baba H. Tumour-associated macrophages are associated with poor prognosis and programmed death ligand 1 expression in oesophageal cancer. Eur J Cancer. 2019;111:38–49. doi: 10.1016/j.ejca.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 79.Harmey JH, Dimitriadis E, Kay E, Redmond HP, Bouchier-Hayes D. Regulation of macrophage production of vascular endothelial growth factor (VEGF) by hypoxia and transforming growth factor beta-1. Ann Surg Oncol. 1998;5:271–278. doi: 10.1007/BF02303785. [DOI] [PubMed] [Google Scholar]
- 80.Kuwabara K, Ogawa S, Matsumoto M, Koga S, Clauss M, Pinsky DJ, Lyn P, Leavy J, Witte L, Joseph-Silverstein J. Hypoxia-mediated induction of acidic/basic fibroblast growth factor and platelet-derived growth factor in mononuclear phagocytes stimulates growth of hypoxic endothelial cells. Proc Natl Acad Sci USA. 1995;92:4606–4610. doi: 10.1073/pnas.92.10.4606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang WJ, Chen C, Zhou ZH, Gao ST, Tee TJ, Yang LQ, Xu YY, Pang TH, Xu XY, Sun Q, Feng M, Wang H, Lu CL, Wu GZ, Wu S, Guan WX, Xu GF. Hypoxia-inducible factor-1 alpha Correlates with Tumor-Associated Macrophages Infiltration, Influences Survival of Gastric Cancer Patients. J Cancer. 2017;8:1818–1825. doi: 10.7150/jca.19057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Osinsky S, Bubnovskaya L, Ganusevich I, Kovelskaya A, Gumenyuk L, Olijnichenko G, Merentsev S. Hypoxia, tumour-associated macrophages, microvessel density, VEGF and matrix metalloproteinases in human gastric cancer: interaction and impact on survival. Clin Transl Oncol. 2011;13:133–138. doi: 10.1007/s12094-011-0630-0. [DOI] [PubMed] [Google Scholar]
- 83.Seven to Gilead: "Eat me". Nat Biotechnol. 2020;38:389. doi: 10.1038/s41587-020-0496-1. [DOI] [PubMed] [Google Scholar]
- 84.Zhao CL, Yu S, Wang SH, Li SG, Wang ZJ, Han SN. Characterization of cluster of differentiation 47 expression and its potential as a therapeutic target in esophageal squamous cell cancer. Oncol Lett. 2018;15:2017–2023. doi: 10.3892/ol.2017.7447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tao H, Qian P, Wang F, Yu H, Guo Y. Targeting CD47 Enhances the Efficacy of Anti-PD-1 and CTLA-4 in an Esophageal Squamous Cell Cancer Preclinical Model. Oncol Res. 2017;25:1579–1587. doi: 10.3727/096504017X14900505020895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Suzuki S, Yokobori T, Tanaka N, Sakai M, Sano A, Inose T, Sohda M, Nakajima M, Miyazaki T, Kato H, Kuwano H. CD47 expression regulated by the miR-133a tumor suppressor is a novel prognostic marker in esophageal squamous cell carcinoma. Oncol Rep. 2012;28:465–472. doi: 10.3892/or.2012.1831. [DOI] [PubMed] [Google Scholar]
- 87.Caligiuri MA. Human natural killer cells. Blood. 2008;112:461–469. doi: 10.1182/blood-2007-09-077438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vivier E, Tomasello E, Baratin M, Walzer T, Ugolini S. Functions of natural killer cells. Nat Immunol. 2008;9:503–510. doi: 10.1038/ni1582. [DOI] [PubMed] [Google Scholar]
- 89.Siemens DR, Hu N, Sheikhi AK, Chung E, Frederiksen LJ, Pross H, Graham CH. Hypoxia increases tumor cell shedding of MHC class I chain-related molecule: role of nitric oxide. Cancer Res. 2008;68:4746–4753. doi: 10.1158/0008-5472.CAN-08-0054. [DOI] [PubMed] [Google Scholar]
- 90.Balsamo M, Manzini C, Pietra G, Raggi F, Blengio F, Mingari MC, Varesio L, Moretta L, Bosco MC, Vitale M. Hypoxia downregulates the expression of activating receptors involved in NK-cell-mediated target cell killing without affecting ADCC. Eur J Immunol. 2013;43:2756–2764. doi: 10.1002/eji.201343448. [DOI] [PubMed] [Google Scholar]
- 91.Yun S, Lee SH, Yoon SR, Myung PK, Choi I. Oxygen tension regulates NK cells differentiation from hematopoietic stem cells in vitro. Immunol Lett. 2011;137:70–77. doi: 10.1016/j.imlet.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 92.Xu B, Chen L, Li J, Zheng X, Shi L, Wu C, Jiang J. Prognostic value of tumor infiltrating NK cells and macrophages in stage II+III esophageal cancer patients. Oncotarget. 2016;7:74904–74916. doi: 10.18632/oncotarget.12484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Liu Y, Cheng Y, Xu Y, Wang Z, Du X, Li C, Peng J, Gao L, Liang X, Ma C. Increased expression of programmed cell death protein 1 on NK cells inhibits NK-cell-mediated anti-tumor function and indicates poor prognosis in digestive cancers. Oncogene. 2017;36:6143–6153. doi: 10.1038/onc.2017.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zheng Y, Li Y, Lian J, Yang H, Li F, Zhao S, Qi Y, Zhang Y, Huang L. TNF-α-induced Tim-3 expression marks the dysfunction of infiltrating natural killer cells in human esophageal cancer. J Transl Med. 2019;17:165. doi: 10.1186/s12967-019-1917-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang Z, Zhu J, Gu H, Yuan Y, Zhang B, Zhu D, Zhou J, Zhu Y, Chen W. The Clinical Significance of Abnormal Tim-3 Expression on NK Cells from Patients with Gastric Cancer. Immunol Invest. 2015;44:578–589. doi: 10.3109/08820139.2015.1052145. [DOI] [PubMed] [Google Scholar]
- 96.Ma Y, Shurin GV, Peiyuan Z, Shurin MR. Dendritic cells in the cancer microenvironment. J Cancer. 2013;4:36–44. doi: 10.7150/jca.5046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Janikashvili N, Bonnotte B, Katsanis E, Larmonier N. The dendritic cell-regulatory T lymphocyte crosstalk contributes to tumor-induced tolerance. Clin Dev Immunol. 2011;2011:430394. doi: 10.1155/2011/430394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Manicassamy S, Pulendran B. Dendritic cell control of tolerogenic responses. Immunol Rev. 2011;241:206–227. doi: 10.1111/j.1600-065X.2011.01015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gabrilovich DI, Ciernik IF, Carbone DP. Dendritic cells in antitumor immune responses. I. Defective antigen presentation in tumor-bearing hosts. Cell Immunol. 1996;170:101–110. doi: 10.1006/cimm.1996.0139. [DOI] [PubMed] [Google Scholar]
- 100.Elia AR, Cappello P, Puppo M, Fraone T, Vanni C, Eva A, Musso T, Novelli F, Varesio L, Giovarelli M. Human dendritic cells differentiated in hypoxia down-modulate antigen uptake and change their chemokine expression profile. J Leukoc Biol. 2008;84:1472–1482. doi: 10.1189/jlb.0208082. [DOI] [PubMed] [Google Scholar]
- 101.Mancino A, Schioppa T, Larghi P, Pasqualini F, Nebuloni M, Chen IH, Sozzani S, Austyn JM, Mantovani A, Sica A. Divergent effects of hypoxia on dendritic cell functions. Blood. 2008;112:3723–3734. doi: 10.1182/blood-2008-02-142091. [DOI] [PubMed] [Google Scholar]
- 102.Nagelkerke A, Bussink J, Mujcic H, Wouters BG, Lehmann S, Sweep FC, Span PN. Hypoxia stimulates migration of breast cancer cells via the PERK/ATF4/LAMP3-arm of the unfolded protein response. Breast Cancer Res. 2013;15:R2. doi: 10.1186/bcr3373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mujcic H, Nagelkerke A, Rouschop KM, Chung S, Chaudary N, Span PN, Clarke B, Milosevic M, Sykes J, Hill RP, Koritzinsky M, Wouters BG. Hypoxic activation of the PERK/eIF2α arm of the unfolded protein response promotes metastasis through induction of LAMP3. Clin Cancer Res. 2013;19:6126–6137. doi: 10.1158/1078-0432.CCR-13-0526. [DOI] [PubMed] [Google Scholar]
- 104.Liao X, Chen Y, Liu D, Li F, Li X, Jia W. High Expression of LAMP3 Is a Novel Biomarker of Poor Prognosis in Patients with Esophageal Squamous Cell Carcinoma. Int J Mol Sci. 2015;16:17655–17667. doi: 10.3390/ijms160817655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Somja J, Demoulin S, Roncarati P, Herfs M, Bletard N, Delvenne P, Hubert P. Dendritic cells in Barrett's esophagus carcinogenesis: an inadequate microenvironment for antitumor immunity? Am J Pathol. 2013;182:2168–2179. doi: 10.1016/j.ajpath.2013.02.036. [DOI] [PubMed] [Google Scholar]
- 106.MartIn-Fontecha A, Sebastiani S, Höpken UE, Uguccioni M, Lipp M, Lanzavecchia A, Sallusto F. Regulation of dendritic cell migration to the draining lymph node: impact on T lymphocyte traffic and priming. J Exp Med. 2003;198:615–621. doi: 10.1084/jem.20030448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ben-Shoshan J, Maysel-Auslender S, Mor A, Keren G, George J. Hypoxia controls CD4+CD25+ regulatory T-cell homeostasis via hypoxia-inducible factor-1alpha. Eur J Immunol. 2008;38:2412–2418. doi: 10.1002/eji.200838318. [DOI] [PubMed] [Google Scholar]
- 108.Clambey ET, McNamee EN, Westrich JA, Glover LE, Campbell EL, Jedlicka P, de Zoeten EF, Cambier JC, Stenmark KR, Colgan SP, Eltzschig HK. Hypoxia-inducible factor-1 alpha-dependent induction of FoxP3 drives regulatory T-cell abundance and function during inflammatory hypoxia of the mucosa. Proc Natl Acad Sci USA. 2012;109:E2784–E2793. doi: 10.1073/pnas.1202366109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yuan XL, Chen L, Li MX, Dong P, Xue J, Wang J, Zhang TT, Wang XA, Zhang FM, Ge HL, Shen LS, Xu D. Elevated expression of Foxp3 in tumor-infiltrating Treg cells suppresses T-cell proliferation and contributes to gastric cancer progression in a COX-2-dependent manner. Clin Immunol. 2010;134:277–288. doi: 10.1016/j.clim.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 110.Kono K, Kawaida H, Takahashi A, Sugai H, Mimura K, Miyagawa N, Omata H, Fujii H. CD4(+)CD25high regulatory T cells increase with tumor stage in patients with gastric and esophageal cancers. Cancer Immunol Immunother. 2006;55:1064–1071. doi: 10.1007/s00262-005-0092-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shen Z, Zhou S, Wang Y, Li RL, Zhong C, Liang C, Sun Y. Higher intratumoral infiltrated Foxp3+ Treg numbers and Foxp3+/CD8+ ratio are associated with adverse prognosis in resectable gastric cancer. J Cancer Res Clin Oncol. 2010;136:1585–1595. doi: 10.1007/s00432-010-0816-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cirri P, Chiarugi P. Cancer associated fibroblasts: the dark side of the coin. Am J Cancer Res. 2011;1:482–497. [PMC free article] [PubMed] [Google Scholar]
- 113.Xing F, Saidou J, Watabe K. Cancer associated fibroblasts (CAFs) in tumor microenvironment. Front Biosci (Landmark Ed) 2010;15:166–179. doi: 10.2741/3613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Petrova V, Annicchiarico-Petruzzelli M, Melino G, Amelio I. The hypoxic tumour microenvironment. Oncogenesis. 2018;7:10. doi: 10.1038/s41389-017-0011-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Underwood TJ, Hayden AL, Derouet M, Garcia E, Noble F, White MJ, Thirdborough S, Mead A, Clemons N, Mellone M, Uzoho C, Primrose JN, Blaydes JP, Thomas GJ. Cancer-associated fibroblasts predict poor outcome and promote periostin-dependent invasion in oesophageal adenocarcinoma. J Pathol. 2015;235:466–477. doi: 10.1002/path.4467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Shields MA, Dangi-Garimella S, Krantz SB, Bentrem DJ, Munshi HG. Pancreatic cancer cells respond to type I collagen by inducing snail expression to promote membrane type 1 matrix metalloproteinase-dependent collagen invasion. J Biol Chem. 2011;286:10495–10504. doi: 10.1074/jbc.M110.195628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zeisberg EM, Potenta S, Xie L, Zeisberg M, Kalluri R. Discovery of endothelial to mesenchymal transition as a source for carcinoma-associated fibroblasts. Cancer Res. 2007;67:10123–10128. doi: 10.1158/0008-5472.CAN-07-3127. [DOI] [PubMed] [Google Scholar]
- 118.Radisky DC, Kenny PA, Bissell MJ. Fibrosis and cancer: do myofibroblasts come also from epithelial cells via EMT? J Cell Biochem. 2007;101:830–839. doi: 10.1002/jcb.21186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wu X, Qiao B, Liu Q, Zhang W. Upregulation of extracellular matrix metalloproteinase inducer promotes hypoxia-induced epithelial-mesenchymal transition in esophageal cancer. Mol Med Rep. 2015;12:7419–7424. doi: 10.3892/mmr.2015.4410. [DOI] [PubMed] [Google Scholar]
- 120.Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324:1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Nobel Prize Outreach. The Nobel Prize in Physiology or Medicine 1931. [cited 24 February 2021]. In: Nobel Prize Outreach [Internet]. Available from: https://www.nobelprize.org/prizes/medicine/1931/summary/
- 122.Eales KL, Hollinshead KE, Tennant DA. Hypoxia and metabolic adaptation of cancer cells. Oncogenesis. 2016;5:e190. doi: 10.1038/oncsis.2015.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Semenza GL. Tumor metabolism: cancer cells give and take lactate. J Clin Invest. 2008;118:3835–3837. doi: 10.1172/JCI37373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Isidoro A, Martínez M, Fernández PL, Ortega AD, Santamaría G, Chamorro M, Reed JC, Cuezva JM. Alteration of the bioenergetic phenotype of mitochondria is a hallmark of breast, gastric, lung and oesophageal cancer. Biochem J. 2004;378:17–20. doi: 10.1042/BJ20031541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lynam-Lennon N, Maher SG, Maguire A, Phelan J, Muldoon C, Reynolds JV, O'Sullivan J. Altered mitochondrial function and energy metabolism is associated with a radioresistant phenotype in oesophageal adenocarcinoma. PLoS One. 2014;9:e100738. doi: 10.1371/journal.pone.0100738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Doherty JR, Cleveland JL. Targeting lactate metabolism for cancer therapeutics. J Clin Invest. 2013;123:3685–3692. doi: 10.1172/JCI69741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kolev Y, Uetake H, Takagi Y, Sugihara K. Lactate dehydrogenase-5 (LDH-5) expression in human gastric cancer: association with hypoxia-inducible factor (HIF-1alpha) pathway, angiogenic factors production and poor prognosis. Ann Surg Oncol. 2008;15:2336–2344. doi: 10.1245/s10434-008-9955-5. [DOI] [PubMed] [Google Scholar]
- 128.Husain Z, Huang Y, Seth P, Sukhatme VP. Tumor-derived lactate modifies antitumor immune response: effect on myeloid-derived suppressor cells and NK cells. J Immunol. 2013;191:1486–1495. doi: 10.4049/jimmunol.1202702. [DOI] [PubMed] [Google Scholar]
- 129.Hagberg H, Andersson P, Lacarewicz J, Jacobson I, Butcher S, Sandberg M. Extracellular adenosine, inosine, hypoxanthine, and xanthine in relation to tissue nucleotides and purines in rat striatum during transient ischemia. J Neurochem. 1987;49:227–231. doi: 10.1111/j.1471-4159.1987.tb03419.x. [DOI] [PubMed] [Google Scholar]
- 130.Ballarín M, Fredholm BB, Ambrosio S, Mahy N. Extracellular levels of adenosine and its metabolites in the striatum of awake rats: inhibition of uptake and metabolism. Acta Physiol Scand. 1991;142:97–103. doi: 10.1111/j.1748-1716.1991.tb09133.x. [DOI] [PubMed] [Google Scholar]
- 131.Zetterström T, Vernet L, Ungerstedt U, Tossman U, Jonzon B, Fredholm BB. Purine levels in the intact rat brain. Studies with an implanted perfused hollow fibre. Neurosci Lett. 1982;29:111–115. doi: 10.1016/0304-3940(82)90338-x. [DOI] [PubMed] [Google Scholar]
- 132.Eltzschig HK, Sitkovsky MV, Robson SC. Purinergic signaling during inflammation. N Engl J Med. 2012;367:2322–2333. doi: 10.1056/NEJMra1205750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Blay J, White TD, Hoskin DW. The extracellular fluid of solid carcinomas contains immunosuppressive concentrations of adenosine. Cancer Res. 1997;57:2602–2605. [PubMed] [Google Scholar]
- 134.Vaupel P, Mayer A. Hypoxia-Driven Adenosine Accumulation: A Crucial Microenvironmental Factor Promoting Tumor Progression. Adv Exp Med Biol. 2016;876:177–183. doi: 10.1007/978-1-4939-3023-4_22. [DOI] [PubMed] [Google Scholar]
- 135.Ohta A. A Metabolic Immune Checkpoint: Adenosine in Tumor Microenvironment. Front Immunol. 2016;7:109. doi: 10.3389/fimmu.2016.00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chambers AM, Matosevic S. Immunometabolic Dysfunction of Natural Killer Cells Mediated by the Hypoxia-CD73 Axis in Solid Tumors. Front Mol Biosci. 2019;6:60. doi: 10.3389/fmolb.2019.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Synnestvedt K, Furuta GT, Comerford KM, Louis N, Karhausen J, Eltzschig HK, Hansen KR, Thompson LF, Colgan SP. Ecto-5'-nucleotidase (CD73) regulation by hypoxia-inducible factor-1 mediates permeability changes in intestinal epithelia. J Clin Invest. 2002;110:993–1002. doi: 10.1172/JCI15337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Young A, Mittal D, Stagg J, Smyth MJ. Targeting cancer-derived adenosine: new therapeutic approaches. Cancer Discov. 2014;4:879–888. doi: 10.1158/2159-8290.CD-14-0341. [DOI] [PubMed] [Google Scholar]
- 139.Vijayan D, Young A, Teng MWL, Smyth MJ. Targeting immunosuppressive adenosine in cancer. Nat Rev Cancer. 2017;17:709–724. doi: 10.1038/nrc.2017.86. [DOI] [PubMed] [Google Scholar]
- 140.Hatfield SM, Kjaergaard J, Lukashev D, Schreiber TH, Belikoff B, Abbott R, Sethumadhavan S, Philbrook P, Ko K, Cannici R, Thayer M, Rodig S, Kutok JL, Jackson EK, Karger B, Podack ER, Ohta A, Sitkovsky MV. Immunological mechanisms of the antitumor effects of supplemental oxygenation. Sci Transl Med. 2015;7:277ra30. doi: 10.1126/scitranslmed.aaa1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wang MX, Ren LM, Shan BE. Inhibitory effects of extracellular adenosine triphosphate on growth of esophageal carcinoma cells. World J Gastroenterol. 2005;11:5915–5919. doi: 10.3748/wjg.v11.i38.5915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Fukuda K, Sakakura C, Miyagawa K, Kuriu Y, Kin S, Nakase Y, Hagiwara A, Mitsufuji S, Okazaki Y, Hayashizaki Y, Yamagishi H. Differential gene expression profiles of radioresistant oesophageal cancer cell lines established by continuous fractionated irradiation. Br J Cancer. 2004;91:1543–1550. doi: 10.1038/sj.bjc.6602187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Scharping NE, Menk AV, Whetstone RD, Zeng X, Delgoffe GM. Efficacy of PD-1 Blockade Is Potentiated by Metformin-Induced Reduction of Tumor Hypoxia. Cancer Immunol Res. 2017;5:9–16. doi: 10.1158/2326-6066.CIR-16-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Fyles AW, Milosevic M, Wong R, Kavanagh MC, Pintilie M, Sun A, Chapman W, Levin W, Manchul L, Keane TJ, Hill RP. Oxygenation predicts radiation response and survival in patients with cervix cancer. Radiother Oncol. 1998;48:149–156. doi: 10.1016/s0167-8140(98)00044-9. [DOI] [PubMed] [Google Scholar]
- 145.Nordsmark M, Bentzen SM, Rudat V, Brizel D, Lartigau E, Stadler P, Becker A, Adam M, Molls M, Dunst J, Terris DJ, Overgaard J. Prognostic value of tumor oxygenation in 397 head and neck tumors after primary radiation therapy. An international multi-center study. Radiother Oncol. 2005;77:18–24. doi: 10.1016/j.radonc.2005.06.038. [DOI] [PubMed] [Google Scholar]
- 146.Olive PL, Banáth JP, Aquino-Parsons C. Measuring hypoxia in solid tumours--is there a gold standard? Acta Oncol. 2001;40:917–923. doi: 10.1080/02841860152708189. [DOI] [PubMed] [Google Scholar]
- 147.Bayer C, Shi K, Astner ST, Maftei CA, Vaupel P. Acute vs chronic hypoxia: why a simplified classification is simply not enough. Int J Radiat Oncol Biol Phys. 2011;80:965–968. doi: 10.1016/j.ijrobp.2011.02.049. [DOI] [PubMed] [Google Scholar]
- 148.Luo D, Liu H, Lin D, Lian K, Ren H. The Clinicopathologic and Prognostic Value of Hypoxia-Inducible Factor-2α in Cancer Patients: A Systematic Review and Meta-Analysis. Cancer Epidemiol Biomarkers Prev. 2019;28:857–866. doi: 10.1158/1055-9965.EPI-18-0881. [DOI] [PubMed] [Google Scholar]
- 149.Tong WW, Tong GH, Chen XX, Zheng HC, Wang YZ. HIF2α is associated with poor prognosis and affects the expression levels of survivin and cyclin D1 in gastric carcinoma. Int J Oncol. 2015;46:233–242. doi: 10.3892/ijo.2014.2719. [DOI] [PubMed] [Google Scholar]
- 150.Driessen A, Landuyt W, Pastorekova S, Moons J, Goethals L, Haustermans K, Nafteux P, Penninckx F, Geboes K, Lerut T, Ectors N. Expression of carbonic anhydrase IX (CA IX), a hypoxia-related protein, rather than vascular-endothelial growth factor (VEGF), a pro-angiogenic factor, correlates with an extremely poor prognosis in esophageal and gastric adenocarcinomas. Ann Surg. 2006;243:334–340. doi: 10.1097/01.sla.0000201452.09591.f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Munipalle PC, Viswanath YK, Davis PA, Scoones D. Prognostic value of hypoxia inducible factor 1α in esophageal squamous cell carcinoma. Dis Esophagus. 2011;24:177–181. doi: 10.1111/j.1442-2050.2010.01122.x. [DOI] [PubMed] [Google Scholar]
- 152.Peerlings J, Van De Voorde L, Mitea C, Larue R, Yaromina A, Sandeleanu S, Spiegelberg L, Dubois L, Lambin P, Mottaghy FM. Hypoxia and hypoxia response-associated molecular markers in esophageal cancer: A systematic review. Methods. 2017;130:51–62. doi: 10.1016/j.ymeth.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 153.Buffa FM, Harris AL, West CM, Miller CJ. Large meta-analysis of multiple cancers reveals a common, compact and highly prognostic hypoxia metagene. Br J Cancer. 2010;102:428–435. doi: 10.1038/sj.bjc.6605450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Harris BH, Barberis A, West CM, Buffa FM. Gene Expression Signatures as Biomarkers of Tumour Hypoxia. Clin Oncol (R Coll Radiol) 2015;27:547–560. doi: 10.1016/j.clon.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 155.Fox NS, Starmans MH, Haider S, Lambin P, Boutros PC. Ensemble analyses improve signatures of tumour hypoxia and reveal inter-platform differences. BMC Bioinformatics. 2014;15:170. doi: 10.1186/1471-2105-15-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ye Y, Hu Q, Chen H, Liang K, Yuan Y, Xiang Y, Ruan H, Zhang Z, Song A, Zhang H, Liu L, Diao L, Lou Y, Zhou B, Wang L, Zhou S, Gao J, Jonasch E, Lin SH, Xia Y, Lin C, Yang L, Mills GB, Liang H, Han L. Characterization of Hypoxia-associated Molecular Features to Aid Hypoxia-Targeted Therapy. Nat Metab. 2019;1:431–444. doi: 10.1038/s42255-019-0045-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Rofstad EK, Sundfør K, Lyng H, Tropé CG. Hypoxia-induced treatment failure in advanced squamous cell carcinoma of the uterine cervix is primarily due to hypoxia-induced radiation resistance rather than hypoxia-induced metastasis. Br J Cancer. 2000;83:354–359. doi: 10.1054/bjoc.2000.1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kato Y, Yashiro M, Fuyuhiro Y, Kashiwagi S, Matsuoka J, Hirakawa T, Noda S, Aomatsu N, Hasegawa T, Matsuzaki T, Sawada T, Ohira M, Hirakawa K. Effects of acute and chronic hypoxia on the radiosensitivity of gastric and esophageal cancer cells. Anticancer Res. 2011;31:3369–3375. [PubMed] [Google Scholar]
- 159.Rohwer N, Dame C, Haugstetter A, Wiedenmann B, Detjen K, Schmitt CA, Cramer T. Hypoxia-inducible factor 1alpha determines gastric cancer chemosensitivity via modulation of p53 and NF-kappaB. PLoS One. 2010;5:e12038. doi: 10.1371/journal.pone.0012038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hammond EM, Giaccia AJ. Hypoxia-inducible factor-1 and p53: friends, acquaintances, or strangers? Clin Cancer Res. 2006;12:5007–5009. doi: 10.1158/1078-0432.CCR-06-0613. [DOI] [PubMed] [Google Scholar]
- 161.Liu L, Ning X, Sun L, Zhang H, Shi Y, Guo C, Han S, Liu J, Sun S, Han Z, Wu K, Fan D. Hypoxia-inducible factor-1 alpha contributes to hypoxia-induced chemoresistance in gastric cancer. Cancer Sci. 2008;99:121–128. doi: 10.1111/j.1349-7006.2007.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Shi WJ, Gao JB. Molecular mechanisms of chemoresistance in gastric cancer. World J Gastrointest Oncol. 2016;8:673–681. doi: 10.4251/wjgo.v8.i9.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Xu HW, Xu L, Hao JH, Qin CY, Liu H. Expression of P-glycoprotein and multidrug resistance-associated protein is associated with multidrug resistance in gastric cancer. J Int Med Res. 2010;38:34–42. doi: 10.1177/147323001003800104. [DOI] [PubMed] [Google Scholar]
- 164.Yue J, Yang Y, Cabrera AR, Sun X, Zhao S, Xie P, Zheng J, Ma L, Fu Z, Yu J. Measuring tumor hypoxia with ¹⁸F-FETNIM PET in esophageal squamous cell carcinoma: a pilot clinical study. Dis Esophagus. 2012;25:54–61. doi: 10.1111/j.1442-2050.2011.01209.x. [DOI] [PubMed] [Google Scholar]
- 165.Fleming IN, Manavaki R, Blower PJ, West C, Williams KJ, Harris AL, Domarkas J, Lord S, Baldry C, Gilbert FJ. Imaging tumour hypoxia with positron emission tomography. Br J Cancer. 2015;112:238–250. doi: 10.1038/bjc.2014.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Melsens E, De Vlieghere E, Descamps B, Vanhove C, Kersemans K, De Vos F, Goethals I, Brans B, De Wever O, Ceelen W, Pattyn P. Hypoxia imaging with 18F-FAZA PET/CT predicts radiotherapy response in esophageal adenocarcinoma xenografts. Radiat Oncol. 2018;13:39. doi: 10.1186/s13014-018-0984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Klaassen R, Bennink RJ, van Tienhoven G, Bijlsma MF, Besselink MG, van Berge Henegouwen MI, Wilmink JW, Nederveen AJ, Windhorst AD, Hulshof MC, van Laarhoven HW. Feasibility and repeatability of PET with the hypoxia tracer [(18)F]HX4 in oesophageal and pancreatic cancer. Radiother Oncol. 2015;116:94–99. doi: 10.1016/j.radonc.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 168.Pastorekova S, Gillies RJ. The role of carbonic anhydrase IX in cancer development: links to hypoxia, acidosis, and beyond. Cancer Metastasis Rev. 2019;38:65–77. doi: 10.1007/s10555-019-09799-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Chiche J, Ilc K, Laferrière J, Trottier E, Dayan F, Mazure NM, Brahimi-Horn MC, Pouysségur J. Hypoxia-inducible carbonic anhydrase IX and XII promote tumor cell growth by counteracting acidosis through the regulation of the intracellular pH. Cancer Res. 2009;69:358–368. doi: 10.1158/0008-5472.CAN-08-2470. [DOI] [PubMed] [Google Scholar]
- 170.Birner P, Jesch B, Friedrich J, Riegler M, Zacherl J, Hejna M, Wrba F, Schultheis A, Schoppmann SF. Carbonic anhydrase IX overexpression is associated with diminished prognosis in esophageal cancer and correlates with Her-2 expression. Ann Surg Oncol. 2011;18:3330–3337. doi: 10.1245/s10434-011-1730-3. [DOI] [PubMed] [Google Scholar]
- 171.Griffiths EA, Pritchard SA, Valentine HR, Whitchelo N, Bishop PW, Ebert MP, Price PM, Welch IM, West CM. Hypoxia-inducible factor-1alpha expression in the gastric carcinogenesis sequence and its prognostic role in gastric and gastro-oesophageal adenocarcinomas. Br J Cancer. 2007;96:95–103. doi: 10.1038/sj.bjc.6603524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Sauerbrei W, Taube SE, McShane LM, Cavenagh MM, Altman DG. Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK): An Abridged Explanation and Elaboration. J Natl Cancer Inst. 2018;110:803–811. doi: 10.1093/jnci/djy088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wilson WR, Hay MP. Targeting hypoxia in cancer therapy. Nat Rev Cancer. 2011;11:393–410. doi: 10.1038/nrc3064. [DOI] [PubMed] [Google Scholar]
- 174.Phillips RM, Hendriks HR, Sweeney JB, Reddy G, Peters GJ. Efficacy, pharmacokinetic and pharmacodynamic evaluation of apaziquone in the treatment of non-muscle invasive bladder cancer. Expert Opin Drug Metab Toxicol. 2017;13:783–791. doi: 10.1080/17425255.2017.1341490. [DOI] [PubMed] [Google Scholar]
- 175.Dirix LY, Tonnesen F, Cassidy J, Epelbaum R, ten Bokkel Huinink WW, Pavlidis N, Sorio R, Gamucci T, Wolff I, Te Velde A, Lan J, Verweij J. EO9 phase II study in advanced breast, gastric, pancreatic and colorectal carcinoma by the EORTC Early Clinical Studies Group. Eur J Cancer. 1996;32A:2019–2022. doi: 10.1016/0959-8049(96)00226-2. [DOI] [PubMed] [Google Scholar]
- 176.Spiegelberg L, van Hoof SJ, Biemans R, Lieuwes NG, Marcus D, Niemans R, Theys J, Yaromina A, Lambin P, Verhaegen F, Dubois LJ. Evofosfamide sensitizes esophageal carcinomas to radiation without increasing normal tissue toxicity. Radiother Oncol. 2019;141:247–255. doi: 10.1016/j.radonc.2019.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.R Core Team. R: A Language and Environment for Statistical Computing. [cited 24 February 2021]. In: The R Foundation [Internet]. 2019; Available from: https://www.r-project.org/
- 178.Tsai YP, Wu KJ. Hypoxia-regulated target genes implicated in tumor metastasis. J Biomed Sci. 2012;19:102. doi: 10.1186/1423-0127-19-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Gordan JD, Bertout JA, Hu CJ, Diehl JA, Simon MC. HIF-2alpha promotes hypoxic cell proliferation by enhancing c-myc transcriptional activity. Cancer Cell. 2007;11:335–347. doi: 10.1016/j.ccr.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Benita Y, Kikuchi H, Smith AD, Zhang MQ, Chung DC, Xavier RJ. An integrative genomics approach identifies Hypoxia Inducible Factor-1 (HIF-1)-target genes that form the core response to hypoxia. Nucleic Acids Res. 2009;37:4587–4602. doi: 10.1093/nar/gkp425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Hammond EM, Asselin MC, Forster D, O'Connor JP, Senra JM, Williams KJ. The meaning, measurement and modification of hypoxia in the laboratory and the clinic. Clin Oncol (R Coll Radiol) 2014;26:277–288. doi: 10.1016/j.clon.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 182.Rademakers SE, Span PN, Kaanders JH, Sweep FC, van der Kogel AJ, Bussink J. Molecular aspects of tumour hypoxia. Mol Oncol. 2008;2:41–53. doi: 10.1016/j.molonc.2008.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Le QT, Courter D. Clinical biomarkers for hypoxia targeting. Cancer Metastasis Rev. 2008;27:351–362. doi: 10.1007/s10555-008-9144-9. [DOI] [PMC free article] [PubMed] [Google Scholar]