Cardiac mitochondrial alterations are suspected to play a key role in the development of diabetes-related heart failure as reported in some animal and few human studies in type 2 diabetes (1). It is yet unclear whether these alterations are induced by diabetes-related metabolic changes or develop secondary to other factors underlying heart failure including micro- and macrovascular disease. We hypothesized that 1) exposure to type 2 diabetes provokes myocardial mitochondrial impairment prior to apparent left ventricular heart failure in humans and 2) these mitochondrial alterations are accompanied by increased oxidative stress, edema, and intracellular inflammation.
The cohort of this cross-sectional clinical study (study number 5263R; ClinicalTrials.gov NCT03386864) comprised adult heart transplant recipients undergoing routine transcatheter ventricular endomyocardial biopsies (EMB) post-transplantation, who received heart transplants of donors without type 2 diabetes. Thus, time between transplantation and EMB (2.9 ± 2.4 years) corresponded to the exposure of the hearts to type 2 diabetes. The first post-transplantation visit was included; exclusion criteria comprised allograft rejection (>0R according to International Society for Heart and Lung Transplantation criteria) and coronary artery disease (assessed via coronary angiography). Participants underwent oral glucose tolerance tests to assess glucose tolerance and insulin sensitivity (oral glucose insulin sensitivity [OGIS]). Cardiac magnetic resonance imaging was conducted at 1.5T to determine ventricular volumes and function, left ventricular T2 relaxation time, global left ventricular longitudinal strain (GLS), and diastolic strain rate. EMBs were attained for assessment of allograft rejection, mRNA expression of nuclear factor κ-light-chain-enhancer of activated B cells p105 subunit (NF-κB1), Toll-like receptor 9 (TLR9), and mitochondrially encoded cytochrome c oxidase I (CO1) and mitochondrial function using high-resolution respirometry in permeabilized myocardial fibers as recently described in detail (2). Thiobarbituric acid reactive substances (TBARS) and oxidation reduction potential (ORP) were measured as markers of systemic oxidative stress as previously described (3).
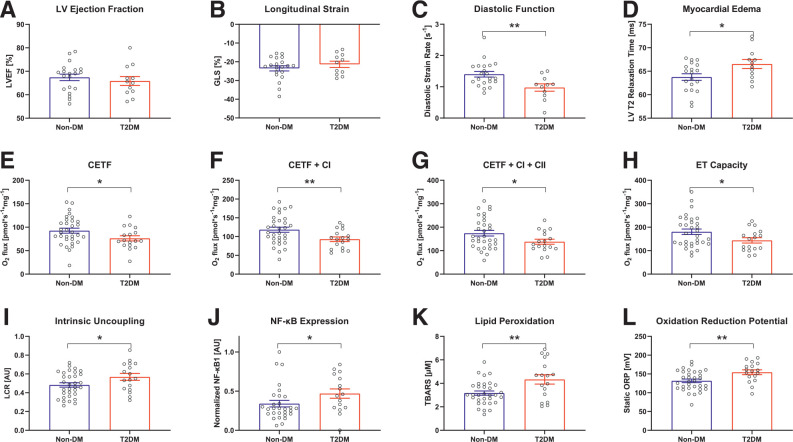
Thirty-two participants had no diabetes (Non-DM group), seventeen had type 2 diabetes (T2DM group). Sex distribution, age, time since transplantation, medication, and comorbidities were comparable between the groups. However, T2DM had higher BMI compared with Non-DM (median [interquartile range] 28.3 [24.5–30.3] vs. 24.6 [21.7–27.2] kg/m2) and were more likely taking β-blockers (59% vs. 25%). T2DM had higher HbA1c, fasting blood glucose, insulin, and free fatty acids but lower OGIS. While ejection fraction, cardiac index, and GLS were comparable, diastolic strain rate was impaired in T2DM and T2 relaxation times were prolonged, indicating higher degree of myocardial edema (Fig. 1A–D). Diastolic strain rate inversely related to fasting glycemia (R2 = 0.33; P < 0.001). In T2DM, myocardial mitochondrial oxidative phosphorylation capacity was 22–27% reduced and mitochondrial coupling was 19% lower (Fig. 1E–H), whereas ORP and TBARS were 17% and 34% higher compared with Non-DM (Fig. 1K and L). Myocardial oxidative capacity related negatively to fasting glycemia (R2 = 0.12; P < 0.05) but positively to OGIS (R2 = 0.24; P < 0.05). Oxidative capacity related inversely to myocardial edema (R2 = 0.15, P < 0.05). Cardiac NF-κB1 expression was 38% higher in T2DM (Fig. 1J) and related to fasting glycemia (R2 = 0.09; P < 0.05) and negatively to complex I respiration (R2 = 0.11; P < 0.05). OGIS related inversely to TLR9 expression (R2 = 0.19; P < 0.05) and myocardial edema (R2 = 0.25; P < 0.05). CO1 expression did not differ between the groups, suggesting comparable mitochondrial content.
Figure 1.
A–D: Different parameters of cardiac function and myocardial edema assessed via cardiac magnetic resonance imaging using a 1.5T scanner (Achieva; Philips, Best, the Netherlands). n = 31–32 (20–21 Non-DM vs. 11 T2DM). E–H: Myocardial mitochondrial respiration under saturated concentrations of different substrates in T2DM compared with Non-DM was assessed using the Oxygraph-2k (Oroboros Instruments, Innsbruck, Austria). Substrates used beyond malate and ADP were octanoyl-l-carnitine (for CETF), glutamate (for CI), and succinate (for CII), which then reflects the oxidative phosphorylation (OXPHOS) capacity. ET capacity was determined after titration of carbonyl cyanide-4-(trifluoromethoxy)phenylhydrazone (FCCP). n = 32 vs. 17. I: Intrinsic uncoupling of the respiratory chain, determined as state 4o divided by ET capacity. n = 32 vs. 17. J: Normalized expression of NF-κB1 (QuantiTect Reverse Transcription Kit; Qiagen, Venlo, the Netherlands). n = 29 vs. 16. K and L: Increased systemic oxidative stress in T2DM with respect to TBARS (measured fluorometrically [BioTek, Bad Friedrichshall, Germany]) and static ORP (measured using the RedoxSYS [Luoxis Diagnostics, Inc., Englewood, CO]). N = 32 vs. 17. Data are means ± SEM. *P < 0.05, **P < 0.01. Unpaired two-tailed t tests were used for all comparisons. AU, arbitrary unit; CETF, electron transferring flavoprotein complex; CI, respiratory chain complex I; CII, respiratory chain complex II; ET capacity, electron transfer pathway capacity; LCR, leak control ratio; LVEF, left ventricular ejection fraction.
This study provides direct evidence that exposure to type 2 diabetes impairs mitochondrial respiratory function in human ventricular myocardium without structural or coronary heart disease, which is tightly related to both insulin resistance and hyperglycemia. This reduction of ventricular mitochondrial function in type 2 diabetes is accompanied by myocardial edema, impaired diastolic strain rate as an early sign of reduced contractility, and intracellular inflammation, which might be promoted by increased systemic oxidative stress. These changes appear within 3 years of diabetes, in the absence of overt heart failure. A recent study examining a similar cohort concluded that type 2 diabetes increases myocardial lipid accumulation, but data on mitochondrial function were not assessed (4). This study provides novel evidence for an impairment of myocardial mitochondrial function in diabetes as known for skeletal muscle and liver (5).
Limitations of the study include the inability to assess mitochondrial function from the donor heart at time of transplantation and the overall small cohort size. Further, limited tissue size prevented us from conducting additional experiments, such as mitochondrial isolation and analyses of further enzyme activities and expression profiles. Of note, immunosuppressive medication of heart transplant recipients was similar in both groups and thereby unlikely affecting the results.
The current study demonstrates that exposure to type 2 diabetes rapidly attenuates ventricular mitochondrial function in apparently healthy human hearts, even in the absence of heart failure or coronary artery disease, pointing toward myocardial energy metabolism as a novel target for the treatment and diagnosis of diabetes-associated heart failure.
Article Information
Acknowledgments. The authors acknowledge the enormous support of people assisting with experimental procedures, data analysis, or discussion, including (in alphabetical order): Sophie Albermann, Julius Borger, Myrko Eßer, Ka Hou Martin Leung, Constanze Moos, Peter Nawroth, Ilka Rokitta, Klaus Witte, and Fariba Zivehe.
Funding. This work was supported by funding from the German Research Council (SFB1116), a grant provided by the research commission of the Medical Faculty, Heinrich-Heine University, Düsseldorf, Germany, the German Center for Diabetes Research (DZD e.V.) and the German Diabetes Center, which is funded by the German Federal Ministry of Health (Berlin, Germany) and the Ministry of Innovation, Science, Research, and Technology of the state North Rhine Westphalia (Düsseldorf, Germany).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. E.Z. contributed to data acquisition, experimental procedures, organization, writing of the first draft, discussion, and writing of the final draft. D.S. contributed to data acquisition, experimental procedures, organization, conception, discussion, and writing of the final draft. T.J. contributed to organization, conception, discussion, and writing of the final draft. F.B., P.H., and D.P. contributed to data acquisition, discussion, and writing of the final draft. H.-P.S. contributed to data acquisition, organization, discussion, and writing of the final draft. U.B., P.A., and A.L. contributed to data acquisition, organization, and discussion. M.K. and M.R. contributed to organization, discussion, and writing of the final draft. R.W. and J.S. contributed to initial conception, data acquisition, organization, discussion, and writing of the final draft. J.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Clinical trial reg. no. NCT03386864, clinicaltrials.gov
E.Z. and D.S. contributed equally.
References
- 1. Jia G, Hill MA, Sowers JR. Diabetic cardiomyopathy: an update of mechanisms contributing to this clinical entity. Circ Res 2018;122:624–638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Scheiber D, Jelenik T, Zweck E, et al. High-resolution respirometry in human endomyocardial biopsies shows reduced ventricular oxidative capacity related to heart failure. Exp Mol Med 2019;51:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jelenik T, Flögel U, Álvarez-Hernández E, et al. Insulin resistance and vulnerability to cardiac ischemia. Diabetes 2018;67:2695–2702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Marfella R, Amarelli C, Cacciatore F, et al. Lipid accumulation in hearts transplanted from nondiabetic donors to diabetic recipients. J Am Coll Cardiol 2020;75:1249–1262 [DOI] [PubMed] [Google Scholar]
- 5. Roden M, Shulman GI. The integrative biology of type 2 diabetes. Nature 2019;576:51–60 [DOI] [PubMed] [Google Scholar]