Abstract
Early COVID-19-targeted legislations reduced public activity and elective surgery such that local neurosurgical care greatly focused on emergent needs. This study examines neurosurgical trauma patients’ dispositions through two neighboring trauma centers to inform resource allocation. We conducted a retrospective review of the trauma registries for two Level 1 Trauma Centers in Santa Clara County, one academic and one community center, between February 1st and April 15th, 2018–2020. Events before a quarantine, implemented on March 16th, 2020, and events from 2018 to 19 were used for reference. Encounters were characterized by injuries, services, procedures, and disposition. Categorical variables were analyzed by the χ2 test, proportions of variables by z-score test, and non-parametric variables by Fisher’s exact test. A total of 1,336 traumas were identified, with 31% from the academic center and 69% from the community center. During the post-policy period, relative to matching periods in years prior, there was a decrease in number of TBI and spinal fractures (24% versus 41%, p < 0.001) and neurosurgical consults (27% versus 39%, p < 0.003), but not in number of neurosurgical admissions or procedures. There were no changes in frequency of neurosurgery consults among total traumas, patients triaged to critical care services, or patients discharged to temporary rehabilitation services. Neurosurgical services were similarly rendered between the academic and community hospitals. This study describes neurosurgical trauma management in a suburban healthcare network immediately following restrictive quarantine during a moderate COVID-19 outbreak. Our data shows that neurosurgery remains a resource-intensive subspeciality, even during restrictive periods when overall trauma volume is decreased.
Abbreviations: ICU, intensive care unit; LOS, length of stay; SIP, Shelter-in-Place; TBI, traumatic brain injury
Keywords: COVID-19, Healthcare systems, Neurosurgery, Quarantine, Trauma
1. Introduction
The severe acute respiratory syndrome coronavirus 2 induced disease, COVID-19, introduced public health policy changes that acutely demanded triage of healthcare resources. For many procedural specialties, including neurosurgery, many elective surgeries were temporarily halted in order to preserve intensive care occupancies and limit community exposures.[1], [2], [3], [4], [5] In addition, legislations requesting for individual quarantines created an additional psychosocial barrier for potential patients seeking medical care.[6] Although decreased volume has been consistently reported, the interaction between neighboring trauma centers, one private and the other public, and their neurotrauma services has not been described.
Santa Clara County represents an important case study to evaluate the impact of COVID-19 on neurosurgical trauma. The area was among the first to be impacted by the virus within the United States, leading to a strict adjustment in healthcare practices.[7] Moreover, the county is home to two neighboring Level 1 Trauma centers: one academic medical center and one community hospital. They are two of five hospitals servicing the Northern California region. During the early pandemic, both hospitals managed moderate COVID-19 infection rates that did not warrant surge team activations.
As traumas are primarily unforeseeable events, they have been previously reported as among the least affected components of neurosurgical care during the pandemic.[5] We evaluated local neurosurgical trauma as one measure of healthcare resource utilization and availability. Specifically, we hypothesized that the conservative solicitation and provision of healthcare during the early pandemic could lead to sequentially related changes in hospital selection, in inpatient triage, and in disposition services.
2. Methods
An IRB-approved retrospective chart review was performed at Stanford Hospital and Santa Clara Valley Medical Center within the Trauma Registry between February 1st to April 15th for the years of 2018–2020. March 16th, 2020 was demarcated as the start point for the shelter-in-place order based on a local government mandate. Thus, pre-policy included the 6-week period between February 1st to March 15. Post-policy included the 1-month period between March 16th to April 15th. Patients treated in the years of 2018 and 2019 were used for comparison to those treated in 2020 for both pre- and post-policy implementations.
The parent cohort included all patients admitted for any trauma at either institution. Deidentified records of each individual trauma reported patient age, emergency department (ED) disposition, admitting service, consulting services, trauma registry codified injuries, associated procedures, length of stays, and hospital disposition. Subgroup analyses were performed on patients with history of neurosurgical involvement based on documentation of traumatic brain injury (TBI) and/or spinal fractures, neurosurgical consults, neurosurgical procedures, and neurosurgical admissions.
ED dispositions were grouped to reflect severity of receiving units. Admission to further critical care services was defined as treatment in the intensive care unit (ICU), pediatric ICU, operating room, pediatric operating room, or death. Admission to stable care was defined as management taking place on a telemetry/stepdown unit, an adult or pediatric floor unit, or an observation unit. Patients could also have been directly admitted or discharged to home, although due to low sample sizes, these were not included in further subgroup analyses.
Hospital discharges were also grouped to reflect severity of receiving facility. Post-hospitalization disposition to transitional rehabilitation services was defined as further recovery with acute care centers, inpatient rehabilitation, and skilled nursing facilities. Post-hospitalization disposition to further serious needs was defined as further management at long-term care hospitals, hospice, or death. Disposition to home included both discharge to home, with or without home health services. Patients who left against medical advice, were incarcerated, discharged to psychiatric units, or discharged without further specification were not further analyzed as subgroups.
2.1. Statistics
Categorical variables were analyzed by the χ2 test; proportions of variables were analyzed by z-score test; comparisons of means were analyzed by two-factor ANOVA; and non-parametric continuous variables were analyzed by Fisher’s exact test. The significance level was set at a two-sided alpha of 0.05. To limit multiple testing, triage to stable care services and to post-hospitalization serious needs were not specifically assessed given their inverse relationships with triage to critical care services and post-hospitalization transitional rehabilitation services. Analyses were produced with Microsoft Excel (Redmond, Washington) and IBM SPSS Statistics (Chicago, Illinois).
3. Results
3.1. Patient census
A total of 1,336 traumas were identified during the study period, with 420 (31%) events from the academic center and 916 (69%) from the community center (Supplementary Table 1). During the 6 weeks prior to the shelter-in-place legislation (February 1st to March 15th), there were 291, 270 and 293 trauma admissions for 2018, 2019, and 2020. Conversely, during the 1 month following the legislation (March 16th to April 15th), there were 197, 179, and 106 total trauma admissions. During the post-policy period, there was a statistically significant decrease in total number of TBI and spinal fractures (p < 0.001) in the combined census of the two trauma centers.
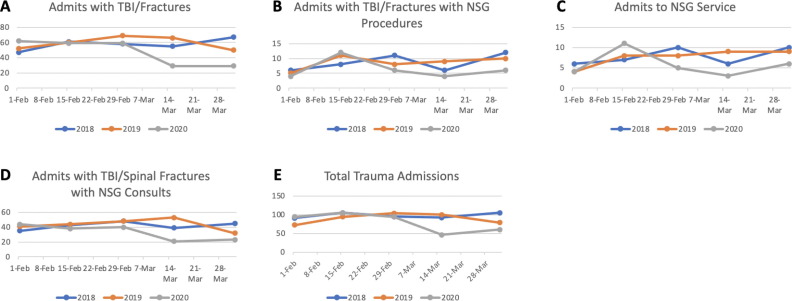
The proportion of total TBI and spinal fractures encountered within the post-policy period of 2020, as compared to the matching period of 2018–19, significantly decreased to 24% (58/238) from 41% (238/585; p < 0.001), and neurosurgical consults decreased to 27% (44/166) from 39% (169/428, p = 0.003, Table 1 , Fig. 1 ). For context, total trauma admissions also significantly decreased to 27% (106/399) in the 2020 post-policy period from 40% (376/937, p < 0.001) in the same time frame in 2018–19.
Table 1.
Comparison of the combined neurosurgical trauma services at SCVMC and SHC between historic (2018 + 2019) and 2020 censuses.
| Pre-SIP | Post-SIP | Test Statistic | p-value | |
|---|---|---|---|---|
| TBI/Fractures | 19.6 | <0.001 | ||
| Historic | 347 | 238 | ||
| Current | 180 | 58 | ||
| NSG Procedure | 1.35 | 0.250 | ||
| Historic | 49 | 37 | ||
| Current | 22 | 10 | ||
| NSG Consults | 8.76 | 0.003 | ||
| Historic | 259 | 169 | ||
| Current | 122 | 44 | ||
| NSG Admits | – | 0.700 | ||
| Historic | 11 | 7 | ||
| Current | 7 | 3 | ||
| Trauma Admits | 22.32 | <0.001 | ||
| Historic | 561 | 376 | ||
| Current | 293 | 106 |
NSG, neurosurgery; SIP = Shelter-in-Place; TBI, traumatic brain injury; - = Fisher’s Exact Test.
Fig. 1.
Line graphs of the combined patient census for Stanford Hospital and Santa Clara Valley Medical Centers in the weeks before and after quarantine implementation. Plots depict number of traumas with A) TBI or spinal fractures B) neurosurgical procedures C) admission to the neurosurgery service and D) neurosurgery consults. Plot E) depicting total traumas. ED, emergency department; NSG, neurosurgery.
However, neurosurgical procedures (31% [10/32] versus 43% [37/86], p = 0.25) and admissions to the neurosurgical service (30% [3/10] versus 39% [7/18], p = 0.70) were not statistically decreased in the post-policy period of 2020 relative to that in 2018–19.
We further evaluated if the policy effects had treatment center-specific effects. TBI and spinal fracture events, neurosurgery procedures, neurosurgical consults, admissions, and total traumas were statistically similar between the academic and county centers (Table 2 , Fig. 1).
Table 2.
Comparison of the neurosurgical trauma services between SCVMC and SHC, before and after the shelter-in-place policy of 2020.
| Pre-SIP | Post-SIP | Test Statistic | p-value | |
|---|---|---|---|---|
| TBI/Fractures | 0.184 | 0.668 | ||
| SHC | 102 | 31 | ||
| SCVMC | 78 | 27 | ||
| NSG Procedure | – | 1 | ||
| SHC | 15 | 7 | ||
| SCVMC | 7 | 3 | ||
| NSG Consults | 0.372 | 0.542 | ||
| SHC | 60 | 24 | ||
| SCVMC | 62 | 20 | ||
| NSG Admits | – | 1 | ||
| SHC | 7 | 3 | ||
| SCVMC | 0 | 0 | ||
| Trauma Admits | 1.09 | 0.297 | ||
| SHC | 102 | 31 | ||
| SCVMC | 191 | 75 |
SIP = Shelter-in-Place; SHC, Stanford Hospital; SCVMC, Santa Clara Valley Medical Center; TBI, traumatic brain injury; - = Fisher’s Exact Test.
3.2. Pediatric analysis
A subgroup analysis to evaluate the pediatric population was additionally performed. During the 6 weeks prior to the shelter-in-place legislation there were 52, 34 and 35 pediatric trauma admissions for 2018, 2019, and 2020 (Supplementary Table 2). For comparison, during the 1 month following the legislation, there were 41, 26, and 8 pediatric trauma admissions, respectively. Thus, the pediatric population was also with a statistically significant decrease in the total traumas (Supplementary Table 3). However, when neurosurgical involvement was assessed, no significant associations between the policy period and number of TBI or fractures, procedures, consults, or admits was identified.
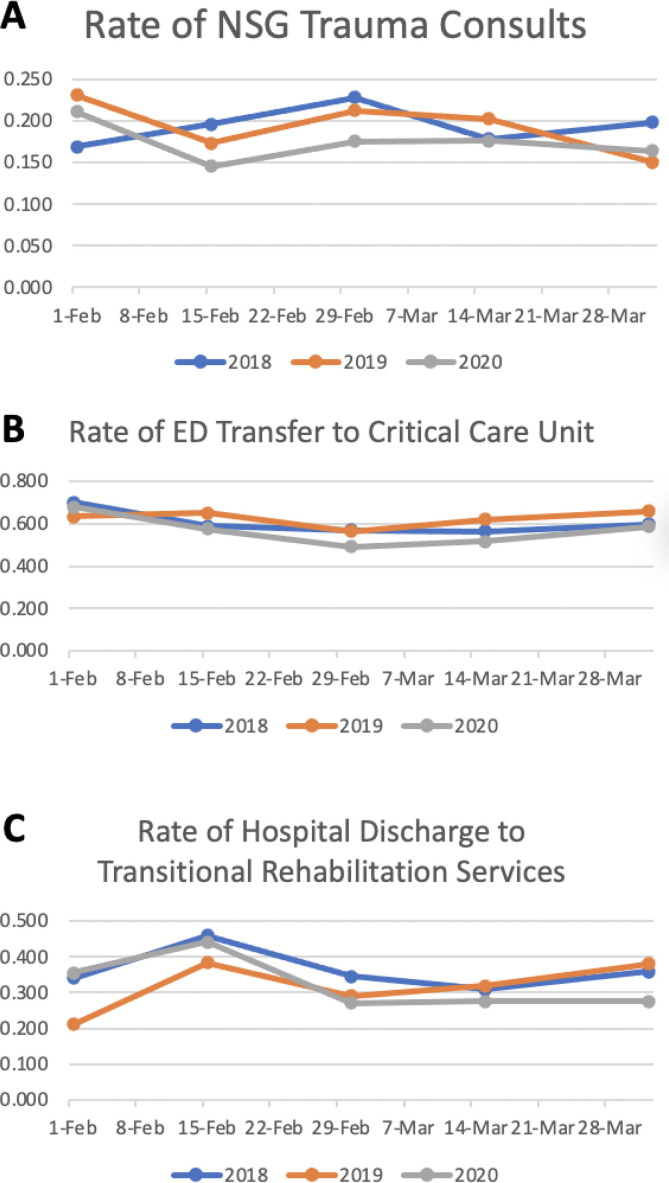
3.3. Hospital management
Rate of neurosurgical involvement was assessed by proportion of overall trauma admissions that merited neurosurgical involvement. Neurosurgery consults were requested for 17.0% (64/377) of all traumas across the two hospital systems following the policy, which was statistically similar to the matching period in 2018–19 (18.3%; 263/1435, p = 0.583, Table 3 , Fig. 2 ). There was also no significant change in the proportion of neurosurgical consults following the policy implementation between hospital systems (Table 4 ).
Table 3.
Comparison of frequencies of neurosurgical trauma consults and patient dispositions at SCVMC and SHC between historic (2018 + 2019) and 2020 censuses.
| Pre-SIP | Post-SIP | Test Statistic | p-value | |
|---|---|---|---|---|
| Consult | ||||
| Historic | 0.200 | 0.183 | 0.149 – pre-SIP | |
| Current | 0.176 | 0.170 | 0.583 – post-SIP | |
| Emergency Department to Critical Care Service | ||||
| Historic | 0.614 | 0.609 | 0.669 – pre-SIP | |
| Current | 0.583 | 0.552 | 0.612-post-SIP | |
| Hospital to Transitional Rehabilitation | ||||
| Historic | 0.340 | 0.340 | 0.774 – pre-SIP | |
| Current | 0.356 | 0.276 | 0.442 – post-SIP | |
| Length of Stay (days) | ||||
| Historic | 5.9 | 8.4 | 0.01 – Historic | |
| Current | 6.9 | 4.9 | 0.25 – Current | |
| 0.41 – Overall model | ||||
SIP = Shelter-in-Place
Fig. 2.
Line graphs of the frequencies at which A) trauma patients were consulted by the neurosurgery service, B) neurosurgical traumas were admitted to a critical care service line after the emergency department evaluation and C) neurosurgical traumas were discharged to a temporary rehabilitation services after hospitalization. ED, emergency department; NSG, neurosurgery.
Table 4.
Comparison of frequencies of neurosurgical trauma consults and patient dispositions between SCVMC and SHC, before and after the shelter-in-place policy of 2020.
| Pre-SIP | Post-SIP | Test Statistic | p-value | |
|---|---|---|---|---|
| Consult | ||||
| SCVMC | 0.178 | 0.144 | 0.249 – SCVMC | |
| SHC | 0.173 | 0.240 | 0.173 – SHC | |
| Emergency Department to Critical Care Service | ||||
| SCVMC | 0.641 | 0.593 | 0.784 – SCVMC | |
| SHC | 0.539 | 0.516 | 0.878 - SHC | |
| Hospital to Transitional Rehabilitation | ||||
| SCVMC | 0.321 | 0.296 | 0.846 – SCVMC | |
| SHC | 0.382 | 0.258 | 0.308 - SHC | |
| Length of Stay (days) | ||||
| SCVMC | 7.3 | 5.1 | ||
| SHC | 6.6 | 4.7 | ||
| 0.92 – Overall model | ||||
For comparison, the ED disposition of trauma patients was also examined. The frequency of occurrence did not significantly differ following the policy implementation. The proportion of patients warranting critical care services (55.2% versus 60.9%, p = 0.612, Table 3 , Fig. 2) remained unchanged across pre- and post-policy periods of 2020. Relative ED disposition patterns did not differ between private and public institutions (Table 4).
3.4. Disposition management
The proportion of hospital discharges to transitional care did not show a statistically significant change between pre- and post-policy periods in 2020 (27.6% [16/58] versus 34.0% [81/238], p = 0.442, Table 3, Fig. 2). There was no difference in these hospital disposition patterns between institutions.
Finally, length of stay for neurosurgical traumas was also assessed across periods. For ANOVA analysis of the overall model (Year × Policy), there was a significant interaction between year of encounter and policy implementation [overall model: F(3,819) = 2.77, p = 0.041, partial eta2 = 0.01]. The interaction of interest was significant [F(1,819) = 5.1, p = 0.024], such that historical LOS pre-policy was less than post-policy (mean LOS pre = 5.9 days, post = 8.4 days, p = 0.01. Current LOS was not significantly affected by SIP (pre = 6.9 days, post = 4.9 days, p = 0.25).
When two-factor ANOVA was used to examine site effects on LOS pre- and post-policy, the overall model and interaction (Site × Policy) were not significant [overall model: F(3,234) = 0.92, p = 0.43, partial eta2 = 0.012, interaction: F(3,234) = 0.009, p = 0.93, partial eta2 < 0.001].
4. Discussion
There is general consensus that the COVID-19 pandemic contributed to a large decrease in surgical volume, including the subspecialty of neurosurgery.[4], [5], [8], [9], [10] Our analysis uniquely examines how neurosurgical traumas, one of the most preserved components of emergent care, were affected within a local network of providers. We show for two comparable institutions that the decrease in neurosurgical traumas were paralleled by decreases in neurosurgical consults, but not neurosurgical admission or procedures. Despite a fall in activity, there was no change in the proportion of total traumas warranting neurosurgery consultation. Likewise, the frequency by which neurosurgical traumas required inpatient admissions and discharges to transitional rehabilitation centers did not change. Further stratification by treatment site (private versus public institution) did not identify institutional variation in the measures.
4.1. Resource utilization
We described an overall decrease in the quantity of neurosurgical care in post-policy period. Using the historical data from 2018 to 19 to calculate an expected number of cases over the one-month period after policy implementation, there were approximately 32.2% (85.6 expected to 58 actual) fewer TBI or spinal fractures events across the county. This translated to approximately 0.92 fewer TBI or spinal fractures per day. Using the same strategy, this projected downstream losses of 26.1% in consult activity, or approximately 0.52 consult events per day. These values suggest that consult activity did not move in direct parallel with the influx of trauma patients and may have been buffered by other subspecialty activities.
The decreased hospital volume observed in our study has been consistently reported by other neurosurgery services.[4], [5] Saad et al. described the Emory health care system across all its subspecialities, whereby functional procedures experienced an 84% decrease. Trauma procedures were the least affected with a 51% decrease.[5] The authors described a stable consult volume and decreases in neurosurgical admission and procedures. While these were opposite our findings, the difference may be attributed to our specific focus on neurosurgical trauma. Meanwhile, Figueroa et al. performed a targeted analysis of the neurotrauma experience at Jackson Memorial Hospital and similarly described 62% and 84% decreases in events and procedures, respectively.
These calculations illustrate where significant clinical and financial impacts manifest for neurosurgical stewardship in the early phases of a pandemic quarantine. However, not all dimensions of the services are immediately disrupted. Based on our data and the statistically insignificant changes identified for neurosurgical admits and procedures, a county of similar catchment should initially sustain staffing and resourcing. The briefly observed declines in procedures and admits from our experience were within expected variance, relative to months prior. A more sustained quarantine or a more severe local pandemic may introduce greater or sooner shocks to these services.
For the general public, our evidence shows that shelter-in-place policies certainly reduce interactions and are protective of neurotrauma. Conversely, for house staff, these are measurable, lost educational opportunities.[5], [9], [10].
4.2. Severity
The county’s hospital neurosurgical patients did not increase the demand for critical care services. This stability was shared in other experiences. Koester et al. described the pandemic response for the Barrow Neurological Institute, where there was no statistically significant change to frequency of emergent cases from the ED. There were, however, fewer nonurgent ED encounters for backpain and headaches.[9] Likewise the authors noted no differences in admissions to the ICU. From an alternative experience, Luostarinen et al. evaluated the hospital course of TBI and SAH patients during the pandemic and noted unchanged mortality rates.[11]
There are nevertheless consistent reports of a proportionally increased case-mix severity at other institutions and neurosurgical subspecialties. Among cerebrovascular cases, there have reported patient aversion to seeking care for mild strokes, leading to increased rates of large vessel occlusion.[12], [13] However, the inpatient trauma case-mix may depend less on a patients’ past medical histories.[8] Our registry only provides trauma-codified injuries rather than specific individuals’ diagnoses, which would have been important for confirming etiology and triage patterns. For example, moderate traumas traditionally granted more intensive care services during the pre-pandemic period may have been downgraded to preserve ICU capacity post-pandemic.
Additionally, monitoring for pediatric, non-accidental trauma during the COVID-19 pandemic has become an increased priority due to changing childcare options. Sidpra et al. with Great Ormond Street Hospital described a nearly fifteen-fold increase in events relative to historical periods.[14] Kovler et al. with the Johns Hopkins experience also cited an increase in child abuse as a proportion of trauma during the COVID-19 period, relative to control (13% versus 4%).[15] In these series, radiographic evidence of TBI existed in over half of cases. Ultimately, our dataset did not identify suspected child maltreatment or physical abuse by ICD-10 coding, and neurosurgical involvement in pediatric traumas was not statistically changed in the study window, but increased surveillance in all healthcare network should be encouraged during periods of increased domestic stressors.
4.3. Institutional interactions
Most importantly our findings showed the two study centers experienced a comparable decrease in volume and triage practices. This is in contrast to early work by Jean et al. who surveyed neurosurgical practices and reported “for profit” were more likely than “non-profit” hospitals to postpone nonemergent cases.[3]
Jean et al.’s characterization was born out in the severe epidemic region of Veneto, Italy, where volume differences were seen across its six hospital centers.[4] Although not statistically validated, the authors proposed that presence of neuro-ICU and academic practices protected institutions from larger disruptions in neurosurgical activities. In Santa Clara County, the academic center is also with a dedicated neuro-ICU, but the county did not experience as severe an epidemic. Nevertheless, in Veneto, the non-academic hospitals were with the most active emergency services. Future work can explore if community centers respond differently to public health directives in resource-stricken settings.
Finally, we show that frequency of discharges to rehabilitation centers did not change in the pandemic period. Discharge pace may have even accelerated, all while patient acuity remained consistent.[9] Although there was no significant difference in LOS between pre- and post-policy in 2020, there was an increase in LOS for the matching periods in years prior, suggesting that prior seasonal LOS increases were not experienced during COVID-19, perhaps related to accelerated discharges. These findings reinforce the feasibility and preparedness of rehabilitation centers for managing neurosurgical patients during a pandemic.[16], [17] These centers remain essential to durable outcomes as they prevent readmissions and promote hospital bed-availability.[17], [18] In the event that rehabilitation centers are overwhelmed, there is overall consensus that tele-rehabilitation is effective for various surgical specialties, although the literature for neurosurgery has been limited.[19], [20], [21]
4.4. Limitations
This study faces the common limitations of a retrospective review, including limited generalizability and covariate availability. The study population also focused on a specific, suburban region in the United States that did not experience an overwhelmed ICU capacity. The county events did not lead to a healthcare system under maximal strain but provides reassurance that neurosurgical reserves are available in more moderate pandemics. Moreover, this study of two neighboring stakeholders of different management styles, private and public, affirms a balanced undertaking of local neurotrauma.
Severity was also not measured by morbidity but rather staff and service-line utilizations. Thus, additional characterization of individual patient-level severity is limited and likely to differ based on catchment populations. In Figueroa et al. where individual traumas were characterized, there were fewer ground level falls, but more falls from height and a 100% increase in gunshot wounds.[8] Thus, aggregate data may yield a neutral change in total severity. Instead, we focused on neighboring hospitals and patient dispositions to understand neurotrauma care across a local network. Future work can consider wider regional models to account for transfer and referral pattern changes.
5. Conclusion
This study describes neurosurgical trauma management in a suburban healthcare network immediately following restrictive quarantine to manage a moderate COVID-19 outbreak.
The shelter-in-place restrictions in Santa Clara County led to a significant decrease in overall trauma as well neurosurgical trauma. However, despite lower trauma volume, there were not statistically significant decreases in neurosurgery procedures and admissions during the same time. There also remained a consistent need for critical care services related to neurosurgical management. We also did not find any significant differences in neurosurgical practice management between private and public institutions in Santa Clara County. Our data shows that neurosurgery remains a resource intensive subspeciality, even during shelter-in-place quarantine periods when overall trauma volume is decreased. These findings will inform hospital triage and personnel resource allocation in future pandemic responses.
Future work can assess the threshold combination of epidemic duration and severity at which there are statistically significant changes in service acuity and operative volume.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jocn.2021.03.017.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Hassan K., Prescher H., Wang F., Chang D.W., Reid R.R. Evaluating the Effects of COVID-19 on Plastic Surgery Emergencies: Protocols and Analysis From a Level I Trauma Center. Ann Plast Surg. 2020;85:S161–S165. doi: 10.1097/SAP.0000000000002459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zagra L., Faraldi M., Pregliasco F., Vinci A., Lombardi G., Ottaiano I., et al. Changes of clinical activities in an orthopaedic institute in North Italy during the spread of COVID-19 pandemic: a seven-week observational analysis. Int Orthop. 2020;44:1591–1598. doi: 10.1007/s00264-020-04590-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien) 2020;162:1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raneri F., Rustemi O., Zambon G., Moro G.D., Magrini S., Ceccaroni Y., et al. Neurosurgery in times of a pandemic: a survey of neurosurgical services during the COVID-19 outbreak in the Veneto region in Italy. Neurosurgical Focus FOC. 2020;49:E9. doi: 10.3171/2020.9.FOCUS20691. [DOI] [PubMed] [Google Scholar]
- 5.Saad H., Alawieh A., Oyesiku N., Barrow D.L., Olson J. Sheltered Neurosurgery During COVID-19: The Emory Experience. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.08.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doglietto F., Vezzoli M., Biroli A., Saraceno G., Zanin L., Pertichetti M., et al. Anxiety in neurosurgical patients undergoing nonurgent surgery during the COVID-19 pandemic. Neurosurgical Focus FOC. 2020;49:E19. doi: 10.3171/2020.9.FOCUS20681. [DOI] [PubMed] [Google Scholar]
- 7.Forrester J.D., Liou R., Knowlton L.M., Jou R.M., Spain D.A. Impact of shelter-in-place order for COVID-19 on trauma activations: Santa Clara County, California, March 2020. Trauma Surg Acute Care Open. 2020;5 doi: 10.1136/tsaco-2020-000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Figueroa J.M., Boddu J., Kader M., Berry K., Kumar V., Ayala V., et al. The Effects of Lockdown During the SARS-CoV-2 Pandemic on Neuro-Trauma Related Hospital Admissions. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.08.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koester S.W., Catapano J.S., Ma K.L., Kimata A.R., Abbatematteo J.M., Walker C.T., et al. COVID-19 and Neurosurgery Consultation Call Volume at a Single Large Tertiary Center With a Propensity-Adjusted Analysis. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rothrock R.J., Maragkos G.A., Schupper A.J., McNeill I.T., Oermann E.K., Yaeger K.A., et al. By the Numbers Analysis of Effect of COVID-19 on a Neurosurgical Residency at the Epicenter. World Neurosurg. 2020;142:e434–e439. doi: 10.1016/j.wneu.2020.07.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luostarinen T., Virta J., Satopää J., Bäcklund M., Kivisaari R., Korja M., et al. Intensive care of traumatic brain injury and aneurysmal subarachnoid hemorrhage in Helsinki during the Covid-19 pandemic. Acta Neurochir (Wien) 2020;162:2715–2724. doi: 10.1007/s00701-020-04583-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.John S., Hussain S.I., Piechowski-Jozwiak B., Dibu J., Kesav P., Bayrlee A., et al. Clinical characteristics and admission patterns of stroke patients during the COVID 19 pandemic: A single center retrospective, observational study from the Abu Dhabi, United Arab Emirates. Clin Neurol Neurosurg. 2020;199 doi: 10.1016/j.clineuro.2020.106227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siegler J.E., Heslin M.E., Thau L., Smith A., Jovin T.G. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020;29 doi: 10.1016/j.jstrokecerebrovasdis.2020.104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sidpra J., Abomeli D., Hameed B., Baker J., Mankad K. Rise in the incidence of abusive head trauma during the COVID-19 pandemic. Arch Dis Child. 2021;106 doi: 10.1136/archdischild-2020-319872. [DOI] [PubMed] [Google Scholar]
- 15.Kovler M.L., Ziegfeld S., Ryan L.M., Goldstein M.A., Gardner R., Garcia A.V., et al. Increased proportion of physical child abuse injuries at a level I pediatric trauma center during the Covid-19 pandemic. Child Abuse Negl. 2020;104756 doi: 10.1016/j.chiabu.2020.104756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pedersini P., Corbellini C., Villafañe J.H. Italian Physical Therapists' Response to the Novel COVID-19 Emergency. Phys Ther. 2020;100:1049–1051. doi: 10.1093/ptj/pzaa060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wittmeier K., Parsons J., Webber S., Askin N., Salonga A. Operational Considerations for Physical Therapy During COVID-19: A Rapid Review. Phys Ther. 2020;100:1917–1929. doi: 10.1093/ptj/pzaa156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Falvey J.R., Krafft C., Kornetti D. The Essential Role of Home- and Community-Based Physical Therapists During the COVID-19 Pandemic. Phys Ther. 2020;100:1058–1061. doi: 10.1093/ptj/pzaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dorsey E.R., Glidden A.M., Holloway M.R., Birbeck G.L., Schwamm L.H. Teleneurology and mobile technologies: the future of neurological care. Nat Rev Neurol. 2018;14:285–297. doi: 10.1038/nrneurol.2018.31. [DOI] [PubMed] [Google Scholar]
- 20.Fiani B., Siddiqi I., Lee S.C., Dhillon L. Telerehabilitation: Development, Application, and Need for Increased Usage in the COVID-19 Era for Patients with Spinal Pathology. Cureus. 2020;12 doi: 10.7759/cureus.10563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohanty A., Srinivasan V.M., Burkhardt J.-K., Johnson J., Patel A.J., Sheth S.A., et al. Ambulatory neurosurgery in the COVID-19 era: patient and provider satisfaction with telemedicine. Neurosurg Focus FOC. 2020;49:E13. doi: 10.3171/2020.9.FOCUS20596. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.